Abstract
Objective: To observe the therapeutic effect of Compound Xuejie Powder combined with negative pressure wound therapy (NPWT) on diabetic foot ulcers and its influence on the blood flow of the dorsal artery in the foot. Methods: A total of 103 patients with diabetic foot ulcers, admitted to our hospital between February 2021 and March 2023, were included in this study. The control group was given NPWT on the basis of conventional treatment such as controlling blood sugar and blood pressure, anti-infection therapy and improving blood circulation, while the observation group was given Compound Xuejie Powder combined with NPWT on the basis of conventional treatment. The two groups were compared in terms of granulation tissue coverage and thickness, wound healing time, levels of inflammatory factors related to Notch signaling pathway in wound exudation, serum angiogenesis factors, and dorsal foot artery blood flow. Results: Before treatment, there were no significant differences between the two groups in the levels of inflammatory factors related to the Notch signaling pathway in wound exudates or serum angiogenesis factors (all P>0.05). After treatment, vascular endothelial growth factor (VEGF) level increased, while the levels of TNF-α, IL-1β, IL-6, IL-17 and chemoattractant factor (pigment epithelium-derived factor, PEDF) decreased in both groups, an these alterations in the observation group were more pronounced compared to the control group (all P<0.05). There was no significant difference in dorsal foot artery blood flow before treatment (all P>0.05); however, Vm, PI, RI and vascular diameter were notably increased in both groups after the treatment, with more pronounced improvements noticed in the observation group (all P<0.05). The total effective rate, granulation tissue coverage rate, and granulation tissue thickness were significantly higher while wound healing time was significantly shorter in the observation group compared to the control group (all P<0.05). Conclusion: In the treatment of diabetic foot ulcers, Compound Xuejie Powder combined with NPWT can effectively inhibit local inflammation, improve the blood flow of the dorsal foot artery and promote ulcer healing.
Keywords: Compound dried blood powder, negative pressure wound therapy, diabetic foot, ulcer, dorsal foot artery blood flow, local inflammation
Introduction
Diabetic foot ulcer (DFU) is a common chronic complication in diabetic patients, involving both microvascular and neural issues, leading to widespread vascular damage and tissue injury in the foot. The incidence of DFU is as high as 25% [1]. Prolonged hyperglycemia can lead to neuropathy, vascular changes, and immune-metabolic disruptions. These conditions, complicated by factors such as infection, foot trauma, and abnormal foot pressure, can lead to the development of foot ulcers. In severe cases, osteomyelitis and necrosis of foot tissues may occur, sometimes necessitating amputation to preserve life [2].
Negative pressure wound therapy (NPWT) is a commonly used method for treating diabetic foot ulcers. By isolating the wound from the external environment, it prevents the invasion of pathogenic microorganisms and removes wound exudate through negative pressure. This helps alleviate local inflammatory stimuli and promotes granulation tissue growth. However, the overall efficacy NPWT alone is not always satisfactory [3].
According to traditional Chinese medicine (TCM) theory, diabetic foot ulcers fall into the categories of “collateral disease” and “Bi syndrome”. Prolonged consumption of body fluids due to diabetes can lead to yin depletion, excessive yangming dryness, impaired blood vessels, and local stagnation of qi and blood, causing stasis and heat obstruction in the vessels. This leads to malnourishment of the tissues and eventual decay of the flesh into pus. The treatment principle involves promoting blood circulation, resolving stasis, and removing necrotic tissue to stimulate the generation of new tissue [4].
The compound blood-stanching powder used in this study is a formula composed of danggui (Angelica sinensis), zicao (Arnebia euchroma), xuejie (Sanguis Draconis), sanqi (Panax notoginseng), jinyinhua (Lonicera japonica), lianqiao (Forsythia suspensa), and gancao (Glycyrrhiza uralensis). This formula is known for its efficacy in promoting blood circulation, resolving stasis, and promoting tissue regeneration, showing good results in ulcerative conditions [5]. This study aims to observe the therapeutic effects of the Compound Xuejie Powder combined with NPWT on diabetic foot ulcers and its impact on dorsalis pedis arterial blood flow.
Materials and methods
Participants
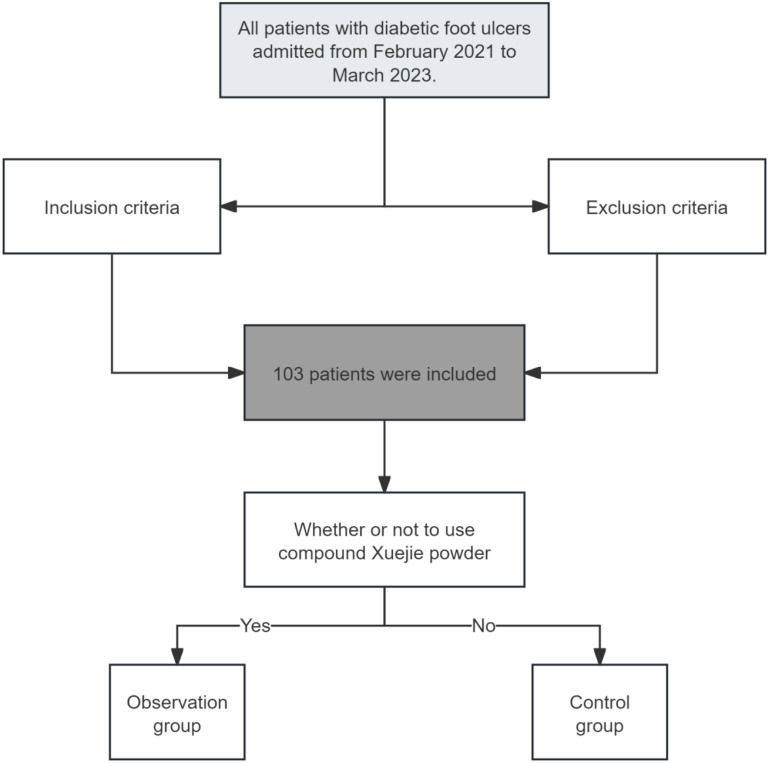
This retrospective study included 103 patients with diabetic foot ulcers treated in our hospital between February 2021 and March 2023. The study flow chart is shown in Figure 1. Inclusion criteria: 1. Meeting the criteria in the “Chinese Guidelines for Diagnosis and Treatment of Diabetic Foot (2019)” [6], including diabetes, skin ulceration, and the presence of neuropathy and/or vascular lesions; 2. Diagnosis of blood stasis obstruction syndrome according to the “Diagnostic and Therapeutic Efficacy Criteria for TCM Diseases” [7], characterized by a purple and dark tongue, stasis spots, minimal or peeled coating, and deep or hesitant pulse. Clinical symptoms included non-healing wounds, persistent necrotic tissue, numbness and coldness in the lower limbs, dark and dull skin, fatigue, drowsiness, and headaches; 3. Adults up to 75 years of age; 4. Wagner classification of 2-4; 5. Ulcer area ≤30 cm [2]; 6. Availability of complete medical history records at the hospital.
Figure 1.
Flow chart of patient enrollment.
Exclusion criteria: 1. Presence of hereditary or infectious diseases; 2. Complications with acute diabetic conditions; 3. An ankle/brachial index (ABI) <0.4; 4. History of radiation exposure, steroid use, chemotherapy, or immunosuppressant use within the last 12 weeks; 5. Ulcers of cancerous, tuberculous, or radiation-induced origin; 6. Allergy to the powder; 7. Presence of other severe systemic diseases that could affect study outcomes.
Treatments
The control group received routine treatment, including blood sugar and blood pressure management, anti-infection measures, and improvement of blood circulation. In addition, negative pressure materials (Wuhan Weisdi Medical Technology Co., Ltd., Wuhan, China) were applied to the wound surface after complete debridement. The material was completely sealed with a semi-permeable membrane and connected to a negative pressure suction device, with the pressure set between -60 to -50 kPa. Under normal circumstances, the negative pressure material was changed every 7 days. If air leakage, bulging, or excessive accumulation of secretions under the film was observed, immediate replacement was performed.
The observation group received Compound Xuejie Powder in addition to the routine treatment and NPWT. After each debridement, the TCM preparation was topically applied. The herbs, consisting of 10 g of Angelica sinensis, 6 g of Lithospermum erythrorhizon, 1 g of Sanguis draconis, 3 g of Panax notoginseng, 10 g of Lonicera japonica, 10 g of Forsythia suspensa, and 6 g of Glycyrrhiza uralensis, were powdered and sieved through a 60-mesh sieve. It was then mixed with sterilized sesame oil to form a paste, which was applied to the wound surface covered with sterile gauze. After 8 hours of external application, the wound was rinsed with normal saline, followed by negative pressure therapy. The efficacy of both groups was evaluated after 4 weeks of treatment.
Detection and efficacy criteria
Before and after treatment, wound exudate from both groups of patients was collected. Enzyme-linked immunosorbent assay (ELISA) was employed to detect the levels of Notch signaling-related inflammatory factors TNF-α, IL-1β, IL-6, IL-17, as well as VEGF and pigment epithelium-derived f actor (PEDF) in the wound exudate. The reagent kit used was from Shanghai Enzyme-linked Biotechnology Co., Ltd. (Shanghai, China), and the instrument used was the MK3 enzyme marker from Thermo Fisher Scientific (Waltham, MA, USA).
Before treatment and after 4 weeks of treatment, a Hitachi Aloka HIVISION Preirus color Doppler ultrasound diagnostic instrument was used to measure the blood flow parameters, mean velocity (Vm), pulsatility index (PI), resistive index (RI), and vessel diameter, of the dorsalis pedis artery on the affected side in both groups. The probe frequency was set at 5-18 MHz. After being coated with an appropriate amount of coupling agent, the probe was placed on the dorsalis pedis artery on the affected side, and the sampling line was angled at less than 60° to the direction of blood flow. Measurements were taken continuously for 3 cardiac cycles, and the average value was recorded.
Efficacy criteria were established based on the “Diagnostic and Therapeutic Efficacy Criteria of Traditional Chinese Medicine [7]” and the “Chinese Expert Consensus on the Prevention and Treatment of Diabetic Foot with Traditional Chinese and Western Medicine (1st Edition) [8]”. Cure: complete healing of ulcers and a reduction of ≥90% in TCM syndrome scores; Significant effectiveness: a reduction of ≥70% in ulcer size and a reduction of ≥70% and <90% in TCM syndrome scores; Effectiveness: a reduction of ≥30% and <70% in ulcer size and a reduction of ≥30% and <70% in TCM syndrome scores; Ineffectiveness: both criteria showing reductions of <30%. Total effective = (cases of cure + significant effectiveness + effectiveness)/total cases *100%.
The primary outcome was the treatment effectiveness represented by rate of wound healing. Secondary outcomes included granulation tissue coverage and thickness, inflammatory markers, angiogenesis factors, and blood flow parameters of the dorsal foot artery.
Statistical analysis
Statistic Package for Social Science (SPSS) 26.0 (IBM, Armonk, NY, USA) was used for data analysis. The data were confirmed to follow a normal distribution and meet the assumption of homogeneity of variance, such as dorsalis pedis artery blood flow, Notch signaling-related inflammatory factors in wound exudate, which were represented as (mean ± standard deviation). Independent sample t-tests were used for comparisons between the two groups. Descriptions in terms of counts (Wagner grades, duration, etc.) were presented as n (%), and the chi-square test was used for comparisons. The significance level was set at α=0.05.
Results
Comparison of baseline information between the two groups of patients
There was no significant difference between the two groups in terms of gender, age, body mass index, course of diabetes, course of diabetic foot, and Wagner grade (all P>0.05, Table 1).
Table 1.
Compares the general information between the two groups
| General information | Control group (n=51) | Observation group (n=52) | χ2/t | P |
|---|---|---|---|---|
| Gender (n) | 0.140 | 0.708 | ||
| Male | 30 (58.82) | 28 (53.85) | ||
| Female | 21 (41.18) | 24 (46.15) | ||
| Age (years) | 64.20±7.47 | 64.46±8.02 | 0.170 | 0.865 |
| Body mass index (kg/m2) | 25.17±1.53 | 25.06±1.51 | 0.367 | 0.714 |
| Course of diabetes (n) | 0.290 | 0.962 | ||
| <10 years | 14 (27.45) | 16 (30.77) | ||
| 10-15 years | 21 (41.18) | 22 (42.31) | ||
| 15-20 years | 10 (19.61) | 9 (17.31) | ||
| >20 years | 6 (11.76) | 5 (9.62) | ||
| Course of Diabetic Foot (n) | 0.849 | 0.838 | ||
| <3 months | 18 (35.29) | 16 (30.77) | ||
| 3-6 months | 16 (31.37) | 20 (38.46) | ||
| 6-9 months | 14 (27.45) | 12 (23.08) | ||
| >9 months | 3 (5.88) | 4 (7.69) | ||
| Wagner grade (n) | 0.372 | 0.830 | ||
| Level 2 | 21 (41.18) | 24 (46.15) | ||
| Level 3 | 18 (35.29) | 18 (34.62) | ||
| Level 4 | 12 (23.53) | 10 (19.23) |
Comparison of Notch signaling-related inflammatory factors in wound exudate between the two groups
There was no significant difference in the level of Notch signaling-related inflammatory factors in wound exudate between the two groups before treatment (P>0.05). However, the levels of TNF-α, IL-1β, IL-6, and IL-17 decreased in both groups after treatment, and these levels in the observation group were significantly lower than those in the control group (all P<0.05), as shown in Table 2.
Table 2.
Comparison of Notch signaling related inflammatory factor levels in wound exudates between the two groups (x̅±s)
| Group | TNF-α (ng/L) | IL-1β (µg/L) | IL-6 (pg/mL) | IL-17 (ng/L) | ||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| Pre-treatment | Post-treatment | Pre-treatment | Post-treatment | Pre-treatment | Post-treatment | Pre-treatment | Post-treatment | |
| Control group | 24.95±2.98 | 15.87±2.42* | 25.56±5.80 | 16.22±3.42* | 18.56±3.56 | 9.21±1.74* | 16.58±3.79 | 12.78±2.06* |
| Observation group | 25.01±3.23 | 7.96±1.87* | 25.17±5.36 | 9.78±2.04* | 18.77±3.28 | 4.58±0.91* | 16.51±3.86 | 9.55±1.47* |
| t | 0.098 | 18.583 | 0.355 | 11.632 | 0.311 | 16.968 | 0.093 | 9.174 |
| P | 0.922 | 0.000 | 0.724 | 0.000 | 0.756 | 0.000 | 0.926 | 0.000 |
P<0.05, compare with pretreatment level.
Comparison of serum angiogenic factors between the two groups
Before treatment, there was no significant difference in serum angiogenic factors between the two groups (P>0.05). However, the serum levels of VEGF increased, while PEDF decreased in both groups after treatment, and the observation group showed notably higher VEGF levels and lower PEDF levels compared to the control group (all P<0.05), as shown in Table 3.
Table 3.
Comparison of serum angiogenesis factor levels between the two groups (x̅±s)
| Group | VEGF (ng/L) | PEDF (mg/L) | ||
|---|---|---|---|---|
|
|
|
|||
| Pre-treatment | Post-treatment | Pre-treatment | Post-treatment | |
| Control group | 58.99±10.14 | 77.25±11.63* | 6.89±1.12 | 4.25±0.78* |
| Observation group | 60.10±10.47 | 89.25±12.75* | 6.93±1.08 | 3.07±0.61* |
| t | 0.546 | 4.988 | 0.185 | 8.562 |
| P | 0.586 | 0.000 | 0.854 | 0.000 |
Notes: VEGF: vascular endothelial growth factor, PEDF: pigment epithelium-derived factor;
P<0.05, compare with pretreatment level.
Comparison of dorsalis pedis artery blood flow between the two groups
Before treatment, there was no significant difference in dorsalis pedis artery blood flow between the two groups (P>0.05). However, the parameters including Vm, PI, RI, and vessel diameter all increased in both groups after treatment, and the observation group demonstrated more pronounced improvements compared to the control group (all P<0.05), as shown in Table 4.
Table 4.
Comparison of blood flow parameters of dorsalis pedis artery between the two groups (x̅±s)
| Group | Vm (ml/s) | PI | RI | Blood vessel diameter (mm) | ||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| Pre-treatment | Post-treatment | Pre-treatment | Post-treatment | Pre-treatment | Post-treatment | Pre-treatment | Post-treatment | |
| Control group | 0.78±0.14 | 1.15±0.28* | 1.44±0.32 | 2.32±0.35* | 0.58±0.08 | 0.69±0.10* | 1.42±0.28 | 1.87±0.31* |
| Observation group | 0.80±0.12 | 1.50±0.35* | 1.45±0.30 | 3.94±0.46* | 0.57±0.09 | 0.87±0.12* | 1.40±0.27 | 2.66±0.35* |
| t | 0.779 | 5.597 | 0.164 | 19.920 | 0.596 | 8.262 | 0.369 | 12.118 |
| P | 0.438 | 0.000 | 0.870 | 0.000 | 0.553 | 0.000 | 0.713 | 0.000 |
Notes: Vm: mean velocity, PI: pulsatility index, RI: resistive index;
P<0.05, compare with pretreatment level.
Comparison of treatment efficacy between the two groups
The total effective rate in the observation group was significantly higher than that of the control group (88.46% vs. 72.55%, P<0.05), as shown in Table 5.
Table 5.
Comparison of treatment efficacy between the two groups (n, %)
| Group | Cure | Significant effectiveness | Effectiveness | Ineffectiveness | Total effective rate |
|---|---|---|---|---|---|
| Control group | 13 (25.49) | 14 (27.45) | 10 (19.61) | 14 (27.45) | 37 (72.55) |
| Observation group | 26 (50.00) | 14 (26.92) | 6 (11.54) | 6 (11.54) | 46 (88.46) |
| χ2 | 4.167 | ||||
| P | 0.041 |
Comparison of coverage rate and thickness of granulation tissue and wound healing time between the two groups
The coverage rate and thickness of granulation tissue in the observation group were all significantly higher than those in the control group, while the wound healing time was shorter than that in the control group (all P<0.05), as shown in Table 6.
Table 6.
Comparison of coverage rate and thickness of granulation tissue and wound healing time between the two groups
| Group | Coverage of granulation tissue (%) | Thickness of granulation tissue (mm) | Wound healing time (d) |
|---|---|---|---|
| Control group | 21.85±4.66 | 2.03±0.54 | 36.98±7.14 |
| Observation group | 35.98±5.07 | 3.29±0.67 | 29.73±5.86 |
| t | 14.718 | 10.496 | 5.639 |
| P | 0.000 | 0.000 | 0.000 |
Discussion
A 2021 epidemiological survey revealed that the global diabetic population was approximately 536 million, and it is predicted to be 783 million by 2045. In China, the diabetic population is around 114 million and expected to reach 151 million by 2045 [9]. Among diabetic patients, the incidence of having a diabetic foot is as high as 25%. Without timely intervention, the disability and mortality rates are significant, with an amputation rate exceeding 19.03% [10]. In this study, Compound Xuejie Powder combined with NPWT significantly improved ulcer healing, reduced inflammation, and enhanced blood flow compared to NPWT alone. The mechanism may involve the inhibition of the Notch signaling pathway, promotion of angiogenesis, and suppression of local inflammation. These findings align with previous studies on the benefits of traditional Chinese medicine in chronic wound management.
Western medical treatment for diabetic feet primarily focuses on controlling blood sugar, wound debridement, and conventional therapies. While NPWT has demonstrated effectiveness in preventing infections and reducing inflammation, slow granulation tissue growth and suboptimal outcomes in some patients may lead to tissue necrosis, potentially necessitating amputation [11].
According to TCM theory, diabetic foot ulcers fall under the category of “collateral diseases”, characterized by blood stasis and collateral blockage, resulting in tissue malnutrition. TCM emphasizes the importance of activating blood circulation, resolving stasis, and promoting tissue regeneration. The herbal formula “Compound Xuejie Powder” [12] consists of various herbs, with Xuejie (Sanguis Draconis) as the principal herb. Xuejie is known for its ability to invigorate blood, dispel stasis, and promote tissue regeneration. The combination of Danggui (Chinese Angelica) and Zicao (Purple Gromwell Root) supports blood circulation and nourishes blood and tissues. These herbs collectively work to promote blood circulation, resolve stasis, and facilitate tissue regeneration [13,14]. The efficacy of combining traditional Chinese medicine with NPWT has been demonstrated in previous studies. Liu et al. [15] showed that such combination improved healing outcomes by enhancing blood flow, reducing inflammation, and expediting wound healing. Our study supports these findings by showing that Compound Xuejie Powder combined with NPWT significantly increases VEGF levels while decreasing inflammatory markers such as TNF-α, IL-1β, IL-6, and IL-17.
This study found that the overall effective rate in the observation group was higher than that in the control group. Additionally, the coverage and thickness of granulation tissue in the observation group were superior to those in the control group, and the healing time was shorter [16]. These results suggest that Compound Xuejie Powder combined with NPWT is more effective in treating diabetic foot ulcers, as it promotes granulation tissue growth and accelerates ulcer healing [17]. This may be attributed to the inhibitory effects of Compound Xuejie Powder on pathogenic microorganisms, its anti-inflammatory properties, improvement of blood rheology, inhibition of platelet aggregation, and thrombolytic effects, collectively stimulating capillary dilation and promoting angiogenesis [18,19].
The Notch signaling pathway plays a crucial role in inflammation and cell proliferation during wound healing. Studies have shown that inhibiting the Notch signaling pathway can reduce the expression of inflammatory factors (TNF-α, IL-1β, IL-6, IL-17) and PEDF, while increasing the expression of VEGF, in rat diabetic foot ulcer models [20]. In this study, both groups showed an increase in VEGF and a decrease in TNF-α, IL-1β, IL-6, IL-17, and PEDF after treatment. Furthermore, the observation group exhibited higher VEGF levels and lower levels of Notch-related inflammatory factors and PEDF compared to the control group. This suggests that Compound Xuejie Powder combined with NPWT can inhibit the Notch signaling pathway, alleviate local inflammation, and promote angiogenesis, representing a crucial mechanism in the treatment of diabetic foot ulcers.
Reduced blood flow in the dorsalis pedis artery is a significant pathological mechanism in diabetic feet [21]. Improving foot blood perfusion can enhance nutritional metabolism, facilitate the absorption of inflammatory exudates, and positively impact the patient’s prognosis. This study found that after treatment, blood flow parameters (Vm, PI, RI, and vessel diameter) increased in both groups. Moreover, the observation group showed better dorsalis pedis artery blood flow compared to the control group. This indicates that Compound Xuejie Powder combined with NPWT can effectively improve dorsalis pedis artery blood flow, likely due to its vasodilatory effects and inhibition of microthrombus formation.
In conclusion, Compound Xuejie Powder combined with NPWT for the treatment of diabetic foot ulcers can inhibit local inflammation, improve dorsalis pedis artery blood flow, and promote ulcer healing. This comprehensive approach aligns with TCM principles and offers a promising therapeutic strategy for diabetic foot ulcer management.
Acknowledgements
This work was supported by the Hainan Provincial Natural Science Foundation (822QN463, 822MS174) and Hainan Province Health Industry Research Project (22A200051).
Disclosure of conflict of interest
None.
References
- 1.Sulicka-Grodzicka J, Szczepaniak P, Jozefczuk E, Urbanski K, Siedlinski M, Niewiara Ł, Guzik B, Filip G, Kapelak B, Wierzbicki K, Korkosz M, Guzik TJ, Mikolajczyk TP. Systemic and local vascular inflammation and arterial reactive oxygen species generation in patients with advanced cardiovascular diseases. Front Cardiovasc Med. 2023;10:1230051. doi: 10.3389/fcvm.2023.1230051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sajjadpour Z, Hoseini Tavassol Z, Aghaei Meybodi HR, Eskandarynasab M, Pejman Sani M, Hasani-Ranjbar S, Larijani B. Evaluating the effectiveness of melatonin in reducing the risk of foot ulcers in diabetic patients. J Diabetes Metab Disord. 2023;22:1073–1082. doi: 10.1007/s40200-023-01289-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tazerouni H, Labbani-Motlagh Z, Amini S, Shahrami B, Sajjadi-Jazi SM, Afhami S, Gholami K, Sadeghi K. Population pharmacokinetics of vancomycin in patients with diabetic foot infection: a comparison of five models. J Diabetes Metab Disord. 2023;22:1385–1390. doi: 10.1007/s40200-023-01259-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Varughese R, H V S, K O S, Mathew M. Prescription auditing and assessment of medication adherence patterns in patients with diabetic foot ulcer. J Diabetes Metab Disord. 2023;22:1255–1261. doi: 10.1007/s40200-023-01241-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cai X, Yang R, Shi W, Cai Y, Ma Z. Exploration of the common pathogenic link between COVID-19 and diabetic foot ulcers: an in silico approach. Health Sci Rep. 2023;6:e1686. doi: 10.1002/hsr2.1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sexton FC, Soh V, Yahya MS, Healy DA. Effectiveness of negative-pressure wound therapy to standard therapy in the prevention of complications after vascular surgery. Minerva Surg. 2024;79:48–58. doi: 10.23736/S2724-5691.23.10096-7. [DOI] [PubMed] [Google Scholar]
- 7.Armstrong DG, Tan TW, Boulton AJM, Bus SA. Diabetic foot ulcers: a review. JAMA. 2023;330:62–75. doi: 10.1001/jama.2023.10578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reardon R, Simring D, Kim B, Mortensen J, Williams D, Leslie A. The diabetic foot ulcer. Aust J Gen Pract. 2020;49:250–255. doi: 10.31128/AJGP-11-19-5161. [DOI] [PubMed] [Google Scholar]
- 9.Baucom MR, Wallen TE, Youngs J, Singer KE, Delman AM, Schuster RM, Blakeman TC, Strilka R, Pritts TA, Goodman MD. Effectiveness of negative pressure wound therapy during aeromedical evacuation following soft tissue injury and infection. Mil Med. 2023;188:295–303. doi: 10.1093/milmed/usad113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Karakousis ND, Pyrgioti EE, Georgakopoulos PN, Apergi K, Popovic DS, Papanas N. Zinc levels and diabetic foot ulcers: a mini review. Int J Low Extrem Wounds. 2023 doi: 10.1177/15347346231214209. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 11.Zhao F, Xie L, Weng Z, Huang Y, Zheng L, Yan S, Shen X. Combined with dynamic serum proteomics and clinical follow-up to screen the serum proteins to promote the healing of diabetic foot ulcer. Endocrine. 2024;84:365–379. doi: 10.1007/s12020-023-03579-1. [DOI] [PubMed] [Google Scholar]
- 12.Souza CF, Borges LB, Oliveira FRMB, Silva PCS, Patricio DO, Rosales TO, Souza NF, Spiller F, Mansur DS, Assreuy J, Sordi R. Cannabinoid CB2 receptor agonist reduces local and systemic inflammation associated with pneumonia-induced sepsis in mice. Eur J Pharmacol. 2023;959:176092. doi: 10.1016/j.ejphar.2023.176092. [DOI] [PubMed] [Google Scholar]
- 13.Ferhaoui N, Tanaka R, Sekizuka T, Kuroda M, Sebaihia M. Whole genome sequencing and pan-genome analysis of Staphylococcus/Mammaliicoccus spp. isolated from diabetic foot ulcers and contralateral healthy skin of Algerian patients. BMC Microbiol. 2023;23:342. doi: 10.1186/s12866-023-03087-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu S, Xu Y, Guo L, Jiang X. A meta-analysis of the effectiveness of antibacterial bone cement in the treatment of diabetic foot skin wound infections. Int Wound J. 2024;21:e14487. doi: 10.1111/iwj.14487. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 15.Mohseni S, Aalaa M, Atlasi R, Mohajeri Tehrani MR, Sanjari M, Amini MR. The effectiveness of negative pressure wound therapy as a novel management of diabetic foot ulcers: an overview of systematic reviews. J Diabetes Metab Disord. 2019;18:625–641. doi: 10.1007/s40200-019-00447-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee JY, Kim S, Sohn HJ, Kim CH, Kim TG, Lee HS. Local myeloid-derived suppressor cells impair progression of experimental autoimmune uveitis by alleviating oxidative stress and inflammation. Invest Ophthalmol Vis Sci. 2023;64:39. doi: 10.1167/iovs.64.13.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sashide Y, Toyota R, Takeda M. Local administration of the phytochemical, quercetin, attenuates the hyperexcitability of rat nociceptive primary sensory neurons following inflammation comparable to lidocaine. J Pain. 2024;25:755–765. doi: 10.1016/j.jpain.2023.10.004. [DOI] [PubMed] [Google Scholar]
- 18.Andriankaja OM, Adatorwovor R, Kantarci A, Hasturk H, Shaddox L, Levine MA. Periodontal disease, local and systemic inflammation in puerto ricans with type 2 diabetes mellitus. Biomedicines. 2023;11:2770. doi: 10.3390/biomedicines11102770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Widigdo DAM, Sofro ZM, Pangastuti HS, Dachlan I. The efficacy of negative pressure wound therapy (NPWT) on healing of diabetic foot ulcers: a literature review. Curr Diabetes Rev. 2024;20:1–11. doi: 10.2174/0115733998229877230926073555. [DOI] [PubMed] [Google Scholar]
- 20.Imcha M, Liew NC, McNally A, Zibar D, O’Riordan M, Currie A, Styche T, Hughes J, Whittall C. Single-use negative pressure wound therapy to prevent surgical site complications in high-risk patients undergoing caesarean sections: a real-world study. Int J Qual Health Care. 2023;35:mzad089. doi: 10.1093/intqhc/mzad089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ueda M, Makoto O, Sakai A. Use of a skin-covering pocket as a local flap and negative pressure wound therapy with instillation and dwell time/negative pressure wound therapy for the treatment of diabetic foot ulcer with calcaneal osteomyelitis: a case report. J Am Podiatr Med Assoc. 2023;113:21-061. doi: 10.7547/21-061. [DOI] [PubMed] [Google Scholar]