Abstract
Objective: To compare the clinical efficacy of arthroscopic outside-in suturing and all-inside suturing in the treatment of discoid lateral meniscus (DLM) injury, and to analyze the influencing factors for clinical efficacy. Methods: We retrospectively selected 30 patients with DLM injury who received arthroscopic all-inside suturing at Wuzhou Workers’ Hospital from January 2020 to December 2022 as the observation group. Another 30 patients who received arthroscopic outside-in suturing during the same period were enrolled as the control group. The surgical indicators, pre- and post-operative knee scores and proprioception difference of knee joint, postoperative complications and clinical efficacy were compared between the two groups. Factors affecting clinical efficacy of patients with DLM injury were identified using Logistic regression analysis. Results: Significant differences were observed in operation time, hospital stay, blood loss and clinical efficacy between the two groups (all P<0.05); however, there was no significant difference in complications (P>0.05). The visual analog score (VAS) scores of both groups decreased over time at 1, 3, 5, 7, 15, and 30 days post-surgery, with the observation group scoring lower than the control group (all P<0.05). At 1, 3, and 6 months after the surgery, the international knee documentation committee (IKDC), Lysholm, and Tegner scores of both groups increased over time, with the observation group scoring higher than the control group (all P<0.05). Six months post-surgery, proprioception differences at 15°, 45°, and 75° of knee flexion were significantly decreased, with greater improvements observed in the observation group (P<0.05). Univariate analysis showed that operation time, IKDC and Lysholm scores at 6 months post-operation, postoperative complications, and suture method were factors influencing treatment outcomes in patients with DLM injury (all P<0.05). Multivariate Logistic regression analysis identified postoperative complications as an independent risk factor for poor treatment outcome in patients with DLM injury (P<0.05). Conclusion: Arthroscopic all-inside suturing for DLM injury offers significant clinical benefits, including shorter operation time and hospital stay, less blood loss, and improved knee joint function with fewer complications. Prolonged operation time, low IKDC and Lysholm scores at 6 months post-operation, postoperative complications and outside-in suturing technique are associated with poorer treatment outcomes in patients with DLM injury.
Keywords: Discoid meniscus injury, outside-in suture method, all-inside suture method, arthroscopy, clinical efficacy
Introduction
The meniscus is composed of fibrocartilage, which is crucial for ensuring voluntary the knee joint movement. It protects the articular cartilage, reduces the weight-bearing load of the knee joint, and absorbs shocks during joint movement [1]. Meniscus injuries are common in sports-related knee injuries, often resulting in severe pain, swelling, and noise during knee joint activity. In severe cases, the knee may lock during flexion and extension, preventing normal movement. If left untreated, it can lead to muscle atrophy around the knee joint and increase the risk of arthritis [2]. Discoid lateral meniscus (DLM) injury is a prevalent type of meniscus injury, with a higher incidence than normal meniscus. It has a high incidence in China and is a major focus of clinical attention [3]. Currently, the primary treatment for DLM injury is surgery. Minimally invasive technology is constantly maturing, which promotes the continuous optimization of the treatment plan for DLM injury [4]. Arthroscopic suturing is a common treatment for DLM injury, with the characteristics of minimal trauma, effective healing promotion, and improved patient prognosis. However, choosing the appropriate suture method during arthroscopy remains a significant challenge [5]. Therefore, this study investigated the effects of different suture methods under arthroscopy in the treatment of DLM injury and analyzed the factors affecting the treatment outcomes.
Materials and methods
General information
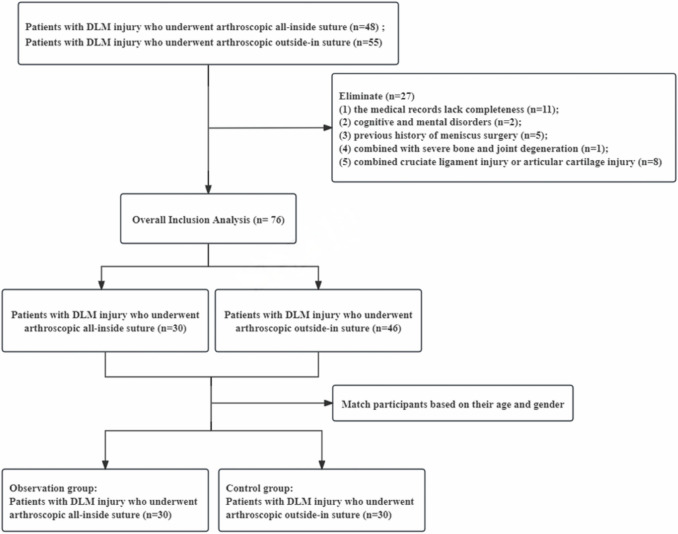
We retrospectively selected 30 patients with DLM injury who underwent arthroscopic surgery with all-inside suturing at Wuzhou Workers’ Hospital from January 2020 to December 2022 as the observation group. Another 30 cases who underwent arthroscopic surgery with outside-in suturing during the same period served as the control group, matched by age and gender (the filtering process is illustrated in Figure 1). This study was approved by the Medical Ethics Committee of Wuzhou Workers’ Hospital.
Figure 1.
Flow chart of case selecting. DLM: discoid lateral meniscus.
Inclusion criteria: Patients meeting the diagnostic criteria for DLM injury with confirmed diagnosis of lateral discoid meniscal injury through imaging [6]; The affected area was tender, and McCauley’s sign was positive; All meniscal tears were lamellar fractures; The tear site was in the white area or the red-white area. Exclusion criteria: Presence with cognitive and mental disorders; Presence of severe bone and joint degeneration; Combined cruciate ligament injury or articular cartilage injury; Previous history of meniscus surgery; Incomplete medical records.
Treatment methods
All patients underwent epidural anesthesia in the supine position. The electric balloon tourniquet was applied, and the injured edge of DLM was refreshed following routine joint exploration and debridement using a 30° arthroscope.
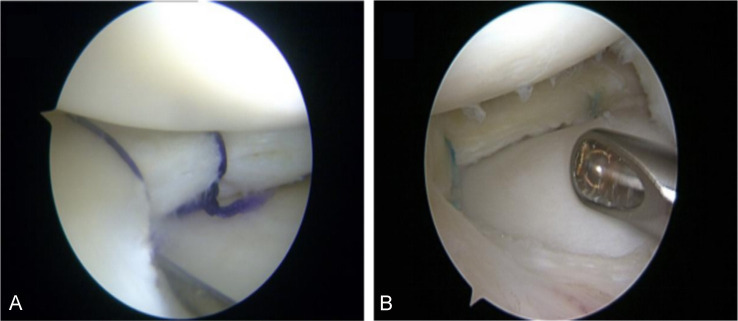
In the control group, the outside-in suture method was used (Figure 2A). With the lead puncture guide needle, a suture was inserted, through the skin and the injured meniscus tissue, into the joint, about 2-4 mm the first needle entry point, and the second guide needle was inserted in the same way, with second guide needle, guide the sutures out of the skin, pull the sutures to the same skin puncture and tie ted. The skin was carefully sutured, and elastic bandages were applied after operation. The number of double needles used depended on the extent of meniscus tear.
Figure 2.
Suture procedure for DLM injury. A: Outside-in suture; B: All-inside suture. DLM: discoid lateral meniscus.
The observation group was treated with the all-inside suture method (Figure 2B). Using conventional medial and lateral approaches, the arthroscope was inserted, and the entire knee was examined. A probe was used to determine the extent and length of the injury. Before repair, the DLM was temporarily repositioned and fixed with a fine needle or probe (through another incision). The sleeve length was determined using the probe, and a Fast-Fix delivery needle was inserted through the fissure sleeve, passing through the torn part of the DLM and reaching the bottom of the depth limiter. The guide needle was swiveled approximately 90°, and then pulled out from the meniscus. The trigger was slid forward to insert the second fixator, ensuring full insertion. All patients had a layered tear, and the suture direction was perpendicular to the tear direction. The delivery needle was then removed from the joint after the suture was passed.
Both groups received the same postoperative treatment, which included applying compression bandages and using adjustable leg braces to immobilize the affected limb in a straight position. Patients were instructed to perform quadriceps isometric contractions and ankle pump exercises immediately after surgery. The knee was allowed to move within a range of 0-90° with brace support within 6 weeks after surgery. The brace was removed based on the patient’s condition after 6 weeks. Full weight-bearing was permitted 8 weeks after surgery, and normal activities could be resumed 6 months after surgery.
Observation index
Primary evaluation indicators
(1) Postoperative pain: Pain intensity was rated on a visual analog scale (VAS) [7] before the surgery, and at 1, 3, 5, 7, 15, and 30 days post-surgery. The VAS score ranges from 0 to 10, with higher the score indicating stronger pain. (2) Restoration of knee function: International knee documentation committee (IKDC) score [8] and Lysholm score [9], each totaling 100 points, were used to assess knee function preoperatively, and at 1 month, 3 months, and 6 months postoperatively. Higher scores indicate better knee functionality. Furthermore, the Tegner score [10], ranging from 0 to 10, was also assessed, with higher score reflecting better knee function. (3) Somatosensory: The passive angle of bilateral knee joints was measured using a knee isokinetic test system preoperatively and at 1 month, 3 months and 6 months postoperatively. Patients wore an eye mask and earplugs while sitting on the kinetic muscle strength tester with their hip and distal leg fixed. Test angles were set at 15°, 45°, and 75°, respectively. The knee joint was passively straightened with the assistance of the strength tester, and patients were asked to sense the stop angle. The difference between the sensed angle and the test angle was recorded. Each angle was tested 3 times, and the average value was taken.
Secondary evaluation index
(1) Surgical indicators: Intraoperative blood loss, operation time and hospital stay were recorded and compared between the two groups. (2) Complications: Complications after surgery were noted, mainly including prolonged postoperative pain, nerve and vascular injury, muscle atrophy, and early arthritis. (3) Clinical curative effect evaluation: The treatment effectiveness was evaluated 6 months post-operation. Cured: No limitation in knee joint activity, and no pain or swelling. Markedly Effective: No limitation in knee joint activity, with significant relief of symptoms such as pain and swelling. Effective: No obvious limitation in knee joint movement, with some pain and clicking symptoms. Ineffective: No obvious limitation in knee joint movement, with some pain and clicking symptoms [11]. Total effective rate = (cured + markedly effective + effective) cases/total cases × 100%.
Statistical methods
SPSS 27.0 was used for data analysis. Count data were expressed as [n (%)], and χ2 test was used for comparison. The measurement data conforming to a normal distribution were expressed as (x̅±s), with paired sample t-test used for intra-group comparisons and independent sample t-test for inter-group comparisons. Quantitative data that deviated from a normal distribution were described using the median and interquartile range [M (Q25, Q75)], and the rank sum test was employed for comparison. Comparisons among different time points were conducted using repeated measure ANOVA or generalized estimation equation. Logistic regression analysis was performed to identify the related influencing factors for curative effect. A p-value of <0.05 was considered statistically significant.
Results
Comparison of general data between the two groups
No significant differences were observed in terms of age, gender, body mass index (BMI), underlying diseases, injury area, nature of injury, and injury side between the two groups (all P>0.05), see Table 1.
Table 1.
Comparison of the two groups in general information
| Data | Observation group (n = 30) | Control group (n = 30) | t/χ2 | P |
|---|---|---|---|---|
| Age (years, x̅±s) | 34.60±6.13 | 35.67±5.52 | 0.708 | 0.482 |
| Gender [n (%)] | 0.601 | 0.438 | ||
| Male | 17 (56.67) | 14 (46.67) | ||
| Female | 13 (43.33) | 16 (53.33) | ||
| BMI (kg/m2, x̅±s) | 22.78±1.85 | 23.62±2.25 | 1.588 | 0.118 |
| Underlying disease [n (%)] | ||||
| Hypertension | 17 (56.67) | 22 (73.33) | 1.832 | 0.176 |
| Diabetes | 6 (20.00) | 10 (33.33) | 1.364 | 0.243 |
| Injury area [n (%)] | 0.300 | 0.584 | ||
| Red and white area | 9 (30.00) | 11 (36.67) | ||
| White area | 21 (70.00) | 19 (63.33) | ||
| Nature of injury [n (%)] | 1.714 | 0.190 | ||
| Acute | 20 (66.67) | 15 (50.00) | ||
| Chronic | 10 (33.33) | 15 (50.00) | ||
| Injury side [n (%)] | 1.699 | 0.196 | ||
| Left knee | 12 (40.00) | 17 (56.67) | ||
| Right knee | 18 (60.00) | 13 (43.33) |
Note: BMI: body mass index.
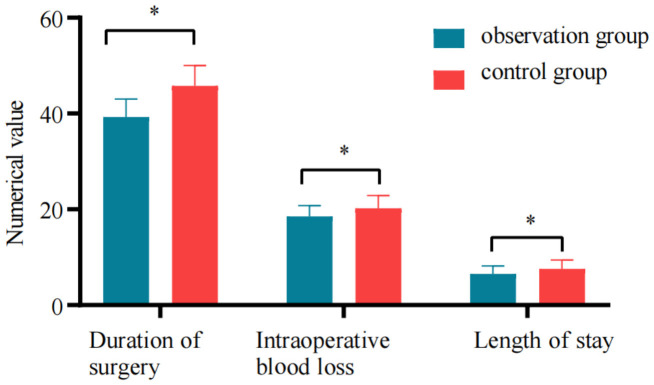
Comparison of surgical indicators and complications between the two groups
Compared to the control group, the observation group demonstrated significantly shorter operation time, hospitalization time and less blood loss (P<0.05), see Figure 3. The incidence of complications in the observation group was slightly lower than that in the control group (20% vs 33.3%), with no statistical difference (P>0.05), as shown in Table 2.
Figure 3.
Comparison of surgical index between the two groups. * compared with the control group, P<0.05.
Table 2.
Comparison of complications between the two groups [n (%)]
| Group | Persistent pain | Nerve and vascular injury | Muscle atrophy | Early arthritis | Total |
|---|---|---|---|---|---|
| Observation group (n = 30) | 2 (6.67) | 1 (3.33) | 1 (3.33) | 2 (6.67) | 6 (20.00) |
| Control group (n = 30) | 3 (10.00) | 2 (6.67) | 2 (6.67) | 3 (10.00) | 10 (33.33) |
| χ2 | 1.364 | ||||
| P | 0.243 |
Comparison of postoperative pain between the two groups
At 1, 3, 5, 7, 15, and 30 days post-surgery, the VAS scores in the observation group was statistically lower compared to those in the control group, indicating a significant main effect of group (all P<0.001). Both groups demonstrated a declining trend in VAS scores over time, with a significant main effect of time (χ2 = 2633.394, P<0.001). Furthermore, an interaction effect between group and time was observed (χ2 = 69.465, P<0.001). See Table 3 for details.
Table 3.
Comparison of VAS scores between the two groups [M (Q25, Q75)]
| Time | Observation group (n = 30) | Control group (n = 30) | Z | P |
|---|---|---|---|---|
| Pre-surgery | 6.5 (5, 9) | 6 (4, 8) | 0.404 | 0.687 |
| 1 day post-surgery | 5.5 (5, 6)# | 6 (4.75, 7)# | 1.348 | 0.178 |
| 3 days post-surgery | 4.5 (4, 6)# | 5 (4.75, 7)# | 1.992 | 0.046 |
| 5 days post-surgery | 4 (3, 5)# | 5 (4, 6)# | 2.590 | 0.010 |
| 7 days post-surgery | 3 (2, 4)# | 4 (3, 5)# | 2.850 | 0.004 |
| 15 days post-surgery | 2 (1, 3)# | 4 (2.75, 4)# | 4.446 | <0.001 |
| 30 days post-surgery | 1.5 (1, 2)# | 3 (2, 3)# | 5.201 | <0.001 |
compare to pre-surgery, P<0.05.
VAS: visual analog score.
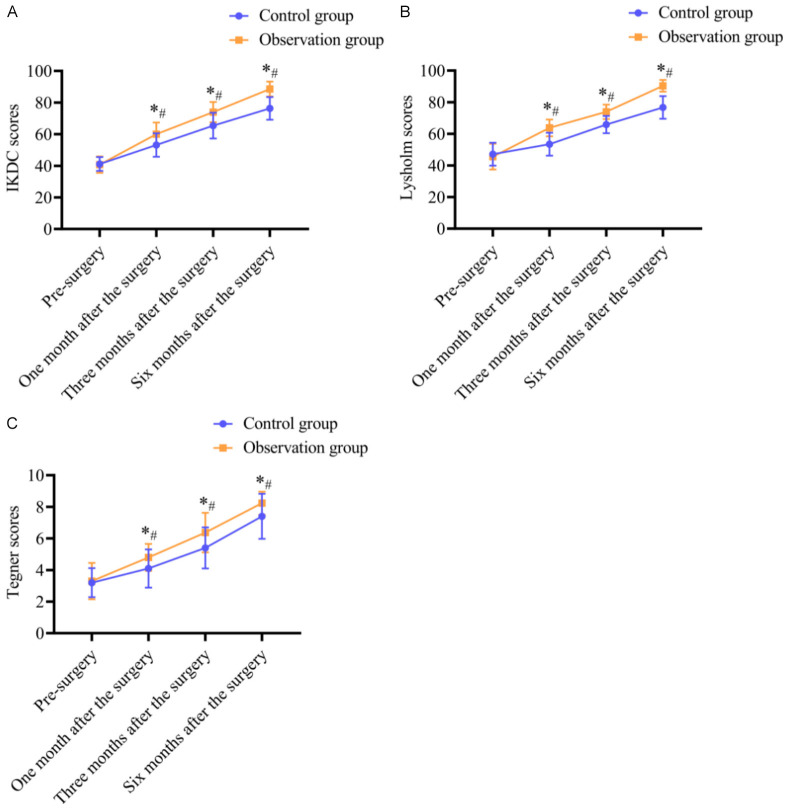
Comparison of knee joint function between the two groups before and after the surgery
At 1, 3, and 6 months post-surgery, the IKDC, Lysholm, and Tegner scores in the observation group were significantly higher than those in the control group, indicating a significant main effect of group (F = 29.866/9.453/5.682, P<0.05). Both groups demonstrated an increasing trend in IKDC, Lysholm, and Tegner scores over time, with a significant main effect of time (F = 762.981/2527.872/1102.396, P<0.05). Furthermore, an interaction effect between group and time was observed (F = 17.014/57.373/10.437, P<0.05), see Figure 4.
Figure 4.
Comparison of IKDC, Lysholm, and Tegner scores between the two groups. IKDC: international knee documentation committee. * compared with the control group, P<0.05; # compared with the pre-surgery, P<0.05.
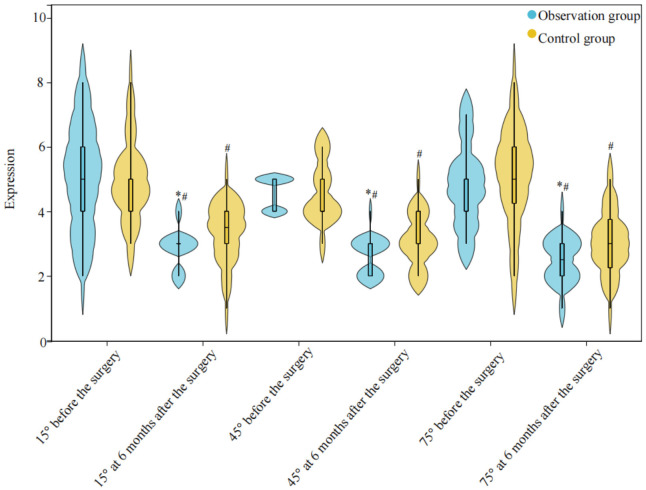
Comparison of proprioception difference of knee joint before and after operation
Six months after surgery, the proprioceptive difference values at 15°, 45° and 75° knee flexion angles decreased in both two groups, and the observation group showed a more significant decrease (P<0.05), see Figure 5.
Figure 5.
Comparison of proprioception difference of knee joint between the two groups before and after operation. * compared with the control group, P<0.05; # compared with the pre-surgery, P<0.05.
Identification of factors affecting treatment efficacy
The clinical effective rate of the observation group was 86.67%, which was higher than 63.33% of the control group (χ2 = 4.356, P = 0.037). The patients were further grouped into an effective group (n = 45) and an ineffective group (n = 15) based on the treatment efficacy.
Univariate analysis identified operation time, IKDC and Lysholm scores at 6 months after operation, postoperative complications, and suture method were found to be influencing factors for treatment efficacy in patients with DLM injury (all P<0.05, Table 4). The above meaningful variables were incorporated into multivariate Logistic regression, and the assignment is shown in Table 5. The results showed that post-operative complications were a risk factor for the poor treatment effect of DLM injury (P<0.05), see Table 6.
Table 4.
Univariate analysis of factors influencing treatment efficacy
| Effective (n = 45) | Ineffective (n = 15) | χ2/t | P | |
|---|---|---|---|---|
| Age (years, x̅±s) | 35.91±5.79 | 32.80±5.39 | 1.832 | 0.072 |
| Gender [n (%)] | 0.556 | 0.456 | ||
| Male | 22 (48.89) | 9 (60.00) | ||
| Female | 23 (51.11) | 6 (40.00) | ||
| BMI (kg/m2, x̅±s) | 23.25±2.02 | 23.02±2.32 | 0.316 | 0.753 |
| Underlying disease [n (%)] | ||||
| Hypertension | 30 (66.67) | 9 (60.0) | 0.220 | 0.639 |
| Diabetes | 17 (37.78) | 3 (20.00) | 1.600 | 0.206 |
| Injury area [n (%)] | 1.600 | 0.206 | ||
| Red and white area | 17 (37.78) | 3 (20.00) | ||
| White area | 28 (62.22) | 12 (80.00) | ||
| Nature of injury [n (%)] | 0.571 | 0.450 | ||
| Acute | 25 (62.50) | 10 (66.67) | ||
| Chronic | 20 (44.44) | 5 (33.33) | ||
| Injury side [n (%)] | 0.090 | 0.764 | ||
| Left knee | 25 (62.50) | 9 (60.00) | ||
| Right knee | 20 (44.44) | 6 (40.00) | ||
| Operation time (min, x̅±s) | 41.71±5.48 | 45.00±2.78 | 2.224 | 0.030 |
| Blood loss (mL, x̅±s) | 19.00±2.59 | 20.47±2.39 | 1.933 | 0.058 |
| Length of hospital stay (day, x̅±s) | 7.09±1.78 | 6.93±1.98 | 0.285 | 0.777 |
| IKDC score (x̅±s) | ||||
| Before the surgery | 41.02±4.66 | 40.60±5.19 | 0.295 | 0.769 |
| 6 months after the surgery | 84.00±8.24 | 76.67±8.42 | 2.970 | 0.004 |
| Lysholm score (x̅±s) | ||||
| Before the surgery | 45.49±7.90 | 48.93±6.53 | 1.522 | 0.133 |
| 6 months after the surgery | 82.82±8.20 | 76.33±10.07 | 2.505 | 0.015 |
| Tegner score (x̅±s) | ||||
| Before the surgery | 3.33±1.02 | 3.00±1.07 | 1.081 | 0.284 |
| 6 months after the surgery | 7.82±1.25 | 7.80±1.08 | 0.062 | 0.951 |
| VAS score [M (Q25, Q75)] | ||||
| Before the surgery | 6 (5, 8) | 8 (4, 9) | 0.578 | 0.563 |
| 30 days after the surgery | 2 (1, 3) | 2 (1, 2) | 0.667 | 0.505 |
| Development of complications [n (%)] | 13.067 | <0.001 | ||
| Yes | 6 (13.33) | 9 (60.00) | ||
| No | 39 (86.67) | 6 (40.00) | ||
| Suturing way [n (%)] | 4.356 | 0.037 | ||
| All-inside suture | 26 (57.78) | 4 (26.67) | ||
| Outside-in suture | 19 (42.22) | 11 (73.33) |
Note: BMI: body mass index; IKDC: international knee documentation committee.
Table 5.
Variable assignments
| Variable | Assignment |
|---|---|
| Clinical effects | 1 = effective, 0 = invalid |
| Operation time | 1 = ≥46 min, 0 = <46 min |
| IKDC score 6 months after surgery | 1 = ≥89 score, 0 = <89 score |
| Lysholm score 6 months after surgery | 1 = ≥87 score, 0 = <87 score |
| Suturing way | 1 = all-inside suture, 0 = outside-in suture |
| Development of complications | 1 = happen, 0 = not happen |
Note: IKDC: international knee documentation committee.
Table 6.
Multivariate Logistic regression analysis
| Variable | B | SE | Wald χ2 | P | OR | 95% CI |
|---|---|---|---|---|---|---|
| Operation time | -0.198 | 0.829 | 0.057 | 0.811 | 0.820 | 0.162-4.161 |
| IKDC score 6 months after surgery | 1.904 | 1.251 | 2.318 | 0.128 | 6.716 | 0.579-77.959 |
| Lysholm score 6 months after surgery | 1.843 | 1.271 | 2.103 | 0.147 | 6.316 | 0.523-76.274 |
| Suturing way | 0.121 | 0.883 | 0.019 | 0.891 | 1.129 | 0.200-6.366 |
| Development of complications | -2.362 | 0.813 | 8.435 | 0.004 | 0.094 | 0.019-0.464 |
Note: IKDC: international knee documentation committee.
Discussion
Due to the lack of ligament guidance in the hypertrophic part of the discoid lateral meniscus (DLM), the femoral condyles are unable to deform accordingly during knee motion. This lack of concentrated stress leads to intra-articular injury [12]. At present, the mainstream treatment of DLM injury is arthroscopic surgery, but different suture methods have different therapeutic effects [13]. This study compared the clinical effects of outside-in sutures and all-inside sutures to determine the optimal treatment for DLM injury and improve patient prognosis.
This study demonstrated a significant decrease in VAS score for both groups following surgical intervention; notably, the score was lower in the observation group compared to the control group. Furthermore, there were marked improvements in IKDC, Lysholm, and Tegner scores in both groups post-surgery; and the improvements were more pronounced in the observation cohort as compared to the control cohort. These outcomes underscore that the all-inside suture approach can substantially ameliorate postoperative discomfort while promoting the recovery of knee joint functionality. Several factors may contribute to this effect, such as smaller incision, minimized meniscus damage, and efficient technique. (1) Smaller Incision: the all-inside suture technique requires only one portal for all necessary operations, resulting in a smaller incision compared to the outside-in suture. There is no need for a cut on the lateral side of the meniscus, reducing the risk of unnecessary nerve injury. (2) Minimized Meniscus Damage: the all-inside suture technique obviates the necessity of extracting meniscal tissue from the wound, thereby minimizing additional damage to the meniscus. (3) Efficient Suture Technique: the all-inside suture technique, combined with the Fast-Fix system, utilizes only two suture-guided fixators during surgery to minimize the number of knots at the joint. This approach alleviates postoperative discomfort and facilitates adherence to rehabilitation exercises, thereby enhancing knee function recovery [14-16]. Subsequent assessments revealed reductions in proprioceptive differences across 15°, 45°, and 75° between the two cohorts following interventions, and Values recorded in the observation group were significantly better compared to those in the control group. These observations proves the efficacy of adopting an all-inside suturing modality for augmenting restoration of proprioceptive faculties in afflicted knees. The precision-based rectification strategies target compromised DLM structures with minimal impact on overall stability and reduced soft-tissue trauma, thereby facilitating subsequent rehabilitative efforts aimed at functional reinstatement [17].
This study also showed that the surgical duration and hospitalization period for the observation group were shorter compared to those of the control group, with less blood loss. We posit that all-inside suturing offers enhanced precision, minimizing damage to surrounding tissues without necessitating an external incision, thereby reducing surgical time and blood loss. Furthermore, patients undergoing all-inside suturing experience milder postoperative pain, facilitating earlier engagement in activities and rehabilitation exercises, consequently leading to a shortened hospital stay. Nevertheless, there is no significant disparity in postoperative complication rates between the two groups. This may be attributed to the minimally invasive nature of both procedures, which reduces the complications like infection, nerve and vascular injury, joint swelling and pain, as well as muscle atrophy commonly associated with open suturing [18,19].
Many studies have indicated that some patients with DLM injury have poor clinical efficacy [20,21]. In this study, multivariate logistic regression analysis was conducted to identify the factors affecting their curative efficacy. The results showed that the operation time, IKDC and Lysholm scores at 6 months after operation, postoperative complications, and suture methods were associated with treatment effect in patients with DLM injury. The duration of operation and postoperative complications are related to the severity of DLM injury. In cases of more severe injuries, such as degree III or IV, the integrity of the meniscus is greatly compromised, increasing the complexity of the surgery and requiring longer operation times. Additionally, severe DLM injuries are more prone to complications, which can negatively impact postoperative outcomes [22]. The choice of surgical suture method also affects the therapeutic effect in patients with DLM injury. Currently, commonly used suture methods include inside-out sutures, outside-in sutures and all-inside sutures, each with its own characteristics. For example, all-inside suturing has less trauma, but it is not suitable for all patients, and sometimes it needs to be combined with other suture methods [23]. Therefore, selecting appropriate suture methods according to the specific conditions of the patient and performing meticulous operation are crucial for successful operation and good recovery.
Conclusion
Arthroscopic all-inside sutures in the treatment of DLM injury has significant clinical effect, with short operation time and hospitalization time, and less blood loss, which is helpful to the recovery of knee joint function and reduces complications. Long operation time, low IKDC and Lysholm scores at 6 months after operation, postoperative complications, and the use of outside-in sutures are associated with poor treatment efficacy in patients with DLM injury. Clinical intervention can be tailored for high-risk patients to promote their recovery.
Disclosure of conflict of interest
None.
References
- 1.Tapasvi S, Shekhar A, Eriksson K. Discoid lateral meniscus: current concepts. J ISAKOS. 2021;6:14–21. doi: 10.1136/jisakos-2017-000162. [DOI] [PubMed] [Google Scholar]
- 2.Kim JH, Ahn JH, Kim JH, Wang JH. Discoid lateral meniscus: importance, diagnosis, and treatment. J Exp Orthop. 2020;7:81. doi: 10.1186/s40634-020-00294-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.He Y, Chen H, Fan Y, Zhou Y, Bao W. Partial resection of lateral discoid meniscus changes lower limb axial alignment - a retrospective cohort study. Knee. 2022;37:171–179. doi: 10.1016/j.knee.2022.06.010. [DOI] [PubMed] [Google Scholar]
- 4.Frisch NB, Keller RA, Mueller JKP, Bandi M, Snethen KG. Treatment of medial collateral ligament injury during total knee arthroplasty with internal suture brace augmentation: a cadaveric and biomechanical study. Orthopedics. 2022;45:e269–e275. doi: 10.3928/01477447-20220425-05. [DOI] [PubMed] [Google Scholar]
- 5.Tao T, Yang W, Tao X, Li Y, Zhang K, Jiang Y, Gui J. Arthroscopic direct anterior-to-posterior suture suspension fixation for the treatment of posterior cruciate ligament tibial avulsion fracture. Orthop Surg. 2022;14:2031–2041. doi: 10.1111/os.13401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harput G, Guney-Deniz H, Nyland J, Kocabey Y. Postoperative rehabilitation and outcomes following arthroscopic isolated meniscus repairs: a systematic review. Phys Ther Sport. 2020;45:76–85. doi: 10.1016/j.ptsp.2020.06.011. [DOI] [PubMed] [Google Scholar]
- 7.Rather AM, Rai S, Rattan V, Jolly SS, Malhotra S. Comparaison of efficacy and safety of fentanyl transdermal patch with oral ketorolac for pain management in dry socket: a randomized clinical trial. J Maxillofac Oral Surg. 2024;23:552–560. doi: 10.1007/s12663-022-01713-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahmed KM, Said HG, Ramadan EKA, Abd El-Radi M, El-Assal MA. Arabic translation and validation of three knee scores, Lysholm Knee Score (LKS), Oxford Knee Score (OKS), and International Knee Documentation Committee Subjective Knee Form (IKDC) SICOT J. 2019;5:6. doi: 10.1051/sicotj/2018054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Andrade ALL, Castro A, Livani B, Belangero WD. Association between Lysholm score and muscular torque deficit after anterior cruciate ligament reconstruction. J Orthop Surg (Hong Kong) 2020;28:2309499020933485. doi: 10.1177/2309499020933485. [DOI] [PubMed] [Google Scholar]
- 10.Kim JS, Choi MY, Kong DH, Ha JK, Chung KS. Does a lower limb balance test after anterior cruciate ligament reconstruction have a significant correlation with postoperative clinical score, stability, and functional performance test? Clin Orthop Surg. 2023;15:402–409. doi: 10.4055/cios21218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Campbell AL, Pace JL, Mandelbaum BR. Discoid lateral meniscus. Curr Rev Musculoskelet Med. 2023;16:154–161. doi: 10.1007/s12178-023-09824-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bisicchia S, Botti F, Tudisco C. Discoid lateral meniscus in children and adolescents: a histological study. J Exp Orthop. 2018;5:39. doi: 10.1186/s40634-018-0153-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Okimura S, Mae T, Tachibana Y, Iuchi R, Nakata K, Yamashita T, Shino K. Biomechanical comparison of meniscus-suture constructs for pullout repair of medial meniscus posterior root tears. J Exp Orthop. 2019;6:17. doi: 10.1186/s40634-019-0186-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Golz AG, Mandelbaum B, Pace JL. All-inside meniscus repair. Curr Rev Musculoskelet Med. 2022;15:252–258. doi: 10.1007/s12178-022-09766-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kennedy MI, Strauss M, LaPrade RF. Injury of the meniscus root. Clin Sports Med. 2020;39:57–68. doi: 10.1016/j.csm.2019.08.009. [DOI] [PubMed] [Google Scholar]
- 16.Mouarbes D, Menetrey J, Marot V, Courtot L, Berard E, Cavaignac E. Anterior cruciate ligament reconstruction: a systematic review and meta-analysis of outcomes for quadriceps tendon autograft versus bone-patellar tendon-bone and hamstring-tendon autografts. Am J Sports Med. 2019;47:3531–3540. doi: 10.1177/0363546518825340. [DOI] [PubMed] [Google Scholar]
- 17.Fillingham YA, Riboh JC, Erickson BJ, Bach BR Jr, Yanke AB. Inside-out versus all-inside repair of isolated meniscal tears: an updated systematic review. Am J Sports Med. 2017;45:234–242. doi: 10.1177/0363546516632504. [DOI] [PubMed] [Google Scholar]
- 18.Zsidai B, Dadoo S, Fox MA, Kaarre J, Grandberg C, Greiner JJ, Musahl V. Arthroscopic all-inside repair of challenging meniscus tears. J ISAKOS. 2023;8:210–212. doi: 10.1016/j.jisako.2023.02.007. [DOI] [PubMed] [Google Scholar]
- 19.Okimura S, Mae T, Tachibana Y, Iuchi R, Nakata K, Yamashita T, Shino K. Biomechanical comparison of meniscus-suture constructs for pullout repair of medial meniscus posterior root tears. J Exp Orthop. 2019;6:17. doi: 10.1186/s40634-019-0186-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bozduman Ö, Gürün E, Cahit Çıtır Ö. The effect of brace use on clinical outcomes after arthroscopic meniscus repair. Eur Rev Med Pharmacol Sci. 2023;27:1863–1868. doi: 10.26355/eurrev_202303_31550. [DOI] [PubMed] [Google Scholar]
- 21.Lu J, Chen Y, Hu M, Sun C. Clinical efficacy of arthroscopy in the treatment of discoid meniscus injury and related risk factors for postoperative pain. Ann Palliat Med. 2022;9:4002–4009. doi: 10.21037/apm-20-1899. [DOI] [PubMed] [Google Scholar]
- 22.van de Graaf VA, Noorduyn JCA, Willigenburg NW, Butter IK, de Gast A, Mol BW, Saris DBF, Twisk JWR, Poolman RW ESCAPE Research Group. Effect of early surgery vs physical therapy on knee function among patients with nonobstructive meniscal tears: the ESCAPE randomized clinical trial. JAMA. 2018;320:1328–1337. doi: 10.1001/jama.2018.13308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hamada M, Tsujii A. Editorial commentary: all-inside double-vertical cross-suture is an effective technique for knee meniscus radial tear repair, but there is no gold-standard evaluation tool for evaluating healing and function of the repaired meniscus. Arthroscopy. 2022;38:1930–1932. doi: 10.1016/j.arthro.2021.12.031. [DOI] [PubMed] [Google Scholar]