Abstract
Objective: To compare the treatment efficacy of conventional restoration techniques versus micro-invasive restoration techniques utilizing a microscope in the restorative treatment for dental caries. Methods: The clinical information of 84 patients who received restorative treatment for dental caries was retrospectively analyzed. Patients were divided into two groups according to the type of restoration they received. The control group (n=42) underwent traditional restorative treatment, while the observation group (n=42) underwent micro-invasive restoration with the use of a microscope. The restoration effect, marginal fit, periodontal soft tissue health (Oral Health Impact Profile-14 (OHIP-14) score), prognostic outcomes, satisfaction rate, and doctor’s posture health were compared between the two groups. Results: The success restoration rate was 92.86% in the control group and 95.24% in the observation group (P > 0.05). The vertical marginal discrepancy, horizontal marginal discrepancy, and absolute marginal discrepancy values were significantly lower in the observation group compared to the control group (all P < 0.05). There was no significant difference in pre-treatment OHIP-14 scores between the two groups (P > 0.05). However, the post-treatment OHIP-14 score was significantly lower in the observation group compared to the control group (P < 0.05). After a 12-month follow-up, the observation group showed higher proportions of A-level restoration integrity, marginal fit, gingival health, fewer secondary caries, and less food impaction compared to the control group (all P < 0.05). The satisfaction rate in the observation group was significantly higher than that in the control group (95.24% vs. 92.86%, P < 0.05). The posture score of doctors in the observation group was significantly better than that in the control group (P < 0.05). Conclusion: Micro-invasive restoration using a microscope, compared to traditional restoration, offers several advantages. It reduces marginal discrepancies, improves periodontal soft tissue health, and enhances prognostic outcomes for patients, while ensuring a satisfactory restoration effect.
Keywords: Micro-invasive restoration with the use of microscope, restoration, periodontal soft tissue, prognostic outcomes
Introduction
With the continuous advancement of dental technology, restorative treatment has become an indispensable part of clinical dental practice [1]. Traditional restorative treatment has been the primary approach; however, studies have highlighted certain limitations and drawbacks associated with this methodology [2]. One significant drawback is the extensive tooth structure preparation required to establish a stable foundation for the fixed restoration, potentially leading to inflammation and pain [2]. Additionally, the extensive use of metallic materials in traditional restorative procedures may compromise aesthetics [3]. Therefore, reducing trauma, enhancing treatment efficiency, and ensuring restorative outcomes have become critical factors in clinical restorative treatment.
The current trend in modern restorative dentistry prioritizes the preservation of natural tooth structure and promotes minimally invasive treatment approaches [4]. In line with this objective, minimally invasive restorative treatment with the aid of a microscope has gained significant popularity as a means to achieve conservative and precise treatment [5]. Compared to traditional restorative methods, minimally invasive restorative treatment with a microscope, enables clinicians to observe the intraoral conditions with enhanced precision and accuracy. Treatment is performed using miniature instruments, reducing damage to the patient’s natural tooth structure and consequently enhancing the quality and prognosis of the restoration [6]. Besides, periodontal soft tissues play a significant role in the restorative outcome and prognosis [7]. Currently, there is a scarcity of comparative research examining the effects of minimally invasive restorative treatment and traditional restorative treatment on the health of periodontal soft tissues and long-term prognosis. Therefore, this study aims to compare the restorative outcomes, marginal adaptation, periodontal soft tissue health, prognosis, complications, and the posture scores of clinicians between the traditional restorative approach and minimally invasive approach. The findings of this study will provide a reference for clinical practice.
Materials and methods
Study population
We retrospectively analyzed the clinical data of 84 patients who underwent restorative treatment for tooth defects at Nanjing Stomatological Hospital from January 2023 to January 2024. The patients were divided into two groups based on the type of restorative treatment they received: a control group (n=42) with traditional restorative treatment, and an observation group (n=42) with minimally invasive restorative treatment under a microscope.
Inclusion and exclusion criteria
Inclusion criteria: ① Patients aged 18 years or older; ② Patients with single or multiple tooth defects; ③ Patients with relatively stable overall health.
Exclusion criteria: ① Patients with systemic diseases; ② Pregnant or lactating women; ③ Patients with chronic diseases such as heart disease, hypertension, or diabetes; ④ Patients with mental disorders or intellectual disabilities; ⑤ Patients who had undergone previous oral surgery or thoes with dental implants.
Methods
To minimize potential confounding factors that could impact treatment outcomes, all patients in the study were treated by the same group of clinicians, and the selection and processing of relevant materials were conducted similarly.
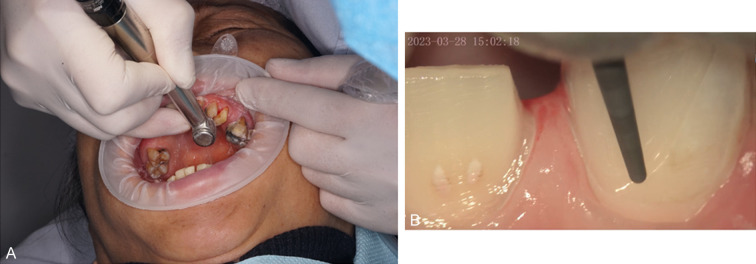
Full crown restoration was performed on the tooth after root canal treatment, considering the patient’s specific condition [8]. Prior to the procedure, either an all-ceramic crown or a porcelain-fused-to-metal crown was prepared, based on the specific requirements. Adequate tooth preparation was carried out, with the aim of preserving enough tooth structure and ensuring enamel thickness of over 1 mm to achieve clear tooth shoulder contours. The thin walls and fragile areas of the tooth structure were cleaned. After tooth preparation, a double-cord gingival retraction technique was adopted. By placing fine cords or tapes between the gingival margin and subgingival sulcus, the gingival tissue was displaced to expose the complete tooth structure and gingival margin. Once the double-cord gingival retraction was completed, a restoration was applied using addition silicone material. The silicone material was placed over the prepared tooth, ensuring complete coverage of the crown and leaving sufficient material thickness for stability. A temporary crown was placed to protect the prepared tooth and provide functionality and aesthetics for the tooth. The restoration mold was subsequently sent to a dental laboratory, where skilled technicians used appropriate materials and techniques to fabricate a full crown that matched the patient’s tooth. After crafting the crown, it was returned for a trial fitting to assess the fit of the crown’s margins, color harmony with adjacent teeth, and occlusion. If the trial fitting was successful, further adhesive steps were implemented: the crown was etched with hydrofluoric acid, dentin was treated, and then rinsed and dried for 120 seconds. A silane coupling agent was then applied and dried for 90 seconds, followed by a dentin adhesive placed in a light-protected environment. The abutment tooth was disinfected with 75% alcohol, dried, and etched with 37% phosphoric acid on the enamel surface. After rinsing and drying, a resin adhesive was applied to bond the restoration, followed by curing. Excess adhesive was removed, and the crown was polished. The difference between the observation group and the control group lies in the fact that the control group did not use a microscope or special instruments during the restorative process. Representative figures of the treatments for the two groups are shown in Figure 1.
Figure 1.
Typical figures of the treatments. A: Traditional restorative treatment; B: Micro-invasive restoration with the use of microscope.
Observational indicators
(1) Restoration outcome: Excellent: The restoration defect-free, highly stable, without marginal loosening, no gingivitis, maintains normal chewing function, and has an excellent aesthetic appearance. Good: The restoration is stable and free of defects, though with noticeable cracks at the margin. Mild gingivitis may be present, with basic restoration of chewing function and good aesthetic appearance. Failure: The restoration displays obvious damage, including looseness and detachment, noticeable cracks at the margin, severe gingivitis, and poor chewing function.
(2) Marginal adaptation: Using a microscope, the horizontal and vertical discrepancies between the termination line of the labial side of the prepared tooth structure and the outermost point of the gingival margin of the metal-ceramic crown were measured.
(3) Periodontal tissue health: The Oral Health Impact Profile-14 (OHIP-14 score) [9] was used to assess the oral health status of patients. The scoring scale consists of 14 questions, each rated on a scale of 0 (never) to 4 (very often), with a total score ranging from 0 to 56. A higher score indicates lower periodontal tissue health.
(4) Prognosis: After 12 months of treatment, the prognosis was assessed using the modified United States Public Health Service (USPHS) evaluation criteria [10] across 5 domains. Integrity: Excellent integrity (Grade A), minor defects without functional impairment (Grade B), fracture or detachment (Grade C); Marginal adaptation: Excellent marginal adaptation, no probe catch (Grade A), marginal catch with inability to penetrate (Grade B), marginal catch with penetration (Grade C); Secondary caries: No secondary caries (Grade A), presence of secondary caries (Grade E); Gingival health: Healthy, no signs of gingival inflammation (Grade A), mild gingival inflammation (Grade B), severe inflammation with periodontal pockets and bleeding on probing (Grade C); Food impaction: Normal interproximal contact, no food impaction (Grade A), loose interproximal contact, food impaction (Grade E).
(5) Satisfaction: Patients were provided with a “Satisfaction Survey Questionnaire” comprising 20 questions developed by Nanjing Stomatological Hospital. Satisfaction was scored on a 5-point scale, with a total score below 70 indicating dissatisfaction, scores between 70 and 89 indicating satisfaction, and scores of 90 or above indicating high satisfaction. Satisfaction rate = (Satisfaction + High Satisfaction)/total number of cases × 100%.
(6) Operator ergonomics: Operator posture during procedures was assessed through side and frontal view photographs, analyzed by two senior dental restoration experts using the modified Dental Operator Posture Assessment Instrument (M-DOPAI) [11]. This instrument includes 12 items, each rated on a scale from 1 (good) to 3 (poor). Eight items have a score range of 1-3, while four items have a score range of 1-2. The total score ranges from 12 to 32, with lower scores indicating better adherence to ergonomic requirements.
Statistical analysis
GraphPad Prism 8 was employed for graphical representation, while SPSS 22.0 was for data analysis. Continuous data were described using mean and standard deviation, with t-tests or analysis of variance (ANOVA) employed to compare the differences between the two groups. Categorical data was described using frequency and percentage, and analyzed using chi-square test or Fisher’s exact test. A significance level of P < 0.05 was considered statistically significant.
Results
Comparison of basic information between the two groups of patients
The control group comprised 42 patients, including 23 males and 19 females. The age ranged from 42 to 61 years, with a mean age of (51.7±4.6) years. The distribution of dental caries was as follows: 11 patients with one carious tooth and 31 patients with two or more carious teeth. Among them, there were 20 cases of pulpitis and 22 cases of periapical periodontitis. The observation group was also comprised of 42 patients, including 25 males and 17 females, with age ranging from 40 to 63 years and a mean age of (51.9±4.8) years. This group had 13 patients with one carious tooth and 29 with two or more carious teeth. Among them, there were 19 cases of pulpitis and 23 cases of periapical periodontitis. The basic characteristics of both groups were comparable, with no statistically significant differences (all P > 0.05, Table 1).
Table 1.
Comparison of basic information between the two groups of patients
| Basic data information | Control group (n=42) | Observation group (n=42) | t/χ2 | P |
|---|---|---|---|---|
| Gender | 0.194 | 0.659 | ||
| Male | 23 | 25 | ||
| Female | 19 | 17 | ||
| Age | 51.7±4.6 | 51.9±4.8 | 0.195 | 0.845 |
| Tooth defects | 0.233 | 0.629 | ||
| 1 | 11 | 13 | ||
| ≥ 2 | 31 | 29 | ||
| Disease | 0.047 | 0.826 | ||
| Pulpitis | 20 | 19 | ||
| Apical periodontitis | 22 | 23 |
Comparison of restoration effects between the two groups of patients
The excellent and good restoration rate in the control group was 92.86%, while that in the observation group was 95.24% (P > 0.05, Table 2).
Table 2.
Comparison of restoration effects between the two groups of patients
| Group | Number of cases | Excellent | Good | Failure | Excellent rate (%) |
|---|---|---|---|---|---|
| Control group | 42 | 14 | 25 | 3 | 92.86% |
| Observation group | 42 | 22 | 18 | 2 | 95.24% |
| χ2 | - | - | - | - | 0.0 |
| P | - | - | - | - | 1.0 |
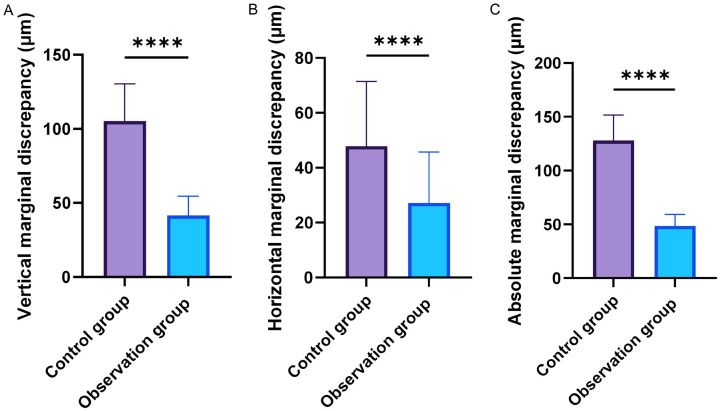
Comparison of marginal adaptation between the two groups of patients
As shown in Figure 2, the vertical marginal discrepancy, horizontal marginal discrepancy, and absolute marginal discrepancy in the control group were (105.32±25.12) µm, (47.92±23.51) µm, and (127.86±20.35) µm, respectively. In the observation group, the vertical marginal discrepancy, horizontal marginal discrepancy, and absolute marginal discrepancy were (41.53±13.04) µm, (27.14±18.63) µm, (48.65±10.61) µm, respectively. These indices in the observation group were all significantly lower than those in the control group (all P < 0.05).
Figure 2.
Comparison of marginal adaptation between the two groups of patients (µm). A: Comparison of vertical marginal discrepancy between the two groups; B: Comparison of horizontal marginal discrepancy between the two groups; C: Comparison of absolute marginal discrepancy between the two groups. Note: ****, P < 0.0001.
Comparison of periodontal soft tissue health between the two groups of patients
As shown in Figure 3, the OHIP-14 scores before and after treatment in the control group were (38.39±5.74) and (20.98±5.35), respectively, while that in the observation group were (38.16±6.03), (14.96±5.06), respectively. There was no significant difference in the OHIP-14 score before treatment between the two groups (P > 0.05). However, the OHIP-14 score after treatment in the observation group was significantly lower than that in the control group (P < 0.05).
Figure 3.
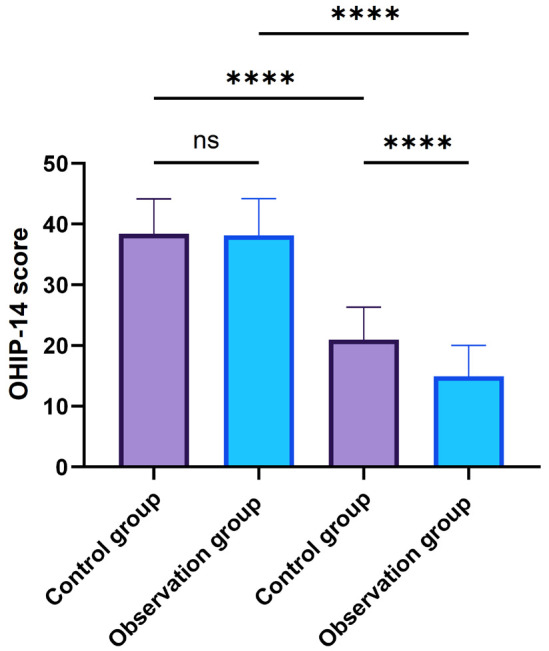
Comparison of periodontal soft tissue health between the two groups of patients. Note: ns, non-significance; OHIP-14 score, Oral health impact profile-14; ns, P > 0.05; ****, P < 0.0001.
Comparison of prognosis between the two groups of patients
After 12 months of treatment, the observation group exhibited a significantly higher proportion of grade A in terms of integrity, marginal adaptation, gingival health, secondary caries, and food impaction compared to the control group (all P < 0.05, Table 3).
Table 3.
Comparison of prognosis between the two groups of patients
| Prognosis (Grade A) | Control group (n=42) | Observation group (n=42) | χ2 | P |
|---|---|---|---|---|
| Integrity | 17 (40.48%) | 26 (61.90%) | 3.859 | 0.049 |
| Edge tightness | 18 (42.86%) | 29 (69.05%) | 5.844 | 0.015 |
| Gum health | 17 (40.48%) | 28 (66.67%) | 5.791 | 0.016 |
| Secondary caries | 23 (54.76%) | 34 (80.95%) | 6.604 | 0.010 |
| Food impaction | 25 (59.52%) | 35 (83.33%) | 5.833 | 0.015 |
Comparison of satisfaction between the two groups of patients
The satisfaction rate in the control group was 80.95%, which was significantly lower than 97.62% in the observation group (P < 0.05, Table 4).
Table 4.
Comparison of satisfaction between the two groups of patients
| Group | Number of cases | Dissatisfaction | Satisfaction | High satisfaction | Satisfaction rate (%) |
|---|---|---|---|---|---|
| Control group | 42 | 11 | 23 | 8 | 80.95% |
| Observation group | 42 | 19 | 22 | 1 | 97.62% |
| χ2 | - | - | - | - | 4.480 |
| P | - | - | - | - | 0.034 |
Comparison of operator’s posture score between the two groups
As shown in Figure 4, the M-DOPAI score for doctors in the control group was (18.36±1.58), while that in the observation group was significantly lower (13.54±0.82) (P < 0.05), indicating better adherence to ergonomic guidelines among doctors in the observation group.
Figure 4.
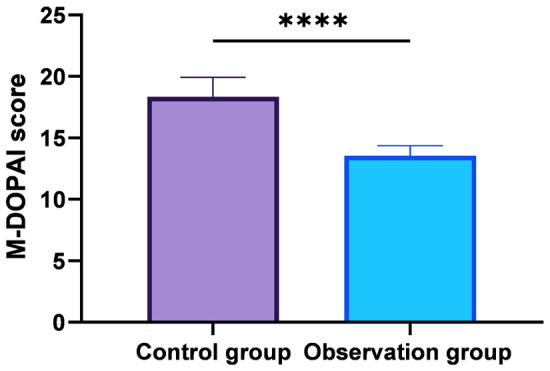
Comparison of posture score between the two groups of doctors. Note: M-DOPAI, modified Dental Operator Posture Assessment Instrument; ****, P < 0.05.
Discussion
Dental caries involves the progressive deterioration, erosion, wear, and fractures of the tooth surface, resulting in the tooth structure loss [12]. Dental caries is usually caused by multiple factors, including poor oral hygiene, unhealthy oral habits (such as nail biting and chewing on hard objects), anomalous tooth morphology, and oral trauma [13]. If left untreated, dental caries can escalate into more severe oral conditions, such as periapical disease, and alveolar bone resorption. Root canal treatment is a commonly employed approach for managing dental caries, particularly when the caries has progressed to affect the pulp, manifesting symptoms such as tooth pain and swelling [14]. This treatment involves removing the infected pulp tissue and diseased tissue, then filling the root canal to block re-infection and preserve the affected tooth, thereby alleviating pain and discomfort [15]. Root canal treatment often precedes restorative procedures especially when the caries is severe, to restore both function and aesthetics of the tooth [16]. Full crown restoration is a typical method used to rehabilitate teeth. Traditional full crown restoration usually requires substantial removal of tooth structure, leaving minimal remaining tooth structure which compromises the restoration’s strength. This can lead to post-treatment issues such as food impaction and gingival inflammation, negatively affecting the patient’s chewing function and overall quality of life after treatment [17]. Studies by Carvalho et al. [18] have found that although traditional full crown restoration with root canal treatment can yield satisfactory outcomes, the periodontal health, restoration integrity, and restoration of chewing function are often suboptimal. Therefore, the search for minimally invasive and precise restorative techniques is of significant importance in improving the periodontal health and prognosis of patients.
With the continuous development of modern restorative dentistry and the introduction of concepts such as “high-quality dentistry” and “esthetic restorations”, the expectations for dental restorations have expanded beyond visual aspects such as materials, tissues, structures, and aesthetics. There is now a demand for restorations that emulate the natural appearance of teeth, including smile line aesthetics, long-term functional stability, and harmony between oral soft and hard tissues. As a result, the utilization of magnification devices in oral restorations has gained significant popularity [19]. Minimally invasive restorations under the microscope enable more precise treatment of dental caries, better preservation of healthy tooth structure, and less trauma, ultimately improving treatment outcomes [20]. In this study, a retrospective analysis was conducted on clinical data from 84 patients who underwent restorative treatment for dental caries in Nanjing Stomatological Hospital. The results indicated that while restoration outcomes were similar between the groups, as corroborated by previous studies [21], the group treated with minimally invasive techniques showed superior marginal adaptation, periodontal health, prognosis, and patient satisfaction.
The benefits of minimally invasive restoration technique include: ① High precision. Minimally invasive restorations under microscopy allow dentists to observe and treat the affected site more precisely using high-magnification microscopy and optical amplifiers, facilitating accurate removal of diseased tissue and improving restoration, thus leading to better treatment outcomes. Bud et al. [3] also support the notion that magnification devices significantly improve both direct and indirect vision, thus increasing the precision of treatments compared to traditional methods. ② Improved Marginal Adaptation. Minimally invasive restorations under microscopy can reduce the gap between the restoration and tooth structure, decreasing marginal discrepancies. This reduction limits bacterial proliferation and food residue, lowering the risk of further caries and restoration detachment. ③ Reduced Tissue Damage. Minimally invasive restorations under microscopy cause minimal damage to the patient’s oral soft tissues during the procedure, promoting quicker healing and better periodontal health, which is crucial for the overall prognosis of the restoration. ④ Enhanced Ergonomics for Dentists. This study also explored the impact of different restoration techniques on the ergonomic health of dentists and found that compared to traditional restorations, microscope-based restorations provided dentists with better ergonomic benefits.
While this study provides some insights into the application value and benefits of minimally invasive restorations using a microscope for dental caries, several limitations still need to be acknowledged: ① Small sample size: With only 84 patients in this study, the small sample size may restrict the overall reliability and generalizability of the findings. ② Selection bias: As a retrospective study, potential biases in patient selection and uncontrolled confounding factors could influence the results. ③ Variation in severity of dental caries: This study did not account for different types and severities of dental caries, which could impact periodontal health and prognosis of the restorations. ④ Short follow-up period: A follow-up period of 12 months in this study restricts the evaluation of the long-term prognosis of the restorations. ⑤ Neglect of psychological factors: This study did not take into account the patients’ acceptance and psychological factors related to different treatment modalities, which could have influenced the research results. Therefore, in the future, it is necessary to expand the sample size, extend the research duration, and strengthen the monitoring and evaluation of other intervention factors to address these limitations.
Conclusion
While offering comparable treatment outcomes, minimally invasive restorations under the microscope outperforms traditional restorations in terms of reducing marginal discrepancy and improving periodontal health and prognosis for patients, leading to higher patient satisfaction and acceptance. Additionally, it supports better ergonomic health among dentists, promoting their overall well-being.
Acknowledgements
This project was supported by “3456” Cultivation Program for Junior Talents of Nanjing Stomatological School, Medical School of Nanjing University (No. 0222C119) and Nanjing Medical Science and Technology Development Fund (No. GBX22306).
Disclosure of conflict of interest
None.
Abbreviations
- OHIP-14 score
Oral health impact profile-14
- M-DOPA
modified dental operator posture assessment instrument
References
- 1.Gomez-Meda R, Esquivel J, Blatz MB. The esthetic biological contour concept for implant restoration emergence profile design. J Esthet Restor Dent. 2021;33:173–184. doi: 10.1111/jerd.12714. [DOI] [PubMed] [Google Scholar]
- 2.Caplan DJ, Li Y, Wang W, Kang S, Marchini L, Cowen HJ, Yan J. Dental restoration longevity among geriatric and special needs patients. JDR Clin Trans Res. 2019;4:41–48. doi: 10.1177/2380084418799083. [DOI] [PubMed] [Google Scholar]
- 3.Li F, Diao Y, Wang J, Hou X, Qiao S, Kong J, Sun Y, Lee ES, Jiang HB. Review of cracked tooth syndrome: etiology, diagnosis, management, and prevention. Pain Res Manag. 2021;2021:3788660. doi: 10.1155/2021/3788660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al Saleh F, AbuZayeda M, Kiat-Amnuay S, Milosevic A. Survey of dental implant and restoration selection by prosthodontists in Dubai. Int J Dent. 2021;2021:8815775. doi: 10.1155/2021/8815775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bud M, Jitaru S, Lucaciu O, Korkut B, Dumitrascu-Timis L, Ionescu C, Cimpean S, Delean A. The advantages of the dental operative microscope in restorative dentistry. Med Pharm Rep. 2021;94:22–27. doi: 10.15386/mpr-1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ballester B, Giraud T, Ahmed HMA, Nabhan MS, Bukiet F, Guivarc’h M. Current strategies for conservative endodontic access cavity preparation techniques-systematic review, meta-analysis, and decision-making protocol. Clin Oral Investig. 2021;25:6027–6044. doi: 10.1007/s00784-021-04080-7. [DOI] [PubMed] [Google Scholar]
- 7.Yu H, Zhao Y, Li J, Luo T, Gao J, Liu H, Liu W, Liu F, Zhao K, Liu F, Ma C, Setz JM, Liang S, Fan L, Gao S, Zhu Z, Shen J, Wang J, Zhu Z, Zhou X. Minimal invasive microscopic tooth preparation in esthetic restoration: a specialist consensus. Int J Oral Sci. 2019;11:31. doi: 10.1038/s41368-019-0057-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang Z, Feng J, Chen JH, Zhao K. Finite element analysis and biomimetic optimal design of full-crown restoration. Zhonghua Yi Xue Za Zhi. 2022;102:2624–2629. doi: 10.3760/cma.j.cn112137-20220319-00584. [DOI] [PubMed] [Google Scholar]
- 9.Campos LA, Peltomäki T, Marôco J, Campos JADB. Use of oral health impact profile-14 (OHIP-14) in different contexts. What is being measured? Int J Environ Res Public Health. 2021;18:13412. doi: 10.3390/ijerph182413412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Durão MA, Andrade AKM, Santos MDCMDS, Montes MAJR, Monteiro GQM. Clinical performance of bulk-fill resin composite restorations using the United States public health service and federation dentaire internationale criteria: a 12-month randomized clinical trial. Eur J Dent. 2021;15:179–192. doi: 10.1055/s-0040-1718639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Partido BB, Henderson RP, Kennedy M. Improving the awareness of musculoskeletal disorder risks among dental educators. J Dent Educ. 2020;84:5–12. doi: 10.21815/JDE.019.158. [DOI] [PubMed] [Google Scholar]
- 12.Patil S, Moafa IH, Bhandi S, Jafer MA, Khan SS, Khan S, Carroll WB, Awan KH. Dental care and personal protective measures for dentists and non-dental health care workers. Dis Mon. 2020;66:101056. doi: 10.1016/j.disamonth.2020.101056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ayedun OS, Oredugba FA, Sote EO. Comparison of the treatment outcomes of the conventional stainless steel crown restorations and the hall technique in the treatment of carious primary molars. Niger J Clin Pract. 2021;24:584–594. doi: 10.4103/njcp.njcp_460_20. [DOI] [PubMed] [Google Scholar]
- 14.Meshram P, Meshram V, Palve D, Patil S, Gade V, Raut A. Comparative evaluation of microleakage around Class V cavities restored with alkasite restorative material with and without bonding agent and flowable composite resin: an in vitro study. Indian J Dent Res. 2019;30:403–407. doi: 10.4103/ijdr.IJDR_767_17. [DOI] [PubMed] [Google Scholar]
- 15.Barbosa AFA, de Lima CO, Moreira T, Sassone LM, Fidalgo TKDS, Silva EJNL. Photodynamic therapy for root canal disinfection in endodontics: an umbrella review. Lasers Med Sci. 2022;37:2571–2580. doi: 10.1007/s10103-022-03569-1. [DOI] [PubMed] [Google Scholar]
- 16.Mazumdar P, Das A, Das UK. Comparative evaluation of microleakage of three different direct restorative materials (silver amalgam, glass ionomer cement, cention N), in Class II restorations using stereomicroscope: an in vitro study. Indian J Dent Res. 2019;30:277–281. doi: 10.4103/ijdr.IJDR_481_17. [DOI] [PubMed] [Google Scholar]
- 17.Bhuva B, Giovarruscio M, Rahim N, Bitter K, Mannocci F. The restoration of root filled teeth: a review of the clinical literature. Int Endod J. 2021;54:509–535. doi: 10.1111/iej.13438. [DOI] [PubMed] [Google Scholar]
- 18.Carvalho MA, Lazari PC, Gresnigt M, Del Bel Cury AA, Magne P. Current options concerning the endodontically-treated teeth restoration with the adhesive approach. Braz Oral Res. 2018;32(Suppl 1):e74. doi: 10.1590/1807-3107bor-2018.vol32.0074. [DOI] [PubMed] [Google Scholar]
- 19.Matei RI, Todor L, Cuc EA, Popescu MR, Dragomir LP, Rauten AM, Porumb A. Microscopic aspects of junction between dental hard tissues and composite material depending on composite insertion: layering versus bulk-fill. Rom J Morphol Embryol. 2019;60:133–138. [PubMed] [Google Scholar]
- 20.Wang YK, Huang C. Establishment and clinical practice of the global diagnostic and theraputic concept of dental esthetic restoration. Zhonghua Kou Qiang Yi Xue Za Zhi. 2023;58:393–397. doi: 10.3760/cma.j.cn112144-20230213-00043. [DOI] [PubMed] [Google Scholar]
- 21.Yu HY, Zhao YW, Li JY, Luo T, Gao J, Liu HC, Liu WC, Liu F, Zhao K, Fei L, Ma CF, JuergenManfred S, Liang SS, Fan L, Gao SS, Zhu ZL, Shen JF, Wang J, Zhu ZM, Zhou XD. Minimal invasive microscopic tooth preparation based on endodontic, periodontal and functional health. Hua Xi Kou Qiang Yi Xue Za Zhi. 2019;37:229–235. doi: 10.7518/hxkq.2019.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]