Abstract
Objective: This study investigates the impact of Internet-based integrated care on breastfeeding outcomes and emotional well-being in primiparous women. Methods: We conducted a retrospective analysis of 154 primiparous women admitted to Baoji People’s Hospital from July 2020 to September 2023. Participants were divided into an observation group (n = 58), which received internet-based integrated care, and a control group (n = 96), which received routine telephone follow-up. We compared breastfeeding outcomes, knowledge, self-efficacy, and infant physical development between the groups, and performed logistic regression to identify risk factors affecting breastfeeding. Results: Before the intervention, there were no significant differences in breastfeeding knowledge and self-efficacy scores between the groups (all P > 0.05). At 6 months postpartum, the observation group had a higher breastfeeding success rate and improved scores in breastfeeding knowledge and self-efficacy (all P < 0.05). Infants in the observation group exhibited better physical development compared to those in the control group (P < 0.05). Logistic regression analysis identified age (P = 0.019), mode of delivery (P = 0.006), and nipple condition (P = 0.029) as independent risk factors for exclusive breastfeeding, while education level (P < 0.001), type of employment (P = 0.002), and daily sucking frequency (P = 0.005) were identified as independent protective factors. Conclusions: The Internet-based integrated care model significantly enhances breastfeeding knowledge, self-efficacy, and exclusive breastfeeding rates among primiparous women, while also supporting better infant physical development.
Keywords: Internet model, integrated care, primiparous women, breastfeeding
Introduction
Breastfeeding, the practice of feeding an infant with a mother’s own milk, is a traditional and highly effective method of ensuring healthy growth and development in infants and young children [1]. Breast milk is rich in immune substances and comprehensive nutritional components that adapt to an infant’s age, meeting their growth needs [2]. It helps establish a healthy gut microbiome, enhances intestinal immunity, and reduces the incidence of allergies [3]. Exclusive breastfeeding for 4-6 months is particularly effective in preventing allergies in infants [4], promoting the development of the nervous system and intelligence, and reducing the risk of obesity later in life [5]. Studies show that children who are exclusively breastfed for longer periods have healthier growth and a lower risk of obesity at age 4 [6,7].
Breastfeeding also benefits maternal health by aiding in a quicker return to a non-pregnant state, shortening birth intervals, reducing postpartum bleeding and obesity, and lowering the risk of urinary tract infections, osteoporosis, and breast and ovarian cancers [8]. Additionally, breastfeeding fosters valuable mother-child bonding time, strengthens the emotional connection, promotes a harmonious parent-child relationship, and reduces the incidence of postpartum depression [9]. Despite these extensive benefits, the global breastfeeding rate remains suboptimal. For instance, the exclusive breastfeeding rate at 6 months is 38.2% in Singapore [10], 39% at 4 months, and 18% at 6 months in Australia [11]. In China, the exclusive breastfeeding rate for infants under 6 months is 29.2%, below the global average, with considerable regional variation [12]. This highlights that breastfeeding challenges remain a significant public health issue.
Internet-based integrated care is an innovative model that combines Internet technology with traditional care methods to provide personalized, continuous care services [13]. This model employs various tools such as mobile text messages, short videos, WeChat public accounts and groups, remote monitoring systems, and online platforms to enhance the accessibility and convenience of breastfeeding support [14]. By integrating the strengths of both online and offline interventions, Internet-based integrated care offers comprehensive breastfeeding support to primiparous women from hospitalization through post-discharge. Grounded in self-efficacy theory, this model allows nurses to provide education, technical guidance, and emotional support, significantly boosting first-time mothers’ breastfeeding confidence and skills.
The novelty of this study lies in its pioneering application of Internet-based integrated care to support breastfeeding among first-time mothers. By leveraging Internet technology, we deliver systematic and continuous breastfeeding counseling and support. This care model addresses the limitations of traditional care regarding time and location, improves the self-efficacy and knowledge level of primiparous women, and promotes higher exclusive breastfeeding rates. Thus it fills a research gap in China and provides a scientific basis and practical guidance for optimizing future breastfeeding support programs.
Materials and methods
Data information
This retrospective analysis utilized data from primiparous women who gave birth at Baoji People’s Hospital between July 2020 and September 2023. The study was approved by the Baoji People’s Hospital Medical Ethics Committee.
Inclusion and exclusion criteria
Maternal Inclusion Criteria: Healthy mothers with normal development and no breast diseases, primiparous women with a full-term singleton pregnancy, possession of a smartphone with the ability to use WeChat, and complete baseline data with telephone follow-up and outpatient review records.
Maternal Exclusion Criteria: Mothers with mental health issues, those unsuitable for breastfeeding, and those with conditions such as diabetes or hypertension.
Infant Inclusion Criteria: Infants with birth weight and length within the normal range, an Apgar score of ≥ 7 at 1 minute after birth, and complete baseline data.
Infant Exclusion Criteria: Preterm infants (gestational age less than 37 weeks), those with obvious deformities or significant medical conditions at birth, or those with metabolic diseases requiring special care or treatment.
Clinical data collection
Clinical data were obtained from electronic medical records and outpatient review records. Baseline data included maternal age, mode of delivery, place of residence, education level, type of occupation, annual family income, nipple condition, daily sucking frequency, breastfeeding success rate, breastfeeding knowledge scores, breastfeeding self-efficacy scores, and neonatal physical development indicators (weight, height, and head circumference). Post-intervention data refer to the period after 6 months of nursing intervention. Infant development indicators were collected during the six-month health check-up.
Nursing care model
Control group
Primiparous women in the control group did not use the Internet-based nursing services and received routine telephone follow-ups. Breastfeeding status and self-efficacy were assessed on the day of discharge, followed by scheduling a nurse visit to the hospital. Regular questionnaires were administered through routine post-discharge telephone follow-ups until 6 months postpartum.
Observation group
Primiparous women in the observation group opted for the Internet-based nursing service. In addition to the routine follow-up received by the control group, these women arranged for senior nurses to provide postpartum home care through WeChat. The healthcare team conducted randomized follow-up visits via WeChat and administered regular questionnaires to provide comprehensive nursing interventions until 6 months postpartum. The details of the intervention are as follows:
Dietary Guidance: Individual counseling sessions were provided, with a total of four dietary interventions arranged-one per week. The first session involved in-person guidance, followed by online recipe suggestions and dietary advice.
Breast Massage: During home visits, the primiparous woman was positioned supine. After cleansing the breasts with warm water, the nursing staff applied emollient oil and used the root of the palm to gently massage the breasts, encircling their base and performing multi-directional motions. One hand supported the lower end of the breast while the other massaged along the mammary ducts from the root to the nipple. Key points such as the danzhong and breast base were massaged in circular and longitudinal motions. Special attention was given to areas with hard nodes, with spiral massages performed clockwise. The thumb and forefinger were used to squeeze 2 cm from the nipple base, ensuring all breast sinuses were addressed. Each session lasted 25 minutes and was conducted once daily. Instruction on the use of breast pumps was also provided, recommending a maximum pumping time of 15 minutes.
Breastfeeding Knowledge and Skills Guidance: Breastfeeding manuals were distributed, explaining the benefits of breastfeeding for both mothers and newborns, as well as its economic value. During the first visit, nurses demonstrated proper newborn handling techniques based on the home environment.
Newborn Care: At the first visit, nurses demonstrated newborn touch techniques, accompanied by soft music, with appropriate room temperature and humidity settings. The standardized procedure involved gentle handling in the order of the head and face, chest, abdomen, and limbs, lasting 15-20 minutes each time, performed twice daily and after bathing. First-time mothers and their families were instructed on newborn bathing and umbilical care, with follow-up on the mother’s mastery of these skills conducted through WeChat.
Psychological Care: Primiparous women were encouraged to share their experiences. Based on their individual situations, methods such as encouragement, soothing, listening, and support were employed to provide psychological guidance.
Grouping
A total of 154 eligible cases were selected according to the inclusion and exclusion criteria and divided into a control group (n = 96) and an observation group (n = 58) based on the chosen intervention plan. The Internet-based integrated care intervention was a voluntary service, not mandatory or guided.
Functional scores
Breastfeeding knowledge score [15]: Assesses the mother’s understanding of the benefits of breastfeeding, feeding positions, and techniques. Each item is scored from 0 to 5, with a total possible score of 100 points. Higher scores indicate greater knowledge.
Breastfeeding self-efficacy score [16]: This score covers skills (20 items) and internal activities (13 items), with a total score range of 33 to 165 points. Scores range from 1 to 5, reflecting levels of confidence from “no confidence” to “very confident”. Higher scores indicate greater self-efficacy.
Observation indicators
Primary observation indicator
Comparison of breastfeeding success rates at 6 months postpartum between the control and observation groups. Logistic regression analysis was conducted to identify independent risk factors for exclusive breastfeeding.
Secondary outcome measures
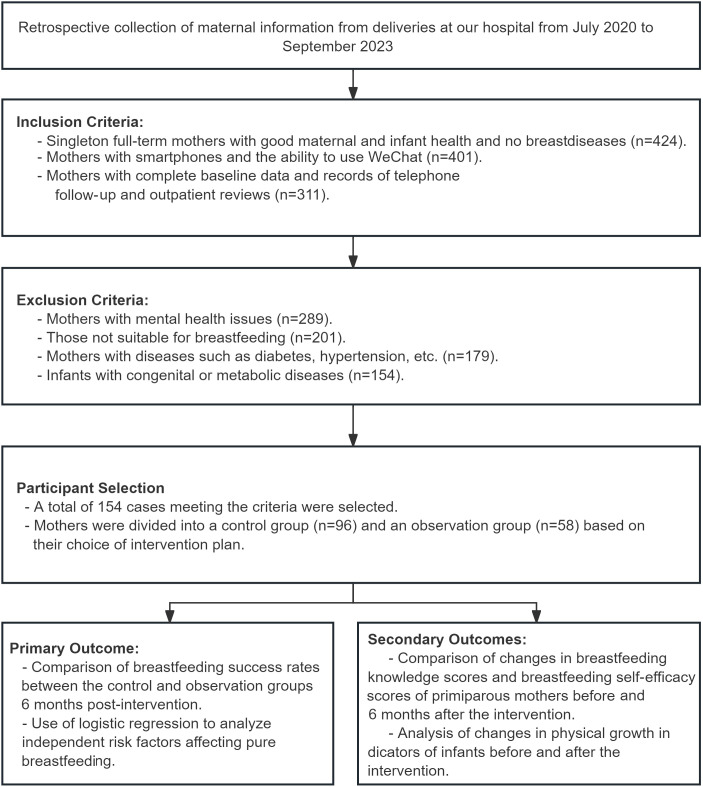
Comparison of breastfeeding knowledge and self-efficacy scores before and after the intervention. Analysis of neonatal physical development indicators before and after the intervention (Figure 1).
Figure 1.
Flow chart of sample screening and result measurement.
Statistical analysis
Data analysis was performed using SPSS software. Measurement data were expressed as mean ± standard deviation (SD ± mean), with normally distributed data analyzed using t-tests. The chi-squared test was used for categorical data. Logistic regression analysis was conducted to identify independent risk factors for exclusive breastfeeding. A P value of < 0.05 was considered statistically significant.
Results
Comparison of baseline data
A comparison of baseline data between the two groups revealed no statistically significant differences in age, mode of delivery, place of residence, education level, occupation, annual family income, nipple condition, and the number of daily suckles between the observation and control groups (all P > 0.05, Table 1).
Table 1.
Comparison of baseline patient data
| Factors | Observation group (n = 58) | Control group (n = 96) | χ2 value | P value |
|---|---|---|---|---|
| Age | ||||
| ≥ 30 years old | 34 | 61 | 0.370 | 0.543 |
| < 30 years old | 24 | 35 | ||
| Mode of delivery | ||||
| Normal delivery | 37 | 48 | 2.781 | 0.095 |
| Cesarean section | 21 | 48 | ||
| Place of residence | ||||
| City | 30 | 44 | 0.503 | 0.478 |
| Village | 28 | 52 | ||
| Educational level | ||||
| ~Junior High School | 12 | 15 | 3.433 | 0.180 |
| High School | 32 | 44 | ||
| College~ | 14 | 37 | ||
| Nature of occupation | ||||
| Full-time | 18 | 36 | 0.664 | 0.415 |
| Part-time | 40 | 60 | ||
| Annual family income | ||||
| < 50 K | 3 | 14 | 3.262 | 0.196 |
| 50 K-150 K | 26 | 39 | ||
| > 150 K | 29 | 43 | ||
| Nipple condition | ||||
| Normal | 53 | 82 | 1.189 | 0.276 |
| Abnormal | 5 | 14 | ||
| Number of sucking times per day | ||||
| < 5 times | 22 | 47 | 1.805 | 0.406 |
| 5-12 times | 32 | 43 | ||
| > 12 times | 4 | 6 |
Comparison of breastfeeding success rates
After six months of intervention, the breastfeeding success rate in the observation group was significantly higher than in the control group (P = 0.001, Table 2). Additionally, the overall breastfeeding success rate in the observation group was higher than in the control group (P = 0.004, Table 2).
Table 2.
Comparison of maternal breastfeeding success rate
| Group | Exclusive Breastfeeding | Mixed feeding | Artificial feeding | Breastfeeding success rate |
|---|---|---|---|---|
| Observation group (n = 58) | 43 | 6 | 9 | 43 (74.14%) |
| Control group (n = 96) | 45 | 23 | 28 | 45 (46.88%) |
| χ2 value | 11.065 | 10.973 | ||
| P value | 0.004 | 0.001 | ||
Comparison of breastfeeding knowledge and self-efficacy scores before and after intervention
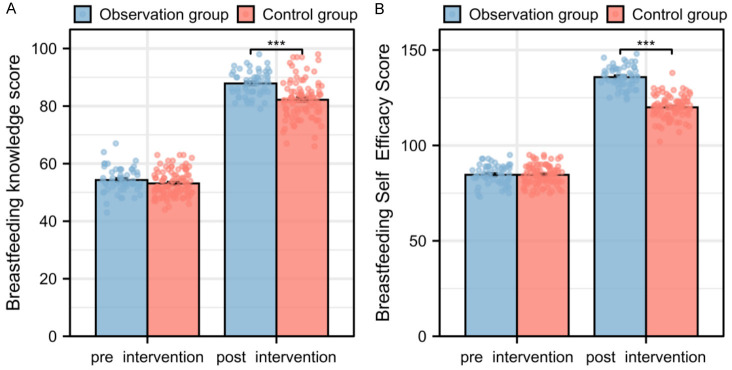
Before intervention, there were no statistically significant differences in breastfeeding knowledge and self-efficacy scores between the two groups (both P > 0.05, Figure 2). However, after the intervention, the breastfeeding knowledge and self-efficacy scores in the observation group were significantly higher than those in the control group, indicating a statistically significant difference (both P < 0.001, Figure 2).
Figure 2.
Comparison of breastfeeding knowledge and self-efficacy scores of first-time mothers before and after intervention. A. Comparison of breastfeeding knowledge scores before and after intervention. B. Comparison of self-efficacy scores of first-time mothers before and after intervention. Note: ***P < 0.001.
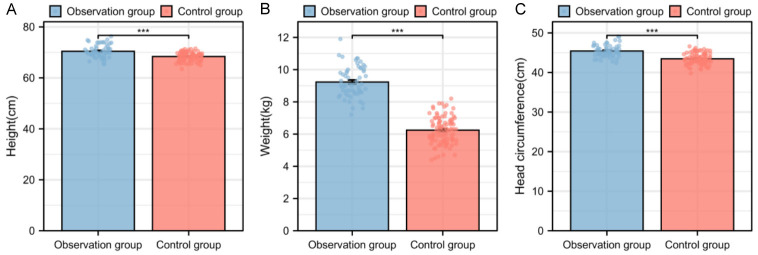
Comparison of newborn physical development indicators before and after maternal intervention
A comparison of neonatal physical development indicators showed that the body weight, height, and head circumference of neonates in the control group were all significantly lower than those in the observation group (all P < 0.001, Figure 3).
Figure 3.
Comparison of physical development indicators of newborns before and after intervention. A. Comparison of newborn height before and after intervention. B. Comparison of newborn weight before and after intervention. C. Comparison of newborn head circumference before and after intervention. Note: ***P < 0.001.
Analysis of risk factors for exclusive breastfeeding
Mothers were divided into two groups based on whether they exclusively breastfed: Exclusive Breastfeeding (n = 88) and Non-Exclusive Breastfeeding (n = 66). The analysis revealed statistically significant differences between the two groups in age (P = 0.010), mode of delivery (P = 0.006), education level (P = 0.003), occupation (P = 0.003), annual family income (P = 0.014), nipple condition (P = 0.016), number of daily suckles (P = 0.015), feeding schedule (P < 0.001), infant weight (P = 0.004), and infant head circumference (P = 0.031) (Table 3). Meaningful indicators were assigned values (Table 4), and multiple logistic regression analysis identified age (P = 0.019), mode of delivery (P = 0.006), and nipple condition (P = 0.029) as independent risk factors for exclusive breastfeeding. Education level (P < 0.001), occupation (P = 0.002), and number of daily suckles (P = 0.005) were identified as independent protective factors for exclusive breastfeeding (Table 5).
Table 3.
Analysis of factors influencing exclusive breastfeeding
| Factors | Exclusive breastfeeding (n = 88) | Non-exclusive breastfeeding (n = 66) | χ2 value | P value |
|---|---|---|---|---|
| Age | ||||
| ≥ 30 years old | 62 | 33 | 6.677 | 0.010 |
| < 30 years old | 26 | 33 | ||
| Mode of delivery | ||||
| Normal delivery | 57 | 28 | 7.617 | 0.006 |
| Cesarean section | 31 | 38 | ||
| Place of residence | ||||
| City | 40 | 34 | 0.555 | 0.456 |
| Village | 48 | 32 | ||
| Educational level | ||||
| ~Junior High School | 10 | 17 | 11.369 | 0.003 |
| High School | 40 | 36 | ||
| College~ | 38 | 13 | ||
| Nature of occupation | ||||
| Full-time | 22 | 32 | 9.135 | 0.003 |
| Part-time | 66 | 34 | ||
| Annual family income | ||||
| < 50 K | 7 | 10 | 8.589 | 0.014 |
| 50 K-150 K | 31 | 34 | ||
| > 150 K | 50 | 22 | ||
| Nipple condition | ||||
| Normal | 82 | 53 | 5.784 | 0.016 |
| Abnormal | 6 | 13 | ||
| Number of sucking times per day | ||||
| < 5 times | 31 | 38 | 8.392 | 0.015 |
| 5-12 times | 49 | 26 | ||
| > 12 times | 8 | 2 | ||
| Nursing care model | ||||
| Control group | 45 | 51 | 10.973 | < 0.001 |
| Observation group | 43 | 15 | ||
| Breastfeeding Knowledge Score | 54.07±4.25 | 52.89±4.56 | -1.627 | 0.106 |
| Breastfeeding Self-Efficacy Score | 85.00 [81.00, 88.00] | 85.00 [81.00, 89.00] | 0.79 | 0.429 |
| Infant weight (kg) | 7.75 [6.25, 9.00] | 6.55 [5.82, 7.52] | -2.862 | 0.004 |
| Infant height (cm) | 69.25 [67.88, 70.32] | 68.75 [67.90, 70.18] | -1.21 | 0.227 |
| Infant head circumference (cm) | 44.46±1.68 | 43.86±1.69 | -2.18 | 0.031 |
Table 4.
Assignment table
| Factors | Assignment |
|---|---|
| Age | ≥ 30 years old = 1, < 30 years old = 2 |
| Mode of delivery | Normal birth = 1, Cesarean birth = 2 |
| Educational level | ~Middle school = 1, High school = 2, college~ = 3 |
| Nature of occupation | Full-time = 1, Part-time = 2 |
| Annual family income | < 50 K = 1, 50-150 K = 2, > 150 K = 3 |
| Nipple condition | Normal = 1, Abnormal = 2 |
| Number of sucking times per day | < 5 times = 1, 5-12 times = 2, > 12 times = 3 |
| Nursing care model | Control group = 1, Observation group = 2 |
| Infant weight (kg) | ≤ 7.54 = 1, > 7.54 = 2 |
| Infant head circumference (cm) | ≤ 43.95 = 1, > 43.95 = 2 |
| Breastfeeding situation | Exclusive breastfeeding = 1, Non-exclusive breastfeeding = 2 |
Table 5.
Multivariate logistics regression analysis
| Factors | β | Std Error | P Value | OR | 95% CI |
|---|---|---|---|---|---|
| Age | 1.056 | 0.448 | 0.019 | 2.874 | 1.216-7.146 |
| Mode of delivery | 1.221 | 0.446 | 0.006 | 3.392 | 1.444-8.408 |
| Educational level | -1.217 | 0.341 | < 0.001 | 0.296 | 0.145-0.56 |
| Nature of occupation | -1.515 | 0.477 | 0.002 | 0.220 | 0.082-0.542 |
| Annual family income | -0.420 | 0.333 | 0.207 | 0.657 | 0.339-1.259 |
| Nipple condition | 1.485 | 0.682 | 0.029 | 4.416 | 1.196-17.95 |
| Number of sucking times per day | -1.051 | 0.378 | 0.005 | 0.349 | 0.161-0.713 |
| Nursing care model | 0.509 | 0.969 | 0.599 | 1.664 | 0.216-10.793 |
| Infant weight (kg) | -0.786 | 0.902 | 0.384 | 0.456 | 0.065-2.493 |
| Infant head circumference (cm) | -0.597 | 0.511 | 0.243 | 0.551 | 0.198-1.494 |
Discussion
Breastfeeding is the optimal method for feeding newborns, offering complete nutrition and immune protection, enhancing immunity, and reducing the risk of disease [17]. The World Health Organization and UNICEF recommend exclusive breastfeeding for the first six months of life, with continued breastfeeding up to two years or longer [18]. Breastfeeding supports brain development, strengthens bowel function, and lowers the risk of allergies, infections, obesity, and chronic diseases such as diabetes. It also fosters a strong emotional bond between mother and child, aids in the mother’s postpartum recovery, and reduces the risk of postpartum complications [19]. In contrast, not breastfeeding can negatively impact newborn health, and artificial feeding can increase the burden on families and society. Therefore, improving breastfeeding rates and duration is crucial for enhancing neonatal health and reducing healthcare burdens.
In this study, we observed that the Internet-based integrated care model significantly improved breastfeeding knowledge scores, self-efficacy scores, and breastfeeding success rates among first-time mothers. Specifically, the performance of mothers in the observation group on these three indicators was superior to that of mothers in the control group. This difference is likely due to the personalized and continuous support provided by the Internet-based integrated care model. The combination of online counseling and offline visits allows first-time mothers to receive timely answers to their questions and emotional support, thereby boosting their confidence in breastfeeding and their ability to manage challenges [20]. This is consistent with findings by Maleki et al., who reported that educational interventions significantly improve mothers’ breastfeeding self-efficacy in a review of 40 randomized controlled trials [21]. Furthermore, the meta-analysis by Sun et al. supports our results, showing that Internet-based breastfeeding intervention models can effectively increase exclusive breastfeeding rates [22]. These findings suggest that Internet-based breastfeeding services can effectively support mothers in their breastfeeding efforts.
Our study also found that newborns of mothers in the observation group had better outcomes in terms of weight, height, and head circumference compared to those in the control group, highlighting the importance of high-quality breastfeeding support for healthy neonatal development. Similar studies by Wong [23] and Chipojola [24] also have emphasized that face-to-face education and telephone follow-up during the antenatal and postnatal periods can effectively improve exclusive breastfeeding rates, partial breastfeeding rates, and breastfeeding self-efficacy at 6 months and 2 months postpartum among first-time mothers. Our findings align with existing literature and further validate the effectiveness of the Internet-based integrated care model in promoting breastfeeding and supporting healthy newborn development. The successful implementation of this model provides a scientific basis and practical guidance for optimizing and promoting future breastfeeding support programs, which is expected to improve breastfeeding rates globally and foster healthy growth in newborns.
Exclusive breastfeeding is the most ideal feeding method during the early growth of infants. It provides essential nutrition, strengthens the infant’s immunity by transferring maternal antibodies through breast milk, promotes intellectual development, and helps prevent obesity and allergic diseases [25]. However, despite its many benefits, exclusive breastfeeding rates are influenced by various factors, including the mother’s personal choices, level of knowledge, social support, and medical conditions [26]. Analyzing these determinants is crucial for improving exclusive breastfeeding rates, as it helps identify and address potential barriers, thereby ensuring optimal growth conditions for infants.
In this study, multivariate logistic regression analysis identified several key factors influencing exclusive breastfeeding among mothers. Younger mothers may encounter more challenges with breastfeeding due to a lack of experience and understanding of the process. Mothers who have undergone cesarean sections may face difficulties initiating breastfeeding early due to postoperative recovery, which can hinder timely skin-to-skin contact and colostrum feeding [27]. Nipple abnormalities may also prevent proper latch, leading to breastfeeding difficulties [28]. Additionally, mothers with higher levels of education are more likely to understand and appreciate the benefits of breastfeeding, making them more likely to adhere to exclusive breastfeeding [29]. Mothers not engaged in full-time work may find it easier to accommodate breastfeeding needs due to more flexible schedules [30]. Furthermore, frequent daily suckling can stimulate mammary gland secretion, increase milk production, and support breastfeeding success [31].
Interestingly, the intervention program itself was not identified as a risk or protective factor for exclusive breastfeeding. This may be because the intervention was designed to offer general support and guidance rather than address individual differences. While the program included enhancements in breastfeeding knowledge, skills training, and psychological support beneficial to all mothers, it may not have been sufficient to address more complex or individualized issues, such as nipple abnormalities or specific medical conditions. Additionally, the acceptance, participation, and quality of implementation by mothers could also influence the program’s effectiveness. Thus, while the intervention program is a positive initiative, it may need to be combined with other personalized support measures to more comprehensively address the various factors influencing exclusive breastfeeding.
This study is valuable but has limitations. The sample size and retrospective design may introduce bias and limit the generalizability of the results. Future research should expand the sample size and adopt prospective randomized controlled trials to enhance the accuracy and reliability of the findings. Moreover, standardization of intervention measures should be strengthened to ensure quality control. Long-term impact evaluations are also crucial to understanding the lasting effects of interventions. Additionally, optimizing intervention strategies for the control group is necessary to more comprehensively assess the efficacy of different support strategies. Future research should also consider regional differences and explore the impact of socioeconomic and cultural backgrounds on breastfeeding to provide a foundation for effective breastfeeding support strategies.
In conclusion, this study compares the impact of the Internet-based integrated care model with traditional care on breastfeeding among first-time mothers. The findings suggest that the Internet-based model significantly improves breastfeeding knowledge, self-efficacy, and the success rate of exclusive breastfeeding among mothers, while also contributing to better physical development indicators in newborns.
Disclosure of conflict of interest
None.
References
- 1.Pérez-Escamilla R, Tomori C, Hernández-Cordero S, Baker P, Barros AJD, Bégin F, Chapman DJ, Grummer-Strawn LM, McCoy D, Menon P, Ribeiro Neves PA, Piwoz E, Rollins N, Victora CG, Richter L 2023 Lancet Breastfeeding Series Group. Breastfeeding: crucially important, but increasingly challenged in a market-driven world. Lancet. 2023;401:472–485. doi: 10.1016/S0140-6736(22)01932-8. [DOI] [PubMed] [Google Scholar]
- 2.Doherty T, Horwood C, Pereira-Kotze C, du Plessis L, Witten C. Stemming commercial milk formula marketing: now is the time for radical transformation to build resilience for breastfeeding. Lancet. 2023;401:415–418. doi: 10.1016/S0140-6736(23)00095-8. [DOI] [PubMed] [Google Scholar]
- 3.O’Leary K. Breastfeeding supports healthy gut bacteria in infants. Nat Med. 2021;6:1–20. doi: 10.1038/d41591-021-00069-7. [DOI] [PubMed] [Google Scholar]
- 4.Mennini M, Arasi S, Fiocchi AG. Allergy prevention through breastfeeding. Curr Opin Allergy Clin Immunol. 2021;21:216–221. doi: 10.1097/ACI.0000000000000718. [DOI] [PubMed] [Google Scholar]
- 5.Luby JL, Belden AC, Whalen D, Harms MP, Barch DM. Breastfeeding and childhood IQ: the mediating role of gray matter volume. J Am Acad Child Adolesc Psychiatry. 2016;55:367–375. doi: 10.1016/j.jaac.2016.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abrego Del Castillo KY, Dennis CL, Wamithi S, Briollais L, McGowan PO, Dol J, Lye SJ. Maternal BMI, breastfeeding and perinatal factors that influence early childhood growth trajectories: a scoping review. J Dev Orig Health Dis. 2022;13:541–549. doi: 10.1017/S2040174421000726. [DOI] [PubMed] [Google Scholar]
- 7.Anderson CE, Whaley SE, Crespi CM, Wang MC, Chaparro MP. Every month matters: longitudinal associations between exclusive breastfeeding duration, child growth and obesity among WIC-participating children. J Epidemiol Community Health. 2020;74:785–791. doi: 10.1136/jech-2019-213574. [DOI] [PubMed] [Google Scholar]
- 8.Henshaw EJ. Breastfeeding and postpartum depression: a review of relationships and potential mechanisms. Curr Psychiatry Rep. 2023;25:803–808. doi: 10.1007/s11920-023-01471-3. [DOI] [PubMed] [Google Scholar]
- 9.Xiao L. Agomelatine for postpartum depression and breastfeeding. Ther Adv Psychopharmacol. 2021;11:20451253211022172. doi: 10.1177/20451253211022172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Roza JG, Fong MK, Ang BL, Sadon RB, Koh EYL, Teo SSH. Exclusive breastfeeding, breastfeeding self-efficacy and perception of milk supply among mothers in Singapore: a longitudinal study. Midwifery. 2019;79:102532. doi: 10.1016/j.midw.2019.102532. [DOI] [PubMed] [Google Scholar]
- 11.Tawia S, Bailey C, McGuire E, James J. Breastfeeding: Australian breastfeeding association volunteers are positive deviants in Australian society. Women Birth. 2020;33:e385–e390. doi: 10.1016/j.wombi.2019.09.001. [DOI] [PubMed] [Google Scholar]
- 12.Liu K, Guo J, Deng W, Su Y. The current status of breastfeeding knowledge and its influencing factors in nursing undergraduates: a cross-sectional study in China. Int J Environ Res Public Health. 2022;20:103. doi: 10.3390/ijerph20010103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yao J, He W, Chen H, Qi Y. Nursing effect of continuous nursing intervention based on “Internet Plus” on patients with severe adrenal tumor. Medicine (Baltimore) 2023;102:e33187. doi: 10.1097/MD.0000000000033187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen Y, Qiu C, Chen J, Li L, Xu J, Sheng Z. Effect of the internet combined with exercise-based individualized nursing intervention in patients with gestational diabetes mellitus. Diabetol Metab Syndr. 2021;13:125. doi: 10.1186/s13098-021-00738-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jiang H, Li M, Yang D, Wen LM, Hunter C, He G, Qian X. Awareness, intention, and needs regarding breastfeeding: findings from first-time mothers in Shanghai, China. Breastfeed Med. 2012;7:526–534. doi: 10.1089/bfm.2011.0124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vieira ES, Caldeira NT, Eugênio DS, Lucca MMD, Silva IA. Breastfeeding self-efficacy and postpartum depression: a cohort study. Rev Lat Am Enfermagem. 2018;26:e3035. doi: 10.1590/1518-8345.2110.3035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brown HK, Taylor C, Vigod SN, Dennis CL, Fung K, Chen S, Guttmann A, Havercamp SM, Parish SL, Ray JG, Lunsky Y. Disability and in-hospital breastfeeding practices and supports in Ontario, Canada: a population-based study. Lancet Public Health. 2023;8:e47–e56. doi: 10.1016/S2468-2667(22)00310-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fan WQ, Chan C, Paterson S, Foster K, Morrow M, Bourne D, Ashworth J. Weekly proactive telephone breastfeeding standard care by lactation consultants in the first month postpartum prolongs breastfeeding for up to 6 months. Nutrients. 2023;15:2075. doi: 10.3390/nu15092075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yu J, Pudwell J, Dayan N, Smith GN. Postpartum breastfeeding and cardiovascular risk assessment in women following pregnancy complications. J Womens Health (Larchmt) 2020;29:627–635. doi: 10.1089/jwh.2019.7894. [DOI] [PubMed] [Google Scholar]
- 20.Almohanna AA, Win KT, Meedya S. Effectiveness of internet-based electronic technology interventions on breastfeeding outcomes: systematic review. J Med Internet Res. 2020;22:e17361. doi: 10.2196/17361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maleki A, Faghihzadeh E, Youseflu S. The effect of educational intervention on improvement of breastfeeding self-efficacy: a systematic review and meta-analysis. Obstet Gynecol Int. 2021;2021:5522229. doi: 10.1155/2021/5522229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sun Y, Gao Y, Zhu Z, Zhu L. Effect of online intervention mode on breastfeeding results: a systematic review and meta-analysis. Reprod Health. 2023;20:164. doi: 10.1186/s12978-023-01701-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wong MS, Mou H, Chien WT. Effectiveness of educational and supportive intervention for primiparous women on breastfeeding related outcomes and breastfeeding self-efficacy: a systematic review and meta-analysis. Int J Nurs Stud. 2021;117:103874. doi: 10.1016/j.ijnurstu.2021.103874. [DOI] [PubMed] [Google Scholar]
- 24.Chipojola R, Chiu HY, Huda MH, Lin YM, Kuo SY. Effectiveness of theory-based educational interventions on breastfeeding self-efficacy and exclusive breastfeeding: a systematic review and meta-analysis. Int J Nurs Stud. 2020;109:103675. doi: 10.1016/j.ijnurstu.2020.103675. [DOI] [PubMed] [Google Scholar]
- 25.Søegaard SH, Andersen MM, Rostgaard K, Davidsson OB, Olsen SF, Schmiegelow K, Hjalgrim H. Exclusive breastfeeding duration and risk of childhood cancers. JAMA Netw Open. 2024;7:e243115. doi: 10.1001/jamanetworkopen.2024.3115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bizon AMBL, Giugliani C, Giugliani ERJ. Women’s satisfaction with breastfeeding and risk of exclusive breastfeeding interruption. Nutrients. 2023;15:5062. doi: 10.3390/nu15245062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cato K, Sylvén SM, Lindbäck J, Skalkidou A, Rubertsson C. Risk factors for exclusive breastfeeding lasting less than two mon ths-Identifying women in need of targeted breastfeeding support. PLoS One. 2017;12:e0179402. doi: 10.1371/journal.pone.0179402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wood NK, Odom-Maryon T, Smart DA. Factors associated with exclusive direct breastfeeding in the first 3 months. Nurs Womens Health. 2022;26:299–307. doi: 10.1016/j.nwh.2022.05.006. [DOI] [PubMed] [Google Scholar]
- 29.Chandrika P, Bhakhri BK, Gathwala G, Narwal V, Chaturvedi A. Risk factors for discontinuation of exclusive breastfeeding by one month of postnatal age among high risk newborns: an institution based case control study. J Clin Diagn Res. 2015;9:SC01–03. doi: 10.7860/JCDR/2015/11570.5999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wu Q, Tang N, Wacharasin C. Factors influencing exclusive breastfeeding for 6 months postpartum: a systematic review. Int J Nurs Knowl. 2022;33:290–303. doi: 10.1111/2047-3095.12360. [DOI] [PubMed] [Google Scholar]
- 31.Rynjah MM, Venkatachalam J, Adhisivam B, Olickal JJ, Sundaram SP, Chinnakali P. Non-exclusive breastfeeding amongst high-risk children: factors and barriers associated with non-exclusive breastfeeding at a tertiary care hospital in Southern India. Niger Postgrad Med J. 2021;28:62–67. doi: 10.4103/npmj.npmj_294_20. [DOI] [PubMed] [Google Scholar]