Abstract
Objective: To investigate the application of Enhanced Recovery After Surgery (ERAS) in the nursing care of patients undergoing Thulium laser prostatectomy and analyze the factors affecting postoperative complications. Methods: This retrospective study analyzed the clinical data of 108 patients who underwent Thulium Laser Prostatectomy in the Zhejiang University Sir Run Run Shaw Alaer Hospital from July 2022 to October 2023. Among them, 58 patients who received nursing care based on the concept of ERAS from January 2023 to October 2023 were assigned to the study group, while the other 50 patients who received conventional nursing care from July 2022 to December 2022 were assigned to the control group. Postoperative recovery indicators, satisfaction with nursing care services, and postoperative complications were analyzed. Logistic regression analysis was used to identify factors affecting complications after Thulium laser prostatectomy. Results: The study group showed significantly shorter time to first flatus, lower pain scores on the first day after surgery, shorter time to first out-of-bed activity, and shorter hospital stay than the control group (all P < 0.0001). Compared with the control group, the study group expressed notably higher nursing care satisfaction (P=0.0151) and showed a significantly lower incidence of postoperative complications (P=0.0236). Logistic regression analysis identified disease duration and nursing care intervention as independent risk factors affecting patient complications. Conclusion: For patients undergoing Thulium Laser Prostatectomy, ERAS contributes to good postoperative recovery and patient satisfaction and less complications. Disease duration and nursing care intervention were identified as independent factors impacting post-operative complications.
Keywords: Enhanced recovery after surgery, thulium laser prostatectomy, nursing care satisfaction, postoperative complications
Introduction
Benign prostatic hyperplasia (BPH) is a prevalent condition affecting the urinary system, primarily observed in middle-aged and elderly individuals. It is characterized by symptoms including urinary urgency, increased frequency of urination, difficulties in initiating and maintaining a steady urine flow, and occasionally mild blood in the urine [1,2]. As the disease progresses, BPH can impair kidney function, significantly affecting the health and quality of life of patients. Thulium laser prostatectomy is a commonly used surgical procedure for treating BPH. This procedure has a short operation time and minimal bleeding, significantly reducing the trauma caused to patients during surgery. This surgical approach is beneficial for promoting patient recovery and facilitating their rehabilitation [3,4]. However, patients undergoing Thulium laser prostatectomy for BPH are often elderly, with many having underlying comorbidities, which can result in slower postoperative recovery, prolonged hospitalization, and increased risk of postoperative infections [5]. Therefore, conducting research to expedite postoperative recovery in patients undergoing thulium laser prostatectomy holds great significance.
Enhanced Recovery After Surgery (ERAS) is a novel perioperative management strategy based on evidence-based medicine. It aims to optimize nursing care interventions and implement a multidisciplinary approach by applying various interventions before, during, and after surgery [6,7]. ERAS can help reduce perioperative trauma and stress responses, shorten hospital stay, and subsequently decrease hospital costs. Nursing based on ERAS involves the implementation of evidence-based interventions throughout the perioperative period [7]. This includes preoperative patient education, optimizing patients’ preoperative condition, infection prevention, advocacy and communication, perioperative fluid management, postoperative pain management, early mobilization, postoperative nausea and vomiting (PONV) prophylaxis, nutritional support, wound care and monitoring, discharge planning and education, as well as providing emotional support to patients and their families [8]. However, there is currently limited research on the value of the concept of ERAS in patients undergoing thulium laser prostatectomy. ERAS protocols have been successfully implemented in various surgical procedures, such as esophageal cancer resection [8] and bariatric surgery [9]. However, the application and outcomes of ERAS in the context of thulium laser prostatectomy require further investigation.
Accordingly, this study retrospectively investigated patients who underwent thulium laser prostatectomy in the Sir Run Run Shaw Hospital Affiliated with Zhejiang University School of Medicine and analyzed the value of the ERAS concept and factors impacting postoperative complications in such patients.
Materials and methods
Sample source
With the approval of the Medical Ethics Committee of the Zhejiang University Sir Run Run Shaw Alaer Hospital (ethnical approval number: Lw2023001), this retrospective study analyzed the clinical data of 150 patients who underwent thulium laser prostatectomy in the Zhejiang University Sir Run Run Shaw Alaer Hospital from July 2022 to October 2023.
Screening and grouping
Based on the following criteria, 108 eligible patients were selected from the initial pool of 150 patients. Inclusion criteria: (1) patients who were clinically diagnosed with prostatic hyperplasia and underwent thulium laser prostatectomy; (2) patients without contraindications for surgery; (3) patients without a history of previous prostate surgery; (4) patients with complete clinical data. Exclusion criteria: (1) patients with concurrent presence of other prostatic diseases; (2) patients with neurogenic bladder; (3) patients with preoperative complications; (4) patients with brain disorders or mental illnesses.
Among the 108 eligible patients, 58 patients who received nursing care based on the concept of ERAS from January 2023 to October 2023 were assigned to the study group, while the other 50 who received conventional care from July 2022 to December 2022 were placed in the control group. The screening and grouping process is detailed in Figure 1.
Figure 1.
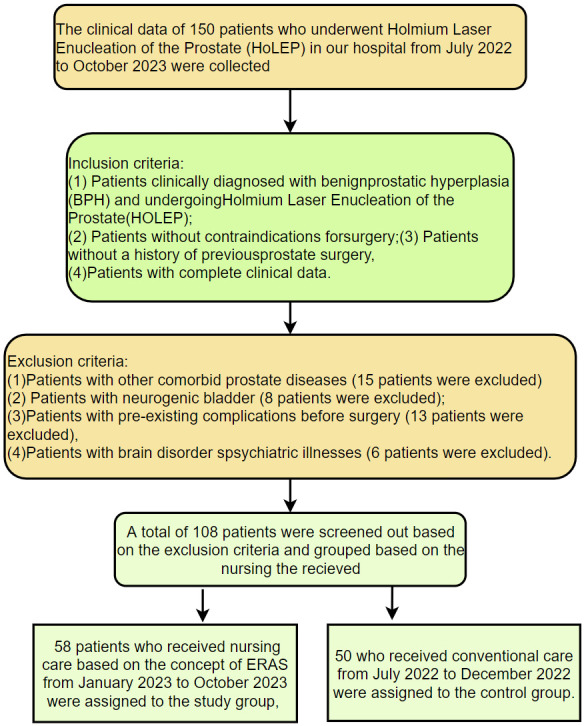
Flow chart of screening and grouping.
Nursing care methods
The control group received conventional nursing care [10], which included preoperative testing, preoperative psychological care, dietary guidance, informing about the surgical procedure, routine skin preparation, bedpan using practice, and regular fasting and fluid restrictions. Postoperatively, the control group received standard care, which included monitoring vital signs, catheter care, observing the patient’s condition, providing dietary and nursing guidance, and giving discharge instructions.
The study group received ERAS-based nursing [11], with the following specific process: (1) Preoperative nursing: After admission, nursing personnel was arranged to thoroughly review the patient’s clinical data and medical history, and implement detailed nursing preparations based on the characteristics of the surgery. A nursing plan was developed based on the patient’s underlying medical conditions. For patients with comorbid diabetes, collaboration with an endocrinologist was necessary to manage blood glucose levels during the perioperative period. Special attention was given to intraoperative bleeding issues as well as postoperative dietary and activity considerations. In addition, respiratory training, meditation training, and simplified health education on the surgical treatment plan were implemented to reduce the negative psychological impact on the surgical treatment and enhance preoperative nutritional support. Patients were instructed to refrain from drinking for 4 hours and eating for 6 hours before the surgery. Patients were provided with detailed information about the specific surgical procedure and potential postoperative adverse reactions in order to alleviate their anxiety levels. (2) Intraoperative nursing: Positioning adjustments were made during the surgery, and cotton pads were placed on pressure areas to prevent localized pressure injuries. After establishing intravenous access, a heating device was used to ensure that the temperature of the infusion fluid was maintained at 32°C to 34°C. The infusion rate was controlled according to the patient’s condition. The operating room temperature was adjusted to 24°C to 26°C, and thin blankets were prepared, with particular attention given to thermal care for the patient’s head and extremities. The exposure of the patient’s skin surface and duration was limited during the surgery. The irrigation solution was preheated to 32°C to 34°C. Warm irrigation was performed using the heated solution to ensure effective bladder irrigation while minimizing the impact of cold stimuli on the patient. The irrigation fluid was promptly replenished as necessary to maintain unobstructed drainage. (3) Postoperative nursing: Observation of the patient’s condition: The patients’ vital signs were closely monitored. For patients with nausea or a tendency to vomit, antiemetic medications can be administered. Additionally, a patient-controlled analgesia pump can be used to assist the patient in adjusting their pain medication usage. Diet and bowel care: Six hours after surgery, a dietary plan was implemented for the patient in the sequence of clear liquid, semi-liquid, and regular diet. The patient was advised to follow a light and balanced diet in their daily routine, with an emphasis on consuming foods rich in protein and fiber to prevent constipation. Urinary catheter care: The urinary catheter was placed in the lower right abdomen of the patient, ensuring that the right lower rib area was in contact with the Y junction of the catheter to maintain its patency.
To ensure that both the control group and the study group receive high-quality care, detailed nursing strategies and measures for each group were carried out, including specific steps and requirements. These guidelines were based on best practices and the latest clinical guidelines. Comprehensive training and education were provided to nursing staff to ensure they are equipped with the knowledge and skills required to implement the nursing strategies. The training included theoretical courses, practical training, and simulation exercises. Clear clinical pathways and workflow processes were established to integrate the nursing strategies into care practices. Responsibility was clearly defined and assigned to ensure effective execution at each stage.
Data collection
Patient clinical data was collected through outpatient visits and medical records, including age, body mass index (BMI), disease duration, comorbidities, bladder stones, anticoagulant therapy, place of residence, time to first postoperative rectal flatus, pain score on the first day after surgery, time to first out-of-bed activity, length of hospital stay, satisfaction with nursing services, and postoperative complications.
Outcome measures
The primary outcome measures encompassed postoperative recovery indicators, including time to first post-operative flatus, pain score on the first day after surgery, time to first out-of-bed activity, length of hospital stay, satisfaction with nursing services at discharge, and occurrence of postoperative complications during hospitalization.
The secondary outcome measures included the baseline data of the two groups. Based on the occurrence of postoperative complications, the patients were divided into the complication group and the non-complication group. Logistic regression analysis was performed to identify factors affecting complications in patients undergoing thulium laser prostatectomy.
Evaluation criterion
Postoperative pain was evaluated using the Numeric Rating Scale (NRS), which uses numbers from 0 to 10 to represent different levels of pain, with higher scores indicating more severe pain [12]. Patient satisfaction with the quality of nursing care service was assessed through a satisfaction survey questionnaire at the time of discharge, including categories such as very satisfied, somewhat satisfied, and dissatisfied, with the first two categories considered in the overall satisfaction rate.
Statistical analyses
SPSS 20.0 was used for statistical analysis, while GraphPad Prism 7 was employed for graphical representation. Counting data were presented as [n (%)] and inter-group comparisons were conducted using χ2 tests. Measurement data were normally distributed and expressed as mean ± standard deviation. Inter-group comparisons were performed using t-tests. Logistic regression was used to analyze the factors influencing the complications. A p-value of < 0.05 was considered statistically significant.
Results
Baseline data of patients
Analysis of the baseline data of the two groups revealed no notable differences between the two groups in terms of age, BMI, disease duration, comorbidities such as diabetes (all P > 0.05, Table 1).
Table 1.
Comparison of baseline data between the two groups
| Factors | Study group (n=58) | Control group (n=50) | P value |
|---|---|---|---|
| Age | 70.41±4.91 | 70.56±4.26 | 0.8640 |
| BMI | 23.54±2.67 | 24.29±3.52 | 0.2141 |
| Course of disease | 3.4±1.1 | 3.6±2.0 | 0.3406 |
| Comorbid diabetics | 0.7247 | ||
| Yes | 12 | 9 | |
| No | 46 | 41 | |
| Comorbid hypertension | 0.9178 | ||
| Yes | 10 | 9 | |
| No | 48 | 41 | |
| Operation time (min) | 73.18±5.76 | 73.18±8.98 | 0.8721 |
| Intraoperative blood loss (mL) | 153.49±23.77 | 154.28±21.79 | 0.2146 |
| Place of residence | 0.8692 | ||
| Rural area | 38 | 32 | |
| Urban area | 20 | 18 |
BMI: Body mass index.
Postoperative recovery indexes of the two groups
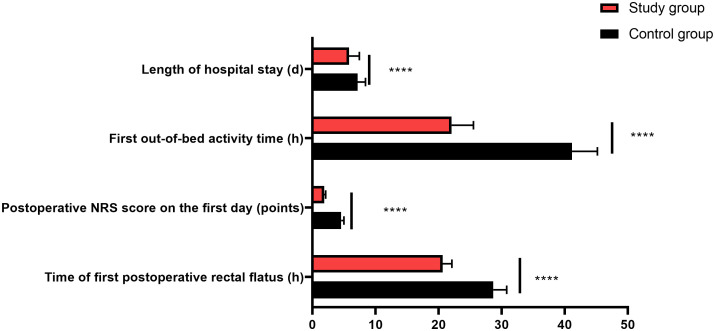
The study group demonstrated significantly shorter time to first postoperative rectal flatus, lower pain scores on the first day after surgery, earlier time to first out-of-bed activity, and shorter length of hospital stay compared to the control group (all P < 0.0001, Figure 2).
Figure 2.
Comparison of postoperative recovery indexes between the two groups. Note: ****P < 0.0001.
Satisfaction rate of nursing care service in the two groups
The study group showed notably higher satisfaction rate with nursing care services than that the control group (P=0.0151, Table 2).
Table 2.
Comparison of nursing care satisfaction between the two groups [n (%)]
| Group | Highly satisfied | Satisfied | Dissatisfied | Total satisfaction rate |
|---|---|---|---|---|
| Control group (n=50) | 19 (38.00%) | 24 (48.00%) | 7 (14.00%) | 43 (86.00%) |
| Study group (n=58) | 36 (62.07%) | 21 (36.21%) | 1 (1.72%) | 57 (98.28%) |
| χ2 | 1.5361 | 5.9001 | ||
| P | 0.2151 | 0.0151 |
Postoperative complications in the two groups
The study group showed a significantly lower incidence of postoperative complications compared to the control group (P=0.0236, Table 3).
Table 3.
Comparison of postoperative complications between the two groups [n (%)]
| Group | Deep vein thrombosis | Urinary incontinence | Urinary tract infection | Total |
|---|---|---|---|---|
| Control group (n=50) | 2 (4.00%) | 5 (10.00%) | 4 (8.00%) | 11 (22.00%) |
| Study group (n=58) | 0 (0%) | 2 (3.45%) | 2 (3.45%) | 4 (6.90%) |
| χ2 | 2.3641 | 1.9021 | 1.0601 | 5.1221 |
| P | 0.1242 | 0.1679 | 0.3032 | 0.0236 |
Analysis of factors influencing postoperative complications in patients
Based on the occurrence of complications in patients, the patients were further categorized into a complication group (n=15) and a non-complication group (n=93). Comparison of relevant data between the two groups revealed that age, disease duration, comorbidities such as diabetes and hypertension, bladder stones, anticoagulant therapy, and nursing care intervention methods showed significant differences between the complication and non-complication groups (Table 4). These significant indicators were assigned with values (Table 5) and subjected to multivariate analysis. Logistic regression analysis revealed that disease duration and nursing care intervention methods were independent risk factors influencing post-operative complications (Table 6).
Table 4.
Univariate analysis of factors affecting post-operative complications
| Factors | Non-complication group (n=93) | Complication group (n=15) | P value |
|---|---|---|---|
| Age | 0.0036 | ||
| ≥ 70 years old | 43 | 13 | |
| < 70 years old | 50 | 2 | |
| BMI | 0.2854 | ||
| ≥ 23 kg/m2 | 51 | 6 | |
| < 23 kg/m2 | 42 | 9 | |
| Course of disease | 0.0428 | ||
| ≥ 3.5 years | 42 | 11 | |
| < 3.5 years | 51 | 4 | |
| Comorbid diabetics | 0.0041 | ||
| Yes | 14 | 7 | |
| No | 79 | 8 | |
| Comorbid hypertension | 0.0140 | ||
| Yes | 13 | 6 | |
| No | 80 | 9 | |
| Bladder stones | 0.0002 | ||
| Yes | 12 | 8 | |
| No | 81 | 7 | |
| Anticoagulation therapy | 0.0237 | ||
| Yes | 8 | 4 | |
| No | 95 | 11 | |
| Nursing care intervention mode | 0.0277 | ||
| Enhanced recovery after surgery | 46 | 12 | |
| Conventional nursing | 47 | 3 | |
| Place of residence | 0.3156 | ||
| Rural area | 62 | 8 | |
| Urban area | 31 | 7 |
BMI: Body mass index.
Table 5.
Assignment table
| Factors | Assignment |
|---|---|
| Age | < 70 years old =0, ≥ 70 years old =1. |
| Disease duration | < 3.5 years =0, ≥ 3.5 years =1. |
| Comorbid diabetics | No =0, Yes =1. |
| Comorbid hypertension | No =0, Yes =1. |
| Bladder stones | No =0, Yes =1. |
| Anticoagulation therapy | < None =0, Yes =1. |
| Nursing care intervention method | Enhanced recovery after surgery nursing =0, Conventional nursing =1. |
| Complications | No complications =0, with complications =1. |
Table 6.
Multivariate logistic regression analysis of factors affecting post-operative complications
| Factors | B | S.E. | Wals | df | Sig. | Exp (B) | 95% C.I. for EXP (B) | |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Lower limit | Upper limit | |||||||
| Age | -0.380 | 0.730 | 0.270 | 1 | 0.603 | 0.684 | 0.164 | 2.861 |
| Disease duration | -1.297 | 0.648 | 4.003 | 1 | 0.045 | 0.273 | 0.077 | 0.974 |
| Comorbid diabetics | 0.611 | 0.709 | 0.742 | 1 | 0.389 | 1.842 | 0.459 | 7.392 |
| Comorbid hypertension | -0.499 | 0.859 | 0.337 | 1 | 0.561 | 0.607 | 0.113 | 3.272 |
| Bladder stones | -1.724 | 1.111 | 2.406 | 1 | 0.121 | 0.178 | 0.020 | 1.575 |
| Anticoagulation therapy | 0.270 | 0.955 | 0.080 | 1 | 0.778 | 1.310 | 0.201 | 8.518 |
| Nursing care intervention method | 1.800 | 0.674 | 7.122 | 1 | 0.008 | 6.048 | 1.613 | 22.681 |
Discussion
Enhanced Recovery After Surgery (ERAS) nursing is a comprehensive nursing model that involves multidisciplinary teamwork [12-15]. It aims to optimize the nursing process for patients before, during, and after surgery to minimize the occurrence of complications, shorten hospital stays, and improve patient recovery speed [16]. This nursing model has been widely applied globally and is widely recognized as an effective approach to improving the care of surgical patients [17,18]. Choi et al. [19] found that the application of ERAS nursing in patients undergoing colon cancer surgery effectively improved patient compliance and enhances survival outcomes. Cao et al. [20] discovered that ERAS nursing can be applied to elderly gastric cancer patients undergoing laparoscopic total gastrectomy, and it helped improve impaired immune function and suppress inflammatory response.
In this study, the application of the ERAS nursing resulted in significantly earlier time of first postoperative rectal flatus in the study group compared to the control group. This can be attributed to several factors. Firstly, the ERAS concept emphasizes early rehabilitation measures such as early mobilization and respiratory training, which promote bowel motility and gas expulsion [21]. Secondly, the importance of fluid intake and dietary management is emphasized to maintain fluid-electrolyte balance and bowel activity, which helps facilitate bowel function recovery [22]. These factors collectively make the ERAS concept more effective in promoting postoperative bowel function recovery. The study group reported notably lower pain scores on the first day after surgery compared to the control group. This can be attributed to the emphasis of the ERAS concept on individualized pain management. By addressing individual patient differences and providing personalized pain management plans based on specific patient conditions and needs, ERAS offers more effective pain relief measures [23]. In addition, the study group demonstrated better performance in terms of the time to first out-of-bed activity and length of hospital stay. The ERAS concept emphasizes early rehabilitation measures, including early mobilization, which facilitates improved blood circulation, prevents complications, and expedites the recovery process, ultimately leading to a shorter hospital stay [24]. The collaboration of multidisciplinary teams, patient education, and expectation management also play crucial roles by providing support and guidance, encouraging patients to engage in early mobilization activities. Chao et al. [25] found that ERAS significantly improved the same-day discharge rate for gynecologic surgery. This is because ERAS pathways have revolutionized perioperative care for patients undergoing gynecologic surgery through a comprehensive approach involving teamwork, optimization, adherence to protocols, and support for data-driven change and improvement. This finding strongly supports the results of this study. Furthermore, in this study, the study group had a postoperative complication rate of 6.90%, significantly lower than the control group. This can be attributed to the ability of the ERAS to ensure patients’ prompt recovery and shorten the recovery time. In contrast, patients in the control group, due to a longer recovery time, are more susceptible to complications. Additionally, the study group had a 98.28% satisfaction rate with nursing care service, significantly higher than 86.00% in the control group. This indicates that the application of the ERAS concept better meets the perioperative care needs of patients. Many similar studies support these findings. For example, Kalogera et al. [26] found that ERAS-based nursing reduced the length of hospital stay and/or increased the proportion of same-day discharge surgeries for patients undergoing minimally invasive colorectal resections alone. It improved patient satisfaction, reduced hospital costs, and maintained low rates of postoperative complications and readmissions. Mark T. Yost et al. [27] discovered that compared to traditional perioperative care, the ERAS nursing for minimally invasive esophagectomy reduced postoperative hospital stay, facilitated early recovery of bowel function, resulted in cost savings, and did not significantly alter the occurrence of perioperative complications. Sims et al. [28] found that ERAS pathway for esophagectomy reduced overall complications, particularly atrial arrhythmias and postoperative ileus, in the first year. The consistency of these research findings suggests that ERAS produce positive effects across different types of surgeries.
Finally, through logistic regression analysis, the study identified disease duration and nursing care intervention methods as independent risk factors influencing complications in patients undergoing thulium laser prostatectomy. The duration of the disease course can reflect the severity of the disease and its impact on the body. A longer disease course may indicate that the disease has progressed to a more advanced stage, resulting in poorer physical condition and a higher surgical risk [29]. Additionally, long-standing diseases may cause other complications or comorbidities, further increasing the complexity and risk of surgery [30]. On the other hand, ERAS nursing care interventions involve a comprehensive, multidisciplinary team approach aimed at promoting patient recovery through standardized nursing care measures and personalized rehabilitation plans [31]. This intervention includes early postoperative mobilization, pain management, fluid management, infection prevention, nutritional support, and other measures that can reduce the incidence of postoperative complications, shorten hospital stays, and promote patient recovery.
While retrospective studies have certain advantages in obtaining historical data and exploring associations, the research results may be influenced by unknown or unrecorded factors, leading to bias. Additionally, the inclusion of a limited number of patients in the study may affect the robustness of the conclusions. Moreover, the inadequate number of complication cases relative to the number of independent variables in the current study raises concerns about spurious associations and diminishes the reliability of the model. This underscores the importance of interpreting the results cautiously and seeking validation through larger sample sizes. Furthermore, the wide range of 95% CIs observed in our study further indicates the instability of the model. In the future, conducting prospective studies with a larger sample size and a broader range of influencing factors would be beneficial to further improve the results of this study.
In conclusion, the application of the concept of ERAS in the nursing care of patients undergoing thulium laser prostatectomy significantly improves postoperative recovery indicators, increases patient satisfaction, and reduces postoperative complications. Additionally, disease duration and nursing care intervention method are independent factors affecting the complications of patients undergoing thulium laser prostatectomy.
Disclosure of conflict of interest
None.
References
- 1.Langan RC. Benign prostatic hyperplasia. Prim Care. 2019;46:223–232. doi: 10.1016/j.pop.2019.02.003. [DOI] [PubMed] [Google Scholar]
- 2.Arnold MJ, Gaillardetz A, Ohiokpehai J. Benign prostatic hyperplasia: rapid evidence review. Am Fam Physician. 2023;107:613–622. [PubMed] [Google Scholar]
- 3.de Figueiredo FCA, Cracco CM, de Marins RL, Scoffone CM. Holmium laser enucleation of the prostate: problem-based evolution of the technique. Andrologia. 2020;52:e13582. doi: 10.1111/and.13582. [DOI] [PubMed] [Google Scholar]
- 4.Das AK, Han TM, Hardacker TJ. Holmium laser enucleation of the prostate (HoLEP): size-independent gold standard for surgical management of benign prostatic hyperplasia. Can J Urol. 2020;27:44–50. [PubMed] [Google Scholar]
- 5.Das A, Han TM, Rudnick B, Hardacker T, Shenot PJ, Shvero A. Holmium laser enucleation of the prostate following previous prostatic urethral lift. J Endourol. 2022;36:111–116. doi: 10.1089/end.2021.0351. [DOI] [PubMed] [Google Scholar]
- 6.Tazreean R, Nelson G, Twomey R. Early mobilization in enhanced recovery after surgery pathways: current evidence and recent advancements. J Comp Eff Res. 2022;11:121–129. doi: 10.2217/cer-2021-0258. [DOI] [PubMed] [Google Scholar]
- 7.Engelman DT, Ben Ali W, Williams JB, Perrault LP, Reddy VS, Arora RC, Roselli EE, Khoynezhad A, Gerdisch M, Levy JH, Lobdell K, Fletcher N, Kirsch M, Nelson G, Engelman RM, Gregory AJ, Boyle EM. Guidelines for perioperative care in cardiac surgery: enhanced recovery after surgery society recommendations. JAMA Surg. 2019;154:755–766. doi: 10.1001/jamasurg.2019.1153. [DOI] [PubMed] [Google Scholar]
- 8.Ashok A, Niyogi D, Ranganathan P, Tandon S, Bhaskar M, Karimundackal G, Jiwnani S, Shetmahajan M, Pramesh CS. The enhanced recovery after surgery (ERAS) protocol to promote recovery following esophageal cancer resection. Surg Today. 2020;50:323–334. doi: 10.1007/s00595-020-01956-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huh YJ, Kim DJ. Enhanced recovery after surgery in bariatric surgery. J Metab Bariatr Surg. 2021;10:47–54. doi: 10.17476/jmbs.2021.10.2.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang Z, Wan X. Urethral recovery after holmium laser enucleation of the prostate. Zhonghua Nan Ke Xue. 2018;24:99–103. [PubMed] [Google Scholar]
- 11.Bielewicz J, Daniluk B, Kamieniak P. VAS and NRS, same or different? Are visual analog scale values and numerical rating scale equally viable tools for assessing patients after microdiscectomy? Pain Res Manag. 2022;2022:5337483. doi: 10.1155/2022/5337483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grant MC, Crisafi C, Alvarez A, Arora RC, Brindle ME, Chatterjee S, Ender J, Fletcher N, Gregory AJ, Gunaydin S, Jahangiri M, Ljungqvist O, Lobdell KW, Morton V, Reddy VS, Salenger R, Sander M, Zarbock A, Engelman DT. Perioperative care in cardiac surgery: a joint consensus statement by the Enhanced Recovery After Surgery (ERAS) Cardiac Society, ERAS International Society, and The Society of Thoracic Surgeons (STS) Ann Thorac Surg. 2024;117:669–689. doi: 10.1016/j.athoracsur.2023.12.006. [DOI] [PubMed] [Google Scholar]
- 13.Malvindi PG, Bifulco O, Berretta P, Galeazzi M, Alfonsi J, Cefarelli M, Zingaro C, Zahedi HM, Munch C, Di Eusanio M. The enhanced recovery after surgery approach in heart valve surgery: a systematic review of clinical studies. J Clin Med. 2024;13:2903. doi: 10.3390/jcm13102903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Piler T, Creutzenberg M, Hofmann HS, Ried M. Modern perioperative care concepts in thoracic surgery: Enhanced Recovery After Thoracic Surgery (ERATS) Zentralbl Chir. 2024;149:116–122. doi: 10.1055/a-1823-1207. [DOI] [PubMed] [Google Scholar]
- 15.Grant MC, Crisafi C, Alvarez A, Arora RC, Brindle ME, Chatterjee S, Ender J, Fletcher N, Gregory AJ, Gunaydin S, Jahangiri M, Ljungqvist O, Lobdell KW, Morton V, Reddy VS, Salenger R, Sander M, Zarbock A, Engelman DT. Perioperative care in cardiac surgery: a joint consensus statement by the Enhanced Recovery After Surgery (ERAS) Cardiac Society, ERAS International Society, and The Society of Thoracic Surgeons (STS) Ann Thorac Surg. 2024;117:669–689. doi: 10.1016/j.athoracsur.2023.12.006. [DOI] [PubMed] [Google Scholar]
- 16.Stenberg E, Dos Reis Falcão LF, O’Kane M, Liem R, Pournaras DJ, Salminen P, Urman RD, Wadhwa A, Gustafsson UO, Thorell A. Guidelines for perioperative care in bariatric surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations: a 2021 update. World J Surg. 2022;46:729–751. doi: 10.1007/s00268-021-06394-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Agarwal V, Divatia JV. Enhanced recovery after surgery in liver resection: current concepts and controversies. Korean J Anesthesiol. 2019;72:119–129. doi: 10.4097/kja.d.19.00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Naftalovich R, Singal A, Iskander AJ. Enhanced Recovery After Surgery (ERAS) protocols for spine surgery - review of literature. Anaesthesiol Intensive Ther. 2022;54:71–79. doi: 10.5114/ait.2022.113961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Choi BY, Bae JH, Lee CS, Han SR, Lee YS, Lee IK. Implementation and improvement of Enhanced Recovery After Surgery protocols for colorectal cancer surgery. Ann Surg Treat Res. 2022;102:223–233. doi: 10.4174/astr.2022.102.4.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cao S, Zheng T, Wang H, Niu Z, Chen D, Zhang J, Lv L, Zhou Y. Enhanced recovery after surgery in elderly gastric cancer patients undergoing laparoscopic total gastrectomy. J Surg Res. 2021;257:579–586. doi: 10.1016/j.jss.2020.07.037. [DOI] [PubMed] [Google Scholar]
- 21.Schotanus MGM, Bemelmans YFL, Grimm B, Heyligers IC, Kort NP. Physical activity after outpatient surgery and enhanced recovery for total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2017;25:3366–3371. doi: 10.1007/s00167-016-4256-1. [DOI] [PubMed] [Google Scholar]
- 22.Kim JY, Wie GA, Cho YA, Kim SY, Sohn DK, Kim SK, Jun MD. Diet modification based on the Enhanced Recovery After Surgery Program (ERAS) in patients undergoing laparoscopic colorectal resection. Clin Nutr Res. 2018;7:297–302. doi: 10.7762/cnr.2018.7.4.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kaye AD, Chernobylsky DJ, Thakur P, Siddaiah H, Kaye RJ, Eng LK, Harbell MW, Lajaunie J, Cornett EM. Dexmedetomidine in Enhanced Recovery After Surgery (ERAS) protocols for postoperative pain. Curr Pain Headache Rep. 2020;24:21. doi: 10.1007/s11916-020-00853-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang H, Mou YK, Liu ZL, Song XC. Application of enhanced recovery after surgery in laryngeal cancer surgery with multi-disciplinary team. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2021;56:221–228. doi: 10.3760/cma.j.cn115330-20200825-00694. [DOI] [PubMed] [Google Scholar]
- 25.Chao L, Lin E, Kho K. Enhanced recovery after surgery in minimally invasive gynecologic surgery. Obstet Gynecol Clin North Am. 2022;49:381–395. doi: 10.1016/j.ogc.2022.02.014. [DOI] [PubMed] [Google Scholar]
- 26.Kalogera E, Glaser GE, Kumar A, Dowdy SC, Langstraat CL. Enhanced recovery after minimally invasive gynecologic procedures with bowel surgery: a systematic review. J Minim Invasive Gynecol. 2019;26:288–298. doi: 10.1016/j.jmig.2018.10.016. [DOI] [PubMed] [Google Scholar]
- 27.Yost MT, Jolissaint JS, Fields AC, Fisichella PM. Enhanced recovery pathways for minimally invasive esophageal surgery. J Laparoendosc Adv Surg Tech A. 2018;28:496–500. doi: 10.1089/lap.2018.0073. [DOI] [PubMed] [Google Scholar]
- 28.Sims CR 3rd, Abou Chaar MK, Kerfeld MH, Cassivi SD, Hofer RE, Nichols FC, Reisenauer J, Saddoughi SS, Shen KR, Stewart TM, Tapias LF, Wigle DA, Blackmon SH. Esophagectomy enhanced recovery after surgery initiative results in improved outcomes. Ann Thorac Surg. 2024;117:847–857. doi: 10.1016/j.athoracsur.2023.10.032. [DOI] [PubMed] [Google Scholar]
- 29.Aspberg J, Heijl A, Bengtsson B. Estimating the length of the preclinical detectable phase for open-angle glaucoma. JAMA Ophthalmol. 2023;141:48–54. doi: 10.1001/jamaophthalmol.2022.5056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Falkner B, Gidding S. Life-course implications of pediatric risk factors for cardiovascular disease. Can J Cardiol. 2021;37:766–775. doi: 10.1016/j.cjca.2021.02.001. [DOI] [PubMed] [Google Scholar]
- 31.Fan E, Zhang K, Wan Y, Hu S. Effects of rapid rehabilitation nursing model on surgical site wound infection and pain of patients with ovarian cancer: a meta-analysis. Int Wound J. 2023;21:e14464. doi: 10.1111/iwj.14464. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]