Abstract
Objective: To explore the hazard element of varus knee osteoarthritis (OA) and its relationship with Ailment severity based on the Kellgren-Lawrence classification. Methods: This study selected a cohort of patients who initially presented without clinical signs of arthritis and did not exhibit knee valgus or varus deformities when assessed from a hip-knee-ankle alignment perspective, focusing on the internal side. As the study progressed some individuals developed OA. Eligible participants were those who had undergone a standard whole lower extremity weight-bearing X-ray examination at our orthopedic outpatient clinic. The study period spanned from January 2021 to April 2022, and the selection criteria were strictly applied throughout this timeframe. Data on clinical and X-ray indices, including fibular head height, Kellgren-Lawrence grade, joint line convergence angle (JLCA), proximal medial tibial angle (MPTA), and Hip-knee-ankle angle, were collected from patients. Results: The study included 23 grade 0, 22 grade I, 32 grade II, 32 grade III, and 97 grade IV Kellgren-Lawrence classified patients. Significant differences in age, gender, and BMI were observed across groups (all P<0.05). With increasing OA severity, fibular head height and MPTA decreased, while JLCA and Hip-knee-ankle angle increased significantly (all P<0.05). Patients with OA exhibited larger fibular head height and MPTA but smaller JLCA and Hip-knee-ankle angle than those without arthritis (all P<0.05). Logistic regression analysis confirmed age, fibular head height, MPTA, JLCA, and Hip-knee-ankle angle as independent risk factors for varus knee OA (all P<0.05). Additionally, there was a strong positive correlation between age and fibular head height with disease severity, but a strong negative correlation between Hip-knee-ankle angle and disease severity (all P<0.05). Conclusion: Patients with varus knee OA have larger fibular head height and MPTA than those without arthritis. Age, fibular head height, and Hip-knee-ankle angle are risk factors for the development of varus knee OA. The severity of arthritis and varus deformity increases with age and fibular head height.
Keywords: Kellgren-Lawrence classification, varus knee articulation, OA, hazard element, ailment degree
Introduction
Knee osteoarthritis (OA) is a degenerative condition that can lead to knee pain and, in severe cases, disability in the lower extremities. The occurrence of OA is closely related to the degenerative changes in the knee joint [1]. Studies suggest that long-term pressure on the medial compartment of the knee significantly increases the incidence of arthritis in that area, up to 10 times more than in the lateral compartment. In clinical practice, X-ray imaging is commonly used to evaluate the degenerative changes in the knee joint and to observe the condition of the medial compartment in patients with varus knee arthritis. However, the changes in lateral structural are easily overlooked [2,3]. Patients with varus knee arthritis exhibit adaptive bending of the proximal fibula. One contributing factor to varus knee arthritis is that the fibula bears part of the body weight, causing the medial tibial plateau to endure more force than the lateral one; Over time, this high load accelerates the collapse of the medial tibial plateau, leading to uneven settlement compared to the lateral plateau [4]. Examinations have shown that in patients with varus knee arthritis, the proximal fibula is higher and exhibits adaptive bending, sometimes reaching the level of the lateral tibial plateau. Previous research has suggested a correlation between the height of the fibular head and the presence of knee arthritis. It is hypothesized that changes in fibular head height may contribute to the onset and progression of arthritis, although these findings have yet to be conclusively proven [5-7]. With this in mind, it was predicted some that some of the studied participants would develop knee arthritis and to examine the potential link between fibular head height and the disease.
We conducted a thorough analysis to identify any risk factors associated with the development and severity of arthritis. Our goal was to explore the specific role that fibular head height might play in the condition, and how this factor interacts with the clinical manifestations of arthritis. By doing so, we sought to contribute to the existing body of knowledge and provide insights that could inform therapeutic approaches and preventive measures for individuals suffering from OA.
Materials and methods
General information
This retrospective study was conducted at the Department of Orthopedics, Shenzhen Guangming People’s Hospital, with the aim of delineating the relationship between OA and specific anatomical parameters. The study period extended from January 2021 to April 2022, during which we systematically identified patients who had received a standard weight-bearing X-ray examination of the lower extremities. This study selected a cohort of patients who originally presented with no clinical OA signs and did not exhibit knee valgus or varus deformities at the initial assessment from a hip-knee-ankle alignment perspective, focusing on the internal side.
A total of 206 participants were enrolled, comprising 90 males and 116 females. The age distribution ranged from 41 to 80 years, with a mean age of 61.27±10.85 years. The average body mass index (BMI) was 25.00±3.74 kg/m2, suggesting a predominantly overweight study population. This examination was approved by the Medical Ethics Committee of Shenzhen Guangming People’s Hospital.
Inclusion criteria: ① Patients without knee valgus or varus deformity (assessed from a hip-knee-ankle alignment perspective) who underwent standard whole lower extremity weight-bearing X-ray examination in the orthopaedic clinic; ② Arthritis diagnosis based on Kellgren-Lawrence grading: no arthritis in grades 0-I, and arthritis in grades II-IV; ③ Complete academic parameters on fibular head height and varus deformity of the knee joint.
Exclusion criteria: (1) Patients whose condition deteriorated suddenly during the examination process; (2) Patients whose other ailments affected the examination results; (3) Patients who encountered unexpected circumstances during the examination, making it difficult to continue; (4) Patients with severe ailments during the examination affecting other parameters.
Examination methods
Data collection
The clinical data of all patients, including age, gender, BMI, and X-ray imaging data, were collected.
X-ray inspection indicators
Fibular Head Height: The height of the fibular head relative to the lateral tibial plateau reflects the relative vertical position of the fibular head. To measure this, the distance between the upper edge of the fibular head and the horizontal tangent passing through the lowest point of the lateral tibial plateau was measured on a full-length frontal X-ray film of the lower extremity in a standard weight-bearing position.
Kellgren-Lawrence Classification: This classification is the radiographic severity grading standard for knee OA (Table 1).
Table 1.
Kellgren-Lawrence grading scale
| Standard | Performance |
|---|---|
| Grade 0 | No obvious irregular changes on X-ray |
| Grade l | Suspected joint space narrowing or suspicious osteophyte formation |
| Grade II | Obvious osteophytes with mild joint space narrowing |
| Grade III | Moderate osteophytes, narrow joint space, mild subchondral sclerosis, and small extent of bone changes |
| Grade IV | Extensive osteophytes, severely narrowed joint space, obvious bone sclerosis, widespread subchondral changes, and marked joint hypertrophy and deformity |
This rule is presented according to the grading of knee articulation degeneration on X-ray films.
Joint Line Convergence Angle (JLCA): The angle between the upper and lower joint lines of the knee joint. Using the method by Lee et al., this is the angle between the articular surface of the distal femur and the plane of the tibial plateau on a full-length frontal X-ray of the lower extremity in a standard weight-bearing position. JLCA reflects the degree of deformity in the knee joint cavity and indicates the extent of cartilage wear and tear. It also illustrates the relationship between intra-articular and lateral soft tissue tension; in patients with varus knee arthritis, there is internal angulation of the superior and inferior joint lines. The greater the JLCA, the more severe the deformity.
Medial Proximal Tibial Angle (MPTA): The internal angle between the tibial plateau plane and the tibial mechanical axis on a standard weight-bearing full-length anteroposterior radiograph of the lower extremity. MPTA reflects the degree of deformity of the tibial plateau. The normal value is 87°. The smaller the MPTA, the more severe the varus deformity.
Hip-Knee-Ankle Angle: The angle between the line connecting the center of the femoral head to the center of the knee and the mechanical axis of the tibia on a full-length frontal X-ray of the lower extremity in a standard weight-bearing position. This axis is the internal side of the line connecting the center of the femoral head to the center of the knee. The hip-knee-ankle angle reflects the overall degree of deformity of the knee joint. The larger the hip-knee-ankle angle, the more severe the knee varus deformity.
Observation indicators
(1) Observing the clinical characteristics of patients with different grades of OA [2]; (2) Comparing imaging measures of patients with different grades according to the Kellgren-Lawrence classification [8]; (3) Identifying the risk factors for varus knee osteoarthritis (OA) based on the Kellgren-Lawrence classification [9]; (4) Analyzing the factors influencing knee varus deformity [3]; (5) Examining the risk factors for varus knee OA and their relationship with disease severity [5].
Each measurement was taken with the aim of providing a comprehensive assessment of knee joint integrity and deformity. To ensure accuracy and reliability, all measurements were conducted by a single, trained investigator who was blinded to the patients’ clinical details.
Statistical methods
SPSS 26.0 was used for data processing. Measurement data were tested for normality, and the data conforming to normal distribution were expressed as mean ± standard deviation (x±s). The inter-group comparison was conducted using independent samples t test, while the intra-group comparison was conducted using paired samples t test. The multi-group comparison was conducted using F-test. Data with non-normality was analyzed using Mann-Whitney U test. Count data rate was expressed as n (%), and compared using χ2 test. The relationships between variables was analyzed by Pearson’s correlation analysis. Multivariate logistic regression was conducted to identify influencing factors. A p-value of less than 0.05 (P<0.05) was considered statistically significant.
Results
Clinical characteristics of patients with different grades of arthritis
This study evaluated a total of 206 patients, categorized according to the Kellgren-Lawrence (KL) grading system for osteoarthritis (OA): 23 cases of KL grade 0, 22 of grade I, 32 of grade II, 32 of grade III, and 97 of grade IV. This distribution includes 45 patients without OA and 161 with OA. A comparative analysis of the demographic and clinical data revealed significant differences in gender distribution and body mass index (BMI) among the grades, as indicated in Table 2 (P<0.05).
Table 2.
Comparison of baseline data among patients with different KL grades of Kellgren-Lawrence
| Kellgren-Lawrence classification | Number of cases | Age | Gender (male/female) |
|---|---|---|---|
| Grade 0 | 23 | 39.41±5.23 | 13/10 |
| Grade I | 22 | 55.52±8.31* | 10/12 |
| Grade II | 32 | 63.44±6.35*,¥ | 15/17 |
| Grade III | 32 | 69.49±6.17*,¥,# | 12/20 |
| Grade IV | 97 | 73.46±6.75*,¥,#,& | 40/57 |
| Statistics | - | 112.63 | 57.686 |
| P value | - | <0.001 | <0.001 |
Notes: KL, Kellgren-Lawrence grade.
compare with Grade 0.
compare with Grade I.
compare with Grade II.
compare with Grade III, P<0.05.
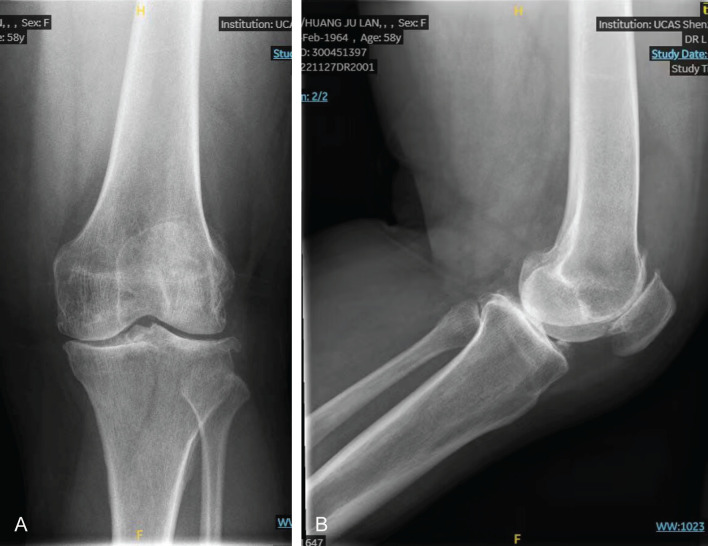
The radiographic assessment, exemplified in Figure 1, presents the typical features of OA. The X-ray images demonstrated hallmark signs such as the narrowing of joint spaces attributed to cartilage degradation, an increase in bone density suggestive of subchondral bone sclerosis, and the formation of osteophytes or bone spurs along the joint margins. Additionally, cystic changes within the subchondral bone are indicative of potential bone necrosis areas.
Figure 1.
Male, 54 years old, knee osteoarthritis. Frontal X-ray (A), lateral X-ray (B).
Comparison of imaging measures among patients with different KL grades
There were significant differences in fibular head height, JLCA, MPTA, and hip-knee-ankle angle among patients with different KL grades (all P<0.05), see Table 3.
Table 3.
Comparison of imaging measurements among patients with different KL grades
| Kellgren-Lawrence classification | Number of cases | Fibular head height (mm) | JLCA (°) | MPTA (°) | Hip-knee-ankle angle (°) |
|---|---|---|---|---|---|
| Grade 0 | 23 | 15.02±2.47 | 0.44±0.35 | 88.03±1.43 | 1.72±1.31 |
| Grade I | 22 | 13.54±2.20* | 1.09±0.48* | 87.71±2.34* | 3.59±2.45* |
| Grade II | 32 | 12.03±2.27*,¥ | 2.19±0.88*,¥ | 86.83±2.63*,¥ | 5.02±3.21*,¥ |
| Grade III | 32 | 9.86±2.50*,¥,# | 2.77±1.28*,¥,# | 86.46±2.40*,¥,# | 6.47±3.16*,¥,# |
| Grade IV | 97 | 7.95±2.80*,¥,#,& | 5.77±2.19*,¥,#,& | 84.69±2.86*,¥,#,& | 9.86±4.83*,¥,#,& |
| Statistics | - | 29.076 | 26.362 | 24.417 | 27.145 |
| P value | - | <0.001 | <0.001 | <0.001 | <0.001 |
Notes: KL, Kellgren-Lawrence grade.
compare with Grade 0.
compare with Grade I.
compare with Grade II.
compare with Grade III, P<0.05.
Disparities in clinical data between patients with arthritis and those without arthritis
There were extensive disparities between the clinical data of patients with arthritis and those without arthritis, mainly revealing that age, fibular man of character altitude and MPTA point of view of individuals with arthritis were notoriously higher than those without arthritis, and the standards of JLCA and knee-knee-ankle point of view were notoriously higher in patients with arthritis. These results between groups were statistically different (P<0.05), as revealed in Table 4.
Table 4.
Comparison of clinical data between patients with and without OA
| Index | Knee osteoarthritis (n=161) | Non-knee osteoarthritis (n=45) | Statistics | P |
|---|---|---|---|---|
| Age | 67.56±6.87 | 60.91±6.26 | 12.878 | <0.001 |
| Gender (male/female) | 67/94 | 23/22 | 0.563 | 0.631 |
| Fibular head height (mm) | 12.56±3.13 | 8.59±1.56 | 22.523 | <0.001 |
| JLCA (°) | 0.78±0.41 | 5.37±2.18 | 25.716 | <0.001 |
| MPTA (°) | 87.56±1.46 | 85.52±1.27 | 23.559 | <0.001 |
| Hip-knee-ankle angle (°) | 2.89±1.17 | 8.91±1.53 | 19.517 | <0.001 |
Notes: JLCA, Joint Line Convergence Angle; MPTA, Medial Proximal Tibial Angle.
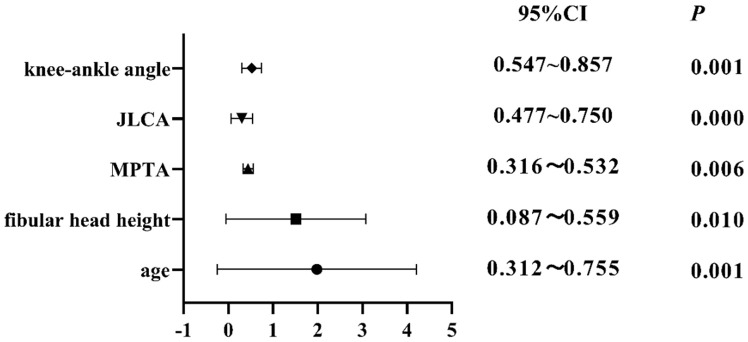
Logistic regression analysis of risk factors for varus knee OA
The multivariate logistic regression analysis was conducted to identify risk factors for varus knee OA. The occurrence of varus knee OA was set as the dependent variable, while age, fibular head height, MPTA, JLCA, and hip-knee-ankle angle were the independent variables. The model selection was based on actual clinical situations. Logistic regression results showed that age, fibular head height, MPTA, JLCA, and hip-knee-ankle angle were independent risk factors for varus knee OA (P<0.05), see Table 5 and Figure 2.
Table 5.
Multivariate logistic regression analysis of risk factors for the varus knee osteoarthritis
| Results of multivariate logistic analysis | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| β | SE | Wald | OR | 95% CI | P | |
| Age | 1.515 | 1.081 | 1.965 | 4.550 | 0.547-0.857 | 0.001 |
| Fibular head height | 1.199 | 0.989 | 1.470 | 3.318 | 0.477-0.750 | 0.000 |
| MPTA (°) | 0.800 | 0.325 | 6.613 | 0.482 | 0.316-0.532 | 0.006 |
| JLCA (°) | 0.232 | 0.093 | 7.501 | 0.261 | 0.087-0.559 | 0.010 |
| Hip-knee-ankle angle (°) | 0.814 | 0.252 | 11.136 | 0.512 | 0.312-0.755 | 0.001 |
Notes: JLCA, Joint Line Convergence Angle; MPTA, Medial Proximal Tibial Angle.
Figure 2.
Multivariate logistic regression analysis of risk factors for the varus knee osteoarthritis.
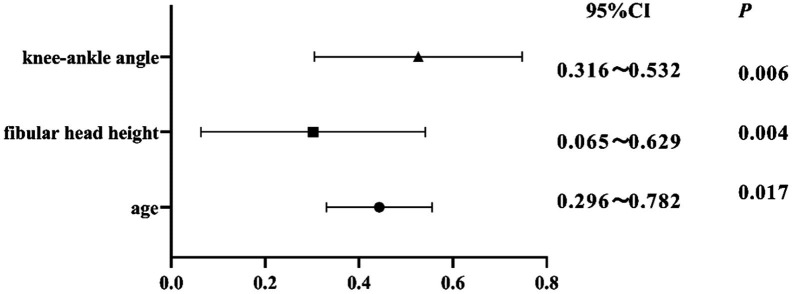
Analysis of influencing factors on the degree of knee varus deformity
A multivariate decomposition value set the degree of knee varus deformity as the examination dependent variable, and age, fibular man of character altitude, MPTA point of view, JLCA and the standard of the knee-knee-ankle point of view as the independent variables, and the model was selected based on the actual clinical situation. The results of logistic regression model decomposition showed that age, fibular man of character altitude and standard of knee-knee-ankle point of view were hazardous elements for varus knee OA (P<0.05), as revealed in Table 6 and Figure 3.
Table 6.
Multivariate logistic regression analysis of risk factors for the degree of knee varus deformity
| Results of multivariate logistic analysis | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| β | SE | Wald | OR | 95% CI | P | |
| Age | 0.800 | 0.325 | 6.613 | 0.482 | 0.316-0.532 | 0.006 |
| Fibular head height | 0.425 | 0.106 | 12.336 | 0.211 | 0.065-0.629 | 0.004 |
| Hip-knee-ankle angle (°) | -0.563 | 0.757 | 10.859 | 0.556 | 0.296-0.782 | 0.017 |
Figure 3.
Multivariate logistic regression analysis of risk factors for the degree of knee varus deformity.
The relationship between risk factors for varus knee OA with disease severity
The risk factors for varus knee OA included age, fibular head height, and hip-knee-ankle angle. Among these, age and fibular head height were positively correlated with the severity of the disease, while the hip-knee-ankle angle was significantly negatively correlated with the severity of the disease (all P<0.05), see Table 7.
Table 7.
Relationship between risk factors of varus knee osteoarthritis and disease severity
| Disease severity | ||
|---|---|---|
|
| ||
| r | P | |
| Age | 0.563 | <0.001 |
| Fibular head height | 0.735 | <0.001 |
| Hip-knee-ankle angle (°) | -0.669 | <0.001 |
Discussion
The fibula includes important structures such as the fibular longus muscle, biceps femoris muscle, fibular collateral ligament, arcuate ligament, and lateral collateral ligament, serving as the attachment point for major ligaments and tendons in the human body [9]. Its position is crucial for the function of these ligaments and tendons, and it is indirectly connected with the popliteal ligament. According to biomechanical studies, when comparing patients with varus knee arthritis to the normal population, it was found that the peak activity level of the biceps femoris muscle was reduced, while the peak activity level of the fibular longus muscle was higher [10].
In this study, logistic regression model analysis showed that age, fibular head height, MPTA, JLCA, and hip-knee-ankle angle were significant risk factors for varus knee OA. The model demonstrated that age, fibular head height, and hip-knee-ankle angle were particularly significant risk factors for varus knee OA. The primary reason for these findings is that knee joint stability is maintained by muscles and ligaments, but a reduction in fibular head height can lead to tendon relaxation and reduced tension in the lateral ligaments of the knee joint [10]. Therefore, changes in fibular head height in varus knee arthritis, or as a manifestation of arthritis, may contribute to knee instability, leading to the incidence and progression of arthritis.
In limiting tibial external rotation, the lateral soft tissue of the knee joint plays a crucial role. The lateral ligament complex, which includes the arcuate ligament, lateral collateral ligament, thoracic ligament, and biceps femoris tendon, provides the greatest resistance to tibial external rotation, particularly during knee flexion at 30° to 45° [11]. The lateral collateral ligament is the most significant force resisting external rotation when the knee is flexed between 0° to 30°, and its tendon complex plays an important role in maintaining knee joint stability during continued flexion.
This study confirmed that the severity of varus knee arthritis is associated with the height of the fibular head. There was a significant positive correlation between age and fibular head height with the severity of the disease. The primary reason is that the elevated relative position of the fibula in patients with varus arthritis leads to decreased lateral soft tissue tension and irregular external rotation of the tibia, which is a manifestation of knee joint instability [12]. Previous studies have confirmed that the external rotation angle of the tibia in patients with arthritis increases irregularly with the severity of the disease. As arthritis severity increases, the irregular external rotation of the tibia also increases [13]. This study’s findings align with these previous conclusions. The deterioration and stiffness of the knee joint are attributed to increased and irregular pressure, such as osteosclerosis and hyperosteogeny, while the increased pressure on the medial compartment of the knee is due to the irregular external rotation of the tibia [14].
The lateral soft tissue of the knee plays an important role in maintaining the normal alignment of the subjoined limb. The posterolateral ligament complex of the knee can limit the varus deformity of the knee. When the knee flexion is 0°-30°, the lateral collateral ligament plays a major role in limiting the varus deformity of the knee [15]. When flexion exceeds 30°, the biceps femoris muscle becomes the primary stabilizer. As the attachment point of ligaments and tendons, the fibular head’s position is critical. The upward movement of the fibular head may weaken the structural function limiting knee varus, aggravating the varus deformity of the knee joint’s lateral structures and destabilizing the coronal plane. Some scholars suggest that due to the mechanical displacement of the fibular head, the force on the fibula is not compressive but tensile in the vertical direction. The height of the fibular head is negatively correlated with the degree of varus deformity in varus knee arthritis. This may also result from tibial plateau collapse, with the “uneven subsidence” theory linking the fibula’s bearing effect to the pathogenesis of varus knee arthritis. This study confirmed that the fibular head height is not only closely related to the severity of varus deformity but also impacts the onset and progression of varus knee arthritis.
Initially, our study selected patients who did not present with clinical signs of arthritis. However, during the study period, some patients developed clinical symptoms of arthritis such as knee varus and joint deformity. This observation can be attributed to the dynamic and progressive nature of osteoarthritis (OA). The study aimed to investigate the risk factors for varus knee OA and its relationship with disease severity using the Kellgren-Lawrence classification system, which can detect subclinical changes in joint structure. The progression to clinical symptoms in some patients could be due to natural disease progression influenced by factors such as age, BMI, and biomechanical factors identified in our study.
Although this study has achieved certain examination results, there are still some limitations. As a retrospective study, it cannot describe the dynamic changes of patients’ arthritis over time. Additionally, X-ray films are two-dimensional images, which cannot evaluate the rotation of bones and joints. Therefore, prospective studies should be conducted in the future to further analyze the risk factors of varus knee OA and its relationship with disease severity based on the Kellgren-Lawrence grading standard [16,17].
In conclusion, the fibular head height in patients with varus knee arthritis was smaller than that in the non-arthritis population, while the hip-knee-ankle angle was higher. Besides age, fibular head height and hip-knee-ankle angle were identified as significant risk factors for varus knee arthritis. The smaller the fibular head height and the larger the hip-knee-ankle angle, the more severe the arthritis and varus deformity.
Disclosure of conflict of interest
None.
References
- 1.Sharma L. Osteoarthritis of the knee. N Engl J Med. 2021;384:51–59. doi: 10.1056/NEJMcp1903768. [DOI] [PubMed] [Google Scholar]
- 2.Pu C, Huang H, Wang Z, Zou W, Lv Y, Zhou Z, Zhang Q, Qiao L, Wu F, Shao S. Extracellular vesicle-associated miR-21 and miR-144 are markedly elevated in serum of patients with hepatocellular carcinoma. Front Physiol. 2018;9:930. doi: 10.3389/fphys.2018.00930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Katz JN, Arant KR, Loeser RF. Diagnosis and treatment of hip and knee osteoarthritis: a review. JAMA. 2021;325:568–578. doi: 10.1001/jama.2020.22171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mahmoudian A, Lohmander LS, Mobasheri A, Englund M, Luyten FP. Early-stage symptomatic osteoarthritis of the knee-time for action. Nat Rev Rheumatol. 2021;17:621–632. doi: 10.1038/s41584-021-00673-4. [DOI] [PubMed] [Google Scholar]
- 5.Lu X, Qian J, Yang B, Li Z, Fan Y, Jiang B. A new radiographic finding of adult symptomatic discoid lateral meniscus. Medicine (Baltimore) 2020;99:e19646. doi: 10.1097/MD.0000000000019646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Misir A, Yildiz KI, Kizkapan TB, Incesoy MA. Kellgren-Lawrence grade of osteoarthritis is associated with change in certain morphological parameters. Knee. 2020;27:633–641. doi: 10.1016/j.knee.2020.04.013. [DOI] [PubMed] [Google Scholar]
- 7.Tsuji M, Akamatsu Y, Kobayashi H, Mitsugi N, Inaba Y, Saito T. Joint line convergence angle predicts outliers of coronal alignment in navigated open-wedge high tibial osteotomy. Arch Orthop Trauma Surg. 2020;140:707–715. doi: 10.1007/s00402-019-03245-0. [DOI] [PubMed] [Google Scholar]
- 8.Li Z, Li M, Du Y, Zhang M, Jiang H, Zhang R, Ma Y, Zheng Q. Femur-tibia angle and patella-tibia angle: new indicators for diagnosing anterior cruciate ligament tears in magnetic resonance imaging. BMC Sports Sci Med Rehabil. 2022;14:66. doi: 10.1186/s13102-022-00462-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Primorac D, Molnar V, Rod E, Jeleč Ž, Čukelj F, Matišić V, Vrdoljak T, Hudetz D, Hajsok H, Borić I. Knee osteoarthritis: a review of pathogenesis and state-of-the-art non-operative therapeutic considerations. Genes (Basel) 2020;11:854. doi: 10.3390/genes11080854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Perry TE, George SA, Lee B, Wahr J, Randle D, Sigurðsson G. A guide for pre-procedural imaging for transcatheter aortic valve replacement patients. Perioper Med (Lond) 2020;9:36. doi: 10.1186/s13741-020-00165-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dainese P, Wyngaert KV, De Mits S, Wittoek R, Van Ginckel A, Calders P. Association between knee inflammation and knee pain in patients with knee osteoarthritis: a systematic review. Osteoarthritis Cartilage. 2022;30:516–534. doi: 10.1016/j.joca.2021.12.003. [DOI] [PubMed] [Google Scholar]
- 12.Van Manen MD, Nace J, Mont MA. Management of primary knee osteoarthritis and indications for total knee arthroplasty for general practitioners. J Am Osteopath Assoc. 2012;112:709–715. [PubMed] [Google Scholar]
- 13.Heidari B. Knee osteoarthritis prevalence, risk factors, pathogenesis and features: part I. Caspian J Intern Med. 2011;2:205–12. [PMC free article] [PubMed] [Google Scholar]
- 14.Raud B, Gay C, Guiguet-Auclair C, Bonnin A, Gerbaud L, Pereira B, Duclos M, Boirie Y, Coudeyre E. Level of obesity is directly associated with the clinical and functional consequences of knee osteoarthritis. Sci Rep. 2020;10:3601. doi: 10.1038/s41598-020-60587-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang Y, Nguyen UDT, Lane NE, Lu N, Wei J, Lei G, Zeng C, Zhang Y. Knee osteoarthritis, potential mediators, and risk of all-cause mortality: data from the osteoarthritis initiative. Arthritis Care Res (Hoboken) 2021;73:566–573. doi: 10.1002/acr.24151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dantas LO, Salvini TF, McAlindon TE. Knee osteoarthritis: key treatments and implications for physical therapy. Braz J Phys Ther. 2021;25:135–146. doi: 10.1016/j.bjpt.2020.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tsokanos A, Livieratou E, Billis E, Tsekoura M, Tatsios P, Tsepis E, Fousekis K. The efficacy of manual therapy in patients with knee osteoarthritis: a systematic review. Medicina (Kaunas) 2021;57:696. doi: 10.3390/medicina57070696. [DOI] [PMC free article] [PubMed] [Google Scholar]