Abstract
Objective: To identify risk factors for postoperative delirium in adult patients undergoing cardiopulmonary bypass. Methods: The medical records of 214 patients who underwent cardiopulmonary bypass at the First Affiliated Hospital of Hunan Normal University from January 2022 to January 2024 were retrospectively analyzed. Based on the occurrence of postoperative delirium, patients were divided into a delirium group (49 cases) and a non-delirium group (165 cases). Outcome measures, including clinical baseline data, preoperative left ventricular ejection fraction (LVEF), preoperative Acute Physiology and Chronic Health Evaluation II (APACHE II) score, anesthesia duration, surgery duration, aortic cross-clamp duration, intraoperative mean arterial pressure (MAP), intraoperative blood loss, length of intensive care unit (ICU) stay, postoperative mechanical ventilation duration, as well as postoperative MAP, were compared between the two groups. Logistic regression analysis was performed to identify the potential factors associated with post-operative delirium in patients. Results: Of the included 214 patients, 49 patients experienced delirium, resulting in an incidence of 22.90%. The delirium group had significantly lower LVEF and significantly higher APACHE II scores compared to the non-delirium group (all P<0.001). No significant difference was observed between the two groups in terms of anesthesia duration, surgery duration, aortic cross-clamp duration, intraoperative MAP, and intraoperative blood loss (all P>0.05). The delirium group experienced significantly longer length of ICU stay and postoperative mechanical ventilation duration as compared to the non-delirium group (all P<0.001), but no significant difference was observed in terms of postoperative MAP between the two groups (P>0.05). Logistic regression analysis identified preoperative New York Heart Association classification (NYHA) (OR: 6.755, 95% CI: 2.529-18.039, P<0.001), preoperative LVEF (OR: 6.886, 95% CI: 2.383-19.899, P<0.001), preoperative APACHE II score (OR: 7.788, 95% CI: 2.740-22.135, P<0.001), length of ICU stay (OR: 9.463, 95% CI: 3.563-25.135, P<0.001), and postoperative mechanical ventilation duration (OR: 9.744, 95% CI: 3.419-27.768, P<0.001) as independent factors influencing the occurrence of delirium in adult patients undergoing cardiopulmonary bypass. Conclusion: Postoperative delirium is a prevalent complication among patients undergoing cardiac surgery. Independent risk factors for postoperative delirium in adult patients undergoing cardiopulmonary bypass during cardiac surgery include preoperative NYHA class III or IV, lower LVEF, higher APACHE II score, an extended length of stay in the ICU, and prolonged postoperative mechanical ventilation duration.
Keywords: Cardiopulmonary bypass in cardiac surgery, delirium, cardiac function, length of ICU stay, postoperative mechanical ventilation
Introduction
Cardiovascular diseases have become a major health threat globally. In China, the prevalence and mortality rates of cardiovascular diseases continue to rise, and the number of cardiac surgeries has significantly increased [1]. Cardiopulmonary bypass plays a critical role in cardiac surgery, and it is utilized in about 70% of cardiac procedures [2]. Despite its importance, cardiopulmonary bypass is associated with neurological complications, specifically postoperative delirium [3].
Postoperative delirium is the most frequently seen neurological complication following adult cardiac surgery with cardiopulmonary bypass [4]. It is typically characterized by patient confusion, difficulty concentrating, disordered thinking, delusions, and hallucinations [5]. It not only causes distress to patients but also imposes an additional burden on healthcare professionals and family members [6].
To address this issue, the European Society of Anaesthesiology released a guideline on postoperative delirium in 2017. The guideline aims to provide evidence-based recommendations for prevention and treatment, including comprehensive discussions on assessment, high-risk factors, and prognosis [4]. Given the relatively high incidence of postoperative delirium in cardiac surgery patients, it has garnered significant attention from healthcare professionals [7]. Postoperative delirium not only increases the risk of complications but also escalates hospitalization costs and mortality rates, imposing a significant burden on medical care and nursing [8]. Moreover, postoperative delirium detrimentally affects long-term cognitive function and brain capabilities, thereby jeopardizing the long-term survival of patients. It has become a major factor influencing the prognosis of adult cardiac surgery patients undergoing cardiopulmonary bypass [9]. In recent years, with advancements in cardiac surgical anesthesia and surgical techniques, there has been an increasing number of patients undergoing surgical treatment, leading to heightened attention on postoperative delirium [10]. Currently, the management of post-operative delirium primarily involves non-pharmacological interventions and supportive care [4]. These interventions often include early mobilization, optimization of sleep-wake cycles, minimizing exposure to environmental stressors, and promoting cognitive stimulation [5]. Pharmacological interventions, such as antipsychotic medications, are reserved for severe cases or when non-pharmacological measures are ineffective [5]. Despite existing strategies, several crucial questions remain unresolved in dealing with post-operative delirium, including how to identify high-risk patients, determine the optimal timing and duration of interventions and implement individualized approaches. Early identification of risk factors for postoperative delirium and preventive measures are of utmost importance. Nonetheless, there is a paucity of research on the risk factors associated with postoperative delirium in adult patients undergoing cardiopulmonary bypass during cardiac surgery. Understanding these risk factors is crucial for developing effective preventive strategies and personalized rehabilitative interventions.
Accordingly, this study retrospectively analyzed the clinical data of 214 cardiac surgery patients admitted to the First Affiliated Hospital of Hunan Normal University from January 2022 to January 2024, aiming to identify potential risk factors for post-operative delirium. This research is innovative in the selection of a specific cardiac surgery type, comprehensive analysis of multiple factors, and identification of independent risk factors. This study contributes to a deeper understanding of postoperative delirium in cardiac surgery and provides insights for the development of targeted preventive and management strategies.
Data and methods
Sampling and grouping
A retrospective analysis was conducted on the clinical data from patients who underwent cardiopulmonary bypass at the First Affiliated Hospital of Hunan Normal University between January 2022 and January 2024. A total of 429 individuals were enrolled for the analysis. After applying the inclusion and exclusion criteria, a final sample of 214 eligible patients was obtained.
Inclusion criteria: Patients aged 18 years or older; patients undergoing cardiac valve replacement surgery with cardiopulmonary bypass; patients without preoperative anxiety, depression, or language disorders; patients with post-operative diagnosis of delirium [11]; patients with complete clinical data.
Exclusion criteria: Patients with preoperative organic brain disease; patients with preexisting psychiatric disorders or cognitive impairments; patients with comorbidities such as chronic liver disease, chronic kidney disease, or chronic lung disease; patients who experienced severe complications postoperatively, such as low cardiac output, major bleeding, or cerebrovascular accidents; patients with recent trauma, infection, or surgery involving the head, brain, or neck; patients who required continuous sedation treatment after operation.
Based on the occurrence of postoperative delirium, patients were assigned to a delirium group (49 cases) or a non-delirium group (165 cases).
This study was conducted after obtaining approval from the ethics committee of the First Affiliated Hospital of Hunan Normal University.
Diagnostic criteria
A specialized training team, consisting of one associate chief nurse and two head nurses, conducted evaluations of patients’ post-operative delirium using the Intensive Care Unit Confusion Assessment Method (CAM-ICU). First, the Richmond Agitation-Sedation Scale (RASS) was used to assess the level of sedation. Patients with scores ranging from -4 to -5 were directly categorized into the delirium group. Patients with scores ranging from -3 to -4 were further evaluated based on the diagnostic criteria for delirium outlined in the Diagnostic and Statistical Manual of Mental Disorders (Fifth edition), published by the American Psychiatric Association [11]. The criteria included: Inattention or lack of focus; acute onset and fluctuating course; altered level of consciousness; disorganized thinking. Delirium was diagnosed if the patient met both of the first two criteria or if either of the last two criteria was present. The assessment was conducted once during the daytime and once at night for postoperative patients in the ICU who regained consciousness. To ensure accurate assessment, sedative medications were discontinued 30 minutes prior to the assessment for patients who had undergone postoperative sedation. Two head nurses performed the evaluation, and in cases of disagreement, the final determination was made by the associate chief nurse.
Data collection
General information, including sex, age, body mass index (BMI), preoperative complications, preoperative organ function and severity were collected. Specific parameters, including preoperative left ventricular ejection fraction (LVEF), preoperative New York Heart Association classification (NYHA), Acute Physiology and Chronic Health Evaluation II (APACHE II score), surgery-related indicators, such as timing of surgery, anesthesia duration, surgery duration, aortic cross-clamp duration, mean arterial pressure (MAP), intraoperative blood loss, and postoperative indicators like length of ICU stay, postoperative mechanical ventilation duration and MAP, were collected from the medical record system.
Outcome measures
(1) Comparative analysis of clinical baseline data between the two groups was conducted [3]. (2) Comparative analysis of preoperative LVEF, preoperative APACHE II score, surgery-related indicators (timing of surgery, anesthesia duration, surgery duration, aortic cross-clamp duration, MAP, intraoperative blood loss), and postoperative indicators (Length of ICU stay, postoperative mechanical ventilation duration and MAP) between the two groups was performed [5,6,12]. (3) Logistic regression analysis was performed to identify the potential factors associated with delirium in patients [13].
Statistical analyses
In this study, statistical analysis was performed using SPSS 20.0 (IBM Corp, Armonk, NY, USA), and graphs were generated using GraphPad Prism 7 (GraphPad Software, San Diego, USA). Counting data were presented as [n (%)] and compared between groups using the chi-square test. Measurement data were normally distributed and described by mean ± standard deviation and the inter-group comparison was conducted using the t-test. Logistic multivariate regression analysis was performed to identify risk factors associated with the occurrence of post-operative delirium. P<0.05 was considered statistically significant.
Results
Baseline data of patients
Comparative analysis of the baseline data between the two groups revealed no significant differences regarding sex, BMI, disease duration, hypertension, timing of surgery, history of smoking, history of alcohol consumption, and place of residence (all P>0.05). However, significant differences were observed in terms of age, diabetes and preoperative NYHA classification (all P<0.05, Table 1).
Table 1.
Comparison of clinical data between the two groups
| Factors | Delirium group (n = 49) | Non-delirium group (n = 165) | χ2/t | P |
|---|---|---|---|---|
| Sex | 0.103 | 0.748 | ||
| Male | 28 | 90 | ||
| Female | 21 | 75 | ||
| Age (years) | 67.34±8.00 | 62.29±5.47 | 5.069 | <0.001 |
| BMI (kg/m2) | 23.29±4.00 | 22.96±3.77 | 0.535 | 0.594 |
| Course of disease | 2.71±0.78 | 2.73±0.83 | 0.174 | 0.862 |
| Comorbid hypertension | 1.799 | 0.180 | ||
| Yes | 10 | 21 | ||
| No | 39 | 144 | ||
| Comorbid diabetes mellitus | 4.727 | 0.030 | ||
| Yes | 20 | 41 | ||
| No | 29 | 124 | ||
| Timing of surgery | 0.131 | 0.718 | ||
| Selective operation | 31 | 109 | ||
| Emergency operation | 18 | 56 | ||
| Preoperative NYHA classification | 18.071 | <0.001 | ||
| I-II | 15 | 107 | ||
| III-V | 34 | 58 | ||
| History of smoking | 2.984 | 0.084 | ||
| Yes | 18 | 40 | ||
| No | 31 | 125 | ||
| History of alcohol consumption | 1.178 | 0.278 | ||
| Yes | 16 | 41 | ||
| No | 33 | 124 | ||
| Place of incidence | 2.522 | 0.112 | ||
| Urban areas | 24 | 60 | ||
| Rural areas | 25 | 105 |
Notes: BMI: body mass index; NYHA: New York Heart Association.
Postoperative delirium occurrence and clinical manifestations
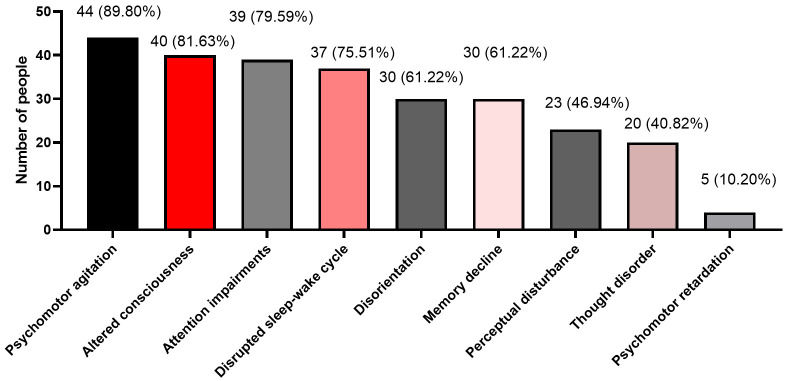
Postoperative delirium was evaluated within the patient cohort. Out of the 214 cases ana-lyzed, 49 patients experienced delirium, yielding an incidence rate of 22.90%. Among the delirious patients, 44 exhibited psychomotor agitation, 40 had altered consciousness, 39 experienced attention impairments, 37 had disrupted sleep-wake cycles, 30 exhibited disorientation, 30 had memory decline, 23 experienced perceptual disturbances, 20 had thought disorder, and 4 exhibited psychomotor retardation (Figure 1).
Figure 1.
Clinical manifestations of postoperative delirium in 49 patients.
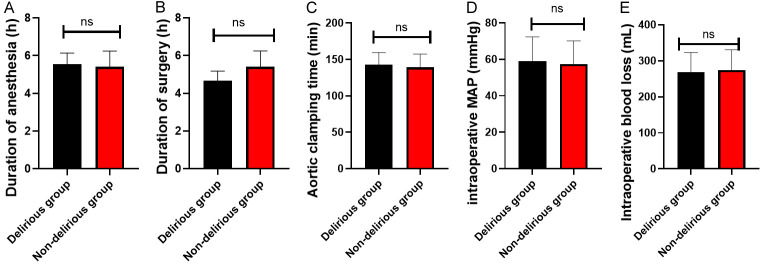
Comparison of preoperative LVEF and APACHE II scores between the two groups
The LVEF and APACHE II score in the delirium group was (51.87±4.61)% and (12.52±3.38) points, respectively; whereas those in the non-delirium group were (56.02±3.61)% and (10.75±4.20) points, respectively (Supplementary Table 1). The delirium group had significantly lower LVEF and higher APACHE II scores compared to the non-delirium group (all P<0.001, Figure 2).
Figure 2.
Comparison of preoperative LVEF and APACHE II score between the two groups. A: Comparison of LVEF between the two groups. B: Comparison of preoperative APACHE II scores between the two groups. Notes: LVEF: Left Ventricular Ejection Fraction; APACHE II: Acute Physiology and Chronic Health Evaluation II. *** indicates P<0.001; **** indicates P<0.0001.
Comparison of surgical parameters
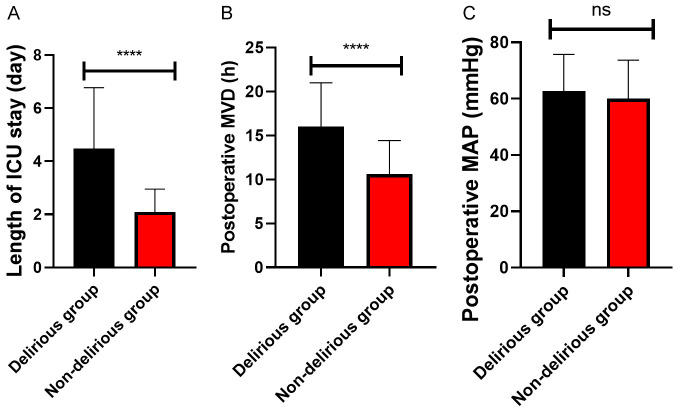
In the delirium group, anesthesia duration, surgery duration, aortic cross-clamp time, intraoperative MAP, and intraoperative blood loss were 5.54±0.60 hours, 4.66±0.52 hours, 142.74±16.70 minutes, 59.09±13.22 mmHg, and 268.39±54.75 mL, respectively; while those in the non-delirium group were 5.41±0.83 hours, 4.56±0.61 hours, 139.06±18.26 minutes, 57.44±12.67 mmHg, and 273.77±56.73 mL, respectively (Supplementary Table 2). Statistical analysis revealed no significant differences between the two groups regarding anesthesia duration, surgical duration, aortic cross-clamp time, intraoperative MAP, and intraoperative blood loss (all P>0.05, Figure 3).
Figure 3.
Comparison of surgical parameters between the two groups. A: Comparison of anesthesia duration between the two groups. B: Comparison of surgical duration between the two groups. C: Comparison of Aortic cross-clamp time between the two groups. D: Comparison of intraoperative mean arterial pressure between the two groups. E: Comparison of intraoperative blood loss between the two groups. Note: ns indicates P>0.05.
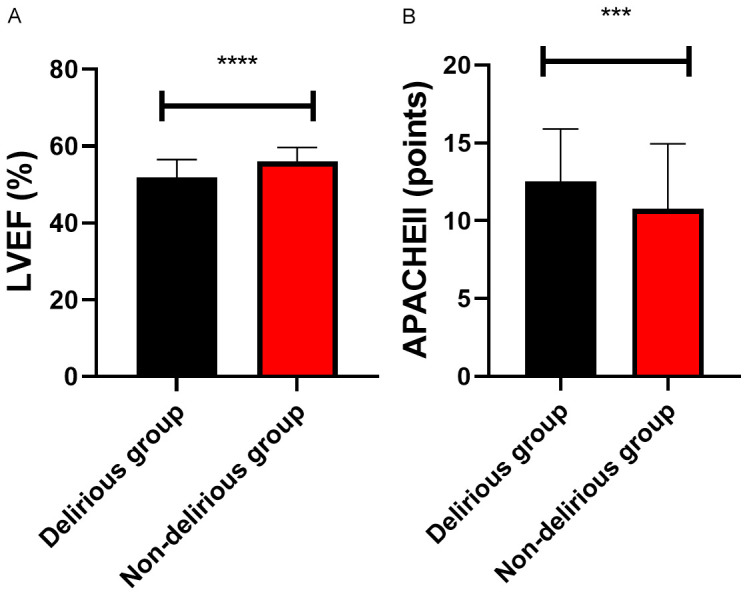
Comparison of postoperative parameters
In the delirium group, the length of ICU stay, postoperative mechanical ventilation duration, and postoperative MAP were 4.47±2.30 days, 16.01±4.98 hours, and 62.70±13.05 mmHg, respectively. Those in the non-delirium group were 2.09±0.86 days, 10.62±3.80 hours, and 60.07±13.65 mmHg, respectively (Supplementary Table 3). The delirium group experienced significantly longer ICU stay and postoperative mechanical ventilation duration than the non-delirium group (all P<0.001). However, no significant difference was found in postoperative MAP between the two groups (P>0.05, Figure 4).
Figure 4.
Comparison of postoperative parameters between the two groups. A: Comparison of length of ICU stay between the two groups. B: Comparison of postoperative mechanical ventilation duration between the two groups. C: Comparison of postoperative mean arterial pressure between the two groups. Notes: ns indicates P>0.05; **** indicates P<0.0001; ICU: intensive care unit; MVD: Mechanical ventilation duration.
Risk factors for postoperative delirium in adult patients undergoing cardiopulmonary bypass
Based on the above results, significant differences were found between the delirium and non-delirium groups in terms of age, comorbid diabetes, preoperative NYHA classification, preoperative LVEF, APACHE II score, length of ICU stay, and duration of postoperative mechanical ventilation. The parameters were then assigned values (Table 2), followed by a logistic regression analysis. Logistic regression analysis identified preoperative NYHA classification (OR: 6.755, 95% CI: 2.529-18.039, P<0.001), preoperative LVEF (OR: 6.886, 95% CI: 2.383-19.899, P<0.001), preoperative APACHE II score (OR: 6.755, 95% CI: 2.740-22.135, P<0.001), leng-th of ICU stay (OR: 9.463, 95% CI: 3.563-25.135, P<0.001), and postoperative mechanical ventilation duration (OR: 9.744, 95% CI: 3.419-27.768, P<0.001) as independent factors influencing the occurrence of delirium in adult patients undergoing cardiopulmonary bypass in cardiac surgery (Table 3).
Table 2.
Assignment table
| Factors | Assignment |
|---|---|
| Age | <63.5 years = 0, ≥63.5 years = 1 |
| Comorbid diabetics | No = 0, Yes = 1 |
| Preoperative NYHA classification | I-II = 0, III-IV = 1 |
| LVEF | ≥55.07 = 0, <55.07 = 1 |
| APACHE II score | <11.50 = 0, ≥11.50 = 1 |
| Length of ICU stay | <2.63 = 0, ≥2.63 = 1 |
| Postoperative mechanical ventilation duration | <11.85 = 0, ≥11.85 = 1 |
| Delirium or not | No delirium = 0, delirium = 1 |
Notes: LVEF: left ventricular ejection fraction; APACHE II: Acute Physiology and Chronic Health Evaluation II; ICU: intensive care unit.
Table 3.
Multivariate logistic regression analysis
| Factors | B | S.E. | Wals | df | Sig. | Exp (B) | 95% C.I. for EXP (B) | |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Lower limit | Upper limit | |||||||
| Age | 0.644 | 0.480 | 1.800 | 1 | 0.180 | 1.905 | 0.743 | 4.882 |
| Comorbid diabetes mellitus | -0.289 | 0.589 | 0.240 | 1 | 0.624 | 0.749 | 0.236 | 2.378 |
| Preoperative NYHA classification | 1.910 | 0.501 | 14.527 | 1 | <0.001 | 6.755 | 2.529 | 18.039 |
| LVEF | 1.930 | 0.541 | 12.701 | 1 | <0.001 | 6.886 | 2.383 | 19.899 |
| APACHE II score | 2.053 | 0.533 | 14.833 | 1 | <0.001 | 7.788 | 2.740 | 22.135 |
| Length of ICU stay | 2.247 | 0.498 | 20.334 | 1 | <0.001 | 9.463 | 3.563 | 25.135 |
| Postoperative mechanical ventilation duration | 2.277 | 0.534 | 18.157 | 1 | <0.001 | 9.744 | 3.419 | 27.768 |
Notes: NYHA: New York Heart Association; LVEF: left ventricular ejection fraction; APACHE II: Acute Physiology and Chronic Health Evaluation II; ICU: intensive care unit.
Discussion
Delirium is a common complication following cardiac bypass surgery, characterized by sudden onset of confusion in patients with normal preoperative mental status [12,13]. This study investigated the risk factors associated with the occurrence of postoperative delirium in adult patients undergoing cardiopulmonary bypass in cardiac surgery. A total of 214 patients undergoing cardiopulmonary bypass in cardiac surgery were enrolled for the study, and among them, 49 patients developed delirium, resulting in an incidence rate of 22.90%. Most patients with delirium exhibited symptoms such as psychomotor agitation, altered level of consciousness, attention disturbances, disrupted sleep-wake cycle, disorientation, and impaired memory. The results highlight that delirium is a frequent complication in adult cardiac bypass surgery, negatively impacting patients’ psychological well-being, cognition, emotions, and behavior [14]. Prior research has reported delirium incidence ranging from 15% to 50% [15]. The 22.90% incidence rate in this study falls within the lower end of this range and is consistent with previous research.
The comparative analysis conducted in this study demonstrated a noteworthy correlation between patients’ age, diabetes, and the incidence of delirium. As individuals age, their physiological reserves, including cognitive function and the adaptive capacity of the nervous system, generally decline, rendering them more vulnerable to postoperative delirium [10,16]. Numerous studies have confirmed advanced age as an important risk factor for postoperative delirium. Elderly patients often have chronic illnesses and undergo polypharmacy, which may increase the risk of delirium. For instance, Rosenberg [17] found a significant increase in the risk of delirium in elderly patients. Additionally, a study on postoperative delirium in esophageal cancer patients suggested that advancing age is a risk factor for delirium and proposed identifying predisposing factors such as age and pre-existing pulmonary diseases, as well as selecting appropriate surgical treatments, to reduce delirium occurrence and improve surgical outcomes [18]. A meta-analysis conducted by Chen et al. found that diabetes is also a risk factor for delirium following cardiac surgery [13]. Furthermore, Visser et al. [14] proposed that diabetes is one of the causes of postoperative delirium in vascular surgery patients. These results suggest that age and diabetes, as patient-related factors, significantly impact the occurrence of postoperative delirium. However, in this study, age and diabetes were not identified as independent risk factors for delirium in patients. This discrepancy may be attributed to the sample size and heterogeneity of the study population.
The study also found significant differences between delirious and non-delirious patients in terms of preoperative NYHA, LVEF, APACHE II score, length of ICU stay, and postoperative mechanical ventilation duration. These factors were identified as independent influencing factors for postoperative delirium in adult cardiac bypass surgery. Preoperative NYHA classification and LVEF are commonly used to assess the severity of cardiac function [19,20]. Poor cardiac function and decreased LVEF may be associated with the severity of heart disease and impaired myocardial function. Chen et al. [12] also found that NYHA classification III or IV was one of the risk factors for postoperative delirium. The APACHE II score is an indicator used to assess the severity and prognosis of critically ill patients [21]. A higher APACHE II score reflects a more severe disease state and worse prognosis, which is associated with an increased incidence of postoperative delirium [22]. Elevated APACHE II scores often reflect a more intense inflammatory response [23], which can disturb neurotransmitter balance and brain function, particularly after major surgeries like cardiac surgery, thereby heightening the risk of delirium [24]. Elevated APACHE II score often indicates a disturbance in the patient’s metabolic and stress response, consequently elevating the risk of delirium [25,26]. Additionally, the ICU environment and mechanical ventilation can negatively affect patients’ sleep and neurological functioning [27,28]. On the other hand, the use of benzodiazepines and opioids, commonly used in the ICU, can also increase the incidence of delirium [29]. Li et al. [30] found that APACHE II score, length of ICU stay, and the use of sedatives are common risk factors for ICU delirium and its duration, which supports the findings of this study. Furthermore, the unfamiliar ICU environment and physical restraints can agitate patients and trigger delirium [31].
Implementing appropriate nursing measures can help prevent the occurrence of delirium. For patients with preexisting diabetes, providing symptomatic treatment to improve their overall condition is crucial. Patients with poor preoperative cardiac function, especially those classified as NYHA III and IV, should receive extra attention, and preoperative measures should be taken to improve their cardiac function according to medical advice [32]. For patients with relatively low LVEF and relatively high APACHE II scores, a tailored and optimized treatment plan should be developed and implemented in collaboration with the medical team, considering the specific circumstances of each patient. It is essential to conduct vigilant monitoring of patients, encompassing assessments of cardiac function, respiratory status, vital signs, and pertinent indicators. Regular assessment of patient’s condition can help promptly adjust treatment plans and nursing measures. In addition, preoperative education and psychological care should be strengthened. Patients should be informed about the necessity of postoperative ICU admission, including what to expect in the ICU environment and associated nursing measures. Implementing these measures will facilitate patients to adapt to the ICU environment. Patients experiencing preoperative tension, anxiety, and insomnia should receive particular attention, with an emphasis on providing enhanced psychological care. Additionally, adherence to extubation criteria is also crucial. When the patient’s condition allows, early removal of organ tubes should be performed for patients who meet the extubation criteria to shorten the duration of mechanical ventilation and facilitate transfer to a general ward.
This study has certain limitations. For example, the sample size was small, which limits the reliability and generalizability of the study. In addition, factors such as educational level, medication history, and blood biochemistry indicators were not accurately assessed, which may affect the interpretation and inference of the results.
In conclusion, postoperative delirium is a prevalent complication among patients undergoing cardiac surgery. This study identifies key factors independently contributing to the development of delirium in adult cardiac bypass surgery patients, including preoperative NYHA classification of III or IV, lower LVEF, higher APACHE II scores, extended ICU stays, and prolonged postoperative mechanical ventilation duration. The presence of numerous intricate risk factors underscores the significance of promptly identifying and addressing these variables in the context of delirium occurrence during adult cardiac bypass surgery.
Disclosure of conflict of interest
None.
Supporting Information
References
- 1.Zhang X, Lu J, Yang Y, Cui J, Zhang X, Xu W, Song L, Wu C, Wang Q, Wang Y, Wang R, Li X. Cardiovascular disease prevention and mortality across 1 million urban populations in China: data from a nationwide population-based study. Lancet Public Health. 2022;7:e1041–e1050. doi: 10.1016/S2468-2667(22)00170-0. [DOI] [PubMed] [Google Scholar]
- 2.Du X, Patel A, Anderson CS, Dong J, Ma C. Epidemiology of cardiovascular disease in China and opportunities for improvement: JACC International. J Am Coll Cardiol. 2019;73:3135–3147. doi: 10.1016/j.jacc.2019.04.036. [DOI] [PubMed] [Google Scholar]
- 3.Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell FE Jr, Inouye SK, Bernard GR, Dittus RS. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291:1753–1762. doi: 10.1001/jama.291.14.1753. [DOI] [PubMed] [Google Scholar]
- 4.Aldecoa C, Bettelli G, Bilotta F, Sanders RD, Audisio R, Borozdina A, Cherubini A, Jones C, Kehlet H, MacLullich A, Radtke F, Riese F, Slooter AJ, Veyckemans F, Kramer S, Neuner B, Weiss B, Spies CD. European Society of Anaesthesiology evidence-based and consensus-based guideline on postoperative delirium. Eur J Anaesthesiol. 2017;34:192–214. doi: 10.1097/EJA.0000000000000594. [DOI] [PubMed] [Google Scholar]
- 5.Mart MF, Williams Roberson S, Salas B, Pandharipande PP, Ely EW. Prevention and management of delirium in the intensive care unit. Semin Respir Crit Care Med. 2021;42:112–126. doi: 10.1055/s-0040-1710572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jin Z, Hu J, Ma D. Postoperative delirium: perioperative assessment, risk reduction, and management. Br J Anaesth. 2020;125:492–504. doi: 10.1016/j.bja.2020.06.063. [DOI] [PubMed] [Google Scholar]
- 7.Ibrahim K, McCarthy CP, McCarthy KJ, Brown CH, Needham DM, Januzzi JL Jr, McEvoy JW. Delirium in the cardiac intensive care unit. J Am Heart Assoc. 2018;7:e008568. doi: 10.1161/JAHA.118.008568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huet O, Gargadennec T, Oilleau JF, Rozec B, Nesseler N, Bouglé A, Kerforne T, Lasocki S, Eljezi V, Dessertaine G, Amour J, Chapalain X EXACTUM and the Atlanrea Study Group. Prevention of post-operative delirium using an overnight infusion of dexmedetomidine in patients undergoing cardiac surgery: a pragmatic, randomized, double-blind, placebo-controlled trial. Crit Care. 2024;28:64. doi: 10.1186/s13054-024-04842-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhao L, Zhu H, Mao W, Zhou X, Xie Y, Li L. Effects of perioperative cognitive function training on postoperative cognitive dysfunction and postoperative delirium: a systematic review and meta-analysis. Front Neurol. 2023;14:1146164. doi: 10.3389/fneur.2023.1146164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oren RL, Kim EJ, Leonard AK, Rosner B, Chibnik LB, Das S, Grodstein F, Crosby G, Culley DJ. Age-dependent differences and similarities in the plasma proteomic signature of postoperative delirium. Sci Rep. 2023;13:7431. doi: 10.1038/s41598-023-34447-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Regier DA, Kuhl EA, Kupfer DJ. The DSM-5: classification and criteria changes. World Psychiatry. 2013;12:92–98. doi: 10.1002/wps.20050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen H, Mo L, Hu H, Ou Y, Luo J. Risk factors of postoperative delirium after cardiac surgery: a meta-analysis. J Cardiothorac Surg. 2021;16:113. doi: 10.1186/s13019-021-01496-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosenberg K. Risk factors for postoperative delirium identified. Am J Nurs. 2022;122:58. doi: 10.1097/01.NAJ.0000890236.06639.f4. [DOI] [PubMed] [Google Scholar]
- 14.Visser L, Prent A, Banning LBD, van Leeuwen BL, Zeebregts CJ, Pol RA. Risk factors for delirium after vascular surgery: a systematic review and meta-analysis. Ann Vasc Surg. 2021;76:500–513. doi: 10.1016/j.avsg.2021.03.034. [DOI] [PubMed] [Google Scholar]
- 15.Martínez-Arnau FM, Buigues C, Pérez-Ros P. Incidence of delirium in older people with cancer: systematic review and meta-analysis. Eur J Oncol Nurs. 2023;67:102457. doi: 10.1016/j.ejon.2023.102457. [DOI] [PubMed] [Google Scholar]
- 16.Kappen PR, Kakar E, Dirven CMF, van der Jagt M, Klimek M, Osse RJ, Vincent APJE. Delirium in neurosurgery: a systematic review and meta-analysis. Neurosurg Rev. 2022;45:329–341. doi: 10.1007/s10143-021-01619-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rosenberg K. Incidence of postoperative delirium is similar with regional and general anesthesia. Am J Nurs. 2022;122:56. doi: 10.1097/01.NAJ.0000827344.66160.9b. [DOI] [PubMed] [Google Scholar]
- 18.Dezube AR, Bravo-Iñiguez CE, Yelamanchili N, De León LE, Tarascio J, Jaklitsch MT, Wee JO. Risk factors for delirium after esophagectomy. J Surg Oncol. 2020;121:645–653. doi: 10.1002/jso.25835. [DOI] [PubMed] [Google Scholar]
- 19.Menzenbach J, Kirfel A, Guttenthaler V, Feggeler J, Hilbert T, Ricchiuto A, Staerk C, Mayr A, Coburn M, Wittmann M PROPDESC Collaboration Group. PRe-operative prediction of postoperative delirium by appropriate screening (PROPDESC) development and validation of a pragmatic POD risk screening score based on routine preoperative data. J Clin Anesth. 2022;78:110684. doi: 10.1016/j.jclinane.2022.110684. [DOI] [PubMed] [Google Scholar]
- 20.Baumhove L, Tromp J, Figarska S, van Essen BJ, Anker SD, Dickstein K, Cleland JG, Lang CC, Filippatos G, Ng LL, Samani NJ, Metra M, van Veldhuisen DJ, Lam CSP, Voors AA, van der Meer P. Heart failure with normal LVEF in BIOSTAT-CHF. Int J Cardiol. 2022;364:85–90. doi: 10.1016/j.ijcard.2022.05.054. [DOI] [PubMed] [Google Scholar]
- 21.Kaur H, Chandran VP, Rashid M, Kunhikatta V, Poojari PG, Bakkannavar SM, Balakrishnan JM, Thunga G. The significance of APACHE II as a predictor of mortality in paraquat poisoning: a systematic review and meta-analysis. J Forensic Leg Med. 2023;97:102548. doi: 10.1016/j.jflm.2023.102548. [DOI] [PubMed] [Google Scholar]
- 22.Khan BA, Perkins AJ, Prasad NK, Shekhar A, Campbell NL, Gao S, Wang S, Khan SH, Marcantonio ER, Twigg HL 3rd, Boustani MA. Biomarkers of delirium duration and delirium severity in the ICU. Crit Care Med. 2020;48:353–361. doi: 10.1097/CCM.0000000000004139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Luo Y, Wang Z, Wang C. Improvement of APACHE II score system for disease severity based on XGBoost algorithm. BMC Med Inform Decis Mak. 2021;21:237. doi: 10.1186/s12911-021-01591-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kotackova L, Marecek R, Mouraviev A, Tang A, Brazdil M, Cierny M, Paus T, Pausova Z, Mareckova K. Bariatric surgery and its impact on depressive symptoms, cognition, brain and inflammation. Front Endocrinol (Lausanne) 2023;14:1171244. doi: 10.3389/fendo.2023.1171244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rahmatinejad Z, Tohidinezhad F, Reihani H, Rahmatinejad F, Pourmand A, Abu-Hanna A, Eslami S. Prognostic utilization of models based on the APACHE II, APACHE IV, and SAPS II scores for predicting in-hospital mortality in emergency department. Am J Emerg Med. 2020;38:1841–1846. doi: 10.1016/j.ajem.2020.05.053. [DOI] [PubMed] [Google Scholar]
- 26.Gonzalez-Baz MD, Pacheco Del Cerro E, Ferrer-Ferrándiz E, Araque-Criado I, Merchán-Arjona R, de la Rubia Gonzalez T, Moro Tejedor MN. Psychometric validation of the Kolcaba general comfort questionnaire in critically ill patients. Aust Crit Care. 2023;36:1025–1034. doi: 10.1016/j.aucc.2022.12.013. [DOI] [PubMed] [Google Scholar]
- 27.Brunker LB, Boncyk CS, Rengel KF, Hughes CG. Elderly patients and management in intensive care units (ICU): clinical challenges. Clin Interv Aging. 2023;18:93–112. doi: 10.2147/CIA.S365968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roshdy A. Respiratory monitoring during mechanical ventilation: the present and the future. J Intensive Care Med. 2023;38:407–417. doi: 10.1177/08850666231153371. [DOI] [PubMed] [Google Scholar]
- 29.Liu SB, Liu S, Gao K, Wu GZ, Zu G, Jie Liu J. Olanzapine for the treatment of ICU delirium: a systematic review and meta-analysis. Ther Adv Psychopharmacol. 2023;13:20451253231152113. doi: 10.1177/20451253231152113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li Y, Yuan D, Li X, Wang S. Risk factors for delirium in intensive care unit and its duration. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2020;32:62–66. doi: 10.3760/cma.j.cn121430-20190909-00011. [DOI] [PubMed] [Google Scholar]
- 31.Ali M, Cascella M. ICU Delirium. In: StatPearls. Treasure Island (FL) ineligible companies; Disclosure: Marco Cascella declares no relevant financial relationships with ineligible companies.: StatPearls Publishing Copyright © 2024, StatPearls Publishing LLC.; 2024. [Google Scholar]
- 32.Yacoub MS, El-Nakhal T, Hasabo EA, Shehata N, Wilson K, Ismail KH, Bakr MS, Mohsen M, Mohamed A, Abdelazim E, Ali HT, Soliman Z, Sayed A, Abdelsayed K, Caliskan K, Soliman O. A systematic review and meta-analysis of the efficacy and safety of Mavacamten therapy in international cohort of 524 patients with hypertrophic cardiomyopathy. Heart Fail Rev. 2024;29:479–496. doi: 10.1007/s10741-023-10375-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.