Abstract
We are reporting the successful treatment of a rare case of spontaneous suprachoroidal hemorrhage (SSCH) in a young refractory glaucoma patient with rhegmatogenous retinal detachment (RRD). The 34-year-old male was admitted to our hospital having experienced pain in his right eye for two days. The patient had a history of glaucoma and long axial length in the right eye with chronic poorly controlled intraocular pressure (IOP) and acute hypotony. Following clinical examinations, the patient was diagnosed with SSCH with RRD in the right eye. The patient underwent drainage of the suprachoroidal hemorrhage and vitrectomy combined with gas injection to address retinal and choroidal detachment. During the following two months, the patient’s retina remained attached. Long axial length and persistent high IOP are two major risk factors of SSCH with RRD, while acute hypotony appeared to be a precipitating factor in this case. Surgeons can consider alternative tamponade options, such as gases, during vitrectomy to treat SSCH with RRD.
Keywords: Spontaneous suprachoroidal hemorrhage, rhegmatogenous retinal detachment, vitrectomy, gas, case report
Introduction
Suprachoroidal hemorrhage (SCH) is an uncommon complication that can result from all types of intraocular surgery [1]. Spontaneous suprachoroidal hemorrhage (SSCH) is even rarer, with only a few documented cases and mainly associated with systemic diseases such as coagulation disorders [2]. SSCH with rhegmatogenous retinal detachment (RRD) is exceedingly uncommon and predominantly observed in geriatric individuals [3,4]. The exact cause of SSCH with RRD is still unclear. Reduced intraocular pressure (IOP) caused by RRD may contribute to SCH. There is evidence that low intraocular pressure may cause sudden changes in vascular gradients, decreased uveoscleral outflow, and the dilation or even rupture of choroidal vessels, thus resulting in blood rupturing into the suprachoroidal space [1]. Drainage surgery alone or vitreoretinal surgery combined with drainage surgery is the most common surgical treatment for SSCH with RRD [1], which exhibits high rates of failure, with silicone oil tamponade considered a mainstay treatment agent [3,4]. Although gas and silicone oil are equally effective in vitrectomy, gas has been shown to be effective for reducing the occurrence of glaucoma and uveitis. In this report, we present the case of a 34-year-old male patient diagnosed with SSCH with RRD, whose conditions were successfully resolved through a single surgical intervention employing gas tamponade instead of silicone oil.
Case report
A 34-year-old male patient who had experienced pain in his right eye for two days was admitted to our hospital. The patient had a history of bilateral congenital cataract. The patient was diagnosed at birth with bilateral cataracts of unknown etiology, which was likely caused by genetic factors. In addition, he knew of no history of systemic and family diseases, or any prior anticoagulant medication history. During a span of 30 years, the individual had undergone surgical interventions for congenital binocular cataract, secondary glaucoma in the right eye that necessitated trabeculectomy, and multiple filtering surgeries due to inadequate control of IOP (with no clear or specific details). Eventually, the patient declined further surgical procedures for the right eye due to excessive scarring of the filter tract. For the past 25 years, the patient has been using brinzolamide eye drops twice daily, while maintaining IOP at 40 mmHg in his right eye. The individual had experienced blindness in the right eye for approximately eight years. The patient had no other ocular history except for phacoemulsification and intraocular lens (IOL) implantation performed 30 years ago for congenital cataract in the left eye. Once admitted, the patient’s visual acuity was assessed. There was no light perception in the right eye and 0.6 in the left eye. IOP was determined to be 8 mmHg in the right eye and 15 mmHg in the left eye. Ocular examination of the right eye (Figure 1) revealed conjunctival scarring, mild corneal edema, absence of IOL, and a superior periiris incision. The vitreous body exhibited slight turbidity without hemorrhage. Retinal detachment was observed along with evident choroidal detachment. No obvious retinal holes were detected due to the masking of vitreous opacity. Ophthalmic examination of the left eye showed an IOL in situ and posterior capsular opacification. Moreover, the remaining anterior segment as well as the vitreous and fundus of the left eye showed no abnormalities. B-ultrasound imaging of the right eye confirmed both retinal and choroidal detachment, and identified a significant number of dense punctate echoes (considered SCH) (Figure 2A). Optical coherence tomography (OCT) of the right eye demonstrated retinal attachment in the macular region (Figure 2B). An IOL master determined the axial length of the right eye to be 28.61 mm. Results from several routine blood tests including a clotting screen, fasting glucose, and liver and kidney functions were normal.
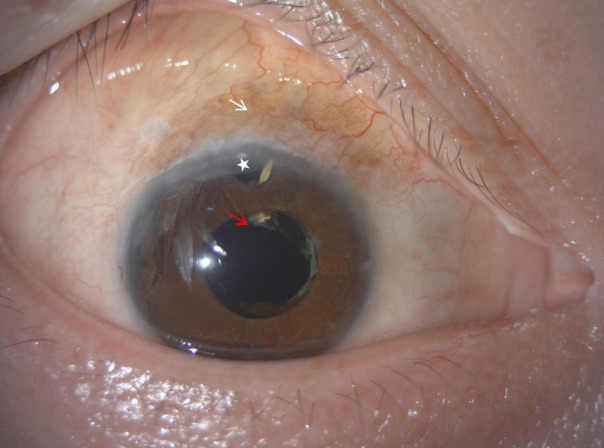
Figure 1.
Presentation of the slit-lamp image of the right eye: Conjunctival scarring (white arrow), absence of intraocular lens (red arrow), and a superior periiris incision (white star).
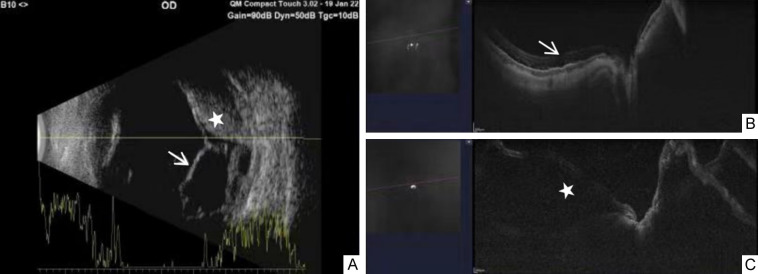
Figure 2.
Presentation of the right eye before surgery. A: B-Scan ultrasonographic confirmed retinal detachment (white arrow) with massive suprachoroidal hemorrhage (white star). B: Optical coherence tomography (OCT) showed macular attachment (white arrow). C: OCT showed aggravated retinal detachment involving the macula (white star).
Failure to detect obvious retinal holes led us to consider the possibility of exudative retinal detachment, although we could not exclude the possibility of RRD because we might have missed the holes. Given the long history of blindness in the patient’s right eye, we decided to take a more conservative approach. Following one week of oral administration of 30 mg dexamethasone and atropine eye drops, ophthalmologic examination of the right eye found no perception of light in the right eye and IOP of 11 mmHg. Although SCH was reduced, retinal detachment did not improve significantly. The patient also experienced relief of pain and was discharged with continued observation under medication.
After three weeks, a review by the ophthalmology department found that the patient had decreased IOP (5 mmHg) in his right eye, and retinal detachment in the right eye had worsened with detectable macular detachment, which was confirmed by OCT (Figure 2C). Subsequently, the patient underwent drainage of the suprachoroidal cavity and vitrectomy with gas tamponade, all of which were performed under local anesthesia. Due to years-long blindness in the right eye, the patient had declined IOL implantation during vitrectomy.
During the surgical procedure, a routine three-channel vitrectomy cannula of size 23 G was inserted at a distance of 3.5 mm from the limbus. An infusion line was inserted into the vitreous cavity. The suprachoroidal cavity was punctured using a 20 G scleral puncture knife located at 1 o’clock at 3.5 mm from the corneal limbus, allowing blood to be expelled under the pressure of the infusion fluid. Subsequent vitrectomy revealed a retinal hole in the superonasal ora serrata, which was promptly closed through laser photocoagulation. Given the near-complete drainage of the hemorrhage accumulation in the choroid cavity and the absence of proliferative vitreoretinopathy (PVR), disinfection air tamponade was employed in the cavity at the conclusion of the surgical procedure.
When examined six days after the surgical procedure, there remained no perception of light in the patient’s right eye, and IOP was 15 mmHg. Retina reattachment was observed, along with the remaining gas interface above (Figure 3A). Additionally, the retinal hole was closed with no hemorrhage in the suprachoroidal cavity (Figure 3B). Macular reattachment was confirmed through OCT imaging (Figure 3C). The patient was referred to a glaucoma specialist for further treatment three weeks after surgery, due to elevated IOP. After two years, the retina remained attached and there was no obvious preretinal proliferation, although the patient’s visual status was still no perception of light in the right eye.
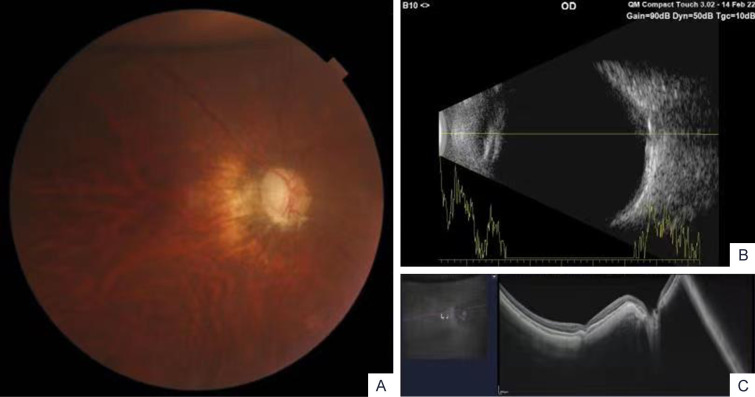
Figure 3.
Presentation of the right eye after surgery. A: Fundus photo showed attached retina with residual gas visible above. B: B-Scan ultrasonography showed retinal reattachment and absorption of suprachoroidal hemorrhage. C: Optical coherence tomography revealed macular reattachment.
Discussion
SCH is a rare event, whose reported incidence ranges from 0.06% to 1.8% [5]. This complication primarily manifests following intraocular surgeries, particularly glaucoma filtration procedures. SCH is associated with risk factors such as systemic hypertension, diabetes mellitus, intraoperative tachycardia, arteriosclerosis, and coagulation disorders [1,5,6]. SSCH is exceedingly rare and has been documented in a very limited number of studies [3,4]. One SSCH risk factor is the use of anticoagulants. SSCH with RRD is an extremely uncommon occurrence [3,4], primarily observed in elderly patients with hypotony, long axial length, and severe vitreous inflammation. Furthermore, there is a high failure rate following vitreoretinal surgeries, which typically involve the use of silicone oil tamponade, in patients suffering from SSCH with RRD.
The exact cause of SSCH with RRD remains uncertain. Zhang et al. conducted a study involving six cases of RRD and extensive SSCH [3], none of whom exhibited any prior history of systemic diseases or oral anticoagulant usage. Similarly, Chai et al. also reported a case of SSCH with RRD in a patient with no history of systemic diseases or oral anticoagulant usage [4]. In our present case report, the patient lacked any history of systemic diseases or anticoagulant usage as well, which is in contrast to cases of SCH following intraocular surgeries. This observation contradicts the systemic factors previously documented for SSCH patients [2]. The mean age of patients in the Zhang et al. study was 56.3 years and the patient in the Chai et al. study was 71 years old. In contrast, the patient in the present case report was 34 years old, suggesting a lack of association between age and SSCH with RRD.
Hypotony is one of the most common characteristics of patients with SSCH with RRD [3,4]. Low IOP may lead to abrupt alterations in the vascular gradient, diminished uveoscleral outflow, and expansion or even rupture of choroidal vessels, resulting in hemorrhage into the suprachoroidal space [1]. Here, the patient experienced a decrease in IOP from prolonged ocular hypertension to 8 mmHg, which triggered the onset of SSCH to some extent. Similarly, previous research also supports the notion that patients suffering from SSCH complicated with RRD should exhibit IOP levels below the normal range (10 mmHg-21 mmHg) [3,4].
Previous investigations have identified the presence of vortex vein varix in conjunction with an elongated axial length as a risk factor for SSCH [6]. Patients in the reports by Zhang et al. and Chai et al. had an abnormal axial length exceeding 30 mm. In the present case report, the patient exhibited an axial length of 28.61 mm, which appears to be a common underlying pathologic factor contributing to bleeding. SCH occurrence may thus be attributed to choroidal effusion resulting from choroidal vasodilation that is caused by long axial length, as well as the decrease in IOP caused by RRD [3,4]. Our patient had a previous history of elevated IOP, which subsequently decreased following retinal detachment. The significant alteration in IOP likely led to rapid expansion of choroidal vessels and subsequent SSCH.
Both gas and silicone oil have comparable efficacy in vitrectomy, with gas demonstrating effectiveness for reducing the occurrence of glaucoma and uveitis. Zhang et al. observed that the presence of PVR hindered the removal of silicone oil in numerous patients [3]. Similarly, the patient in Chai et al. involved a subsequent surgical procedure to remove the retinal proliferative membrane [4]. In contrast, our case study achieved remarkable outcomes by employing a gas rather than silicone oil tamponade, obviating the necessity for additional operations. Such favorable outcomes may be attributed to three factors. First, a degenerative hole was present, as smaller tear breaks have been demonstrated to reduce the risk of failure compared to larger tear breaks [7]. Second, the absence of PVR made gas tamponade more effective. Finally, the utilization of a 23 G instead of 20 G operation, which caused less damage and yielded better outcomes [8].
Conclusion
Despite this patient’s relatively young age and lack of systemic illnesses, the combination of long axial length, persistent high IOP, and acute hypotony contributed to the development of SCH with RRD. Our findings suggest that eye surgeons should pay particular attention to patients with myopia and refractory glaucoma since they may be at higher risk of retinal detachment and SSCH. Moreover, silicone oil tamponade should not be considered the only treatment choice in patients with SSCH with RRD. In future vitrectomy for treating SCH with RRD, alternative tamponade options, such as gas, should be considered in order to minimize the necessity of multiple or repeat procedures.
Acknowledgements
This work was supported by the Science and Technology Development Project of Shandong Second Medical University, China (No. 2023FYM087).
Disclosure of conflict of interest
None.
References
- 1.Chu TG, Green RL. Suprachoroidal hemorrhage. Surv Ophthalmol. 1999;43:471–486. doi: 10.1016/s0039-6257(99)00037-5. [DOI] [PubMed] [Google Scholar]
- 2.Akkan Aydoğmuş FS, Serdar K, Kalayci D, Çelik A. Spontaneous suprachoroidal hemorrhage associated with iatrogenic coagulopathy. Retin Cases Brief Rep. 2019;13:174–175. doi: 10.1097/ICB.0000000000000554. [DOI] [PubMed] [Google Scholar]
- 3.Zhang J, Zhu XH, Tang LS. Rhegmatogenous retinal detachment associated with massive spontaneous suprachoroidal hemorrhage and prognosis of pars plana vitrectomy. Int J Ophthalmol. 2014;7:850–854. doi: 10.3980/j.issn.2222-3959.2014.05.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chai F, Zeng L, Li C, Zhao X. Spontaneous suprachoroidal hemorrhage in a high myopia patient with rhegmatogenous retinal detachment: a case report and literature review. Biosci Rep. 2019;39:BSR20181454. doi: 10.1042/BSR20181454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wood EH, Moinuddin O, Rao P, Drenser KA, Trese MT, Capone A Jr. Surgical management of suprachoroidal hemorrhage in younger patients. Ophthalmic Surg Lasers Imaging Retina. 2019;50:454–458. doi: 10.3928/23258160-20190703-08. [DOI] [PubMed] [Google Scholar]
- 6.Milani P, Mazzola M, Bergamini F. Suprachoroidal haemhorrage and vortex vein varix: a potential association. Eur J Ophthalmol. 2022;32:NP130–NP133. doi: 10.1177/1120672120964033. [DOI] [PubMed] [Google Scholar]
- 7.Adelman RA, Parnes AJ, Michalewska Z, Ducournau D European Vitreo-Retinal Society (EVRS) Retinal Detachment Study Group. Clinical variables associated with failure of retinal detachment repair: the European Vitreo-Retinal Society retinal detachment study report number 4. Ophthalmology. 2014;121:1715–1719. doi: 10.1016/j.ophtha.2014.03.012. [DOI] [PubMed] [Google Scholar]
- 8.Chen GH, Tzekov R, Jiang FZ, Mao SH, Tong YH, Li WS. Iatrogenic retinal breaks and postoperative retinal detachments in microincision vitrectomy surgery compared with conventional 20-gauge vitrectomy: a meta-analysis. Eye (Lond) 2019;33:785–795. doi: 10.1038/s41433-018-0319-5. [DOI] [PMC free article] [PubMed] [Google Scholar]