Abstract
Purpose: The purpose of this study was to explore the application value of Neuman’s nursing model in perioperative nursing for patients undergoing modified radical mastectomy. Method: A retrospective collection of data from breast cancer patients treated at Shanxi Bethune Hospital between January 2019 and December 2022 was conducted. Patients who received conventional nursing interventions were included in the conventional group. Patients who received intervention using Neuman’s nursing model were placed in the study group. The psychological and physiological stress levels, quality of life, complications, nursing quality, and patient satisfaction during the perioperative period were compared between the two groups. Results: Postoperatively, the incidences of psychological stress, physiological stress, and complications in breast cancer patients who were intervened by Neuman’s nursing model were significantly lower than those of patients receiving conventional nursing (all P < 0.05). Their quality of life was significantly higher than that of patients in the conventional group (P < 0.05). Nursing personnel under Neuman’s nursing model scored significantly higher in terms of nursing operations, nursing attitude, completion of nursing work, and patient’s cooperation (all P < 0.05). There was a significant difference in the degree of satisfaction between the two groups, with higher rates of “very satisfied” and “satisfied” patients in the Neuman’s nursing model group compared to the conventional nursing group (Z=-2.036, P=0.042). Conclusion: The use of Neuman’s nursing model in perioperative nursing for breast cancer patients can reduce the incidence of psychological and physiological stress. It improves nursing quality, patient’s quality of life, and satisfaction with nursing.
Keywords: Breast cancer, modified radical mastectomy, Neuman’s nursing model, perioperative period, nursing quality
Introduction
The latest global cancer statistics revealed the incidence of breast cancer (BC) in women is 11.7%, surpassing lung cancer (11.4%). This makes breast cancer the most common cancer threatening women’s health and lives [1]. In China, due to a lack of health awareness, quite many people do not undergo annual health examinations and are often unaware of the disease until it has progressed significantly, increasing the difficulty and cost of treatment. Zhang et al. [2] have demonstrated that nearly 13% of BC patients in China spend over 40% of their family income on treatment. This indicates that BC endangers the health of patients and places significant financial pressure on their families and society.
The various methods used to treat BC include surgery, endocrine therapy, chemotherapy, targeted therapy, radiotherapy, and immunotherapy. With surgery remaining the most used in clinical practice [3-7]. BC surgery includes lumpectomy and radical mastectomy. Factors such as tumor nature, breast size, and recurrence rate limit the application of lumpectomy, resulting in few breast cancer patients choosing this treatment method [8,9]. Radical mastectomy, includes the preservation of pectoralis major in Patey’s mode and preservation of both the pectoralis major and pectoralis minor in Auchincloss’ mode. This is the most commonly used method for treating BC. Surgery can effectively remove the lesions and prolong the patient’s survival. It can cause damage to the patient’s skin, breasts, muscles, and tissue structures, leading to conditions such as soft tissue fibrosis and decreased muscle contractility [10]. After surgery, complications such as cutaneous lymphedema, functional impairment on the affected side, and shoulder dysfunction can cause significant distress for the patient [11,12]. The loss of breasts resulting from surgery alters the patient’s appearance, causing a psychological stress response. It is clinically necessary to provide excellent nursing care for BC patients to minimize their physiological and psychological stress [13].
The perioperative period is crucial for patients with BC, as they face various stresses, including the threat to their life from the disease, the risks associated with surgery, the pain of the wound, and the loss of social function [14]. This timeframe is pivotal for engaging in functional exercises, preventing complications, and bolstering mental health. Without effective nursing intervention during this time, patient’s treatment compliance, treatment effectiveness, and quality of life will be greatly affected. Research has shown that patients with BC experience psychological issues and negative feelings during this period [15,16]. Using this special period to help patients and their relatives adopt appropriate coping techniques and make adjustments in physiological function, psychological state, self-esteem, self-efficacy, and coping methods is essential for enhancing their quality of life.
Based on a holistic view, Neuman’s nursing model emphasizes that the human body is a complex system that includes psychological, physiological, and spiritual dimensions. All of these can interact with external stressors. Applying of tertiary prevention using Neuman’s nursing model helps patients manage stressors and maintain a dynamic balance in their bodies. Neuman’s nursing model has been applied in mental disorders, antenatal care, and even cancer, but its effectiveness in perioperative nursing for patients with breast cancer remains underexplored [17-19]. This study aimed to evaluate the effectiveness of Neuman’s nursing model during the perioperative period for patients undergoing radical mastectomy, to establish and refine a nursing model that addresses both the physical and mental problems of patients undergoing breast cancer surgery.
Materials and methods
General materials
The clinical data of BC patients treated at Shanxi Bethune Hospital from January 2019 to December 2022 were retrospectively analyzed. The conventional management model was implemented from January 2019 to December 2020. Neuman’s nursing model was adopted from January 2021 to December 2022. The inclusion criteria: (1) women newly diagnosed of unilateral breast cancer [20], (2) patients with indications for modified radical mastectomy and underwent this surgery at our hospital, (3) aged between 18 and 70, and (4) patients with consciousness and capability to express their willingness accurately. The exclusion criteria: (1) recurrent breast tumors, (2) primary tumors of organs or metastasis of BC to organs, (3) severe chronic diseases such as heart failure or respiratory failure, and (4) coagulation disorders or abnormal hematopoietic system. This study was approved by the Ethics Committee of Shanxi Bethune Hospital. The BC patients included in the study numbered 50 (belonging to the conventional group) received conventional nursing and 50 (belonging to the study group) received care under Neuman’s nursing model.
Nursing methods
The conventional nursing model was utilized in the conventional group. The primary components consisted of health education, monitoring patients’ conditions, and preventing complications such as venous thrombosis, oozing of fluid or blood at the puncture site, and infection. During the preoperative phase, nursing efforts focused on patient education. This involved providing a detailed explanation of the procedure, anticipated effects, risks, and postoperative care. Psychological support was provided to alleviate the patient’s preoperative anxiety. A health assessment was conducted to evaluate the patient’s overall condition. Laboratory tests and nutritional assessments were completed. Pain management assessments, skin preparation, and instructions regarding preoperative fasting and water deprivation were provided. Intraoperative care centered around monitoring vital signs and managing patients’ pain, ensuring effective communication with the surgical team, and promptly addressing any issues that may arise during the operation. Postoperative care included regular assessment of pain levels, adjusting analgesic regimens, observing the healing of the surgical wound, changing dressings, preventing infection, and encouraging early mobilization to enhance blood circulation and lung function.
The study group adopted the Newman nursing model [21], and the specifics were as follows: (1) Primary prevention interventions: Initially, patients’ psychological state, physiological state, and social adaptability were assessed. The sources of stress were identified, and interventions were implemented to reduce the patients’ stress response and reinforce the flexible line of defense. Nursing staff focused on guiding patients in terms of diet and lifestyle, eliminating external influencing factors, and maintaining the dynamic balance of the system. They interacted with patients in various ways to eliminate or weaken negative psychological states such as tension, fear, anxiety, and depression. (2) Secondary prevention interventions: For patients with severe stress response, targeted measures were taken. Examples of successful treatment were introduced to relieve their tension, especially for patients with severe adverse emotions. Patients were encouraged to actively communicate with others and express their thoughts to identify and address new stressors promptly. (3) Tertiary prevention interventions: As patients showed signs of recovery, they were encouraged to communicate with friends and family to foster a sense of belonging. Examples of positive outcomes from modified radical mastectomy were provided to help patients visualize a hopeful future. Regular follow-ups were conducted to monitor changes in patients’ signs. Personalized health education was provided. Early functional exercises were implemented to maintain patients’ physical and mental well-being.
The implementation of the Newman nursing plan included three different nursing stages: preoperative, intraoperative, and postoperative. (1) In the preoperative stage of radical mastectomy, the application of the Newman care model focuses on assessing the patient’s understanding of the surgery, psychological state, and identifying stressors. Nurses communicated with patients to understand their cognitive level, concerns, and expectations for surgery. The physiological condition of the patient was evaluated, including pain levels, vital signs, and risk of complications. Based on the results of the assessment, a care plan was developed including providing detailed surgical information, conducting psychological support and education, and preparing the postoperative support system that the patient may need. (2) In the intraoperative stage, the Newman model emphasized maintaining the physiological stability of the patient and preventing stressors. Nurses closely monitored the vital signs of patients to ensure the safety of anesthesia and surgical procedures. Nurses prepared to respond to any emergencies such as bleeding, infection, or allergic reactions. The goal of intraoperative care is to reduce the patient’s physical and psychological stress response and lay a good foundation for postoperative recovery through effective pain management and best surgical nursing practice. (3) In the postoperative stage, the Neuman nursing model was applied to promote the rapid recovery and early mobilization of patients. Nurses assessed the patient’s pain control, wound healing, and stability of vital signs. Postoperative education was provided, including instructions on wound care, activity guidelines, and medication information. Patients were encouraged to engage in self-care activities, such as breathing exercises and early mobilization, under the guidance of nurses, to promote the recovery of lung function and physical abilities. Prior to discharge, it is important to ensure that the patient and their family understand the significance of postoperative care and that necessary community resources and follow-up plans are available to support the patient’s continued recovery at home.
Observation indicators
(1) The psychological and physiological stresses were assessed and compared between two groups of patients in the perioperative period. Psychological stress was assessed using the Self-Rating Anxiety Scale (SAS) and the Self-Rating Depression Scale (SDS) [22,23]. The maximum score for SAS and SDS was 80 points. The higher the score, the higher the level of anxiety and depression. A total SAS and SDS scores of less than 50 and 53 points respectively indicates normal state. The Cronbach’s alpha of SAS and SDS were 0.83 and 0.73, respectively. Physiological stress was assessed by IL-6 and CRP, indicators that reflect inflammation and immune response, respectively. The higher the index value, the greater the surgical stress. Systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR) were used as supplementary indicators of physiological stress. (2) Disease indicators were compared between the two groups of patients: serum carbohydrate antigen 153 (Carbohydrate antigen153, CA153) and carcinoembryonic antigen (Carcinoma embryonic antigen, CEA). (3) The quality of life of patients was assessed using the SF-36 [24]. Screening included 8 scales (physical functioning, role physical, body pain, general health, vitality, social functioning, role emotional, and mental health) with a total of 36 items. The score of SF-36 ranges from 0 to 100. The higher the score, the better the quality of life. The Cronbach’s alpha of SF-36 was 0.92. (4) Postoperative complications in patients were recorded, mainly including subcutaneous effusion, flap necrosis, and incision dehiscence. (5) The nursing quality was assessed using a questionnaire designed by our hospital. These included 4 items: nursing operations, nursing attitude, completion of nursing work, and patient’s cooperation with nursing staff. The score of each item ranged from 0 to 25 points. The higher the score, the higher the nursing quality. (6) Newcastle Satisfaction with Nursing Scales (NSNS) was used to assess patient’s satisfaction with nursing [25]. There were 19 items included. The score of each item ranged from 1 (very dissatisfied) to 5 (very satisfied) with a maximum score of 95. A total score of over 85 indicated “very satisfied”, 80 to 85 indicated “satisfied”, 70 to 79 indicates “neutral”, and of less than 69 indicates “dissatisfied”. The Cronbach’s alpha of NSNS is 0.86.
Statistical analysis
All data from this study were analyzed using SPSS 25 and GraphPad 8.3. Quantitative data with a normal distribution were expressed as (x̅±s). The t-test was used to determine differences between groups. Categorical data were expressed as n (%) and analyzed using χ2 test. Ranked data were compared using the rank sum test. P < 0.05 indicated a significant difference.
Results
Comparison of general data between the two groups of patients
The general data of BC patients under different nursing models are presented in Table 1, and the two groups were comparable in terms of age, BMI, pathology, underlying disease, marital status, and education level (all P > 0.05).
Table 1.
General data of patients in two groups
| Conventional group (n=50) | Study group (n=50) | t/χ2 | P | |
|---|---|---|---|---|
| Age (years old) | 52.16±7.46 | 51.37±7.16 | 0.540 | 0.590 |
| BMI (kg/m2) | 25.13±0.75 | 24.97±0.81 | 1.025 | 0.308 |
| Pathology | 0.925 | 0.630 | ||
| Invasive ductal carcinoma | 35 (70.00) | 33 (66.00) | ||
| Papillary carcinoma | 11 (22.00) | 10 (20.00) | ||
| Others | 4 (8.00) | 7 (14.00) | ||
| Diabetes or hypertension | 0.219 | 0.640 | ||
| Yes | 13 (26.00) | 11 (22.00) | ||
| No | 37 (74.00) | 39 (78.00) | ||
| Marital status | 0.832 | 0.494 | ||
| Married | 39 (78.00) | 35 (70.00) | ||
| Single | 11 (22.00) | 15 (30.00) | ||
| Education level | 1.028 | 0.598 | ||
| Primary school and below | 12 (24.00) | 14 (28.00) | ||
| Middle or high school | 26 (52.00) | 28 (56.00) | ||
| College degree or above | 12 (24.00) | 8 (16.00) |
Note: BMI: Body Mass Index.
Comparison of psychological stress of perioperative patients
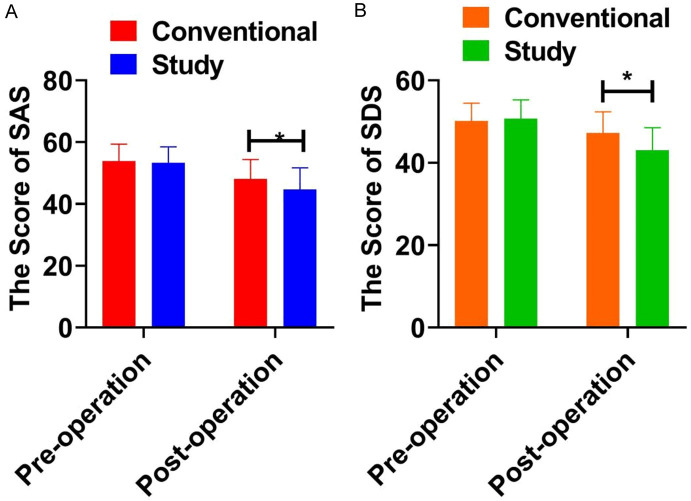
When comparing the psychological stress of perioperative patients in the two groups, it was found that before the operation, patients in both groups did not significantly differ in their SAS and SDS scores (all P > 0.05). After the surgery, there was a significant difference in SAS and SDS scores between the two groups of patients. Patients in the study group experienced a greater decrease in SAS and SDS scores compared with those in the conventional group (all P < 0.05), as shown in Table 2 and Figure 1.
Table 2.
Psychological stress of perioperative patients
| Indicators | Time | Conventional group (n=50) | Study group (n=50) | t | P |
|---|---|---|---|---|---|
| SAS | Pre-operation | 53.87±5.49 | 53.32±5.18 | 0.515 | 0.608 |
| Post-operation | 48.09±6.28 | 44.73±6.97 | 2.532 | 0.129 | |
| t | 4.900 | 6.994 | |||
| P | < 0.001 | < 0.001 | |||
| SDS | Pre-operation | 50.31±4.35 | 50.74±4.51 | 0.688 | 0.493 |
| Post-operation | 47.20±5.16 | 43.09±5.42 | 3.844 | < 0.001 | |
| t | 3.070 | 7.672 | |||
| P | 0.003 | < 0.001 |
Note: SAS: Self-Rating Anxiety Scale, SDS: Self-Rating Depression Scale.
Figure 1.
Psychological stress of perioperative patients. A. The score of SAS; B. The score of SDS. Note: SAS: Self-Rating Anxiety Scale, SDS: Self-Rating Depression Scale. * indicates P < 0.05.
Comparison of physiological stress of perioperative patients
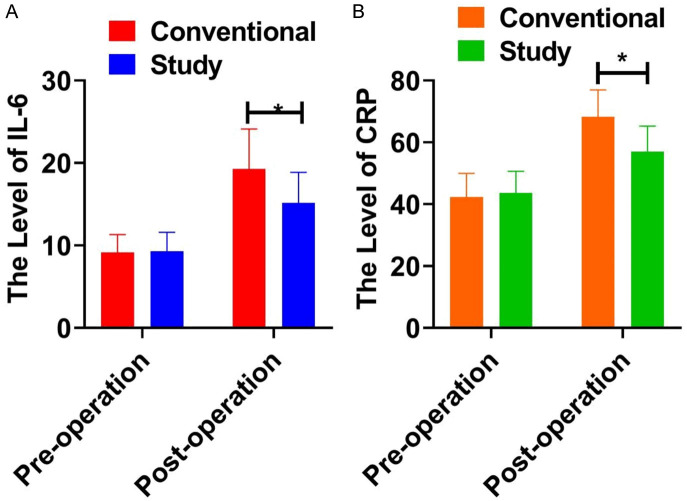
When comparing the physiological stress between perioperative patients in the two groups, it was found that there was no significant difference in the IL-6 level and CRP level between the two groups before the operation (P > 0.05). After the operation, the IL-6 level, and CRP level of the patients in both groups increased significantly. The study group patients exhibited a smaller increase in IL-6 level and CRP level (P < 0.05). No statistical differences were observed in SBP, DBP, and HR levels between two groups before and after treatment (all P > 0.05), as shown in Table 3 and Figure 2.
Table 3.
Physiological stress of perioperative patients
| Indicators | Time | Conventional group (n=50) | Study group (n=50) | t | P |
|---|---|---|---|---|---|
| IL-6 (pg/L) | Pre-operation | 9.16±2.14 | 9.31±2.27 | 0.340 | 0.735 |
| Post-operation | 19.26±4.86 | 15.16±3.71 | 4.742 | < 0.001 | |
| t | 12.450 | 9.511 | |||
| P | < 0.001 | < 0.001 | |||
| CRP (pg/L) | Pre-operation | 42.37±7.59 | 43.61±7.04 | 0.847 | 0.399 |
| Post-operation | 68.29±8.66 | 57.01±8.19 | 6.692 | < 0.001 | |
| t | 15.920 | 8.773 | |||
| P | < 0.001 | < 0.001 | |||
| SPB (mmHg) | Pre-operation | 109.41±7.62 | 108.72±8.56 | 0.426 | 0.671 |
| Post-operation | 110.34±9.13 | 111.08±8.91 | 0.410 | 0.682 | |
| t | 0.553 | 1.351 | |||
| P | 0.582 | 0.180 | |||
| DBP (mmHg) | Pre-operation | 71.29±6.21 | 72.41±7.09 | 0.994 | 0.322 |
| Post-operation | 70.52±5.81 | 71.49±6.83 | 0.765 | 0.446 | |
| t | 0.688 | 0.712 | |||
| P | 0.493 | 0.478 | |||
| HR (bpm) | Pre-operation | 82.37±10.80 | 81.40±8.96 | 0.489 | 0.626 |
| Post-operation | 81.49±9.07 | 80.82±9.45 | 0.362 | 0.718 | |
| t | 0.441 | 0.315 | |||
| P | 0.660 | 0.753 |
Note: IL-6: Interleukin-6, CRP: C-reactive protein, SBP: systolic blood pressure, DBP: diastolic blood pressure, HR: heart rate.
Figure 2.
Physiological stress of perioperative patients. A. The level of IL-6; B. The level of CRP. Note: IL-6: Interleukin-6, CRP: C-reactive protein. * indicates P < 0.05.
Comparison of disease-specific indexes between the two groups
There was no significant difference in the levels of CA153 and CEA between the two groups before surgery (all P > 0.05). After surgery, the levels of CA153 and CEA in the two groups were significantly lower than those before surgery (all P < 0.05). There was no significant difference between the two groups (all P > 0.05), as shown in Table 4.
Table 4.
Comparison of disease-specific indexes between the two groups
| Grouping | CA153 (U/mL) | CEA (ng/mL) | ||
|---|---|---|---|---|
|
|
|
|||
| Pre-operation | Post-operation | Pre-operation | Post-operation | |
| Conventional group (n=50) | 27.25±4.28 | 23.18±4.04* | 6.41±1.96 | 5.29±1.54* |
| Study group (n=50) | 26.91±4.85 | 23.73±3.67* | 6.83±1.84 | 5.11±1.37* |
| t | 0.372 | 0.713 | 1.105 | 0.618 |
| P | 0.711 | 0.478 | 0.272 | 0.538 |
Note: CA153: Carbohrdyate antigen 153, CEA: Carcinoma embryonic antigen.
Compared with pre-operation;
P < 0.05.
Comparison of perioperative life quality between two groups of patients
Before the surgery, there was no significant difference in the quality of life between the two groups of patients (P > 0.05). After the surgery, both groups of patients reported a significant improvement in quality of life. Patients in the study group exhibited significantly higher scores than the patients in the conventional group (P < 0.05), as shown in Table 5.
Table 5.
Comparison of life quality before and after operation
| Grouping | Before operation | After operation | t | P |
|---|---|---|---|---|
| Conventional group (n=50) | 42.15±6.71 | 45.09±5.24 | 2.442 | 0.016 |
| Study group (n=50) | 42.84±6.29 | 49.32±5.08 | 5.667 | < 0.001 |
| t | 0.531 | 4.098 | ||
| P | 0.570 | < 0.001 |
Comparison of complications between two groups
Postoperative complications, including subcutaneous effusion, flap necrosis, and incision dehiscence, were more common in the conventional group compared to the study group. A significant difference in the total incidence of complications between the two groups (P < 0.05), as shown in Table 6.
Table 6.
Complications after operation
| Grouping | Subcutaneous effusion | Flap necrosis | Incision dehiscence | Total incidence |
|---|---|---|---|---|
| Conventional group (n=50) | 7 (14.00) | 3 (6.00) | 3 (6.00) | 13 (26.00) |
| Study group (n=50) | 3 (6.00) | 1 (2.00) | 1 (2.00) | 5 (10.00) |
| χ2 | 4.336 | |||
| P | 0.037 |
Assessment of nursing quality during the perioperative period
When comparing the nursing quality between the two groups, it was found that nursing staff under Neuman’s nursing model scored significantly higher than those under a conventional nursing model in nursing operations, nursing attitude, completion of nursing work, and patient cooperation with nursing staff (all P < 0.05), as displayed in Table 7.
Table 7.
Assessment of nursing quality during the perioperative period
| Grouping | Nursing operations | Nursing attitude | Completion of nursing work | Patient’s cooperation with nursing staff |
|---|---|---|---|---|
| Conventional group (n=50) | 20.11±1.45 | 19.22±2.01 | 18.25±3.15 | 18.11±2.15 |
| Study group (n=50) | 21.09±1.52 | 20.76±1.96 | 19.74±2.98 | 20.94±1.85 |
| t | 3.299 | 3.879 | 2.430 | 7.055 |
| P | 0.001 | < 0.001 | 0.017 | < 0.001 |
Patient’s satisfaction with nursing during the perioperative period
The study group reported higher levels of satisfaction (satisfied and very satisfied) compared to the conventional group. The rank sum test indicated a significant difference in patient satisfaction levels between the groups (Z=-2.036, P=0.042), as displayed in Table 8.
Table 8.
Patient’s satisfaction with nursing during the perioperative period
| Grouping | Very satisfied | Satisfied | Neutral | Dissatisfied |
|---|---|---|---|---|
| Conventional group (n=50) | 13 (26.00) | 14 (28.00) | 17 (34.00) | 6 (12.00) |
| Study group (n=50) | 19 (38.00) | 18 (36.00) | 11 (22.00) | 2 (4.00) |
| Z | -2.036 | |||
| P | 0.042 | |||
Discussion
Patients experience a variety of physiological dysfunctions and mental health challenges during the perioperative period. Improving the quality of nursing care for breast cancer patients during this critical period significantly improves treatment effectiveness and quality of life. Founded by Neuman, an American nursing scientist, the Neuman’s nursing model conceptualizes patient’s body as a holistic system [26]. When stressors overcome the body’s defense system, the body may deploy various responses to maintain balance and coordination between the internal and external environments. Providing appropriate nursing interventions at different stages when stressors break through the body’s defense system helps patients maintain stability in their internal and external environment. Neuman’s nursing theory advocates for tertiary prevention, focusing on improving the patient’s physiological and psychological state during the postoperative stage to enhance the patient’s prognosis.
For patients, the diagnosis of BC and its surgical treatment represent a sudden and profound crisis. Due to the location of the tumor, patients experience pronounced emotional disturbances. These are stress responses that are difficult to avoid [27]. Psychological stresses during the perioperative period include feelings of worry, tension, anxiety, and fear. These constitute a complex process of psychological change. The mental state of BC patients varies at different stages of the perioperative period, with different causes. Before the operation, patients and their families are concerned about the life-threatening nature of the tumor and the risk of surgical complications, leading to anxiety and negative emotions. These emotions persist even after the operation. The surgical process has both positive and negative effects on the psychological problems of BC patients. Surgery removes the abnormal mass caused by the tumor, saving the patient’s life and alleviating some anxiety. Surgical treatment can trigger new anxiety due to the pain and discomfort caused by the incision, and concerns about the outcome of the operation [28]. Patients who undergo modified radical mastectomy may worry about their appearance and how they are perceived by their families, particularly their spouses. This introduces new stressors. Patients experience significant psychological stress in response to these stressors, in turn leads to immune dysfunction and affects their recovery and quality of life. It is crucial to pay sufficient attention to the psychological stress experienced by BC patients.
This study found that BC patients in the study group experienced a certain degree of psychological stress, the degree was significantly lower than that of patients in the conventional group. It can be observed that with the assistance of tertiary prevention interventions based on Neuman’s nursing model, the negative emotions of patients were alleviated at various stages of the perioperative period, contributing to an enhanced patients’ quality of life. The reason for this improvement is rooted in primary prevention intervention that strengthens patients’ defense mechanisms, enabling them to respond better to stress and relieving it to some extent. Secondary prevention intervention ensures emotional stability by utilizing internal or external factors to enhance resistance and reduce physical response. Tertiary prevention intervention reinforces the effects of secondary prevention intervention. Through active communication and discussion about the value of life, patients are more likely to foster a stronger sense of identity and satisfaction, effectively reducing tension and anxiety and ultimately improving their quality of life. In this study, after surgical treatment, the disease-specific indicators CA153 and CEA levels significantly decreased in both groups of patients, but there was no significant difference between the two groups. This suggested that the decrease in CA153 and CEA levels is related to surgery and has not been influenced by nursing methods.
This study found that Newman nursing can decrease the levels of IL-6 and CRP to some extent, alleviating the physiological stress state of patients. IL-6 and CRP are two biomarkers that play crucial roles in inflammation and immune response. They are closely linked to the physiological stress state of patients [29]. In breast cancer patients, surgical trauma triggers an inflammatory response in the body, resulting in elevated IL-6 and CRP levels, indicating increased physiological stress in patients [30]. IL-6 is a multifunctional cytokine that is involved in regulating immunity and acute phase responses. During inflammation, the release of IL-6 can stimulate hepatocytes to produce CRP, an acute phase response protein. Elevated levels of CRP are commonly associated with inflammation, tissue damage, and infection. After surgery, increased IL-6 and CRP levels are associated with the body’s inflammatory response and healing processes. High levels of IL-6 and CRP are linked to poor prognosis and an increased risk of complications [31]. The Newman nursing model addresses the physical and psychological stress experienced by patients by comprehensively assessing their needs and providing personalized nursing interventions. This includes pain management, psychological support, nutritional support, and early mobilization. These interventions may have a regulatory effect on the inflammatory response. By reducing IL-6 and CRP levels after surgery, the Newman nursing model may help alleviate the inflammatory burden on patients, improve their physiological stress, and promote postoperative recovery. Maintaining low levels of IL-6 and CRP may help reduce the risk of postoperative complications, such as infection, cardiovascular events, and pulmonary complications [32-34]. The research results of Wang et al. [33] showed that the IL-6 level of patients in the postoperative infection group of breast cancer was significantly increased. Mikkelsen et al. [34] showed in their study that serum CRP was related to the prognosis of patients with metastatic breast cancer. This improved the physiological stress state of patients (reducing the levels of IL-6 and CRP). Through the Neuman care model it can promote postoperative recovery and have a positive impact on the long-term health outcomes of patients.
Nursing quality and patient satisfaction are important indicators for evaluating nursing work. These indicators ensure smooth medical work and help improve patients’ compliance. Mervis JS et al. [35] agreed that patients’ satisfaction with nursing could reflect the quality of medical services. Fremmelevholm A et al. [36] have mentioned that patients’ satisfaction with individualized nursing can affect their quality of life. This study has shown that compared to the conventional nursing model, Neuman’s nursing model resulted in higher nursing quality. Patients who received care under Neuman’s nursing model during the perioperative period expressed greater satisfaction with the nursing services. This study believes that Neuman’s nursing model can improve the psychological and physiological state of BC patients during the perioperative period and enhance their satisfaction with nursing work and increase their compliance.
This study demonstrated that the Neuman nursing model can significantly improve the psychological and physical conditions of breast cancer patients, promoting their recovery. This study presents certain limitations. These include a small sample size and the fact that all samples were derived from the same center, may limit the generalizability of the findings. This was a retrospective analysis. The study was restricted to existing data. The use of a self-developed nursing quality questionnaire might lack broader validation, affecting the study’s authority. Future research should aim to conduct multicenter, large-sample, prospective studies, and employ widely recognized standardized questionnaires to enhance the reliability and applicability of the findings. Such studies would provide more scientifically robust guidance for optimizing nursing care for breast cancer patients in the perioperative period.
Conclusions
The importance of nursing in the rehabilitation of BC patients during the perioperative period includes, identifying an effective nursing model that promotes both psychological and physiological well-being is essential. This study compared the effects of different nursing modes on breast cancer patients and found that Neuman’s nursing mode can significantly alleviate patients’ psychological and physiological stress, leading to a reduction in complications and an improvement in quality of life. The study revealed that the application of Neuman’s nursing model resulted in a significant improvement in nursing quality and patients’ satisfaction with nursing care. It is believed that by implementing Neuman’s nursing model during the perioperative period for breast cancer, patients will enhance their health and foster a more harmonious doctor-patient relationship by increasing patients’ satisfaction with nursing care.
Disclosure of conflict of interest
None.
References
- 1.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Zhang W, Zhang BL, He JJ, Fan JH, Li J, Zhang B, Yang HJ, Xie XM, Tang ZH, Li H, Li JY, Wang SL, Qiao YL, Huang R, Zhang P. Clinicopathological characteristics and treatment of young women with breast cancer in China: a nationwide multicenter 10-year retrospective study. Gland Surg. 2021;10:175–185. doi: 10.21037/gs-20-574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jonczyk MM, Jean J, Graham R, Chatterjee A. Surgical trends in breast cancer: a rise in novel operative treatment options over a 12 year analysis. Breast Cancer Res Treat. 2019;173:267–274. doi: 10.1007/s10549-018-5018-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tripathy D, Im SA, Colleoni M, Franke F, Bardia A, Harbeck N, Hurvitz SA, Chow L, Sohn J, Lee KS, Campos-Gomez S, Villanueva Vazquez R, Jung KH, Babu KG, Wheatley-Price P, De Laurentiis M, Im YH, Kuemmel S, El-Saghir N, Liu MC, Carlson G, Hughes G, Diaz-Padilla I, Germa C, Hirawat S, Lu YS. Ribociclib plus endocrine therapy for premenopausal women with hormone-receptor-positive, advanced breast cancer (MONALEESA-7): a randomised phase 3 trial. Lancet Oncol. 2018;19:904–915. doi: 10.1016/S1470-2045(18)30292-4. [DOI] [PubMed] [Google Scholar]
- 5.Iwamoto T, Kajiwara Y, Zhu Y, Iha S. Biomarkers of neoadjuvant/adjuvant chemotherapy for breast cancer. Chin Clin Oncol. 2020;9:27. doi: 10.21037/cco.2020.01.06. [DOI] [PubMed] [Google Scholar]
- 6.Lev S. Targeted therapy and drug resistance in triple-negative breast cancer: the EGFR axis. Biochem Soc Trans. 2020;48:657–665. doi: 10.1042/BST20191055. [DOI] [PubMed] [Google Scholar]
- 7.Shah C, Bauer-Nilsen K, McNulty RH, Vicini F. Novel radiation therapy approaches for breast cancer treatment. Semin Oncol. 2020;47:209–216. doi: 10.1053/j.seminoncol.2020.05.003. [DOI] [PubMed] [Google Scholar]
- 8.Du H, Liu X, Li F, Xue Z, Li Y, Qian B. Anesthetic effect of ultrasound-guided multiple-nerve blockade in modified radical mastectomy in patients with breast cancer. Medicine (Baltimore) 2021;100:e24786. doi: 10.1097/MD.0000000000024786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grujic D, Giurgi-Oncu C, Oprean C, Crainiceanu Z, Secosan I, Rivis I, Papava I, Vernic C, Bredicean C. Well-being, depression, and anxiety following oncoplastic breast conserving surgery versus modified radical mastectomy followed by late breast reconstruction. Int J Environ Res Public Health. 2021;18:9320. doi: 10.3390/ijerph18179320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang J, Huang L, Wu F, Wang G, Wu L, Huang B, Lin Y, Li D, Ma C. Tailoring PTV expansion to improve the dosimetry of post modified radical mastectomy intensity-modulated radiotherapy for left-sided breast cancer patients by using 4D CT combined with cone beam CT. J Appl Clin Med Phys. 2021;22:139–146. doi: 10.1002/acm2.13244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu YF, Liu JE, Zhu Y, Mak YW, Qiu H, Liu LH, Yang SS, Chen SH. Development and validation of a nomogram to predict the risk of breast cancer-related lymphedema among Chinese breast cancer survivors. Support Care Cancer. 2021;29:5435–5445. doi: 10.1007/s00520-021-06122-y. [DOI] [PubMed] [Google Scholar]
- 12.Zhang Y, Li N, Chen J, Luo X, Li M, Yan J. Breast cancer-related lymphedema risk-management behaviors among chinese breast cancer survivors and relationships with socio-demographic and clinical characteristics: a longitudinal study. Patient Prefer Adherence. 2022;16:797–808. doi: 10.2147/PPA.S356750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.de la Borbolla Martinez GD, Martinez MEH, Raygoza NP. Nursing intervention in women who developed lymphedema after undergoing a modified radical mastectomy: a pre-experimental study. Ecancermedicalscience. 2018;12:827. doi: 10.3332/ecancer.2018.827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moorthy A, Lowry D, Edgley C, Casey MB, Buggy D. Effect of perioperative cognitive behavioural therapy on chronic post-surgical pain among breast cancer patients with high pain catastrophising characteristics: protocol for a double-blinded randomised controlled trial. Trials. 2022;23:66. doi: 10.1186/s13063-022-06019-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shorofi SA, Nozari-Mirarkolaei F, Arbon P, Bagheri-Nesamie M. Depression and sleep quality among Iranian women with breast cancer. Asian Pac J Cancer Prev. 2021;22:3433–3440. doi: 10.31557/APJCP.2021.22.11.3433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li Z, Geng W, Yin J, Zhang J. Effect of one comprehensive education course to lower anxiety and depression among Chinese breast cancer patients during the postoperative radiotherapy period - one randomized clinical trial. Radiat Oncol. 2018;13:111. doi: 10.1186/s13014-018-1054-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Van der Draai DA, Van Duijn E, De Beurs DP, Bexkens A, Beekman ATF. Factors of specialized mental health care use in the Netherlands: a scoping review applying Andersen-Newman’s care utilization model. Health Serv Insights. 2021;14:11786329211048134. doi: 10.1177/11786329211048134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tesfaye G, Chojenta C, Smith R, Loxton D. Application of the Andersen-Newman model of health care utilization to understand antenatal care use in Kersa district, Eastern Ethiopia. PLoS One. 2018;13:e0208729. doi: 10.1371/journal.pone.0208729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Imaizumi S, Honda A, Fujiwara Y, Iio Y. Caring partnership within Newman’s theory of health as expanding consciousness: aiming for patients to find meaning in their treatment experiences. Asia Pac J Oncol Nurs. 2021;8:725–731. doi: 10.4103/apjon.apjon-2147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cardoso F, Kyriakides S, Ohno S, Penault-Llorca F, Poortmans P, Rubio IT, Zackrisson S, Senkus E ESMO Guidelines Committee. Electronic address: clinicalguidelines@esmo.org. Early breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up†. Ann Oncol. 2019;30:1194–1220. doi: 10.1093/annonc/mdz173. [DOI] [PubMed] [Google Scholar]
- 21.Endo E. Margaret Newman’s theory of health as expanding consciousness and a nursing intervention from a unitary perspective. Asia Pac J Oncol Nurs. 2017;4:50–52. doi: 10.4103/2347-5625.199076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dunstan DA, Scott N. Norms for Zung’s self-rating anxiety scale. BMC Psychiatry. 2020;20:90. doi: 10.1186/s12888-019-2427-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chagas MH, Tumas V, Loureiro SR, Hallak JE, Trzesniak C, de Sousa JP, Rodrigues GG, Santos Filho A, Crippa JA. Validity of a Brazilian version of the Zung self-rating depression scale for screening of depression in patients with Parkinson’s disease. Parkinsonism Relat Disord. 2010;16:42–5. doi: 10.1016/j.parkreldis.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 24.Abbasi-Ghahramanloo A, Soltani-Kermanshahi M, Mansori K, Khazaei-Pool M, Sohrabi M, Baradaran HR, Talebloo Z, Gholami A. Comparison of SF-36 and WHOQoL-BREF in measuring quality of life in patients with type 2 diabetes. Int J Gen Med. 2020;13:497–506. doi: 10.2147/IJGM.S258953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rodriguez-Herrera C, Lopez-Jimenez JJ, Del Toro-Valero A, Torres-Carrillo NM, Torres-Carrillo N, Godinez-Pena CA, Mendez-Magana AC, Herrera-Godina MG, Fletes-Rayas AL. The Newcastle satisfaction with nursing scales in a Mexican oncology hospital. Afr Health Sci. 2021;21:60–66. doi: 10.4314/ahs.v21i1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mitsugi M, Endo E, Ikeda M. Recognizing one’s own care pattern in cancer nursing and transforming toward a unitary nursing practice based on margaret Newman’s theory. Asia Pac J Oncol Nurs. 2020;7:225–228. doi: 10.4103/apjon.apjon_1_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosenberg SM, Dominici LS, Gelber S, Poorvu PD, Ruddy KJ, Wong JS, Tamimi RM, Schapira L, Come S, Peppercorn JM, Borges VF, Partridge AH. Association of breast cancer surgery with quality of life and psychosocial well-being in young breast cancer survivors. JAMA Surg. 2020;155:1035–1042. doi: 10.1001/jamasurg.2020.3325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Al-Hilli Z, Wilkerson A. Breast surgery: management of postoperative complications following operations for breast cancer. Surg Clin North Am. 2021;101:845–863. doi: 10.1016/j.suc.2021.06.014. [DOI] [PubMed] [Google Scholar]
- 29.Lever-van Milligen BA, Lamers F, Smit JH, Penninx BWJH. Physiological stress markers, mental health and objective physical function. J Psychosom Res. 2020;133:109996. doi: 10.1016/j.jpsychores.2020.109996. [DOI] [PubMed] [Google Scholar]
- 30.Cui Y, Cui S, Lu W, Wang Y, Zhuo Z, Wang R, Zhang D, Wu X, Chang L, Zuo X, Zhang W, Mei H, Zhang M. CRP, IL-1alpha, IL-1beta, and IL-6 levels and the risk of breast cancer: a two-sample Mendelian randomization study. Sci Rep. 2024;14:1982. doi: 10.1038/s41598-024-52080-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shimura T, Shibata M, Gonda K, Murakami Y, Noda M, Tachibana K, Abe N, Ohtake T. Prognostic impact of interleukin-6 and C-reactive protein on patients with breast cancer. Oncol Lett. 2019;17:5139–5146. doi: 10.3892/ol.2019.10183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang AY, Ganocy SJ, Owusu C, Gao K. Associations among irritability, high-sensitivity C-reactive protein/interleukin-6, and depression in patients with early-stage breast cancer undergoing chemotherapy: a prospective study. J Acad Consult Liaison Psychiatry. 2022;63:260–267. doi: 10.1016/j.jaclp.2021.08.012. [DOI] [PubMed] [Google Scholar]
- 33.Wang C, Han W, Gu Y. Changes in the levels of T lymphocytes and inflammatory factors in the peripheral blood of breast cancer patients during postoperative chemotherapy. Gland Surg. 2020;9:2155–2161. doi: 10.21037/gs-20-818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mikkelsen MK, Lindblom NAF, Dyhl-Polk A, Juhl CB, Johansen JS, Nielsen D. Systematic review and meta-analysis of C-reactive protein as a biomarker in breast cancer. Crit Rev Clin Lab Sci. 2022;59:480–500. doi: 10.1080/10408363.2022.2050886. [DOI] [PubMed] [Google Scholar]
- 35.Mervis JS, Phillips TJ. Pressure ulcers: prevention and management. J Am Acad Dermatol. 2019;81:893–902. doi: 10.1016/j.jaad.2018.12.068. [DOI] [PubMed] [Google Scholar]
- 36.Fremmelevholm A, Soegaard K. Pressure ulcer prevention in hospitals: a successful nurse-led clinical quality improvement intervention. Br J Nurs. 2019;28:S6–S11. doi: 10.12968/bjon.2019.28.6.S6. [DOI] [PubMed] [Google Scholar]