Abstract
Objective: To investigate the association between postoperative cognitive dysfunction (POCD) and anemia in elderly patients with gastrointestinal tumors. Methods: A retrospective analysis was conducted on 184 elderly patients treated at Yanchang County People’s Hospital from May 2019 to March 2022. The patients were divided into a normal hemoglobin group (n=109) and an anemia group (n=75) based on their preoperative hemoglobin levels. Cognitive function was assessed using MMSE and MoCA scales at preoperative day 1 and postoperative day 1, 3, and 7. Levels of S100β, TNF-α, and IL-6 were measured. Intraoperative data were recorded. POCD incidence was evaluated at 3 and 7 days postoperatively. Pearson correlation and ROC curve analyses were conducted, and logistic regression was conducted to identify risk factors for POCD. Results: The anemia group had significantly lower postoperative MMSE and MoCA scores and higher levels of inflammatory factors (all P<0.05) compared to the normal hemoglobin group. No significant differences in intraoperative data were observed between the groups (P>0.05). POCD incidence on postoperative day 3 and 7 was higher in the anemia group (38.66% and 30.67%) compared to that in the normal group (11.01% and 7.34%) (P<0.05). AUCs for hemoglobin levels in predicting POCD on postoperative day 3 and 7 were 0.858 and 0.865. Independent risk factors for POCD included age >70 years, education ≤6 years, and anemia. Conclusions: Anemia is associated with lower cognitive function scores, higher POCD incidence, and increased inflammatory factors in elderly gastrointestinal tumor patients after operation.
Keywords: Elderly, gastrointestinal tumors, postoperative, cognitive dysfunction, anemia
Introduction
Postoperative cognitive dysfunction (POCD) is a common neurological complication primarily characterized with memory loss, inability to concentrate, decreased language comprehension, and even personality changes [1]. POCD can lead to prolonged recovery periods, increased hospital stays, higher mortality rates, and increased medical costs [2]. A study by Monk et al. [3] pointed out that POCD almost doubled the mortality rate in patients within three months after surgery, emphasizing the importance of early identification and intervention of POCD.
Previous research identified various factors that may affect cognitive function, including surgical time, anesthesia, age, and alcohol abuse [4,5]. With the aging population, the susceptibility of elderly individuals and those living alone to POCD has increased, bringing significant pressure to society and families [6]. Therefore, in-depth research into the etiology and mechanisms of POCD, especially preoperative risk factors and their potential mechanisms, is crucial for the prevention and treatment of POCD.
Cancer patients often experience a decline in iron nutrition status, leading to tumor-related anemia, which may negatively impact the effectiveness of cancer treatment and patient survival [7]. Tumor-related anemia mainly includes anemia secondary to cancer, post-chemotherapy anemia, and anemia caused by chronic kidney disease related to cancer [8]. A study by Wang et al. [9] found that more than half of the patients with stage III-IV lung cancer had anemia.
Anemia has been proven to be associated with various adverse cerebrovascular events, postoperative pulmonary complications, in-hospital mortality, delirium, and other complications [10]. Stauder et al. [11] emphasized that even mild anemia could significantly affect the physical and cognitive abilities and quality of life of elderly patients. However, the relationship between anemia and cognitive function remains controversial. A study by Myint et al. [12] found no significant association between anemia and cognitive outcomes in elderly patients undergoing acute surgery. Patients with malignant gastrointestinal tumors often present with preoperative anemia, but its impact on postoperative cognitive function is not yet clear.
In this study, we retrospectively investigated the association between postoperative cognitive function and anemia in elderly patients with gastrointestinal tumors.
Information and methodology
Study subjects
With approval from the Ethics Committee of Yanchang County People’s Hospital, this study retrospectively collected the clinical data from patient’s medical records. A total of 184 elderly patients with gastrointestinal tumors who underwent laparoscopic surgery from May 2019 to March 2022 in Yanchang County People’s Hospital were included.
Inclusion criteria: Aged between 60 to 85 years; Diagnosis of gastrointestinal malignancies confirmed by pathological findings; Surgical treatment of gastrointestinal malignant tumors with laparoscopy at our institution; Complete medical records available.
Exclusion criteria: Previous history of epilepsy, Parkinson’s history, depression, schizophrenia, etc.; Incomplete evaluation due to severe dementia, coma, or concomitant illnesses; Use of medications that affect the central nervous system; Alcohol abuse or substance addiction; Hearing or vision impairments; Involvement in other surgeries or a secondary surgery; and pre-operative impairment of cognitive functioning as determined by MMSE (Modified Mental State Examination) Scale; Life expectancy of less than 3 months.
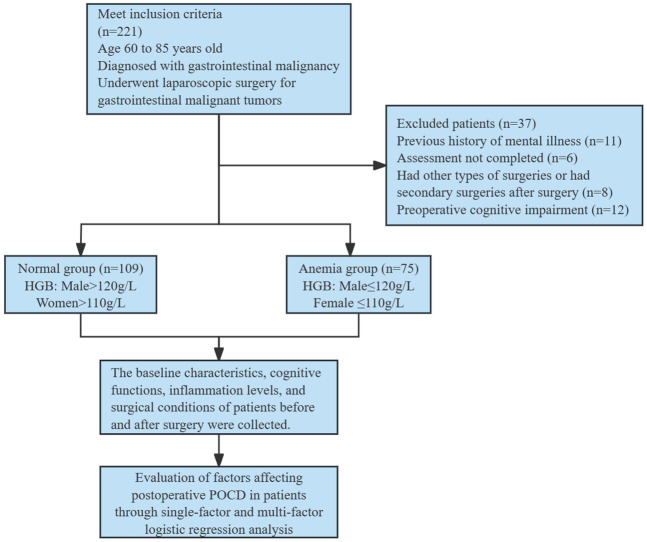
Patients were divided into 2 groups according to their preoperative hemoglobin (HGB) concentration: the normal hemoglobin group (HGB: men >120 g/L, women >110 g/L, n=109), and the anemia group (HGB: men ≤120 g/L, women ≤110 g/L, n=75). The case selection flow chart is shown in Figure 1.
Figure 1.
Flowchart for patient enrollment. HGB: hemoglobin; POCD: postoperative cognitive dysfunction.
Surgical method
After anesthesia, the patient was positioned in the lithotomy position for surgery. Carbon dioxide pneumoperitoneum was established at the umbilicus, and the operation was performed using the three-hole or four-hole method. A laparoscope was inserted into the abdominal cavity to locate the lesion. The tumor lesion was carefully separated and removed, the lymph node tissue was cleared. A 5 cm auxiliary incision was made at the exterior of the lesion site for specimen removal. After tumor extraction, routine anastomosis was performed. Finally, the abdominal cavity was flushed and sutured [13].
Data collection
Baseline characteristics, MMSE scores, Montreal Cognitive Assessment (MOCA) scores, levels of S100 Calcium-binding Protein β (s-100β), tumor Necrosis Factor α (TNF-α) and interleukin-6 (IL-6), and surgical details of the patients were extracted from electronic medical records.
The MMSE scale consists of six domains: orientation, immediate memory, attention and calculation, delayed memory, language, and visuospatial skills, with a total score of 30 points. A preoperative MMSE score of ≤23 points indicates preoperative cognitive dysfunction [14]. It’s worth noting that the assessment should be completed within 10 minutes.
The MOCA scale, another tool for assessing cognitive function, consists of nine domains: executive functioning, memory, language, orientation, numeracy, abstraction, visual perception, naming, and attention, also with a total score of 30; and a lower score indicates worse cognitive performance [15].
Outcome measurements
Primary outcomes: (1) MMSE score and MoCA score were assessed in both groups at preoperative day 1 and postoperative day 1, 3, and 7. (2) The degree of anemia was evaluated according to HGB level, and the relationship between postoperative cognitive function and anemia was analyzed using Pearson correlation. (3) The incidence of POCD was compared between the two groups at 3 days and 7 days after surgery.
Secondary outcomes: (1) The inflammatory indicators S-100β, TNF-α and IL-6 were detected in both groups at preoperative day 1 and postoperative day 1, 3, and 7. (2) The surgical conditions in the two groups were compared, including operation time, intraoperative blood loss, and infusion volume. (3) The predictive value of anemia for postoperative POCD was evaluated by drawing ROC curves. (4) Univariate and multivariate logistic regression analyses were conducted to identify the independent factors for POCD in patients at 3 days and 7 days after surgery.
Statistical methods
SPSS version 24.0 (IBM Corp.) was used for data analysis. Continuous variables were expressed as mean ± SD, and categorical variables were expressed as n (%). Between-group comparisons for continuous data were conducted using Student’s t-test, while categorical data were analyzed using the χ2 test. The relationship between cognitive function and anemia degree was determined by Pearson correlation. Univariate and multivariate logistic regression analyses were used to identify the independent factors for POCD in patients at 3 days and 7 days after surgery. P<0.05 was considered with statistical significance.
Results
Comparison of baseline information between the two groups
Comparison of baseline data showed that there was no statistical difference between the two groups in terms of age, gender, body mass index (BMI), tumor size, surgical site, history of previous surgeries, American Society of Anesthesiologists (ASA) grading, and years of education (all P>0.05), as shown in Table 1.
Table 1.
Baseline information of patients in the two groups
| Normal group (n=109) | Anemia group (n=75) | χ2 | P | |
|---|---|---|---|---|
| Age (years) | 0.449 | 0.503 | ||
| ≤70 | 44 (40.37) | 34 (45.33) | ||
| >70 | 65 (59.63) | 41 (54.67) | ||
| Gender | 0.718 | 0.397 | ||
| Male | 69 (63.30) | 52 (69.33) | ||
| Female | 40 (36.70) | 23 (30.67) | ||
| BMI (kg/m2) | 0.702 | 0.402 | ||
| ≤23.9 | 83 (76.15) | 61 (81.33) | ||
| >23.9 | 26 (23.85) | 14 (18.67) | ||
| Tumor size (cm) | 0.434 | 0.510 | ||
| <5 | 66 (60.55) | 49 (65.33) | ||
| ≥5 | 43 (39.45) | 26 (34.67) | ||
| Surgical site | 0.081 | 0.776 | ||
| Stomachs | 50 (45.87) | 36 (48.00) | ||
| Colorectal | 59 (54.13) | 39 (52.00) | ||
| Previous surgical history | 0.434 | 0.510 | ||
| Yes | 37 (33.94) | 22 (29.33) | ||
| No | 72 (66.06) | 53 (70.67) | ||
| ASA classification | 0.624 | 0.732 | ||
| I | 8 (7.34) | 5 (6.67) | ||
| II | 65 (59.63) | 49 (65.33) | ||
| III | 36 (33.03) | 21 (28.00) | ||
| Years of education (years) | 0.663 | 0.416 | ||
| ≤6 | 33 (30.28) | 27 (36.00) | ||
| >6 | 76 (69.72) | 48 (64.00) |
BMI: body mass index; ASA: American Society of Anesthesiologists.
Comparison of cognitive function between the two groups at various time points
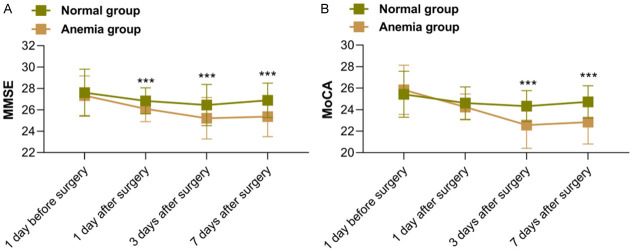
There was no significant difference in the MMSE score and MoCA score between the two groups on the first day before surgery (both P>0.05). However, on the 1st, 3rd and 7th day after surgery, the MMSE scores of the anemia group were significantly lower than those of the normal group (all P<0.05). Additionally, on the 3rd and 7th day after surgery, the MoCA scores of the anemia group were also significantly lower than those of the normal group, see Figure 2.
Figure 2.
Comparison of MMSE score (A) and MoCA score (B) between the two groups across various time points. MMSE: Brief Mental State Examination; MoCA: Montreal Cognitive Assessment. ***P<0.001.
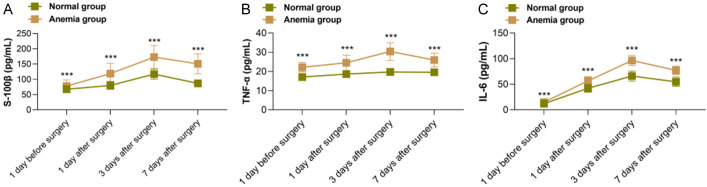
Comparison of inflammatory factor levels between the two groups at various time points
The levels of inflammatory factors s-100β, TNF-α, and IL-6 were compared between the groups before and after the operation. The results showed that levels of these factors were all significantly lower in the anemia group than those in the control group at preoperative day 1 and postoperative day 1, 3 and 7 (all P<0.05), see Figure 3.
Figure 3.
Comparison of the inflammatory factor levels between the two group across various time points. A. S-100β levels. B. TNF-α levels. C. IL-6 levels. s-100β: S100 calcium-binding protein β; TNF-α: tumor necrosis factor α; IL-6: Interleukin-6. ***P<0.001.
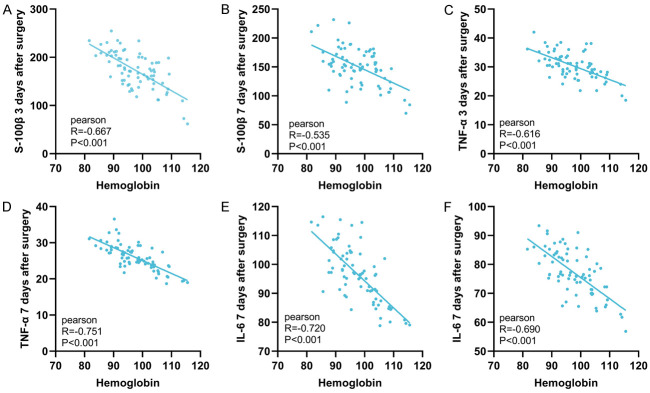
Relationship between postoperative inflammatory factor level and hemoglobin level in anemia patients
Pearson’s correlation analysis showed that in the anemic group, the inflammatory factors S-100β, TNF-α, and IL-6 on postoperative 3 days and 7 days were negatively correlated with hemoglobin levels (all P<0.001), as seen in Figure 4.
Figure 4.
The relationship between postoperative inflammatory factors and the degree of Anemia in anemic patients. A. In the anemic group, the level of S-100β on postoperative day 3 was negatively correlated with hemoglobin levels (R=-0.667, P<0.001). B. In the anemic group, the level of S-100β on postoperative day 7 was negatively correlated with hemoglobin levels (R=-0.535, P<0.001). C. In the anemic group, the level of TNF-α on postoperative day 3 was negatively correlated with hemoglobin levels (R=-0.616, P<0.001). D. In the anemic group, the level of TNF-α on postoperative day 7 was negatively correlated with hemoglobin levels (R=-0.751, P<0.001). E. In the anemic group, the level of IL-6 on postoperative day 3 was negatively correlated with hemoglobin levels (R=-0.720, P<0.001). F. In the anemic group, the level of IL-6 on postoperative day 7 was negatively correlated with hemoglobin levels (R=-0.690, P<0.001). s-100β: S100 calcium-binding protein β; TNF-α: tumor necrosis factor α; IL-6: Interleukin-6.
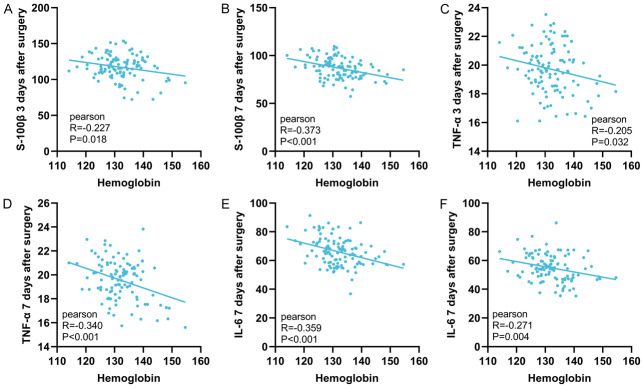
Relationship between postoperative inflammatory factor level and hemoglobin level in non-anemia patients
Pearson’s correlation analysis showed that in the normal group, the inflammatory factors S-100β, TNF-α, and IL-6 on postoperative 3 days and 7 days were negatively correlated with hemoglobin levels (all P<0.05), but the correlation was weaker than that in the anemic group, as seen in Figure 5.
Figure 5.
The relationship between postoperative inflammatory factors and the degree of anemia in non-anemic patients. A. In the normal group, the level of S-100β on postoperative day 3 was negatively correlated with hemoglobin levels (R=-0.227, P=0.018). B. In the normal group, the level of S-100β on postoperative day 7 was negatively correlated with hemoglobin levels (R=-0.373, P<0.001). C. In the normal group, the level of TNF-α on postoperative day 3 was negatively correlated with hemoglobin levels (R=-0.205, P=0.032). D. In the normal group, the level of TNF-α on postoperative day 7 was negatively correlated with hemoglobin levels (R=-0.340, P<0.001). E. In the normal group, the level of IL-6 on postoperative day 3 was negatively correlated with hemoglobin levels (R=-0.359, P<0.001). F. In the normal group, the level of IL-6 on postoperative day 7 was negatively correlated with hemoglobin levels (R=-0.271, P=0.004). s-100β: S100 calcium-binding protein β; TNF-α: tumor necrosis factor α; IL-6: Interleukin-6.
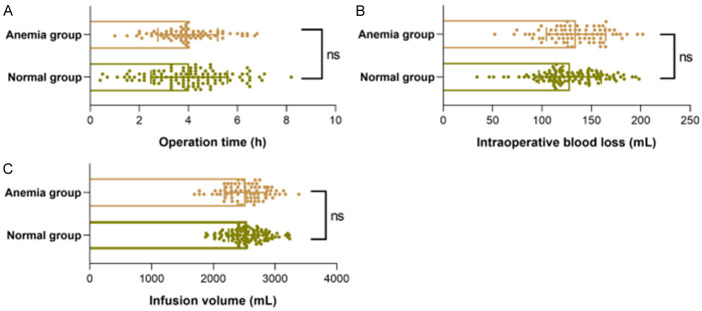
Comparison of surgical indicators between the the two groups
Analysis of surgery-related conditions showed that there were no statistical differences between the two groups in terms of operation time, intraoperative bleeding, and infusion volume (all P>0.05), see Figure 6.
Figure 6.
Comparison of surgery-related indices between the two groups of patients. A. Operation time. B. Intraoperative blood loss. C. Amount of fluid infusion.
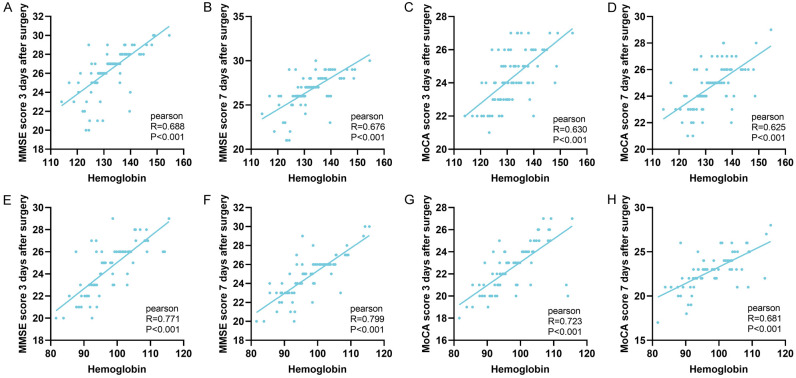
Relationship between postoperative cognitive function and hemoglobin level
Pearson correlation analysis showed that in both groups, the patient’s MMSE score and MoCA score were positively correlated with the hemoglobin level (P<0.001), see Figure 7.
Figure 7.
The relationship between postoperative cognitive function and anemia degree. A. In the normal group, the MMSE score on postoperative day 3 was positively correlated with the hemoglobin level (R=0.688, P<0.001). B. In the normal group, the MMSE score on postoperative day 7 was positively correlated with the hemoglobin level (R=0.676, P<0.001). C. In the normal group, the MoCA score on postoperative day 3 was positively correlated with the hemoglobin level (R=0.630, P<0.001). D. In the normal group, the MoCA score on postoperative day 7 was positively correlated with the hemoglobin level (R=0.625, P<0.001). E. In the anemia group, the MMSE score on postoperative day 3 was positively correlated with the hemoglobin level (R=0.771, P<0.001). F. In the anemia group, the MMSE score on postoperative day 7 was positively correlated with the hemoglobin level (R=0.799, P<0.001). G. In the anemia group, the MoCA score on postoperative day 3 was positively correlated with the hemoglobin level (R=0.723, P<0.001). H. In the anemia group, the MoCA score on postoperative day 7 was positively correlated with the hemoglobin level (R=0.681, P<0.001). MMSE: Brief Mental State Examination; MoCA: Montreal Cognitive Assessment.
Comparison of POCD incidence between the two groups
Comparing the incidence of POCD between the two groups showed that the POCD incidence in the normal group at 3 days and 7 days postoperative (11.01% and 7.34%) were significantly lower than those in the anemic group (38.66% and 30.67%) (P<0.05), as shown in Table 2.
Table 2.
Comparison of POCD incidence between the two groups
| POCD on postoperative day 3 | P | POCD on postoperative day 7 | P | |
|---|---|---|---|---|
| Normal group (n=109) | 12 (11.01) | <0.001 | 8 (7.34) | <0.001 |
| Anemia group (n=75) | 29 (38.66) | 23 (30.67) |
POCD: postoperative cognitive dysfunction.
The predictive value of anemia degree for POCD
The ROC curve was used to test the predictive value of patient’s hemoglobin level for the occurrence of POCD at 3 days and 7 days after surgery. The results showed that the areas under the curve (AUCs) of hemoglobin level for predicting the occurrence of POCD 3 days and 7 days after surgery were 0.858 and 0.865, respectively, as shown in Figure 8 and Table 3.
Figure 8.
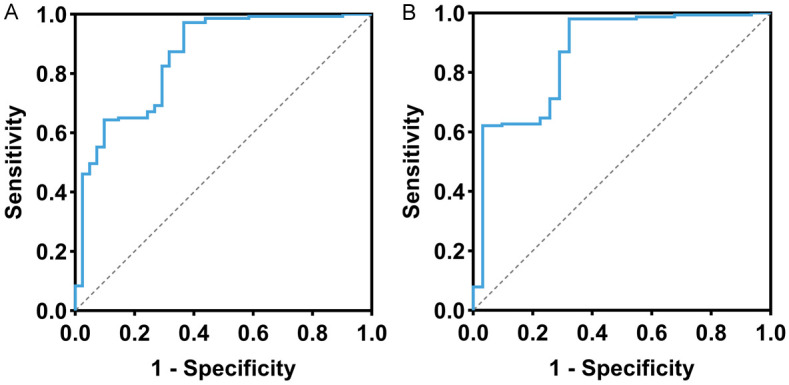
ROC curve of anemia degree in predicting POCD. A. ROC curve of anemia degree in predicting POCD on postoperative day 3. B. ROC curve of anemia degree in predicting POCD on postoperative day 7. POCD: postoperative cognitive dysfunction.
Table 3.
ROC curve data
| AUC | 95% CI | Specificity | Sensitivity | Youden index | Cut off | |
|---|---|---|---|---|---|---|
| ROC curve of anemia degree in predicting POCD on postoperative day 3 | 0.858 | 0.788-0.927 | 63.41% | 97.20% | 60.62% | 94.795 |
| ROC curve of anemia degree in predicting POCD on postoperative day 7 | 0.865 | 0.786-0.944 | 67.74% | 98.04% | 65.78% | 93.265 |
POCD: postoperative cognitive dysfunction; AUC: area under the curve.
Univariate analysis of factors affecting POCD
Analysis by one-way logistic regression revealed that age (OR=2.404, P=0.025), years of education (OR=0.357, P=0.005), and anemia status (OR=5.096, P<0.001) might be the factors affecting POCD at postoperative 3 days, while years of education (OR=0.444, P=0.043) and anemia status (OR=5.584, P<0.001) were possible factors affecting POCD at postoperative 7 days, as shown in Table 4.
Table 4.
Univariate analysis of risk factors for POCD
| POCD on postoperative day 3 | POCD on postoperative day 7 | |||
|---|---|---|---|---|
|
|
|
|||
| OR (95% CI) | P | OR (95% CI) | P | |
| Age (years), ≤70/>70 | 2.404 (1.146-5.359) | 0.025 | 2.008 (0.893-4.859) | 0.103 |
| Gender, male/female | 0.864 (0.401-1.787) | 0.698 | 0.750 (0.309-1.697) | 0.504 |
| Body mass index (kg/m2), ≤23.9/>23.9 | 1.016 (0.419-2.286) | 0.970 | 1.061 (0.394-2.572) | 0.901 |
| Tumor size (cm), <5/≥5 | 0.537 (0.241-1.130) | 0.113 | 0.428 (0.162-1.008) | 0.065 |
| Surgical site, stomach/colorectum | 0.794 (0.394-1.594) | 0.515 | 0.791 (0.362-1.718) | 0.551 |
| History of previous surgery, yes/no | 1.183 (0.565-2.599) | 0.664 | 1.187 (0.523-2.889) | 0.692 |
| ASA classification, I/II/III | 1.081 (0.586-2.000) | 0.802 | 0.932 (0.470-1.841) | 0.839 |
| Years of education (years), ≤6/>6 | 0.357 (0.174-0.729) | 0.005 | 0.444 (0.202-0.981) | 0.043 |
| Anemia, yes/no | 5.096 (2.438-11.233) | <0.001 | 5.584 (2.423-14.120) | <0.001 |
POCD: postoperative cognitive dysfunction.
Multivariate analysis of factors affecting POCD
Multivariate logistic regression analysis of the significant factors with P<0.05 in the univariate analysis showed that age >70 years (OR=2.404, P=0.025), years of education ≤6 years (OR=0.365, P=0.011), and anemia (OR=5.735, P<0.001) were the independent risk factors for POCD at postoperative 3 days, while years of education ≤6 years (OR=0.456, P=0.064) and anemia (OR=5.516, P<0.001) were independent risk factors for POCD at postoperative 7 days, as shown in Table 5.
Table 5.
Multivariate analysis of risk factors for POCD
| POCD on postoperative day 3 | POCD on postoperative day 7 | |||
|---|---|---|---|---|
|
|
|
|||
| OR (95% CI) | P | OR (95% CI) | P | |
| Age (years), ≤70/>70 | 2.826 (1.261-6.749) | 0.015 | ||
| Years of education (years), ≤6/>6 | 0.365 (0.165-0.794) | 0.011 | 0.456 (0.198-1.050) | 0.064 |
| Anemia, yes/no | 5.735 (2.638-13.234) | <0.001 | 5.516 (2.374-14.055) | <0.001 |
POCD: postoperative cognitive dysfunction.
Discussion
The exact pathogenesis of postoperative cognitive dysfunction (POCD) remains unclear, despite some studies having linked it with central nervous system inflammation, cholinergic system dysfunction, neuronal apoptosis, and oxidative stress injury [16,17]. In addition, anemia may lead to insufficient oxygen supply to the brain, causing brain hypoxia injury [18]. Recent studies have found a high POCD incidence in tumor patients, which may be related to systemic inflammation, oxidative stress, proinflammatory cytokines caused by tumors, and treatments such as chemotherapy and radiotherapy [19,20]. With aging, physiological changes reduce individuals’ tolerance to trauma and anesthesia, increase the risk of POCD and potentially leading to long-term POCD and increased postoperative mortality [21]. Elderly patients are susceptible to POCD, especially within the first 72 hours after surgery, due to the lack of compensation in their cardiovascular system [22]. The aging process is accompanied by changes in hematopoietic and inflammatory regulation, leading to a higher prevalence of anemia and increased levels of inflammation in older adults [23].
In our study, we observed a decreasing trend in both the post-operative MMSE score and MOCA score in elderly patients with gastrointestinal tumors. Comparison of the MMSE and MOCA scores showed that patients with anemia had significantly lower MMSE scores than those without anemia at postoperative 1 day, 3 days, and 7 days. Similarly, the MOCA scores of anemic patients were significantly lower than those of non-anemic patients at postoperative 3 days and 7 days. These findings suggest that anemic patients are more likely to experience impaired postoperative cognitive function compared to non-anemic patients.
Both anemia and surgery induce inflammation in patients, and prolonged inflammation is associated with neurodegeneration and poor cognitive performance. Inflammation can disrupt the structural and functional integrity of the blood-brain barrier, resulting in synaptic plasticity loss and neuronal apoptosis, which impede the recovery of brain function after surgery [24]. In our study, we observed elevated postoperative levels of s-100β, TNF-α, and IL-6 in both groups, with significantly higher levels in anemic patients at preoperative 1 day, and postoperative 1 day, 3 days, and 7 days. These findings indicate an elevated inflammatory response after surgery in patients complicated with anemia. Mahalingam et al. [25] statistically analyzed 209 patients with gastrointestinal tumors and found that the prevalence of anemia and systemic inflammatory response was 52.63% and 62.21%, respectively, and that anemia was significantly correlated with systemic inflammation. Our study also revealed a significant negative correlation between the levels of postoperative inflammatory factors (S-100β, TNF-α, IL-6) and hemoglobin levels in anemic patients, suggesting the more severe the anemia, the stronger the postoperative inflammatory response. This may be attributed to the combined action of multiple mechanisms and factors. First, anemia leads to tissue ischemia, promoting the activation of hypoxia-inducible factors and oxidative stress within cells, which in turn stimulates the expression and release of inflammatory factors [26]. Second, anemic patients experience poorer postoperative recovery ability, leading to a prolonged inflammatory response at the trauma site and higher levels of inflammatory factors [27]. In non-anemic patients, postoperative inflammatory factors were also negatively correlated with hemoglobin levels, but the correlation was weaker than that in anemic patients. This may be because non-anemic patients have higher hemoglobin levels, resulting in a relatively weaker inflammatory response.
We analyzed the relationship between postoperative cognitive function and the anemia severity in the two groups of patients using Pearson correlation analysis. The results showed that in both groups, the MMSE score and MoCA score were positively correlated with the hemoglobin level at postoperative 3 days and 7 days, aligning with a previous study where hemoglobin level was positively correlated with memory and cognition in 2,758 elderly subjects aged 60 and above [28]. This suggests that postoperative cognition decreases as anemia worsens. Therefore, preoperative monitoring and optimization of patients’ hemoglobin levels will help improve patients’ postoperative cognitive function. When comparing the POCD incidence at postoperative 3 days and 7 days between the two groups, we observed that the POCD incidence at both time points was significantly lower in non-anemic patients compared to anemic patients. Univariate and multivariate logistic regression analyses identified age >70 years, years of education ≤6 years, and anemia as independent risk factors for POCD on postoperative day 3. Similarly, years of education ≤6 years and anemia were identified as independent risk factors for POCD on postoperative day 7. Wang et al. [29] followed up 207,203 participants aged 60 and above without dementia for 16 years and found that patients with anemia and high inflammation tended to have a higher risk of dementia. They suggested that anemia may limit cerebral blood flow, leading to insufficient cerebral oxygen supply, and that a long-term inflammatory environment may further damage cognitive function. ROC curve analysis in our study showed that the AUCs for hemoglobin level in predicting POCD on postoperative day 3 and day 7 were 0.858 and 0.865, suggesting that the degree of anemia may be a potential predictor of POCD.
The association between age and cognitive decline is well-established, with an increased risk of cognitive impairment as age advances [30,31]. In the early postoperative period, higher age may exacerbate the stress response, subsequently contributing to cognitive decline. However, as time progresses and the body begins to recover, the initial stress period typically subsides from postoperative day 7, and effective management of postoperative complications may have occurred. Consequently, age may no longer independently contribute to the development POCD at the 7-day mark.
Furthermore, studies have suggested that individuals with fewer years of education may have lower cognitive reserves, indicating inadequate development of brain structure and function. This deficiency may result in a heightened reliance on neuroprotective mechanisms during the postoperative period, thereby increasing the risk of POCD [32]. Additionally, patients with anemia often exhibit frailty, which serves as an indicator of increased vulnerability. Frailty is associated with a higher risk of mitochondrial dysfunction and impaired cognitive performance [33]. Mitochondrial dysfunction leads to the overproduction of reactive oxygen species, causing oxidative damage to neurons and subsequently reducing cognitive function. Consequently, anemia emerges as an independent risk factor for postoperative POCD in patients [34].
Despite the association we observed between postoperative POCD and anemia in elderly patients with gastrointestinal tumors, there are some limitations in this study. First, due to the retrospective nature, data on anemia-related micronutrient levels, iron intake, and serum ferritin may not be fully collected, which may affect cognitive function. Second, retrospective studies may introduce selection bias and affect the generalizability of the results. The single-center nature of the study may limit the extrapolation of the results, and there may be other unconsidered factors that affect cognitive function. Besides, the biological mechanisms between anemia and cognitive function should be explored. In the study by Weiskopf et al. [35], hemoglobin-based oxygen carriers were transfused into five patients with cognitive impairment, enabling them to regain consciousness after treatment. By combining such insights with the factors identified in this study, a more personalized and in-depth understanding can be provided for the postoperative management of elderly patients, thereby developing effective prevention and treatment strategies.
In conclusion, anemia is associated with the incidence of COPD in elderly patients with gastrointestinal tumors. Patients with anemia are more susceptible to lower postoperative cognitive function, higher POCD incidence, and elevated postoperative levels of inflammatory factors. Age >70 years, years of education ≤6 years, and anemia were independent risk factors for POCD in patients on postoperative day 3, whereas years of education ≤6 years and anemia were independent risk factors for POCD on postoperative day 7.
Disclosure of conflict of interest
None.
References
- 1.van Sinderen K, Schwarte LA, Schober P. Diagnostic criteria of postoperative cognitive dysfunction: a focused systematic review. Anesthesiol Res Pract. 2020;2020:7384394. doi: 10.1155/2020/7384394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lu J, Zhang Y, Hao Q, Zhou H, Zong Y. IDO-Kynurenine pathway mediates NLRP3 inflammasome activation-induced postoperative cognitive impairment in aged mice. Int J Neurosci. 2023:1–11. doi: 10.1080/00207454.2023.2262741. [DOI] [PubMed] [Google Scholar]
- 3.Monk TG, Weldon BC, Garvan CW, Dede DE, van der Aa MT, Heilman KM, Gravenstein JS. Predictors of cognitive dysfunction after major noncardiac surgery. Anesthesiology. 2008;108:18–30. doi: 10.1097/01.anes.0000296071.19434.1e. [DOI] [PubMed] [Google Scholar]
- 4.Yang X, Huang X, Li M, Jiang Y, Zhang H. Identification of individuals at risk for postoperative cognitive dysfunction (pocd) Ther Adv Neurol Disord. 2022;15:17562864221114356. doi: 10.1177/17562864221114356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arefayne NR, Berhe YW, van Zundert AA. Incidence and factors related to prolonged postoperative cognitive decline (POCD) in elderly patients following surgery and anaesthesia: a systematic review. J Multidiscip Healthc. 2023;16:3405–3413. doi: 10.2147/JMDH.S431168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Luo A, Yan J, Tang X, Zhao Y, Zhou B, Li S. Postoperative cognitive dysfunction in the aged: the collision of neuroinflammaging with perioperative neuroinflammation. Inflammopharmacology. 2019;27:27–37. doi: 10.1007/s10787-018-00559-0. [DOI] [PubMed] [Google Scholar]
- 7.Gilreath JA, Rodgers GM. How I treat cancer-associated anemia. Blood. 2020;136:801–813. doi: 10.1182/blood.2019004017. [DOI] [PubMed] [Google Scholar]
- 8.Abdel-Razeq H, Hashem H. Recent update in the pathogenesis and treatment of chemotherapy and cancer induced anemia. Crit Rev Oncol Hematol. 2020;145:102837. doi: 10.1016/j.critrevonc.2019.102837. [DOI] [PubMed] [Google Scholar]
- 9.Wang L, Shao ZH. Relationship between anemia and clinical features and prognosis of advanced lung cancer patients. Zhonghua Zhong Liu Za Zhi. 2018;40:512–516. doi: 10.3760/cma.j.issn.0253-3766.2018.07.006. [DOI] [PubMed] [Google Scholar]
- 10.Mo K, Ortiz-Babilonia C, Al Farii H, Raad M, Musharbash FN, Neuman BJ, Kebaish KM. Increased severity of anemia is associated with postoperative complications following an adult spinal deformity surgery. World Neurosurg. 2022;167:e541–e548. doi: 10.1016/j.wneu.2022.08.045. [DOI] [PubMed] [Google Scholar]
- 11.Stauder R, Valent P, Theurl I. Anemia at older age: etiologies, clinical implications, and management. Blood. 2018;131:505–514. doi: 10.1182/blood-2017-07-746446. [DOI] [PubMed] [Google Scholar]
- 12.Myint PK, Owen S, McCarthy K, Pearce L, Moug SJ, Stechman MJ, Hewitt J, Carter B. Is anemia associated with cognitive impairment and delirium among older acute surgical patients? Geriatr Gerontol Int. 2018;18:1025–1030. doi: 10.1111/ggi.13293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu J, Tian JM, Liu GZ, Sun JN, Gao PF, Zhang YQ, Yue XQ. Application of remimazolam transversus abdominis plane block in gastrointestinal tumor surgery. World J Gastrointest Oncol. 2023;15:2101–2110. doi: 10.4251/wjgo.v15.i12.2101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jia X, Wang Z, Huang F, Su C, Du W, Jiang H, Wang H, Wang J, Wang F, Su W, Xiao H, Wang Y, Zhang B. A comparison of the mini-mental state examination (MMSE) with the montreal cognitive assessment (MoCA) for mild cognitive impairment screening in Chinese middle-aged and older population: a cross-sectional study. BMC Psychiatry. 2021;21:485. doi: 10.1186/s12888-021-03495-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pinto TCC, Machado L, Bulgacov TM, Rodrigues-Junior AL, Costa MLG, Ximenes RCC, Sougey EB. Is the montreal cognitive assessment (MoCA) screening superior to the mini-mental state examination (MMSE) in the detection of mild cognitive impairment (MCI) and Alzheimer’s disease (AD) in the elderly? Int Psychogeriatr. 2019;31:491–504. doi: 10.1017/S1041610218001370. [DOI] [PubMed] [Google Scholar]
- 16.Hampel H, Mesulam MM, Cuello AC, Farlow MR, Giacobini E, Grossberg GT, Khachaturian AS, Vergallo A, Cavedo E, Snyder PJ, Khachaturian ZS. The cholinergic system in the pathophysiology and treatment of Alzheimer’s disease. Brain. 2018;141:1917–1933. doi: 10.1093/brain/awy132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sikora E, Bielak-Zmijewska A, Dudkowska M, Krzystyniak A, Mosieniak G, Wesierska M, Wlodarczyk J. Cellular senescence in brain aging. Front Aging Neurosci. 2021;13:646924. doi: 10.3389/fnagi.2021.646924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mistry N, Mazer CD, Sled JG, Lazarus AH, Cahill LS, Solish M, Zhou YQ, Romanova N, Hare AGM, Doctor A, Fisher JA, Brunt KR, Simpson JA, Hare GMT. Red blood cell antibody-induced anemia causes differential degrees of tissue hypoxia in kidney and brain. Am J Physiol Regul Integr Comp Physiol. 2018;314:R611–R622. doi: 10.1152/ajpregu.00182.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ding Y, Yu J, Cui F, Li J. Comparison of intravenous and inhalational anesthetic on postoperative cognitive outcomes in elderly patients undergoing cancer surgery: systematic review and meta-analysis. J Perianesth Nurs. 2022;37:683–690. doi: 10.1016/j.jopan.2021.11.017. [DOI] [PubMed] [Google Scholar]
- 20.Zhang Y, Bao HG, Lv YL, Si YN, Han L, Wang HY, Gao YJ, Jiang WQ, Zhang C. Risk factors for early postoperative cognitive dysfunction after colorectal surgery. BMC Anesthesiol. 2019;19:6. doi: 10.1186/s12871-018-0676-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhao J, Dai T, Ding L, Liang Y, Yuan W, Jiang Y, Zheng Y. Correlation between neutrophil/lymphocyte ratio, platelet/lymphocyte ratio and postoperative cognitive dysfunction in elderly patients with esophageal cancer. Medicine (Baltimore) 2023;102:e33233. doi: 10.1097/MD.0000000000033233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang W, Ma Y, Liu Y, Wang P, Liu Y. Effects of dexmedetomidine anesthesia on early postoperative cognitive dysfunction in elderly patients. ACS Chem Neurosci. 2022;13:2309–2314. doi: 10.1021/acschemneuro.2c00173. [DOI] [PubMed] [Google Scholar]
- 23.Xu W, Zheng Y, Suo Z, Fei K, Wang Y, Liu C, Li S, Zhang M, Zhang Y, Zheng Z, Ni C, Zheng H. Effect of dexmedetomidine on postoperative systemic inflammation and recovery in patients undergoing digest tract cancer surgery: a meta-analysis of randomized controlled trials. Front Oncol. 2022;12:970557. doi: 10.3389/fonc.2022.970557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zheng ZH, Tu JL, Li XH, Hua Q, Liu WZ, Liu Y, Pan BX, Hu P, Zhang WH. Neuroinflammation induces anxiety- and depressive-like behavior by modulating neuronal plasticity in the basolateral amygdala. Brain Behav Immun. 2021;91:505–518. doi: 10.1016/j.bbi.2020.11.007. [DOI] [PubMed] [Google Scholar]
- 25.Mahalingam S, Amaranathan A, Sathasivam S, Udayakumar KP. Correlation of preoperative anemia subtypes with tumor characteristics, systemic inflammation and immediate postoperative outcomes in gastrointestinal cancer patients - a prospective observational study. J Gastrointest Cancer. 2023;54:1220–1230. doi: 10.1007/s12029-022-00902-3. [DOI] [PubMed] [Google Scholar]
- 26.Acevedo-Leon D, Monzo-Beltran L, Perez-Sanchez L, Naranjo-Morillo E, Gomez-Abril SA, Estan-Capell N, Banuls C, Saez G. Oxidative stress and DNA damage markers in colorectal cancer. Int J Mol Sci. 2022;23:11664. doi: 10.3390/ijms231911664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Singh S, Gudzenko V, Fink MP. Pathophysiology of perioperative anaemia. Best Pract Res Clin Anaesthesiol. 2012;26:431–439. doi: 10.1016/j.bpa.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 28.Winchester LM, Newby D, Ghose U, Hu P, Green H, Chien S, Ranson J, Faul J, Llewellyn D, Lee J, Bauermeister S, Nevado-Holgado A. Anemia, hemoglobin concentration and cognitive function in the Longitudinal Ageing Study in India-Harmonized Diagnostic Assessment of Dementia (LASI-DAD) and the Health and Retirement Study. medRxiv [Preprint] 2024 2024.01.22.24301583. [Google Scholar]
- 29.Wang J, Wang C, Li X, Guo J, Dove A, Cui Z, Xu W. Association of anemia with cognitive function and dementia among older adults: the role of inflammation. J Alzheimers Dis. 2023;96:125–134. doi: 10.3233/JAD-230483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang S, Chen B, Yuan M, Liu S, Fan H, Yang X, Zou Q, Pu Y, Cai Z. Enriched oxygen improves age-related cognitive impairment through enhancing autophagy. Front Aging Neurosci. 2024;16:1340117. doi: 10.3389/fnagi.2024.1340117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Logan S, Baier MP, Owen DB, Peasari J, Jones KL, Ranjit R, Yarbrough HP, Masingale AM, Bhandari S, Rice HC, Kinter MT, Sonntag WE. Cognitive heterogeneity reveals molecular signatures of age-related impairment. PNAS Nexus. 2023;2:pgad101. doi: 10.1093/pnasnexus/pgad101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cheval B, Saoudi I, Maltagliati S, Fessler L, Farajzadeh A, Sieber S, Cullati S, Boisgontier MP. Initial status and change in cognitive function mediate the association between academic education and physical activity in adults over 50 years of age. Psychol Aging. 2023;38:494–507. doi: 10.1037/pag0000749. [DOI] [PubMed] [Google Scholar]
- 33.Solanki A, Rajendran A, Mohan S, Raj R, Vundinti BR. Mitochondrial DNA variations and mitochondrial dysfunction in Fanconi anemia. PLoS One. 2020;15:e0227603. doi: 10.1371/journal.pone.0227603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu J, Mai P, Yang Z, Wang Z, Yang W, Wang Z. Piceatannol protects PC-12 cells against oxidative damage and mitochondrial dysfunction by inhibiting autophagy via SIRT3 pathway. Nutrients. 2023;15:2973. doi: 10.3390/nu15132973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weiskopf RB, Davenport R, Cap AP, Reddy V, Waters JH, Cserti-Gazdewich C. Increasing hemoglobin concentration with an artificial oxygen carrier improves severe anemia-induced degraded cognitive function. J Trauma Acute Care Surg. 2021;91(Suppl 2):S182–S185. doi: 10.1097/TA.0000000000003261. [DOI] [PubMed] [Google Scholar]