Abstract
Objective: To investigate the high-risk factors for early pulmonary bacterial infection following lung transplantation and their association with long-term mortality. Methods: A retrospective analysis was conducted on 142 lung transplant recipients treated at Wuxi People’s Hospital between January 2018 and July 2022. After applying predefined inclusion and exclusion criteria, 111 cases were analyzed. Univariate and multivariate logistic regression analyses were performed to identify independent risk factors for early pulmonary infection post-transplantation. Additionally, univariate and multivariate Cox regression analyses were used to identify independent prognostic factors affecting one-year survival post-transplantation. Results: Univariate analysis identified age, bacterial infection in donor lungs, and operation duration as risk factors for early pulmonary infection (all P < 0.05). Multivariate analysis was confirmatory for these as independent risk factors (all P < 0.05). Univariate analysis also showed that intraoperative blood loss and oxygenation index impacted one-year survival (P < 0.05). Multivariate analysis was confirmatory for these as independent risk factors (P < 0.05). Conclusion: Early pulmonary bacterial infection was not found to be an independent factor affecting 1-year survival. However, substantial intraoperative blood loss and a reduced oxygenation index were identified as independent risk factors associated with increased mortality within 1 year post-transplantation.
Keywords: Pulmonary infection, lung transplantation, intraoperative bleeding, prognostic factors
Introduction
Lung transplantation is a critical treatment for patients with end-stage lung disease. Annually, over 4,000 lung transplants are performed worldwide, providing a significant extension of life and enhancement of quality for these patients [1]. Despite technological advancements improving patient outcomes, donor shortages remain a significant bottleneck [2]. To mitigate this issue, some regions have broadened donor criteria, including the acceptance of older donors and those with a history of smoking. While this approach may slightly reduce overall survival rates, it is considered beneficial given the high mortality rates on waiting lists [3,4].
In China, lung transplantation developed later than in more technologically advanced countries, leading to gaps in both quantity and quality. However, the field is rapidly advancing, and the establishment of a robust system and the creation of domestic guidelines are crucial for its progress.
Despite improvements in transplantation technology and postoperative care enhancing survival and quality of life [5], early pulmonary bacterial infections post-transplant remain a significant challenge. They affect the success of the transplant and patient survival. Studies have shown that such infections are a major cause of mortality in the first 30 days following transplantation, second only to graft failure [6]. Bacterial infections are particularly prevalent, with bacterial pathogens identified in nearly 80% of transplant recipients, underscoring the importance of managing infectious complications to improve outcome [7].
Lung transplantation is the most effective treatment modality and standard of care for late-stage pulmonary disease. However, a significant disparity between the supply and demand of lung sources places end-stage patients at a high risk of death while awaiting transplantation [8]. Current allocation systems for lung sources prioritize factors expected to influence long-term outcome and prognosis following transplantation. Yet, perioperative factors, particularly lung infections, critically impact patients’ immediate health and well-being [9]. Thus, a thorough examination of early pulmonary bacterial infections and other perioperative risk factors, along with optimizing the donor allocation and perioperative management, are essential for enhancing the quality of life and survival rate of transplant recipients.
The aim of this study was to investigate a correlation between early pulmonary bacterial infection and other high-risk factors with long-term survival and mortality risk post-transplantation. By gaining a deeper understanding and analysis of these factors, this research seeks to offer clearer and more effective preventive and management strategies for transplant success. This study will help bridge the existing knowledge gap in managing and preventing post-transplant infections.
Methods and materials
Ethics statement
This study was reviewed and approved by the Ethics Committee of Wuxi People’s Hospital (Approval Number: 2023-KY23171).
Clinical data collection
The study population comprised 142 lung transplant recipients treated at Wuxi People’s Hospital from January 2018 to July 2022, who were retrospectively analyzed to identify risk factors and outcomes post-transplant. Clinical data were gathered using the Lung Transplant Registry Data Sheet Management Platform. Data collected included patient age, gender, body mass index (BMI), presence of donor lung bacterial infection, oxygenation index, disease type, functional status, history of hypertension, history of smoking, duration of surgery, cold ischemia time, intraoperative blood loss, intraoperative hemorrhage, and patient infections. All patients were monitored for a minimum of one year or until death, with missing data censored during the follow-up period.
Participant inclusion and exclusion criteria
Inclusion criteria: (1) Patients must have a complete clinical profile. (2) Patients diagnosed with wet lung cancer who underwent a lung transplant. (3) Patients meeting the diagnostic criteria for pulmonary infection as defined in reference [10].
Exclusion criteria: (1) Recent history of malignant tumors (within the past 2 years). (2) Uncorrectable dysfunction of heart, liver, kidney, or other vital organs. (3) Uncorrectable bleeding tendencies. (4) Acute conditions such as septicemia, myocardial infarction, or liver failure. (5) High-risk chronic infections and/or drug resistance. (6) Active tuberculosis. (7) Significant chest wall or spinal deformities. (8) Poor compliance or inability to cooperate with treatment or follow-up. (9) Untreated mental illness or uncontrolled mental conditions. (10) Lack of family support or social security. (11) Obesity classified as class II to III (BMI > 35.0 kg/m2). (12) Poor nutritional and functional status with limited rehabilitation potential. (13) Persistent engagement in serious habits such as alcohol, tobacco, or narcotics use within the last 6 months.
Criteria for pulmonary infections
Pulmonary bacterial infections were diagnosed according to the Chinese Technical Code for Diagnosis, Treatment, and Follow-up of Postoperative Complications after Lung Transplantation (2019 edition) [11]. The criteria include: (1) Presence of typical signs and symptoms, such as changes in the character of sputum. (2) Laboratory tests indicating elevated inflammation markers (neutrophils, white blood cells, C-reactive protein, and procalcitonin) and positive bacterial sputum cultures. (3) Imaging (chest CT or X-ray) revealing new or progressive lung lesions indicative of pneumonia, or normal imaging for bronchiectasis with moderate interstitial exudate.
Sample screening and grouping
In this study, we screened a total of 111 samples that met the inclusion criteria, comprising 21 non-infected patients and 90 infected patients. Patients were subsequently categorized into non-infected and infected groups.
Outcome measures
The study employed logistic regression analysis to identify independent risk factors contributing to infections in patients. Additionally, Cox regression analysis was utilized to determine independent prognostic factors affecting one-year survival rate.
Statistical analysis
Data analysis was conducted using SPSS software version 26.0. Quantitative data were expressed as mean ± standard deviation, and comparisons between two groups were made using the t-test. Categorical data were presented as cases (%) and analyzed using the chi-square test. Survival differences between groups were assessed using the Kaplan-Meier method, with the log-rank test applied for statistical significance. Cox regression analysis was used to identify independent risk factors affecting one-year survival. Logistic regression analysis was reiterated to explore the factors contributing to patient infections. Data visualization was performed using GraphPad Prism software version 8.00. Statistical significance was set at p < 0.05.
Results
Univariate analysis of pulmonary infections in patients
The analysis of clinical data from infected and uninfected patients revealed significant risk factors for lung infection, including bacterial infection of the donor lung, patient age, and operation time (Table 1, all P < 0.05).
Table 1.
Univariate analysis of patients
| Factor | Infection group (n = 90) | Uninfected group (n = 21) | χ2 value | P value |
|---|---|---|---|---|
| Age | ||||
| ≥ 55 years | 68 | 10 | 6.361 | 0.012 |
| < 55 years | 22 | 11 | ||
| Gender | ||||
| Male | 50 | 13 | 0.280 | 0.597 |
| Female | 40 | 8 | ||
| Body mass index | ||||
| ≥ 25 kg/m2 | 22 | 6 | 0.154 | 0.695 |
| < 25 kg/m2 | 68 | 15 | ||
| Bacterial infection of donor lung | ||||
| Yes | 36 | 3 | 4.940 | 0.026 |
| No | 54 | 18 | ||
| Oxygenation index | ||||
| ≥ 300/mmHg | 58 | 17 | 2.117 | 0.146 |
| < 300/mmHg | 32 | 4 | ||
| Type of disease | ||||
| Idiopathic interstitial pulmonary fibrosis | 21 | 5 | 0.748 | 0.862 |
| Secondary interstitial pulmonary fibrosis | 23 | 5 | ||
| Pneumoconiosis | 11 | 4 | ||
| The rest | 35 | 7 | ||
| Functional status | ||||
| Activity limitations | 80 | 18 | 0.166 | 0.684 |
| No activity restrictions | 10 | 3 | ||
| History of hypertension | ||||
| Yes | 27 | 6 | 0.017 | 0.897 |
| No | 63 | 15 | ||
| History of smoking | ||||
| Yes | 55 | 15 | 0.778 | 0.378 |
| No | 35 | 6 | ||
| Operation time | ||||
| ≥ 6 h | 41 | 4 | 4.963 | 0.026 |
| < 6 h | 49 | 17 | ||
| Cold ischemia time | ||||
| ≥ 8 h | 45 | 12 | 0.348 | 0.555 |
| < 8 h | 45 | 9 | ||
| Intraoperative blood loss | ||||
| ≥ 1000 mL | 40 | 12 | 1.103 | 0.294 |
| < 1000 mL | 50 | 9 | ||
| Intraoperative blood transfusion volume | ||||
| ≥ 1000 mL | 37 | 11 | 0.881 | 0.348 |
| < 1000 mL | 53 | 10 |
Logistic regression for lung infections
After performing the univariate analysis, values were assigned to the identified risk factors (Table 2). A subsequent multifactorial logistic regression analysis was conducted, revealing that age, bacterial infection of donor lung, and operation time were independent risk factors associated with lung infection (Table 3, all P < 0.05).
Table 2.
Risk-factor assignment table
| Factor | Assignment |
|---|---|
| Age | ≥ 55 = 1, < 55 = 0 |
| Bacterial infection of donor lung | Yes = 1, no = 0 |
| Operation time | ≥ 6 h = 1, < 6 h = 0 |
| Infection | Infected = 1, uninfected = 0 |
Table 3.
Multifactorial logistic regression analysis for lung infections
| Factor | β | Standard error | Chi-square value | P value | OR value | 95% CI | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Lower limit | Upper limit | ||||||
| Age | 1.257 | 0.538 | 5.466 | 0.019 | 3.516 | 1.225 | 10.087 |
| Bacterial infection of donor lung | 1.397 | 0.685 | 4.155 | 0.042 | 4.043 | 1.055 | 15.491 |
| Operation time | 1.459 | 0.627 | 5.414 | 0.02 | 4.301 | 1.259 | 14.697 |
Prognostic analysis of patients’ 1-year survival
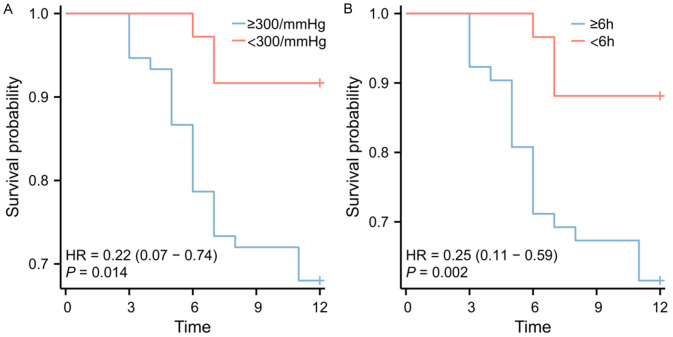
Cox regression analysis was conducted to evaluate the factors influencing patients’ 1-year survival. Univariate analysis identified the receptor oxygenation index and intraoperative blood loss as independent risk factors; however, these factors were associated with early pulmonary infection rather than directly affecting 1-year survival (all P < 0.05, Table 4). Further multivariate Cox regression analysis demonstrated that the receptor oxygenation index and intraoperative blood loss were indeed independent prognostic risk factors affecting 1-year survival (both P < 0.05, Table 5 and Figure 1).
Table 4.
Univariate Cox regression
| Factor | β | Standard error | P value | HR | 95% CI | |
|---|---|---|---|---|---|---|
|
| ||||||
| Lower limit | Upper limit | |||||
| Types of Lung Diseases | -0.115 | 0.160 | 0.472 | 0.891 | 0.652 | 1.219 |
| Infection | 0.358 | 0.542 | 0.509 | 1.431 | 0.495 | 4.137 |
| High blood pressure | 0.175 | 0.408 | 0.668 | 1.192 | 0.535 | 2.652 |
| Bacterial infection of donor lung | -0.243 | 0.422 | 0.565 | 0.785 | 0.343 | 1.792 |
| Functional status | 1.341 | 1.019 | 0.188 | 3.825 | 0.519 | 28.189 |
| Cold ischemia time | 0.384 | 0.392 | 0.327 | 1.469 | 0.681 | 3.165 |
| Age | 0.956 | 0.542 | 0.078 | 2.601 | 0.899 | 7.523 |
| Operation time | 0.187 | 0.387 | 0.628 | 1.206 | 0.565 | 2.577 |
| Intraoperative blood loss | 1.382 | 0.440 | 0.002 | 3.983 | 1.683 | 9.427 |
| Intraoperative blood transfusion | -0.312 | 0.399 | 0.434 | 0.732 | 0.335 | 1.599 |
| Body mass index | 0.039 | 0.439 | 0.930 | 1.039 | 0.440 | 2.458 |
| History of smoking | 0.613 | 0.439 | 0.163 | 1.847 | 0.781 | 4.368 |
| Gender | -0.549 | 0.387 | 0.157 | 0.578 | 0.270 | 1.234 |
| Receptor oxygenation index | -1.501 | 0.613 | 0.014 | 0.223 | 0.067 | 0.741 |
Table 5.
Multifactor Cox regression
| Factor | β | Standard error | P value | HR | 95% CI | |
|---|---|---|---|---|---|---|
|
| ||||||
| Lower limit | Upper limit | |||||
| Intraoperative blood loss | 1.324 | 0.440 | 0.003 | 3.757 | 1.586 | 8.898 |
| Receptor oxygenation index | 1.324 | 0.440 | 0.003 | 3.757 | 1.586 | 8.898 |
Figure 1.
Survival curves for risk factors affecting 1-year survival in lung transplant patients. A. Survival curve for oxygenation index. B. Survival curve for intraoperative blood loss.
Discussion
Lung transplantation offers a vital therapeutic option for patients with chronic end-stage lung disease. Compared to other organ transplants, lung transplantation has a lower survival rate, primarily due to the high incidence of postoperative infections and rejection [12]. However, advances in surgical techniques, optimized immunosuppressive regimens, and enhanced infection prevention strategies have significantly reduced the mortality rate among lung transplant recipients [13]. Despite these improvements, factors such as the use of postoperative immunosuppressive drugs, denervation of the allograft lungs, impairment of the cough reflex, dysfunctional mucociliary clearance, and impaired lymphatic drainage continue to make lung infections a prevalent complication post-transplantation [12].
According to McCort et al. [14], between 50% and 85% of lung transplant recipients experience at least one postoperative bacterial lung infection, with the majority occurring shortly after the procedure. Furthermore, a retrospective study from a single center in Poland involving 97 lung transplant patients found that 69% developed pulmonary bacterial infections during their hospital stays [15]. These findings highlight the importance of comprehensive analyses to identify risk factors associated with early pulmonary bacterial infection post-transplantation. Moreover, understanding the relationship between these risk factors and long-term mortality is crucial. By studying these factors, we can develop more scientifically grounded and practical prevention and management guidelines to enhance the success rate of lung transplantations and improve patients’ quality of life and outcomes.
In this study, both univariate and multivariate logistic regression analyses identified bacterial infection of donor lungs, patient age, and operation time as independent risk factors significantly influencing the rate of postoperative lung infections. These findings are consistent with previous research and highlight the importance of these factors in managing infection risk after lung transplantation. For instance, prior studies have suggested that older age may elevate infection risk due to altered immune response and underlying disease conditions in patients [16]. The detection of bacterial infections in donor lungs underscores the critical role of thorough donor screening and preoperative prophylaxis in mitigating infection risk, aligning with other research that has examined infection risks associated with donor conditions [17,18]. Additionally, we found that extended surgery durations may increase infection risk due to prolonged immunosuppression and mechanical ventilation. This is consistent with prior findings in that regard [19].
These insights provide valuable information for clinical practice, emphasizing the need for optimized surgical procedures, stringent donor screening, and effective preoperative anti-infective measures to reduce postoperative infection risks in lung transplantation. This not only offers clinicians clearer and more specific guidance but also opens new avenues for future research on improving postoperative outcomes and reducing infection risks in lung transplant recipients. Furthermore, the identification of these independent risk factors paves the way for developing more personalized and targeted infection prevention and management strategies to enhance quality of life and survival of lung transplant patients.
Early pulmonary bacterial infections following lung transplantation significantly contribute to mortality. The International Society for Heart and Lung Transplantation reports that the main causes of death within 30 days of transplantation are graft failure and bacterial infections, with viral infections becoming more prevalent after this period [20]. Studies indicate that lung infections are the second most common cause of mortality within the first 30 days post-transplantation and become the primary cause between 30 days and 1 year [21,22]. The respiratory tract is frequently the predominant site of infection post-transplantation, with bacterial pneumonia being the most common infectious complication [23].
In this study, our analysis did not identify lung infection as an independent prognostic factor affecting 1-year survival. Although infection poses a significant clinical challenge, it did not show a statistically significant impact on 1-year survival in this sample. This may have been attributable to the limited sample size or the presence of confounding factors. Conversely, the study identified receptor oxygenation index and intraoperative blood loss as independent prognostic factors affecting 1-year survival. Substantial intraoperative blood loss, which can lead to hypovolemic shock and multi-organ dysfunction due to poor tissue perfusion, heightens early mortality risk. This is supported by findings from Tamagawa et al., who noted that intraoperative blood loss is a critical prognostic factor in pancreatic cancer surgery, with minimizing of bleeding being essential for improved outcome [24].
The oxygenation index, reflecting the body’s oxygen exchange efficiency, is another crucial factor. A decrease in this index signals inadequate tissue oxygenation, potentially leading to organ failure and increased infection risk, thus directly escalating early mortality risk among patients. Lee et al. highlighted the prognostic value of oxygenation indices, noting significant differences in the median ROX (ratio of oxygenation to respiratory rate) indices between survivors and non-survivors, with non-survivors presenting lower indices [25].
This study highlights the impact of infections and related complications on patient prognosis after lung transplantation, yet it is subject to several limitations. First, the small sample size may have affected the accuracy and generalizability of the findings. Second, while multiple factors associated with lung infections and patient prognosis were identified, the study did not fully capture all possible influences or the complex interactions between them. Finally, the focus was primarily on early bacterial pneumonia and intraoperative blood loss, possibly overlooking other critical factors such as viral and fungal infections, airway complications, and overall patient health.
To address these limitations, future research should consider improving study design, such as increasing the sample size, conducting multicenter studies, and employing diverse analytical methods to enhance the accuracy of assessing the impact of infection risk and other complications on prognosis after lung transplantation.
In conclusion, while early pulmonary bacterial infection was not identified as an independent prognostic factor significantly affecting 1-year survival, massive intraoperative blood loss and decreased oxygenation index did prove to be independent prognostic risk factors in this regard. Based on these findings, it is recommended that clinical efforts should prioritize the management of intraoperative bleeding and maintenance of the oxygenation index to optimize outcome.
Acknowledgements
This study was supported by the National Natural Science Foundation of China (No. 82070059).
Written informed consent was signed from all patients.
Disclosure of conflict of interest
None.
References
- 1.Kolaitis NA. Lung transplantation for pulmonary arterial hypertension. Chest. 2023;164:992–1006. doi: 10.1016/j.chest.2023.04.047. [DOI] [PubMed] [Google Scholar]
- 2.Nakajima D, Nagata S, Kayawake H, Tanaka S, Yamada Y, Yutaka Y, Ohsumi A, Hamaji M, Chen-Yoshikawa TF, Date H. Successful lung transplant cases with ex vivo lung perfusion assessment of extended criteria donor lungs. Gen Thorac Cardiovasc Surg. 2022;70:406–412. doi: 10.1007/s11748-022-01774-x. [DOI] [PubMed] [Google Scholar]
- 3.Noda K, Furukawa M, Chan EG, Sanchez PG. Expanding donor options for lung transplant: extended criteria, donation after circulatory death, ABO incompatibility, and evolution of Ex vivo lung perfusion. Transplantation. 2023;107:1440–1451. doi: 10.1097/TP.0000000000004480. [DOI] [PubMed] [Google Scholar]
- 4.Bisbee CR, Sherard C, Kwon J, Hashmi ZA, Gibney BC, Rajab T. Devices for donor lung preservation. Expert Rev Med Devices. 2022;19:959–964. doi: 10.1080/17434440.2022.2151359. [DOI] [PubMed] [Google Scholar]
- 5.Neizer H, Singh GB, Gupta S, Singh SK. Addressing donor-organ shortages using extended criteria in lung transplantation. Ann Cardiothorac Surg. 2020;9:49–50. doi: 10.21037/acs.2019.10.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chambers DC, Yusen RD, Cherikh WS, Goldfarb SB, Kucheryavaya AY, Khusch K, Levvey BJ, Lund LH, Meiser B, Rossano JW, Stehlik J International Society for Heart and Lung Transplantation. The registry of the international society for heart and lung transplantation: thirty-fourth adult lung and heart-lung transplantation report-2017; focus theme: allograft ischemic time. J Heart Lung Transplant. 2017;36:1047–1059. doi: 10.1016/j.healun.2017.07.016. [DOI] [PubMed] [Google Scholar]
- 7.Tosi D, Palleschi A. Advances in lung transplantation. Cells. 2023;12:923. doi: 10.3390/cells12060923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bos S, Vos R, Van Raemdonck DE, Verleden GM. Survival in adult lung transplantation: where are we in 2020? Curr Opin Organ Transplant. 2020;25:268–273. doi: 10.1097/MOT.0000000000000753. [DOI] [PubMed] [Google Scholar]
- 9.van den Bogaart L, Cipriano A, Koutsokera A, Manuel O. Understanding rare infections post-lung transplantation. Expert Rev Respir Med. 2021;15:325–338. doi: 10.1080/17476348.2021.1843428. [DOI] [PubMed] [Google Scholar]
- 10.Torres A, Niederman MS, Chastre J, Ewig S, Fernandez-Vandellos P, Hanberger H, Kollef M, Li Bassi G, Luna CM, Martin-Loeches I, Paiva JA, Read RC, Rigau D, Timsit JF, Welte T, Wunderink R. International ERS/ESICM/ESCMID/ALAT guidelines for the management of hospital-acquired pneumonia and ventilator-associated pneumonia: guidelines for the management of hospital-acquired pneumonia (HAP)/ventilator-associated pneumonia (VAP) of the European Respiratory Society (ERS), European Society of Intensive Care Medicine (ESICM), European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and Asociacion Latinoamericana del Torax (ALAT) Eur Respir J. 2017;50:1700582. doi: 10.1183/13993003.00582-2017. [DOI] [PubMed] [Google Scholar]
- 11.Hu CX, Chen WH, He JX, Jiang GN, Li XS, Wei D, Wu B, Zhang J, Wang C, Chen JY. Lung transplantation in China between 2015 and 2018. Chin Med J (Engl) 2019;132:2783–2789. doi: 10.1097/CM9.0000000000000543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gagliotti C, Morsillo F, Moro ML, Masiero L, Procaccio F, Vespasiano F, Pantosti A, Monaco M, Errico G, Ricci A, Grossi P, Nanni Costa A SInT Collaborative Study Group. Infections in liver and lung transplant recipients: a national prospective cohort. Eur J Clin Microbiol Infect Dis. 2018;37:399–407. doi: 10.1007/s10096-018-3183-0. [DOI] [PubMed] [Google Scholar]
- 13.Leard LE, Holm AM, Valapour M, Glanville AR, Attawar S, Aversa M, Campos SV, Christon LM, Cypel M, Dellgren G, Hartwig MG, Kapnadak SG, Kolaitis NA, Kotloff RM, Patterson CM, Shlobin OA, Smith PJ, Solé A, Solomon M, Weill D, Wijsenbeek MS, Willemse BWM, Arcasoy SM, Ramos KJ. Consensus document for the selection of lung transplant candidates: an update from the International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 2021;40:1349–1379. doi: 10.1016/j.healun.2021.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McCort M, MacKenzie E, Pursell K, Pitrak D. Bacterial infections in lung transplantation. J Thorac Dis. 2021;13:6654–6672. doi: 10.21037/jtd-2021-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wojarski J, Ochman M, Medrala W, Kulaczkowska Z, Karolak W, Maruszewski M, Urlik M, Wozniak-Grygiel E, Sioła M, Latos M, Biniszkiewicz P, Pyrc K, Zeglen S. Bacterial infections during hospital stay and their impact on mortality after lung transplantation: a single-center study. Transplant Proc. 2018;50:2064–2069. doi: 10.1016/j.transproceed.2017.11.080. [DOI] [PubMed] [Google Scholar]
- 16.Joean O, Welte T, Gottlieb J. Chest infections after lung transplantation. Chest. 2022;161:937–948. doi: 10.1016/j.chest.2021.10.014. [DOI] [PubMed] [Google Scholar]
- 17.Samanta P, Clancy CJ, Nguyen MH. Fungal infections in lung transplantation. J Thorac Dis. 2021;13:6695–6707. doi: 10.21037/jtd-2021-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marriott DJ, Orla Morrissey C. Common infections following lung transplantation. Essentials in Lung Transplantation. 2018;31:173–219. [Google Scholar]
- 19.Paglicci L, Borgo V, Lanzarone N, Fabbiani M, Cassol C, Cusi MG, Valassina M, Scolletta S, Bargagli E, Marchetti L, Paladini P, Luzzi L, Fossi A, Bennett D, Montagnani F. Incidence and risk factors for respiratory tract bacterial colonization and infection in lung transplant recipients. Eur J Clin Microbiol Infect Dis. 2021;40:1271–1282. doi: 10.1007/s10096-021-04153-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Paglicci L, Borgo V, Lanzarone N, Fabbiani M, Cassol C, Cusi MG, Valassina M, Scolletta S, Bargagli E, Marchetti L, Paladini P, Luzzi L, Fossi A, Bennett D, Montagnani F. Incidence and risk factors for respiratory tract bacterial colonization and infection in lung transplant recipients. Eur J Clin Microbiol Infect Dis. 2021;40:1271–1282. doi: 10.1007/s10096-021-04153-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fishman JA. Infections in immunocompromised hosts and organ transplant recipients: essentials. Liver Transpl. 2011;17(Suppl 3):S34–S37. doi: 10.1002/lt.22378. [DOI] [PubMed] [Google Scholar]
- 22.Konishi Y, Miyoshi K, Kurosaki T, Otani S, Sugimoto S, Yamane M, Oto T, Toyooka S. Airway bacteria of the recipient but not the donor are relevant to post-lung transplant pneumonia. Gen Thorac Cardiovasc Surg. 2020;68:833–840. doi: 10.1007/s11748-019-01273-6. [DOI] [PubMed] [Google Scholar]
- 23.Kim T, Yeo HJ, Jang JH, Kim D, Jeon D, Kim YS, Cho WH. Prognostic impact of preoperative respiratory colonization on early-onset pneumonia after lung transplantation. J Thorac Dis. 2022;14:1900–1908. doi: 10.21037/jtd-21-1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tamagawa H, Aoyama T, Yamamoto N, Kamiya M, Murakawa M, Atsumi Y, Numata M, Kazama K, Hara K, Yukawa N, Rino Y, Masuda M, Morinaga S. The impact of intraoperative blood loss on the survival of patients with stage II/III pancreatic cancer. In Vivo. 2020;34:1469–1474. doi: 10.21873/invivo.11931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee CU, Jo YH, Lee JH, Kim J, Park SM, Hwang JE, Lee DK, Park I, Jang DH, Lee SM. The index of oxygenation to respiratory rate as a prognostic factor for mortality in sepsis. Am J Emerg Med. 2021;45:426–432. doi: 10.1016/j.ajem.2020.09.052. [DOI] [PubMed] [Google Scholar]