Abstract
Aims: To explore the efficacy and safety of lumbar sympathetic ganglion radiofrequency combined with anhydrous ethanol in treating pain associated with osteonecrosis of the femoral head, providing clinical reference. Methods: This retrospective study involved 101 patients with osteonecrosis of the femoral head. According to the different treatment methods, the patients were classified into an observation group where lumbar sympathetic ganglion radiofrequency combined with anhydrous ethanol therapy was applied (n=51) and a control group where lumbar sympathetic ganglion radiofrequency alone was applied (n=50). The Visual Analogue Scale (VAS) was used to assess the joint pain. Harris hip joint scores, incidence of complications, levels of inflammatory factors (hs-CRP and IL-6), and overall therapeutic effects were also compared between the two groups. Results: The total effective rate of the observation group was significantly higher than that of the control group (P<0.05). The VAS score of joint pain was significantly lower in the observation group as compared with the control group (P<0.05). Harris scores were higher in the observation group than in the control group (P<0.05). The observation group had significantly lower levels of hs-CRP and IL-6 than the control group (P<0.001). In addition, there was no difference between the two groups in the incidence of complications (P=0.11). Conclusion: Lumbar sympathetic ganglion radiofrequency combined with anhydrous ethanol provides an effective method for treating avascular necrosis of the femoral head, with good therapeutic effects on improving blood supply to the femoral head and relieving pain, and with good safety profile.
Keywords: Lumbar sympathetic ganglion radiofrequency, anhydrous ethanol, osteonecrosis of the femoral head
Introduction
Osteonecrosis of the femoral head (ONFH) is a clinically challenging disease, defined by the International Society for Bone Circulation and the American Society of Orthopedic Surgeons as the interruption or damage of blood supply to the femoral head. This interruption leads to the death of bone cells and bone marrow components, followed by tissue repair that results in structural changes of the femoral head, collapse of the femoral head, thus causing joint pain and functional impairment in patients, with an incidence rate ranging from 0.005% to 0.1% of the general population [1]. The epidemiology of avascular necrosis is influenced by a variety of factors, including age, gender, underlying medical conditions, and lifestyle choices [2,3]. It is more common in individuals between the ages of 30 and 50, with a higher prevalence in males compared to females [4]. Other risk factors for avascular necrosis include trauma to the hip joint, corticosteroid use, excessive alcohol consumption, and certain medical conditions such as sickle cell disease and lupus. Research has shown that in middle-aged patients, the primary treatment for ONFH is hip preservation therapy [5], with the main goals to relieve pain, restore hip joint function, and avoid or delay total hip replacement surgery [6]. Therefore, early intervention for ONFH and preserving the patient’s hip joint, is currently the key treatment focus and hot topic of concern.
Currently, hip preservation methods include medications, physical therapy, core decompression, and hip replacement surgery [7-9]. Lumbar sympathetic nerve block with anhydrous ethanol injection and radiofrequency thermocoagulation are commonly used therapeutic methods for the treatment of avascular necrosis of the femoral head in pain clinic. Both procedures are performed under local anesthesia, with minimal damage, in line with the concept of minimally invasive treatment, and are safe and effective. However, the exact efficacy of anhydrous ethanol injection and radiofrequency thermocoagulation in comparison to hip arthroplasty is not clear. The limited range of radiofrequency (5 mm), variations in the size, shape, and position of the sympathetic nerve chain, as well as suboptimal distribution of anhydrous ethanol flow, can lead to incomplete destruction or blockage of the sympathetic nerve chain, resulting in suboptimal treatment outcomes and potential recurrence [10-13]. Currently, there are no reports on the combined use of lumbar sympathetic nerve radiofrequency thermocoagulation and anhydrous ethanol injection in treating ONFH.
Considering the potential limitations of a single treatment modality, this study aims to compare the efficacy and safety of lumbar sympathetic nerve radiofrequency thermocoagulation combined with anhydrous ethanol injection versus lumbar sympathetic nerve radiofrequency thermocoagulation alone.
Materials and methods
Clinical data
In this retrospective study, a total of 101 cases with early-stage ONFH that were treated in the Affiliated Hospital of Hebei University of Engineering, Handan from June 2020 to February 2022 were selected as the research subjects. According to the different treatment methods, these patients were classified into an observation group where lumbar sympathetic ganglion radiofrequency combined with anhydrous ethanol therapy was applied (n=51), and a control group where single lumbar sympathetic ganglion radiofrequency therapy was applied (n=50). This study was approved by the ethics committee of Affiliated Hospital of Hebei University of Engineering.
Inclusion criteria: Patients diagnosed with stage I or II ONFH; Patients presenting with early symptoms such as hip joint pain, limited hip joint mobility, limping, and knee joint pain; Patients agreeing to undergo examinations involving magnetic resonance imaging (MRI) and CT scans; Patients who received a definitive diagnosis and staging through X-ray, CT, and MRI examinations; Patients with complete clinical data.
Exclusion criteria: Patients with local soft tissue or systemic infection at the puncture site; Patients with psychological disorders that couldn’t cooperate to complete clinical observation, affecting the evaluation of therapeutic effect; Patients with significant dysfunction of heart, brain, liver, lung, kidney function, and abnormal coagulation function.
Treatment
The control group received lumbar sympathetic ganglion radiofrequency therapy. The patient was positioned comfortably on the procedure table, and vital signs were monitored. The skin overlying the lumbar sympathetic ganglion area was cleaned and sterilized. A local anesthetic was injected into the skin and deeper tissues to numb the area and reduce discomfort during the procedure. Using fluoroscopy, a type of real-time X-ray imaging, the interventional radiologist located the lumbar sympathetic ganglion in the lower back region. A thin, insulated needle electrode was inserted through the skin and positioned near the lumbar sympathetic ganglion under fluoroscopic guidance. The interventional radiologist performed sensory and motor testing to ensure the correct placement of the electrode near the lumbar sympathetic ganglion. Once the correct placement was confirmed, radiofrequency energy was delivered through the electrode to create a lesion or heat lesion around the lumbar sympathetic ganglion. This disrupted the pain signals transmitted by the sympathetic nerves. After confirming no blood, fluid, or air during retraction, the impedance of the surrounding tissue at the tip of the test electrode was set to be 200-550 Ω. Then, under 0.3-0.5 V, 50 Hz sensory stimulation and 1.3-1.5 V, 2 Hz motor stimulation, any abnormal sensation or muscle contraction was observed. Finally, continuous radiofrequency at 70°C for 180 s, 80°C for 180 s, and 90°C for 180 s was applied. Then, the electrode was removed, and a small bandage was applied to the puncture site. The patient was monitored for a short period before being discharged with post-procedure instructions.
The observation group received an anhydrous ethanol injection as part of their treatment in addition to the steps outlined above for the control group. Following the completion of radiofrequency therapy, 3 ml of 75% anhydrous ethanol was injected into the lumbar sympathetic ganglion to further disrupt the nerve signals and provide pain relief. The patient was monitored for a short period after the procedures to observe if there were any immediate complications. Pain relief may be experienced immediately or may take a few days to become effective.
Observed indicators
The primary indicators included pain assessment and hip joint function. Pain was assessed using Visual Analogue Scale (VAS) [14]. The higher the VAS score, the more severe the pain. Hip joint function was evaluated using the Harris Score [15]. Higher Harris scores indicate better recovery of hip joint function. The Harris score categorizes hip function recovery of ONFH patients into excellent (≥90), good (80-90, including 80), medium (70-80, including 70), and poor (<70).
The secondary indicators included general clinical characteristics, such as gender, age, disease course, painful area, history of smoking, drinking, diabetes, hypertension, coronary heart disease, chronic kidney disease, chronic obstructive pulmonary disease, therapeutic effects, inflammatory factors (hs-CRP and IL-6) and incidence of complications. The criteria for assessing therapeutic effects: ① Markedly effective efficacy: Percentage of pain relief ≥75%; ② Effective efficacy: Percentage of pain relief between 50% and 75%; ③ Ineffective efficacy: Percentage of pain relief ≤25%. Overall effective rate = [(Markedly effective cases + Effective cases)/total number of cases] * 100%. The inflammatory factors: Using EDTA-K2 anticoagulant vacuum blood collection tubes, four groups of patients had 5 ml of blood drawn from the cubital vein before anesthesia, 1 hour after surgery, 6 hours after surgery, and 24 hours after surgery. The collected venous blood was divided, labeled, and stored in a 4°C refrigerator. The blood was promptly centrifuged at 4000 r/min for 10 minutes, and the serum was stored in a -70°C freezer. After the specimen collection was completed, ELISA method was used to detect the concentrations of hs-CRP and IL-6 in the serum. The detection methods followed the operation steps of the hs-CRP (hs-CRP; Wuhan Yipu Biotechnology Co., Ltd., Cat. No. CK-E11093), and IL-6 (IL-6; Chuzhou shinuoda Biological Technology Co., Ltd., Cat. No. SND-H1935) enzyme-linked immunosorbent assay kits.
Follow-up
All primary indicators and inflammatory factors were assessed at the first week, third month, sixth month and twelfth month after intervention.
Statistical analysis
In this study, data analysis was performed using SPSS 22.0. GraphPad Prism 9.0 was used for figure plotting. Count data were expressed as numbers and percentage, and comparison was performed using chi-square test or Fisher’s exact test. The Shapiro-Wilk test was used to analyze whether the quantitative data followed a normal distribution. Data following a normal distribution were expressed as Mean ± standard deviation, and the comparisons between the two groups were conducted using t-test; while those not following a normal distribution were compared between the two groups using Kruskal-Wallis test. For the comparison among multiple time points, repeated measurement of variance with post-hoc LSD-t test was conducted. All tests were two-tailed, and P<0.05 was considered statistically significant.
Results
Clinical characteristics
The mean age was 55.6±6.9 years in the observation group and 52.68±7.6 years in the control group (P=0.012). The disease course was 5.1±3.2 days in the observation group and 5.3±3.3 days in the control group (P=0.095). Furthermore, no significant difference was observed in baseline data such as gender, painful area, FICAT staging (Ficat and Arlet classification), smoking, drinking, diabetes, hypertension, coronary heart disease, chronic kidney disease, chronic obstructive pulmonary disease and anemia between the two groups (all P>0.05) (Table 1).
Table 1.
Comparison of general information between the two groups of patients
| Observation group (n=51) | Control group (n=50) | t | P | |
|---|---|---|---|---|
| Gender | 0.562 | 0.757 | ||
| Male | 36 | 35 | ||
| Female | 15 | 15 | ||
| Age | 55.6±6.9 | 52.68±7.6 | 2.697 | 0.102 |
| Disease course | 5.1±3.2 | 5.3±3.3 | 2.984 | 0.095 |
| Painful area | 0.756 | 0.651 | ||
| Hips | 51 | 50 | ||
| Groin | 51 | 50 | ||
| Knee | 12 | 11 | ||
| FICAT staging | 3.316 | 0.069 | ||
| Phase I | 36 | 34 | ||
| Phase II | 15 | 17 | ||
| Smoking | 36 | 35 | 1.983 | 0.983 |
| Drinking | 15 | 16 | 2.695 | 0.058 |
| Diabetes | 23 | 24 | 0.022 | 0.997 |
| Hypertension | 19 | 20 | 0.247 | 0.619 |
| Coronary heart disease | 13 | 16 | 0.342 | 0.066 |
| Chronic kidney disease | 9 | 6 | 2.206 | 0.137 |
| Chronic obstructive pulmonary disease | 7 | 7 | 0.381 | 0.537 |
| Anemia | 6 | 4 | 0.628 | 0.428 |
Note: FICAT: Ficat and Arlet classification.
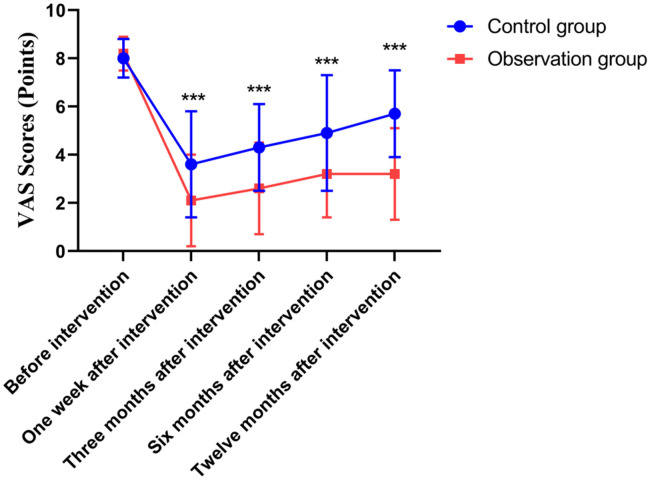
Comparison of VAS scores
Before intervention, the VAS score of the observation group was (8.2±0.7) points, while that of the control group was (8.0±0.8) points, the difference was not significant. After one week, 3 months, 6 months, and 12 months of intervention, the VAS scores of both groups decreased compared to before treatment, and the cores at each time point in the observation group were all significantly lower than those in the control group (all P<0.05) (Figure 1).
Figure 1.
Comparison of VAS scores between the two groups. ***P<0.001, compared with the control group.
Comparison of Harris hip joint scores
The mean Harris hip joint scores before intervention was 56.68±7.6 in the observation group and 55.6±6.9 in the control group (P=0.757). However, the mean Harris hip joint scores post-operatively at one week, 3 months, 6 months, and 12 months in the observation group were 78.68±5.6, 84.3±3.3, 89.3±5.3, and 93.3±3.1, respectively, and those in the control group were 60.6±4.9, 65.1±3.2, 68.3±4.2, and 72.47±2.3, respectively. The Harris hip joint scores increased significantly as compared to that before the intervention in both groups; and the observation group exhibited significantly higher scores than the control group at each time point (P=0.045, P=0.015, P=0.006, and P=0.003) (Table 2).
Table 2.
Comparison of Harris hip joint scores between the two groups
| Control group (n=50) | Observation group (n=51) | T | P | |
|---|---|---|---|---|
| Before intervention | 55.6±6.9 | 56.68±7.6 | 0.562 | 0.757 |
| One week after intervention | 60.6±4.9 | 78.68±5.6 | 6.697 | 0.045 |
| Three months after intervention | 65.1±3.2 | 84.3±3.3 | 8.984 | 0.015 |
| Six months after intervention | 68.3±4.2 | 89.3±5.3 | 9.756 | 0.006 |
| Twelve months after intervention | 72.47±2.3 | 93.3±3.1 | 10.628 | 0.003 |
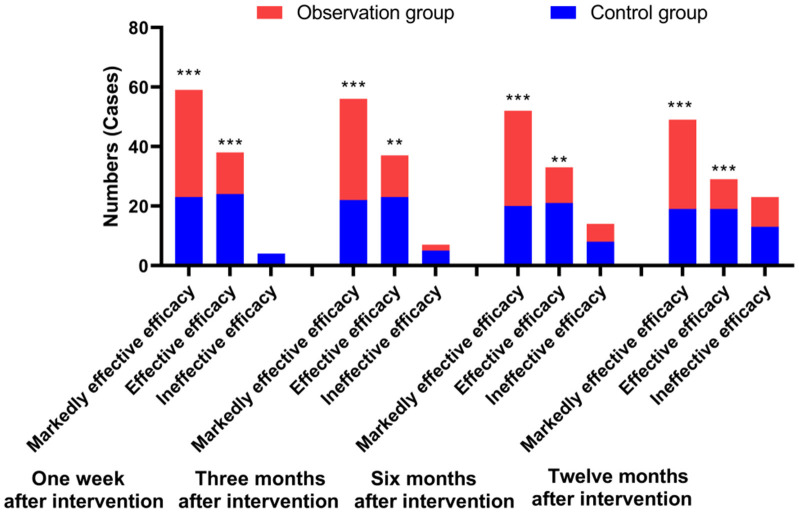
Comparison of therapeutic effects
After one week, 3, 6 and 12 months of intervention, the treatment efficacy in the two groups of patients was evaluated. The results revealed the effective rate in the observation group was significantly higher than that in the control group at each time point (97.5% VS. 88%, 96.1% VS. 87%, 94% VS. 80%, and 90% VS. 78%, all P<0.05) (Figure 2).
Figure 2.
Comparison of therapeutic effects between the two groups. **P<0.01 and ***P<0.001, compared with the control group.
Comparison of incidence of complications
A comparison of incidence of complications between the observation and control groups is summarized in Table 3. The results showed that when compared to the control group, the observation group had a lower incidence of complications (4% VS. 11.8%); however, the difference was not significant (P=0.11).
Table 3.
Comparison of incidence of complications between the two groups
| Observation group (n=51) | Control group (n=50) | Χ2 | P | |
|---|---|---|---|---|
| Lower limb discomfort or fatigue | 2 | 6 | 0.5 | 0.11 |
| Infection | 0/0.00 | 0/0.00 | - | - |
| Bone marrow ischemic damage | 0/0.00 | 0/0.00 | - | - |
| Genital femoral neuritis | 0/0.00 | 0/0.00 | - | - |
| Total incidence rate | 2 | 6 | 0.5 | 0.11 |
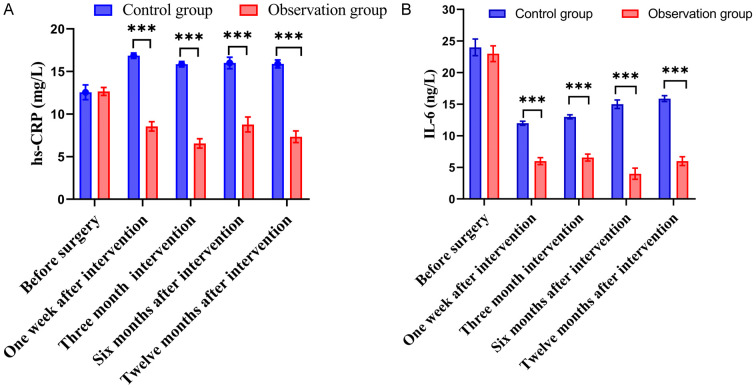
Comparison of inflammatory factors
Using ELISA, the serum levels of hsCRP and IL-6 were measured in the patients of the two groups before and after treatments. The two groups were comparable in the levels of hsCRP and IL-6 before intervention. However, after intervention, the observation group exhibited significantly lower levels of hsCRP and IL-6 than the control group at each time point (all P<0.001) (Figure 3).
Figure 3.
Comparison of inflammatory factors between the two groups. A. hs-CRP; B. IL-6. Note: hs-CRP: High-sensitivity C-reactive protein, IL-6: Interleukin-6. ***P<0.001, compared with the control group.
Discussion
Lumbar sympathetic ganglion radiofrequency combined with anhydrous ethanol can effectively alleviate pain in patients with osteonecrosis of the femoral head (ONFH). Avascular necrosis of the femoral head is a challenging condition to manage, as it can cause severe pain and disability in affected individuals. Traditional treatments such as medication, physical therapy, and surgery may not always provide adequate pain relief or address the underlying cause of the condition [16,17]. In this context, the lumbar sympathetic ganglion radiofrequency combined with anhydrous ethanol offers a promising alternative for pain management. This approach targets the lumbar sympathetic ganglion, a cluster of nerves located near the spine that plays a role in transmitting pain signals [18]. The procedure involves inserting electrodes around the lumbar sympathetic ganglion and using the heat generated by high-frequency current to destroy the conduction function of the ganglion; in the meanwhile, anhydrous ethanol, a substance with neurotoxicity that can damage the structure and function of nerve cells, is injected to reduce the perception of pain. This method is used for treating chronic pain such as lumbar disc herniation, lumbar degenerative changes, lumbar nerve root pain, and lumbar spinal stenosis [19-21]. However, there is currently no research on the application of lumbar sympathetic ganglion radiofrequency combined with anhydrous ethanol in patients with ONFH.
Lumbar sympathetic ganglion radiofrequency combined with anhydrous ethanol can significantly improve the Harris hip score in patients with ONFH. The reason for this improvement lies in the fact that lumbar sympathetic ganglion radiofrequency can effectively relieve pain and inflammation in the hip joint [22-24]. Lumbar sympathetic ganglion radiofrequency can disrupt the transmission of pain signals from the hip joint to the brain, thereby reducing pain and discomfort in the affected area [25].
Lumbar sympathetic ganglion radiofrequency combined with anhydrous ethanol can significantly improve the knee joint function of patients with femoral head necrosis. The reason for this improvement lies in the fact that lumbar sympathetic ganglion radiofrequency can effectively block the sympathetic nerve fibers that innervate the knee joint, thereby reducing pain and inflammation in the joint [26]. Anhydrous ethanol, when injected into the lumbar sympathetic ganglion, can further enhance the nerve blockage effect and provide longer-lasting pain relief [27]. The mechanism behind this treatment involves interrupting the transmission of pain signals from the knee joint to the brain by blocking the sympathetic nerve fibers. This helps reduce pain perception and inflammation in the joint, allowing for improved mobility and function [28]. Additionally, the use of anhydrous ethanol can cause degeneration of the nerve fibers, leading to a more prolonged pain relief effect.
Additionally, in our study, we found that the lumbar sympathetic ganglion radiofrequency combined with anhydrous ethanol significantly decreased the inflammatory reaction in patients with femoral head necrosis. Studies have shown that radiofrequency combined with anhydrous ethanol can reduce the inflammatory reaction in the sympathetic nerve denervation area, decrease the adrenergic release in the dorsal root ganglion, inhibit sympathetic activity by stimulating α2-adrenergic receptors and/or upregulating α2-adrenoceptors, inhibit spinal microglia activation and reduce the expression of inflammatory cytokines (IL-1β, IL-6, and TNF-α) [29]. Radiofrequency of the lumbar sympathetic ganglion can disrupt the abnormal sympathetic nerve activity, which helps to improve local blood circulation and microcirculation [30]. This, in turn, can alleviate the ischemia and hypoxia state in the femoral head region. At the same time, anhydrous ethanol has a certain cytotoxic effect. When used in combination with radiofrequency, it can further act on the lesion site, helping to reduce the activity of inflammatory cells and the release of inflammatory mediators [31]. By inhibiting the inflammatory response, it can slow down the progression of inflammation and reduce the damage caused by inflammation to the femoral head tissue. However, the mechanisms of inflammatory cytokine blockade for pain relief are complex and need to be further studied.
Interestingly, the combined use of radiofrequency of the lumbar sympathetic ganglion and anhydrous ethanol improves the clinical treatment efficiency in patients with ONFH. Radiofrequency of the lumbar sympathetic ganglion can disrupt the abnormal sympathetic nerve activity. By regulating the sympathetic nerve function, it helps to improve local blood circulation in the femoral head region [32]. This can enhance the delivery of nutrients and oxygen to the necrotic area, promoting tissue repair and regeneration. Furthermore, the combined approach may have a synergistic effect. The radiofrequency treatment lays the foundation for improving blood supply [33], and the administration of anhydrous ethanol can strengthen the therapeutic effect on pain, jointly enhancing the overall clinical treatment outcome. It can slow down the progression of the disease, relieve pain, and improve the patient’s quality of life and prognosis.
Our study does have a few limitations. First, as a retrospective study, it may have inherent biases due to the nature of data collection, such as incomplete or inaccurate records. Additionally, there may be limitations in generalizability, as the sample size and specific patient characteristics of the retrospective analysis may not fully represent the entire population of femoral head necrosis patients. Furthermore, the lack of a prospective controlled trial means that the results may not be as conclusive and reliable as those from a well-designed perspective study. Therefore, multi center large sample study is needed for further verification.
In conclusion, the treatment of avascular necrosis of the femoral head with lumbar sympathetic ganglion radiofrequency combined with anhydrous ethanol provides an effective method for improving blood supply to the femoral head, relieving pain, and demonstrating good therapeutic effects. It also has good safety, as it does not affect the conduction function of lower limb sensation and motor nerves, making it easily accepted by patients.
Acknowledgements
This work was supported by Hebei Medical Science Research Project (No. 20220666).
Disclosure of conflict of interest
None.
References
- 1.Huang TH, Liu HC, Yeh TC, Hou JY, Lin CY. Osteonecrosis (avascular necrosis) of knee and tibia. J Pediatr. 2020;217:210–210. e1. doi: 10.1016/j.jpeds.2019.10.009. [DOI] [PubMed] [Google Scholar]
- 2.Fan XL, Wang WT, Wang J, Xiao R. Current management of avascular necrosis of the metacarpal head: a comprehensive literature review. Int J Surg. 2023;109:1509–1517. doi: 10.1097/JS9.0000000000000377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lu Y, Chen X, Lu X, Sun C, Li M, Chen G, Long Z, Gao Y, Zhang H, Huang M, Ji C, Fan H, Liu D, Hao Y, Wang H, Zhang L, Zhang H, Lu J, Wang Z, Li J. Reconstructing avascular necrotic femoral head through a bioactive β-TCP system: from design to application. Bioact Mater. 2023;28:495–510. doi: 10.1016/j.bioactmat.2023.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wells ME, Dunn JC. Pathophysiology of avascular necrosis. Hand Clin. 2022;38:367–376. doi: 10.1016/j.hcl.2022.03.011. [DOI] [PubMed] [Google Scholar]
- 5.Chen S, Fu K, Cai Q, Feng Y, He H, Gao Y, Zhu Z, Jin D, Sheng J, Zhang C. Development of a risk-predicting score for hip preservation with bone grafting therapy for osteonecrosis. iScience. 2024;27:109332. doi: 10.1016/j.isci.2024.109332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Okike K, Chan PH, Prentice HA, Paxton EW, Burri RA. Association between uncemented vs cemented hemiarthroplasty and revision surgery among patients with hip fracture. JAMA. 2020;323:1077–1084. doi: 10.1001/jama.2020.1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sohatee MA, Ali M, Khanduja V, Malviya A. Does hip preservation surgery prevent arthroplasty? Quantifying the rate of conversion to arthroplasty following hip preservation surgery. J Hip Preserv Surg. 2020;7:168–182. doi: 10.1093/jhps/hnaa022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ossendorff R, Thimm D, Wirtz DC, Schildberg FA. Methods of conservative intra-articular treatment for osteoarthritis of the hip and knee. Dtsch Arztebl Int. 2023;120:575–581. doi: 10.3238/arztebl.m2023.0154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jildeh TR, Abbas MJ, Buckley P, Okoroha KR. The use of biologics for hip preservation. Curr Rev Musculoskelet Med. 2021;14:145–154. doi: 10.1007/s12178-021-09695-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tao JC, Huang B, Wang TT, Xie KY, He QL, Ni HD, Zhu JJ, Lu YP, Zhang L, Yao M. Observation on the efficacy of CT-guided lumbar sympathetic chemical destructive block in the treatment of cold sensation of limbs. Zhonghua Yi Xue Za Zhi. 2020;100:2586–2590. doi: 10.3760/cma.j.cn112137-20200513-01525. [DOI] [PubMed] [Google Scholar]
- 11.Zhang JH, Deng YP, Geng MJ. Efficacy of the lumbar sympathetic ganglion block in lower limb pain and its application prospects during the perioperative period. Ibrain. 2022;8:442–452. doi: 10.1002/ibra.12069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Naber J, Lee N, Kapural L. Clinical efficacy assessment of cooled radiofrequency ablation of the hip in patients with avascular necrosis. Pain Manag. 2019;9:355–359. doi: 10.2217/pmt-2018-0083. [DOI] [PubMed] [Google Scholar]
- 13.Karaoğlu SŞ, Sari S, Ekin Y, Özkan Y, Aydin ON. The effect of conventional radiofrequency thermocoagulation of femoral and obturator nerves’ articular branches on chronic hip pain: a prospective clinical study. Pain Med. 2024;25:444–450. doi: 10.1093/pm/pnae016. [DOI] [PubMed] [Google Scholar]
- 14.Goudman L, Pilitsis JG, Billet B, De Vos R, Hanssens K, Billot M, Roulaud M, Rigoard P, Moens M. The level of agreement between the numerical rating scale and visual analogue scale for assessing pain intensity in adults with chronic pain. Anaesthesia. 2024;79:128–138. doi: 10.1111/anae.16151. [DOI] [PubMed] [Google Scholar]
- 15.Goh GS, Liow MHL, Chen JY, Tay DK, Lo NN, Yeo SJ. The patient acceptable symptom state for the knee society score, oxford knee score and short form-36 following unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2023;31:1113–1122. doi: 10.1007/s00167-021-06592-x. [DOI] [PubMed] [Google Scholar]
- 16.Bothorel H, Pernoud A, Christofilopoulos P. Translation and cross-cultural adaptation into french of the harris hip score and the modified harris hip score. Patient Relat Outcome Meas. 2024;15:81–91. doi: 10.2147/PROM.S439707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lei H, Zhou Z, Liu L, Gao C, Su Z, Tan Z, Feng P, Liu M, Zhou C, Fan Y, Zhang X. Icariin-loaded 3D-printed porous Ti6Al4V reconstruction rods for the treatment of necrotic femoral heads. Acta Biomater. 2023;169:625–640. doi: 10.1016/j.actbio.2023.07.057. [DOI] [PubMed] [Google Scholar]
- 18.Ding Y, Yao P, Li H, Zhao R, Zhao G. Evaluation of combined radiofrequency and chemical blockade of multi-segmental lumbar sympathetic ganglia in painful diabetic peripheral neuropathy. J Pain Res. 2018;11:1375–1382. doi: 10.2147/JPR.S175514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Florek R, Sheehan C, Alessi F. Percutaneous lumbar sympathectomy: technique and clinical outcome review. J Vasc Interv Radiol. 2013;24:S135. [Google Scholar]
- 20.Kulkarni KR, Kulkarni RM. Study of chemical neurolysis, radiofrequency ablation and combined radiofrequency with chemical neurolysis of lumbar sympathetic ganglion in peripheral vascular diseases of the lower limbs. Glob J Anes & Pain Med. 2020;3:272–80. [Google Scholar]
- 21.Park AW, Hwan Baek J. Radiofrequency ablation therapy for large benign thyroid nodules. Mayo Clin Proc. 2018;93:1327–1328. doi: 10.1016/j.mayocp.2018.05.007. [DOI] [PubMed] [Google Scholar]
- 22.Zacharias NA, Karri J, Garcia C, Lachman LK, Abd-Elsayed A. Interventional radiofrequency treatment for the sympathetic nervous system: a review article. Pain Ther. 2021;10:115–141. doi: 10.1007/s40122-020-00227-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gunduz OH, Kenis-Coskun O. Ganglion blocks as a treatment of pain: current perspectives. J Pain Res. 2017;10:2815–2826. doi: 10.2147/JPR.S134775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhu Y, Jin Z, Zhang Y, Jiang B, Yan L, Tian X, Zhang M, Luo Y. Anhydrous ethanol improves efficiency of radiofrequency ablation for the treatment of benign thyroid nodules: a prospective randomized controlled trial. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2020;42:331–337. doi: 10.3881/j.issn.1000-503X.11512. [DOI] [PubMed] [Google Scholar]
- 25.Zhang L, Qiu Y, Zhao W, Wang X. Ultrasound-guided lumbar sympathetic ganglion block: a visual teaching method. Asian J Surg. 2022;45:2382–2383. doi: 10.1016/j.asjsur.2022.05.172. [DOI] [PubMed] [Google Scholar]
- 26.Gazioğlu Türkyılmaz G, Rumeli Ş. The effect of consecutive facet medial branch radiofrequency denervation and dorsal root ganglion pulse radiofrequency therapy on lumbar facet joint pain. Agri. 2023;35:220–227. doi: 10.14744/agri.2022.42713. [DOI] [PubMed] [Google Scholar]
- 27.Jang JN, Park S, Park JH, Song Y, Kim YU, Kim DS, Sohn JE, Park S. Output current and efficacy of pulsed radiofrequency of the lumbar dorsal root ganglion in patients with lumbar radiculopathy: a prospective, double-blind, randomized pilot study. Pain Physician. 2023;26:E797–E804. [PubMed] [Google Scholar]
- 28.Jang JN, Park S, Park JH, Song Y, Choi S, Kim YU, Park S. Comparison of efficacy according to voltage of pulsed radiofrequency treatment to lumbar dorsal root ganglion in patient with lumbar radiculopathy: pilot study. Medicine (Baltimore) 2023;102:e33617. doi: 10.1097/MD.0000000000033617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhu Y, Zhang M, Jin Z, Tian X, Zhang Y, Xie F, Song Q, Yan L, Jiang B, Tang J, Luo Y. Solid benign thyroid nodules (>10 ml): a retrospective study on the efficacy and safety of sonographically guided ethanol ablation combined with radiofrequency ablation. Int J Hyperthermia. 2020;37:157–167. doi: 10.1080/02656736.2020.1717647. [DOI] [PubMed] [Google Scholar]
- 30.Li Z, Zhang K, Lin SM, Mi DH, Cao N, Wen ZZ, Li ZX. Radiofrequency ablation combined with percutaneous ethanol injection for hepatocellular carcinoma: a systematic review and meta-analysis. Int J Hyperthermia. 2017;33:237–246. doi: 10.1080/02656736.2016.1237681. [DOI] [PubMed] [Google Scholar]
- 31.Li WD, Ding XY, Sun W, Guo XD, Sun SS, Shen YJ, Li L, Li W, Chen JL. CT-guided percutaneous chemical ablation combined with radiofrequency ablation for hepatocellular carcinomas in high-risk locations: lobaplatin vs. ethanol. Am J Transl Res. 2022;14:6726–6736. [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang JH, Deng YP, Geng MJ. Efficacy of the lumbar sympathetic ganglion block in lower limb pain and its application prospects during the perioperative period. Ibrain. 2022;8:442–452. doi: 10.1002/ibra.12069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Marliana A, Yudianta S, Subagya DW, Setyopranoto I, Setyaningsih I, Tursina Srie C, Setyawan R, Rhatomy S. The efficacy of pulsed radiofrequency intervention of the lumbar dorsal root ganglion in patients with chronic lumbar radicular pain. Med J Malaysia. 2020;75:124–129. [PubMed] [Google Scholar]