Abstract
Introduction
Advances in treatment have transformed cancer from a fatal to a chronic illness. This requires healthcare professionals, particularly nurses, to have advanced knowledge and collaborative skills. However, challenges persist in implementing patient-centered care in the context of evolving treatment complexity.
Objectives
This study aimed to clarify nurses’ support practices in providing cancer pharmacotherapy at a university hospital in Japan and compare these practices based on nurses’ years of experience.
Methods
A questionnaire survey was conducted from February to April 2023 among 430 nurses involved in provision of cancer pharmacotherapy at a Japanese university hospital. Nurses were asked about the types of support they provided during care for patients undergoing cancer pharmacotherapy. Nurses’ cancer pharmacotherapy support practices were extracted using factor analysis, and differences in support scores by years of experience were examined.
Results
Responses were received from 184 nurses (42.8% response rate). Three support factors were identified: “Providing patient-centered cancer pharmacotherapy,” “Management of continued cancer pharmacotherapy treatment,” and “Assessment of and response to physical symptoms.” Scores for “Providing patient-centered cancer pharmacotherapy” were significantly lower than those for the other two factors (p < .001). The group with ≥10 years of nursing experience had statistically significantly lower practice scores than those with 4–9 years of experience.
Conclusions
Enhancing nursing education and interprofessional collaboration are crucial to overcome barriers to patient-centered cancer care. Continuous learning opportunities are essential to adapt to evolving cancer treatment protocols and ensure delivery of patient-centered care, particularly for experienced nurses.
Keywords: cancer drug therapy, nurses, questionnaire survey, university hospital
Introduction
Recent developments in medical technology have enabled the early detection and treatment of cancer, and the 5-year survival rate for patients with cancer has improved globally (Challinor et al., 2020; Sant et al., 2001). This means perceptions of cancer have changed from a deadly to a chronic disease (Takahashi, 2016, 2023). Advances in cancer treatment and the increased complexity of treatment are attributable to the widespread use of outpatient chemotherapy (McKenzie et al., 2011; Tewes et al., 2021) and the emergence of molecular target drugs and immune checkpoint inhibitors (Dine et al., 2017; Peterson & Steele-Moses, 2016). Therefore, healthcare professionals are required to have up to date knowledge and adopt interprofessional collaborative approaches.
Review of Literature
Nurses often administer drugs in cancer pharmacotherapy; therefore, they require a wide range of knowledge and skills (Korhan et al., 2017; Luokkamaki et al., 2021). Factors such as extravascular leakage and side effects may prevent treatment continuation (Chfiri et al., 2022; Coolbrandt et al., 2018; Kimmel et al., 2018) and cause distress for patients because of further injuries in addition to their cancer. Therefore, observation of physical symptoms and drug administration are among nurses’ key roles. Nurses also provide information about the impact of drugs on patients’ daily lives and any necessary precautions based on knowledge of drug characteristics and the patient's treatment plan; this means they play a key role in the safe and secure implementation of cancer pharmacotherapy (Coyne et al., 2019).
Previous studies reported that nurses observed patients’ physical changes over time and provided appropriate advice and guidance based on patients’ needs (Casanovas Blanco, 2019; Mumtaz et al., 2022; Zumstein-Shaha et al., 2020). A systematic review found that nurses’ interventions during cancer pharmacotherapy could improve patients’ quality of life and physical well-being (Rodríguez-Matesanz et al., 2022). Behavioral interventions offered by nurses for patients undergoing cancer pharmacotherapy were shown to provide relief for side effects of anticancer drugs such as anticipatory nausea and vomiting (Hunter et al., 2020). These findings suggest that evidence-based practices could ensure high quality care is provided for patients undergoing cancer pharmacotherapy treatment.
The development of new drugs in cancer pharmacotherapy has changed the standard care provided (Michaeli et al., 2023). Previous studies reported that nurses experienced difficulties with knowledge and skills related to cancer treatment (Ko & Kiser-Larson, 2016; Sato et al., 2014). Miyashita et al. (2014) surveyed nurses at a university hospital in Japan and found they experienced high levels of difficulties in communicating with patients and families, difficulties with system and community collaboration, and difficulties related to their own knowledge and skills. Therefore, nurses need to acquire and update sufficient knowledge and skills, especially as cancer pharmacotherapy is rapidly evolving.
Medication administration errors have been associated with nurses’ educational background and years of experience (Kerari & Innab, 2021). Similarly, nurses’ years of experience could make a difference in their ability to support patients and safely administer medication in cancer pharmacotherapy. Although a previous study identified difficulties with common items across departments and divisions in cancer nursing (Miyashita et al., 2014), no studies quantitatively identified individual nurses’ practices in cancer pharmacotherapy, or compared their practices by nurses’ years of experience.
The purpose of this study was to describe the support provided to patients by nurses involved in cancer pharmacotherapy at a university hospital and compare nurses’ practices based on their years of experience.
Methods
Study Design
We used a descriptive quantitative cross-sectional research design with data collected via both web- and paper-based surveys to explore the reality of patient support for cancer pharmacotherapy and related factors at a regional cancer treatment cooperation base hospital in Japan. This study followed the STROBE guideline.
Setting and Participants
The study setting was a university hospital in the Kanto region of Japan (Hospital A), a regional cancer treatment cooperation base hospital. Inclusion criteria of participants were registered nurses working in the wards and outpatient departments where pharmacotherapy regimens were registered at Hospital A. Nurses working in unit-based departments (e.g., intensive care unit, orthopedic wards, cardiology, psychiatric ward, COVID-19 managed ward, and operating rooms) were excluded due to the specialized nature of care. Also, the study excluded nurses on extended leave (e.g., maternity leave, sick leave).
We used a convenience sampling method to recruit participants. The questionnaire was distributed to eligible nurses (n = 430) at Hospital A from February to April 2023. Participants were informed that withdrawal from the study would not affect their work evaluation and voluntarily participated in this study.
Variables
Participants were asked about their nursing practices with cancer pharmacotherapy patients. Questionnaire items were developed for this study that covered the general content expected of nurses when providing cancer pharmacotherapy, regardless of the type of cancer.
Draft questionnaire items were developed with reference to the Manual of Cancer Drug Therapy and Biologic Therapy (revised June 2022), which was based on the latest evidence (Japanese Society of Cancer Nursing et al., 2023; Japanese Society of Medical Oncology, 2023, 2024; National Cancer Center Hospital, 2018) and currently used in Hospital A. This manual had been designed to be accessible to all professionals involved in cancer pharmacotherapy at Hospital A, regardless of their job title. It covered basic information on cancer pharmacotherapy, including the roles and actions of physicians, nurses, and pharmacists, how to make treatment decisions, and the regimen ordering system. The manual also described the types of drugs used in chemotherapy, how to administer these drugs, observation points during drug administration, how to deal with extravascular leakage and drug hypersensitivity reactions, and the use of observation and recording sheets in the hospital.
Based on the roles and actions of nurses described in this manual (Supplemental File 1), draft questionnaire items were developed by a nurse certified in cancer chemotherapy nursing, a certified nurse specialist in cancer nursing, a deputy nursing manager, a frontline nurse manager in the outpatient chemotherapy unit, and a university faculty member with expertise in cancer nursing. The research team members then reviewed the candidate items’ face validity and developed 18 items for this study (Supplemental File 2).
The instructional statement for the support section of the survey was: “This section asks you about the support you provide to patients undergoing cancer drug therapy and the degree to which you give patients each support type.” Participants were asked to rate each item on a 5-point scale (0 = not applicable, 1 = never, 2 = rarely, 3 = occasionally, and 4 = always). While these steps were taken to ensure the content validity and validity of the scale, it should be noted that full psychometric validation has not yet been completed.
The complete questionnaire, including all 18 items and the demographic data collection section, is provided in Supplemental File 3. Demographic data collected included age, educational background, and years of experience as a nurse and in the current department.
Data Collection
The Microsoft Forms online survey platform and a paper-based questionnaire were used for data collection in this study. Research request forms with a QR code for the web survey and paper-based questionnaires were distributed by the ward nurse manager of Hospital A to nurses in each department. Participants could choose to respond either via the online survey or on paper, depending on their preferences. Completed paper-based questionnaires were posted in collection boxes located in each department.
Statistical Analyses
Descriptive statistics were calculated for participants’ characteristics. The frequency of each response option was calculated for the 18 support items for patients undergoing cancer pharmacotherapy. Next, exploratory factor analysis using maximum likelihood with Promax rotation was conducted to identify items with commonality as the support provided by nurses after excluding cases with responses of “Not applicable.” Cronbach's alpha was calculated to assess the reliability of the scale.
Multiple comparisons between the identified factors using Wilcoxon's signed rank test were conducted to determine the types of support that were provided to patients undergoing cancer pharmacotherapy. In addition, nurses were divided into three groups based on years of experience: <3 years, 4–9 years, and ≥10 years. The support scores were compared with multiple comparisons using Mann–Whitney's U-test. RStudio software (version 2023.06.1+524) for windows was used for the analyses, with the significance level set at 5%.
Ethical Considerations
This study was approved by the Institutional Ethics Review Board of the XXXX University. Participants were informed about the purpose and methods of the study in written form, along with the voluntary nature of their participation in the study and how their personal data would be protected. A section requesting consent to participate in the study was placed at the beginning of the questionnaire, and only cases where consent was obtained were included in the analyses.
Results
Demographic Data
Overall, 430 questionnaires were distributed and 184 responses were received; 128 via the web and 56 in paper form (valid response rate: 42.8%). Half of the participants were aged in their 20s and 70.7% had a bachelor's degree (Table 1). The largest proportion of participants (34.8%) had more than 10 years of nursing experience, and 43.5% had <3 years of experience in their current department.
Table 1.
Demographic Data.
| (N = 184) | ||
|---|---|---|
| n | % | |
| Age | ||
| 20s | 92 | 50.0 |
| 30s | 47 | 25.5 |
| 40s | 31 | 16.8 |
| Over 50 | 14 | 7.6 |
| Education | ||
| Vocational and junior colleges | 50 | 27.2 |
| Bachelor's degree | 130 | 70.7 |
| Graduate degree | 2 | 1.1 |
| Years of experience as a clinical nurse | ||
| Below 1 | 18 | 9.8 |
| 1~3 | 42 | 22.8 |
| 4~5 | 17 | 9.2 |
| 6~9 | 43 | 23.4 |
| Above 10 | 64 | 34.8 |
| Years of experience working in the unit | ||
| Below 1 | 36 | 19.6 |
| 1~3 | 80 | 43.5 |
| 4~5 | 30 | 16.3 |
| 6~9 | 29 | 15.8 |
| Above 10 | 9 | 4.9 |
| Settings | ||
| Inpatient | 158 | 85.9 |
| Outpatient | 26 | 14.1 |
Note: cases with missing values were excluded.
Extent of Support Provided to Patients Receiving Cancer Pharmacotherapy
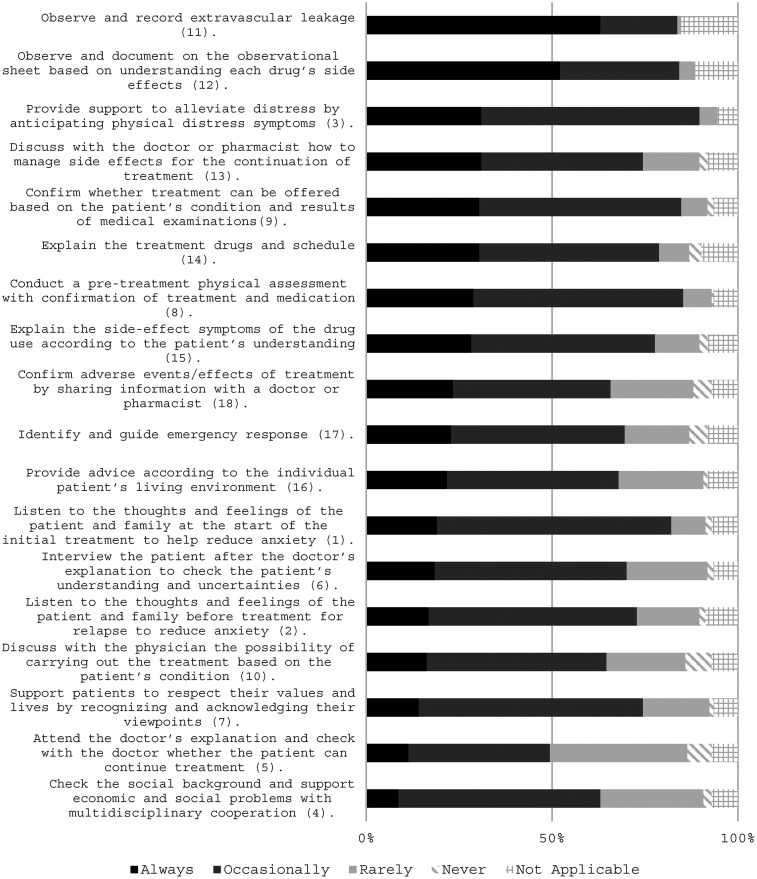
The type of support provided to patients (18 items) and extent of support delivery is shown in Figure 1. Two items that were answered as “Always” by more than 50% of participants were “Observe and record extravascular leakage” (63.0%) and “Observe and document on the observational sheet based on understanding each drug's side effects” (52.2%).
Figure 1.
Contents of support and extent of delivery.
For 17 items, the combined percentage of “Always” and “Occasionally” responses for each item was more than 50%. Four items had relatively high percentages of “Never” and “Rarely” responses: “Attend the doctor's explanation and check with the doctor whether the patient can continue treatment” (43.5%), “Check the social background and support economic and social problems with multidisciplinary cooperation” (29.9%), “Discuss with the physician the possibility of carrying out the treatment based on the patient's condition” (28.3%), and “Confirm adverse events/effects of treatment by sharing information with a doctor or pharmacist” (27.2%).
Scoring the Support Provided to Patients Undergoing Cancer Pharmacotherapy
Table 2 shows the results of the 18-item exploratory factor analysis. Three factors were extracted based on factor loadings of 0.4 or higher. The first factor was labeled “Providing patient-centered cancer pharmacotherapy” as it indicated the degree to which the nurse delivered patient-centered cancer pharmacotherapy. Factor two addressed “Management of continued cancer pharmacotherapy treatment,” which reflected the degree to which the nurse managed patients’ continuous cancer pharmacotherapy. Factor three was labeled “Assessment of and response to physical symptoms” as it indicated the assessment of and response to physical symptoms such as side effects.
Table 2.
Results of the Exploratory Factor Analysis.
| Factor loadings | ||||
|---|---|---|---|---|
| I | Ⅱ | III | ||
| Total 18 items α = 0.92 | ||||
| Providing patient-centered cancer pharmacotherapy (α = 0.85) | ||||
| 1 | Listen to the thoughts and feelings of the patient and family at the start of the initial treatment to help reduce anxiety. | 0.719 | −0.257 | 0.313 |
| 2 | Listen to the thoughts and feelings of the patient and family before treatment for relapse to reduce anxiety. | 0.869 | −0.124 | 0.034 |
| 4 | Check the social background and support economic and social problems with multidisciplinary cooperation. | 0.615 | 0.179 | −0.185 |
| 5 | Attend the doctor's explanation and check with the doctor whether the patient can continue treatment. | 0.613 | 0.177 | −0.161 |
| 7 | Support patients to respect their values and lives by recognizing and acknowledging their viewpoints. | 0.580 | 0.129 | 0.073 |
| 6 | Interview the patient after the doctor's explanation to check the patient's understanding and uncertainties. | 0.479 | 0.042 | 0.201 |
| 10 | Discuss with the physician the possibility of carrying out the treatment based on the patient's condition. | 0.499 | 0.169 | −0.049 |
| Management of continued cancer pharmacotherapy treatment (α = 0.87) | ||||
| 14 | Explain the treatment drugs and schedule. | −0.071 | 0.575 | 0.373 |
| 15 | Explain the side-effect symptoms of the drug use according to the patient's understanding. | −0.142 | 0.706 | 0.312 |
| 16 | Provide advice according to the individual patient's living environment. | 0.281 | 0.734 | −0.149 |
| 17 | Identify and guide emergency response. | 0.003 | 0.774 | −0.014 |
| 18 | Confirm adverse events/effects of treatment by sharing information with a doctor or pharmacist. | 0.280 | 0.612 | −0.104 |
| 13 | Discuss with the doctor or pharmacist how to manage side effects for the continuation of treatment. | −0.049 | 0.395 | 0.348 |
| Assessment of and response to physical symptoms (α = 0.82) | ||||
| 11 | Observe and record extravascular leakage. | −0.108 | 0.020 | 0.773 |
| 12 | Observe and document on the observational sheet based on understanding each drug's side effects. | −0.100 | 0.065 | 0.742 |
| 3 | Provide support to alleviate distress by anticipating physical distress symptoms. | 0.365 | 0.028 | 0.447 |
| 8 | Conduct a pretreatment physical assessment with confirmation of treatment and medication. | 0.406 | −0.106 | 0.475 |
| 9 | Confirm whether treatment can be offered based on the patient's condition and results of medical examinations. | 0.344 | 0.009 | 0.429 |
| Proportion of variance explained (%) | 0.19 | 0.15 | 0.13 | |
| Cumulative proportion of variance explained (%) | 0.19 | 0.34 | 0.47 | |
| Interfactor correlations | I | Ⅱ | III | |
| 1.00 | 0.62 | 0.62 | ||
| 1.00 | 0.58 | |||
| 1.00 | ||||
The mean scores were 2.88 ± 0.50 for “Providing patient-centered cancer pharmacotherapy,” 3.06 ± 0.60 for “Management of continued cancer pharmacotherapy treatment,” and 3.44 ± 0.41 for “Assessment of and response to physical symptoms.” Multiple comparisons showed statistically significant differences in all combinations (p < .001).
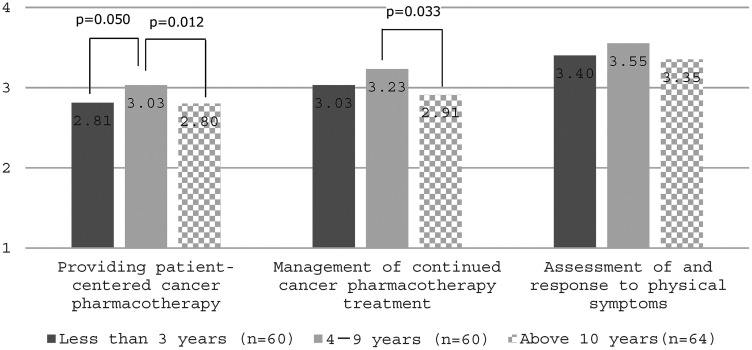
Comparison of Support by Years of Nursing Experience
Scores for support types provided to patients undergoing cancer pharmacotherapy were compared by years of nursing experience (Figure 2). Scores for “Providing patient-centered cancer pharmacotherapy” were highest for nurses with 4–9 years of experience and were statistically significantly higher than those with ≥10 years of experience (p = .012). There was also a trend for nurses with <3 years of nursing experience to have lower scores than those with 4–9 years of experience, although this was not statistically significant (p = .050). For “Management of continued cancer pharmacotherapy treatment,” scores were highest for nurses with 4–9 years of experience and were statistically significantly higher than those with ≥10 years of experience (p = .033). There were no statistically significant differences between groups for “Assessment of and response to physical symptoms.”
Figure 2.
Comparison of nursing support by years of nursing experience.
Discussion
This study quantitatively identified the practices of nonspecialized nurses in a Japanese university hospital working with patients undergoing drug therapy, regardless of the cancer type. Nurses’ practice varied by their years of experience. In particular, the low degree of implementation by nurses with more years of experience in patient-centered cancer chemotherapy highlighted a need for continuing education.
Support Provided to Patients Undergoing Cancer Pharmacotherapy
Certain side effects and complications resulting from cancer treatment may last for an extended period or become permanent. In particular, cancer pharmacotherapy requires prevention, early detection, and early treatment of drug extravasation (Kreidieh et al., 2016). Although extravascular leakage and adverse reactions are factors that can hinder the continuation of treatment (Chfiri et al., 2022; Coolbrandt et al., 2018; Kimmel et al., 2018), these events are preventable with continuous observation and early intervention. In this study, the observation of extravascular leakage and side-effect symptoms appeared to have been particularly well implemented.
In the Japanese context, barriers to nurses attending decision-making discussions with patients with cancer have been identified as lack of awareness of the need for discussion, lack of collaboration between healthcare providers, and lack of role recognition and communication (Harada & Kimura, 2021). For example, an item that was implemented by relatively few participants in our study was “Attend the doctor's explanation and confirm with the doctor whether the patient is able to receive or continue treatment.” Reasons for this finding may be a lack of awareness among professionals about the need for nurses to attend explanations, lack of coordination of informed consent opportunities for patients, and lack of communication between professional groups. However, this item could have had multiple meanings (e.g., attending the doctor's explanation, checking the patient together with the doctor), meaning the wording of the item might have influenced its lower score.
In this study, the factor covering implementation of patient-centered cancer pharmacotherapy scored lower than the other two factors. A previous study among nurses involved in cancer nursing at a university hospital reported nurses had difficulties communicating with patients and families, difficulties with their own skills, and difficulties in explaining medical conditions to patients (Miyashita et al., 2014). Another study conducted among nurses in designated cancer hospitals also reported that patient-centered care practices for older patients with cancer were not well implemented, and indicated practice-related factors included knowledge of cancer nursing and dementia (Ikeda et al., 2024). These findings suggested nurses are required to acquire knowledge about cancer pharmacotherapy and enhance their interprofessional collaborative competencies to effectively implement patient-centered cancer pharmacotherapy.
Intervention Points to Improve Care for Patients Undergoing Cancer Pharmacotherapy
Half of the participants in this study were aged in their 20s and most had a bachelor's degree, which reflects the unique characteristics nurses working in university hospitals in Japan (Miyashita et al., 2014; Sakakibara & Ikezaki, 2022; Tomotaki et al., 2020). Nurses who were involved in cancer nursing at university hospitals for <4 years reported high levels of difficulties related to communication, knowledge, and skills in cancer nursing (Miyashita et al., 2014). In this study, the group with <3 years of nursing experience tended to score lower in the implementation of patient-centered cancer pharmacotherapy than those with more nursing experience, although this was not statistically significant. This may be attributable to the need for communication with multiple professional groups and knowledge of cancer pharmacotherapy required to implement patient-centered cancer pharmacotherapy.
Globally, oncology nursing has developed markedly over the last 20 years (Challinor et al., 2020; Mak, 2019), and the first Core Curriculum for Oncology Nursing in Japan was developed in 2010 by the Japanese Society of Cancer Nursing (Japanese Society of Cancer Nursing, 2010). In this study, the low scores of nurses with ≥10 years of experience in implementing patient-centered cancer pharmacotherapy and managing continued cancer pharmacotherapy may reflect practice based on experience and few opportunities to systematically learn basic concepts and knowledge of cancer nursing. Therefore, nurses may need opportunities to learn both the basics and the latest knowledge of cancer nursing, regardless of their years of experience. A previous study showed that nurses who received continuous information and communication technology (ICT)-based education reported reduced difficulty in caring for patients with cancer (Nakamura et al., 2023). In hospitals, ICT can be used to develop education in an on-demand format to support nurses’ continuous learning. Furthermore, there has been growing interest in advanced practice nurses who have received specialized education and training in cancer nursing (Galassi et al., 2023). Improvement of the education system could also be explored; oncology nursing certified nurse specialists and certified oncology pharmacotherapy nurses taking the lead for education in the hospital setting.
Strengths and Limitations
This study had several limitations. First, this study was conducted at one university hospital, which presents challenges in generalizing the findings. However, the demographics of the study participants were similar to those reported in studies conducted at other university hospitals. Second, the reliability and validity of the scales used in this study were not fully verified. In this study, a scale to measure nursing support practices commonly implemented in wards and outpatient clinics regardless of department was developed based on a manual used in Hospital A. Although the content validity was ensured by research team members and the reliability by evaluated with Cronbach's alpha coefficient, some items were interpreted as having a double meaning; therefore, caution should be exercised in interpreting the results. Despite these limitations, the strength of this study is that it quantitatively revealed the practices of nonspecialized nurses involved in cancer chemotherapy and provided suggestions for nurse education strategies.
Further studies could consider modifying the scale items, and also assessing support practices with the scale developed by Onodera et al. (2013) to evaluate nurses’ difficulty with cancer care, which is an existing scale for a wide range of nurses involved in oncology nursing.
Implications for Practice
This quantitative study demonstrated the need to strengthen education for nurses working in cancer chemotherapy and improve interprofessional collaboration. The findings suggest that experienced nurses may be inadequately supported in delivering patient-centered cancer pharmacotherapy. Ongoing learning opportunities are important, regardless of years of experience. One key strategy is to provide educational programs tailored to nurses’ years of experience, ensuring all staff can deliver high-quality, patient-centered care in the rapidly evolving field of cancer treatment.
Conclusion
Nurses involved in cancer pharmacotherapy at Hospital A in Japan were implementing patient-centered cancer pharmacotherapy, managing ongoing cancer pharmacotherapy, and assessing and responding to patients’ physical symptoms. Although they evaluated themselves as competent in assessing and responding to physical symptoms, the implementation of patient-centered cancer pharmacotherapy remained a challenge.
Supplemental Material
Supplemental material, sj-docx-1-son-10.1177_23779608241288718 for Nurses’ Perceptions of Support in Cancer Pharmacotherapy at a University Hospital: A Descriptive Quantitative Study by Masatoshi Saiki, Yoko Fujisawa, Naoko Sakai, Nobuko Tsukahara, Yuriko Okamoto, Motohiro Sano, Junko Kusunoki, Mariko Masujima, Ikuko Sakai and Tomoko Majima in SAGE Open Nursing
Supplemental material, sj-docx-2-son-10.1177_23779608241288718 for Nurses’ Perceptions of Support in Cancer Pharmacotherapy at a University Hospital: A Descriptive Quantitative Study by Masatoshi Saiki, Yoko Fujisawa, Naoko Sakai, Nobuko Tsukahara, Yuriko Okamoto, Motohiro Sano, Junko Kusunoki, Mariko Masujima, Ikuko Sakai and Tomoko Majima in SAGE Open Nursing
Supplemental material, sj-docx-3-son-10.1177_23779608241288718 for Nurses’ Perceptions of Support in Cancer Pharmacotherapy at a University Hospital: A Descriptive Quantitative Study by Masatoshi Saiki, Yoko Fujisawa, Naoko Sakai, Nobuko Tsukahara, Yuriko Okamoto, Motohiro Sano, Junko Kusunoki, Mariko Masujima, Ikuko Sakai and Tomoko Majima in SAGE Open Nursing
Supplemental material, sj-doc-4-son-10.1177_23779608241288718 for Nurses’ Perceptions of Support in Cancer Pharmacotherapy at a University Hospital: A Descriptive Quantitative Study by Masatoshi Saiki, Yoko Fujisawa, Naoko Sakai, Nobuko Tsukahara, Yuriko Okamoto, Motohiro Sano, Junko Kusunoki, Mariko Masujima, Ikuko Sakai and Tomoko Majima in SAGE Open Nursing
Acknowledgments
We express our gratitude to the study participants for generously dedicating their valuable time to completing the questionnaires.
Footnotes
Credit Authorship Contribution Statement: Masatoshi Saiki: conceptualization, methodology, formal analysis, and writing—original draft preparation; Yoko Fujisawa: conceptualization, methodology, investigation, and writing—review and editing; Naoko Sakai: conceptualization, methodology, formal analysis, investigation, and writing—review and editing; Nobuko Tsukahara: conceptualization, investigation, and writing—review and editing; Yuriko Okamoto: conceptualization, methodology, investigation, and writing—review and editing; Motohiro Sano: conceptualization, methodology, and writing—review and editing; Junko Kusunoki: conceptualization and writing—review and editing; Mariko Masujima: conceptualization and writing—review and editing; Ikuko Sakai: conceptualization, and writing—review and editing; Tomoko Majima: conceptualization, formal analysis, investigation, project administration, and writing—review and editing.
Data Availability Statement: The participants of this study did not give written consent for their data to be shared publicly. Therefore, due to the sensitive nature of the research, supporting data is not available. The data that support the findings of this study are available from the corresponding author, Tomoko Majima, upon reasonable request.
Data Deposition: The study data cannot be publicly shared.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics Approval Statements: This study was approved by the Institutional Ethics Review Board of the Chiba University Graduate School of Nursing (#NR4-105). Participants were informed about the purpose and methods of the study in written form, along with the voluntary nature of their participation in the study and how their personal data would be protected. A section requesting consent to participate in the study was placed at the beginning of the questionnaire, and only cases where consent was obtained were included in the analyses.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Masatoshi Saiki https://orcid.org/0000-0001-6247-965X
Motohiro Sano https://orcid.org/0000-0001-7608-9695
Supplemental Material: Supplemental material for this article is available online.
References
- Casanovas Blanco M. (2019). Critical review of emergency department management of chemotherapy complications in cancer patients. European Journal of Cancer Care, 28(2), 1–15. 10.1111/ecc.12974 [DOI] [PubMed] [Google Scholar]
- Challinor J. M., Alqudimat M. R., Teixeira T. O. A., Oldenmenger W. H. (2020). Oncology nursing workforce: Challenges, solutions, and future strategies. The Lancet Oncology, 21(12), e564–e574. 10.1016/S1470-2045(20)30605-7 [DOI] [PubMed] [Google Scholar]
- Chfiri A., Karti S., Jalal A., Jaafari A., Alaoui M., Sabur S., El Harti A., Diouri M. (2022). Extravasation: Surgical management and prevention. European Journal of Medical and Health Sciences, 4(4), 22–29. 10.24018/ejmed.2022.4.4.1363 [DOI] [Google Scholar]
- Coolbrandt A., Wildiers H., Laenen A., Aertgeerts B., De Casterlé B. D., Van Achterberg T., Milisen K. (2018). A nursing intervention for reducing symptom burden during chemotherapy. Oncology Nursing Forum, 45(1), 115–128. 10.1188/18.ONF.115-128 [DOI] [PubMed] [Google Scholar]
- Coyne E., Northfield S., Ash K., Brown-West L. (2019). Current evidence of education and safety requirements for the nursing administration of chemotherapy: An integrative review. European Journal of Oncology Nursing, 41, 24–32. 10.1016/j.ejon.2019.05.001 [DOI] [PubMed] [Google Scholar]
- Dine J., Gordon R., Shames Y., Kasler M. K., Barton-Burke M. (2017). Immune checkpoint inhibitors: An innovation in immunotherapy for the treatment and management of patients with cancer. Asia-Pacific Journal of Oncology Nursing, 4(2), 127–135. 10.4103/apjon.apjon_4_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galassi A., Anwarali S., Challinor J. (2023). Global challenges and initiatives in oncology nursing education. Annals of Palliative Medicine, 12(3), 633–645. 10.21037/apm-22-1120 [DOI] [PubMed] [Google Scholar]
- Harada T., Kimura Y. (2021). Barriers to attending end of life discussions with advanced cancer patients as perceived by ward nurses. Journal of Japanese Society of Cancer Nursing, 35, 158–167. 10.18906/jjscn.35_158_harada [DOI] [Google Scholar]
- Hunter J. J., Maunder R. G., Sui D., Esplen M. J., Chaoul A., Fisch M. J., Bassett R. L., Harden-Harrison M. M., Lagrone L., Wong L., Baez-Diaz L., Cohen L. (2020). A randomized trial of nurse-administered behavioral interventions to manage anticipatory nausea and vomiting in chemotherapy. Cancer Medicine, 9(5), 1733–1740. 10.1002/cam4.2863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikeda S., Aoyanagi M., Nakaya R., Yoshimura M., Sumi N. (2024). Factors related to person-centered care for older patients with cancer and dementia in designated cancer hospitals. Cancer Nursing, 10–1097. 10.1097/NCC.0000000000001338 [DOI] [PubMed] [Google Scholar]
- Japanese Society of Cancer Nursing. (2010). Core curriculum for oncology nursing. In Japanese Society of Cancer Nursing. The Education and Research Activity Board of the Japanese Society of Cancer Nursing. https://jscn.or.jp/core/doc/panf_2010e.pdf [Google Scholar]
- Japanese Society of Cancer Nursing, Japanese Society of Medical Oncology, & Japanese Society of Pharmaceutical Oncology. (Eds.) (2023). Guidelines for the management of chemotherapy extravasation (3rd ed.). Kanehara & Co., Ltd. [Google Scholar]
- Japanese Society of Medical Oncology. (Ed.) (2023). Guidelines for cancer immunotherapy [Gan menekiryoho gaidorain] (3rd ed.). Kanehara & Co., Ltd. [Google Scholar]
- Japanese Society of Medical Oncology. (Ed.) (2024). Clinical oncology update-essentials [Shin Rinsyosyuyougaku]. Nankodo Co., Ltd. [Google Scholar]
- Kerari A., Innab A. (2021). The influence of nurses’ characteristics on medication administration errors: An integrative review. SAGE Open Nursing, 7, 1–17. 10.1177/23779608211025802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimmel J., Fleming P., Cuellar S., Anderson J., Haaf C. M. (2018). Pharmacological management of anticancer agent extravasation: A single institutional guideline. Journal of Oncology Pharmacy Practice, 24(2), 129–138. 10.1177/1078155217690924 [DOI] [PubMed] [Google Scholar]
- Ko W., Kiser-Larson N. (2016). Stress levels of nurses in oncology outpatient units. Clinical Journal of Oncology Nursing, 20(2), 158–164. 10.1188/16.CJON.158-164 [DOI] [PubMed] [Google Scholar]
- Korhan E. A., Dilemek H., Mercan S., Yilmaz D. U. (2017). Determination of attitudes of nurses in medical errors and related factors. International Journal of Caring Scaring Sciences, 10(2), 794–801. https://www.internationaljournalofcaringsciences.org/docs/17_dilemek_oroginal_10_2.pdf . [Google Scholar]
- Kreidieh F. Y., Moukadem H. A., El Saghir N. S. (2016). Overview, prevention and management of chemotherapy extravasation. World Journal of Clinical Oncology, 7(1), 87–97. 10.5306/wjco.v7.i1.87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luokkamaki S., Harkanen M., Saano S., Vehvilainen-Julkunen K. (2021). Registered nurses’ medication administration skills: A systematic review. Scandinavian Journal of Caring Sciences, 35(1), 37–54. 10.1111/scs.12835 [DOI] [PubMed] [Google Scholar]
- Mak S. S. S. (2019). Oncology nursing in Hong Kong: Milestones over the past 20 years. Asia-Pacific Journal of Oncology Nursing, 6(1), 10–16. 10.4103/apjon.apjon_46_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenzie H., Hayes L., White K., Cox K., Fethney J., Boughton M., Dunn J. (2011). Chemotherapy outpatients’ unplanned presentations to hospital: A retrospective study. Supportive Care in Cancer, 19(7), 963–969. 10.1007/s00520-010-0913-y [DOI] [PubMed] [Google Scholar]
- Michaeli D. T., Michaeli J. C., Michaeli T. (2023). Advances in cancer therapy: Clinical benefit of new cancer drugs. Aging, 15(12), 5232–5234. 10.18632/aging.204839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyashita M., Onodera M., Kumata M., Ogiri N., Asano R., Ogasawara K., Goto A., Shibata H., Syoji Y., Sengoku M., Kazuko Y., Noriko M. (2014). Difficulty with cancer care and related factors among nurses at Tohoku University Hospital Mitsunori. Palliative Care Research, 9(3), 158–166. 10.2512/jspm.9.158 [DOI] [Google Scholar]
- Mumtaz D. F., Effendy C., Haryani H. (2022). Impact of pre-chemotherapy education with audio visual methods on the self-efficacy of symptom management in patients with cancer. Journal of Cancer Education, 37(5), 1546–1552. 10.1007/s13187-021-02006-1 [DOI] [PubMed] [Google Scholar]
- Nakamura M., Zhu M., Maeda K., Toda M., Mori N. (2023). A basic survey on the learning needs of nurses caring for patients with intractable cancer in Japan based on conceptual education integrating oncology and palliative care. Journal of Cancer Education, 38(4), 1170–1176. 10.1007/s13187-022-02245-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Cancer Center Hospital, D. of N. (Ed.) (2018). Skill up on cancer chemotherapy and biotherapy nursing: Learning from National Cancer Center Japan (1st ed.). Nankodo Co., Ltd. [Google Scholar]
- Onodera M., Kumata M., Ogiri N., Asano R., Ogasawara K., Goto A., Shibata H., Syoji Y., Sengoku M., Yamauti K., Monma N., Miyashita M. (2013). Development of scale to measure nurses’ difficulty with cancer care (NDCC). Palliative Care Research, 8(2), 240–247. 10.2512/jspm.8.240 [DOI] [Google Scholar]
- Peterson J. J., Steele-Moses S. K. (2016). Update on new therapies with immune checkpoint inhibitors. Clinical Journal of Oncology Nursing, 20(4), 405–410. 10.1188/16.CJON.405-410 [DOI] [PubMed] [Google Scholar]
- Rodríguez-Matesanz I., Ambrosio L., Domingo-Oslé M., Elizondo-Rodríguez N., la Rosa-Salas V., Garcia-Vivar C. (2022). Are nursing interventions effective in improving quality of life in cancer survivors? A systematic review. Cancer Nursing, 45(1), E134–E145. 10.1097/NCC.0000000000000901 [DOI] [PubMed] [Google Scholar]
- Sakakibara N., Ikezaki S. (2022). Recognition of augmentative and alternative communication among neurology ward nurses in university hospitals. Journal of Japan Academy of Nursing Science, 42(0), 385–390. 10.5630/jans.42.385 [DOI] [Google Scholar]
- Sant M., Capocaccia R., Coleman M. P., Berrino F., Gatta G., Micheli A., Verdecchia A., Faivre J., Hakulinen T., Coebergh J. W. W., Martinez-Garcia C., Forman D., Zappone A., Oberaigner W., Storm H., Aareleid T., Mace-Lesec’h J., Chaplain G., Carli P. M., Lawrence G. (2001). Cancer survival increases in Europe, but international differences remain wide. European Journal of Cancer, 37(13), 1659–1667. 10.1016/S0959-8049(01)00206-4 [DOI] [PubMed] [Google Scholar]
- Sato K., Inoue Y., Umeda M., Ishigamori I., Igarashi A., Togashi S., Harada K., Miyashita M., Sakuma Y., Oki J., Yoshihara R., Eguchi K. (2014). A Japanese region-wide survey of the knowledge, difficulties and self-reported palliative care practices among nurses. Japanese Journal of Clinical Oncology, 44(8), 718–728. 10.1093/jjco/hyu075 [DOI] [PubMed] [Google Scholar]
- Takahashi M. (2016). Cancer survivorship: Current status of research, care, and policy in Japan. Japanese Journal of Clinical Oncology, 46(7), 599–604. 10.1093/jjco/hyw057 [DOI] [PubMed] [Google Scholar]
- Takahashi M. (2023). Cancer survivorship care: Challenges and opportunities in Japan. Japanese Journal of Clinical Oncology, 53(9), 757–763. 10.1093/jjco/hyad054 [DOI] [PubMed] [Google Scholar]
- Tewes M., Baumann F., Teufel M., Ostgathe C. (2021). Symptoms during outpatient cancer treatment and options for their management. Deutsches Arzteblatt International, 118(17), 291–297. 10.3238/arztebl.m2021.0028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomotaki A., Fukahori H., Sakai I. (2020). Exploring sociodemographic factors related to practice, attitude, knowledge, and skills concerning evidence-based practice in clinical nursing. Japan Journal of Nursing Science, 17(1), 1–9. 10.1111/jjns.12260 [DOI] [PubMed] [Google Scholar]
- Zumstein-Shaha M., Ferrell B., Economou D. (2020). Nurses’ response to spiritual needs of cancer patients. European Journal of Oncology Nursing, 48, Article 101792. 10.1016/j.ejon.2020.101792 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-son-10.1177_23779608241288718 for Nurses’ Perceptions of Support in Cancer Pharmacotherapy at a University Hospital: A Descriptive Quantitative Study by Masatoshi Saiki, Yoko Fujisawa, Naoko Sakai, Nobuko Tsukahara, Yuriko Okamoto, Motohiro Sano, Junko Kusunoki, Mariko Masujima, Ikuko Sakai and Tomoko Majima in SAGE Open Nursing
Supplemental material, sj-docx-2-son-10.1177_23779608241288718 for Nurses’ Perceptions of Support in Cancer Pharmacotherapy at a University Hospital: A Descriptive Quantitative Study by Masatoshi Saiki, Yoko Fujisawa, Naoko Sakai, Nobuko Tsukahara, Yuriko Okamoto, Motohiro Sano, Junko Kusunoki, Mariko Masujima, Ikuko Sakai and Tomoko Majima in SAGE Open Nursing
Supplemental material, sj-docx-3-son-10.1177_23779608241288718 for Nurses’ Perceptions of Support in Cancer Pharmacotherapy at a University Hospital: A Descriptive Quantitative Study by Masatoshi Saiki, Yoko Fujisawa, Naoko Sakai, Nobuko Tsukahara, Yuriko Okamoto, Motohiro Sano, Junko Kusunoki, Mariko Masujima, Ikuko Sakai and Tomoko Majima in SAGE Open Nursing
Supplemental material, sj-doc-4-son-10.1177_23779608241288718 for Nurses’ Perceptions of Support in Cancer Pharmacotherapy at a University Hospital: A Descriptive Quantitative Study by Masatoshi Saiki, Yoko Fujisawa, Naoko Sakai, Nobuko Tsukahara, Yuriko Okamoto, Motohiro Sano, Junko Kusunoki, Mariko Masujima, Ikuko Sakai and Tomoko Majima in SAGE Open Nursing