Abstract
Total Knee Arthroplasty (TKA) is a surgery that is commonly performed on older adults to improve their quality of life. However, the increasing use of knee joint prostheses has led to a rise in the incidence of Prosthetic Joint Infections (PJI) in patients after TKA. Different clinical studies have looked at the occurrence of PJI after TKA in different regions, but they have drawn varying conclusions. To better understand this topic, we conducted a meta-analysis and bibliometric study using data from multiple databases. Our research found that the estimated prevalence of PJI after TKA is approximately 1.08% across different regions, but there is still considerable variation. Additionally, our regression analysis of sub-groups shows significant differences in follow-up periods. Furthermore, our comprehensive bibliometric analysis identifies current research trends, “hotspots” related to TKA-related PJI, influential nations, organizations, and noteworthy publications. Our analysis provides valuable insights to guide future research in this area.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13018-024-05099-8.
Keywords: Periprosthetic joint infection, Total knee arthroplasty, Incidence, Epidemiology, Meta-analysis, Bibliometric analysis
Introduction
Total knee arthroplasty (TKA) is a well-established, safe, and effective procedure, widely performed in orthopedics to enhance quality of life and restore function in patients with knee arthritis [1, 2]. The growing number of knee prostheses being implanted is largely attributed to the increasing life expectancy of the elderly population and their heightened demand for an improved quality of life [3, 4]. About 1 million knee and hip replacements are performed in the U.S. each year, and that number is expected to double by 2030 [5]. In China, with nearly 110 million knee osteoarthritis patients in 2016, the potential patient population in need of TKA is huge [6]. The dramatic increase in surgical volume poses unprecedented challenges to perioperative management and postoperative rehabilitation.
The reasons for TKA surgical failure requiring revision are complex and varied and include PJI, instability, component misalignment, polyethylene or metal wear, loose cement, periprosthetic fracture, instability, or knee stiffness [7, 8]. PJI is a major contributor to TKA failure and the incidence is on the rise [9]. Although the incidence of PJI reported after TKA is in the range of 0.5-2%, the overall global burden is substantial [10]. Once PJI occurs, its consequences can be catastrophic, causing significant impacts on society, families, and individuals. Risk factors for developing PJI after TKA have been reported and include hypertension, diabetes mellitus, hyperlipidemia, nephropathy, urinary tract infection, overweight, wound complications, and poor nutritional support [11, 12]. In conclusion, diagnosing and treating PJI is particularly challenging in orthopedic practice. The complexity arises from the difficulty in accurately identifying the infection, coupled with the need for tailored treatment strategies that address both infection eradication and complications. In 2018, new diagnostic criteria for PJI were introduced internationally, improving the sensitivity and specificity of PJI diagnosis [13, 14]. The Musculoskeletal Infection Society defines the major criteria for diagnosing PJI as either the presence of two positive cultures of the same organism obtained through standard culture methods or the presence of a sinus tract with evidence of communication to the joint or direct visualization of the prosthesis. Additionally, minor criteria include several indicators such as elevated C-reactive protein, elevated D-dimer levels, and elevated erythrocyte sedimentation rate, among others, which can also support the diagnosis of PJI [13]. However, numerous clinical studies have often been inconsistent in their results, with significant variations. Therefore, more comprehensive identification of potential risk factors and the incidence of PJI is critical.
In this study, we used meta-analysis combined with bibliometrics to investigate the prevalence and potential risk factors of PJI. Meta-analysis and bibliometrics can altogether help us to systematically analyze and combine data from multiple studies, comprehensively assess the value of literature, and provide strong data support for our research [15, 16].
Method
Meta-analysis
This is a systematic review registered with the Prospero repository under the ID CRD42024527125. The search for relevant studies began at the start of the project and continued until March 2024. The search included three major medical repositories: PubMed, Embase, and Web of Science. The search terms used were “infection or infections or PJI”, “prevalence or incidence or epidemiology”, and “TKA or knee or arthroplasty”, combined with “periprosthetic or implant or prosthesis or prosthesis-related or periprosthesis-related”. There were no language restrictions during the search, and the final search was conducted on March 15, 2024.
Inclusion and exclusion criteria
Inclusion criteria: patients of any age who have undergone primary total knee arthroplasty (TKA); no restrictions on publication date; studies with large sample sizes were preferred; and the research should report the incidence of prosthetic joint infection (PJI) after primary TKA. Exclusion criteria: reviews, case studies, protocols, abstracts, personal commentaries, letters, posters, conference abstracts or laboratory-based investigations; studies without sufficient data or not accessible; and research not related to PJI patients.
Data extraction
Evaluation of study articles was based on their titles and abstracts. Abstracts and any articles without abstracts were chosen for a full-text assessment. Two researchers independently extracted data from the selected studies and cross-verified the findings to maintain the accuracy of the information. In instances of discrepancies, a third researcher was brought in to resolve the discrepancy(Table 1).
Table 1.
Characteristics of the database-based studies of PJI
| Study | Country | PJI | Primary TKA | Male PJI | Male TKA | Female PJI | Female TKA | Year | Age | Follow-up time | Data Sources | Publication Year |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yoon H.K. et al. 2023 | Korea | 34 | 7019 | 5 | / | 29 | / | 2003–2019 | 69.2 | > 12 m | Single institution | 2023 |
| Ashkenazi I. et al. 2023 | Israel | 7 | 1590 | / | / | / | / | 2011.1-2021.4 | 69.9(± 9.8) | / | Single institution | 2023 |
| Hameed D. et al. 2023 | USA | 81 | 5000 | / | / | / | / | 2015–2020 | 66 | 12–24 m | Database | 2023 |
| Stevoska S. et al. 2022 | Australia | 24 | 2666 | / | 1011 | / | 1655 | 2011–2020 | / | / | Single institution | 2022 |
| Kurtz S.M. et al. 2022 | USA | 619 | 89,837 | / | / | / | / | 2010–2017 | > 65 | 0–24 m | Database | 2022 |
| Hasenauer M.D. et al. 2022 | USA | 105 | 8462 | 56 | 3176 | 49 | 5466 | 2006–2018 | 66.9(33–95) | / | Single institution | 2022 |
| Bozzo A. et al.2022 | Canada | 1834 | 129,613 | / | 50,453 | / | 79,160 | 2002–2016 | > 50 | / | Database | 2022 |
| Yang Q.F. et al. 2021 | China | 2455 | 1,227,244 | / | / | / | / | 2005–2014 | > 18 | / | Database | 2021 |
| Baier C. et al. 2019 | Germany | 75 | 2439 | / | / | / | / | 2007–2010 | / | / | Single institution | 2019 |
| Siu K.T. et al. 2018 | China(Hong Kong) | 34 | 2543 | 10 | 539 | 24 | 2004 | 1993–2013 | 69(21–91) | / | Single institution | 2018 |
| Poultsides L.A. et al. 2018 | USA | 47 | 17,959 | / | 6525 | / | 11,434 | 2000–2009 | 68.15(12.6–96.8) | / | Database | 2018 |
| Klement M.R. et al. 2016 | USA | 7629 | 1,271,464 | / | 39,355 | / | 154,749 | 2005–2011 | / | / | Database | 2016 |
| Alp E. et al. 2016 | Turkey | 11 | 241 | / | / | / | / | 2011.4-2013.4 | 64 | / | Single institution | 2016 |
| Lee Q.J. et al. 2015 | Hongkong | 8 | 1133 | 4 | / | 4 | / | 2011–2014 | / | / | Single institution | 2015 |
| Jämsen E. et al. 2010 | Finland | 24 | 2647 | 12 | 784 | 12 | 1863 | 2002–2006 | 70 (35–97) | > 6 m | Single institution | 2010 |
| Pasticci M.B. et al. 2007 | Italy | 3 | 171 | / | 62 | / | 109 | 1997–2002 | 71(37–82) | > 24 m | Single institution | 2007 |
| Cook J.L. et al. 2007 | USA | 15 | 3013 | 7 | / | 8 | / | 1985–2004 | 67(40–79) | / | Single institution | 2007 |
| Wang FD et al. 2018 | China(Taiwan) | 178 | 10,768 | / | 3527 | / | 7241 | 2002–2014 | > 18(中位数73) | 0–36 m | Single institution | 2018 |
| Ko MS et al. 2021 | Korea | 12,474 | 560,954 | / | / | / | / | 2005–2018 | / | / | Database | 2021 |
| Jung P et al. 2017 | New Zealand | 44 | 9481 | 31 | 4348 | 13 | 5085 | 2013–2015 | 70 | 0-90d | Database | 2017 |
| Phillips JE et al. 2006 | England | 41 | 4788 | / | / | / | / | 1987–2001 | 67.6(49–85) | 13.8 m | Single institution | 2006 |
| Keemu H. et al. 2023 | Finland | 484 | 62,087 | / | 22,941 | / | 39,146 | 2014–2020 | / | / | Database | 2023 |
| Bourget Murray J. et al. 2023 | Canada | 275 | 39,038 | / | / | / | / | 2013.1-2020.3 | / | 0–3 m | Database | 2023 |
| Jin X. et al. 2022 | Australia | 192 | 191,914 | 2002.1-2017.12 | / | 0–3 m | Database | 2022 | ||||
| Teo B.J.X. et al. 2018 | Singapore | 4 | 905 | 1 | 194 | 3 | 711 | 2004–2014 | 65.9 ± 7.7 | / | Single institution | 2018 |
| Koh C.K. et al. 2017 | New Zealand | 169 | 11,134 | 2000–2015 | 69 (9.7) | 0–180 m | Single institution | 2017 | ||||
| Fan J.C.H. et al. 2008 | China(Hong Kong) | 5 | 479 | 1 | 83 | 4 | 396 | 1997–2006 | 69(40–88) | 46(1-107)m | Single institution | 2008 |
Quality assessment
We used the JBI Quality Appraisal Tool for Systematic Reviews and Meta-Analyses to evaluate article quality. This tool examines study selection, data compilation, and presentation of findings, allowing readers to gauge a study’s reliability and relevance. It’s a critical instrument by the Australian-based Joanna Briggs Institute. For detailed scores, see Additional file 1: Table 1. Higher scores mean better research quality and less bias. We ranked studies into High (scores below 49%), medium (scores between 50 and 69%), and low (scores exceeding 70%) quality categories.
Data analysis
The study’s data was analyzed using the Meta module in R version 4.0.5. We converted incidence rates using the logarithm method and tested normality using the Shapiro-Wilk test. We used Q and I2 statistics to assess heterogeneity, with P < 0.05 and I2 > 50% indicating statistical heterogeneity [15]. In general, when P > 0.05 (for Q statistic) and I2 < 50%, the combined result is statistically homogeneous and a fixed-effects model can be used; when P > 0.05 and I2 > 50%, it indicates statistical heterogeneity and a random-effects model should be used. We used a forest plot to display incidence rates and the Egger test to assess publication bias. Meta-regression analysis was used to examine heterogeneity. Subgroup analyses were conducted by publication time, geographic location, gender, search standards, age range, and post-THA PJI incidence time.
Bibliometrics analysis
Data acquisition and search strategy
For this study, we relied on the Web of Science Core Collection (WOSCC) as our principal database for gathering information. On March 12, 2024, we executed a search according to a predetermined protocol: (TS = (total knee arthroplasty)) AND TS = (infection). We did not limit our search to any specific language. To maintain the integrity and pertinence of the selected articles, we excluded various forms of content, including editorials, letters, conference abstracts, revisions, conference proceeding papers, book sections, and retracted articles.
Data analysis
Data was gathered from publications in the Web of Science Core Collection and analyzed using two specialized bibliometric tools: R version 4.2.0 and VOSviewer. The R-based package Bibliometrix was used to process the data set, which enabled the creation of a range of bibliometric indicators and visual outputs. This comprehensive toolset supports the overall processes of data importation, management, thorough analysis, and visual display of bibliometric information.
VOSviewer is a web and knowledge graph visualization software for developing scientometrics [17]. VOSviewer can be used to identify highly effective journals and co-cited journals Importing the research data into VOSviewer for visualization allows us to analyze different elements, including countries, journals, and keywords. The research data was imported into VOSviewer for analysis, the appropriate parameters were set, and then visualizations including citations, bibliographic coupling, co-citations, or co-authors were performed.In the visual maps created by VOSviewer, each point is represented by a circular icon with a label indicating its identity. Co-occurrence analysis reveals that circles with greater size signify higher frequencies of occurrence. The color of these circular elements is determined by the cluster to which they belong. The thickness of the lines connecting the nodes reflects the intensity and significance of the relationship and the correlation between specific nodes.
Result
Meta-analysis
Literature search and included studies
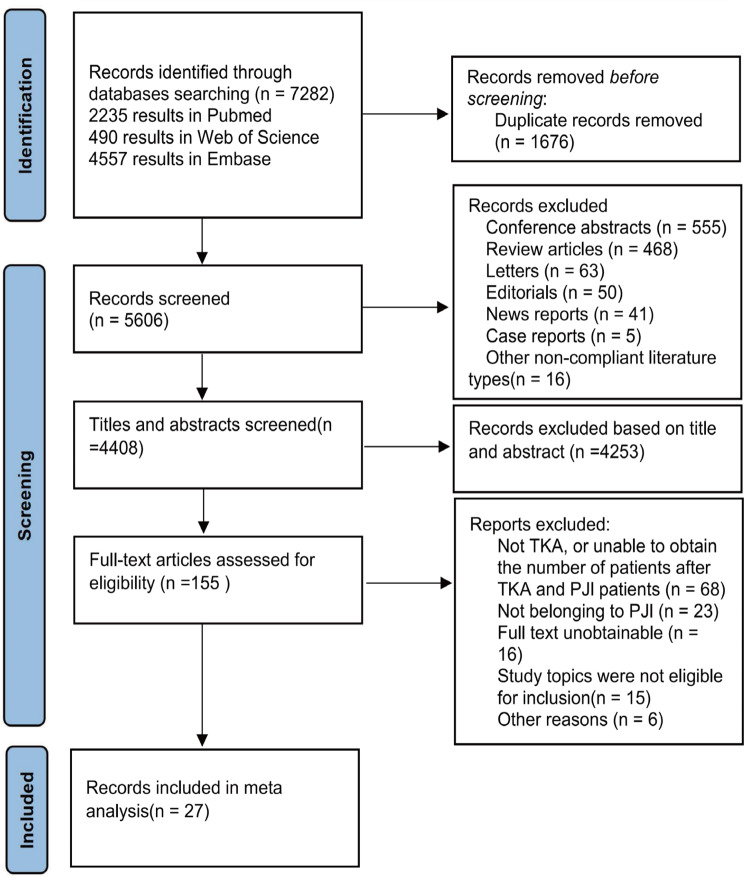
Using the search term “Arthroplasty, Replacement, Knee“[Mesh] OR “Arthroplasties, Replacement, Knee” OR “Arthroplasty, Knee Replacement” OR “Knee Replacement Arthroplasties” OR “Knee Replacement Arthroplasty” OR “Replacement Arthroplasties, Knee” OR “Knee Arthroplasty, Total” OR “Arthroplasty, Total Knee” OR “Total Knee Arthroplasty” OR “Replacement, Total Knee” OR “Total Knee Replacement” OR “Knee Replacement, Total” OR “Knee Arthroplasty” OR “Arthroplasty, Knee” OR “Arthroplasties, Knee Replacement” OR “Replacement Arthroplasty, Knee” resulted in 7282 records from the 3 databases (2235 results in Pubmed; 90 results in Web of Science; 4557 results in Embase). After duplicate removal, our literature searches yielded 5606 articles. We screened 4408 potentially relevant reports, reviewed 155 articles in full-text, and fnally included 27 studies in the analysis. Details of the inclusion process are shown in Fig. 1. The characteristics of studies are summarized in Table 1. The 27 studies, with a combined population of 3,664,589, cover 4 continents (America, Oceania, Europe, and Asia) and 13 countries (including the USA, Australia, China, Korea, Finland, Canada, New Zealand, England, Singapore, Italy, Turkey, Germany and Israel). The JBI quality assessment showed that 11 studies had a high risk bias, 10 studies had a moderate risk bias, and 6 studies had a low risk bias. The whole process was done by two researchers. A third researcher decides when disagreements arise.
Fig. 1.
Candidate study selection workflow for metaanalysis
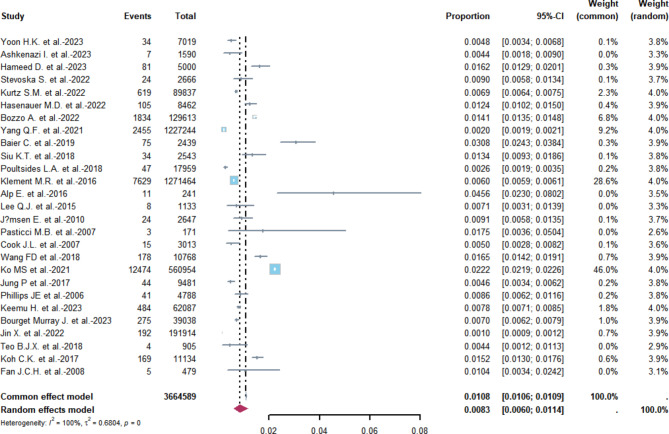
Overall incidence of PJI
Based on the figure presented, a meta-analysis was conducted to estimate the incidence rates of PJI. The combined fixed-effects model estimate of the overall PJI incidence rate was found to be 1.08% (95% CI 1.06–1.09%). Meanwhile, the overall combined random-effects estimate was 0.83% (95% CI 0.6–1.14%). It is important to note that the heterogeneity was found to be extremely high (I2 = 100%; Heterogeneity test P = 0), we therefore adopted the results of the random effects(Fig. 2).
Fig. 2.
Forest plot of the overall incidence of PJI in the database-based studies. The size of the squares represents the proportion (95% CI) for each of the studies. The size of the diamonds represent the overall proportion (95% CI)
Incidence of PJI by publication time
According to the literature included in this study, the publication time of papers was divided into two categories: those published within the last ten years and those published more than ten years ago. The purpose of categorization was to estimate the incidence rate of PJI. The study included 22 papers published between 2014 and 2023. The fixed effects overall combined estimate of PJI occurrence rate was 1.08% (95% CI 1.06–1.09%), while the random effects overall combined estimate was 0.83% (95%CI 0.6–1.14%). Since I2 > 50%, we adopted the results of the random effects here. The high degree of heterogeneity (I2 = 100%; Heterogeneity test P = 0) suggested significant variation among the included papers. Before 2013, the study included five papers, and the fixed effects overall combined estimate of PJI occurrence rate was 0.82% (95% CI 0.67%-1.01%). The random effects overall combined estimate was 0.82% (95%CI 0.63-1.07%), which also showed low heterogeneity (I2 = 35%; Heterogeneity test P = 0.19) (Supplementary material: Fig. 1).
Incidence of PJI by sex
Several studies have shown that there are gender differences in the incidence rate of PJI. For males, the overall estimate of the incidence rate for PJI was 1.33% (95% CI 1.11–1.6%) under a combined fixed-effect, and 1.29% (95% CI 0.84–1.97%) under a random-effects model, indicating no high heterogeneity (I2 = 74%; Heterogeneity test P < 0.01). For females, the overall estimate of the incidence rate for PJI was 0.78% (95% CI 0.64–0.94%) in a fixed-effects model, and 0.67% (95% CI 0.41–1.10%) in a random-effects model, with less heterogeneity observed (I2 = 79%; Heterogeneity test P < 0.01) (Supplementary material: Fig. 2).
Incidence of PJI by geographic location of conducted studies
Our study analyzed the incidence rate of PJI (Periprosthetic Joint Infection) based on the geographic location of conducted studies. The studies included four major continents: Asia, North America, Oceania, and Europe. In Asia, we found that the fixed effect summary estimate of PJI incidence rate was 1.49% (95% CI 1.47–1.51%), whereas the random effect summary estimate was 0.90% (95% CI 0.50–1.63%). The heterogeneity was extreme (I2 = 100%; Heterogeneity test P < 0.01). In North America, the fixed and random effects summary estimates of PJI incidence were 0.71% (95% CI 0.70–0.73%) and 0.77% (95% CI 0.50–1.16%), respectively. The heterogeneity was high (I2 = 99%; Heterogeneity test P < 0.01). For Oceania, the fixed effect summary estimate for PJI was 0.38% (95% CI 0.35–0.42%), and the random effect summary estimate was 0.50% (95% CI 0.16–1.60%). We observed extreme heterogeneity (I2 = 100%; Heterogeneity test P < 0.01). Finally, in Europe, the fixed effect summary estimate of PJI incidence was 0.93% (95% CI 0.86–1.01%), and the random effect summary estimate was 1.23% (95% CI 0.70–2.16%). We found extreme heterogeneity (I2 = 97%; Heterogeneity test P < 0.01) in this continent as well (Supplementary material: Fig. 3). The latter result is therefore acceptable.
Incidence of PJI by follow-up time
It has been reported in previous studies that PJI can occur up to one year after TKA. Therefore, we divided our study into two groups: those within a year and those over a year and conducted a subgroup analysis based on follow-up time. For studies that followed up within a year, the overall fixed effect estimation of PJI occurrence rate was 0.95% (95% CI 0.90–1.01%), and the overall random effect estimation of occurrence rate was 1.11% (95% CI 0.74–1.66%), showing high heterogeneity (I2 = 97%; heterogeneity test P < 0.01). For studies with follow-up times exceeding one year, the fixed effect institution’s overall merged estimated rate of PJI occurrence was 0.35% (95% CI 0.32–0.38%), and the random effect institution’s overall merged estimated rate of PJI occurrence was 0.41% (95% CI 0.16–1.06%), again showing high heterogeneity (I2 = 99%; Heterogeneity test P < 0.01).
Publication bias
We performed an analysis to detect publication bias in the studies that we included. The funnel plot (Supplementary material: Fig. 3) shows some asymmetry on both sides of the symmetry axis among the studies. However, we also conducted the Egger test (Supplementary material: Fig. 6) and found that there is no statistically significant publication bias (P > 0.05).
Sensitivity analyses
We carefully examined and excluded each piece of literature that we included in our analysis. We also looked at how much influence each individual study had on the overall effect size. Our findings showed that there was no significant change in the effect size, which indicates that the included studies were stable and reliable (Supplementary material: Fig. 6).
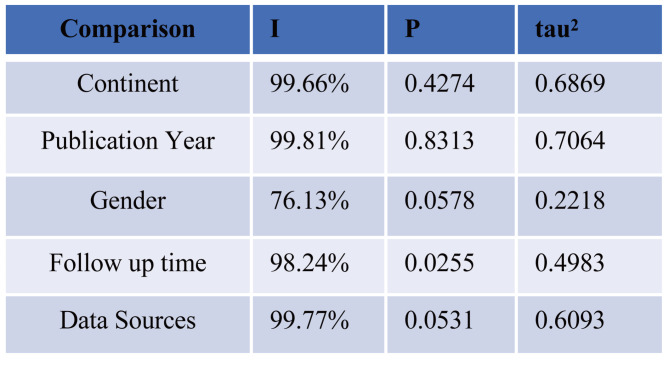
Meta-regression
We conducted a Meta univariate regression analysis on subgroups to address the issue of high heterogeneity. The results indicate that, in database-based research, the follow-up time is the source of heterogeneity (P < 0.05), while the other factors are not (P > 0.05) (Fig. 3).
Fig. 3.
The Meta-regression analysis
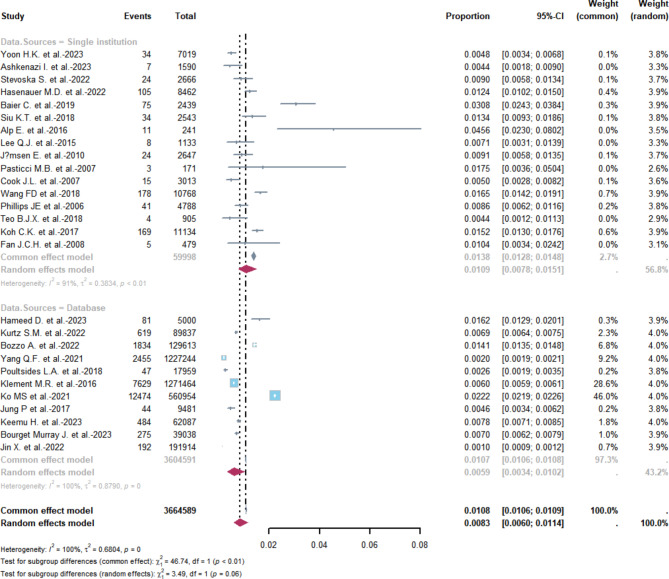
Incidence of PJI by Data sources
In the single-institution studies, a total of 16 research papers were analyzed. As shown in Fig. 4 The overall combined occurrence rate of PJI was estimated to be 1.38% (95% CI 1.28–1.48%) with a fixed effect, while the total combined occurrence rate was estimated to be 1.09% (95% CI 0.78–1.51%) with a random effect. However, there was a high level of heterogeneity (I2 = 91%; heterogeneity test P < 0.01). In the case of database studies, a total of 11 papers were analyzed. The overall combined occurrence rate of PJI was estimated to be 1.07% (95% CI 1.06–1.08%) with a fixed effect, while the overall combined occurrence rate was estimated to be 0.59% (95% CI 0.34–1.02%) with a random effect. The level of heterogeneity was extremely high (I2 = 100%; heterogeneity test P = 0). We therefore choose the latter one.
Fig. 4.
Incidence of PJI from a single institution or database
Bibliometric analysis
Basic data summary
In this study, we primarily utilized the Web of Science Core Collection (WOSCC) database as our principal information source. On March 14, 2024, a predefined search strategy was employed: (TS=(total knee arthroplasty)) AND TS=(infection). No language restrictions were enforced on the publications. To ensure quality and relevance, several types of materials, such as editorials, letters, conference abstracts, revisions, proceedings, book chapters, and retracted publications, were excluded.
A total of 3,831 articles were subsequently analysed in this study. Authored by 12,715 researchers from 3,670 institutions across 70 countries since 1994, these papers were published across 442 different journals. Each article, on average, has been cited 28.48 times. According to Lotka’s Law, the authors that contribute to a research study (1.2) make up 50% of the total number of authors.
Annual number of publications
Since 2009, there has been a notable surge in the volume of scholarly articles published on PJI following primary TKA. The growth rate in that year was 32.5%, and subsequently, up until the end of 2023, research institutions globally have averaged yearly contributions of 233 articles in this field (Fig. 5 ) (Supplementary materiale: Table 2).
Fig. 5.
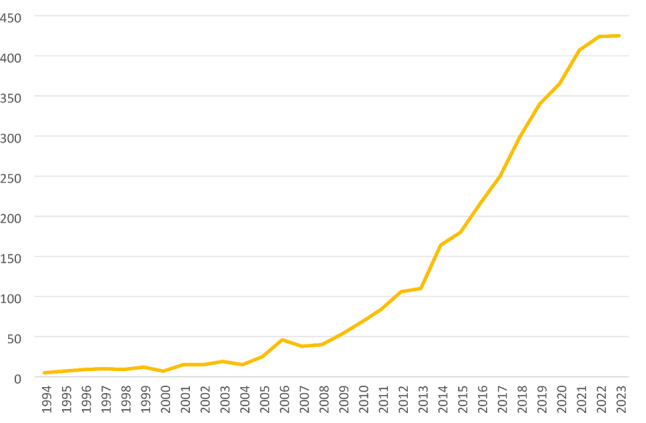
Annual publication numbers from 1994 to 2023
Analysis of the countries with the highest productivity
The greatest volume of publications comes from the USA (n = 1557), followed by Germany (n = 522), China (n = 338), England (n = 228), Italy (n = 184), Spain (n = 165), France (n = 160), and Switzerland (n = 108). All other countries/regions have published fewer than 100 articles each. Most research collaborations involve the USA and other countries, with the top four being between the USA and China (n = 43), USA and Israel (n = 39), USA and England (n = 32), and USA and Germany (n = 32).
Analysis of the most productive journals
The top ten journals in publication volume, as presented above, have contributed to 44.17% (1692 out of 3831) of the total articles in this field. Three of them are based in the United States, another three in the United Kingdom, and the remaining three in Germany. They are primarily from the sphere of Orthopedics, however, some represent other fields such as Surgery, Rheumatology, and Sports Sciences (Table 2).
Table 2.
The table of most productive journals
| Journal | Articles | IF(2023) | field/JCR |
|---|---|---|---|
| JOURNAL OF ARTHROPLASTY | 784 | 3.5 | ORTHOPEDICS (Q1) |
| CLINICAL ORTHOPAEDICS AND RELATED RESEARCH | 189 | 4.2 | ORTHOPEDICS(Q1)/SURGERY (Q1) |
| JOURNAL OF BONE AND JOINT SURGERY AMERICAN VOLUME | 157 | 5.3 | ORTHOPEDICS(Q1)/SURGERY (Q1) |
| BONE … JOINT JOURNAL | 111 | 4.6 | ORTHOPEDICS(Q1)/SURGERY (Q1) |
| ARCHIVES OF ORTHOPAEDIC AND TRAUMA SURGERY | 108 | 2.3 | ORTHOPEDICS(Q2)/SURGERY (Q2) |
| INTERNATIONAL ORTHOPAEDICS | 95 | 2.7 | ORTHOPEDICS(Q2) |
| BMC MUSCULOSKELETAL DISORDERS | 64 | 2.3 | ORTHOPEDICS(Q3)/RHEUMATOLOGY(Q4) |
| KNEE SURGERY SPORTS TRAUMATOLOGY ARTHROSCOPY | 62 | 3.8 | ORTHOPEDICS(Q1)/SPORT SCIENCES(Q1)/SURGERY(Q1) |
| JOURNAL OF KNEE SURGERY | 61 | 1.7 | ORTHOPEDICS(Q3) |
| JOURNAL OF ORTHOPAEDIC SURGERY AND RESEARCH | 61 | 2.6 | ORTHOPEDICS (Q2) |
Analysis of the most cited publications
Table 3 shows that the top ten most-cited research papers in this field were published around 2010. The most frequently cited paper is “ZIMMERLI W, 2004”, which provides a comprehensive overview of the pathogenesis, diagnosis, and treatment of PJI.
Table 3.
The top 10 most cited publications
| Paper | DOI | Total Citations | TC per Year | Journal | IF | JCR |
|---|---|---|---|---|---|---|
| ZIMMERLI W, 2004, NEW ENGL J MED | 10.1056/NEJMra040181 | 2114 | 100.67 | The New England Journal of Medicine | 158.5 | Q1 |
| OSMON DR, 2013, CLIN INFECT DIS | 10.1093/cid/cis803 | 1673 | 139.42 | Clinical Infectious Diseases | 11.8 | Q1 |
| KURTZ SM, 2012, J ARTHROPLASTY | 10.1016/j.arth.2012.02.022 | 1190 | 91.54 | The Journal of arthroplasty | 3.5 | Q1 |
| TANDE AJ, 2014, CLIN MICROBIOL REV | 10.1128/CMR.00111 − 13 | 1058 | 96.18 | Clinical Microbiology Reviews | 36.8 | Q1 |
| PARVIZI J, 2018, J ARTHROPLASTY | 10.1016/j.arth.2018.02.078 | 1016 | 145.14 | The Journal of arthroplasty | 3.5 | Q1 |
| TRAMPUZ A, 2007, NEW ENGL J MED | 10.1056/NEJMoa061588 | 948 | 52.67 | The New England Journal of Medicine | 158.5 | Q1 |
| PULIDO L, 2008, CLIN ORTHOP RELAT R | 10.1007/s11999-008-0209-4 | 915 | 53.82 | Clinical Orthopaedics and Related Research | 4.2 | Q1 |
| PARVIZI J, 2011, CLIN ORTHOP RELAT R | 10.1007/s11999-011-1971-2 | 836 | 59.71 | Clinical Orthopaedics and Related Research | 4.2 | Q1 |
| KURTZ SM, 2008, J ARTHROPLASTY | 10.1016/j.arth.2007.10.017 | 717 | 42.18 | The Journal of arthroplasty | 3.5 | Q1 |
| DEL POZO JL, 2009, NEW ENGL J MED | 10.1056/NEJMcp0905029 | 575 | 35.94 | The New England Journal of Medicine | 158.5 | Q1 |
Analysis of keywords
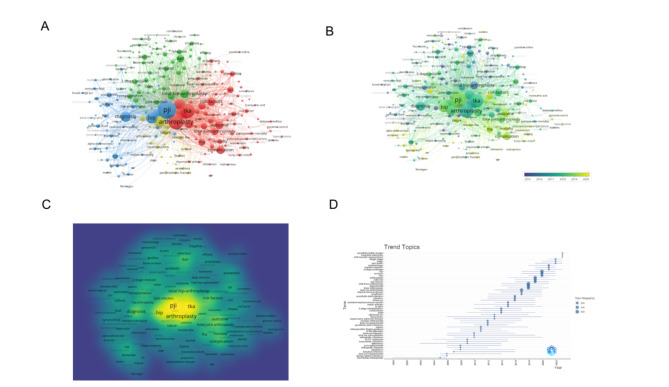
After consolidating keywords with the same meaning, our search yielded a total of 7519 author keywords. We then filtered out keywords that occurred less than 20 times, resulting in 249 keywords that met our filtering criteria. Figure 2 displays the frequency of these keywords; the larger the yellow circle, the higher the keyword’s occurrence.
Figure 6A provides a visual analysis of the relationships between these high-frequency keywords. The size of each node corresponds to the frequency of the keyword, while the distance between two nodes indicates their degree of correlation. Keywords located closely together are grouped into the same cluster (denoted by color), reflecting the central research themes of that specific branch. The keyword analysis resulted in four clusters. Cluster 1, highlighted in red, includes high-frequency words reflecting the prevention of PJI, such as risk-factors, outcome, complication, risk, and prevention. Cluster 2, colored in green, contains keywords like dair, management, reimplantation, biofilm, 2-stage revision, antibiotic, two-stage revision, indicative of PJI treatment. Cluster 3, marked in blue, features keywords such as diagnosis, crp, culture, sonication, septic arthritis, fluid, which centers on PJI diagnosis. Lastly, Cluster 4, denoted in yellow, represents the management of initial TKA and revision failure with keywords such as revision, failure, prosthesis, follow-up, revision tka, reconstruction, salvage, survival.
Fig. 6.
A network visualization of author keywords; B visualisation map summarising the themes of the previous years from a temporal point of view; C Visualisation maps of different research branch networks; D Popular Hot Topic Words of the Past Years
Research topics are not stagnant; a chronological assessment of keywords from previous years can reveal the shift of research focus in this field. In Fig. 6B, darker colors indicate earlier research periods, and lighter colors represent more recent studies. Combined with the viewpoint of different research branches displayed in Fig. 6C, it’s noticeable that until 2018, PJI diagnosis and treatment were the focal points of research. From 2018, researchers gravitated towards PJI prevention and management post-occurrence. Figure 6D demonstrates these shifting research trends from the perspective of popular keywords over the years. The notable keywords for the recent two years in the field include povidone-iodine lavage, long-term outcomes, arthroscopic synovectom.
Discussion
Meta-analysis
Our research has found that the total incidence rate of PJI stands at 0.83%. However, when we analyzed different sources of data, we found a significant difference in the incidence of PJI between database sources and individual institutions. The former showed an incidence of only 1.09%, while the latter recorded an incidence rate of 0.59%. This difference may be due to several factors, including the vast population data available in the databases compared to smaller sample sizes in individual institutions. The incidence of PJI after TKA in the general population ranges from 0.5 to 2.3% in USA, which is different from our results [18]. We believe that this difference may be due to the larger number of TKA recipients in the United States. The treatment of TKA presents a significant challenge due to numerous factors influencing the incidence of PJI. This is a research area that is being actively pursued by many scholars.
In 2013, the International Consensus Meeting (ICM) introduced new diagnostic criteria for PJI, which resolved previous confusion about its diagnosis. As a result, we analyzed the data before and after 2014, the year the new criteria were established. The analysis showed that the incidence rate of PJI was lower (0.82%) before 2014 compared to the period after 2014 (1.08%). This suggests that the introduction of new diagnostic criteria has led to better detection of PJI, which was previously overlooked. The two main risk factors for PJI can be divided into patient-related and surgical-related factors. The patient-related factors include gender, age, obesity, systemic diseases like diabetes, smoking, hypoalbuminemia, and preoperative intra-articular injection for TKA [19–25]. The surgical-related factors, on the other hand, include the side of the operation, duration of anesthesia, patella resurfacing, and blood transfusion [26–28]. Medical technology has made managing PJI easier, but reducing its incidence rate still requires significant work.
Gender is a significant factor that affects the incidence of PJI, as per previous research [29–31]. The occurrence of PJI is higher in males (1.29%) than in females (0.67%). The reasons behind this discrepancy could be due to men being more active and aggressive post-TKA, as well as gender-based differences in pharmacokinetics [31–33]. There is not enough research available on the gender-based incidence of the disease, and more observations are needed to establish the same.
The economic and welfare standards of different nations or regions may have an impact on their medical standards [34]. In a recent study, it was found that among the four groups analyzed - Asia, North America, Oceania, and Europe - Asia had a significantly higher incidence of PJI. This could be attributed to various factors such as surgical standards, sterility conditions during operations, and people’s conceptual awareness in underdeveloped regions. These factors may all contribute to the higher occurrence of PJI in Asia [34, 35].Although improving medical standards in underdeveloped areas is a challenging task, we are confident that advancements in time will eventually enhance them.
The incidence and duration of an infection are crucial factors that help in formulating a treatment plan. PJI can be identified within 90 days after surgery, but in some cases, they can be diagnosed as late as six months up to a year later [36–38]. Our research shows a difference between the short-term incidence rate of PJI, which is 1.11%, and its later incidence rate, which is 0.41%. Although the incidence of PJI reduces over an extended period, it is still recommended to monitor patients for an extended period to avoid potential repercussions caused by such infections.
Statistics on the incidence of PJI are often based on clinical studies of a single institution or various databases. In this regard, we conducted a subgroup analysis using data from both sources. Our findings indicate that the incidence of PJI from a single institution is notably higher (1.09%) than that from databases (0.59%). This aligns with the reported incidence of PJI after total hip arthroplasty [15]. However, relying solely on databases for incidence data may lead to underestimation of the actual incidence of PJI.
Bibliometrics
As a branch of information science, bibliometrics plays an increasingly vital role in scientific domains, especially within the field of medicine. Through bibliometrics, we are able to discern the overall trends, hotspots, and directions of research in a short span of time. Additionally, it provides a visual and simplified structure of knowledge, affording significant convenience to research processes [39, 40]. Web of Science (WoS) is the world’s largest and most comprehensive academic resource hub, encompassing fields such as biomedicine and natural science, and boasting a great number of core journals [41]. The literature data in our study is sourced from this platform. Beyond that, WoS also contains cited references, authors, sources, and publication years. In summary, it offers rapid search capability, advanced search, and citation search, all of which assist us in efficiently and accurately locating desired articles and journal information.
Global research status
An analysis of literature related to PJI after TKA from 1994 to 2023 reveals that an average of 127.7 papers per year has been published on this subject. In 2011, the number of global publications reached 100 for the first time. This milestone was upstaged in 2016 when the count exceeded 200, reaching over 300 in 2019, and surpassing 400 in 2021. This surge possibly correlates with an increase in TKA numbers due to growing trends of an aging population, and a rise in the incidence of PJI [42, 43]. Despite the growing number of publications, the research intensity in this area remains relatively low compared to other domains, and there is a lack of high-level research reports.
The quantity of articles published within a specific research field can, to a certain extent, appraise the research competence of a country or institution in that area [44]. When looking at the involved nations, the United States far outpaces all others in terms of the volume of publications, markedly surpassing Germany and China, which are ranked second and third, respectively.Seven out of the top ten organizations based on highest publication volume are from the United States, while the remaining three are from Germany. The ‘Journal of Arthroplasty’ has published the highest number of studies related to PJI following TKA. The number of publications in this field is almost twice that of the second and third most published journals - ‘Clinical Orthopaedics and Related Research’ and ‘Journal of Bone and Joint Surgery American Volume’. However, citation analysis indicates a different ranking order for these journals, which is likely due to the fact that significant studies in this field are primarily published in ‘The New England Journal of Medicine’ and ‘Clinical Infectious Diseases’, rather than in the ‘Journal of Arthroplasty’. High-quality clinical studies often require multicenter and large samples, and while there is some collaboration among researchers in various countries, further collaboration is needed to advance the field.
The co-occurrence network map, created by analyzing frequently appearing keywords in the publications included in this study, reveals four clusters of research hotspots related to PJI after TKA. These clusters include risk factors, management, diagnosis, and revision. Several salient themes have been recognized within these clusters, which bear higher weight and larger co-occurrence link strength. For example, the replacement branch mirrors the management of failures post the initial TKA and revision surgeries. The research on PJI after TKA primarily focuses on risk factors, diagnosis, and treatment. Future studies could pivot on these directions, with the aim to provide references and guidance for the prevention and treatment of PJI after TKA. For instance, the search for new serum markers with high specificity to enhance diagnosis efficiency, or the renewal of perioperative management methods to reduce the risks of PJI.
Limitations
This study has several limitations: First, Our analysis may have gaps in search coverage, but our funnel plot analysis shows minimal impact on results due to limited studies in some subgroups. Second, Although we recognize the differences in methodology and outcomes between database-based studies and clinical research, the high heterogeneity of database-based studies limits our ability to obtain a homogeneous estimate of PJI incidence rate. Third, the collected and screened article data are all sourced from the Web of Science Core Collection, inevitably leading to data omission.This study includes only English-language articles, potentially causing selection bias. Lastly, but equally significant, the Web of Science Core Collection is constantly updated, rendering our analysis results in this study time-constrained. Despite these limitations, our findings still pave the way for guiding future research.
Conclusion
Our research has found that the total incidence rate of PJI stands at 0.83%. However, when we analyzed different sources of data, we found a significant difference in the incidence of PJI between database sources and individual institutions. The former showed an incidence of only 1.09%, while the latter recorded an incidence rate of 0.59%. Bibliometric studies analyzing the occurrence of PJI after TKA have shown a yearly increase in the number of publications in this field. The United States is the leading country in terms of the quantity of published papers, and is home to institutions that have made the biggest scientific impact. The most influential publication in this area is a literature review by Professor Zimmerli in 2004, which provides a comprehensive summary of the pathogenesis, diagnosis, and treatment of PJI.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Author contributions
Tao Ma and Decai Hou wrote the article. Tao Ma and Jun Jiao collected the data. Decai Hou, Dawei Guo, and Shuzheng Lv designed the study. Dawei Guo contributed toward data analysis, Tao Ma, and Decai Hou drafting and critically revising the paper, and All authors agreed to be accountable for all aspects of the work. All authors reviewed the manuscript and approved the submitted version.
Funding
Not applicable.
Data availability
Publicly available datasets were analyzed in this study. This data can be found here: www.cdc.gov/nchs/nhanes.
Declarations
Consent for publication
All authors agreed on the manuscript.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Felson DT, Lawrence RC, Hochberg MC, McAlindon T, Dieppe PA, Minor MA, Blair SN, Berman BM, Fries JF, Weinberger M, Lorig KR, Jacobs JJ, Goldberg V. Osteoarthritis: new insights. Part 2: treatment approaches. Ann Intern Med. 2000;133:726–37. [DOI] [PubMed] [Google Scholar]
- 2.Jones CA, Beaupre LA, Johnston DW, Suarez-Almazor ME. Total joint arthroplasties: current concepts of patient outcomes after surgery. Clin Geriatr Med. 2005;21:527–41, vi. [DOI] [PubMed]
- 3.Izakovicova P, Borens O, Trampuz A. Periprosthetic joint infection: current concepts and outlook. EFORT Open Rev. 2019;4:482–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kapadia BH, Berg RA, Daley JA, Fritz J, Bhave A. Mont M.A. Periprosthetic joint infection. Lancet. 2016;387:386–94. [DOI] [PubMed] [Google Scholar]
- 5.Sloan M, Premkumar A, Sheth NP. Projected Volume of Primary Total Joint Arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am. 2018;100:1455–60. [DOI] [PubMed] [Google Scholar]
- 6.Tang X, Wang S, Zhan S, Niu J, Tao K, Zhang Y, Lin J. The prevalence of symptomatic knee osteoarthritis in China: results from the China Health and Retirement Longitudinal Study. Arthritis Rheumatol. 2016;68(3):648–53. [DOI] [PubMed] [Google Scholar]
- 7.Tay KS, Lo NN, Yeo SJ, Chia SL, Tay DK, Chin PL. Revision total knee arthroplasty: causes and outcomes. Ann Acad Med Singap. 2013;42(4):178–83. [PubMed] [Google Scholar]
- 8.Leta TH. Revision knee arthroplasty in Norway 1994–2011. A register-based study with focus on implant survival, causes and risk of re-revision, pain relief, functional outcome, patient satisfaction, and health related quality of life. Bergen, Norway: University of Bergen; 2017. [Google Scholar]
- 9.Thiele K et al. Current failure mechanisms after knee arthroplasty have changed: polyethylene wear is less common in revision surgery. J Bone Joint Surg Am Vol 97,9 (2015): 715–20. [DOI] [PubMed]
- 10.McMaster Arthroplasty Collaborative (MAC). Risk Factors for Periprosthetic Joint Infection Following Primary Total Hip Arthroplasty: A 15-Year, Population-Based Cohort Study. J Bone Joint Surg Am. 2020 Mar 18;102(6):503-509. [DOI] [PubMed]
- 11.Patel A, Pavlou G, Mújica-Mota RE, Toms AD. The epidemiology of revision total knee and hip arthroplasty in England and Wales: a comparative analysis with projections for the United States. A study using the National Joint Registry dataset. Bone Joint J. 2015;97–B(8):1076–81. [DOI] [PubMed] [Google Scholar]
- 12.Kunutsor SK, Whitehouse MR, Blom AW, Beswick AD, INFORM Team. Re-infection outcomes following one- and two-stage Surgical revision of infected hip prosthesis: a systematic review and Meta-analysis. PLoS ONE. 2015;10(9):e0139166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Parvizi J, Tan TL, Goswami K, Higuera C, Della VC, Chen AF, et al. The 2018 definition of periprosthetic hip and knee infection: an evidence-based and validated criteria. J Arthroplast. 2018;33(5):1309–14. [DOI] [PubMed] [Google Scholar]
- 14.Guan H, Fu J, Li X, Chai W, Hao L, Li R, Zhao J, Chen J. The 2018 new definition of periprosthetic joint infection improves the diagnostic efficiency in the Chinese population. J Orthop Surg Res. 2019;14(1):151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zeng Z-J et al. Incidence of periprosthetic joint infection after primary total hip arthroplasty is underestimated: a synthesis of meta-analysis and bibliometric analysis. J Orthop Surg Res 18,1 610. 21 Aug. 2023. [DOI] [PMC free article] [PubMed]
- 16.Abramo G, D’Angelo C, Di Costa F. National research assessment exercises: a comparison of peer review and bibliometrics rankings. Scientometrics. 2011;89(3):929–41. [Google Scholar]
- 17.van Eck N, Waltman L. Software Survey: VOSviewer, a computer program for Bibliometric Mapping. Scientometrics. 2010;84(2):523–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Premkumar A, Kolin DA, Farley KX, Wilson JM, McLawhorn AS, Cross MB, Sculco PK. Projected Economic Burden of Periprosthetic Joint Infection of the hip and knee in the United States. J Arthroplast. 2021;36:1484–e14893. [DOI] [PubMed] [Google Scholar]
- 19.Ko MS, Choi CH, Yoon HK, Yoo JH, Oh HC, Lee JH, Park SH. Risk factors of postoperative complications following total knee arthroplasty in Korea: a nationwide retrospective cohort study. Medicine. 2021;100:e28052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McMaster Arthroplasty Collaborative (MAC). Incidence and predictors of prosthetic joint infection following primary total knee arthroplasty: a 15-year population-based cohort study. J Arthroplast. 2022;37:367–e3721. [DOI] [PubMed] [Google Scholar]
- 21.Bozic KJ, Lau E, Kurtz S, Ong K, Berry DJ. Patient-related risk factors for postoperative mortality and Periprosthetic Joint Infection in Medicare patients undergoing TKA. Clin Orthop Relat Res. 2012;470:130–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen J, Cui Y, Li X, Miao X, Wen Z, Xue Y, Tian J. Risk factors for deep infection after total knee arthroplasty: a meta-analysis. Arch Orthop Trauma Surg. 2013;133:675–87. [DOI] [PubMed] [Google Scholar]
- 23.Singh JA, Schleck C, Harmsen WS, Jacob AK, Warner DO, Lewallen DG. Current tobacco use is associated with higher rates of implant revision and deep infection after total hip or knee arthroplasty: a prospective cohort study. BMC Med. 2015;13:283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Man SL-C, Chau W-W, Chung K-Y, Ho KKW. Hypoalbuminemia and obesity class II are reliable predictors of peri-prosthetic joint infection in patient undergoing elective total knee arthroplasty. Knee Surg Relat Res. 2020;32:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bedard NA, Pugely AJ, Elkins JM, Duchman KR, Westermann RW, Liu SS, Gao Y, Callaghan JJ. Do intraarticular injections increase the risk of infection after TKA? Clin. Orthop Relat Res. 2017;475:45–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Peersman G, Laskin R, Davis J, Peterson MGE, Richart T. Prolonged Operative Time correlates with increased infection rate after total knee arthroplasty. HSSJ. 2006;2:70–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pilling RW, Moulder E, Allgar V, Messner J, Sun Z, Mohsen A. Patellar resurfacing in primary total knee replacement: a meta-analysis. J Bone Jt Surg Am. 2012;94:2270–8. [DOI] [PubMed] [Google Scholar]
- 28.Memtsoudis SG, Ma Y, González Della Valle A, Mazumdar M, et al. Perioperative outcomes after unilateral and bilateral total knee arthroplasty. J Am Soc Anesthesiol. 2009;111:1206–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Anneberg M, Troelsen A, Gundtoft P, Sørensen HT, Pedersen AB. Temporal trends in revision rate due to knee periprosthetic joint infection: a study of 115,120 cases from the Danish knee Arthroplasty Register. Acta Orthop. 2023;94:616–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bae KJ, Chae YJ, Jung SJ, Gong HS. Incidence and risk factors for periprosthetic joint infection: a common data model analysis. Jt Dis Relat Surg. 2022;33(2):303–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lin YH, Lin CH, Huang YY, Liu PH, Lin YC. Effect of Taiwan’s Diabetes Shared Care Program on the risk of periprosthetic joint infection after total joint arthroplasty in patients with type 2 diabetes mellitus: an eight-year population-based study. J Hosp Infect. 2024;145:34–43. [DOI] [PubMed] [Google Scholar]
- 32.Zucker I, Prendergast BJ. Sex differences in Pharmacokinetics. Handb Exp Pharmacol. 2023;282:25–39. [DOI] [PubMed] [Google Scholar]
- 33.Metcalf RW, Rowe T, Tersteeg M, Dombrowski ME, Odum S, Otero JE. The influence of patient sex on outcomes following one-stage and two-stage revision for Periprosthetic Joint Infection in total joint arthroplasty. Antibiot (Basel). 2023;12(9):1392. Published 2023 Aug 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Leta TH, Fenstad AM, Lygre SHL, et al. The use of antibiotic-loaded bone cement and systemic antibiotic prophylactic use in 2,971,357 primary total knee arthroplasties from 2010 to 2020: an international register-based observational study among countries in Africa, Europe, North America, and Oceania. Acta Orthop. 2023;94:416–25. Published 2023 Aug 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Laubscher K, Dey R, Nortje M, Held M, Kauta N. Primary hip and knee arthroplasty at district level is safe and may reduce the burden on tertiary care in a low-income setting. BMC Musculoskelet Disord. 2022;23(1):1014. Published 2022 Nov 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Petis SM, Perry KI, Mabry TM, Hanssen AD, Berry DJ, Abdel MP. Two-Stage Exchange Protocol for Periprosthetic Joint Infection Following Total Knee Arthroplasty in 245 knees without prior treatment for infection. J Bone Joint Surg Am. 2019;101(3):239–49. [DOI] [PubMed] [Google Scholar]
- 37.Petis SM, Abdel MP, Perry KI, Mabry TM, Hanssen AD, Berry DJ. Long-term results of a 2-Stage Exchange Protocol for Periprosthetic Joint Infection Following Total Hip Arthroplasty in 164 hips. J Bone Joint Surg Am. 2019;101(1):74–84. [DOI] [PubMed] [Google Scholar]
- 38.Lichstein P, Su S, Hedlund H, Suh G, Maloney WJ, Goodman SB, et al. Treatment of periprosthetic knee infection with a two-stage protocol using static spacers. Clin Orthop Relat Res. 2016;474(1):120–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thompson DF, Walker CK. A descriptive and historical review of bibliometrics with applications to medical sciences. Pharmacotherapy. 2015;35:551–9. [DOI] [PubMed] [Google Scholar]
- 40.Cooper I, Diane. Bibliometrics basics. J Med Libr Association: JMLA 103,4 (2015): 217–8. [DOI] [PMC free article] [PubMed]
- 41.Thomaidou AC, Goulielmaki M, Tsintarakis A, Zoumpourlis P, Toya M, Christodoulou I, et al. Mirna-guided regulation of mesenchymal stem cells derived from the umbilical cord: paving the way for stem-cell based regeneration and therapy. Int J Mol Sci. 2023;24:9189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rupp M, Walter N, Lau E, Worlicek M, Kurtz SM, Alt V. Recent trends in revision knee arthroplasty in Germany. Sci Rep. 2021 Jul 29;11(1):15479. [DOI] [PMC free article] [PubMed]
- 43.Rupp MLE. M.Alt V.Projections of primary TKA and THA in Germany from 2016 through 2040. Clin Orthop Relat Res. 2020;478:1622–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Moed HF, Halevi G. Multidimensional assessment of scholarly research impact. J Assoc Inf Sci Technol. 2015;66:1988–2002. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found here: www.cdc.gov/nchs/nhanes.