Abstract
A 63-year-old Japanese female presented with fever. Computed tomography showed multiple nodules in both lungs. Corticosteroids and antibiotics were administered to treat suspected organizing and bacterial pneumonia, resulting in no improvement and respiratory failure worsened. Surgical lung biopsy revealed infiltration of CD3, CD56, Granzyme B, and EBV-encoded RNA-ISH-positive atypical lymphocytes. She was diagnosed with primary pulmonary extranodal NK/T-cell lymphoma (ENKL) and died two months after diagnosis with only a temporary effectiveness of chemotherapy. We should consider the possibility of ENKL and perform prompt and appropriate biopsy for early diagnosis in cases where empiric therapy is ineffective for suspected pneumonia.
Keywords: Multiple nodules, Extranodal NK/T cell lymphoma, Surgical lung biopsy
Highlights
-
•
Primary pulmonary ENKL has a poor prognosis owing to rapid disease progression.
-
•
Its clinical features often mimic those of bacterial pneumonia.
-
•
There is concern that delayed diagnosis may lead to poor outcomes.
-
•
A sufficiently large amount of biopsy tissue is required for an accurate diagnosis.
1. Introduction
Primary pulmonary lymphoma (PPL) is a rare clinical entity, representing only 0.5–1% of lung neoplasia cases [1]. Among PPLs, mucosa-associated lymphoid tissue lymphoma accounts for over 80 % of cases, whereas the other types of lymphoma, including extranodal NK/T cell lymphoma (ENKL), which is associated with Epstein-Barr virus (EBV) infection, are rare. Although ENKL predominantly affects the upper respiratory tract, including the nasal cavity, nasopharynx, and sinuses, it can also occur in areas other than the nasal cavity, such as the skin, small intestine, and testis [2]. In a previous report of 136 ENKL cases, 68 % were nasal and 26 % were extranasal, with the latter having worse prognosis [3]. Among extranasal ENKL cases, lung involvement is relatively rare (14 %) compared to intestinal (37 %) and skin (26 %) involvement. Herein, we report a case of primary pulmonary ENKL diagnosed using thoracoscopic lung biopsy despite respiratory failure.
2. Case presentation
A 63-year-old Japanese female complaining of fever that had persisted for two weeks visited the hospital. Computed tomography (CT) showed multiple bilateral lung nodules. Blood culture test results were negative, and echocardiography revealed no vegetation. Although her soluble interleukin-2 receptor (sIL-2R, 673 U/mL) level was elevated, bone marrow aspiration revealed no abnormalities. Bronchoscopy revealed no specific findings on transbronchial lung biopsy, lymphocytosis in the bronchoalveolar lavage fluid (BALF), no malignant cell in BALF cytology and negative BALF bacterial culture. Based on these findings, organizing pneumonia or bacterial pneumonia was suspected, and steroid pulse therapy and antibiotic treatment were initiated but resulted in no improvement in radiological findings. Twenty-four days after the first visit, she was referred to our hospital for further examination.
On admission, blood pressure was 123/78 mmHg, pulse rate was 81 beats/min, body temperature was 36.0 °C, and respiratory rate was 18/min. Oxygen saturation was 94 % with 3 L/min of oxygen supplementation via a nasal cannula. Physical examination revealed mild anemia of the eyelid conjunctiva and a lung murmur.
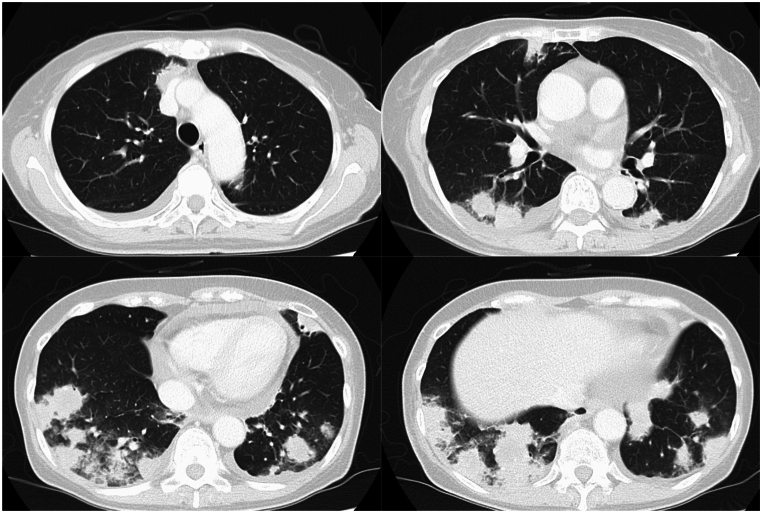
As shown in Table 1, blood tests revealed elevated lactate dehydrogenase and sIL-2R levels with normal leukocyte counts. CT showed multiple mass lesions with marginal irregularities and ground-glass opacity, a small amount of bilateral pleural effusion, and hepatosplenomegaly, but no lymphadenopathy in the thoracic or abdominal cavity (Fig. 1).
Table 1.
Laboratory data on admission.
| Complete blood counts | Biochemistry | |||||||
|---|---|---|---|---|---|---|---|---|
| WBC | 3560 | /μL | Alb | 2.9 | g/dL | CEA | 1.6 | ng/mL |
| Neut. | 77.3 | % | AST | 46 | U/L | CYFRA | 2.6 | ng/mL |
| Lymph. | 17.4 | % | ALT | 42 | U/L | Pro-GRP | 28.1 | pg/mL |
| Mono. | 3.9 | % | LDH | 439 | U/L | β-D glucan | ⟨6 | pg/mL |
| Eosi. | 0 | % | T-bil | 2.3 | mg/dL | HIV-1 RNA | ⟨20 | copy/mL |
| Abnormal lymph | 0 | % | BUN | 11.4 | mg/dL | EBV DNA | 70 | 10(3)copy/mL |
| RBC | 413 | 10(4)/μL | Cre | 0.3 | mg/dL | |||
| Hb | 11.3 | g/dL | Na | 137 | mEq/L | |||
| Plt | 4.8 | 10(4)/μL | K | 3.3 | mEq/L | |||
| Coagulation tests | Cl | 7.9 | mEq/L | |||||
| PT-INR | 0.91 | CRP | 1.4 | mg/dL | ||||
| APTT | 27.1 | s | sIL-2R | 1467 | U/mL | |||
| Fib | 287.1 | mg/dL | ferritin | 284 | ng/mL | |||
| D-dimer | 0.8 | μ/mL | KL-6 | 294 | U/mL | |||
Fig. 1.
Chest computed tomography on admission showed multiple mass lesions with marginal irregularities and ground-glass opacity.
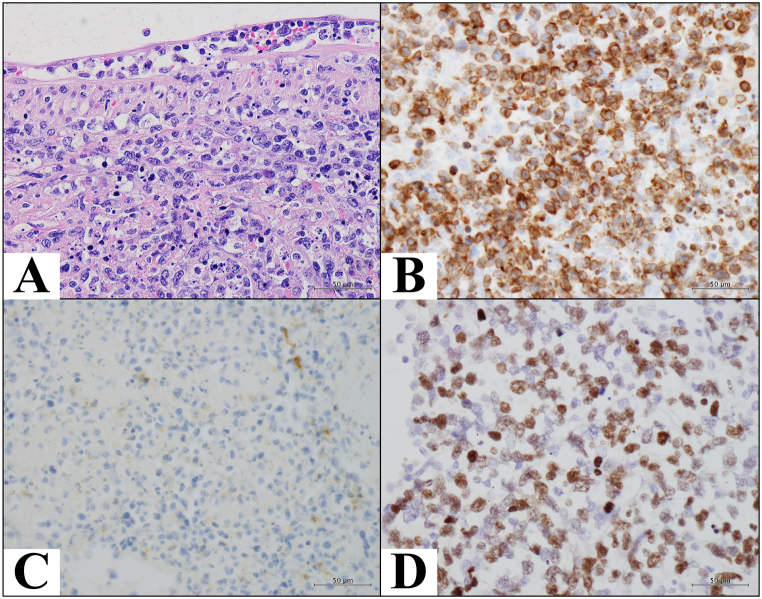
On the second day of hospitalization, since the respiratory failure was worsening and more robust biopsy procedure that could lead to a definitive diagnosis was needed, thoracoscopic lung biopsy was performed on the peripheral lingular segment of the left lung. Histopathological examination revealed diffuse infiltration and proliferation of medium-to-large atypical lymphocytes with coagulative necrosis (Fig. 2). Immunohistochemically, the tumor cells were positive for CD3, CD56, TIA-1, granzyme B, and Ki-67 (labeling index, 98 %) and negative for CD20, CD79a, and CD30. Furthermore, in situ hybridization for EBV-encoded RNA was positive, strongly supporting the diagnosis of NK/T-cell lymphoma. Additionally, with no extrapulmonary lesions or a history of ENKL, the patient was diagnosed with primary pulmonary ENKL. Although she required mechanical ventilation for a few days because of severe respiratory failure, DeVIC therapy (dexamethasone, etoposide, ifosfamide, carboplatin), which was administered on day 9, showed remarkable efficacy, and her respiratory condition promptly recovered. CT showed mixed improvement and exacerbation of the pulmonary lesions, and the patient was treated with SMILE therapy (dexamethasone, methotrexate, ifosfamide, L-asparaginase, etoposide) on day 30. However, this therapy was ineffective. On the 51st day of hospitalization, the patient died of progressive disease.
Fig. 2.
Pathological findings of the thoracoscopic lung biopsy. Diffuse infiltration and proliferation of medium to large, atypical lymphocytes were observed (hematoxylin and eosin; × 400 (A)). The tumor cells were positive for CD3 (B) and CD56 (C) by immunohistochemistry. Furthermore, in situ hybridization for Epstein-Barr virus (EBV)-encoded RNA (EBER) was positive (D).
3. Discussion
ENKL is an EBV-associated progressive disease with poor prognosis, predominantly affecting the nasal cavity and upper respiratory tract. In this case, we diagnosed ENKL via thoracoscopic lung biopsy despite respiratory failure in the patient. Chemotherapy was initiated while the patient was on a ventilator because of respiratory failure, and the patient was weaned from the ventilator after a temporary response. However, she died of progressive disease.
There have been 19 reported cases [[4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20]] of primary pulmonary ENKL with detailed information on the clinical course, including the present case. As summarized in Table 2, most patients presented with persistent fever (n = 16/19) and cough (n = 13/19). Five patients presented with dyspnea. Bilateral nodules, masses, and/or infiltrates were often observed on CT (n = 12/19), although unilateral infiltrates and/or masses (n = 6/19) or diffuse ground-glass opacities were also reported (n = 1/19). Based on the above findings, 12 of the 19 patients were clinically diagnosed with bacterial pneumonia and initially treated with antibiotics, although 18 of the 19 patients showed normal or decreased peripheral white blood cell counts on admission, which is an atypical clinical presentation for bacterial pneumonia.
Table 2.
A summary of clinical features of published 19 case reports [[4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20]].
| N = 19 | |
|---|---|
| Symptom | |
| Fever | 16 |
| Cough | 13 |
| Dyspnea | 5 |
| CT sign | |
| Bilateral nodules, masses, and/or infiltrates | 12 |
| Unilateral infiltrates and/or masses | 6 |
| Diffuse ground-glass opacities | 1 |
| White blood cell counts | |
| Normal or decreased | 18 |
| Increased | 1 |
| Treated with antibiotics initially | 12 |
| Biopsy modalitya(diagnostic/non-diagnostic) | |
| Bronchoscopy | 10(5/5) |
| Transthoracic needle biopsy | 9(6/3) |
| Surgical biopsy | 5(4/1) |
Excluding four cases diagnosed by other modalities: one via thoracentesis, one via liver biopsy and two via autopsy.
For pathological diagnosis, bronchoscopy was performed in 10 cases, of which 5 were diagnostic, including one case in which the patient underwent a second procedure. Transthoracic needle biopsy was performed in 9 cases and surgical lung biopsy (SLB) in 5 cases, of which 6 and 4 of them, respectively, were diagnostic. In the other cases, one was diagnosed via thoracentesis, one via liver biopsy, and two via autopsy. As ENKL has a strong tendency for necrosis in tumor tissues, a sufficiently large amount of biopsy tissue is required for an accurate diagnosis.
The reported outcomes of patients with primary pulmonary ENKL were poor. Eight of the 19 patients received the best supportive care and died within a month. Nine of the 11 patients treated with chemotherapy, including the present case, died within 7 months, and only 2 patients were cured. Therefore, for the suspected pneumonia case, we should include ENKL in the differential diagnosis and select appropriate biopsy method, including SLB, for early diagnosis and treatment, especially when the patient's white blood cell count is within the normal range and/or antimicrobial therapy is ineffective.
4. Conclusion
Primary pulmonary ENKL has a poor prognosis owing to rapid disease progression. Because its clinical features often mimic those of bacterial pneumonia, primary pulmonary ENKL should be suspected in patients with an atypical clinical course for an infectious disease. Furthermore, as ENKL has a strong tendency for necrosis, we should select appropriate biopsy method to take sufficient amount of specimens for an accurate diagnosis.
Patient consent for publication
Patient's consent was obtained through an opt-out method.
Funding source
This study did not receive any financial support.
CRediT authorship contribution statement
Michihiko Tanaka: Writing – original draft. Yasushi Horimasu: Writing – review & editing. Kazuma Kawamoto: Writing – review & editing, Data curation. Taro Edahiro: Writing – review & editing, Data curation. Kakuhiro Yamaguchi: Writing – review & editing, Data curation. Shinjiro Sakamoto: Writing – review & editing, Data curation. Takeshi Masuda: Writing – review & editing, Data curation. Taku Nakashima: Writing – review & editing, Data curation. Hiroshi Iwamoto: Writing – review & editing, Data curation. Kazunori Fujitaka: Writing – review & editing, Data curation. Hironobu Hamada: Writing – review & editing, Data curation. Tatsuo Ichinohe: Writing – review & editing, Data curation. Noboru Hattori: Writing – review & editing, Data curation.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
No conflicts of interest.
Handling Editor: DR AC Amit Chopra
References
- 1.Borie R., Wislez M., Antoine M., Copie-Bergman C., Thieblemont C., Cadranel J. Pulmonary mucosa-associated lymphoid tissue lymphoma revisited. Eur Respir. 2016;47:1244–1260. doi: 10.1183/13993003.01701-2015. [DOI] [PubMed] [Google Scholar]
- 2.Li S., Feng X., Li T., et al. Extranodal NK/T-cell lymphoma, nasal type: a report of 73 cases at MD Anderson Cancer Center. Am. J. Surg. Pathol. 2013;37:14–23. doi: 10.1097/PAS.0b013e31826731b5. [DOI] [PubMed] [Google Scholar]
- 3.Au W.Y., Weisenburger D.D., Intragumtornchai T., et al. Clinical differences between nasal and extranasal natural killer/t-cell lymphoma: a study of 136 cases from the International Peripheral T-Cell Lymphoma project. Blood. 2009;113:3931–3937. doi: 10.1182/blood-2008-10-185256. [DOI] [PubMed] [Google Scholar]
- 4.Lee B.H., Kim S.Y., Kim M.Y., et al. CT of nasal-type T/NK cell lymphoma in the lung. J. Thorac. Imag. 2006;21:37–39. doi: 10.1097/01.rti.0000179472.46877.28. [DOI] [PubMed] [Google Scholar]
- 5.Laohaburanakit P., Hardin K.A. NK/T cell lymphoma of the lung: a case report and review of literature. Thorax. 2006;61:267–270. doi: 10.1136/thx.2004.025767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tai C.F., Chang L.Y., Lin D.T., Lin K.H., Jou S.T., Yang Y.L. A case of natural killer cell lymphoma presenting with bilateral pleural effusions and hemophagocytic lymphohistocytosis. Pediatr. Blood Cancer. 2009;52:666–669. doi: 10.1002/pbc.21943. [DOI] [PubMed] [Google Scholar]
- 7.Liu C.H., Wang H.H., Perng C.L., Peng C.K., Chian C.F., Shen C.H. Primary extranodal NK/T-cell lymphoma of the lung: mimicking bronchogenic carcinoma. Thorac Cancer. 2014;5:93–96. doi: 10.1111/1759-7714.12021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oshima K., Tanino Y., Sato S., et al. Primary pulmonary extranodal natural killer/T-cell lymphoma: nasal type with multiple nodules. Eur. Respir. J. 2012;40:795–798. doi: 10.1183/09031936.00123911. [DOI] [PubMed] [Google Scholar]
- 9.Gong L., Wei L.X., Huang G.S., et al. Identification of genuine primary pulmonary NK cell lymphoma via clinicopathologic observation and clonality assay. Diagn. Pathol. 2013;19:140. doi: 10.1186/1746-1596-8-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gui W., Yang B., Shen Q., et al. Successful treatment with L-asparaginase-based regimen for primary pulmonary NK/T cell lymphoma: a case report and review of the literature. Clin. Res. J. 2015;9:493–496. doi: 10.1111/crj.12156. [DOI] [PubMed] [Google Scholar]
- 11.Lee S., Shin B., Yoon H., Lee J.Y., Chon G.R. A case of primary pulmonary NK/T cell lymphoma presenting as pneumonia. Respir Med Case Rep. 2015;17:1–4. doi: 10.1016/j.rmcr.2015.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Takahasi H., Horio Y., Kojima K., et al. A case of primary pulmonary extranodal NK/T-cell lymphoma diagnosed by bronchoalveolar lavage. J Jpn Soc Respir Endosc. 2015;37:423–428. (in Japanese, Abstract in English) [Google Scholar]
- 13.Chien C.C., Lee H.S., Lin M.H., Hsieh P.P. Primary extranodal natural killer/T-cell lymphoma of bronchus and lung: a case report and review of literature. Thorac Cancer. 2016;7:140–144. doi: 10.1111/1759-7714.12254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Song M.J., Kim J.Y., Choi J.S., et al. Primary pulmonary extranodal natural killer/T-cell lymphoma, nasal type presenting as diffuse ground glass opacities: a case report. J. Kor. Med. Sci. 2017;32:1727–1730. doi: 10.3346/jkms.2017.32.10.1727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang J., Wang M., Yang X., Liu C., He X. Primary pulmonary extranodal NK/T- cell lymphoma of nasal type misdiagnosed as pneumonia: a case report and literature review. Medicine (Baltim.) 2017;96 doi: 10.1097/MD.0000000000008914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mori H., Ebisawa K., Nishimura M., Kanazawa K. Late diagnosis: a case of rapidly progressive extranodal NK/T cell lymphoma, nasal type. BMJ Case Rep. 2018 doi: 10.1136/bcr-2017-221019. bcr2017221019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Qiu Y., Hou J., Hao D., Zhang D. Primary pulmonary NK/T-cell lymphoma: a case report and literature review. Mol Clin Oncol. 2018;8:753–756. doi: 10.3892/mco.2018.1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yabushita T, Yoshioka S, Furumiya T, et al. The impact of early diagnosis on the prognosis of extranodal NK/T-cell lymphoma with massive lung involvement: a case report. BMC Pulm. Med. 19:48. [DOI] [PMC free article] [PubMed]
- 19.Hu Q., Xu L., Zhang X., Wang J., Zhou Z. Primary pulmonary extranodal natural killer/T-cell lymphoma (ENKTL), nasal type. Two case reports and literature review. Medicine (Baltim.) 2020;99 doi: 10.1097/MD.0000000000020822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang Y., Wang Z., Wu C., Zhao X., Ji N., Huang M. Primary pulmonary extranodal NK/T-cell lymphoma: a case report and literature review. Transl. Cancer Res. 2020;9:7359–7365. doi: 10.21037/tcr-20-2151. [DOI] [PMC free article] [PubMed] [Google Scholar]