Abstract
Few studies have explored the association between residential noise exposure and burnout. In this study, we investigated the association between residential noise exposure and burnout prevalence among 5416 health-care workers in Taiwan from 2012 to 2017. Burnout was evaluated using the Mandarin version of the Copenhagen Burnout Inventory by considering both continuous and binary measures. We applied ordinary Kriging models to calculate the annual average residential noise exposure at an individual level. Multivariable linear regression models and logistic regression models were employed. Restricted cubic splines were used to explore dose–response relationships. The median age of the health-care workers was 31.5 years. In the multivariable linear regression models, exposure to residential noise (per 1 dBA) was associated with increases in personal burnout and work-related burnout scores by 1.59 ± 0.25 and 1.38 ± 0.20, respectively. In the multivariable logistic regression models, the adjusted odds ratios were 1.24 (95% confidence interval [CI]: 1.16, 1.32) for personal burnout and 1.19 (95% CI: 1.13, 1.26) for work-related burnout per 1-dBA increase in residential noise exposure. Linear dose–response associations of burnout with residential noise level were detected. Our findings suggest that exposure to residential noise may increase the risk of burnout among health-care workers.
Keywords: Burnout, Cross-sectional study, Healthcare workers, Mediation analysis, Residential noise exposure
Subject terms: Environmental sciences, Health occupations
Introduction
Noise exposure is a pervasive public health hazard that can cause not only hearing disorders1 but also sleep disorders, cardiovascular disease, and impaired cognitive function2–5. Researchers have extended their focus from occupational noise to environmental noise1,6–9. A study conducted in six European countries revealed that traffic noise was the leading cause of disease burden, second only to fine particulate air pollution10. A European environment agency reported that more than 100 million people in Europe are exposed to harmful levels of noise pollution in their environment, with 22 million individuals experiencing chronic high annoyance and 6.5 million enduring chronic high sleep disturbance11.
A growing body of evidence has indicated that environmental noise exposure is linked to mental health problems such as annoyance and disturbed sleep1,12. Affecting approximately 16% of the global population, psychiatric disorders constitute a formidable public health challenge13. Burnout, particularly that affecting health-care workers, has been recognized as a major mental health concern14,15. Shanafelt et al. reported that more than half of U.S. physicians experience symptoms of burnout15. A stress response characterized by emotional exhaustion, physical fatigue, and cognitive wariness, burnout is associated with declines in the physical and mental health of health-care workers, which may in turn compromise quality of care and patient safety16,17. A prospective longitudinal study detected a significant association between a high level of burnout and an increase in self-perceived major medical errors18. To develop effective strategies for preventing burnout, modifiable risk factors must be identified.
Several epidemiological studies have reported the positive associations of occupational noise with burnout, stress, and annoyance among nurses18–23. By contrast, few studies have examined the effect of occupational noise exposure on the risk of burnout among other types of health-care workers, such as physicians or medical technicians. Furthermore, epidemiological studies have indicated that compared with daytime noise exposure, nighttime noise exposure has stronger associations with sleep and cardiovascular disease24,25. This implies the potential adverse role of residential noise in the development of burnout. Long-term residential noise exposure can also lead to poor sleep, resulting in increased burnout1,26. Compared with hospital environmental noise (caused by the use of medical equipment and alarms), residential environmental noise is more likely to be controlled by policy-based environmental noise control strategies. Therefore, we conducted a cross-sectional study to systematically investigate the association of burnout with annual average exposure to residential noise exposure among health-care workers.
Results
Study population characteristics
The characteristics of the 5416 individuals enrolled in the present study are summarized in Table 1. The medians (Q1, Q3) of age and body mass index (BMI) were 31.5 (26.0, 38.8) years and 22 (19.9, 24.9), respectively. The medians (Q1, Q3) for weekly working hours and daily sleeping hours were 42 (40, 48) hours and 7 (6, 7) hours, respectively (Table 1). The men-to-women ratio was approximately 1:3. The prevalence of smoking, alcohol consumption, hypertension, and diabetes mellitus were 6.1%, 31.7%, 4.0%, and 1.3%, respectively (Table 1). The median (Q1, Q3) of personal burnout score was 45.8 (33.3, 58.3), and 32.7% of the study population was classified as having moderate-to-high burnout. The median (Q1, Q3) of the work-related burnout score was 46.4 (35.7, 53.6), and 50.1% of the study population was classified as having moderate-to-high burnout (Table 1). Residential noise level ranged from 53.16 to 67.52 dBA, with the median (Q1, Q3) being 63.48 (62.93, 64.12) dBA (Table S1).
Table 1.
Characteristics of healthcare workers by median level of residential noise pollution.
| Characteristics | Available N | Overall | < 63 dB Lden (N = 1748) |
≥ 63 dB Lden (N = 3668) |
P-value |
|---|---|---|---|---|---|
| Age (Year), median (Q1, Q3) | 5416 | 31.5 (26.0, 38.8) | 28.6 (24.7, 35.5) | 32.8 (26.9, 40.0) | < 0.001 |
| Female, n (%) | 5416 | 4103 (75.8) | 1326 (75.9) | 2777 (75.1) | 0.905 |
| Smoking, n (%) | 5197 | 318 (6.1) | 113 (6.64) | 205 (5.86) | 0.271 |
| Alcohol consumption, n (%) | 2943 | 933 (31.7) | 334 (32.8) | 599 (31.1) | 0.348 |
| Body mass index, (kg/m2), median (Q1, Q3) | 4999 | 22.0 (19.9, 24.9) | 21.8 (19.6, 24.7) | 22.1 (20.0, 25.1) | < 0.001 |
| Working hours (hours), median (Q1, Q3) | 2242 | 42.0 (40.0, 48.0) | 40.0 (40.0, 48.0) | 42.3 (40.0, 48.0) | 0.570 |
| Sleep hours (hours), median (Q1, Q3) | 2242 | 7.0 (6.0, 7.0) | 7.0 (6.0, 7.0) | 6.5 (6.0, 7.0) | 0.027 |
| Hypertension, n (%) | 5416 | 218 (4.0) | 54 (3.1) | 164 (4.5) | 0.016 |
| Diabetes mellitus, n (%) | 5416 | 68 (1.3) | 13 (0.7) | 55 (1.5) | 0.020 |
| Job type, n (%) | < 0.001 | ||||
| Physician group | 5416 | 475 (8.8) | 158 (9.0) | 317 (8.6) | |
| Nursing group | 5416 | 1393 (25.7) | 523 (29.9) | 870 (23.7) | |
| Administration group | 5416 | 630 (11.6) | 203 (11.6) | 427 (11.6) | |
| Medical technician group | 5416 | 500 (9.2) | 162 (9.3) | 338 (9.2) | |
| Unknown | 5416 | 2418 (44.7) | 702 (40.2) | 1716 (46.8) | |
| Burnout, personal (score), median (Q1, Q3) | 5416 | 45.8 (33.3, 58.3) | 45.8 (33.3, 54.2) | 45.8 (33.3, 58.3) | < 0.001 |
| Categorical, n (%) | |||||
| Level: low (≤ 50) | 5416 | 3644 (67.3) | 1252 (71.6) | 2392 (65.2) | < 0.001 |
| Level: moderate (51–69) | 5416 | 1010 (18.7) | 287 (16.4) | 723 (19.7) | |
| Level: high (≥ 70) | 5416 | 762 (14.1) | 209 (12.0) | 553 (15.1) | |
| Burnout, work-related (score), median (Q1, Q3) | 5416 | 46.4 (35.7, 53.6) | 42.9 (35.7, 53.6) | 46.4 (35.7, 53.6) | 0.001 |
| Categorical, n (%) | |||||
| Level: low (≤ 45) | 5416 | 2700 (49.9) | 930 (53.2) | 1770 (48.3) | 0.001 |
| Level: moderate (46–59) | 5416 | 1817 (33.6) | 565 (32.3) | 1252 (34.1) | |
| Level: high (≥ 60) | 5416 | 899 (16.6) | 253 (14.5) | 646 (17.6) | |
Q1 first quartile, Q3third quartile.
Residential noise exposure–burnout association
In the linear regression model, for each 1-dBA increase in the annual average residential noise level, personal and work-related burnout scores increased by 1.43 ± 0.24 and 1.10 ± 0.20 in the crude model, respectively (Table 2). Burnout score was significantly associated with noise exposure after adjustment for age, sex, BMI, smoking status, working hours, sleeping hours, hypertension, diabetes mellitus, and job type (P < 0.001; Table 2, model 2). The scores of individuals exposed to a noise level of ≥ 63 dBA were significantly higher—specifically, 2.36 ± 0.54 higher for personal burnout and 1.87 ± 0.44 higher for work-related burnout—than those of individuals exposed to a noise level of < 63 dBA (P < 0.001; Table 2, model 2).
Table 2.
Estimated associations of average annual residential noise exposure with burnout score between 2012 and 2018.
| Crude model | Model 1a | Model 2b | ||||
|---|---|---|---|---|---|---|
| β (SD) | P value | β (SD) | P value | β (SD) | P value | |
| Personal burnout | ||||||
| Noise exposure | ||||||
| Per 1 dBA ↑ | 1.43 (0.24) | < 0.001 | 1.60 (0.25) | < 0.001 | 1.59 (0.25) | < 0.001 |
| <63 dBA | Reference | Reference | Reference | |||
| ≥63 dBA | 2.29 (0.53) | < 0.001 | 2.48 (0.54) | < 0.001 | 2.36 (0.54) | < 0.001 |
| Work-related burnout | ||||||
| Noise exposure | ||||||
| Per 1 dBA ↑ | 1.10 (0.20) | < 0.001 | 1.38 (0.20) | < 0.001 | 1.38 (0.20) | < 0.001 |
| <63 dBA | Reference | Reference | Reference | |||
| ≥63 dBA | 1.51 (0.44) | < 0.001 | 1.97 (0.4) | < 0.001 | 1.87 (0.44) | < 0.001 |
BMI body mass index, SD standard deviation.
aAdjusted for age, sex, BMI, smoking status, alcohol consumption, hypertension, diabetes mellitus, working hours, and sleeping hours.
bAdjusted for age, sex, BMI, smoking status, alcohol consumption, hypertension, diabetes mellitus, working hours, sleeping hours, and job type.
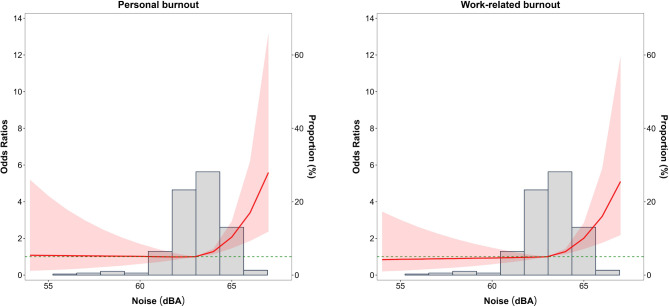
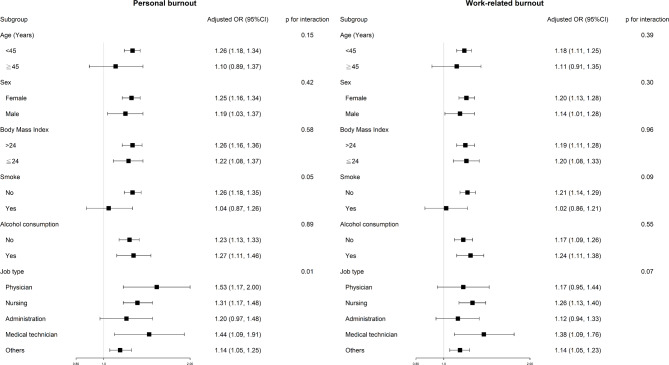
In the logistic regression model, each 1-dBA increase in residential noise level was associated with a 24% (95% confidence interval [CI]: 16%, 32%) increase in the risk of moderate or high personal burnout and a 19% (95% CI: 13%, 26%) increase in the risk of moderate or high work-related burnout (Table 3, model 2). Compared with individuals with an annual average residential noise exposure of < 63 dBA, those with an annual average exposure of ≥ 63 dBA had a 36% (95% CI: 19%, 54%) higher risk of personal burnout and a 29% (95% CI: 15%, 46%) higher risk of work-related burnout (Table 3, model 2). A positive association was identified between residential noise exposure and burnout, and this correlation increased in magnitude with the level of exposure to noise hazards (Fig. 1). When noise exposure surpassed 67 dBA, the risk of both personal fatigue and work-related exhaustion increased by more than fivefold (Fig. 1). In the subgroup analysis, we observed that the associations between residential noise exposure and personal burnout were significantly modified by job type (P for interaction = 0.01, Fig. 2).
Table 3.
Association of average annual residential noise exposure and burnout status between 2012 and 2018.
| Crude Model | Model 1a | Model 2b | |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Personal burnout (low vs. moderate and high level) | |||
| Noise exposure | |||
| Per 1 dBA ↑ | 1.22 (1.15–1.29) | 1.24 (1.16–1.32) | 1.24 (1.16–1.32) |
| < 63 dBA | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| ≥ 63 dBA | 1.35 (1.19–1.52) | 1.37 (1.20–1.55) | 1.36 (1.19–1.54) |
| Work-related burnout (low vs. moderate and high level) | |||
| Noise exposure | |||
| Per 1 dBA ↑ | 1.14 (1.08–1.21) | 1.19 (1.13–1.26) | 1.19 (1.13–1.26) |
| < 63 dBA | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| ≥ 63 dBA | 1.22 (1.09–1.37) | 1.30 (1.16–1.47) | 1.29 (1.15–1.46) |
BMI body mass index, OR odd ratio.
aAdjusted for age, sex, BMI, smoking status, alcohol consumption, hypertension, diabetes mellitus, working hours, and sleeping hours.
bAdjusted for age, sex, BMI, smoking status, alcohol consumption, hypertension, diabetes mellitus, working hours, sleeping hours, and job type.
Fig. 1.
Adjusted odds ratios (ORs) for burnout status according to the annual average noise levels (dBA). Solid lines represent adjusted ORs based on restricted cubic splines for each variability scale with knots at the 10th (as a reference), 50th and 90th percentiles. Shaded areas represent 95% confidence intervals (CIs).
Fig. 2.
Association between residential noise exposure and personal- and work-related burnout in stratified analyses.
In sensitivity analyses, significantly positive associations were noted under various burnout score thresholds (low or moderate vs. high; Table S2) and under various combinations of confounders (Tables S3,S4). The natural direct effect of residential noise exposure on personal and work-related burnout was 36% and 30% higher, respectively, in cases with high levels of residential noise exposure (≥ 63 dBA) than in cases with low levels of residential noise exposure (< 63 dBA). The natural indirect effect was increased by 1% for both personal and work-related burnout (Table S5). Our mediation analysis revealed that the proportion of mediation in the total effect ranged from 1.9 to 2.9% (Table S5).
Discussion
In the present study, annual average residential noise exposure was positively associated with burnout in health-care workers. Higher burnout risks associated with noise exposure were observed among physicians, nursing staff, and medical technicians than among administrators. Our findings also indicate different dose–response associations between residential noise exposure and burnout. When a noise exposure level of 63 dBA was used as a reference, the odds ratio (OR) for the risk of burnout doubled with a noise exposure of 65 dBA and increased by fivefold with a noise exposure of 67 dBA. To the best of our knowledge, we are the first to examine the direct and indirect effects (mediated by sleep deprivation) of residential noise on risk burnout. We discover that the association between residential noise exposure and burnout was partially mediated by sleep deprivation, suggesting the significant roles of pathways other than sleep.
Although epidemiological studies have reported associations between residential noise exposure and mental health27–30, the evidence on the effect of noise exposure on burnout is limited19,21,23,31,32. For noise exposure, previous studies have mostly relied on self-reported data instead of environmental noise measurements in the field19,21,23,31,32. Among these studies, three reported an association between noise exposure and burnout19,21,31, whereas two did not identify such an association23,32. McCullagh et al. (2022) identified the associations of noise exposure with greater stress and burnout scores in a study of 3818 nurses in the United States21. In a cross-sectional study of 151 nurses in Iran, Alidosti et al. (2016) discovered that higher exposure to environmental noise was associated with a higher risk of burnout19. Koch et al. (2015) reported that among childcare workers, the third tertile of subjective noise was associated with a 4.4 times higher risk of personal burnout relative to the lowest tertile31. However, Merces et al. (2020) conducted a cross-sectional study of 1125 primary health-care nursing professionals in Brazil and reported no significant association between noise exposure (negligible vs. unbearable) and burnout32. Terzi et al. (2019) conducted a cross-sectional study to assess the association of noise exposure, measured with a hand-held sound level meter at intensive care units, with burnout in 150 nurses23. No significant association between noise levels (≤ 60.99 dBA; 61–70.99 dBA; ≥ 71 dBA) and burnout (P > 0.05) was detected. The conflicting findings of the studies on the association between noise exposure and burnout may be explained by the discrepancies in the assessment of noise exposure between studies. Furthermore, most studies used a single-variable approach, with only Koch et al. (2015) adjusting for potential confounders such as workplace-related stresses, working hours, and psychosocial situations31. Additionally, the subjective perception of noise (measured using questionnaires) and objective noise exposure (measured using instruments) can both influence the effects of noise on clinical health outcomes33. Therefore, further studies involving the simultaneous use of multiple noise metrics are required to evaluate the association between noise and burnout.
We discovered that high proportions of health-care workers experienced personal burnout (30.1%) and work-related burnout (50.1%). Comparatively, a systematic review conducted in Taiwan, which reviewed 15 studies that used the Copenhagen Burnout Inventory (CBI) to assess physician burnout, reported average personal burnout scores ranging from 43.3 to 57.0 and work-related burnout scores from 39.9 to 57.034. Our study’s scores of 48.2 for personal burnout and 46.8 for work-related burnout align with these ranges. Furthermore, two systematic reviews that investigated burnout among health-care workers in various countries—including Australia, Egypt, Malaysia, Saudi Arabia, South Africa, and the United States—revealed that personal burnout prevalence and work-related burnout prevalence ranged from 38.3 to 75% and from 30.1 to 75.1%, respectively35,36. This variability in burnout prevalence may be attributed to differences in study populations, as well as national and workplace environments. More research is required to assess whether the effect of noise exposure remains significant across regions with varying prevalence rates of burnout.
In the subgroup analysis, we discovered that non-smokers had a higher risk of noise-related burnout compared with smokers (P-value for interaction = 0.05). A previous cross-sectional study on hospital workers in Taiwan reported that smokers had lower burnout scores relative to non-smokers37. One explanation could be that smoking activates the mesolimbic dopaminergic pathways, thereby enabling smokers to resist the negative effects of environmental noise exposure38. Additionally, smoking may impair the oxygen supply to the basal end of the cochlea, leading to increased auditory thresholds and consequently altered perceptions of noise39,40.
The biological mechanisms underlying the association between residential noise exposure and burnout remain unclear. A study suggested that long-term exposure to aircraft noise leads to hypothalamic–pituitary–adrenal (HPA) axis dysregulation and a flattened cortisol rhythm characterized by a small morning–evening difference41,42. Flattened diurnal cortisol profiles have been reported to be associated with fatigue, burnout, and vital exhaustion43–45. However, large-scale prospective investigations are required to evaluate the role of HPA axis dysregulation in the association between environmental noise exposure and burnout.
The present study has several strengths. First, the large study population provided adequate statistical power for assessing the association between residential noise exposure and burnout. Second, to the best of our knowledge, we are the first to explore the relationship between residential noise and burnout, along with the role of sleep in this relationship. The limitations of the present study are as follows. First, regardless of the consistency of the dose–response association between residential noise exposure and burnout, the cross-sectional nature of this investigation precluded causal inference. Second, we cannot completely exclude the possibility of residual confounding. The examination of various factors, such as occupational noise exposure (including music or other forms of noise from the headphones or earbuds of people in the vicinity), individual perceptions of noise, and psychosocial risk factors (e.g., stress, workload, shift work, family situation, interpersonal conflict, or lack of organizational justice), were not within the scope of the present study. However, given that we examined the data of health-care workers from a single hospital, the effects of organization-level variance on our findings were not considered. Furthermore, our results remained robust after we adjusted for average weekly working hours and job title in the model as proxies for work stress, shift work type, and workload. In our subgroup analysis, significant and positive associations were identified between noise exposure and burnout among physicians, nurses, and medical technicians (Table S6). Third, in our assessment of noise exposure, our use of a relatively large spatial resolution (1 km × 1 km) could have influenced individual estimates. However, because of the sparse distribution of noise stations, selecting a smaller grid resulted in higher root mean square error values. Fourth, given the healthy-worker effect, the association between residential noise exposure and burnout could have been underestimated.
In conclusion, residential noise exposure was associated with burnout among health-care workers. Although residential noise exposure may be considered for policy interventions aimed at burnout prevention, further studies, particularly large-scale prospective studies, are should be conducted to corroborate our findings.
Methods
Data source and study population
The data analyzed in our study were obtained from the Clinical Research Data Repository through the iHi platform operated by China Medical University Hospital (CMUH) in Taichung, Taiwan. Established in 2017 by the Big Data Center and the Office of Information Technology of CMUH, this integrated database contains information on approximately 2.8 million patients who sought care at CMUH between January 1, 2003, and December 31, 201846.
We conducted a cross-sectional study of various health-care workers at CMUH, namely administrators, medical technicians, nurses, and physicians. In the context of our study, the term “administrators” refers to non-medical personnel working within the hospital, including general office staff, researchers, and assistants. When undergoing their mandatory annual medical check-up, these employees are required to complete a burnout questionnaire. Personal information, lifestyle, and risk factors related to burnout were obtained from questionnaire records or electronic medical records. Because the questionnaire data were first made electronically available in 2012, we examined data on 5697 health-care workers for the period from January 1, 2012, to December 31, 2017. After excluding 279 individuals without available noise exposure data because of incomplete address information, the dataset comprising 5416 health-care workers were subjected to further analysis. Our study was approved by the Big Data Center of CMUH and the Research Ethical Committee/Institutional Review Board of CMUH, which waived the requirement for informed consent. Additionally, our study was conducted in accordance with the ethical guidelines outlined in the Declaration of Helsinki.
Outcome definition
Burnout status was defined on the basis of the Chinese version of the CBI (C-CBI), which consists of two subscales that assess work-related burnout and personal burnout47. The C-CBI was validated and demonstrated to have high internal consistency in a Taiwanese study (Cronbach’s alpha > 0.86) and correlations with other burnout-related factors47. Items in the C-CBI are scored on a Likert scale, with scores of 0, 25, 50, 75, and 100 corresponding to “never,” “seldom,” “sometimes,” “often,” and “always” responses, respectively. The total burnout score is calculated from the mean score of each question. Six questions are used to assess personal burnout (e.g., “How often do you feel emotionally exhausted?”), and seven questions are used to measure work-related burnout (e.g., “Is your work emotionally exhausting?”). In our study, personal burnout and work-related burnout were classified as low (average scores of ≤ 50 for personal burnout and ≤ 45 for work-related burnout), moderate (average scores of 50–70 for personal burnout and 45–60 for work-related burnout), and high (average scores of ≥ 70 for personal burnout and ≥ 60 for work-related burnout) in accordance with the recommendations of the Council of Labor Affairs, Executive Yuan, Taiwan48. In subsequent analyses, we treated burnout as both a continuous variable and a binary variable (low vs. moderate or high)48.
Residential noise exposure assessment
We estimated residential noise exposure from 2003 to 2017 by analyzing data collected by environmental noise stations maintained by the Taiwan Environmental Protection Administration in Taichung (Figs. S1,S2). During the study period, 21 noise stations were operational in 2012, and this number increased to 24 from 2013 to 2017. Of these 24 stations, half were traffic-related and located near major thoroughfares, whereas the other half were general environmental stations situated in typical neighborhoods. For each station, we initially calculated the day–evening–night levels (i.e., weighted equivalents of continuous noise levels; Lden dBA) on the basis of the number of effective days within each season, after which we estimated the annual average noise level. To estimate the spatial distribution of noise exposure, we performed ordinary kriging in ArcGIS (ArcMap, version 10.5; ESRI, Redlands, CA, USA). A widely applied interpolation approach, kriging has been employed to estimate noise exposure in various studies49–51. The spatial resolution of the annual noise exposure assessment was defined by 1 km × 1 km grids. The mean of the cross-validation root mean square error of each year was 4.9 ± 0.8 dBA (Fig. S3). To obtain data on individual-level noise exposure, we assigned the annual average noise data for each grid cell to each individual on the basis of their residential address. In subsequent analyses, we treated noise exposure as both a continuous variable and a binary variable (based on the median noise level of 63 dBA).
Covariates
The following covariates were considered: age at medical examination (continuous), sex (female vs. male), smoking status (ever vs. never), alcohol consumption (ever vs. never), BMI, diabetes mellitus (yes vs. no), hypertension (yes vs. no), working hours (continuous), sleeping hours (continuous), and job type (administrators, medical technicians, nurses, physicians, and others). Working hours were defined as the average number of hours worked per week in the past month prior to the date of the medical examination. Sleeping hours were defined as the average number of hours slept per day. Queries regarding working hours and sleeping hours were presented as open-ended questions. We used International Classification of Diseases, Ninth Revision (ICD-9) diagnoses and a history of using glucose-lowering or antihypertensive agents to define diabetes mellitus (ICD-9: 250) and hypertension (ICD-9: 401–405).
Statistical analysis
Continuous variables are expressed as medians (first quartile [Q1], third quartile [Q3]), and categorical variables are expressed as frequencies and percentages. To replace missing values for smoking status (4%), alcohol consumption (46%), BMI (8%), working hours (59%), and sleeping hours (59%), we performed multiple imputation by using an iterative Markov chain Monte Carlo procedure with 20 imputations and 100 iterations52. We employed univariable and multivariable linear regression models (β ± standard deviation) and logistic regression models (OR, 95% CI) to evaluate the associations between noise exposure and burnout. In model 1, adjustments were made for age, sex, BMI, smoking status, alcohol consumption, working hours, sleeping hours, hypertension, and diabetes mellitus. In model 2 (the full model), adjustments were made for job type. Burnout status (low vs. moderate or high) was selected as the main outcome for the models in subsequent analyses because it is more reflective of the effects of noise exposure than burnout score is. Furthermore, a restricted cubic spline model with three knots located at the 10th, 50th, and 90th percentiles of the overall noise distribution was employed to characterize the dose–response relationship between noise exposure and burnout. We performed a subgroup analysis to determine whether the association between noise exposure and burnout was modified by age (< 45 vs. ≥45 years), sex (male vs. female), BMI (< 24 vs. ≥24), smoking (yes vs. no), alcohol consumption (yes vs. no), and job type (administrators, medical technicians, nurses, physicians, and other). We included interaction terms for noise exposure and each of these factors to expand our model. Sensitivity analyses were conducted for various burnout score thresholds (low and moderate vs. high), and additional analyses were performed with varying combinations of confounders. Given the evidence supporting the associations between noise and sleep and between sleep deprivation and burnout, we conducted a mediation analysis to determine whether the association between noise exposure and burnout was mediated through sleep deprivation (≤ 6 h)26,52,53. The mediation analysis was performed using the SAS PROC CAUSALMED procedure, with the same control variable as those in the main analyses30. The CAUSALMED procedure is a statistical procedure that is based on the counterfactual framework, where regression-based estimation is used to estimate causal effects30. The outcome (burnout) and mediator (sleep deprivation) were dichotomized into low vs. moderate or high, and ≤ 6 vs. >6 h, respectively. For exposure (noise), we assessed the effects of both continuous and categorical scales (< 63 vs. ≥63 dBA), using 1000 bootstrap resamples to compute the CIs for causal mediation effects.
All analyses were performed using the following software: SAS software, Version 9.4, of the SAS System for Window (SAS Institute, Cary, NC, USA) and R (version 3.2.3; R Foundation for Statistical Computing, Vienna, Austria). On the basis of a two-sided test, the significance level was set at α = 0.05.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to thank Professor Jing-Shiang Hwang his insightful comments and suggestions that improved the manuscript. We appreciate the iHi Clinical Research Platform from the Big Data Center of CMUH for the data exploration, administrative, and statistical analytic support. We would like to thank the Health and Welfare Data Science Center (HWDC), Ministry of Health Welfare, and Health Data Science Center, China Medical University for providing administrative, technical, and funding support. This manuscript was edited by Wallace Academic Editing.
Author contributions
YTL wrote the initial draft of the manuscript. YTL, HYC, SJL, WCC, RTL, CCK and TCC were involved in acquisition of data and interpretation of results. YTL, CCK and TCC were involved in conception/design and data analysis. CCK and TCC sought funding and provided overall supervision. The authors read and approved the final manuscript.
Funding
This work was supported by the National Science and Technology Council, Taiwan [grant number: NSTC 111-2314-B-039-085, MOST 110-2321-B-468-001]; Academia Sinica, Taiwan [grant number: AS-SS-109-02]; and China Medical University Hospital, Taichung, Taiwan [grant number: DMR-113-177, DMR-108-BC-7, DMR-111-001].
Data availability
The corresponding author will on request detail the restrictions and any conditions under which access to some data may be provided.
Competing interests
The authors declare no competing interests.
Ethics approval
The study received approval from the Big Data Center of CMUH and the Research Ethical Committee/Institutional Review Board of CMUH, which waived the requirement for informed consent. Additionally, this study adhered to the ethical guidelines outlined in the Declaration of Helsinki.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Chin-Chi Kuo and Ta-Chien Chan contributed equally to this work.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-73649-5.
References
- 1.Basner, M. et al. Auditory and non-auditory effects of noise on health. Lancet. 383, 1325–1332. 10.1016/s0140-6736(13)61613-x (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vienneau, D. et al. Long-term exposure to transportation noise and diabetes mellitus mortality: a national cohort study and updated meta-analysis. Environ. Health: Global Access. Sci. Source. 23, 46. 10.1186/s12940-024-01084-0 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Faulkner, J. P. & Murphy, E. Estimating the harmful effects of environmental transport noise: an EU study. Sci. Total Environ. 811, 152313. 10.1016/j.scitotenv.2021.152313 (2022). [DOI] [PubMed] [Google Scholar]
- 4.Aasvang, G. M. et al. Burden of disease due to transportation noise in the nordic countries. Environ. Res. 231, 116077. 10.1016/j.envres.2023.116077 (2023). [DOI] [PubMed] [Google Scholar]
- 5.Münzel, T. et al. Transportation noise Pollution and Cardiovascular Health. Circul. Res. 134, 1113–1135. 10.1161/circresaha.123.323584 (2024). [DOI] [PubMed] [Google Scholar]
- 6.Dzhambov, A. M. & Dimitrova, D. D. Residential road traffic noise as a risk factor for hypertension in adults: systematic review and meta-analysis of analytic studies published in the period 2011–2017. Environ. Pollut. 240, 306–318. 10.1016/j.envpol.2018.04.122 (2018). [DOI] [PubMed] [Google Scholar]
- 7.Onakpoya, I. J., O’Sullivan, J., Thompson, M. J. & Heneghan, C. J. The effect of wind turbine noise on sleep and quality of life: a systematic review and meta-analysis of observational studies. Environ. Int. 82, 1–9. 10.1016/j.envint.2015.04.014 (2015). [DOI] [PubMed] [Google Scholar]
- 8.Stansfeld, S. A. et al. Aircraft and road traffic noise and children’s cognition and health: a cross-national study. Lancet. 365, 1942–1949. 10.1016/s0140-6736(05)66660-3 (2005). [DOI] [PubMed] [Google Scholar]
- 9.Zare Sakhvidi, M. J., Zare Sakhvidi, F., Mehrparvar, A. H., Foraster, M. & Dadvand, P. Association between noise exposure and diabetes: a systematic review and meta-analysis. Environ. Res. 166, 647–657. 10.1016/j.envres.2018.05.011 (2018). [DOI] [PubMed] [Google Scholar]
- 10.Hänninen, O. et al. Environmental burden of disease in Europe: assessing nine risk factors in six countries. Environ. Health Perspect. 122, 439–446. 10.1289/ehp.1206154 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.agency, E. e. Health risks caused by environmental noise in Europe. https://www.eea.europa.eu/publications/health-risks-caused-by-environmental. Accessed 16 Aug 2023.
- 12.Hegewald, J. et al. Traffic noise and Mental Health: a systematic review and Meta-analysis. Int. J. Environ. Res. Public. Health. 17 10.3390/ijerph17176175 (2020). [DOI] [PMC free article] [PubMed]
- 13.Rehm, J. & Shield, K. D. Global burden of Disease and the impact of Mental and Addictive disorders. Curr. Psychiatry Rep. 21, 10. 10.1007/s11920-019-0997-0 (2019). [DOI] [PubMed] [Google Scholar]
- 14.Morse, G., Salyers, M. P., Rollins, A. L., Monroe-DeVita, M. & Pfahler, C. Burnout in mental health services: a review of the problem and its remediation. Adm. Policy Ment Health. 39, 341–352. 10.1007/s10488-011-0352-1 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shanafelt, T. D. et al. Changes in burnout and satisfaction with work-life balance in Physicians and the General US Working Population between 2011 and 2014. Mayo Clin. Proc. 90, 1600–1613. 10.1016/j.mayocp.2015.08.023 (2015). [DOI] [PubMed] [Google Scholar]
- 16.Melamed, S., Shirom, A., Toker, S., Berliner, S. & Shapira, I. Burnout and risk of cardiovascular disease: evidence, possible causal paths, and promising research directions. Psychol. Bull. 132, 327–353. 10.1037/0033-2909.132.3.327 (2006). [DOI] [PubMed] [Google Scholar]
- 17.Salyers, M. P. et al. The relationship between Professional Burnout and Quality and Safety in Healthcare: a Meta-analysis. J. Gen. Intern. Med. 32, 475–482. 10.1007/s11606-016-3886-9 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.West, C. P., Tan, A. D., Habermann, T. M., Sloan, J. A. & Shanafelt, T. D. Association of resident fatigue and distress with perceived medical errors. Jama. 302, 1294–1300. 10.1001/jama.2009.1389 (2009). [DOI] [PubMed] [Google Scholar]
- 19.Alidosti, M., Babaei Heydarabadi, A., Baboli, Z., Nazarbigi, H. & Mobasheri, M. Association between job burnout and noise pollution among nurses in Behbahan city, Iran. J. Fundamentals Mental Health. 18, 103–108. 10.22038/jfmh.2016.6676 (2016). [Google Scholar]
- 20.Applebaum, D., Fowler, S., Fiedler, N., Osinubi, O. & Robson, M. The impact of environmental factors on nursing stress, job satisfaction, and turnover intention. J. Nurs. Adm. 40, 323–328. 10.1097/NNA.0b013e3181e9393b (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McCullagh, M. C., Xu, J., Dickson, V. V., Tan, A. & Lusk, S. L. Noise exposure and quality of Life among nurses. Workplace Health Saf. 70, 207–219. 10.1177/21650799211044365 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morrison, W. E., Haas, E. C., Shaffner, D. H., Garrett, E. S. & Fackler, J. C. Noise, stress, and annoyance in a pediatric intensive care unit. Crit. Care Med. 31, 113–119. 10.1097/00003246-200301000-00018 (2003). [DOI] [PubMed] [Google Scholar]
- 23.Terzi, B., Azizoğlu, F., Polat, Ş., Kaya, N. & İşsever, H. The effects of noise levels on nurses in intensive care units. Nurs. Crit. Care. 24, 299–305. 10.1111/nicc.12414 (2019). [DOI] [PubMed] [Google Scholar]
- 24.Münzel, T. et al. Adverse Cardiovascular effects of Traffic noise with a focus on Nighttime noise and the New WHO noise guidelines. Annu. Rev. Public Health. 41, 309–328. 10.1146/annurev-publhealth-081519-062400 (2020). [DOI] [PubMed] [Google Scholar]
- 25.Smith, M. G., Cordoza, M. & Basner, M. Environmental noise and effects on Sleep: an update to the WHO Systematic Review and Meta-analysis. Environ. Health Perspect. 130, 76001. 10.1289/ehp10197 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Söderström, M., Jeding, K., Ekstedt, M., Perski, A. & Akerstedt, T. Insufficient sleep predicts clinical burnout. J. Occup. Health Psychol. 17, 175–183. 10.1037/a0027518 (2012). [DOI] [PubMed] [Google Scholar]
- 27.Clark, C., Paunovic, K. & WHO Environmental Noise Guidelines for the European Region. A systematic review on environmental noise and quality of Life, Wellbeing and Mental Health. Int. J. Environ. Res. Public. Health. 15 10.3390/ijerph15112400 (2018). [DOI] [PMC free article] [PubMed]
- 28.Jensen, H. A. R., Rasmussen, B. & Ekholm, O. Neighbour and traffic noise annoyance: a nationwide study of associated mental health and perceived stress. Eur. J. Public. Health. 28, 1050–1055. 10.1093/eurpub/cky091 (2018). [DOI] [PubMed] [Google Scholar]
- 29.Sygna, K., Aasvang, G. M., Aamodt, G., Oftedal, B. & Krog, N. H. Road traffic noise, sleep and mental health. Environ. Res. 131, 17–24. 10.1016/j.envres.2014.02.010 (2014). [DOI] [PubMed] [Google Scholar]
- 30.Yung, Y. F. et al. Causal mediation analysis with the CAUSALMED procedure. In Proceedings of the SAS Global Forum 2018 Conference (pp. 1991–2018). SAS Institute Inc, Cary, NC. (2018).
- 31.Koch, P., Stranzinger, J., Nienhaus, A. & Kozak, A. Musculoskeletal symptoms and risk of Burnout in Child Care workers - a cross-sectional study. PLoS One. 10, e0140980. 10.1371/journal.pone.0140980 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Merces, M. C. D. et al. Prevalence and Factors Associated with Burnout Syndrome among Primary Health Care nursing professionals: a cross-sectional study. Int. J. Environ. Res. Public. Health. 17 10.3390/ijerph17020474 (2020). [DOI] [PMC free article] [PubMed]
- 33.Birk, M., Ivina, O., von Klot, S., Babisch, W. & Heinrich, J. Road traffic noise: self-reported noise annoyance versus GIS modelled road traffic noise exposure. J. Environ. Monit. 13, 3237–3245. 10.1039/c1em10347d (2011). [DOI] [PubMed] [Google Scholar]
- 34.Tsai, Y. L., Tung, Y. C. & Cheng, Y. Surveys of Burnout among Physicians in Taiwan. J. Acute Med. 8, 86–98. 10.6705/j.jacme.201809_8(3).0002 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reardon, M., Abrahams, R., Thyer, L. & Simpson, P. Review article: prevalence of burnout in paramedics: a systematic review of prevalence studies. Emerg. Med. Australasia: EMA. 32, 182–189. 10.1111/1742-6723.13478 (2020). [DOI] [PubMed] [Google Scholar]
- 36.Alahmari, M. A. et al. Prevalence of Burnout in Healthcare Specialties: a systematic review using Copenhagen and Maslach Burnout inventories. Med. Sci. Monitor: Int. Med. J. Experimental Clin. Res. 28, e938798. 10.12659/msm.938798 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lin, Y. L. et al. Modifiable risk factors related to burnout levels in the medical workplace in Taiwan: cross-sectional study. BMJ open. 9, e032779. 10.1136/bmjopen-2019-032779 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Petrelli, F., Scuri, S., Tanzi, E., Nguyen, C. & Grappasonni, I. Public health and burnout: a survey on lifestyle changes among workers in the healthcare sector. Acta bio-medica: Atenei Parmensis. 90, 24–30. 10.23750/abm.v90i1.7626 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li, X., Rong, X., Wang, Z. & Lin, A. Association between smoking and noise-Induced hearing loss: a Meta-analysis of Observational studies. Int. J. Environ. Res. Public. Health. 17 10.3390/ijerph17041201 (2020). [DOI] [PMC free article] [PubMed]
- 40.Prabhu, P., Varma, G., Dutta, K. K., Kumar, P. & Goyal, S. Influence of smoking on Ultra-high-frequency Auditory Sensitivity. J. Int. Adv. Otology. 13, 110–112. 10.5152/iao.2017.3412 (2017). [DOI] [PubMed] [Google Scholar]
- 41.Lefèvre, M. et al. Effects of aircraft noise exposure on saliva cortisol near airports in France. Occup. Environ. Med. 74, 612–618. 10.1136/oemed-2016-104208 (2017). [DOI] [PubMed] [Google Scholar]
- 42.Spreng, M. Possible health effects of noise induced cortisol increase. Noise Health. 2, 59–64 (2000). [PubMed] [Google Scholar]
- 43.Grossi, G., Perski, A., Osika, W. & Savic, I. Stress-related exhaustion disorder–clinical manifestation of burnout? A review of assessment methods, sleep impairments, cognitive disturbances, and neuro-biological and physiological changes in clinical burnout. Scand. J. Psychol. 56, 626–636. 10.1111/sjop.12251 (2015). [DOI] [PubMed] [Google Scholar]
- 44.Kumari, M. et al. Self-reported sleep duration and sleep disturbance are independently associated with cortisol secretion in the Whitehall II study. J. Clin. Endocrinol. Metab. 94, 4801–4809. 10.1210/jc.2009-0555 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ter Wolbeek, M., van Doornen, L. J., Coffeng, L. E., Kavelaars, A. & Heijnen, C. J. Cortisol and severe fatigue: a longitudinal study in adolescent girls. Psychoneuroendocrinology. 32, 171–182. 10.1016/j.psyneuen.2006.12.003 (2007). [DOI] [PubMed] [Google Scholar]
- 46.Chiang, H. Y. et al. Association between Preoperative Blood Glucose Level and hospital length of stay for patients undergoing appendectomy or laparoscopic cholecystectomy. Diabetes care. 44, 107–115. 10.2337/dc19-0963 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yeh, W. Y., Cheng, Y., Chen, C. J., Hu, P. Y. & Kristensen, T. S. Psychometric properties of the Chinese version of Copenhagen burnout inventory among employees in two companies in Taiwan. Int. J. Behav. Med. 14, 126–133. 10.1007/bf03000183 (2007). [DOI] [PubMed] [Google Scholar]
- 48.Lin, R. T., Lin, Y. T., Hsia, Y. F. & Kuo, C. C. Long working hours and burnout in health care workers: non-linear dose-response relationship and the effect mediated by sleeping hours-A cross-sectional study. J. Occup. Health. 63, e12228. 10.1002/1348-9585.12228 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Aumond, P. et al. Kriging-based spatial interpolation from measurements for sound level mapping in urban areas. J. Acoust. Soc. Am. 143, 2847. 10.1121/1.5034799 (2018). [DOI] [PubMed] [Google Scholar]
- 50.Huang, T., Chan, T. C., Huang, Y. J. & Pan, W. C. The Association between noise exposure and metabolic syndrome: a longitudinal cohort study in Taiwan. Int. J. Environ. Res. Public. Health. 17 10.3390/ijerph17124236 (2020). [DOI] [PMC free article] [PubMed]
- 51.Tsai, K. T., Lin, M. D. & Chen, Y. H. Noise mapping in urban environments: a Taiwan study. Appl. Acoust. 70, 964–972. 10.1016/j.apacoust.2008.11.001 (2009). [Google Scholar]
- 52.Austin, P. C., White, I. R., Lee, D. S. & van Buuren, S. Missing Data in Clinical Research: a tutorial on multiple imputation. Can. J. Cardiol. 37, 1322–1331. 10.1016/j.cjca.2020.11.010 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zaharna, M. & Guilleminault, C. Sleep, noise and health: review. Noise Health. 12, 64–69. 10.4103/1463-1741.63205 (2010). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The corresponding author will on request detail the restrictions and any conditions under which access to some data may be provided.