Abstract
Background
TV46000 is a long-acting subcutaneous antipsychotic (LASCA) formulation of risperidone approved for the treatment of schizophrenia in adults.
Methods
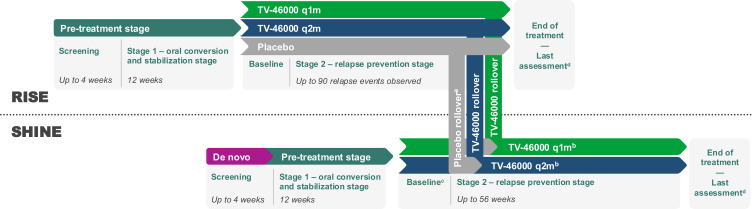
The RISE study (NCT03503318) compared TV-46000 once monthly (q1m) and once every 2 months (q2m) with placebo (1:1:1) in patients with schizophrenia who underwent stabilization on oral risperidone. The SHINE study (NCT03893825) evaluated the long-term safety, tolerability, and effectiveness of TV-46000 in patients who completed RISE without relapse (rollover; placebo rollover randomized [1:1] to q1m or q2m; TV-46000 rollover continued assigned treatment) or who were newly recruited (de novo; randomized [1:1] to q1m or q2m after oral stabilization). Patient-centered outcomes included the Schizophrenia Quality of Life Scale (SQLS), the 5-Level EuroQoL 5-Dimensions Questionnaire (EQ-5D-5L), the Personal and Social Performance Scale (PSP), and the Drug Attitudes Inventory 10-item version (DAI-10).
Results
In RISE, SQLS least-squares mean changes (SE) improved to last assessment (LA) for TV-46000 q1m (–4.15 [1.03]) and q2m (–3.28 [1.06]) but worsened for placebo (1.75 [1.07]; P<0.001 for both). PSP, EQ5D-5L, and DAI-10 showed similar trends. In SHINE, SQLS decreased (improved) at LA for both TV-46000 q1m (−0.43 [0.98]) and q2m (−2.16 [0.98]); reductions were observed in the de novo (q2m only) and placebo rollover (q1m and q2m) cohorts, but not for the TV46000 rollover cohort. Results for PSP, EQ5D-5L, and DAI-10 were consistent with those reported in the RISE study.
Conclusion
Improvements in patient-centered outcomes were observed across cohorts, with the largest improvements observed for patients who began TV-46000 during SHINE (ie, de novo and placebo rollover cohorts), while gains made during RISE were minimally improved or maintained in the TV-46000 rollover cohort, indicating the benefit of uninterrupted TV-46000 treatment. These data support the effectiveness of TV-46000 to improve patient-centered outcomes in patients with schizophrenia.
Keywords: schizophrenia, long-acting injectable, risperidone, patient-centered outcomes
Plain Language Summary
RISE and SHINE were clinical studies where patients with schizophrenia received TV-46000. TV-46000 is injected under the skin once monthly or once every 2 months to treat schizophrenia in adults. In RISE, patients took pills for the first 3 months, and then received injections under the skin. Some patients received inactive (placebo) injections. Comparing results among groups showed the effectiveness and side effects of TV-46000. Patients who completed RISE could continue into SHINE. SHINE included patients who had not been part of RISE as well. All patients received TV-46000 in SHINE to see if results were the same long term. This report summarizes the results of patient-centered outcomes. These included measures of quality of life and attitudes toward the medicine. In RISE, quality of life and attitudes toward the medicine improved with TV-46000, but worsened with placebo. In SHINE, the patient-centered outcomes also improved. The largest improvements were for patients who began taking TV-46000 during SHINE. This analysis showed that there is a benefit in taking TV-46000 for longer times without breaks. It also showed that TV-46000 improves quality of life and attitudes toward the medicine.
Introduction
Schizophrenia is a chronic disease that imposes serious physical, social, and economic burden on those affected by it.1 The disease affects more than 20 million individuals globally,2 and has a lifetime prevalence of ~1% globally3,4 and ~0.5–1.9% in the United States.5,6 Preventing relapse is an important goal of maintenance treatment in patients with psychotic disorders, including schizophrenia.7 Relapse may lead to hospitalization/rehospitalization,7,8 slow and incomplete recovery,8 progressive cognitive and functional decline,8,9 treatment-resistant illness,8 and reduced ability to maintain employment or relationships.8 Nonadherence with antipsychotic medication is the most common and most strongly associated predictor of relapse in schizophrenia.10
Patient-centered outcomes, and more specifically patient-reported outcomes (PROs), allow clinicians and researchers to gather data on medical conditions and treatments from the perspective of the patients.11 These outcomes provide perspectives that differ from measures of psychopathology, from informing patients and clinicians on treatment selection12 to providing patients’ perspectives on domains (such as fatigue and pain) that are difficult to measure with clinical outcomes alone,12 and can potentially describe outcomes that are relevant to the definitions of recovery.13–18 Although exact definitions of recovery in schizophrenia have not been determined, several suggestions have been made that recovery should include not only clinical improvements but also social/functional improvements.19–21 In a recently published scoping review22 of clinical outcome assessments used in the past 10 years in the field of schizophrenia and related disorders, a large portion of the 66 outcome assessments investigated were patient reported, suggesting that the implementation of PROs is becoming increasingly important in the field of schizophrenia.22 Mental health-specific and schizophrenia-specific PROs were also found to have strong psychometric properties (reliability and external validity).22,23
Patient-centered outcomes have been increasingly included in clinical trials, and their inclusion is now encouraged by various regulatory bodies,12,24–26 including the United States Food and Drug Administration (FDA).27 PRO data collected during clinical trials inform regulatory bodies about patient perspectives when deriving conclusions about treatment effects at the time of medical product approval.27
The use of long-acting injectable antipsychotics (LAIs) in the treatment of schizophrenia has been associated with reduced relapse and hospitalization rates over daily oral antipsychotic agents, as well as improved treatment adherence and quality of life (QoL).28–34
TV-46000 is a long-acting subcutaneous antipsychotic (LASCA) that combines risperidone and an innovative, copolymer-based drug delivery technology in a suspension suitable for subcutaneous use. TV-46000 was approved in 2023 by the FDA for the treatment of schizophrenia in adults based on the results of 2 Phase 3 clinical studies.35 The RIsperidone Subcutaneous Extended-release (RISE) study (NCT03503318) demonstrated that TV46000 administered once monthly (q1m) or once every 2 months (q2m) significantly prolonged time to impending relapse by 5.0 (P<0.0001) and 2.7 (P<0.0001) times, respectively, versus placebo. In addition, the proportion of patients with impending relapse at week 24 was significantly lower for patients receiving TV-46000 q1m (7%) and q2m (11%) compared with placebo (28%, P<0.0001 for both), and the proportion of patients who maintained stability at endpoint was significantly higher for both TV-46000 q1m (87%) and q2m (80%) compared with placebo (61%, P<0.0001 and P=0.0001, respectively).36 TV-46000 showed a favorable benefit–risk profile. After randomization, the most frequently reported treatment-related adverse events (ie, ≥5% of patients in either TV-46000 group) that occurred more often in patients receiving TV-46000 q1m or TV-46000 q2m versus placebo were injection site nodules (7% for TV-46000 q1m, 7% for TV-46000 q2m, 3% for placebo), weight increased (4%, 6%, 2%, respectively), and extrapyramidal disorder (5%, 3%, 0%, respectively).36 The Safety in Humans of TV-46000 sc INjection Evaluation (SHINE) study (NCT03893825) evaluated the long-term safety and tolerability of TV-46000 administered subcutaneously in adult and adolescent patients with schizophrenia. Results demonstrated that TV46000 administered q1m or q2m was generally well tolerated and had a benefit–risk profile consistent with other formulations of risperidone and previous studies with TV-46000.37–39 After randomization, frequent treatment-related AEs (≥3% of patients in either group) were injection site pain (5% for TV-46000 q1m; 4% for TV-46000 q2m) and injection site nodule (2% for TV-46000 q1m, 6% for TV-46000 q2m). Serious adverse events were reported for 8 (5%) patients in the TV-46000 q1m group and 11 (7%) in the TV-46000 q2m group, and 3 (2%) and 5 (3%) patients, respectively, discontinued the study because of adverse events. Here, results from the patient-centered outcomes assessed in these studies are presented.
Methods
Data from 2 studies, RISE and SHINE, were analyzed.
Study Design, Participants, and Interventions
The RISE Study
The RISE study was a double-blind, placebo-controlled, randomized, relapse-prevention study designed to compare subcutaneous TV-46000 administered q1m or q2m with placebo (Figure 1). Inclusion criteria, exclusion criteria, and dosing were previously described,36 but briefly were as follows: In stage 1 (oral conversion and stabilization stage), patients aged 13–65 years with a diagnosis of schizophrenia >1 year were eligible if they required chronic treatment with an antipsychotic, had ≥1 relapse within 24 months before screening, had a history of response to an antipsychotic agent (other than clozapine) <1 year before screening, and had a Positive and Negative Syndrome Scale (PANSS) total score <100 at screening. Patients received oral risperidone once daily for 12 weeks at an appropriate dose based on investigator judgment (aged ≥18 years: 2–5 mg/day; aged <18 years: 2–4 mg/day).
Figure 1.
Study design (RISE and SHINE).
Notes: aPatients in the rollover cohort who received placebo in RISE started TV-46000 at a dose equivalent to their oral stabilization dose from stage 1 of RISE. bPatients in the de novo cohort and patients who received placebo in RISE (placebo rollover) were randomized 1:1 in SHINE to receive TV-46000 q1m or q2m for up to 56 weeks; patients who received TV-46000 in RISE (TV-46000 rollover) continued their assigned dosing regimen. cFor the rollover cohort, the baseline visit was the end-of-treatment visit in RISE; for the de novo cohort, the baseline visit was the first day of the maintenance period (stage 2) in SHINE. dLast assessment was defined as the last available nonmissing value no later than the end-of-treatment visit. Only patients who did not relapse during the study or discontinue had end-of-treatment measurements, whereas last assessment encompassed all patients regardless of relapse or discontinuation of treatment.
Abbreviations: q1m, once monthly; q2m, once every 2 months.
In stage 2 (the maintenance/relapse-prevention stage), patients who were stabilized on oral risperidone treatment (12 weeks) were randomized to receive treatment with corresponding injectable doses of TV46000 q1m, TV-46000 q2m, or inactive placebo in a 1:1:1 ratio until they had a relapse, discontinued from the study, or the study was ended because the prespecified study-terminating criterion of ≥90 total relapse events occurred. Oral risperidone dosages of 2 mg/day, 3 mg/day, 4 mg/day, and 5 mg/day corresponded to 50 mg, 75 mg, 100 mg, and 125 mg of TV-46000 q1m, and 100 mg, 150 mg, 200 mg, and 250 mg TV-46000 q2m, respectively. Stabilization was defined as meeting all of the following criteria for ≥4 consecutive weeks:36 outpatient status; PANSS total score ≤80; no more than moderate positive psychotic symptoms on the PANSS, as measured by a score ≤4 on each of the following items: conceptual disorganization, suspiciousness, hallucinatory behavior, and unusual thought content; Clinical Global Impression-Severity (CGI-S) score ≤4 (moderately ill), and Clinical Global Impression-Severity of Suicidality (CGI-SS) score ≤2 (mildly suicidal) on part 1 and ≤5 (minimally worsened) on part 2. The primary endpoint was time to impending relapse in stage 2.
The SHINE Study
The SHINE study was a multicenter, double-blind, parallel-group study in which patients who completed the RISE study without relapse (placebo rollover and TV-46000 rollover cohorts), as well as patients who participated for the first time (de novo cohort), were enrolled (Figure 1). Patients who were newly enrolled were subject to the same eligibility and stabilization criteria as in RISE and completed the 12-week oral stabilization stage (stage 1) before proceeding to the maintenance stage (stage 2). Patients in the rollover cohorts entered SHINE at stage 2, with the end-of-treatment (EoT) visit for RISE considered as baseline visit for SHINE. Patients in the de novo and placebo rollover cohorts were randomized 1:1 in SHINE to receive TV-46000 q1m or q2m for up to 56 weeks; patients in the TV-46000 rollover cohort continued their assigned dosing regimen. The primary endpoint was the frequency of all AEs.
Patient-Centered Outcomes
Patient-centered outcomes were measured in the RISE and SHINE studies with the Personal and Social Performance scale (PSP), the Schizophrenia Quality of Life Scale (SQLS), the European Quality of Life 5-Dimension 5-Level (EQ-5D-5L) descriptive items and visual analog scale (VAS), and the Drug Attitude Inventory 10-item version (DAI-10), all regularly used in clinical trials in which patients have been stabilized prior to randomization.40–44 Outcomes were assessed at screening, baseline/randomization, last assessment (LA), and EoT. LA was defined as the last available nonmissing value no later than the EoT visit. Only patients who did not relapse during the study or discontinue had EoT measurements, whereas LA encompassed all patients regardless of relapse or discontinuation of treatment. In both studies, PSP, SQLS, EQ-5D-5L, and DAI-10, were evaluated as exploratory efficacy endpoints. All outcomes were assessed in adult patients because of the lack of validation of these measures in the younger age group.
The PSP (clinician-reported) is a 100-point single-item rating scale that measures the patient’s functioning in 4 categories: socially useful activities (eg, housework, work, and study), personal and social relationships (with partners, family, or friends), self-care (personal hygiene and appearance), and disturbing and aggressive behaviors.40,45 Scores below 30 indicate such poor functioning and that intensive supervision is needed, whereas higher scores indicate better personal and social functioning, with scores of 91–100 indicating more than adequate functioning.46
The SQLS (patient-reported) is a 33-item scale, categorized into 2 domains: psychosocial feelings (20 items) and cognition and vitality (13 items).41 Individual domain and total scores are standardized by a scoring algorithm to a range of 0 (best health status) to 100 (worst health status).
The EQ-5D-5L (patient-reported) is a 2-part questionnaire.43,44,47,48 In part 1 (descriptive items), patients rate their health state in 5 dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) using a scale of 1 (no problems) to 5 (extreme problems). Responses are combined into a 5-digit code (1 digit per dimension) from which an index score is derived. In part 2 (VAS), patients rate their overall health state on a 100-mm VAS; a rating of 0 represents the worst imaginable health state, and a rating of 100 represents the best imaginable health state.
The DAI-10 (patient-reported) consists of 10 statements covering 3 domains (subjective positive, subjective negative, and attitude toward medication). Patient responses (true/false) to the items/statements are interpreted and a total score ranging from –10 to +10 is calculated.42,49 A positive total score indicates a positive attitude toward psychiatric medications, and vice versa.
Statistical Analysis
For each of the patient-centered outcomes assessed, change from baseline was calculated as least-squares mean (LSM) and 95% CI using a mixed model repeated measures model with treatment arm, patient identifier, study visit, and stratification variable as factors and baseline score as covariate. For the RISE study, results of the TV-46000 q1m and q2m groups were each compared with placebo, with no comparisons between the active treatment groups. SQLS and DAI-10 were prespecified as key secondary endpoints, and PSP and EQ-5D-5L VAS were prespecified as exploratory efficacy endpoints. However, because an endpoint higher in the hierarchy (proportion of patients who achieved remission for TV-46000 overall vs placebo) did not show statistical significance between treatment and placebo, all endpoints included in this report were analyzed as exploratory, only nominally computed, and were not interpreted inferentially. Results were descriptively analyzed for the SHINE study.
Results
Patient Characteristics
In the RISE study, 543 adult patients were randomized (intent-to-treat population) to receive TV-46000 q1m (n=183), TV-46000 q2m (n=179), or placebo (n=181). In the SHINE study, 333 adult patients (106 de novo and 227 rollover [172 from TV-46000 and 55 from placebo]) were randomized to TV-46000 q1m (n=173) or q2m (n=160). Of those, 331 patients were treated: TV-46000 q1m (n=171) or q2m (n=160). Treatment groups were generally similar regarding baseline characteristics (Table 1).
Table 1.
Key Patient Baseline Characteristics (ITT Population)
| Placebo | TV-46000 q1m | TV-46000 q2m | Total | ||
|---|---|---|---|---|---|
| RISE | |||||
| n=181 | n=183 | n=179 | N=543 | ||
| Age, years, median (range) | 52.0 (19–65) | 54.0 (19–65) | 51.0 (20–65) | 52.0 (19–65) | |
| Male, n (%) | 110 (61) | 112 (61) | 110 (61) | 332 (61) | |
| Race, n (%) | Black/African American | 104 (57) | 108 (59) | 110 (61) | 322 (59) |
| White | 68 (38) | 72 (39) | 66 (37) | 206 (38) | |
| Other | 9 (5) | 3 (2) | 3 (2) | 15 (3) | |
| Disease length, years, mean (SD) | 20.6 (12.21) | 22.9 (11.86) | 19.0 (12.29) | 20.8 (12.21) | |
| Time since most recent relapse, months, mean (SD) | 10.5 (6.80) | 9.7 (6.67) | 10.2 (7.49) | 10.2 (6.98) | |
| PANSS total score, mean (SD) | 61.0 (10.38) | 61.5 (9.60) | 61.4 (10.29) | – | |
| CGI-S score, mean (SD)a | 3.3 (0.67) | 3.3 (0.59) | 3.2 (0.66) | – | |
| SHINEb | |||||
| n=171 | n=160 | N=331 | |||
| Age, years, median (range) | 54.0 (20–67) | 53.0 (19–67) | 54.0 (19–67) | ||
| Male, n (%) | 111 (65) | 103 (64) | 214 (65) | ||
| Race, n (%) | Black/African American | 89 (52) | 89 (56) | 178 (54) | |
| White | 79 (46) | 66 (41) | 145 (44) | ||
| Other | 3 (2) | 5 (3) | 8 (2) | ||
| Disease length, years, mean (SD) | 22.7 (12.26) | 19.6 (11.97) | 21.2 (12.20) | ||
| Time since most recent relapse, months, mean (SD) | 20.7 (10.28) | 21.6 (10.65) | 21.2 (10.46) | ||
| PANSS total score, mean (SD)c | 57.5 (11.05) | 56.9 (10.57) | 57.2 (10.81) | ||
| CGI-S score, mean (SD)a | 3.1 (0.62) | 3.0 (0.67) | 3.1 (0.64) | ||
Notes: aAssessed in safety analysis population. RISE: placebo (n=179), TV-46000 q1m (n=183), TV-46000 q2m (n=179), TV-46000 total (n=362), all patients (n=541); SHINE: TV-46000 q1m (n=172), TV-46000 q2m (n=162), TV-46000 total/all patients (n=334). bTwo adult patients were randomized but not treated. cPresented for all adult patients: n (TV-46000 q1m)=173, n (TV-46000 q2m)=160, n (all patients)=333.
Abbreviations: –, not available; CGI-S, Clinical Global Impression-Severity; ITT, intent-to-treat; PANSS, Positive and Negative Syndrome Scale; q1m, once monthly; q2m, once every 2 months.
Patient-Centered Outcomes
Stage 1: Oral Conversion and Stabilization Phase
In the RISE study, mean (SE) PSP, SQLS, EQ-5D-5L VAS, and DAI-10 scores substantially improved with oral risperidone from screening to randomization/baseline for all groups, whereas scores for individual EQ-5D-5L descriptive items remained unchanged or showed minor improvements (Table 2).
Table 2.
RISE Study: Patient-Centered Outcomes Scores
| Mean (SE) | Placebo | TV-46000 q1m | TV-46000 q2m | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Screening | Random-ization/ Baseline | EoT | LA | Screening | Random-ization/ Baseline | EoT | Nominal P valuea | LA | Nominal P valuea | Screening | Random-ization/ Baseline | EoT | Nominal P valuea | LA | Nominal P valuea | |
| PSP | 59.9 (0.99) | 63.7 (0.86) | 67.3 (1.28) | 60.6 (1.08) | 59.6 (0.95) | 63.3 (0.87) | 65.1 (1.33) | 0.2887 | 63.7 (1.06) | 0.0012 | 61.7 (0.89) | 65.1 (0.81) | 66.8 (1.25) | 0.0803 | 64.8 (0.96) | 0.0043 |
| SQLS | 40.9 (1.18) | 34.0 (1.20) | 32.1 (1.89) | 35.1 (1.34) | 39.5 (1.26) | 33.1 (1.24) | 23.9 (1.74) | 0.0001 | 28.1 (1.29) | <0.0001 | 41.4 (1.27) | 34.2 (1.17) | 27.1 (1.95) | 0.0009 | 29.9 (1.34) | 0.0005 |
| EQ-5D-5L descriptive items | ||||||||||||||||
| Mobility | 1.3 (0.06) | 1.4 (0.06) | 1.4 (0.09) | 1.4 (0.06) | 1.4 (0.06) | 1.4 (0.06) | 1.1 (0.05) | 0.0016 | 1.2 (0.04) | 0.0102 | 1.4 (0.06) | 1.3 (0.04) | 1.3 (0.08) | 0.1917 | 1.3 (0.06) | 0.5609 |
| Self-care | 1.3 (0.05) | 1.2 (0.05) | 1.2 (0.07) | 1.2 (0.05) | 1.2 (0.05) | 1.2 (0.05) | 1.1 (0.04) | 0.1163 | 1.2 (0.04) | 0.2987 | 1.3 (0.05) | 1.1 (0.04) | 1.2 (0.05) | 0.4206 | 1.2 (0.04) | 0.6092 |
| Usual activities | 1.7 (0.07) | 1.5 (0.06) | 1.6 (0.08) | 1.5 (0.06) | 1.7 (0.06) | 1.6 (0.06) | 1.3 (0.07) | 0.0645 | 1.4 (0.05) | 0.0047 | 1.8 (0.07) | 1.5 (0.05) | 1.4 (0.07) | 0.4454 | 1.4 (0.05) | 0.2422 |
| Pain/discomfort | 1.6 (0.06) | 1.6 (0.07) | 1.7 (0.13) | 1.7 (0.8) | 1.6 (0.06) | 1.6 (0.06) | 1.3 (0.06) | <0.0001 | 1.4 (0.05) | <0.0001 | 1.6 (0.06) | 1.5 (0.06) | 1.3 (0.07) | 0.0002 | 1.5 (0.06) | 0.0057 |
| Anxiety/depression | 2.1 (0.07) | 1.8 (0.06) | 2.0 (0.10) | 2.0 (0.07) | 1.9 (0.07) | 1.8 (0.07) | 1.5 (0.07) | 0.0002 | 1.6 (0.06) | <0.0001 | 2.2 (0.08) | 1.8 (0.07) | 1.7 (0.09) | 0.026 | 1.8 (0.07) | 0.0247 |
| EQ-5D-5L VAS | 76.1 (1.32) | 80.0 (1.30) | 79.0 (1.79) | 77.3 (1.41) | 76.4 (1.25) | 79.1 (1.28) | 84.0 (1.52) | 0.0048 | 80.4 (1.21) | 0.0147 | 75.8 (1.22) | 81.2 (1.02) | 83.8 (1.42) | 0.0053 | 81.3 (1.14) | 0.0192 |
| DAI-10 | 5.8 (0.26) | 6.1 (0.24) | 5.6 (0.4) | 5.2 (0.31) | 5.7 (0.26) | 5.8 (0.27) | 6.8 (0.34) | 0.0037 | 6.2 (0.30) | 0.0129 | 5.2 (0.26) | 5.7 (0.23) | 6.2 (0.4) | 0.0859 | 5.5 (0.32) | 0.2854 |
Notes: aVersus placebo for change from baseline/randomization (LSM difference).
Abbreviations: DAI-10, Drug Attitude Inventory 10-item version; EoT, end of treatment; EQ-5D-5L, European Quality of Life 5-level EQ-5D; LA, last assessment; LSM, least-squares mean; PSP, Personal and Social Performance scale; q1m, once monthly; q2m, once every 2 months; SQLS, Schizophrenia Quality of Life Scale.
During the oral stabilization phase of the SHINE study, the de novo group showed improvements from screening to randomization in mean (SE) PSP, SQLS, and DAI-10 scores (Table 3), minor decreases in EQ-5D-5L VAS scores (Table 3), and no change or minor improvements in individual EQ-5D-5L descriptive item scores (Table 3).
Table 3.
SHINE Study: Patient-Centered Outcomes Scores
| Mean (SE) | TV-46000 q1m | TV-46000 q2m | ||||||
|---|---|---|---|---|---|---|---|---|
| Screening | Randomization/Baseline | EoT | LA | Screening | Randomization/Baseline | EoT | LA | |
| PSP | ||||||||
| Overall | 55.5 (2.98) | 62.3 (1.33) | 64.6 (1.57) | 63.4 (1.44) | 49.8 (3.32) | 63.6 (1.30) | 65.7 (1.65) | 64.3 (1.56) |
| De novo | 55.5 (2.98) | 55.9 (3.27) | 57.0 (5.20) | 57.0 (3.60) | 49.8 (3.32) | 56.5 (3.17) | 54.2 (6.01) | 55.4 (4.11) |
| Placebo rollover | – | 66.7 (1.94) | 71.5 (2.15) | 70.6 (2.05) | – | 67.6 (1.86) | 68.3 (2.08) | 68.7 (2.10) |
| TV-46000 rollover | – | 64.9 (1.34) | 65.3 (1.62) | 64.9 (1.56) | – | 66.8 (1.25) | 69.0 (1.37) | 68.1 (1.33) |
| SQLS | ||||||||
| Overall | 37.4 (2.42) | 28.7 (1.21) | 25.2 (1.53) | 27.7 (1.39) | 33.8 (1.92) | 29.0 (1.24) | 24.9 (1.34) | 26.3 (1.21) |
| De novo | 37.4 (2.42) | 34.5 (2.09) | 34.4 (3.42) | 34.5 (2.53) | 33.8 (1.92) | 31.8 (2.01) | 24.4 (2.20) | 27.4 (1.99) |
| Placebo rollover | – | 30.6 (2.48) | 18.9 (1.62) | 21.0 (2.09) | – | 30.1 (2.60) | 26.2 (2.67) | 26.6 (2.56) |
| TV-46000 rollover | – | 24.7 (1.67) | 23.5 (1.99) | 25.8 (1.93) | – | 26.8 (1.87) | 24.6 (1.99) | 25.6 (1.86) |
| EQ-5D-5L descriptive items | ||||||||
| Mobility | ||||||||
| Overall | 1.4 (0.11) | 1.2 (0.04) | 1.3 (0.07) | 1.3 (0.06) | 1.2 (0.08) | 1.3 (0.05) | 1.3 (0.06) | 1.3 (0.05) |
| De novo | 1.4 (0.11) | 1.4 (0.09) | 1.3 (0.11) | 1.3 (0.08) | 1.2 (0.08) | 1.2 (0.08) | 1.2 (0.10) | 1.2 (0.06) |
| Placebo rollover | – | 1.2 (0.10) | 1.1 (0.10) | 1.1 (0.10) | – | 1.5 (0.14) | 1.4 (0.12) | 1.4 (0.12) |
| TV-46000 rollover | – | 1.1 (0.04) | 1.3 (0.10) | 1.4 (0.10) | – | 1.3 (0.08) | 1.3 (0.09) | 1.3 (0.08) |
| Self-care | ||||||||
| Overall | 1.1 (0.04) | 1.2 (0.04) | 1.2 (0.5) | 1.2 (0.5) | 1.1 (0.04) | 1.2 (0.04) | 1.2 (0.06) | 1.2 (0.05) |
| De novo | 1.1 (0.04) | 1.3 (0.09) | 1.1 (0.07) | 1.1 (0.05) | 1.1 (0.04) | 1.2 (0.08) | 1.2 (0.09) | 1.1 (0.06) |
| Placebo rollover | – | 1.2 (0.10) | 1.1 (0.10) | 1.1 (0.09) | – | 1.1 (0.07) | 1.1 (0.07) | 1.1 (0.06) |
| TV-46000 rollover | – | 1.1 (0.04) | 1.2 (0.08) | 1.2 (0.08) | – | 1.1 (0.05) | 1.3 (0.09) | 1.2 (0.08) |
| Usual activities | ||||||||
| Overall | 1.6 (0.14) | 1.4 (0.05) | 1.4 (0.06) | 1.4 (0.06) | 1.5 (0.10) | 1.4 (0.05) | 1.4 (0.07) | 1.4 (0.06) |
| De novo | 1.6 (0.14) | 1.5 (0.09) | 1.2 (0.08) | 1.2 (0.06) | 1.5 (0.10) | 1.3 (0.07) | 1.2 (0.08) | 1.2 (0.06) |
| Placebo rollover | – | 1.6 (0.12) | 1.4 (0.13) | 1.5 (0.12) | – | 1.4 (0.11) | 1.6 (0.14) | 1.6 (0.14) |
| TV-46000 rollover | – | 1.3 (0.07) | 1.5 (0.10) | 1.5 (0.09) | – | 1.4 (0.07) | 1.4 (0.10) | 1.4 (0.09) |
| Pain/discomfort | ||||||||
| Overall | 1.6 (0.12) | 1.5 (0.06) | 1.4 (0.07) | 1.5 (0.07) | 1.4 (0.09) | 1.5 (0.06) | 1.4 (0.06) | 1.4 (0.05) |
| De novo | 1.6 (0.12) | 1.8 (0.12) | 1.6 (0.15) | 1.6 (0.10) | 1.4 (0.09) | 1.5 (0.10) | 1.2 (0.08) | 1.2 (0.06) |
| Placebo rollover | – | 1.5 (0.18) | 1.3 (0.17) | 1.3 (0.16) | – | 1.8 (0.20) | 1.6 (0.14) | 1.6 (0.14) |
| TV-46000 rollover | – | 1.2 (0.06) | 1.4 (0.09) | 1.5 (0.10) | – | 1.3 (0.07) | 1.4 (0.08) | 1.4 (0.07) |
| Anxiety/depression | ||||||||
| Overall | 1.9 (0.15) | 1.7 (0.06) | 1.7 (0.08) | 1.7 (0.07) | 1.8 (0.12) | 1.7 (0.06) | 1.6 (0.07) | 1.7 (0.06) |
| De novo | 1.9 (0.15) | 1.9 (0.13) | 1.9 (0.21) | 1.7 (0.14) | 1.8 (0.12) | 1.6 (0.10) | 1.5 (0.15) | 1.6 (0.12) |
| Placebo rollover | – | 1.8 (0.14) | 1.7 (0.12) | 1.7 (0.11) | – | 2.0 (0.15) | 2.0 (0.15) | 2.0 (0.14) |
| TV-46000 rollover | – | 1.5 (0.06) | 1.6 (0.09) | 1.6 (0.09) | – | 1.7 (0.09) | 1.6 (0.09) | 1.6 (0.09) |
| EQ-5D-5L VAS | ||||||||
| Overall | 82.1 (1.92) | 81.1 (1.10) | 83.6 (1.22) | 82.7 (1.12) | 84.7 (2.01) | 83.1 (1.02) | 84.6 (1.12) | 84.0 (1.03) |
| De novo | 82.1 (1.92) | 77.8 (2.06) | 81.3 (2.66) | 81.1 (2.06) | 84.7 (2.01) | 83.8 (1.99) | 87.8 (2.18) | 86.0 (1.76) |
| Placebo rollover | – | 79.9 (2.48) | 84.1 (2.33) | 83.9 (2.23) | – | 80.4 (2.14) | 80.6 (3.04) | 80.5 (2.81) |
| TV-46000 rollover | – | 83.3 (1.47) | 84.4 (1.64) | 83.4 (1.59) | – | 83.7 (1.39) | 84.7 (1.34) | 84.0 (1.38) |
| DAI-10 | ||||||||
| Overall | 5.7 (0.52) | 6.6 (0.24) | 6.6 (0.29) | 6.2 (0.30) | 6.4 (0.50) | 6.6 (0.26) | 6.3 (0.25) | 6.5 (0.23) |
| De novo | 5.7 (0.52) | 7.0 (0.41) | 5.7 (0.65) | 5.8 (0.55) | 6.4 (0.50) | 7.6 (0.37) | 6.9 (0.58) | 7.2 (0.40) |
| Placebo rollover | – | 5.7 (0.62) | 6.7 (0.81) | 6.2 (0.83) | – | 5.6 (0.59) | 6.4 (0.46) | 6.4 (0.44) |
| TV-46000 rollover | – | 6.6 (0.33) | 6.9 (0.33) | 6.5 (0.39) | – | 6.3 (0.39) | 6.1 (0.35) | 6.1 (0.33) |
Abbreviations: –, not applicable; DAI-10, Drug Attitude Inventory 10-item version; EoT, end of treatment; EQ-5D-5L, European Quality of Life 5-level EQ-5D; LA, last assessment; LSM, least-squares mean; PSP, Personal and Social Performance scale; q1m, once monthly; q2m, once every 2 months; SQLS, Schizophrenia Quality of Life Scale.
Stage 2: Maintenance Stage
PSP
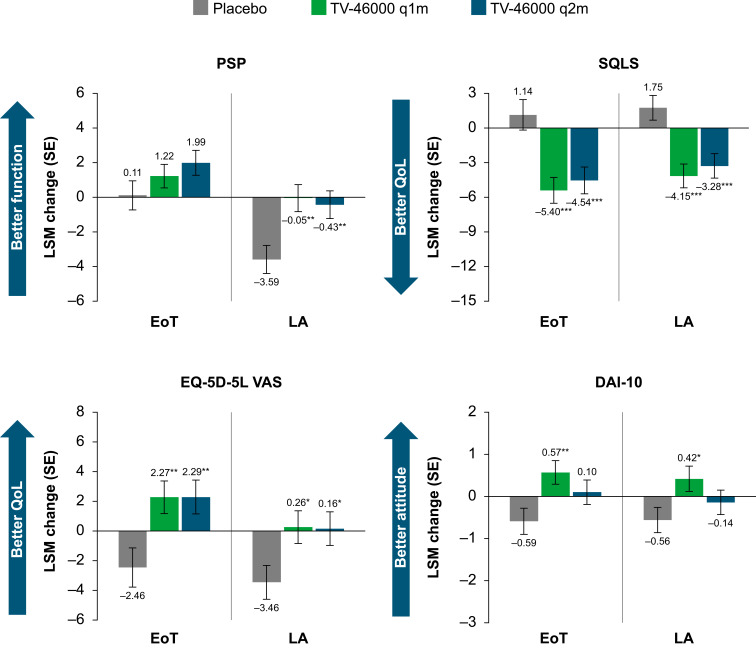
After substantial improvements during the oral stabilization phase in the RISE study, mean PSP total scores at EoT remained steady from randomization/baseline to EoT in all active treatment groups (Table 2). The change from baseline in PSP total score showed numeric differences favoring active treatment at EoT (LSM [SE]: q1m, 1.22 [0.68]; q2m, 1.99 [0.72]; P>0.05 for both) compared with the placebo group (0.11 [0.84]) (Figure 2). At LA, significant improvement (P<0.01 for both) from baseline was observed for TV-46000 q1m (−0.05 [0.78]) and q2m (−0.43 [0.80]) treatment groups, compared with placebo (−3.59 [0.81]; Figure 2). These improvements were driven by all 4 PSP domains: personal and social relationships (LSM difference versus placebo: q1m, −0.19 [P<0.05]; q2m, –0.16 [P<0.05]); socially useful activities (−0.20 [P<0.05]; –0.14 [P>0.05]); disturbing and aggressive behavior (−0.17 [P<0.01]; –0.14 [P<0.05]); and self-care (−0.12 [P>0.05]; –0.11 [P>0.05]).
Figure 2.
RISE study: PSP, SQLS, EQ-5D-5L VAS, and DAI-10 scores at EoT and LA.
Notes: *Nominal P<0.05, **nominal P<0.01, ***nominal P<0.001 vs placebo for change from baseline/randomization (least-squares means difference).
Abbreviations: DAI-10, Drug Attitude Inventory 10-item version; EoT, end of treatment; EQ-5D-5L VAS, European Quality of Life 5-level EQ-5D visual analog scale; LA, last assessment; PSP, Personal and Social Performance scale; q1m, once monthly; q2m, once every 2 months; QoL, quality of life; SQLS, Schizophrenia Quality of Life Scale.
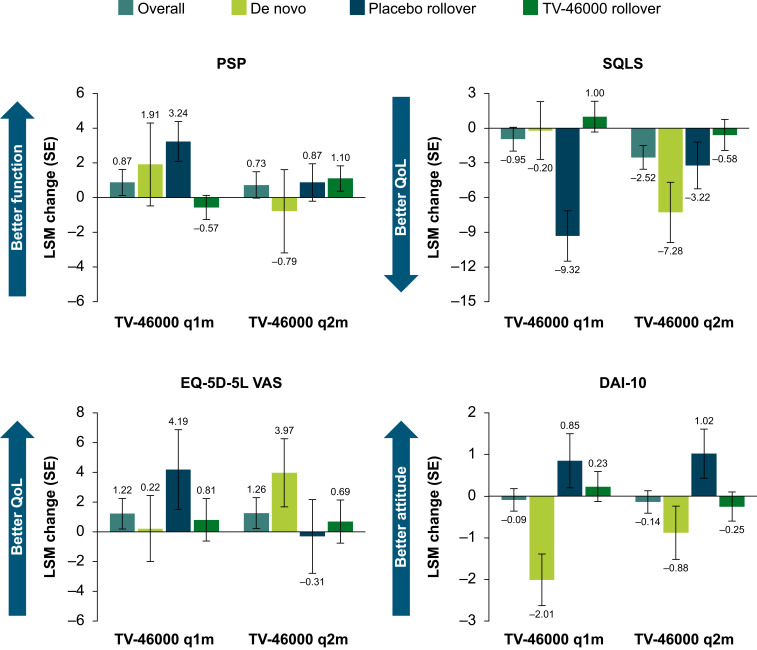
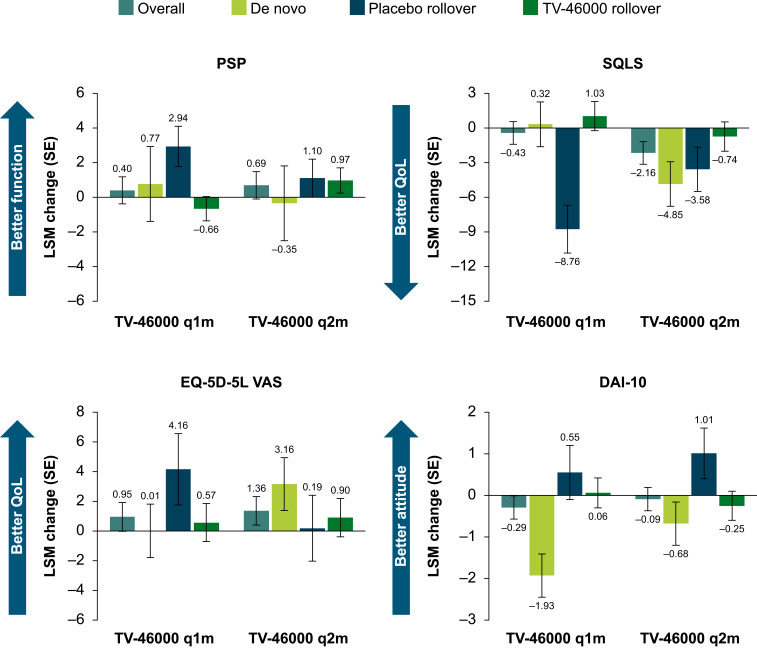
PSP total scores showed minimal changes over time in the SHINE study, with no meaningful differences between treatment groups. At EoT, a numeric improvement from baseline was observed for both the TV-46000 q1m (LSM [SE] change from baseline, 0.87 [0.75]) and q2m (0.73 [0.76]) treatment groups (Table 3 and Figure 3). At LA, a numeric improvement from randomization/baseline was observed for both the TV-46000 q1m (LSM change, 0.40 [SE, 0.78]) and q2m (0.69 [0.79]) treatment groups (Table 3 and Figure 4). The largest improvements in PSP total scores were seen in patients in the placebo rollover cohort (mean change, 2.0 [SE, 0.73]) compared with the TV-46000 rollover cohort (0.6 [0.43]), where improvements from RISE were maintained, and the de novo cohort (0.2 [1.36]), where the improvements observed during the oral stabilization period in SHINE were maintained (Table 3).
Figure 3.
SHINE study: Overall, De novo, Placebo rollover, and TV-46000 rollover PSP, SQLS, EQ-5D-5L VAS, and DAI-10 LSM change scores at EoT.
Abbreviations: DAI-10, Drug Attitude Inventory 10-item version; EoT, end of treatment; EQ-5D-5L VAS, European Quality of Life 5-level EQ-5D visual analog scale; LA, last assessment; PSP, Personal and Social Performance scale; q1m, once monthly; q2m, once every 2 months; QoL, quality of life; SQLS, Schizophrenia Quality of Life Scale.
Figure 4.
SHINE study: Overall, De novo, Placebo rollover, and TV-46000 rollover PSP, SQLS, EQ-5D-5L VAS, and DAI-10 LSM change scores at LA.
Abbreviations: DAI-10, Drug Attitude Inventory 10-item version; EoT, end of treatment; EQ-5D-5L VAS, European Quality of Life 5-level EQ-5D visual analog scale; LA, last assessment; PSP, Personal and Social Performance scale; q1m, once monthly; q2m, once every 2 months; QoL, quality of life; SQLS, Schizophrenia Quality of Life Scale.
SQLS
After substantial improvements during the oral stabilization phase, mean SQLS scores continued to improve (decrease) in the RISE study from randomization/baseline to EoT for both TV-46000 groups, while these scores remained similar in the placebo group (P<0.001 for change from baseline for both TV-46000 groups vs placebo) (Table 2). LSM changes (SE) demonstrated improvement from randomization/baseline to EoT for TV-46000 (q1m, –5.40 [1.12]; q2m, –4.54 [1.16]), but worsened for placebo (1.14 [1.32]; P<0.001 for each vs placebo) (Table 2 and Figure 2). The mean SQLS scores continued to improve (decrease) from randomization/baseline to LA for both TV-46000 q1m (LSM change [SE], −4.15 [1.03]) and q2m (−3.28 [1.06]), while these scores worsened in the placebo group (1.75 [1.07]; P<0.001 for both) (Table 2 and Figure 2).
In the SHINE study, reductions in SQLS were observed for both treatment groups at EoT compared with baseline, with a numerically larger reduction for TV-46000 q2m (LSM change from baseline [SE], −2.52 [1.03]) than for q1m (−0.95 [1.03]) (Table 3 and Figure 3). Reductions in SQLS (indicating improvement) were observed for both treatment groups at LA compared with baseline, with a numerically larger reduction for TV-46000 q2m (LSM change, −2.16 [0.98]) than for q1m (−0.43 [SE, 0.98]) (Table 3 and Figure 4). Reductions were also observed for patients in the de novo cohort (LSM change [SE]: q1m, 0.32 [1.94]; q2m, −4.85 [1.93]) and placebo rollover cohort (−8.76 [2.07]; −3.58 [1.92]), but were maintained with no change for the TV-46000 rollover cohort (1.03 [1.26]; −0.74 [1.27]); within these prior TV-46000 treatment cohorts, no consistent trend was observed across dosing regimens (Table 3 and Figure 4).
EQ-5D-5L VAS
In the RISE study, EQ-5D-5L VAS changes from baseline (LSM [SE]) demonstrated improvement from randomization/baseline to EoT for the TV-46000 groups (q1m, 2.27 [1.1]; q2m, 2.29 [1.14]), and worsened for the placebo group (–2.46 [1.32]; P<0.01 for LSM difference for each vs placebo) (Table 2 and Figure 2). Changes from baseline in EQ-5D-5L VAS scores demonstrated a significant improvement from randomization/baseline to LA for both TV-46000 q1m (LSM change [SE], 0.26 [1.10]) and q2m (0.16 [1.13]) and worsened for the placebo group (–3.46 [1.14]; P<0.05 both) (Table 2 and Figure 2).
At EoT in the SHINE study, EQ-5D-5L VAS scores (mean [SE]) were in the same range as for RISE for both groups: TV-46000 q1m, 83.6 (1.22); q2m, 84.6 (1.12), and largely remained the same as at randomization/baseline (Table 3). There were no meaningful differences in LSM change (SE) from baseline between EQ-5D-5L VAS scores of the 3 prior TV-46000 treatment cohorts at EoT: de novo (TV-46000 q1m, 0.22 [2.22]; q2m, 3.97 [2.29]); placebo rollover (4.19 [2.68]; –0.31 [2.48]); and TV-46000 rollover (0.81 [1.43]; 0.69 [1.45]) (Table 3 and Figure 3). At LA in the SHINE study, mean (SE) EQ-5D-5L VAS scores were in the same range as for RISE for both treatment groups (TV-46000 q1m, 82.7 [1.12]; q2m, 84.0 [1.03]) and were largely unchanged from randomization/baseline (Table 3). There were no meaningful differences in LSM change (SE) from baseline between EQ-5D-5L VAS scores of the 3 prior TV-46000 treatment cohorts at LA: de novo (q1m, 0.01 [1.80]; q2m, 3.16 [1.78]); placebo rollover (4.16 [2.40]; 0.19 [2.22]), and TV-46000 rollover (0.57 [1.28]; 0.90 [1.29]) (Table 3 and Figure 4).
EQ-5D-5L Descriptive Items
After minor improvements during the oral stabilization phase in RISE, EQ-5D-5L descriptive item scores improved between randomization/baseline and EoT for mobility (TV-46000 q1m group only), pain/discomfort, and anxiety/depression (both TV-46000 groups), while scores remained steady in the placebo group (P<0.05 for change from baseline for each TV-46000 group vs placebo) (Table 2). EQ-5D-5L descriptive item scores improved between randomization/baseline and LA for mobility, usual activities, pain/discomfort, and anxiety/depression for TV-46000 groups, while scores remained steady in the placebo group; differences between TV-46000 and placebo were generally significant (Table 2).
In SHINE, mean changes in EQ-5D-5L descriptive items from randomization/baseline to EoT and LA were minimal (<1.5 and <0.5, respectively) for all dimensions in both treatment groups, with no meaningful differences between prior TV-46000 treatment cohorts (Table 3).
DAI-10
In RISE, after substantial improvements during the oral stabilization phase, DAI-10 LSM changes (SE) demonstrated continued improvement to EoT for TV-46000 (q1m, 0.57 [0.28]; q2m, 0.10 [0.29]; P<0.01 for TV-46000 q1m and total, P>0.05 for TV-46000 q2m, all versus placebo) but worsened for placebo (–0.59 [0.31]) (Table 2 and Figure 2). Baseline DAI-10 total scores were positive (indicating a favorable view of treatment) and improved to LA for the TV-46000 q1m group (LSM change [SE], 0.42 [0.30]; P<0.05), while scores decreased for the placebo group (–0.56 [0.30]); DAI-10 scores also decreased slightly for the TV-46000 q2m group (–0.14 [0.29]), but the amount of decrease was significantly smaller versus placebo (P<0.05) (Table 2 and Figure 2).
In SHINE, baseline mean (SE) DAI-10 total scores were also positive—6.6 (0.24) in the TV-46000 q1m group, and 6.6 (0.26) in the q2m group—and were minimally changed at EoT (6.6 [0.29] and 6.3 [0.25], respectively) (Table 3 and Figure 3). Overall, DAI-10 total scores were minimally changed from baseline to LA in SHINE (LSM change [SE]: q1m, –0.29 [0.28]; q2m, –0.09 [0.28]) (Table 3 and Figure 4). Within prior TV-46000 treatment cohorts, total scores decreased in the de novo cohort (–1.93 [0.52]; –0.68 [0.52]), increased in the placebo rollover cohort (0.55 [0.65]; 1.01 [0.61]), and, on average, remained unchanged in the TV-46000 rollover cohort (0.06 [0.36]; –0.25 [0.35]) (Table 3 and Figure 4).
Discussion
Results for patient-centered outcomes from the RISE and SHINE studies provided insight on patient functioning, QoL, and treatment satisfaction in response to treatment with TV-46000. In the RISE study, patients in the TV-46000 q1m and/or q2m groups showed significant improvements in PSP, SQLS, EQ-5D, 5L, and DAI-10 scores compared to placebo. This was seen despite the well-established placebo response that often impacts results in schizophrenia clinical trials. Assuming we did incur a placebo response, the difference from active treatment being masked by it and the true difference was likely greater than what was observed. Furthermore, long-term data from the SHINE study, where no placebo group was included, support the findings from the RISE study.
Psychosocial functioning, measured by PSP scores, showed numeric improvements from screening to randomization/baseline with TV-46000 in both the RISE and SHINE studies. In the RISE study, patients in the TV-46000 treatment groups had significantly better psychosocial functioning than those in the placebo group at LA. In the SHINE study, total scores showed minor improvements at LA, particularly in the placebo rollover cohort.
In previous studies, LAIs showed promising results in terms of psychosocial functioning: patients with schizophrenia who were treated with paliperidone palmitate (PP) q1m50 and once every 3 months,51 showed significant improvements in PSP versus placebo. Patients with schizophrenia who were treated with a risperidone LAI had significantly higher PSP scores (indicating improvement) than those treated with oral risperidone.52 Furthermore, patients treated with PP q1m had fewer PSP worsening events than those treated with a paliperidone extended-release formulation, perhaps related to improved treatment adherence with the LAI formulation.53 However, in some studies conducted in patients with schizophrenia, no significant differences in PSP scores were found between patients treated with oral and LAI risperidone.54–56
In the RISE study, SQLS scores were significantly improved for both TV-46000 groups from randomization/baseline to LA compared with placebo. Scores were also numerically improved in the SHINE study, where improvements were observed for both treatment groups at LA. Reductions were also observed for patients in the de novo and placebo rollover cohorts, but not for the TV-46000 rollover cohort. Patients in the TV-46000 rollover cohort did, however, maintain improvements from RISE with continued TV-46000 treatment in SHINE. These results are similar to those found in the Risperdal Consta Trial Of Relapse Prevention And Effectiveness (ConstaTRE) relapse-prevention study, in which patients were treated with a risperidone LAI or quetiapine.57 In that study, significant improvements in SQLS scores were observed from baseline to month 24 in the risperidone LAI group, as well as in the quetiapine group.57
The EQ-5D-5L descriptive items for mobility and usual activities were significantly improved from randomization/baseline to LA in the RISE study for the q1m group, whereas pain/discomfort and anxiety/depression were significantly improved in both TV-46000 groups. These changes were maintained or showed minimal improvement in the SHINE study, with no meaningful differences between prior TV-46000 treatment cohorts. EQ-5D-5L-VAS scores were significantly improved for both TV-46000 groups compared with placebo in the RISE study, and remained stable in the SHINE study, with a slightly larger numeric improvement in the de novo cohort.
Treatment satisfaction, measured by DAI-10, improved for all TV-46000 treatment groups in the RISE study—significantly so in the TV-46000 q1m group. No significant differences were observed among prior TV-46000 treatment cohorts in the SHINE study. Similar results were found in a prospective cohort study conducted in the United States, where the mean DAI-10 scores for participants receiving LAIs were higher than those receiving oral antipsychotics.58 In another study, most patients preferred a risperidone LAI over oral risperidone (72.6%) or other oral antipsychotics (78.4%), and were satisfied with the risperidone LAI (90.1%).59 In a recent survey that was administered to patients and health care professionals (HCPs) who had ≥2 experiences with TV-46000 as part of the SHINE study, varied responses were gathered in terms of treatment preferences.60 Most patients preferred injections over oral delivery (59%), flexible dosing intervals (59%), and short needles (68%), whereas most HCPs preferred to have flexibility in terms of dosing options (78%), injection frequency (84%), and route of administration (59%). In addition, 90% of patients reported that they would prefer to continue using TV-46000, rather than returning to their previous medication (oral or LAI), and 92% of patients and 96% of HCPs were satisfied with TV-46000.
LAIs have been shown to improve adherence and reduce the risk of relapse in patients with schizophrenia,61,62 but data on their effect on quality of life and treatment satisfaction are limited.63 PRO results from the RISE and SHINE studies, presented here, provide evidence on patients’ experience of TV-46000 q1m and q2m administered long-term. Patient-centered outcomes can highlight unmet needs and allow patients to communicate their experiences and objective treatment expectations.11 However, PROs assessing day-to-day functioning in patients with schizophrenia may at times not agree with objective evidence, including performance-based assessments of cognition or functional capacity64–67 or of social functioning.68 Therefore, careful evaluation of a combination of assessments is needed.69
Limitations
According to the inclusion criteria, patients were required to have been responsive to antipsychotic treatment in the previous year and needed to be responsive to oral risperidone in order to be randomized to stage 2; thus, the sample studied was enriched for risperidone responders. Other exclusions (substance use disorder, risk of suicide/violent behavior, clinically significant Diagnostic and Statistical Manual of Mental Disorders, fifth edition, diagnosis other than schizophrenia) may also limit generalizability to the wider population of people with schizophrenia.
Conclusion
Patient-centered outcomes improved with oral risperidone during the 12-week oral conversion and stabilization phase of RISE; these improvements were maintained, and in some cases continued to improve, with TV-46000 during the relapse-prevention phase of the study and into SHINE. Improvements were observed across prior TV-46000 treatment cohorts, with the largest improvements observed for patients who began TV-46000 during SHINE (ie, patients who were newly enrolled [de novo cohort] or who received placebo in RISE [placebo rollover cohort]), while gains made during RISE were minimally improved or maintained in patients who continued their assigned TV-46000 regimen in SHINE (ie, TV-46000 rollover cohort), indicating the benefit of uninterrupted TV-46000 treatment. Taken together, these data support the effectiveness of TV-46000 to improve patient-centered outcomes in patients with schizophrenia.
Acknowledgments
The authors thank the patients and clinicians who participated in these trials. The authors also thank Ortal Pelleg, BSc, Shayna Taylor, MPH, Simone Mangold, Michal Benedek, MSc, Liran Petrushka, MSc, and Tali Moldovan, MBA, all of Teva Pharmaceutical Industries Ltd, for their contributions to the conduct of the study. Medical writing support for the development of this manuscript, under the direction of the authors, was provided by Holly Engelman, PhD, Nycole Maza, PhD, Anneke Brand, PhD, and Jennifer C. Jaworski, MS, BCMAS, CMPP, and editing support by Kelsey Gribbon, MS, all of Ashfield MedComms, an Inizio company, and funded by Teva Branded Pharmaceutical Products R&D, Inc.
Data Sharing Statement
Qualified researchers may request access to patient-level data and related study documents, including the study protocol and the statistical analysis plan. Requests will be reviewed for scientific merit, product approval status, and conflicts of interest. Patient-level data will be de-identified, and study documents will be redacted to protect the privacy of trial participants and to protect commercially confidential information. Please email USMedInfo@tevapharm.com to make your request.
Ethics Approval and Informed Consent
This article is based on analyses from two studies (RISE and SHINE), which were both conducted in accordance with the Declaration of Helsinki. Ethical approval for RISE and SHINE was obtained from the Western IRB (20190551, 20180568, ICO1-18-072 [WCG]), New York State Psychiatric Institute (approval numbers not used), Copernicus Group (20190551, 20180568), and Republic of Bulgaria/Ethics Committee for Clinical Trials (KEMI/CT-0412, EKKI/ST-0985). Written informed consent or assent was obtained after study procedures were fully explained and before any study procedures were performed.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable to all aspects of the work.
Disclosure
Dr Citrome has been a consultant for AbbVie/Allergan, Acadia, Adamas, Alkermes, Angelini, Astellas, Avanir, Axsome, Biogen, BioXcel, Boehringer Ingelheim, Cadent Therapeutics, Cerevel, Clinilabs, COMPASS, Delpor, Eisai, Enteris BioPharma, HLS Therapeutics, Idorsia, INmune Bio, Impel, Intra-Cellular Therapies, Janssen, Karuna, Lundbeck, Luye, Lyndra, MapLight, Marvin, Medavante-ProPhase, Merck, Mitsubishi-Tanabe Pharma, Neumora, Neurocrine, Neurelis, Noema, Novartis, Noven, Otsuka, Ovid, Praxis, Recordati, Relmada, Reviva, Sage, Sumitomo/Sunovion, Supernus, Teva, University of Arizona, Vanda, Wells Fargo, and one-off ad hoc consulting for individuals/entities conducting marketing, commercial, or scientific scoping research; he has been a speaker for AbbVie/Allergan, Acadia, Alkermes, Angelini, Axsome, BioXcel, Eisai, Idorsia, Intra-Cellular Therapies, Janssen, Lundbeck, Neurocrine, Noven, Otsuka, Recordati, Sage, Sunovion, Takeda, Teva, and CME activities organized by medical education companies such as Medscape, NACCME, NEI, Vindico, and Universities and Professional Organizations/Societies; he owns a small number of shares of common stock in Bristol-Myers Squibb, Eli Lilly, J & J, Merck, and Pfizer purchased (>10 years ago) and has stock options in Reviva; and he receives royalties/publishing Income from Taylor & Francis (Editor-in-Chief, Current Medical Research and Opinion, 2022 to the present), Wiley (Editor-in-Chief, International Journal of Clinical Practice, through end of 2019), UpToDate (reviewer), Springer Healthcare (book), Elsevier (topic editor for psychiatry for the journal Clinical Therapeutics). Dr Suett is an employee and/or shareholder of Teva UK Limited. Dr Franzenburg is an employee and/or shareholder of Teva Branded Pharmaceutical Products R&D, Inc. Dr Eshet is an employee and/or shareholder of Teva Pharmaceutical Industries Ltd. Dr Elgart is an employee and/or shareholder of Teva Pharmaceutical Industries Ltd. Mr Davis 3rd is an employee and/or shareholder of Teva Branded Pharmaceutical Products R&D, Inc. Dr Harary is an employee and/or shareholder of Teva Pharmaceutical Industries Ltd. Ms Tohami is an employee and/or shareholder of Teva Pharmaceutical Industries Ltd. Dr Mychaskiw is an employee and/or shareholder of Teva Pharmaceutical Industries Ltd. Dr Kane has been a consultant for or received honoraria from Alkermes, Allergan, Boehringer-Ingelheim, Cerevel, Click Therapeutics, Dainippon Sumitomo, Eli Lilly, EnVivo Pharmaceuticals (Forum), Forest (Allergan), Genentech, HealthRhythms, HLS Therapeutics, Indivior, Intra-Cellular Therapies, Janssen, Johnson & Johnson, Karuna Therapeutics, LB Pharmaceuticals, Lundbeck, Lyndra Therapeutics, Merck, Minerva, Neurocrine Biosciences, Newron, Novartis, NW PharmaTech, Otsuka, Pierre Fabre, Reviva Pharmaceuticals, Roche, Saladax Biomedical, Sunovion, Takeda, and Teva Pharmaceuticals; has received grant support from Otsuka, Lundbeck, and Janssen; and is a shareholder of North Shore Therapeutics, LB Pharmaceuticals and Vanguard Research Group; has received royalties from UpToDate. The authors report no other conflicts of interest in this work.
References
- 1.Buckley PF. Treatment of schizophrenia: let’s talk dollars and sense. Am J Manag Care. 1998;4(3):369–383. Erratum in: Am J Manag Care. 1998;4(4):611. [PubMed] [Google Scholar]
- 2.GBD 2019. Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiat. 2022;9(2):137–150. doi: 10.1016/S2215-0366(21)00395-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Biagi E, Capuzzi E, Colmegna F, et al. Long-acting injectable antipsychotics in schizophrenia: literature review and practical perspective, with a focus on aripiprazole once-monthly. Adv Ther. 2017;34(5):1036–1048. doi: 10.1007/s12325-017-0507-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Institute for Health and Care Excellence. Psychosis and schizophrenia in adults: prevention and management. 2014. Available from: http://www.nice.org.uk/guidance/cg178. Accessed June 17, 2021. [PubMed]
- 5.Patel KR, Cherian J, Gohil K, Atkinson D. Schizophrenia: overview and treatment options. P T. 2014;39(9):638–645. [PMC free article] [PubMed] [Google Scholar]
- 6.Wu EQ, Shi L, Birnbaum H, Hudson T, Kessler R. Annual prevalence of diagnosed schizophrenia in the USA: a claims data analysis approach. Psychol Med. 2006;36(11):1535–1540. doi: 10.1017/S0033291706008191 [DOI] [PubMed] [Google Scholar]
- 7.Csernansky JG, Mahmoud R, Brenner R. A comparison of risperidone and haloperidol for the prevention of relapse in patients with schizophrenia. N Engl J Med. 2002;346(1):16–22. doi: 10.1056/NEJMoa002028 Erratum in: N Engl J Med. 2002;346(18):1424. [DOI] [PubMed] [Google Scholar]
- 8.Kane JM. Treatment strategies to prevent relapse and encourage remission. J Clin Psychiatry. 2007;68(14):27–30. [PubMed] [Google Scholar]
- 9.Levander S, Jensen J, Gråwe R, Tuninger E. Schizophrenia–progressive and massive decline in response readiness by episodes. Acta Psychiatr Scand Suppl. 2001;2001(408):65–74. doi: 10.1034/j.1600-0447.2001.104s408065.x [DOI] [PubMed] [Google Scholar]
- 10.Alvarez-Jimenez M, Priede A, Hetrick SE, et al. Risk factors for relapse following treatment for first episode psychosis: a systematic review and meta-analysis of longitudinal studies. Schizophr Res. 2012;139(1–3):116–128. doi: 10.1016/j.schres.2012.05.007 [DOI] [PubMed] [Google Scholar]
- 11.Mercieca-Bebber R, King MT, Calvert MJ, Stockler MR, Friedlander M. The importance of patient-reported outcomes in clinical trials and strategies for future optimization. Patient Relat Outcome Meas. 2018;9:353–367. doi: 10.2147/PROM.S156279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.H-J Au, Ringash J, Brundage M, et al. Added value of health-related quality of life measurement in cancer clinical trials: the experience of the NCIC CTG. Exp Rev Pharmacoecon Outcome Res. 2010;10(2):119–128. doi: 10.1586/erp.10.15 [DOI] [PubMed] [Google Scholar]
- 13.Mead S, Copeland ME. What recovery means to us: consumers’ perspectives. Community Ment Health J. 2000;36(3):315–328. doi: 10.1023/a:1001917516869 [DOI] [PubMed] [Google Scholar]
- 14.Farkas M, Gagne C, Anthony W, Chamberlin J. Implementing recovery oriented evidence based programs: identifying the critical dimensions. Community Ment Health J. 2005;41(2):141–158. doi: 10.1007/s10597-005-2649-6 [DOI] [PubMed] [Google Scholar]
- 15.Resnick SG, Fontana A, Lehman AF, Rosenheck RA. An empirical conceptualization of the recovery orientation. Schizophr Res. 2005;75(1):119–128. doi: 10.1016/j.schres.2004.05.009 [DOI] [PubMed] [Google Scholar]
- 16.Peebles SA, Mabe PA, Davidson L, Fricks L, Buckley PF, Fenley G. Recovery and systems transformation for schizophrenia. Psychiatr Clin North Am. 2007;30(3):567–583. doi: 10.1016/j.psc.2007.04.009 [DOI] [PubMed] [Google Scholar]
- 17.Davidson L, O’Connell MJ, Tondora J, Lawless M, Evans AC. Recovery in serious mental illness: a new wine or just a new bottle? Prof Psychol Res Pr. 2005;36(5):480–487. doi: 10.1037/0735-7028.36.5.480 [DOI] [Google Scholar]
- 18.Substance Abuse and Mental Health Services Administration. SAMHSA’s Working Definition of Recovery. 2012. Available from: https://store.samhsa.gov/sites/default/files/d7/priv/pep12-recdef.pdf. Accessed June 16, 2023.
- 19.Novick D, Haro JM, Suarez D, Vieta E, Naber D. Recovery in the outpatient setting: 36-month results from the Schizophrenia Outpatients Health Outcomes (SOHO) study. Schizophr Res. 2009;108(1–3):223–230. doi: 10.1016/j.schres.2008.11.007 [DOI] [PubMed] [Google Scholar]
- 20.Jääskeläinen E, Juola P, Hirvonen N, et al. A systematic review and meta-analysis of recovery in schizophrenia. Schizophr Bull. 2013;39(6):1296–1306. doi: 10.1093/schbul/sbs130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dassa D, Boyer L, Benoit M, Bourcet S, Raymondet P, Bottai T. Factors associated with medication non-adherence in patients suffering from schizophrenia: a cross-sectional study in a universal coverage health-care system. Aust N Z J Psychiat. 2010;44(10):921–928. doi: 10.3109/00048674.2010.493503 [DOI] [PubMed] [Google Scholar]
- 22.Citrome L, Mychaskiw MA, Cortez A, Opler M, Sopina L, Kotak S. Clinical outcome assessment instruments in schizophrenia: a scoping literature review with a focus on the potential of patient-reported outcomes. Innov Clin Neurosci. 2023;20(4–6):14–33. [PMC free article] [PubMed] [Google Scholar]
- 23.Seow LSE, Tan THG, Abdin E, Chong SA, Subramaniam M. Comparing disease-specific and generic quality of life measures in patients with schizophrenia. Psychiatry Res. 2019;273:387–393. doi: 10.1016/j.psychres.2019.01.034 [DOI] [PubMed] [Google Scholar]
- 24.Awad AG, Voruganti LN. The impact of newer atypical antipsychotics on patient-reported outcomes in schizophrenia. CNS Drugs. 2013;27(8):625–636. doi: 10.1007/s40263-013-0070-1 [DOI] [PubMed] [Google Scholar]
- 25.Calvert M, Kyte D, Mercieca-Bebber R, et al. Guidelines for inclusion of patient-reported outcomes in clinical trial protocols: the SPIRIT-PRO extension. JAMA. 2018;319(5):483–494. doi: 10.1001/jama.2017.21903 [DOI] [PubMed] [Google Scholar]
- 26.Kristensen S, Mainz J, Baandrup L, et al. Conceptualizing patient-reported outcome measures for use within two Danish psychiatric clinical registries: description of an iterative co-creation process between patients and healthcare professionals. Nord J Psychiat. 2018;72(6):409–419. doi: 10.1080/08039488.2018.1492017 [DOI] [PubMed] [Google Scholar]
- 27.US Department of Health and Human Services. Guidance for industry—patient-reported outcome measures: use in medical product development to support labeling claims. US Food and Drug Administration. 2009. Available from: https://www.fda.gov/media/77832/download. Accessed October 5, 2023.
- 28.Greene M, Yan T, Chang E, Hartry A, Touya M, Broder MS. Medication adherence and discontinuation of long-acting injectable versus oral antipsychotics in patients with schizophrenia or bipolar disorder. J Med Econ. 2018;21(2):127–134. doi: 10.1080/13696998.2017.1379412 [DOI] [PubMed] [Google Scholar]
- 29.Kishimoto T, Hagi K, Kurokawa S, Kane JM, Correll CU. Long-acting injectable versus oral antipsychotics for the maintenance treatment of schizophrenia: a systematic review and comparative meta-analysis of randomised, cohort, and pre-post studies. Lancet Psychiat. 2021;8(5):387–404. doi: 10.1016/S2215-0366(21)00039-0 [DOI] [PubMed] [Google Scholar]
- 30.Pilon D, Joshi K, Tandon N, et al. Treatment patterns in Medicaid patients with schizophrenia initiated on a first- or second-generation long-acting injectable versus oral antipsychotic. Patient Prefer Adherence. 2017;11:619–629. doi: 10.2147/PPA.S127623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Subotnik KL, Casaus LR, Ventura J, et al. Long-acting injectable risperidone for relapse prevention and control of breakthrough symptoms after a recent first episode of schizophrenia: a randomized clinical trial. JAMA Psychiatry. 2015;72(8):822–829. doi: 10.1001/jamapsychiatry.2015.0270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Olagunju AT, Clark SR, Baune BT. Long-acting atypical antipsychotics in schizophrenia: a systematic review and meta-analyses of effects on functional outcome. Aust N Z J Psychiat. 2019;53(6):509–527. doi: 10.1177/0004867419837358 [DOI] [PubMed] [Google Scholar]
- 33.Kane JM, Correll CU. Past and present progress in the pharmacologic treatment of schizophrenia. J Clin Psychiatry. 2010;71(9):1115–1124. doi: 10.4088/JCP.10r06264yel [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Citrome L. Long-acting injectable antipsychotics: what, when, and how. CNS Spectr. 2021;26(2):118–129. doi: 10.1017/S1092852921000249 [DOI] [PubMed] [Google Scholar]
- 35.Teva Neuroscience, Inc. Uzedy™ (Risperidone) Extended-Release Injectable Suspension. Prescribing Information. 2024. [Google Scholar]
- 36.Kane JM, Harary E, Eshet R, et al. Efficacy and safety of TV-46000, a long-acting, subcutaneous, injectable formulation of risperidone, for schizophrenia: a randomised clinical trial in the USA and Bulgaria. Lancet Psychiat. 2023;10(12):934–943. doi: 10.1016/S2215-0366(23)00288-2 [DOI] [PubMed] [Google Scholar]
- 37.Perlstein I, Merenlender Wagner A, Gomeni R, et al. Population pharmacokinetic modeling and simulation of TV-46000: a long-acting injectable formulation of risperidone. Clin Pharmacol Drug Dev. 2022;11(7):865–877. doi: 10.1002/cpdd.1078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Merenlender Wagner A, Elgart A, Perlstein I, et al. Phase 1 open-label study assessing the pharmacokinetics and safety of TV-46000, a novel long-acting subcutaneous injectable formulation of risperidone. Eur Neuropsychopharmacol. 2021;53:S339–S340. doi: 10.1016/j.euroneuro.2021.10.436 [DOI] [Google Scholar]
- 39.Kane JM, Eshet R, Harary E, et al. A long-term safety and tolerability study of TV-46000 for subcutaneous use in adult and adolescent patients with schizophrenia: a phase 3, randomized, double-blinded clinical trial. CNS Drugs. 2024;38(8):625–636. Epub ahead of print. doi: 10.1007/s40263-024-01102-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nasrallah H, Morosini P, Gagnon DD. Reliability, validity and ability to detect change of the Personal and Social Performance scale in patients with stable schizophrenia. Psychiatry Res. 2008;161(2):213–224. doi: 10.1016/j.psychres.2007.11.012 [DOI] [PubMed] [Google Scholar]
- 41.Isjanovski V, Naumovska A, Bonevski D, Novotni A. Validation of the Schizophrenia Quality of Life Scale Revision 4 (SQLS-R4) among patients with schizophrenia. Open Access Maced J Med Sci. 2016;4(1):65–69. doi: 10.3889/oamjms.2016.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nielsen RE, Lindstrom E, Nielsen J, Levander S. DAI-10 is as good as DAI-30 in schizophrenia. Eur Neuropsychopharmacol. 2012;22(10):747–750. doi: 10.1016/j.euroneuro.2012.02.008 [DOI] [PubMed] [Google Scholar]
- 43.Pitkänen A, Välimäki M, Endicott J, et al. Assessing quality of life in patients with schizophrenia in an acute psychiatric setting: reliability, validity and feasibility of the EQ-5D and the Q-LES-Q. Nord J Psychiat. 2012;66(1):19. doi: 10.3109/08039488.2011.593099 [DOI] [PubMed] [Google Scholar]
- 44.Prieto L, Sacristán JA, Hormaechea JA, Casado A, Badia X, Gómez JC. Psychometric validation of a generic health-related quality of life measure (EQ-5D) in a sample of schizophrenic patients. Curr Med Res Opin. 2004;20(6):827. doi: 10.1185/030079904125003674 [DOI] [PubMed] [Google Scholar]
- 45.Morosini PL, Magliano L, Brambilla L, Ugolini S, Pioli R. Development, reliability and acceptability of a new version of the DSM-IV Social and Occupational Functioning Assessment Scale (SOFAS) to assess routine social functioning. Acta Psychiatr Scand. 2000;101(4):323–329. [PubMed] [Google Scholar]
- 46.Jelastopulu E, Giourou E, Merekoulias G, Mestousi A, Moratis E, Alexopoulos EC. Correlation between the Personal and Social Performance scale (PSP) and the Positive and Negative Syndrome Scale (PANSS) in a Greek sample of patients with schizophrenia. BMC Psychiatry. 2014;14(1):197. doi: 10.1186/1471-244X-14-197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001;33(5):337–343. doi: 10.3109/07853890109002087 [DOI] [PubMed] [Google Scholar]
- 48.EuroQol Group. EuroQol—a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 49.Hogan TP, Awad AG, Eastwood R. A self-report scale predictive of drug compliance in schizophrenics: reliability and discriminative validity. Psychol Med. 1983;13(1):177–183. doi: 10.1017/s0033291700050182 [DOI] [PubMed] [Google Scholar]
- 50.Hough D, Gopal S, Vijapurkar U, Lim P, Morozova M, Eerdekens M. Paliperidone palmitate maintenance treatment in delaying the time-to-relapse in patients with schizophrenia: a randomized, double-blind, placebo-controlled study. Schizophr Res. 2010;116(2–3):107–117. doi: 10.1016/j.schres.2009.10.026 [DOI] [PubMed] [Google Scholar]
- 51.Berwaerts J, Liu Y, Gopal S, et al. Efficacy and safety of the 3-month formulation of paliperidone palmitate vs placebo for relapse prevention of schizophrenia: a randomized clinical trial. JAMA Psychiatry. 2015;72(8):830–839. doi: 10.1001/jamapsychiatry.2015.0241 [DOI] [PubMed] [Google Scholar]
- 52.Barrio P, Batalla A, Castellví P, et al. Effectiveness of long-acting injectable risperidone versus oral antipsychotics in the treatment of recent-onset schizophrenia: a case-control study. Int Clin Psychopharmacol. 2013;28(4):164–170. doi: 10.1097/YIC.0b013e3283611cc3 [DOI] [PubMed] [Google Scholar]
- 53.Levitan B, Markowitz M, Turkoz I, Fu DJ, Gopal S, Alphs L. Benefit-risk assessment of paliperidone oral extended-release tablet versus monthly injectable for maintenance treatment of schizophrenia. Int Clin Psychopharmacol. 2016;31(6):315–322. doi: 10.1097/YIC.0000000000000141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wykes T, Rose D, Williams P, David AS. Working alliance and its relationship to outcomes in a randomized controlled trial (RCT) of antipsychotic medication. BMC Psychiatry. 2013;13(1):28. doi: 10.1186/1471-244X-13-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rosenheck RA, Krystal JH, Lew R, et al. Long-acting risperidone and oral antipsychotics in unstable schizophrenia. N Engl J Med. 2011;364(9):842–851. doi: 10.1056/NEJMoa1005987 Erratum in: N Engl J Med. 2011;364(13):1281. [DOI] [PubMed] [Google Scholar]
- 56.An efficacy and safety study of long acting injectable risperidone and oral risperidone in participants with schizophrenia or schizoaffective disorder. ClinicalTrials.gov identifier: NCT00992407. 2014. Available from: https://clinicaltrials.gov/study/NCT00992407. Accessed October 23, 2023.
- 57.Rouillon F, Eriksson L, Burba B, Raboch J, Kaprinis G, Schreiner A. Functional recovery results from the risperidone long-acting injectable versus quetiapine relapse prevention trial (ConstaTRE). Acta Neuropsychiat. 2013;25(5):297–306. doi: 10.1017/neu.2013.7 [DOI] [PubMed] [Google Scholar]
- 58.Joshi K, Lafeuille MH, Kamstra R, et al. Real-world adherence and economic outcomes associated with paliperidone palmitate versus oral atypical antipsychotics in schizophrenia patients with substance-related disorders using Medicaid benefits. J Comp Eff Res. 2018;7(2):121–133. doi: 10.2217/cer-2017-0043 [DOI] [PubMed] [Google Scholar]
- 59.Docherty JP, Jones R, Turkoz I, Lasser RA, Kujawa M. Evaluation of a treatment manual for risperidone long-acting injectable. Community Ment Health J. 2007;43(3):267–280. doi: 10.1007/s10597-006-9081-4 [DOI] [PubMed] [Google Scholar]
- 60.Robinson DG, Suett M, Wilhelm A, et al. Patient and healthcare professional preferences for characteristics of long-acting injectable antipsychotic agents for the treatment of schizophrenia. Adv Ther. 2023;40(5):2249–2264. doi: 10.1007/s12325-023-02455-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tiihonen J, Mittendorfer-Rutz E, Majak M, et al. Real-world effectiveness of antipsychotic treatments in a nationwide cohort of 29 823 patients with schizophrenia. JAMA Psychiatry. 2017;74(7):686–693. doi: 10.1001/jamapsychiatry.2017.1322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nielsen RE, Hessellund KB, Valentin JB, Licht RW. Second-generation LAI are associated to favorable outcome in a cohort of incident patients diagnosed with schizophrenia. Schizophr Res. 2018;202:234–240. doi: 10.1016/j.schres.2018.07.020 [DOI] [PubMed] [Google Scholar]
- 63.Brasso C, Bellino S, Bozzatello P, et al. Second Generation Long-Acting Injectable Antipsychotics in Schizophrenia: the Patient’s Subjective Quality of Life, Well-Being, and Satisfaction. J Clin Med. 2023;12(22):6985. doi: 10.3390/jcm12226985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Au HJ, Ringash J, Brundage M, et al. Determinants of real-world functional performance in schizophrenia subjects: correlations with cognition, functional capacity, and symptoms. Am J Psychiat. 2006;163(3):418–425. doi: 10.1176/appi.ajp.163.3.418 [DOI] [PubMed] [Google Scholar]
- 65.Sabbag S, Twamley EM, Vella L, Heaton RK, Patterson TL, Harvey PD. Assessing everyday functioning in schizophrenia: not all informants seem equally informative. Schizophr Res. 2011;131(1–3):250–255. doi: 10.1016/j.schres.2011.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Durand D, Strassnig M, Sabbag S, et al. Factors influencing self-assessment of cognition and functioning in schizophrenia: implications for treatment studies. Eur Neuropsychopharmacol. 2015;25(2):185–191. doi: 10.1016/j.euroneuro.2014.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.McKibbin C, Patterson TL, Jeste DV. Assessing disability in older patients with schizophrenia: results from the WHODAS-II. J Nerv Ment Dis. 2004;192(6):405–413. doi: 10.1097/01.nmd.0000130133.32276.83 [DOI] [PubMed] [Google Scholar]
- 68.Patterson TL, Semple SJ, Shaw WS, et al. Self-reported social functioning among older patients with schizophrenia. Schizophr Res. 1997;27(2–3):199–210. doi: 10.1016/S0920-9964(97)00078-9 [DOI] [PubMed] [Google Scholar]
- 69.Gould F, McGuire LS, Durand D, et al. Self-assessment in schizophrenia: accuracy of evaluation of cognition and everyday functioning. Neuropsychology. 2015;29(5):675–682. doi: 10.1037/neu0000175 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Qualified researchers may request access to patient-level data and related study documents, including the study protocol and the statistical analysis plan. Requests will be reviewed for scientific merit, product approval status, and conflicts of interest. Patient-level data will be de-identified, and study documents will be redacted to protect the privacy of trial participants and to protect commercially confidential information. Please email USMedInfo@tevapharm.com to make your request.