Abstract
Aims
Surgical limb sparing for knee-bearing paediatric bone sarcoma is considered to have a clinically significant influence on postoperative function due to complications and leg-length discrepancies. However, researchers have not fully evaluated the long-term postoperative functional outcomes. Therefore, in this study, we aimed to elucidate the risk factors and long-term functional prognosis associated with paediatric limb-sparing surgery.
Methods
We reviewed 40 patients aged under 14 years who underwent limb-sparing surgery for knee bone sarcoma (15 cases in the proximal tibia and 25 in the distal femur) between January 2000 and December 2013, and were followed up for a minimum of five years. A total of 35 patients underwent reconstruction using artificial materials, and five underwent biological reconstruction. We evaluated the patients’ postoperative complications, survival rate of reconstruction material, and limb, limb function, and leg-length discrepancy at the final follow-up, as well as the risk factors for each.
Results
Complications were observed in 55% (22/40) of patients. The limb survival and reconstruction material rates at five and ten years were 95% and 91%, and 88% and 66%, respectively. Infection was the only risk factor in both survivals (p < 0.001, p = 0.019). In the 35 patients with limb preservation, the median International Society of Limb Salvage (ISOLS) score at the final follow-up was 80 (47% to 97%). Younger age (p = 0.027) and complications (p = 0.005) were poor prognostic factors. A negative correlation was found between age and leg-length discrepancy (R = −0.426; p = 0.011). The ISOLS scores were significantly lower in patients with a leg-length discrepancy of more than 5 cm (p = 0.005).
Conclusion
Young age and complications were linked to an unfavourable functional prognosis. Leg-length correction was insufficient, especially in very young children, resulting in decreased function of the affected limb. Limb-sparing surgery for these children remains a considerable challenge.
Cite this article: Bone Jt Open 2024;5(10):868–878.
Keywords: Limb-sparing surgery, Functional outcome, Paediatric bone sarcoma, paediatric bone sarcomas, limb-sparing surgery, knee, functional outcomes, infections, Leg-length discrepancies, distal femoral, postoperative complications, Biological reconstruction, limb salvage
Introduction
The most common malignant bone sarcoma in children is osteosarcoma, which accounts for 60% of cases and most commonly affects the knee joint.1 Wide resection and neoadjuvant chemotherapy is the standard treatment for osteosarcoma. Currently, the five-year survival rate for patients with osteosarcoma without metastases has improved to approximately 70%.2 Furthermore, advances in diagnostic imaging and surgical techniques have made it possible to spare limbs in nearly 90% of cases. Therefore, it is crucial to achieve good long-term limb function.3,4
Two types of reconstruction can be performed after wide resection: biological and artificial material reconstruction. However, in children, both types of reconstruction often result in long-term functional loss due to the subsequent leg-length discrepancy.3-5 Therefore, many cases require multiple surgeries to correct these discrepancies, and the high frequency of postoperative complications remains a significant challenge.5,6
In this study, we analyze the risk factors affecting postoperative limb function in limb-sparing surgery for paediatric bone sarcomas and discuss what is needed to improve postoperative limb function.
Methods
Study design
This multicentre, retrospective, observational research was conducted by the Higashi-Nihon Orthopaedic and Paediatric Sarcoma Group, Japan. The study was approved by the Ethical Review Committee of each institution, information about the conduct of the study was disclosed using an opt-out procedure, and the opportunity to refuse participation was guaranteed. Information obtained from medical records and radiological images was retrospectively analyzed.
Inclusion criteria
The inclusion criteria were as follows: 1) patients with malignant bone tumours around the knee; 2) children aged < 14 years at the time of initial diagnosis; 3) patients treated with limb-sparing surgery at the authors’ four institutions between January 2000 and December 2013; and 4) patients who were followed up for at least five years after the initial limb-sparing surgery. Patients with insufficient clinical information were excluded.
Patients
This series included 19 males and 21 females. The median age at initial surgery was 11 years (IQR 10 to 13), and the median postoperative follow-up time was 135.2 months (IQR 95.2 to 166.1). The histological subtypes included 39 patients with osteosarcoma and one patient with pleomorphic sarcoma. In total, 25 tumours were located in the distal femur and 15 in the proximal tibia. The median tumour size was 8.7 cm (IQR 7.1 to 11.0). According to the American Joint Committee on Cancer staging (seventh classification),7 715 cases (38%) were stage IIA, 24 (60%) were stage IIB, and one (2%) was stage IVB.
Treatment
All 40 patients underwent wide tumour resection (R0 resection). Biological reconstruction using autologous bone was performed in five patients for whom joint preservation was possible (frozen bone (n = 2), pasteurized bone (n = 2), and irradiated bone (n = 1)), while endoprosthesis was performed in 35 patients for whom joint preservation was impossible. Expandable endoprostheses were used in 24 patients aged < 12 years old who were skeletally immature, nine of whom underwent a two-stage reconstruction with ceramic spacers because the medullary cavity was too small to insert the expandable endoprosthesis at the time of initial surgery (n = 2), and because the custom-made expandable prostheses were not available in time for surgery (n = 7). Modular prostheses were used in the remaining 11 patients, who were older than 12 years old and relatively skeletally mature. All patients underwent pre-/postoperative adjuvant chemotherapy using methotrexate, doxorubicin, and cisplatin with or without ifosfamide as per the following protocol: JCOG0905 (n = 6);8 NECO95 (n = 4);8,9 ISG/OS1 (n = 2);10 other (n = 28). None of the patients received adjuvant radiotherapy.
Follow-up
Routine medical follow-up, including physical examination, radiographs, and chest or whole-body CT, was performed at three-month intervals for two years, then every four to six months for three years, and then annually.
Oncological results
At the final follow-up, the patients were categorized into three groups based on their prognosis: those who remained disease-free, those who displayed no signs of disease, and those who continued to live with the disease.
Complications
Postoperative complications were classified according to the Extended Clavien-Dindo classification of surgical complications,11 and the time of onset, the number of operations for the complication, and risk factors were evaluated for those with > grade IIIb complications requiring surgical intervention. A complication was classified as late if it occurred more than six months following the first surgery, and as early if it occurred within six months of the initial procedure. The available surgical procedures for addressing issues such as debridement, amputation, arthrodesis, and one- or two-stage revisions after prosthesis removal were also investigated.
Reconstruction and limb survival
The duration of the reconstructions and limb survival were determined from the initial surgery to the occurrence of revision, amputation, or the most recent follow-up. Success of limb salvage was determined by whether the patient retained their limb at the final follow-up, irrespective of any complications or revisions. Risk factors affecting reconstruction and limb survival were also analyzed.
Leg-length discrepancy
Healthcare providers measured the limb-length discrepancy through a physical examination or radiograph during the follow-up. A discrepancy of > 2 cm was considered for the use of a shoe lift or endoprosthetic expansion, and > 4 cm for distraction osteogenesis. At the last follow-up, we assessed the difference in limb length and analyzed the factors influencing the limb-length discrepancy.
Function
Limb function at the final follow-up was assessed using scores established by the International Society of Limb Salvage (ISOLS).12 We analyzed the factors that influenced limb function.
Statistical analysis
We conducted statistical analyses using GraphPad Prism 8 software (GraphPad, USA). We used Fisher’s exact test or logistic regression analysis to compare two groups of categorical variables, the Mann-Whitney U test to examine discrete variables, and the Spearman’s r test to analyze continuous variables. Researchers employed the Kruskal-Wallis test to analyze discrete variables when comparing three or more groups, and used the chi-squared test to analyze categorical variables. We used the Kaplan-Meier method to calculate the survival time, and the log-rank test to compare survival times. A p-value < 0.05 was considered statistically significant.
Results
Characteristics of the patients
Table I summarizes the comparisons of patient characteristics for each reconstruction. The age at the surgery was significantly lower in the expandable prosthesis and ceramic spacer groups than in the modular prosthesis and biological reconstruction groups, with a median age of 11 years (7 to 13), 12 years (5 to 13), 14 years (12 to 15), and 14 years (7 to 14), respectively (p = 0.001, all chi-squared test). The tumour size tended to be larger in the modular prosthesis and ceramic spacer group than in the expandable prosthesis and biological reconstruction group (p = 0.092), while the tumour location (p = 0.210) and TNM classification (p = 0.276, all chi-squared test) did not differ significantly between reconstructions.
Table I.
Patient demographics and tumour data.
| Variable | Total (n = 40) | Reconstruction methods | ||||
|---|---|---|---|---|---|---|
| Expandable prosthesis (n = 15) | Spacer (n = 9) | Modular prosthesis (n = 11) | Biological reconstruction (n = 5) | p-value | ||
| Patient data | ||||||
| Sex, n (%) | 0.357* | |||||
| Male | 19 (48) | 6 (40) | 5 (56) | 4 (36) | 4 (80) | |
| Female | 21 (52) | 9 (60) | 4 (44) | 7 (64) | 1 (20) | |
| Median age at operation, yrs (IQR) | 11 (10 to 13) | 11 (9 to 11) | 12 (10 to 12) | 14 (13 to 14) | 14 (10 to 14) | 0.001† |
| Median height at operation, cm (IQR) | 147.3 (136.5 to 163.9) |
141.8 (135.0 to 146.2) |
140.0 (126.8 to 146.5) |
163.2 (153.7 to 167.5) |
170.0 (149.0.0 to 170.0) | 0.005† |
| Tumour data | ||||||
| Site, n (%) | 0.210* | |||||
| Distal femur | 25 (63) | 11 (73) | 3 (33) | 8 (73) | 3 (60) | |
| Proximal tibia | 15 (37) | 4 (27) | 6 (67) | 3 (27) | 2 (40) | |
| Median maximum tumour diameter, cm (IQR) | 8.7 (7.1 to 11.0) | 7.6 (6.4 to 9.3) | 9.7 (8.1 to 10.8) | 10.4 (8.6 to 13.5) | 6.4 (5.2 to 8.6) | 0.092† |
| TNM, n (%) | 0.276* | |||||
| Stage IIA | 15 (38) | 8 (53) | 2 (22) | 2 (18) | 3 (60) | |
| Stage IIB | 24 (60) | 7 (47) | 7 (78) | 8 (73) | 2 (40) | |
| Stage IVB | 1 (2) | 0 | 0 | 1 (9) | 0 | |
| Oncological results | ||||||
| Median follow-up, mths (IQR) | 135.2 (95.2 to 166.1) | 108.0 (96.6 to 141.8) | 183.5 (161.3 to 203.2) |
113.6 ( 85.2 to 121.8) | 121.6 (105.0 to 180.6) | 0.022† |
| Local recurrence, n (%) | ||||||
| Yes | 0 | 0 | 0 | 0 | 0 | |
| No | 40 (100) | 15 (100) | 9 (100) | 11 (100) | 5 (100) | |
| Distant metastases, n (%) | 0.124* | |||||
| Yes | 8 (20) | 2 (13) | 0 | 4 (36) | 2 (40) | |
| No | 32 (80) | 13 (87) | 9 (100) | 7 (64) | 3 (60) | |
| Outcome at the final follow-up, n (%) | 0.124* | |||||
| CDF | 32 (80) | 13 (87) | 9 (100) | 7 (64) | 3 (60) | |
| NED | 8 (20) | 2 (13) | 0 | 4 (36) | 2 (40) | |
Chi-squared test.
Kruskal-Wallis test.
CDF, continuous disease-free; NED, no evidence of disease.
The follow-up time of the ceramic spacer group was significantly longer than that of the expandable prosthesis, modular prosthesis, and biological reconstruction groups (p = 0.022, Kruskal-Wallis test), while no cases showed local recurrence. Eight patients showed distant metastasis, all of whom had pulmonary metastases and remained disease-free after resection. The oncological outcomes at the final follow-up included continuous freedom from disease in 32 patients and no evidence of disease in eight. The oncological outcomes did not differ significantly between reconstructions (p = 0.124, chi-squared test).
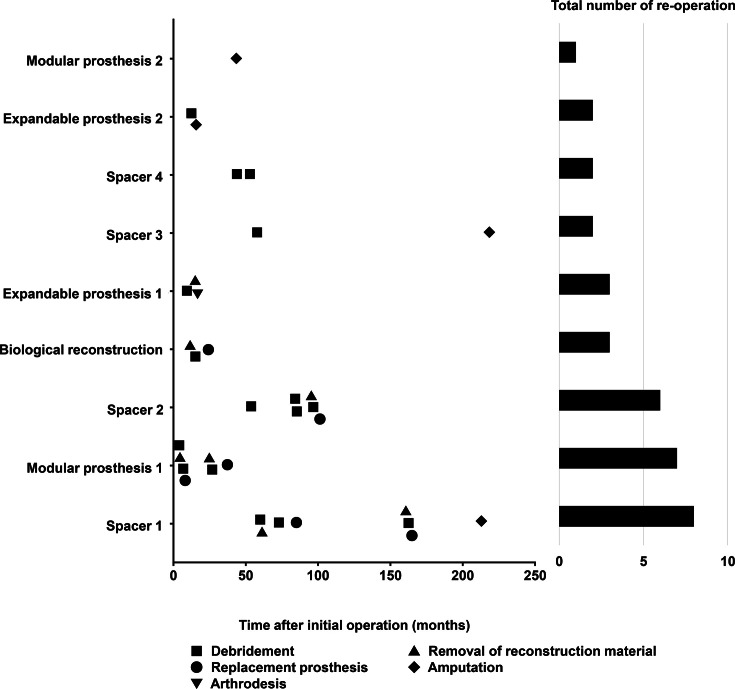
Complications
Table II shows the frequency, type, and number of surgeries for complications among each reconstruction. We observed no significant difference in the complication frequency between reconstructions for both grade IIIB (p = 0.378) and IV (p = 0.858) cases. The median time of complication onset was 35.3 months (0.3 to 112.3, with early onset (four cases) and late onset (18 cases). Complications included infection in nine cases, implant fracture in six, wound dehiscence in four, fracture in three, loosening and dislocation in two each, and nonunion, malalignment, and contracture in one each (including duplicate patients). The median number of surgeries for each complication was 1.5 (IQR 1 to 2); infection had the highest number of surgeries, with a median of 3 (IQR 2 to 6) (p = 0.082, chi-squared test). We assessed the potential biases between groups regarding the presence (n = 9) or absence (n = 31) of infection, but found no significant bias related to the method of reconstruction (p = 0.342, chi-squared test), sex (p = 0.457), age (p = 0.271), site (p = 0.440), or maximum tumour diameter (p = 0.227). Figure 1 describes the details of surgical treatment for infections. Surgical treatment ultimately cured the infection in eight of the nine cases. The median number of surgeries required for healing was 3 (IQR 2 to 6), and the median duration of surgery from initial surgery was 54.0 months (IQR 12.7 to 55.1). Four cases required reconstruction material removal, and four cases required amputation. Moreover, 134.8 months after onset, the remaining patient underwent two debridements, but remains uncured and is still undergoing treatment.
Table II.
Complications and number of reoperations.
| Variable | Total (n = 40) | Reconstruction methods | ||||
|---|---|---|---|---|---|---|
| Expandable prosthesis (n = 15) | Spacer (n = 9) | Modular prosthesis (n = 11) | Biological reconstruction (n = 5) | p-value | ||
| Complication, n (%) | ||||||
| Yes | 22 (55) | 6 (40) | 5 (56) | 8 (73) | 3 (60) | 0.872* |
| Grade IIIB, n (%) | 21 (53) (45 surgeries) |
6 (40) (8 surgeries) |
5 (56) (18 surgeries) |
8 (73) (15 surgeries) |
2 (40) (4 surgeries) |
0.378* |
| Grade IV, n (%) | 4 (10) (5 surgeries) |
2 (13) (3 surgeries) |
1 (11) (1 surgery) |
1 (13) (1 surgery) |
0 | 0.858* |
| Unknown, n (%) | 2 (5) (7 surgeries) |
0 | 1 (11) (1 surgery) |
0 | 1 (20) (6 surgeries) |
|
| No, n (%) | 18 (45) | 9 (60) | 4 (44) | 3 (27) | 2 (40) | |
| Complication details, n (%) | ||||||
| Infection | 9 (23) | 2 (13) | 4 (44) | 2 (18) | 1 (20) | 0.342* |
| Implant fracture | 6 (15) | 2 (13) | 0 | 3 (27) | 1 (20) | |
| Wound dehiscence | 4 (10) | 1 (7) | 1 (11) | 2 (18) | 0 | |
| Fracture | 3 (8) | 0 | 1 (11) | 0 | 2 (40) | |
| Loosening | 2 (5) | 1 (7) | 0 | 1 (9) | 0 | |
| Dislocation | 2 (5) | 0 | 0 | 1 (9) | 1 (20) | |
| Malalignment | 1 (3) | 1 (7) | 0 | 0 | 0 | |
| Contracture | 1 (3) | 1 (7) | 0 | 0 | 0 | |
| Nonunion | 1 (3) | 0 | 0 | 0 | 1 (20) | |
| Number of reoperations, n (%) | ||||||
| 1 | 10 (25) | 4 (27) | 1 (11) | 5 (45) | 0 (0.0) | 0.339† |
| 2 | 7 (18) | 1 (7) | 2 (22) | 2 (18) | 2 (40) | |
| 3 | 1 (3) | 1 (7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| 4 | 2 (5) | 0 (0.0) | 1 (11) | 0 (0.0) | 1 (20) | |
| 5 | 1 (3) | 0 (0.0) | 0 (0.0) | 1 (9) | 0 (0.0) | |
| 6 | 1 (3) | 0 (0.0) | 1 (11) | 0 (0.0) | 0 (0.0) | |
Chi-squared test.
Fisher’s exact test.
Fig. 1.
Details of surgery for infection, including the timing and surgical types of the nine infected cases. The surgical types for infection are indicated as follows: ■, debridement; ▲, removal of reconstruction material; ●, arthroplasty prosthesis;▼, arthrodesis; ◆ amputation. Each case shows the reconstruction methods for limb-sparing surgery on the left vertical axis. The time period from the date of the limb-sparing surgery is shown on the horizontal axis. A bar graph on the right vertical axis shows the number of surgeries for infection.
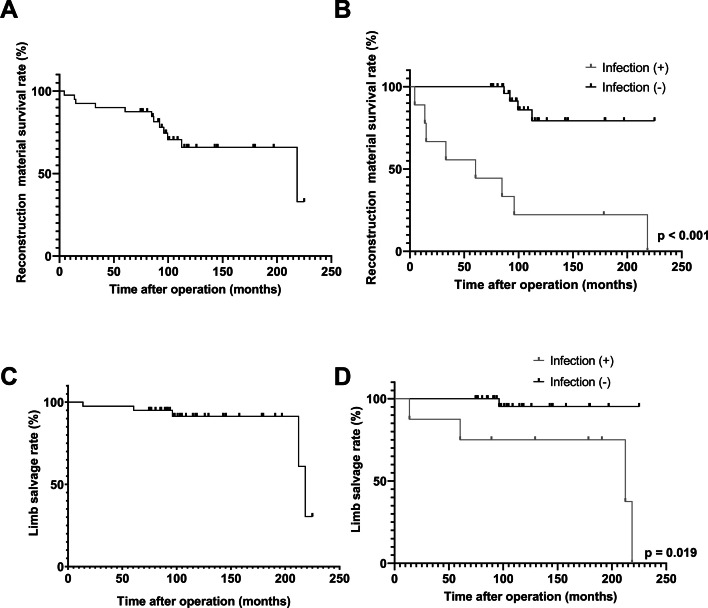
Reconstruction survival
The survival rate of reconstructions was 88% at five years and 66% at ten years (Figure 2a). Overall, 12 of 40 cases (30%) underwent reconstruction material removal, and the median time to removal from first surgery was 92.0 months (IQR 28.5 to 96.8). The causes contributing to the removal of reconstructions were all complications, including infection in eight cases, implant fracture in two, and fracture and loosening in one each. Univariate analysis was performed for postoperative complications, infection, age, sex, height, tumour size, and site as risk factors associated with the survival of reconstruction material. Postoperative complications (p < 0.001) and infection (p < 0.001) were identified as risk factors. The ten-year reconstruction survival rate was significantly lower in cases with infection (22%) compared to those without infection (79%) (p < 0.001) (Figure 2b).
Fig. 2.
Kaplan-Meier analysis. a) Reconstruction material survival rate. b) Comparison of reconstruction material survival rates among patients with postoperative infection. c) Limb salvage rate. d) Comparison of limb salvage rates among patients with postoperative infection.
Limb survival
After five years, the limb survival rate was 95%, decreasing to 91% after ten years, and five of 40 cases (13%) received femoral amputation during the follow-up (Figure 2c). The median time to amputation from first surgery was 96.2 months (13.7 to 218.5). All amputations were also due to complications. Of these, four were infections and one was a post-irradiation pseudoarthrosis. All infection cases were late onset. We performed univariate analysis to identify postoperative complications, infection, age, sex, height, tumour size, and site as risk factors associated with limb survival. As a result, only infection (p < 0.001) was identified as a risk factor. The ten-year limb survival rate was significantly lower in cases with infection (75%) compared to those without (95%) (p = 0.019) (Figure 2d).
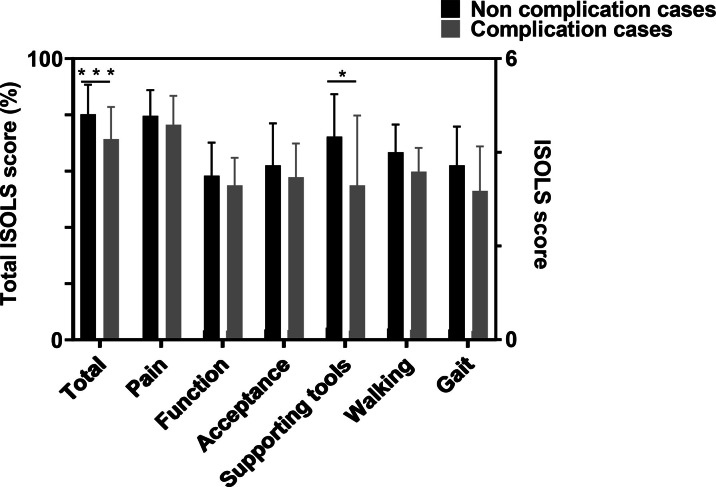
Function
The median ISOLS score at the final follow-up was 80%(47% to 97%) in 35 cases with limb salvage, which was not significantly different from the score of 70% (67% to 80%) in five cases with amputation (p = 0.310, Mann-Whitney U test). According to the results of univariate analysis, age at surgery (p = 0.135), reconstruction with artificial material (p = 0.134), complications (p = 0.023), and infection (p = 0.031) were candidate factors of low function, while multivariate analysis revealed that age at surgery (p = 0.027) and complications (p = 0.005) were independent risk factors (Table III). Infection was excluded in this multivariate analysis due to multiplicity issues. Among all six terms of the ISOLS score, the score of ‘supporting tools’ was significantly lower in cases with complications (n = 22; median 3 points) compared to those without (n = 18; median 5 points) (p = 0.027) (Figure 3). The correlation between age at surgery and the ISOLS score in each term was examined, and the ‘gait’ score was identified as being significantly lower at a younger age (R = 0.362; p = 0.033) (Supplementary Figure a).
Table III.
Univariate and multivariate analyses of factors influencing International Society of Limb Salvage scores.
| Variable | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| Coefficient of regression | 95% CI | p-value | Coefficient of regression | 95% CI | p-value | |
| Age, yrs | 1.21 | -0.40 to 2.81 | 0.135 | 1.62 | 0.19 to 3.05 | 0.027 |
| Tumour size, cm | 0.31 | -1.04 to 1.66 | 0.639 | |||
| Artificial reconstruction | 9.37 | -3.02 to 21.76 | 0.134 | 9.62 | -1.23 to 20.47 | 0.080 |
| Proximal femur | 3.65 | -4.70 to 12.00 | 0.380 | |||
| Complication | 8.82 | 1.27 to 16.24 | 0.023 | 10.43 | 3.39 to 17.47 | 0.005 |
Simple and multiple linear regression analysis using GraphPad Prism 8.
Fig. 3.
Bar graph displaying all six International Society of Limb Salvage (ISOLS) items and the total functional scores among postoperative complications. The left vertical axis represents percentages, and the right vertical axis represents scores. The median ISOLS score for complicated cases (n = 22) is indicated by black bars, and the median ISOLS score for uncomplicated cases (n = 18) is indicated by grey bars. *p < 0.05; **p < 0.01; ***p < 0.001.
Leg-lengthening procedure
Lengthening procedures for an expandable prosthesis were performed in 13 of 24 patients with an expandable endoprosthesis (including three spacers). The median patient age at the initial lengthening procedure was 13 years (IQR 11 to 14). The median number of surgeries was 3 (IQR 2 to 4) and median amount of extension per surgery was 1.4 cm (IQR 1.4 to 1.6), respectively. The complications of endoprosthesis expansion were shortening in three patients and peroneal nerve palsy in one. Among five patients, two underwent biological reconstruction, and two out of nine spacers underwent distraction osteogenesis. The median age at the initial lengthening procedure was 14 years (IQR 12 to 16). The median extension and duration of the procedure were 5.1 cm (IQR 4.8 to 5.9) and 11 months (IQR 8 to 13), respectively. Complications relating to distraction osteogenesis included infection at the pin site in one patient, which occurred five months after the procedure.
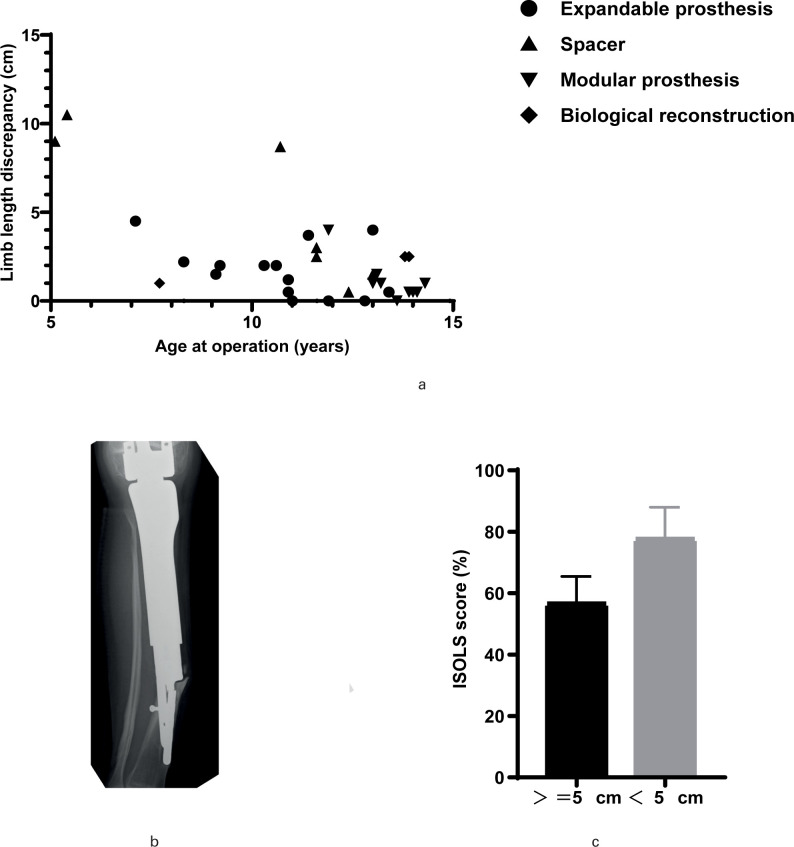
Leg-length discrepancy
The median leg-length discrepancy at the final follow-up in these 17 patients was 2.0 cm (IQR 1.2 to 3.7), with 2.1 cm (IQR 1.2 to 2.5) in endoprosthesis expansion and 3.0 cm (IQR 2.0 to 5.0) in distraction osteogenesis, respectively. In contrast, the remaining 18 patients with limb sparing who did not undergo a leg-lengthening procedure had a median age of 13 years (IQR 12 to 14) at the initial surgery and a median leg-length discrepancy of 1.0 cm (IQR 0.5 to 2.4) at the final follow-up. The leg-length discrepancy was larger in the ceramic spacer group (median 3.0 cm (IQR 2.0 to 8.9)) than in the modular prosthesis group (1.0 cm (IQR 0.5 to 1.4)) (p = 0.069). Additionally, there was a strong negative correlation between leg-length discrepancy and age at surgery (R = -0.426; p = 0.011) (Figure 4a).
Fig. 4.
a) Correlation between leg-length discrepancy and age at limb-sparing surgery. The leg-length discrepancy at the last follow-up is shown on the vertical axis, and the age at surgery is shown on the horizontal axis. b) A five-year-old boy underwent limb-sparing surgery and a two-step reconstruction from a spacer to an expandable prosthesis. Radiographs show a peri-stem fracture of the expandable prosthesis at age 15. c) Comparison of International Society of Limb Salvage (ISOLS) scores between cases with leg-length discrepancies ≥ 5 cm (n = 3) and those without (n = 32). The ISOLS score percentage is shown on the vertical axis. **p < 0.01.
Leg-length discrepancies of > 5 cm were observed in the three cases. In Case 1, the patient underwent reconstruction with a spacer at five years old, before undergoing arthroplasty with an expandable prosthesis at 12 years old. Complication surgery was performed at age 15 and 17 due to stem fracture (Figure 4b) and stem sinking, respectively, resulting in inadequate leg lengthening. At the last follow-up, the patient was aged 19 years and had a leg-length difference of 10.5 cm (Supplementary Figure ba). In Case 2, the patient underwent reconstruction with a spacer at age five years, and femur lengthening with distraction osteogenesis at aged ten years. The lengthening was interrupted at 5 cm due to chronic osteomyelitis from a pin site infection. The patient has no desire to revise to an expandable prosthesis and is currently under observation. At the last follow-up, the patient was aged 12 years and had a leg-length difference of 9.0 cm (Supplementary Figure bb). In Case 3, the patient underwent reconstruction with a spacer at aged ten years, and arthroplasty with an expandable prosthesis at aged 14 years. However, postoperative infection occurred due to skin necrosis, and extension was not possible. At the last follow-up, the patient was aged 26 years and had a leg-length difference of 8.7 cm (Supplementary Figure bc). The ISOLS scores of the three patients with leg-length discrepancies of > 5 cm were significantly lower (median 60%) than those of the 32 patients with leg-length discrepancies of < 5 cm (median 80%; p = 0.005, Mann-Whitney U test) (Figure 4c).
Discussion
In recent years, limb-sparing surgery has become the mainstay of surgery for sarcomas of the limbs; however, there is less research on the extended functional results of limb-sparing surgery for paediatric bone sarcoma, and the clinical issues are not clearly outlined.3,4,6,12-17 In this study, we investigated the postoperative complications, reconstruction and limb survival, limb function, and leg-length disparity at the last follow-up in 40 children who underwent limb-sparing surgery for bone sarcoma around the knee and were followed up for longer than five years. The results revealed that young age at surgery and postoperative infection were the most significant factors affecting reconstruction, limb survival, and postoperative limb function, while young age at surgery was the most significant factor in future leg-length discrepancies. We believe that these results highlight important considerations when selecting paediatric limb-sparing surgery.
The frequency of grade III or higher surgical complications of limb-sparing surgery for children or young adults with bone sarcoma around the knee has been reported to be very high, ranging from 42% to 90%.13,18 Futani et al16 reported the surgical outcomes of 33 patients with sarcoma who were alive at the time of analysis, with a mean age of ten years and a mean follow-up of 12.3 years (5.9 to 20).6-11 Moreover, 22 cases were reconstructed with prostheses, and 11 were biologically reconstructed. Deep infection (27%) was the most common complication in the prosthesis reconstruction cases, while implant failure (27%) and pseudoarthrosis (27%) were the most common complications in the biological reconstruction cases, followed by deep infection (18%).16 The treatment and cure rates for postoperative deep infection have been reported as 5% for debridement, 50% for one-stage revision, and 58% for two-stage revision.19,20 In this study, the frequency of grade III or higher postoperative complications was 55%, with infection being the most common in nine cases (41%), similar to the findings of previous reports. None of the cases were cured by debridement alone, instead requiring two-stage revision in four cases and amputation in four cases.
The five-year survival rates of reconstruction material for limb-sparing surgery for paediatric bone sarcoma around the knee have been reported to be 46% to 77%.15,16,21 In a systematic review, Groundland et al4 summarized the outcomes of 442 paediatric patients (mean age 11 years (5 to 17)), with bone sarcomas around the knee, treated with limb-sparing surgery. The reconstruction material survival rates were higher for the distal femur than for the proximal tibia, and were higher in the prostheses for both sites (distal femur 70.8% for prostheses and 61.3% for biological reconstruction; proximal tibia 66.6% for prostheses and 42.9% for biological reconstruction). Postoperative infection was the main reason for the failure of reconstruction material. In this study, the five-year survival rate for reconstruction material was 88%, which is better than the previously reported rate. Moreover, the rate was 66% at ten years, which further decreased with long-term follow-up. Postoperative complications, especially infection, were significant risk factors for the survival of reconstructive materials, as found in a previous report.4 Conversely, there were no significant differences in the site of origin (distal femur vs proximal tibia) or the method of reconstruction (prosthesis vs biological reconstruction), probably due to the small number of included cases.
The amputation rate after limb-sparing surgery for paediatric bone sarcomas around the knee ranged from 8% to 15%, with a higher rate reported for proximal tibiae (15.5%) than for distal femora (8.5%).4,16,22-24 Furthermore, infection (50.0% to 100%), local recurrence (33.3% to 50%), vessel occlusion (25.0%), and nonunion (25.0%) were also cited as factors in amputation. Only one complication was reported as early onset, while all other 32 complications were late onset.4,16,22-24 In this series, the amputation rate was 13%, with late infection being the most common cause, similar to the findings of previous reports. However, unlike previous reports, there was no significant difference in the amputation rate according to the tumour site.
The ISOLS score after limb-sparing surgery for paediatric bone sarcoma around the knee has been reported to range from 75.9% to 85.0%,4,12-16,18,21,23,25 but few studies have analyzed the risk factors influencing the ISOLS score. Groundland et al4 reported that the ISOLS scores were lower in distal femoral cases (prosthesis 79.1%; biological reconstruction 75.9%) than in proximal tibial cases (prosthesis 82.5%; biological reconstruction 85.0%). In our study, young age and postoperative complications were found to be risk factors for lower ISOLS scores, while there were no significant differences in tumour site or method of reconstruction.
A leg-length discrepancy of ≥ 2 cm is an indication for leg-length correction surgery because it decreases the function of the affected limb.3-5,13,16 Generally, two types of leg-length correction after the surgery for paediatric bone sarcoma of the lower limb are performed: extension of the expandable prosthesis and leg-lengthening. In the review by Groundland et al,4 the mean number of extensions and amount of lengthening of an expandable prosthesis were reported to be four times and 46.5 mm (4 to 195) for the distal femur and 5.7 times (1 to 9) and 31.3 mm (20 to 65) for the proximal tibia.1-20 Futani et al16 reported a total of 18 extensions with a mean extension of 1.5 cm (SD 0.4) per extension for the six patients who underwent extension of the expandable prosthesis, and a total of 16 operations with a mean extension of 9.3 cm (SD 7.8) per extension for the 13 patients who underwent distraction osteogenesis. In our series, the amount of extension and number of surgeries for expandable prostheses were similar to those reported previously, but the amount of elongation for leg-lengthening was less than that reported previously, perhaps due to the small number of cases and the fact that all patients had only one surgery.
Futani et al16 reported that leg-length correction improves the function of the affected limb as the leg-length difference decreases. They also reported that 15 of 19 cases (79%) who underwent leg-lengthening procedures had a residual leg-length difference of ≥ 2 cm at the final follow-up. Conversely, in a review paper limited to the prosthesis group, only 13% of cases had a leg-length difference of ≥ 2 cm at the final follow-up.4 In our series, the leg-length discrepancy at the last follow-up was also less in the prosthesis extension cases than in the leg-lengthening procedure cases. These results suggest that expandable prosthesis cases have a smaller final leg-length difference than biological reconstruction cases.
Limb-sparing surgery for very young children under five years of age has only been rarely reported. Kager et al26 summarized the clinical course of 15 cases of osteosarcoma around the knee (ten distal femur and five proximal tibia) at age ≤ five years and reported that limb-sparing surgery was performed in only two cases (13%), while the remaining 13 cases (87%) underwent amputation or rotationplasty. In this series, two five-year-old patients with osteosarcoma underwent two-staged reconstructions from a spacer to an expandable prosthesis, with leg-length discrepancies of 9.0 cm and 10.5 cm, respectively, at the final follow-up, and an ISOLS score of 60% in both cases, representing poor function. Currently, limb-sparing surgery for very young children is challenging in terms of long-term limb function.
This study has two major limitations. First, there is insufficient comparison of functional prognosis with reconstructive methods due to the small number of cases. Second, the leg-length difference may have been underestimated because two patients were aged ≤ 14 years at the last follow-up.
In conclusion, we summarize the long-term results of 40 patients who underwent limb-sparing surgery for paediatric bone sarcomas around the knee. The reconstruction material and limb had ten-year survival rates of 66% and 91%, respectively, and infection was a risk factor for both survival rates. Age and postoperative complications were the primary causes of the low function of the affected limbs.
Take home message
- In limb-sparing surgery for paediatric bone sarcomas around the knee, the ten-year survival rates of the reconstruction material and limb were 66% and 91%, respectively.
- Lower limb dysfunction was associated with younger age and postoperative complications.
- Leg length correction was insufficient, especially in very young children, resulting in decreased function of the affected limb.
Author contributions
T. Sekita: Writing – original draft, Data curation, Formal analysis, Investigation
N. Asano: Conceptualization, Data curation, Writing – original draft, Writing – review & editing, Project administration, Funding acquisition
H. Kobayashi: Conceptualization, Writing – review & editing, Investigation
T. Yonemoto: Conceptualization, Writing – review & editing, Investigation
E. Kobayashi: Conceptualization, Writing – review & editing
T. Ishii: Conceptualization, Writing – review & editing
A. Kawai: Conceptualization, Writing – review & editing
R. Nakayama: Conceptualization, Writing – review & editing, Data curation
Funding statement
The authors disclose receipt of the following financial or material support for the research, authorship, and/or publication of this article: N. Asano reports a grant from KAKENHI (21K15601) of Japan Society for the Promotion of Science for this study.
ICMJE COI statement
N. Asano reports a grant from KAKENHI (21K15601) of Japan Society for the Promotion of Science for this study.
Data sharing
The data that support the findings for this study are available to other researchers from the corresponding author upon reasonable request.
Acknowledgements
We wish to thank Ryota Ishii of the Department of Biostatistics, University of Tsukuba, for his advice on statistical analysis. And we also thank Takeshi Hirose of the Division of Musculoskeletal Oncology, National Cancer Center Hospital, and Masato Saito of the Department of Orthopedic Surgery, Keio University School of Medicine, for their cooperation in data collection.
Ethical review statement
The study was approved by the Ethical Review Committee of each institution, and information about the conduct of the study was disclosed using an opt-out procedure and the opportunity to refuse participation was guaranteed.
Open access funding
The open access fee for this article was self-funded.
Supplementary material
Figure showing the correlation of each International Society of Limb Salvage score item with age at operation, and a full-length lower limb radiograph in three cases with leg length discrepancy of more than 5 cm at last follow-up.
© 2024 Sekita et al. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/
Contributor Information
Tetsuya Sekita, Email: tetsuya5528@gmail.com.
Naofumi Asano, Email: asanonaofumi@gmail.com.
Hiroshi Kobayashi, Email: hiroshi.buster@gmail.com.
Tsukasa Yonemoto, Email: tyonemot@chiba-cc.jp.
Eisuke Kobayashi, Email: ekobayas@ncc.go.jp.
Takeshi Ishii, Email: tishii@chiba-cc.jp.
Akira Kawai, Email: akawai@ncc.go.jp.
Robert Nakayama, Email: robert.a2@keio.jp.
Data Availability
The data that support the findings for this study are available to other researchers from the corresponding author upon reasonable request.
References
- 1. Williams RF, Fernandez-Pineda I, Gosain A. Pediatric sarcomas. Surg Clin North Am. 2016;96(5):1107–1125. doi: 10.1016/j.suc.2016.05.012. [DOI] [PubMed] [Google Scholar]
- 2. Isakoff MS, Bielack SS, Meltzer P, Gorlick R. Osteosarcoma: current treatment and a collaborative pathway to success. J Clin Oncol. 2015;33(27):3029–3035. doi: 10.1200/JCO.2014.59.4895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Levin AS, Arkader A, Morris CD. Reconstruction following tumor resections in skeletally immature patients. J Am Acad Orthop Surg. 2017;25(3):204–213. doi: 10.5435/JAAOS-D-15-00619. [DOI] [PubMed] [Google Scholar]
- 4. Groundland JS, Ambler SB, Houskamp LDJ, Orriola JJ, Binitie OT, Letson GD. Surgical and functional outcomes after limb-preservation surgery for tumor in pediatric patients: a systematic review. JBJS Rev. 2016;4(2):e2. doi: 10.2106/JBJS.RVW.O.00013. [DOI] [PubMed] [Google Scholar]
- 5. Yao W, Cai Q, Wang J, Gao S. Treatment of osteosarcoma around the knee in skeletally immature patients. Oncol Lett. 2017;14(5):5241–5248. doi: 10.3892/ol.2017.6903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Grimer RJ, Aydin BK, Wafa H, et al. Very long-term outcomes after endoprosthetic replacement for malignant tumours of bone. Bone Joint J. 2016;98-B(6):857–864. doi: 10.1302/0301-620X.98B6.37417. [DOI] [PubMed] [Google Scholar]
- 7. Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17(6):1471–1474. doi: 10.1245/s10434-010-0985-4. [DOI] [PubMed] [Google Scholar]
- 8. Iwamoto Y, Tanaka K. The activity of the Bone and Soft Tissue Tumor Study Group of the Japan Clinical Oncology Group. Jpn J Clin Oncol. 2012;42(6):467–470. doi: 10.1093/jjco/hys059. [DOI] [PubMed] [Google Scholar]
- 9. Iwamoto Y, Tanaka K, Isu K, et al. Multiinstitutional phase II study of neoadjuvant chemotherapy for osteosarcoma (NECO study) in Japan: NECO-93J and NECO-95J. J Orthop Sci. 2009;14(4):397–404. doi: 10.1007/s00776-009-1347-6. [DOI] [PubMed] [Google Scholar]
- 10. Ferrari S, Ruggieri P, Cefalo G, et al. Neoadjuvant chemotherapy with methotrexate, cisplatin, and doxorubicin with or without ifosfamide in nonmetastatic osteosarcoma of the extremity: an Italian sarcoma group trial ISG/OS-1. J Clin Oncol. 2012;30(17):2112–2118. doi: 10.1200/JCO.2011.38.4420. [DOI] [PubMed] [Google Scholar]
- 11. Katayama H, Kurokawa Y, Nakamura K, et al. Extended clavien-dindo classification of surgical complications: Japan clinical oncology group postoperative complications criteria. Surg Today. 2016;46(6):668–685. doi: 10.1007/s00595-015-1236-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Albergo JI, Gaston CL, Aponte-Tinao LA, et al. Proximal tibia reconstruction after bone tumor resection: are survivorship and outcomes of endoprosthetic replacement and osteoarticular allograft similar? Clin Orthop Relat Res. 2017;475(3):676–682. doi: 10.1007/s11999-016-4843-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Henderson ER, Pepper AM, Marulanda G, Binitie OT, Cheong D, Letson GD. Outcome of lower-limb preservation with an expandable endoprosthesis after bone tumor resection in children. J Bone Joint Surg Am. 2012;94-A(6):537–547. doi: 10.2106/JBJS.I.01575. [DOI] [PubMed] [Google Scholar]
- 14. Ness KK, Neel MD, Kaste SC, et al. A comparison of function after limb salvage with non-invasive expandable or modular prostheses in children. Eur J Cancer. 2014;50(18):3212–3220. doi: 10.1016/j.ejca.2014.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Tan PX, Yong BC, Wang J, et al. Analysis of the efficacy and prognosis of limb-salvage surgery for osteosarcoma around the knee. Eur J Surg Oncol. 2012;38(12):1171–1177. doi: 10.1016/j.ejso.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 16. Futani H, Minamizaki T, Nishimoto Y, Abe S, Yabe H, Ueda T. Long-term follow-up after limb salvage in skeletally immature children with a primary malignant tumor of the distal end of the femur. J Bone Joint Surg Am. 2006;88-A(3):595–603. doi: 10.2106/JBJS.C.01686. [DOI] [PubMed] [Google Scholar]
- 17. Schiller C, Windhager R, Fellinger EJ, Salzer-Kuntschik M, Kaider A, Kotz R. Extendable tumour endoprostheses for the leg in children. J Bone Joint Surg Br. 1995;77-B(4):608–614. [PubMed] [Google Scholar]
- 18. Staals EL, Colangeli M, Ali N, Casanova JM, Donati DM, Manfrini M. Are complications associated with the Repiphysis(®) expandable distal femoral prosthesis acceptable for its continued use? Clin Orthop Relat Res. 2015;473(9):3003–3013. doi: 10.1007/s11999-015-4355-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Morii T, Morioka H, Ueda T, et al. Deep infection in tumor endoprosthesis around the knee: a multi-institutional study by the Japanese musculoskeletal oncology group. BMC Musculoskelet Disord. 2013;14:51. doi: 10.1186/1471-2474-14-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hardes J, Gebert C, Schwappach A, et al. Characteristics and outcome of infections associated with tumor endoprostheses. Arch Orthop Trauma Surg. 2006;126(5):289–296. doi: 10.1007/s00402-005-0009-1. [DOI] [PubMed] [Google Scholar]
- 21. Wilkins RM, Miller CM. Reoperation after limb preservation surgery for sarcomas of the knee in children. Clin Orthop Relat Res. 2003;(412):153–161. doi: 10.1097/01.blo.0000072466.53786.83. [DOI] [PubMed] [Google Scholar]
- 22. Donati D, Giacomini S, Gozzi E, et al. Knee arthrodesis with a temporary spacer performed in malignant tumor around the knee. Arch Orthop Trauma Surg. 2002;122(2):123–128. doi: 10.1007/s004020100327. [DOI] [PubMed] [Google Scholar]
- 23. Schindler OS, Cannon SR, Briggs TW, Blunn GW. Stanmore custom-made extendible distal femoral replacements. Clinical experience in children with primary malignant bone tumours. J Bone Joint Surg Br. 1997;79-B(6):927–937. doi: 10.1302/0301-620x.79b6.7164. [DOI] [PubMed] [Google Scholar]
- 24. Alman BA, De Bari A, Krajbich JI. Massive allografts in the treatment of osteosarcoma and Ewing sarcoma in children and adolescents. J Bone Joint Surg Am. 1995;77-A(1):54–64. doi: 10.2106/00004623-199501000-00008. [DOI] [PubMed] [Google Scholar]
- 25. Kang S, Lee JS, Park J, Park S-S. Staged lengthening and reconstruction for children with a leg-length discrepancy after excision of an osteosarcoma around the knee. Bone Joint J. 2017;99-B(3):401–408. doi: 10.1302/0301-620X.99B3.38018. [DOI] [PubMed] [Google Scholar]
- 26. Kager L, Zoubek A, Dominkus M, et al. Osteosarcoma in very young children: experience of the Cooperative Osteosarcoma Study Group. Cancer. 2010;116(22):5316–5324. doi: 10.1002/cncr.25287. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings for this study are available to other researchers from the corresponding author upon reasonable request.