Abstract
Objectives:
This study aimed to map the incidence of acute respiratory infections (ARIs) among under-5 children in Indonesia, address the triple burden of malnutrition, and analyze the impact of malnutrition on ARIs, taking into account the environmental and wealth disparities in Indonesia.
Methods:
This study utilized an ecological design, analyzing aggregate data from the Indonesia Nutrition Survey, 2022. It encompassed 33 provinces and 486 districts/cities, involving a total of 334 878 children under 5 years of age. Partial least squares structural equation modeling was employed to investigate the relationships among wealth, environment, malnutrition (stunting, wasting, and underweight), and ARIs.
Results:
The proportion of ARI cases in Indonesia was generally concentrated in central Sumatra, the western and eastern parts of Java, and eastern Papua. In contrast, the northern part of Sumatra, central Kalimantan, central Sulawesi, and central Papua had a higher proportion of malnutrition cases compared to other regions. Negative associations were found between malnutrition and ARIs (path coefficient =-0.072; p<0.01) and between wealth and environment (path coefficient =-0.633; p<0.001), malnutrition (path coefficient=-0.399; p<0.001), and ARIs (path coefficient=-0.918; p<0.001).
Conclusions:
An increasing wealth index is expected to contribute to reducing ARIs, malnutrition and environmental burdens in the future. This study emphasizes the necessity for focused strategies that address both immediate health challenges and the underlying socioeconomic determinants to improve child health outcomes in the Indonesian context.
Keywords: Respiratory tract infections, Socioeconomic disparities in health, Malnutrition, Child, Indonesia
GRAPHICAL ABSTRACT
INTRODUCTION
Acute respiratory infections (ARIs) continue to pose significant public health challenges worldwide, affecting both the upper respiratory tract (nose, vocal cords, and ears) and the lower respiratory tract (trachea, bronchi, bronchioles, and alveoli). Common symptoms of ARIs include the common cold and influenza [1]. The World Health Organization (WHO) reports that ARIs are responsible for approximately 20% of all deaths in children under 5 years old. These infections account for 3.5% of the global disease burden and are responsible for 30% to 50% of pediatric outpatient visits and over 30% of pediatric hospital admissions in developing countries [2,3]. ARIs are a significant contributor to child mortality rates, which range from 19% to 21% in regions such as Southeast Asia, the Eastern Mediterranean, and Africa [4]. In Indonesia, the most recent data from the Indonesia Health Survey, conducted by the Indonesia Ministry of Health, shows an ARI incidence rate of 4.8% in 2023 [5]. Notably, the geographical distribution of ARI incidence varies significantly, with the highest rates reported in the provinces of Papua Tengah (11.8%), Papua Pegunungan (10.7%), Jawa Timur (8.8%), Banten (8.1%), and Papua (8.1%) [5].
Studies have reported that poverty [6], inadequate hygiene practices, and the use of unclean cooking fuels [7] are associated with higher morbidity from ARIs among children under 5 years old in developing countries. Additionally, ARIs in these countries are linked to malnutrition [8]. A study in Zambia demonstrated that malnourished children face a 1.5 times greater risk of acquiring ARIs compared to those with normal nutritional profiles [8]. Poor environmental conditions and nutritional status further exacerbate the incidence of ARIs.
Numerous studies have explored the links between malnutrition, compromised cell-mediated immunity, and the heightened incidence and mortality of gastrointestinal or respiratory infections in children under 5 years of age [9]. However, to our knowledge, there is a lack of comprehensive studies that use community-based secondary data to examine the relationship between the burden of ARIs and malnutrition in Indonesia, underscoring a significant gap in knowledge. The substantial incidence of ARIs within the Indonesian healthcare system, along with persistent malnutrition rates that exceed national targets, highlights the urgent need for comprehensive intervention measures [10]. Indonesia’s diverse geographic, socioeconomic, and environmental landscapes can worsen both malnutrition and ARIs incidence. Consequently, this study aims to map the incidence of ARIs, assess the burden of malnutrition, and analyze the reciprocal impact of malnutrition on ARIs, taking into account Indonesia’s environmental and wealth disparities.
METHODS
Study Design and Setting
This study utilized an ecological design, analyzing aggregate data from the 2022 Indonesia Nutrition Survey. Conducted nationally, the survey adopted a cross-sectional methodology with a 2-stage stratified cluster sampling process [11]. Briefly, it aimed to investigate infant nutrition, with a particular focus on specific and sensitive nutritional intervention approaches to map further policies needed for malnutrition issues in Indonesia. Trained enumerators, such as midwives, nurses, nutritionists, and public health professionals, directly measured anthropometric parameters. These measurements included the weight, length, or height of infants, and the upper arm circumference of adolescent girls, women of reproductive age, and pregnant women, using standardized equipment during interviews [11].
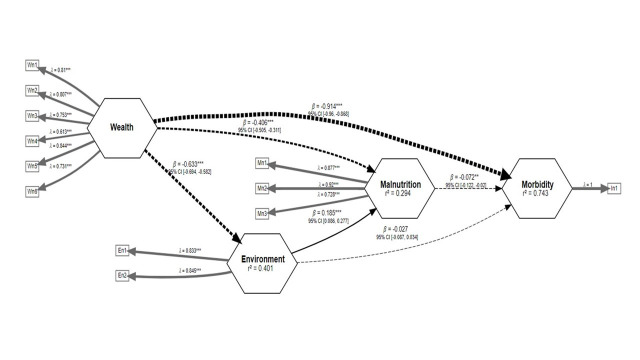
This study mapped the geographical distribution of the triple burden of malnutrition at the district/city level. Indonesia is administratively divided into 2 levels of local government, comprising 38 provinces and 514 districts/cities as of 2024 (Supplemental Material 1). Given the significant socioeconomic variations among districts/cities in Indonesia [12], this study further explores how the proportion of environmental conditions and welfare at the district/city level influences malnutrition and morbidity due to ARIs in children. The initial dataset, obtained from the Ministry of Health, Indonesia, included 33 provinces and 486 districts/cities, participating in a nutrition survey conducted from September 2022 to November 2022 (Figure 1). The survey covered a total of 334 878 children under 5 years of age. Only healthy children were included in the anthropometric measurement process (n=308 472, 92.1%). The Indonesia Nutrition Status Survey did not collect data in the province of Nusa Tenggara Timur, which includes 22 districts/cities, and instead, data from the Central Bureau of Statistics were used to estimate the nutritional status of infants in these areas. Additionally, data collection was not conducted in 6 districts of Papua due to security concerns. Districts/cities where data collection was not feasible were excluded from the final analysis of this study.
Figure. 1.
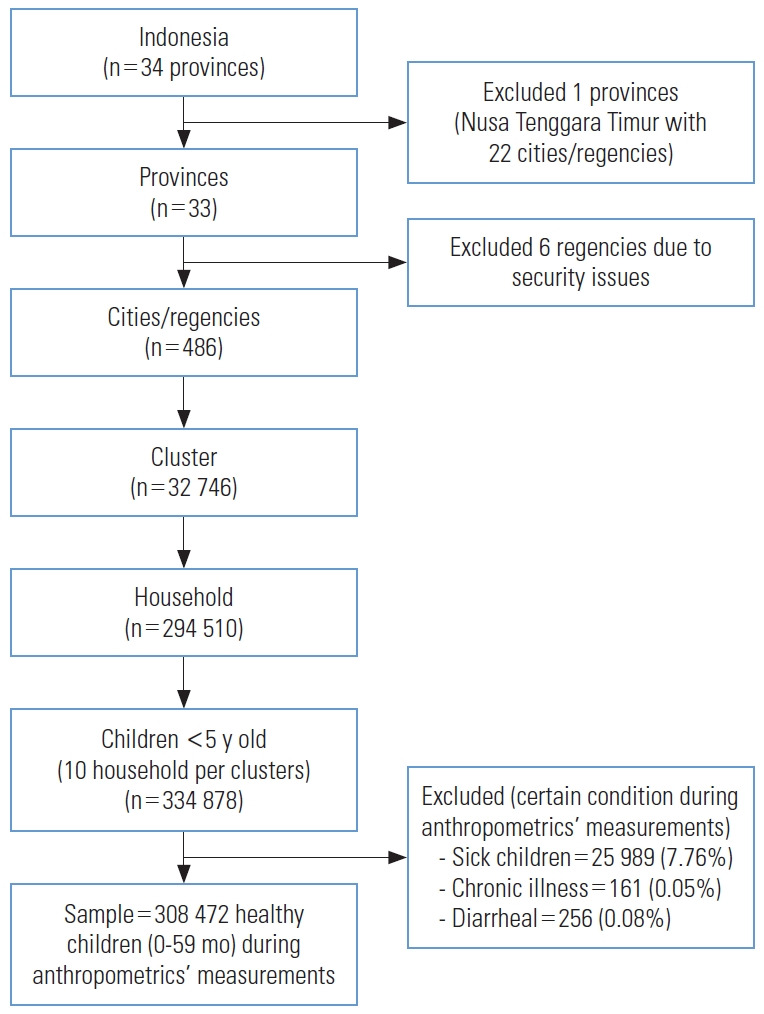
Flow chart for data selection.
Data Procedures and Variables
The data of the nutrition survey were collected through face-to-face interviews with parents or caregivers, along with anthropometric measurements taken at the individual level. These data were then aggregated at the district/city level for analysis in this study. The primary outcome variable of interest is the history of morbidity due to ARIs, characterized by symptoms such as fever, cough lasting less than 2 weeks, runny nose, and/or sore throat, all diagnosed by a medical doctor within the month preceding the survey visit. The anthropometric indicators used to assess a child’s nutritional status included Z-scores for height-for-age (HA), weight-for-height (WH), and weight-for-age (WA). These scores are calculated based on the child’s age, height, and weight, and they are commonly employed to evaluate a child’s nutritional status [13]. This study also incorporated household environmental variables, such as residual fuel cooking (kerosene, charcoal, or firewood) at home and shared latrine usage. Additionally, the study examined ownership of household items including washing machines (yes/no), smartphones (yes/no), computers/personal computers (yes/no), motorcycles (yes/no), cars, and televisions (LCD/LED) of at least 32 inches (yes/no).
Statistical Analysis
Calculation of nutritional status indicators
Malnutrition encompasses stunting, being underweight, and wasting. This study calculated the height-for-age Z score (HAZ), weight-for-height Z score (WHZ), and weight-for-age Z score (WAZ) [13]. Stunting, wasting, and being underweight are defined by a Z score of less than -2 standard deviations [13]. Additionally, this study employed the composite index of anthropometric failure to map the triple burden of malnutrition among children under 5 years old. The nutritional status calculations were performed using the “anthro” package in R version 4.3.1 (R Foundation for Statistical Computing, Vienna, Austria), developed by the WHO [14].
Descriptive statistics
This study compiled data on wealth, environment, malnutrition, and ARIs from 486 city and regency levels. Additionally, it mapped malnutrition and ARIs using digital administrative maps obtained from the Ministry of Health, Indonesia. The natural Jenks breaks optimization method was employed to investigate the spatiotemporal patterns of these conditions [15].
PLS-SEM models
The study aimed to examine the relationship between the environment, wealth, malnutrition (stunting, wasting, and underweight), and morbidity due to ARIs. In this study, morbidity is considered a latent variable, with malnutrition also treated as a latent variable and suspected to act as a moderator for observed variables or risk factors, such as environment and wealth. To explore these relationships, given the non-normally distributed data, the study utilizes partial least squares structural equation modeling (PLS-SEM) analysis [16]. This analysis included 2 approaches: the association between latent variables (inner model) and the association between indicators within latent variables (outer model). Each latent variable, except for morbidity, comprises environment (2 items), wealth (6 items), and malnutrition (3 items) (Supplemental Material 2). The PLS-SEM models tested include one with a direct correlation between environment and wealth with morbidity (model 1) and another where the correlation between environment and wealth is mediated by malnutrition (model 2). The adequacy of model fit for both the outer and inner models is subsequently evaluated.
The evaluation of the outer models included examining internal consistency reliability, reflective indicator loading, and convergent validity [16]. Tests for internal consistency reliability using Cronbach’s alpha, rhoA, and rhoC indicated sufficient reliability for all variables, with scores exceeding 0.7 [9]. The collinearity statistics test results showed a variance inflation factor (VIF) value of less than 5, indicating no multicollinearity [9]. Additionally, the average variance extracted (AVE) values for all variables exceeded the threshold of 0.5 [9]. The assessment of the inner model involved examining the latent variable with the coefficient of determination (R2). A model is considered to demonstrate goodness-of-fit when R2>0 and a Q2 exceeds 0.35 [17]. Spearman’s rank-order cross-correlation coefficient (ρ) was estimated to investigate the relationship between variables incorporated within the model. If the variables were found to be highly correlated (|ρ|>0.8), we selected the variable with the strongest statistical correlation with the dependent variable and discarded the other variables [18]. This study employed bootstrapping procedures for the measurement models and the structural model. These procedures were used to calculate the standard errors of coefficients, facilitating the assessment of their statistical significance without relying on distribution assumptions [16]. This analysis was conducted using the “seminr” package in R version 4.3.1 (R Foundation for Statistical Computing).
Ethics Statement
This study analyzed data authorized for use by the Ministry of Health, Indonesia. The epidemiological data employed in this investigation had been anonymized beforehand to ensure complete confidentiality. Since the analysis involved publicly accessible data without any identifying details, ethical clearance was not required. The study was conducted in accordance with the principles set forth in the 2013 revision of the Declaration of Helsinki.
RESULTS
Descriptive Statistics
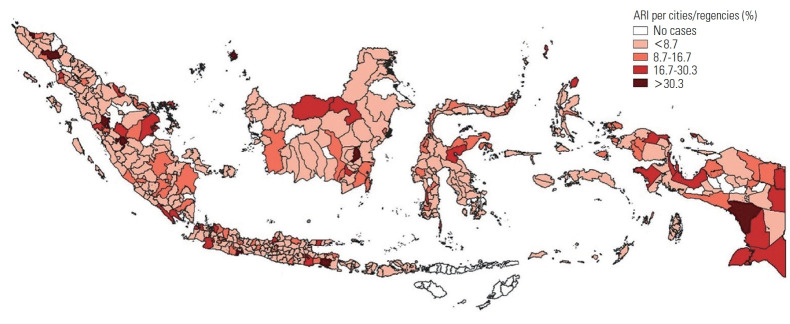
A total of 94.6% (486/514) of the cities/districts included in this study, encompassing 92.1% (308 472/334 878) of children under 5 years of age, served as the basis for unit-level analysis. The majority of cities/districts in Indonesia reported cases of children diagnosed with ARIs by healthcare professionals. Almost all major islands in Indonesia reported ARIs among children, with approximately one-third of children in these cities/districts having been diagnosed with the condition. ARIs tended to be concentrated in central Sumatra, the western and eastern parts of Java, and eastern Papua (Figure 2). The highest incidence of ARIs was reported in Tabalong (52.3%) in the Province of South Kalimantan, Asmat (49.6%) and Deiyai (42.5%) in the Province of Papua, Pidie Jaya (40.2%) in the Province of Aceh, and Natuna (37.9%) in the Province of Riau Islands. As depicted in Supplemental Material 3, regions such as the northern part of Sumatra (Subulussalam [40.5%]), central Kalimantan (Murung Raya [37.6%]), and central Papua (Asmat [51.7%], Yahukimo [50.7%], and Tolikara [47.2%]) exhibited a high incidence of malnutrition cases compared to other areas. Generally, Java showed a lower incidence of malnutrition issues than other islands. Specific regions within Indonesia exhibited significant rates of malnutrition, indicating the incidence of malnutrition problems (stunting, wasting, underweight) in several cities/districts in northern Sumatra, central Kalimantan, Sulawesi, and Papua (Table 1). Conversely, areas close to Java, such as the southern part of Sumatra and Bali, tended not to exhibit significant rates of malnutrition issues.
Figure. 2.
Geographical distribution of acute respiratory infections (ARIs) among children under 5 years old in Indonesia at the city/regency level. Darker shades of orange signify a higher proportion of ARIs in these areas.
Table 1.
Descriptive statistics of wealth, environment, malnutrition and morbidity per region
| Parameters | Region (%)1 |
||||||
|---|---|---|---|---|---|---|---|
| Sumatera (n = 154) | Java (n = 119) | Bali and Nusa Tenggara (n = 19) | Kalimantan (n = 56) | Sulawesi (n = 81) | Maluku (n = 21) | Papua (n = 37) | |
| Wealth | |||||||
| Having a washing machine | 60.3 | 58.4 | 44.7 | 62.0 | 51.8 | 41.9 | 32.4 |
| Having a handphone/smartphone | 91.1 | 92.6 | 91.0 | 93.0 | 89.4 | 81.3 | 66.0 |
| Having a computer/personal computer | 21.3 | 27.0 | 23.0 | 23.0 | 20.3 | 18.2 | 17.8 |
| Having a motorcycle | 93.5 | 94.0 | 91.8 | 93.6 | 86.4 | 66.2 | 52.4 |
| Having a car | 16.9 | 20.1 | 20.1 | 16.4 | 14.3 | 5.1 | 6.3 |
| Having a television (LCD/LED), at least 32 inchs | 39.4 | 37.1 | 34.8 | 40.3 | 32.5 | 31.1 | 26.9 |
| Environment | |||||||
| Residual fuel cooking | 5.6 | 3.8 | 7.0 | 3.4 | 19.8 | 98.4 | 96.7 |
| Shared latrine | 7.4 | 6.7 | 10.3 | 7.7 | 12.1 | 13.3 | 23.5 |
| Malnutrition | |||||||
| Stunting | 18.4 | 16.4 | 17.3 | 21.9 | 23.0 | 23.3 | 29.4 |
| Underweight | 14.1 | 13.4 | 14.4 | 18.2 | 18.1 | 21.1 | 18.6 |
| Wasted | 6.9 | 6.9 | 6.2 | 8.8 | 8.3 | 11.0 | 10.2 |
| Morbidity | |||||||
| Acute respiratory infection | 5.5 | 6.4 | 2.6 | 5.6 | 4.6 | 5.1 | 12.9 |
The percentages indicate the averages of proportion in the regions among cities/regencies’ level.
Model Fit Evaluation
This study compared 2 models: model 1, which posited a direct correlation between environment and wealth, and model 2, which assumed no such direct correlation, in relation to morbidity. The evaluation outcomes for the outer models revealed no issues with collinearity and confirm the validity of all indicators (Table 2). Additionally, Table 2 shows consistent results from the model evaluation, as demonstrated by Cronbach’s alpha, composite reliability, and AVE, all of which met established testing standards and indicated that the exogenous variable moderately explained the endogenous variables. Spearman’s rank-order cross-correlation analysis was used to investigate the relationships between variables incorporated within the model (Supplemental Material 4). It is important to note that no strong correlations were observed between the variables. The R2 value of 0.756 and Q2 value of 0.827, obtained from the inner models, suggested strong applicability of the endogenous latent variables for model specifications and estimations. The analysis of both inner and outer measurements suggested that the model effectively captured the relationship between exogenous and endogenous constructs.
Table 2.
Model fit evaluation of PLS-SEM analysis
| Latent | Wealth | Environment | Malnutrition | ARIs |
|---|---|---|---|---|
| Cronbach’s alpha | 0.854 | 0.579 | 0.811 | 1.000 |
| rhoA | 0.893 | 0.826 | 0.882 | 1.000 |
| rhoC | 0.863 | 0.580 | 0.889 | 1.000 |
| Average variance extracted | 0.583 | 0.704 | 0.715 | 1.000 |
| R 2 | N/A | 0.401 | 0.294 | 0.743 |
PLS-SEM, partial least squares structural equation modeling; ARIs, acute respiratory infections; N/A, not available.
Structural Model Evaluation
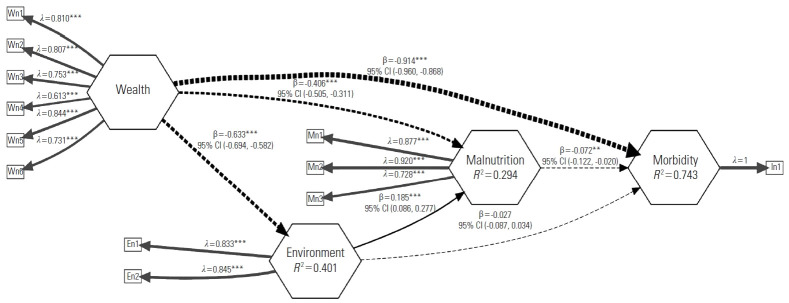
To assess the structural associations among environment, wealth, malnutrition, and morbidity due to ARIs, this study employed the partial least squares bootstrap method with 1000 re-samplings to ascertain statistical significance without relying on distribution assumptions (Supplemental Material 5). The results indicated a negative impact of malnutrition on morbidity due to ARIs (path coefficient=-0.072; p<0.01) (Figure 3). Generally, there is a negative association between wealth and environment (path coefficient=-0.633; p<0.001), malnutrition (path coefficient=-0.406; p<0.001), and ARIs (path coefficient=-0.914; p<0.001). This suggests that wealth, as indicated by ownership of appliances such as washing machines, cell phones, computers, motorcycles, cars, and televisions, explains 63.3%, 40.6%, and 91.4% of the variance in environment, malnutrition, and morbidity due to ARIs, respectively. Given the consistent path coefficient values for wealth with malnutrition and morbidity due to ARIs, malnutrition serves as a complementary mediator to wealth and morbidity due to ARIs. Conversely, the association between environment, malnutrition, and morbidity due to ARIs shows that the environment is positively associated with malnutrition (path coefficient=0.185; p<0.001) but does not directly associate with morbidity due to ARIs (path coefficient=-0.027; p<0.01). Thus, malnutrition acts as an indirect-only mediator between environmental factors and ARIs based on these findings. We excluded environment parameters in the structural model as crude path coefficients and compared the model with and without environment adjustments to perform sensitivity analysis. The sensitivity analysis results revealed a consistent association between wealth, malnutrition, and ARIs (Supplemental Material 6).
Figure. 3.
Structural equation model of the interplay among environment, wealth, malnutrition, and morbidity. Rectangles represent indicators and parameters, while hexagons represent latent constructs. Straight arrows denote positive correlations, while dotted arrows represent negative correlations between the variables. Lambda (λ) and Beta (β) signify outer loading scores and path coefficients respectively. The 95% confidence interval (CI) is included for path coefficients. **p<0.01, ***p<0.001.
DISCUSSION
Overall, this nationwide study in Indonesia reveals that the incidence of ARIs was widespread across the country, with the highest rates observed in Papua compared to other regions. Similarly, the prevalence of malnutrition was more pronounced in the eastern regions of Indonesia, including Kalimantan, Sulawesi, Maluku, and Papua. These issues were further exacerbated by socioeconomic and environmental factors, which tend to increase the risk of both malnutrition and ARIs. Notably, the data indicate a negative association between wealth and both malnutrition and ARIs, suggesting that an increase in the wealth index could help reduce the burden of ARIs, malnutrition, and environmental challenges in the future.
This study highlights the correlation between lower wealth levels and a higher incidence of malnutrition and ARIs within a specific geographical area. Additional research supports the notion that wealth levels significantly influence environmental hygiene, as well as the rates of malnutrition and ARIs [19]. Studies conducted in Cambodia and Bangladesh indicate that increased wealth levels reduce the risk of ARI infections among infants under 5 years old [20,21]. Higher family income is linked to better living conditions, enhanced nutrition, and greater access to healthcare, all of which positively affect children’s health. Financial strain on parents is associated with negative impacts on children’s health, including undernutrition, impaired cognitive development, and weakened immune systems, which increase their vulnerability to diseases [21]. Children from financially stable families are more likely to enjoy secure housing and access to health-promoting environments compared to their counterparts from impoverished backgrounds [21].
This study reveals that malnutrition serves as a mediating factor in the relationship between wealth and ARIs. The likelihood of malnutrition varies by household wealth across developing countries, with economic globalization playing a complex role that may reduce wealth disparities but exacerbate malnutrition among the poorest populations [22,23]. These wealth disparities intensify the significant equity challenges in health, while geographical barriers pose undeniable challenges in Indonesia due to its diverse topographical landscape. The wealth inequity in Indonesia is significantly influenced by geographical challenges in certain areas, including islands, mountainous regions, and areas prone to disasters, which hinder efforts to reduce disparities. Provinces in eastern Indonesia, which are geographically mountainous and remote, have less frequent engagement in maternal and child health services at healthcare facilities compared to those in western Indonesia [24]. This disparity is due to several factors, including a shortage of midwives and medical doctors, a scarcity of healthcare facilities, extended travel times, and high costs associated with accessing healthcare [24,25]. These conditions lead to delayed diagnoses and increased severity of conditions upon arrival at healthcare services. Additionally, social globalization increases the likelihood of malnutrition across all wealth strata, particularly affecting affluent households in lower-income developing countries [23]. Inadequate nutrition was closely associated with additional risk factors for respiratory illness stemming from poverty. Notably, food insecurity may escalate the risk of morbidity due to inadequate nutrient intake, as various nutrients crucially support immune function [26]. Furthermore, underprivileged children often live in overcrowded, damp dwellings, are less likely to receive vaccinations, and are more susceptible to infections that compromise the respiratory system during early childhood [27]. Reduced household income decreases purchasing power, limits food availability, and lowers household food security. This directly affects food consumption and nutrient intake among household members to varying degrees [28].
Our results indicated that ARIs are more prevalent in the Java Island region, particularly in the western and eastern parts of Java, as well as in eastern Papua. Additionally, the burden of malnutrition has been observed beyond Java Island. This study also highlights that malnutrition and ARIs together contribute approximately 7% to the path coefficients. The study found that the western part of Indonesia, specifically the Sumatera and Java regions, is more developed in terms of wealth and environmental issues. This finding is supported by the assumption that Java Island is the center of development and economic activity, whereas regions outside Java, especially in eastern Indonesia, tend to experience less development and economic growth [29]. Epidemiological modeling in Jakarta, Indonesia, has reported that an ARIs outbreak in this area could lead to subsequent outbreaks in surrounding regions [30]. Despite limited information on household transmission in areas of high population density and cross-region transmission in Jakarta, Indonesia’s high population density and connectivity to other regions [31] may accelerate the transmission and spread of ARIs across the country.
The Indonesian Ministry of Health has reported that socioeconomic development in eastern Indonesia tends to be lower compared to western Indonesia [32]. This study shows a higher prevalence of households in eastern Indonesia using residual fuels for cooking, which is linked to increased rates of malnutrition and ARIs. The choice to use residual fuels like firewood is influenced by its plentiful availability and the limited financial capacity of the local population, further compounded by the high costs of cleaner fuel alternatives. Despite the Indonesian government’s successful introduction of policies in 2007 to replace kerosene and firewood with liquid petroleum gas (LPG) [33], implementing these policies has been challenging in eastern Indonesia. The region’s mountainous terrain and limited land transportation access have hindered these efforts. Therefore, eastern Indonesia is likely to face complex health issues, including low immunization coverage, poor sanitation, and malnutrition [34]. Similar research conducted in Ghana and Nigeria has found that less developed areas have a higher incidence of ARIs among children under 5 years old [35,36]. The disparity in socioeconomic status in these regions affects both the understanding and awareness of ARI symptoms.
The Indonesian Government has implemented various initiatives to prevent malnutrition, focusing particularly on improving wealth. Numerous studies in Indonesia have documented the effectiveness of wealth enhancement programs that include cash transfers [37,38]. These programs aim to enable the purchase of nutritious food for children under 5 years old and pregnant mothers. They also provide health and nutrition education, and encourage the use of healthcare services [37,38]. Similar research in India indicates that income gains from cash transfers improve the nutritional status of children under 5 years old and strengthen family resilience against food security challenges. This improvement is achieved by increasing maternal awareness about choosing nutrient-rich foods, reallocating household spending towards food, and improving access to healthcare services [37,39]. Although conditional cash transfers may not significantly increase long-term wealth levels in Indonesia, they do make a substantial contribution to family investments in the long-term health and education of children [38]. Additionally, the initiative to switch from residual fuel cooking to cleaner alternatives like gas/LPG could be reconsidered, especially in eastern Indonesia. Currently, there is no empirical evidence to assess the effectiveness of this program in reducing the incidence of ARIs. However, there has been a national decline in ARIs among children under 5 years old, from 11.2% in 2007 to 5.1% in 2013 [40]. Although it is challenging to directly quantify the impact of this program on ARIs, the social and health benefits of transitioning to clean cooking fuels could help address health challenges in eastern Indonesia, including reducing the prevalence of malnutrition and ARIs [33,40].
While this study utilized a large sample size and considered the incidence of the triple burden of malnutrition at the city and regency levels, it faced several limitations. First, the ecological study design relied on cross-sectional secondary data, which may restrict the ability to infer causality over time. Nevertheless, ecological studies are beneficial as they allow for efficient use of existing population data, facilitating the assessment of correlations between potential risk factors and various disease outcomes in settings constrained by limited local resources and time. The validity of this study should be further evaluated using different study designs, such as cohort studies. Second, the definition of ARI cases was based on reports from parents, mothers, or caregivers about experiences in the month preceding the study home visit, as documented by medical professionals. This approach may lead to an underestimation of the actual incidence of ARIs in the community. Third, the use of an PLS-SEM model to explore potential causal pathways affecting the incidence of ARIs and malnutrition represents a novel approach. Although structural path models have advantages over multivariable fixed effects models by accommodating complex interactions between variables, it is important to recognize that the theoretical model was developed iteratively based on prior theory and may not fully capture all pathways influencing ARIs and malnutrition. Fourth, certain regions identified as having limited resources, such as restricted access to healthcare, prevalent malnutrition, and inadequate drinking water and sanitation, were excluded from this study due to data unavailability and security concerns. This exclusion could affect the impartiality of the research findings [40]. Despite these limitations, this study provides valuable insights into the relationship between wealth, malnutrition, and the incidence of ARIs. It also highlights the importance of enhancing wealth strategies to combat malnutrition and infectious diseases in children under 5 years of age. This could be particularly effective through non-cash transfer mechanisms targeting specific areas of malnutrition and ARIs, such as food cash assistance, health and nutrition education, government reinforcement, and multisectoral approaches.
In conclusion, our study offers comprehensive insights into the epidemiology of ARIs and malnutrition among children in Indonesia, highlighting significant disparities related to regional environments and wealth. By employing robust statistical methods, we revealed structural associations between the environment, wealth, malnutrition, and morbidity, thereby illuminating the complex interactions among these factors. These findings emphasize the critical need for targeted interventions that address both immediate health concerns and the underlying socioeconomic determinants to enhance child health outcomes in Indonesia.
Acknowledgements
We thank the Ministry of Health, the Republic of Indonesia for providing the linked data.
Footnotes
Data Availability
Anonymized datasets generated during the study are available on request from the corresponding author.
Conflict of Interest
The authors have no conflicts of interest associated with the material presented in this paper.
Funding
None.
Author Contributions
Conceptualization: Purnama TB, Wagatsuma K, Saito R. Data curation: Purnama TB. Formal analysis: Purnama TB, Wagatsuma K. Funding acquisition: None. Methodology: Purnama TB, Wagatsuma K, Saito R. Project administration: Purnama TB. Visualization: Purnama TB, Wagatsuma K. Writing – original draft: Purnama TB, Wagatsuma K, Saito R. Writing – review & editing: Purnama TB, Wagatsuma K, Pane M, Saito R.
Supplemental Materials
Supplemental materials are available at https://doi.org/10.3961/jpmph.24.246.
The Provincial of Bali, Nusa Tenggara Barat and Nusa Tenggara Timur is grouped in the Bali and Nusa Tenggara (light green). The Provincial of Maluku and Maluku Utara included in Maluku region (brown). The Provincial of Bangka Belitung and Kepulauan Riau is included in Sumatera (blue)
Notes: Darker shades of orange indicate a higher proportion of underweight (A), wasted (B), stunting (C), and the triple burden of malnutrition problems (D) at the city/regency level.
REFERENCES
- 1.Selvaraj K, Chinnakali P, Majumdar A, Krishnan IS. Acute respiratory infections among under-5 children in India: a situational analysis. J Nat Sci Biol Med. 2014;5(1):15–20. doi: 10.4103/0976-9668.127275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization. Child mortality (under 5 years); 2022 [cited 2024 Mar 29]. Available from: https://www.who.int/news-room/fact-sheets/detail/levels-and-trends-in-child-under-5-mortality-in-2020.
- 3. World Health Organization. Children aged <5 years with acute respiratory infection (ARI) symptoms taken to facility (%); 2023 [cited 2024 Mar 29]. Available from: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/3147.
- 4.Alemayehu S, Kidanu K, Kahsay T, Kassa M. Risk factors of acute respiratory infections among under five children attending public hospitals in southern Tigray, Ethiopia, 2016/2017. BMC Pediatr. 2019;19(1):380. doi: 10.1186/s12887-019-1767-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ministry of Health, Indonesia. Indonesia Health Survey of 2023. Jakarta: Ministry of Health; 2023 (Indonesian) [Google Scholar]
- 6.Simen-Kapeu A, Bogler L, Weber AC, Ntambi J, Zagre NM, Vollmer S, et al. Prevalence of diarrhoea, acute respiratory infections, and malaria over time (1995-2017): a regional analysis of 23 countries in West and Central Africa. J Glob Health. 2021;11:13008. doi: 10.7189/jogh.11.13008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Islam M, Islam K, Dalal K, Hossain Hawlader MD. In-house environmental factors and childhood acute respiratory infections in under-five children: a hospital-based matched case-control study in Bangladesh. BMC Pediatr. 2024;24(1):38. doi: 10.1186/s12887-024-04525-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mulambya NL, Nanzaluka FH, Sinyangwe NN, Makasa M. Trends and factors associated with acute respiratory infection among under five children in Zambia: evidence from Zambia’s demographic and health surveys (1996-2014) Pan Afr Med J. 2020;36:197. doi: 10.11604/pamj.2020.36.197.18799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rodríguez L, Cervantes E, Ortiz R. Malnutrition and gastrointestinal and respiratory infections in children: a public health problem. Int J Environ Res Public Health. 2011;8(4):1174–1205. doi: 10.3390/ijerph8041174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lowe C, Kelly M, Sarma H, Richardson A, Kurscheid JM, Laksono B, et al. The double burden of malnutrition and dietary patterns in rural Central Java, Indonesia. Lancet Reg Health West Pac. 2021;14:100205. doi: 10.1016/j.lanwpc.2021.100205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ministry of Health, Indonesia. Indonesia nutrition status survey of 2022 results book [cited 2024 Mar 25]. Available from: https://repository.badankebijakan.kemkes.go.id/id/eprint/4855/ (Indonesian)
- 12.Mulyanto J, Kringos DS, Kunst AE. Socioeconomic inequalities in healthcare utilisation in Indonesia: a comprehensive survey-based overview. BMJ Open. 2019;9(7):e026164. doi: 10.1136/bmjopen-2018-026164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WHO Multicentre Growth Reference Study Group WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr Suppl. 2006;450:76–85. doi: 10.1111/j.1651-2227.2006.tb02378.x. [DOI] [PubMed] [Google Scholar]
- 14. Schumacher D. Package ‘anthro’. Computation of the WHO child growth standards; 2023 [cited 2024 Mar 27]. Available from: https://github.com/worldhealthorganization/anthro.
- 15.Lai PC, So FM, Chan KW. Spatial epidemiological approaches in disease mapping and analysis. Boca Raton: CRC Press; 2009. pp. 71–74. [Google Scholar]
- 16.Hair Jr JF, Hult GT, Ringle CM, Sarstedt M. A primer on partial least squares structural equation modeling (PLS-SEM). 3rd edition. Thousand Oaks: SAGE Publications; 2021. pp. 105–115. [Google Scholar]
- 17.Chin WW. The partial least squares approach or structural equation modeling. In: Marcoulieds GA, editor. Modern methods for business research. Mahwah: Lawrence Erlbaum; 1998. pp. 295–336. [Google Scholar]
- 18.Chan YH. Biostatistics 104: correlational analysis. Singapore Med J. 2003;44(12):614–619. [PubMed] [Google Scholar]
- 19.Ekholuenetale M, Nzoputam CI, Okonji OC, Barrow A, Wegbom AI, Edet CK. Differentials in the prevalence of acute respiratory infections among under-five children: an analysis of 37 sub-Saharan countries. Glob Pediatr Health. 2023;10:2333794X231156715. doi: 10.1177/2333794X231156715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yaya S, Bishwajit G. Burden of acute respiratory infections among under-five children in relation to household wealth and socioeconomic status in Bangladesh. Trop Med Infect Dis. 2019;4(1):36. doi: 10.3390/tropicalmed4010036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Um S, Vang D, Pin P, Chau D. Trends and determinants of acute respiratory infection symptoms among under-five children in Cambodia: analysis of 2000 to 2014 Cambodia demographic and health surveys. PLOS Glob Public Health. 2023;3(5):e0001440. doi: 10.1371/journal.pgph.0001440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alao R, Nur H, Fivian E, Shankar B, Kadiyala S, Harris-Fry H. Economic inequality in malnutrition: a global systematic review and meta-analysis. BMJ Glob Health. 2021;6(12):e006906. doi: 10.1136/bmjgh-2021-006906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seferidi P, Hone T, Duran AC, Bernabe-Ortiz A, Millett C. Global inequalities in the double burden of malnutrition and associations with globalisation: a multilevel analysis of Demographic and Health Surveys from 55 low-income and middle-income countries, 1992-2018. Lancet Glob Health. 2022;10(4):e482–e490. doi: 10.1016/S2214-109X(21)00594-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Laksono AD, Wulandari RD, Rohmah N, Rukmini R, Tumaji T. Regional disparities in hospital utilisation in Indonesia: a cross-sectional analysis data from the 2018 Indonesian Basic Health Survey. BMJ Open. 2023;13(1):e064532. doi: 10.1136/bmjopen-2022-064532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hosseinpoor AR, Nambiar D, Tawilah J, Schlotheuber A, Briot B, Bateman M, et al. Capacity building for health inequality monitoring in Indonesia: enhancing the equity orientation of country health information system. Glob Health Action. 2018;11(sup1):1419739. doi: 10.1080/16549716.2017.1419739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ullah MB, Mridha MK, Arnold CD, Matias SL, Khan MS, Siddiqui Z, et al. Factors associated with diarrhea and acute respiratory infection in children under two years of age in rural Bangladesh. BMC Pediatr. 2019;19(1):386. doi: 10.1186/s12887-019-1738-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sinha IP, Lee AR, Bennett D, McGeehan L, Abrams EM, Mayell SJ, et al. Child poverty, food insecurity, and respiratory health during the COVID-19 pandemic. Lancet Respir Med. 2020;8(8):762–763. doi: 10.1016/S2213-2600(20)30280-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Syafiq A, Fikawati S, Gemily SC. Household food security during the COVID-19 pandemic in urban and semi-urban areas in Indonesia. J Health Popul Nutr. 2022;41(1):4. doi: 10.1186/s41043-022-00285-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hill H. What’s happened to poverty and inequality in Indonesia over half a century? Asian Dev Rev. 2021;38(1):68–97. doi: 10.1162/adev_a_00158. [DOI] [Google Scholar]
- 30.Nasution YN, Sitorus MY, Sukandar K, Nuraini N, Apri M, Salama N. The epidemic forest reveals the spatial pattern of the spread of acute respiratory infections in Jakarta, Indonesia. Sci Rep. 2024;14(1):7619. doi: 10.1038/s41598-024-58390-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Central Agency of Statistics DKI Jakarta Province. DKI Jakarta Province in figures 2022 [cited 2024 Mar 29]. Available from: https://jakarta.bps.go.id/id/publication/2022/02/25/5979600247867d861a1f334c/provinsi-dki-jakarta-dalam-angka-2022.html (Indonesian)
- 32. Ministry of Health, Indonesia. Indonesia health profile. Jakarta: Ministry of Health, Indonesia; 2018 (Indonesian) [Google Scholar]
- 33.Astuti SP, Day R, Emery SB. A successful fuel transition? Regulatory instruments, markets, and social acceptance in the adoption of modern LPG cooking devices in Indonesia. Energy Res Soc Sci. 2019;58:101248. doi: 10.1016/j.erss.2019.101248. [DOI] [Google Scholar]
- 34.Wadi Y, Rantetampang AL, Sandjaja B, Mallongi A. Factors influencing acute respiratory infection incidence to child under five years in sentani health primary Jayapura district. Int J Sci Healthc Res. 2019;4(1):274–283. [Google Scholar]
- 35.Adesanya OA, Chiao C. A multilevel analysis of lifestyle variations in symptoms of acute respiratory infection among young children under five in Nigeria. BMC Public Health. 2016;16(1):880. doi: 10.1186/s12889-016-3565-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Seidu AA, Ameyaw EK, Ahinkorah BO, Baatiema L, Appiah F. Ecological zone and symptoms of acute respiratory infection among children under five in Ghana: 1993-2014. SSM Popul Health. 2019;8:100414. doi: 10.1016/j.ssmph.2019.100414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hartarto RB, Susamto AA, Rizkan M, Hajar I, Safira L, Mostafa E. Conditional cash transfer and stunting prevention: evidence from Bima, West Nusa Tenggara. Cogent Soc Sci. 2023;9(2):2260607. doi: 10.1080/23311886.2023.2260607. [DOI] [Google Scholar]
- 38.Cahyadi N, Hanna R, Olken BA, Prima RA, Satriawan E, Syamsulhakim E. Cumulative impacts of conditional cash transfer programs: experimental evidence from Indonesia. Am Econ J Econ Policy. 2020;12(4):88–110. doi: 10.1257/pol.20190245. [DOI] [Google Scholar]
- 39.Vazir S, Engle P, Balakrishna N, Griffiths PL, Johnson SL, Creed-Kanashiro H, et al. Cluster-randomized trial on complementary and responsive feeding education to caregivers found improved dietary intake, growth and development among rural Indian toddlers. Matern Child Nutr. 2013;9(1):99–117. doi: 10.1111/j.1740-8709.2012.00413.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thoday K, Benjamin P, Gan M, Puzzolo E. The Mega Conversion Program from kerosene to LPG in Indonesia: lessons learned and recommendations for future clean cooking energy expansion. Energy Sustain Dev. 2018;46:71–81. doi: 10.1016/j.esd.2018.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The Provincial of Bali, Nusa Tenggara Barat and Nusa Tenggara Timur is grouped in the Bali and Nusa Tenggara (light green). The Provincial of Maluku and Maluku Utara included in Maluku region (brown). The Provincial of Bangka Belitung and Kepulauan Riau is included in Sumatera (blue)
Notes: Darker shades of orange indicate a higher proportion of underweight (A), wasted (B), stunting (C), and the triple burden of malnutrition problems (D) at the city/regency level.