Abstract
Introduction and importance
Meckel's diverticulum (MD) is an unusual clinical condition that occurs in approximately 2–4 %. The complications are more common in children, with a low prevalence in adults, with the main complication in adults being intestinal obstruction followed by diverticulitis with or without perforation.
Case presentation
We present a 30-year-old female patient with a history of an appendectomy. She attends the emergency room due to a four-day history of pain in the lower abdominal quadrants, tachycardia, and leukocytosis, with an abdominal CT scan identifying an inflammatory process of the ileum, suggesting a Meckel's diverticulum, urachus remnant, or foreign body.
The patient was taken to surgery, and inflammatory adhesions, including a perforated Meckel's diverticulum with necrotic signs and purulent production, were evidenced. Intestinal resection and ileal anastomosis were performed with no complications at 90 days.
Clinical discussion
Preoperative diagnosis is difficult in cases with associated inflammatory conditions and is generally made incidentally during surgery and less frequently with CT scans.
Surgical management for patients with MD is still controversial and depends on many factors, including symptoms, related complications, characteristics of the diverticulum, and the patient's clinical condition. Currently, no standardized surgical technique exists, and cases should be individualized.
Conclusion
Meckel's diverticulum perforation is a rare complication in the adult population and remains a diagnostic and surgical challenge, and the final decision must be individualized.
Keywords: Meckel's diverticulum, Perforation, Outcomes, Case report, Colombia
Highlights
-
•
Meckel's diverticulum in adults still represents a surgical challenge.
-
•
There is no standardized surgical technique for patients with perforated Meckel’s diverticulum
-
•
Meckel’s diverticulum complications should be treated aggressively to avoid remnant ectopic tissue and further complications.
1. Introduction
Meckel's diverticulum (MD) is an unusual clinical condition that occurs in approximately 2–4 % [1,2] due to a fetal development abnormality in the fourth to sixth gestation week due to a failure in the obliteration of the intestinal duct leading not only to an MD but also omphalomesenteric fistula or omphalomesenteric cyst [3]. The lifetime risk of presenting any complication is between 4 and 7 %; nevertheless, in older patients (> 80 years old), it's less frequent, reaching 0.5 % in some case series [[1], [2], [3]]. It's estimated that in cases of acute abdomen presented to the emergency room, one case in 400 is due to any complication of MD, being the most frequent intestinal obstruction (40–50 %) followed by diverticulitis and perforation [4] Even with the diagnostic modalities in the present time, diagnosis is often performed intraoperatively [[2], [3], [4]]. There is no standardized surgical technique between diverticulectomy and intestinal resection with anastomosis [1].
This article aims to present a case of a perforated Meckel's diverticulum in an adult female patient in Colombia.
2. Presentation of the case
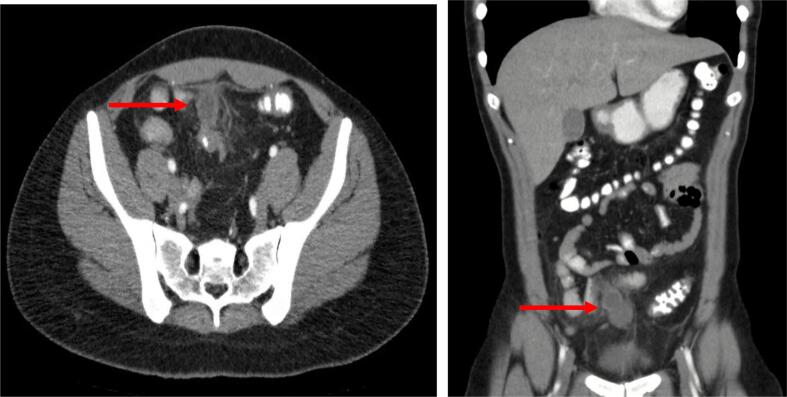
After ethical and institutional approval, previous informed consent was filled, following SCARE guidelines [5]. We present A 30-year-old female patient with a history of an open appendectomy, left inguinal herniorrhaphy, and left salpingectomy due to an ectopic pregnancy who attends the emergency room due to a four-day history of pain in the lower abdominal quadrants, initially located in the right lower quadrant, accompanied by vomiting. In the initial physical examination, the patient had tachycardia (Heart rate 100 bpm) and pain in the lower quadrants. Labs with leukocytosis of 19,300 gb/dL, neutrophilia of 81 %, normal creatinine levels, and a negative pregnancy test. Diagnostic images were indicated, with an abdominal computed tomography identifying a hypodense hypogastric lesion, peripheral mesenteric fat edema, and inflammatory compromise of the adjacent ileum and sigmoid colon. Therefore, having as the primary diagnostic suspicion of a Meckel's diverticulum versus an inflammatory or infectious process of a urachus remnant or even a granuloma due to a foreign body due to the patient's multiple previous surgical interventions. (Fig. 1).
Fig. 1.
Tomographic findings. Red Arrow: Inflammatory process in the distal ileum.
Consequently, the patient was taken to a diagnostic laparoscopy, finding a contained perforated Meckel's diverticulum, with a 1 cm long base, perforated 60 cm away from the ileocecal valve, with a 3 × 3 cm cavity with necrotic signs and adhered to the middle abdominal line in contact with the sigmoid colon. Additionally, evidence of visceral-visceral adhesions, an inflammatory mass involving the sigmoid colon, distal ileum, the ileocecal valve, and the greater omentum with significant inflammation, and evidence of a 3 × 3 cm cavity located in the pelvis, with a purulent, fetid production of 20 cc. A release of adhesions was performed, and microbiological cultures were obtained. Given the lack of a safe window to dissect along the sigmoid colon, the initial laparoscopy was converted to a medial infra umbilical and supraumbilical laparotomy.
A more extensive adhesion liberation was performed, finding adhesions between the abdominal wall of the right lower quadrant, the greater omentum, and the suprapubic area. Thus achieving traction of the inflammatory mass, then revealing the perforated Meckel's diverticulum (Fig. 2). Intestinal resection and anastomosis were performed, preserving 5 cm of healthy tissue proximal and distal to the lesion. A lateral-lateral ileal anastomosis with mechanical suture was performed. Finally, due to the inflammatory compromise of the greater omentum, an omentectomy was performed, and a 19fr Blake drain was placed. Surgical time was 95 min, with 30 cc of intraoperative bleeding. Pathology reports severe peritonitis, acute serositis, and follicular lymphoid hyperplasia. Cultures obtained report sensible Escherichia coli, Klebsiella pneumoniae, and Proteus mirabilis. The overall length of stay was six days, with no complications after 30, 60, and 90 days.
Fig. 2.
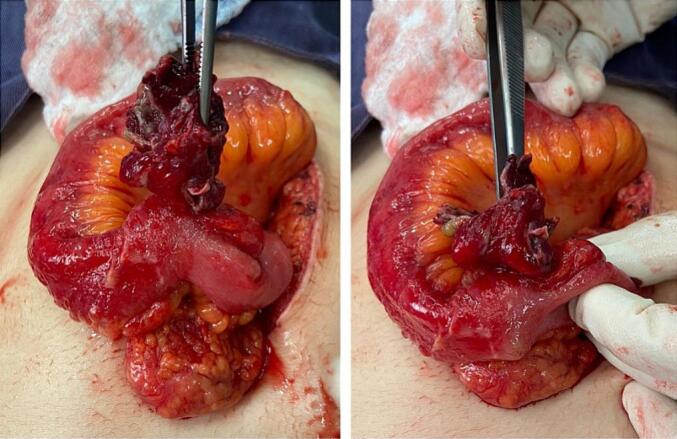
Surgical findings.
3. Discussion
First described by Hildanus in 1598 and better characterized by Meckel in 1809 [1,3], Meckel's diverticulum is the most common congenital abnormality found in the gastrointestinal tract, reaching an incidence rate between 2 and 4 % [1,2]. It's considered a true diverticulum and contains all the intestinal layers; since it comes from pluripotential cells, MD could contain cells differentiated to gastric (50 %), pancreatic (5 %), and in less proportion of patients colonic or hepato-biliary cells [6] Meckel's diverticulum is better known by pediatric surgeons than general surgeons due to its higher prevalence in patients <16 years old, associated with higher rates of acute complications such as bleeding, and is considered the most frequent in the pediatric population [1] Nevertheless, in patients older than 16 years old, there is a lifetime risk of 4–7 % of any complication; intestinal obstruction is recognized as the most frequent acute condition related to MD in the adult population; however, diverticulitis and perforation are as well complications evidenced in this patients, in lesser than 1 and 3 % respectively [3]. Perforation is rare and most often related to obstruction of the lumen due to stercolith, foreign body, or gastric ectopic tissue [[1], [2], [3]].
Diagnosis is challenging and requires a high index of suspicion; “Meckel Scan” (mTc-Pertechnectate scintigraphy) is recognized as the preferred diagnostic method, with sensitivity rates that reach 86–90 % and specificity of 95–100 %, according to some case series [[6], [7], [8], [9]]. Nevertheless, this image requires the presence of gastric ectopic tissue. Depending on the clinical presentation, some diagnostic methods could be feasible; for example, in cases of gastrointestinal bleeding, red blood cell tomography could be used with sensitivity and specificity rates of 90 % [9]. In the acute abdomen, computed tomography could suggest the presence of MD, as in our case; however, preoperative diagnosis is difficult in cases with associated inflammatory conditions [4,6,9]. Nevertheless, in the adult population, diagnosis is often made intraoperatively or as an incidental finding during other abdominal procedures in particular patients with acute appendicitis [6]; for that reason, there is a well-known rule to locate and recognize an MD, more frequently localized 2 ft. from the ileocecal valve, in the antimesenteric border, with 2 in. of length measure [1,9].
Surgical management for patients with MD is still controversial. It depends on many factors, including symptoms or complications related to the disease, the length of the diverticula [3,6,8,9], and the patient's clinical condition. However, no standardized surgical technique exists, and cases should be individualized.
Surgical management is mandatory for symptomatic cases and is still a matter of debate regarding the type of surgical procedure indicated; in cases of diverticulitis, bleeding, or incidental finding, diverticula resection is considered appropriate [9]. Nevertheless, there is an inherent risk of leaving ectopic tissue, with a high risk of recurrence. Some authors recommend intestinal resection with anastomosis, trying to resect all the ectopic tissue and avoid the recurrence of any complications [1,3,6,9]. Case series reported in Colombia reported low morbidity and mortality rates for cases of small bowel resection and anastomosis, either end-to-end or lateral-lateral [9]. In our case, the patient presented with an acute abdomen due to perforation with intra-abdominal abscess, and management of the diverticulum is intestinal resection and anastomosis, with no complications at 30, 60, or 90 days.
The management of perforated diverticulitis is not frequent in our population, and our case increases the literature regarding this topic, including surgical characteristics and postoperative outcomes.
4. Conclusion
Meckel's diverticulum in the adult population remains a surgical challenge. Perforation is a rare complication, and according to the present literature, surgical technique is still a matter of debate. Cases should be individualized.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Consent
Written informed consent was obtained from the patient to publish this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal by request.
Ethical approval
Ethical approval of the institutional committee was obtained from previous publication.
Funding
This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contribution
C.E.R.C and I.S. had the research idea.
C.E.R.C, I.S, L.R.G, and D.G.G. participated in drafting the article and revised it critically for important intellectual content.
C.E.R.C, I.S, L.R.G and D.G.G contributed substantially to the conception and design, acquisition of data, analysis, and interpretation of data.
Guarantor
Carlos Eduardo Rey Chaves.
Research registration number
None.
Declaration of competing interest
The authors do not declare any conflict of interest.
Acknowledgments
To our patient.
References
- 1.Lequet J., Menahem B., Alves A., Fohlen A., Mulliri A. Meckel’s diverticulum in the adult. J. Visc. Surg. 2017 Sep;154(4):253–259. doi: 10.1016/j.jviscsurg.2017.06.006. Epub 2017 Jul 9. PMID: 28698005. [DOI] [PubMed] [Google Scholar]
- 2.Mohammed A.A., Rasheed Mohammed M. Emergency presentations of Meckel’s diverticulum in adults. Surg Res Pract. 2022 Aug;25(2022):6912043. doi: 10.1155/2022/6912043. PMID: 36060297; PMCID: PMC9436618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sagar J., Kumar V., Shah D.K. Meckel’s diverticulum: a systematic review. J. R. Soc. Med. 2006 Oct;99(10):501–505. doi: 10.1177/014107680609901011. Erratum in: J. R. Soc. Med. 2007 Feb;100(2):69. PMID: 17021300; PMCID: PMC1592061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park J.J., Wolff B.G., Tollefson M.K., Walsh E.E., Larson D.R. Meckel diverticulum: the Mayo Clinic experience with 1476 patients (1950-2002) Ann. Surg. 2005 Mar;241(3):529–533. doi: 10.1097/01.sla.0000154270.14308.5f. PMID: 15729078; PMCID: PMC1356994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A., Collaborators. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2023 May 1;109(5):1136–1140. doi: 10.1097/JS9.0000000000000373. (PMID: 37013953; PMCID: PMC10389401) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yahchouchy E.K., Marano A.F., Etienne J.C., Fingerhut A.L. Meckel’s diverticulum. J. Am. Coll. Surg. 2001 May;192(5):658–662. doi: 10.1016/s1072-7515(01)00817-1. (PMID: 11333103) [DOI] [PubMed] [Google Scholar]
- 7.Bani-Hani, K., Shatnawi, N. Meckel's diverticulum: comparison of incidental and symptomatic cases. World J. Surg. 28, 917–920 (2004). https://doi.org/ 10.1007/s00268-004-7512-3. [DOI] [PubMed]
- 8.Weinstein E.C., Cain J.C., Remine W.H. Meckel’s diverticulum: 55 years of clinical and surgical experience. JAMA. 1962 Oct;20(182):251–253. doi: 10.1001/jama.1962.03050420027007. (PMID: 13999637) [DOI] [PubMed] [Google Scholar]
- 9.Hernández J.D., Valencia G., Girón F., García Sierra A.M., Núñez-Rocha R.E., Rodríguez L.M., Rey Chaves C.E., Londoño E.E., Nassar R. Meckel’s diverticulum: analysis of 27 cases in an adult population. Front. Surg. 2023 Dec;18(10):1327545. doi: 10.3389/fsurg.2023.1327545. PMID: 38179318; PMCID: PMC10765580. [DOI] [PMC free article] [PubMed] [Google Scholar]