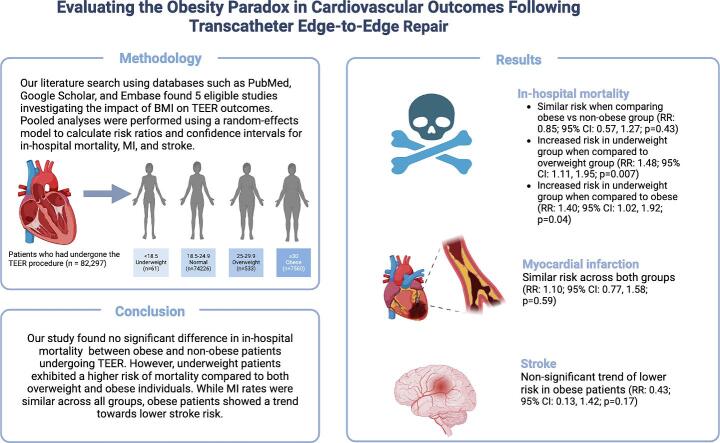
Graphical abstract
Keywords: Obesity paradox, Transcatheter Edge-to-Edge Repair, Body mass index, Myocardial infarction, Stroke, In-hospital mortality
Abstract
Background
The impact of body mass index (BMI) on Transcatheter Edge-to-Edge Repair (TEER) outcomes remains uncertain, with studies showing conflicting results. Some suggest an ’obesity paradox’ exists, favoring better outcomes for obese patients and worse outcomes for underweight patients, while others report no significant impact of BMI.
Methodology
We systematically searched major databases for studies on baseline BMI and post-procedural outcomes in TEER patients. Patients were grouped by BMI: underweight (<18.5 kg/m2), normal (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), and obese (≥30 kg/m2). Data were pooled using a random-effects model, with risk ratios (RRs) and their 95 % confidence intervals (CIs) as effect measures. Statistical significance was set at p < 0.05.
Results
Our study, analyzing five observational studies with 7580 obese and 74,717 non-obese patients, found no significant difference in in-hospital mortality between the groups (RR: 0.85; p = 0.427). Subgroup analysis indicated a higher mortality risk for underweight patients compared to overweight (RR: 1.48; p = 0.006) and obese patients (RR: 1.40; p = 0.036), though the difference between underweight and normal-weight patients was not significant (RR: 1.18; p = 0.216). The risks of myocardial infarction (RR: 1.10; p = 0.592) and stroke (RR: 0.43; p = 0.166) were also similar between obese and non-obese patients.
Conclusions
In conclusion, our analysis found no significant difference in in-hospital mortality, myocardial infarction or stroke risk between obese and non-obese patients undergoing TEER. However, underweight patients may have a higher risk of in-hospital mortality compared to overweight and obese individuals, highlighting the potential impact of BMI on outcomes in TEER patients.
1. Introduction
Mitral regurgitation (MR) and tricuspid regurgitation (TR) are common valvular heart diseases that can arise from either primary structural abnormalities of the valve itself (e.g., leaflet degeneration causing poor leaflet coaptation) or from conditions like infective endocarditis that damage the valve, leading to regurgitation without coaptation failure. Alternatively, these diseases can develop from secondary causes related to ventricular dysfunction, both of which result in incomplete valve closure and the backflow of blood into the atria [1], [2], [3]. While the severity of these disorders varies, they may lead to adverse cardiovascular events and heart failure if left untreated [4]. Surgical valve replacement or repair has long been the available treatment option; however, they may not be accessible to patients with high surgical risks and comorbidities [4], [5]. Percutaneous interventions are therefore considered appropriate for such patients, and various transcatheter techniques have emerged in recent years [6], [7], [8].
Transcatheter Edge‐to‐Edge Repair (TEER) is a minimally invasive procedure effective in treating MR and TR [9], [10], [11], [12]. The MitraClip system is the most widely used device for TEER, and its implantations are increasing worldwide [11], [13], [14]. Studies have shown its effectiveness in improving clinical outcomes, reducing patients’ symptoms, and lowering rehospitalization rates, as well as being associated with reduced rates of adverse events [11], [13], [15]. However, patient selection for TEER remains a point of debate, and certain characteristics, such as the body mass index (BMI) of the patients, have been shown to influence the success of the procedure [16], [17]. Despite obesity being a known risk factor for cardiovascular diseases (CVD), several studies have demonstrated better prognosis in obese patients, especially suffering from coronary artery disease (CAD) undergoing percutaneous coronary intervention (PCI) as compared to their normal or underweight counterparts [17], [18]. This is referred to as the ‘obesity paradox.’ However, the literature provides conflicting results in valvular conditions (such as MR or TR) about the impact of BMI on MitraClip procedural outcomes with some studies showing no discernible effect to others demonstrating the obesity paradox [16], [19], [20].
Considering the significant literature gap about this paradox, our meta-analysis aims to evaluate the impact of BMI categories: underweight, normal-weight, overweight, and obesity, on short-term and long-term clinical outcomes in patients undergoing TEER using the MitraClip system.
2. Material and methods
Our meta-analysis was conducted according to the guidelines outlined by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [21]. The study protocol was formally registered with the International Prospective Register of Systematic Reviews (PROSPERO) under the identifier CRD42024578749.
2.1. Literature search and study selection
We conducted an extensive electronic search on August 12, 2024, across multiple databases, including PubMed, Embase, Scopus, Cochrane and Web of Science from inception to August 2024. The aim was to identify all studies examining the relationship between baseline BMI status and post-procedural outcomes in patients undergoing TEER. Our search strategy utilized medical subject headings (MeSH) terms and free text keywords: “Body Mass Index” OR “BMI” OR “Underweight” OR “Overweight” OR “Overweight” OR “Obese” OR “MitraClip” OR “Transcatheter mitral valve repair” OR “TEER” OR “Transcatheter edge-to-edge repair” OR “Tricuspid regurgitation” OR “Mitral regurgitation”. Boolean operators such as “AND” and “OR” were used to create a search strategy in combination with keywords. These terms were employed in various combinations using Boolean operators such as “AND” and “OR” to optimize the search results. Additionally, we manually reviewed the reference lists of all identified articles to ensure that no relevant studies were overlooked in the initial search. A detailed description of the search strategy is available in Supplementary Table 1.
The studies identified through the literature search were imported into EndNote X9 (Clarivate Analytics, USA), where duplicates were removed. Two authors (A.G. and M.D.T.) independently screened the studies by reviewing the titles and abstracts, followed by a full-text review of the selected articles. In cases of disagreement, a third author (S.M.) was consulted to reach a consensus.
2.2. Eligibility criteria
2.2.1. Inclusion criteria
The inclusion criteria for the studies were based on the PECO framework (Population, Exposure, Comparison, and Outcome) commonly used in systematic reviews and meta-analyses. In this framework, 'P' represents patients undergoing TEER for MR or TR, 'E' refers to obese patients, 'C' refers to non-obese patients, and 'O' includes in-hospital mortality, myocardial infarction, and stroke as outcomes. Thus, the inclusion criteria included: [1] studies involving patients undergoing TEER for MR or TR, [2] studies comparing post-procedural outcomes according to the baseline BMI of patients, and [3] studies reporting any of the pre-specified outcomes.
2.2.2. Exclusion criteria
The exclusion criteria included studies that did not provide data on the association between baseline BMI and post-procedural outcomes in TEER patients or had overlapping populations. We also excluded non-peer-reviewed articles, non-English publications, case reports, case series, commentaries, editorials, review articles and meta-analyses.
2.3. Data extraction
Data extraction from the included studies was performed by two authors (S.M. and M.D.T.) using a pre-tested Excel sheet, capturing details such as the first author's name, publication year, country of origin, study design, sample size and reported outcomes. Data was extracted by categorizing patients into four BMI groups: underweight (BMI<18.5 kg/m2), normal-weight (BMI 18.5–24.9 kg/m2), overweight (BMI 25–29.9 kg/m2) and obese (BMI≥30 kg/m2). Underweight, normal-weight and overweight patients were included in the non-obese group.
2.4. Quality assessment of the included studies
The quality of the non-randomized studies included in this systematic review and meta-analysis was evaluated using the Newcastle Ottawa Scale (NOS) [22]. This scale assesses studies based on several criteria, including the representativeness of the exposed cohort, selection of the non-exposed cohort, ascertainment of exposure, evidence of outcome absence at the study's outset, cohort comparability, outcome assessment, and follow-up adequacy. The risk of bias was categorized into low risk (7–10points), moderate risk (4–6 points), and high risk (0–3 points). Two reviewers (A.M.K and M.D.T.) independently carried out this assessment.
2.5. Statistical analysis
Statistical analyses were conducted using R software version 4.4.1 using the “meta” package. The analysis included the calculation of pooled risk ratios (RRs) and 95 % confidence intervals (CIs) for dichotomous outcomes, utilizing the Mantel-Haenszel random effects model for pooling results from the studies. Forest plots were generated to visually present the results. A p-value of less than 0.05 was considered statistically significant. Heterogeneity among the studies was assessed using the Higgins I2 test [23]. Sensitivity analyses, using a leave-one-out approach, were performed to explore the sources of potential heterogeneity by excluding one study at a time, thereby assessing each study's impact on the overall estimate. Publication bias was assessed by visually inspecting the funnel plots.
3. Results
3.1. Study selection and characteristics
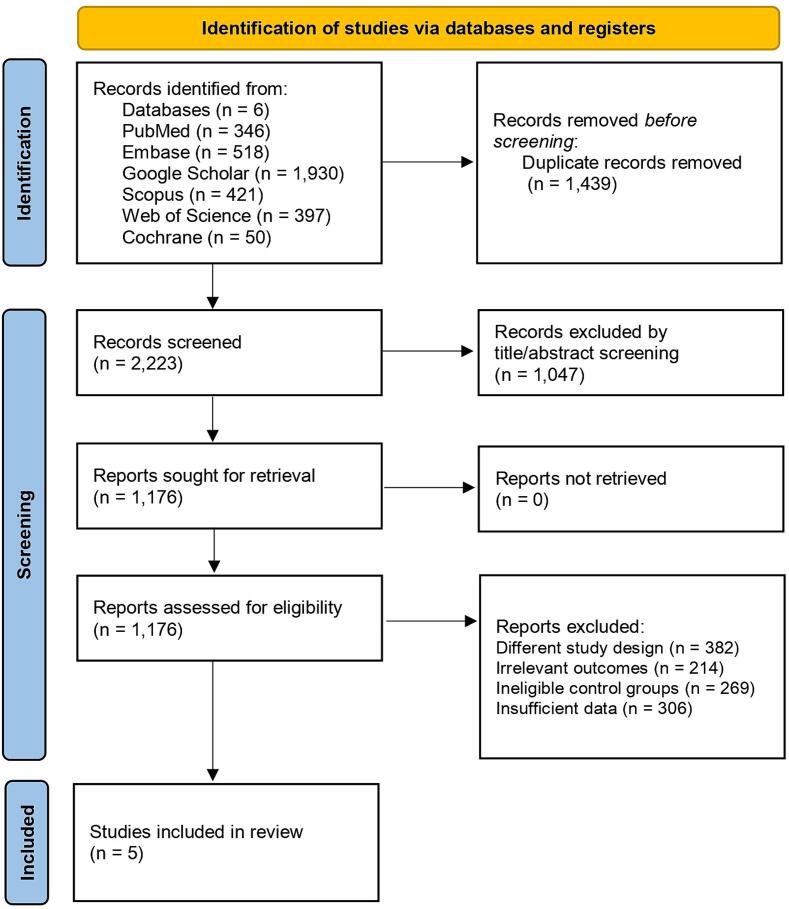
A total of 3,662 records were identified from various databases. After removing 1,439 duplicates, 2,223 studies were further screened based on title and abstract. A total of 1,176 studies were assessed using their full texts after removing studies that did not meet our inclusion criteria. Further text screening resulted in the exclusion of 382 studies due to different study designs, 214 studies for reporting irrelevant outcomes, 269 studies with ineligible control groups, and 306 studies due to insufficient data. Ultimately, five studies (16,19,24–26) met the inclusion criteria and were included in the final analysis. This selection process is depicted in the PRISMA flowchart (Fig. 1).
Fig. 1.
The 2020 Preferred Reporting Items for Systematic Reviews and Meta-Analyses Flowchart.
Our meta-analysis included 82,297 participants, with 7,580 in the obese group and 74,717 in the non-obese group, with the female percentages of 44 % and 51 %, respectively. The mean age of participants ranged from 70 to 80 years across the studies. Hypertension was reported in 44 % of non-obese and 53 % of obese patients, while 26 % and 49 % were diabetic in the two groups, respectively. Two studies reported functional mitral valve regurgitation in 66 % of non-obese and 73 % of obese patients. All included studies involved patients undergoing TEER for MR. None of the studies included patients undergoing TEER in TR, as no study met our inclusion criteria. Approximately 13 % of non-obese and 15 % of obese patients had a prior history of myocardial infarction, whereas a history of prior stroke was present in 5 % of patients in both groups. The detailed baseline characteristics of the studies and the demographic details of the patients are summarized in Table 1, Table 2, respectively.
Table 1.
Baseline characteristics of included studies.
| Study | Study design | Country of origin |
Participants, n |
Sex (Females), n |
Age (years), Mean ± SD |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Underweight | Normal weight | Overweight | Obese | Underweight | Normal weight | Overweight | Obesity | Underweight | Normal weight | Overweight | Obesity | |||
| Agarwal 2023 | Observational study | USA | NR | 23,289 | NR | 3,176 | NR | 10,503 | NR | 1673 | NR | 78.4 ± 13.735 | NR | 71.35 ± 15.85 |
| Keller 2020 | Observational study | Germany | NR | 12,546 | NR | 1,017 | NR | 4,959 | NR | 462 | NR | 76.67 ± 6.67 | NR | 73.67 ± 7.42 |
| Kalbacher 2020 | Observational study | Germany | 49 | 293 | 296 | 132 | 39 | 107 | 97 | 58 | 78.8 ± 7.4 | 76.5 ± 8.1 | 75.0 ± 8.2 | 71.9 ± 9.8 |
| Keller 2022 | Observational study | Germany | 12 | 220 | 237 | 80 | 10 | 135 | 104 | 43 | 79.47 ± 10.90 | 80.23 ± 7.09 | 78.83 ± 6.86 | 74.30 ± 7.04 |
| Shamaki 2023 | Observational study | USA | NR | 37,775 | NR | 3,175 | NR | 16,583 | NR | 1,606 | NR | 76.5 ± 77.743 | NR | 70.7 ± 45.078 |
Abbreviations: NR: Not reported; SD: standard deviation
Table 2.
Demographic details of participants in the included studies.
 |
Abbreviations; NR: Not reported; MI: Myocardial infarction; PCI: Percutaneous coronary intervention
3.2. Endpoints
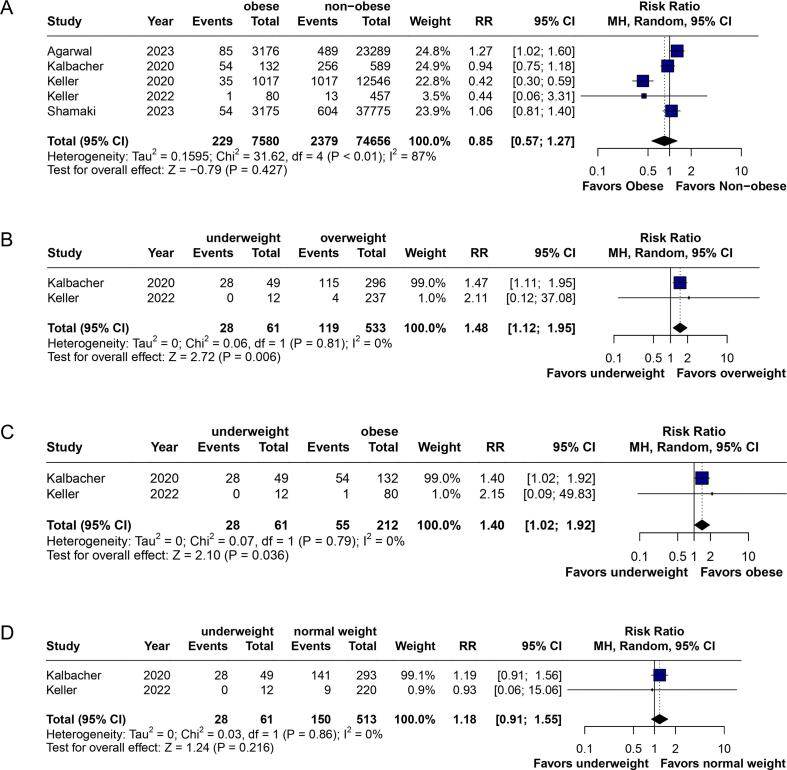
3.2.1. In-hospital mortality
Five studies reported the outcome of in-hospital mortality [16], [19], [24], [25], [26]. The pooled analysis revealed no statistically significant difference between the obese and non-obese patients (RR: 0.85; 95 % CI: 0.57 to 1.27; p = 0.427; I2 = 87 %) (Fig. 2-A). High heterogeneity was observed among the studies. Upon performing the leave-one-out sensitivity analysis, the heterogeneity was reduced to 30 % by excluding Keller et al. 2020 [16]) (Supplementary Fig. 1. The subgroup analysis showed a significantly higher risk of in-hospital mortality for underweight patients compared to overweight (RR: 1.48; 95 % CI: 1.12 to 1.95; p = 0.006) (Fig. 2-B) and obese patients (RR: 1.40; 95 % CI: 1.02 to 1.92; p = 0.036) (Fig. 2-C). However, the comparison between underweight and normal-weight patients did not show statistical significance (RR: 1.18; 95 % CI: 0.91 to 1.55; p = 0.216) (Fig. 2-D).
Fig. 2.
Forest plots for the comparison of in-hospital mortality between (A) obese and non-obese patients, (B) underweight and overweight patients, (C) underweight and obese patients, and (D) underweight and normal weight patients undergoing Transcatheter Edge‐to‐Edge Repair (TEER).
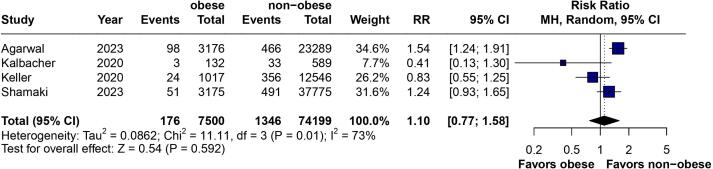
3.2.2. Myocardial infarction
The outcome of myocardial infarction was reported by four studies [16], [19], [25], [26]. According to the pooled analysis, the risk of MI was comparable between the two groups (RR: 1.10; 95 % CI: 0.77 to 1.58; p = 0.592; I2 = 73 %) (Fig. 3) and the difference was not statistically insignificant. Moderate heterogeneity was observed among the studies, which reduced to 61 % after excluding Agarwal et al. 2023 [25] from the analysis (Supplementary Fig. 2).
Fig. 3.
Forest plot for the comparison of myocardial infarction between obese and non-obese patients undergoing Transcatheter Edge‐to‐Edge Repair (TEER).
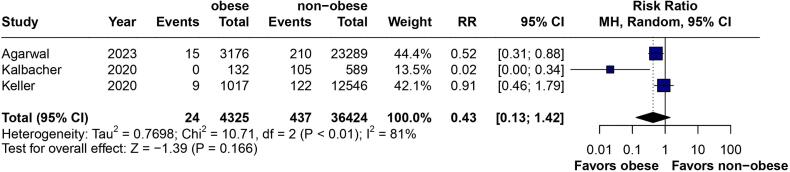
3.2.3. Stroke
Three studies reported data on the outcome of stroke [16], [19], [25]. Based on the pooled analysis, there was no statistically significant difference between the two groups (RR: 0.43; 95 % CI: 0.13 to 1.42; p = 0.166; I2 = 81 %) (Fig. 4). High heterogeneity was observed among the studies. The leave-one-out sensitivity analysis reduced the heterogeneity to 39 % after excluding Kalbacher et al. 2020 [19] (Supplementary Fig. 3).
Fig. 4.
Forest plot for the comparison of stroke between obese and non-obese patients undergoing Transcatheter Edge‐to‐Edge Repair (TEER).
3.2.4. Quality assessment and publication bias
According to the Newcastle-Ottawa Scale, the risk of bias for all included studies was rated as 'low' (Supplementary Table 2). Visual inspection of the funnel plots showed a symmetrical appearance, indicating no to low risk of publication bias (Supplementary Fig. 4).
4. Discussion
Our study aimed to investigate the impact of BMI on the outcomes of TEER procedures in patients with both TR and MR by categorizing the patients into four distinct BMI groups (underweight, normal-weight, overweight, and obese). Our meta-analysis included five observational studies and a substantial cohort of 82,297 patients. Previous studies have established both underweight and overweight statuses as significant predictors of mortality in CVDs [27]. Our study included 7580 in the obese group and 74,717 in the non-obese group. Both groups had a similar mean age range of 70 to 80 years, with prior stroke affecting 5 % of patients in each group. Additionally, the prevalence of prior myocardial infarction was 13 % to 15 % across the two groups.
A multitude of studies have indicated a potential protective effect of overweight and obesity against mortality in patients with pre-existing heart conditions, including coronary artery disease, atrial fibrillation, and heart failure, as well as those undergoing interventional procedures such as transcatheter aortic valve replacement (TAVR) and TEER for symptomatic MR [19], [28], [29], [30], [31], [32], [33], [34]. Although these studies primarily defined obesity as a BMI of 30 kg/m2 or higher, the consistency and underlying mechanisms of this paradoxical finding remain a subject of ongoing debate within the scientific community. To our knowledge, this meta-analysis is the first of its kind to comprehensively study the impact of BMI on TEER outcomes. Our analysis did not reveal a significant difference in mortality rates between obese and non-obese patients (p = 0.427). However, upon conducting a subgroup analysis, a nuanced picture emerged. Notably, underweight patients demonstrated a significantly elevated risk of in-hospital mortality compared to both overweight (p = 0.006) and obese (p = 0.036) patients. Our results corroborate the findings of the MIVNUT registry study by Caneiro‐Queija et al., which demonstrated a significant link between moderate-severe malnutrition and adverse outcomes following TEER, including increased mortality and heart failure readmission [35]. Although the comparison between underweight and normal-weight individuals did not reach statistical significance (p = 0.216), the trend suggests a potentially increased risk, warranting further investigation in larger studies. These findings emphasize the importance of considering the entire BMI spectrum when evaluating patient risk and informing the development of tailored management strategies.
The “obesity paradox” refers to the unexpected finding that individuals who are overweight or obese, despite being at increased risk of developing heart disease, often exhibit better outcomes and lower mortality rates compared to normal-weight individuals once they have been diagnosed with a heart condition. Excess weight may serve as a protective factor in certain populations. This is particularly relevant for older, frail individuals with multiple health conditions, as increased body mass can potentially act as a nutritional reserve [36]. Furthermore, overweight and obese individuals might be better equipped to withstand the metabolic stress of acute cardiovascular events, surgeries, or interventions [36], [37], [38], [39], [40]. A recent systematic review by El-Andari et al. demonstrated a similar trend in heart valve surgery, where patients with higher BMI showed either favorable or comparable mortality rates at various timepoints compared to those with normal or low BMI, with the latter group tending to have worse outcomes [41]. Additionally, elevated BMI might confer protection against inflammation by influencing lipoprotein production [37]. It is important to note that BMI, while commonly used, may not be an ideal measure of adiposity. BMI does not distinguish between excess fat and lean muscle mass, meaning that individuals with higher BMI may have increased muscle mass rather than increased adiposity. This limitation may contribute to the observed 'obesity paradox,' as patients with greater muscle mass could experience better outcomes independent of their fat levels [42]. Some researchers have even proposed that normal weight in older populations with CVD may be an indicator of underlying, undetected health issues rather than a protective factor [37], [43], [44].
Approximately half of patients undergoing TEER procedures exhibit frailty [45], a condition characterized by decreased physical function and nutritional decline [46]. Frail patients are at significantly elevated risk of mortality and heart failure hospitalization compared to their counterparts [45]. Malnutrition, a core component of frailty assessment, likely contributed to the adverse outcomes observed in a substantial portion of the study population. Consequently, malnutrition, independent of MR treatment efficacy, may be a critical determinant of CVD outcomes in this patient cohort. Conversely, it is crucial to acknowledge that TEER procedures can effectively treat patients with both malnutrition and frailty [45]. Recognizing the heightened in-hospital mortality risk among underweight patients undergoing TEER necessitates a paradigm shift in patient care. Comprehensive preoperative evaluations, including nutritional assessment and risk stratification, are essential for identifying vulnerable individuals. Existing research supports the beneficial impact of nutritional interventions on hospitalized patients, with potential reductions in length of stay and readmission rates [47].
While myocardial infarction rates remained consistent across BMI groups, a non-significant trend toward decreased stroke risk was observed in obese patients. This potential protective effect against stroke might be attributed to factors such as altered metabolic or coagulation profiles associated with obesity. However, the absence of statistical significance precludes definitive conclusions.
5. Limitations
This study provides a thorough review of the literature; however, it has some limitations. First, the observational nature of the included studies increases the risk of bias due to confounding factors. Second, the relatively small number of studies, combined with underpowered outcomes, could affect the reliability of the effect estimate. Third, we observed high heterogeneity in all outcomes, which we attempted to address via sensitivity analyses. However, this could introduce variability and affect the reliability of the results. Fourth, no studies were found that examined the effect of BMI on procedural outcomes of TEER in patients with TR, which limits the generalizability of our results to this population. Lastly, our study did not stratify patients based on prevailing co-morbidities, which may influence the outcomes.
6. Conclusion
In conclusion, our study found no significant association between obesity and in-hospital mortality when comparing obese and non-obese groups. However, subgroup analyses indicated a potential increased risk of in-hospital mortality among underweight individuals compared to overweight and obese patients. These findings suggest that underweight status may pose a greater risk than obesity for in-hospital mortality. Additionally, we found no substantial differences in myocardial infarction or stroke rates between obese and non-obese individuals. Further research is needed to investigate the factors linking increased hospital mortality to underweight status and the impact of BMI on long-term outcomes in TEER patients.
CRediT authorship contribution statement
Aman Goyal: Writing – review & editing, Writing – original draft, Software, Methodology, Formal analysis, Data curation, Conceptualization. Surabhi Maheshwari: Writing – review & editing, Writing – original draft, Software, Formal analysis, Data curation, Conceptualization. Muhammad Daoud Tariq: Writing – original draft, Methodology, Investigation, Formal analysis, Data curation. Eeshal Zulfiqar: Writing – review & editing, Writing – original draft, Software, Methodology, Investigation, Formal analysis. Abdul Moiz Khan: Writing – original draft, Methodology, Formal analysis, Data curation. Humza Saeed: Writing – review & editing, Writing – original draft, Methodology, Formal analysis, Data curation. Mohamed Daoud: Writing – review & editing, Writing – original draft, Validation, Supervision, Methodology, Conceptualization. Gauranga Mahalwar: Writing – review & editing, Writing – original draft, Validation, Supervision, Methodology, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors have no acknowledgements to declare.
Funding
None.
Ethical considerations
No ethical approval was required for this study design, as all data were obtained from publicly available sources.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijcha.2024.101519.
Contributor Information
Aman Goyal, Email: amanmgy@gmail.com.
Surabhi Maheshwari, Email: maheshwarisurabhi24@gmail.com.
Muhammad Daoud Tariq, Email: dawoodch258@gmail.com.
Eeshal Zulfiqar, Email: eeshalzulfiqar12@gmail.com.
Abdul Moiz Khan, Email: abdulmoizkhanali@gmail.com.
Humza Saeed, Email: hamzasaeed309@gmail.com.
Mohamed Daoud, Email: drmohameddaoudmd@gmail.com.
Gauranga Mahalwar, Email: mahalwg@ccf.org.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Nkomo V.T., Gardin J.M., Skelton T.N., Gottdiener J.S., Scott C.G., Enriquez-Sarano M. Burden of valvular heart diseases: a population-based study. LancetLond Engl. 2006;368(9540):1005–1011. doi: 10.1016/S0140-6736(06)69208-8. [DOI] [PubMed] [Google Scholar]
- 2.Enriquez-Sarano M., Akins C.W., Vahanian A. Mitral regurgitation. LancetLond Engl. 2009;373(9672):1382–1394. doi: 10.1016/S0140-6736(09)60692-9. [DOI] [PubMed] [Google Scholar]
- 3.Hahn R.T. Tricuspid regurgitation. N Engl J Med. 2023;388(20):1876–1891. doi: 10.1056/NEJMra2216709. [DOI] [PubMed] [Google Scholar]
- 4.Dziadzko V., Clavel M.A., Dziadzko M., Medina-Inojosa J.R., Michelena H., Maalouf J., et al. Outcome and undertreatment of mitral regurgitation: a community cohort study. LancetLond Engl. 2018;391(10124):960–969. doi: 10.1016/S0140-6736(18)30473-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zack C.J., Fender E.A., Chandrashekar P., Reddy Y.N.V., Bennett C.E., Stulak J.M., et al. National trends and outcomes in isolated tricuspid valve surgery. J Am Coll Cardiol. 2017;70(24):2953–2960. doi: 10.1016/j.jacc.2017.10.039. [DOI] [PubMed] [Google Scholar]
- 6.Rodés-Cabau J., Hahn R.T., Latib A., Laule M., Lauten A., Maisano F., et al. Transcatheter therapies for treating tricuspid regurgitation. J Am Coll Cardiol. 2016;67(15):1829–1845. doi: 10.1016/j.jacc.2016.01.063. [DOI] [PubMed] [Google Scholar]
- 7.Feldman T., Kar S., Elmariah S., Smart S.C., Trento A., Siegel R.J., et al. Randomized comparison of percutaneous repair and surgery for mitral regurgitation: 5-year results of EVEREST II. J Am Coll Cardiol. 2015;66(25):2844–2854. doi: 10.1016/j.jacc.2015.10.018. [DOI] [PubMed] [Google Scholar]
- 8.Goyal A., Sulaiman S.A., Pancholi V., Jain H., Daoud M., Sohail A.H. Celebrating a breakthrough: FDA greenlights TriClip G4 for tricuspid regurgitation: an editorial. Int J Surg. 2024;110(9):5317. doi: 10.1097/JS9.0000000000001628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nishimura R.A., Otto C.M., Bonow R.O., Carabello B.A., Erwin J.P., Fleisher L.A., et al. 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with Valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135(25) doi: 10.1161/CIR.0000000000000503. e1159–95. [DOI] [PubMed] [Google Scholar]
- 10.Braun D., Orban M., Nabauer M., Orban M., Gross L., Englmaier A., et al. Transcatheter treatment of severe tricuspid regurgitation using the edge-to-edge repair technique in the presence and absence of pacemaker leads. JACC Cardiovasc Interv. 2017;10(19):2014–2016. doi: 10.1016/j.jcin.2017.07.010. [DOI] [PubMed] [Google Scholar]
- 11.von Bardeleben R.S., Hobohm L., Kreidel F., Ostad M.A., Schulz E., Konstantinides S., et al. Incidence and in-hospital safety outcomes of patients undergoing percutaneous mitral valve edge-to-edge repair using MitraClip: five-year German national patient sample including 13,575 implants. EuroIntervention J Eur Collab Work Group Interv Cardiol Eur Soc Cardiol. 2019;14(17):1725–1732. doi: 10.4244/EIJ-D-18-00961. [DOI] [PubMed] [Google Scholar]
- 12.Goyal A, Sulaiman SA, Safi D, Mehta K, Jain H, Jain J, et al. Transcatheter edge-to-edge repair in valvular heart disease: a comprehensive exploration of equipment, efficacy, gender, racial, and socioeconomic disparities, and future prospects. Cardiol Rev. doi: 10.1097/CRD.0000000000000742. [DOI] [PubMed]
- 13.Bedogni F., Testa L., Rubbio A.P., Bianchi G., Grasso C., Scandura S., et al. Real-world safety and efficacy of transcatheter mitral valve repair with mitraclip: thirty-day results from the italian society of interventional cardiology (GIse) registry of transcatheter treatment of mitral valve RegurgitaTiOn (GIOTTO) Cardiovasc Revascularization Med. Mol. Interv. 2020;21(9):1057–1062. doi: 10.1016/j.carrev.2020.01.002. [DOI] [PubMed] [Google Scholar]
- 14.Otto C.M., Nishimura R.A., Bonow R.O., Carabello B.A., Erwin J.P., Gentile F., et al. 2020 ACC/AHA guideline for the management of patients with Valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;143(5):e35–e71. doi: 10.1161/CIR.0000000000000932. [DOI] [PubMed] [Google Scholar]
- 15.Puls M., Lubos E., Boekstegers P., von Bardeleben R.S., Ouarrak T., Butter C., et al. One-year outcomes and predictors of mortality after MitraClip therapy in contemporary clinical practice: results from the German transcatheter mitral valve interventions registry. Eur Heart J. 2016;37(8):703–712. doi: 10.1093/eurheartj/ehv627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keller K., Hobohm L., Geyer M., Kreidel F., Ostad M.A., Lavie C.J., et al. Impact of obesity on adverse in-hospital outcomes in patients undergoing percutaneous mitral valve edge-to-edge repair using MitraClip® procedure - Results from the German nationwide inpatient sample. Nutr Metab Cardiovasc Dis NMCD. 2020;30(8):1365–1374. doi: 10.1016/j.numecd.2020.04.009. [DOI] [PubMed] [Google Scholar]
- 17.Schenkeveld L., Magro M., Oemrawsingh R.M., Lenzen M., de Jaegere P., van Geuns R.J., et al. The influence of optimal medical treatment on the “obesity paradox”, body mass index and long-term mortality in patients treated with percutaneous coronary intervention: a prospective cohort study. BMJ Open. 2012;2(1):e000535. doi: 10.1136/bmjopen-2011-000535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Amundson D.E., Djurkovic S., Matwiyoff G.N. The obesity paradox. Crit Care Clin. 2010;26(4):583–596. doi: 10.1016/j.ccc.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 19.Kalbacher D., Tigges E., Boekstegers P., Puls M., Plicht B., Eggebrecht H., et al. Underweight is associated with inferior short and long-term outcomes after MitraClip implantation: results from the German TRAnscatheter mitral valve interventions (TRAMI) registry. Am. Heart J. 2020;222:73–82. doi: 10.1016/j.ahj.2019.12.022. [DOI] [PubMed] [Google Scholar]
- 20.Elagizi A., Kachur S., Lavie C.J., Carbone S., Pandey A., Ortega F.B., et al. An Overview and Update on Obesity and the Obesity Paradox in Cardiovascular Diseases. Prog Cardiovasc Dis. 2018;61(2):142–150. doi: 10.1016/j.pcad.2018.07.003. [DOI] [PubMed] [Google Scholar]
- 21.Moher D., Shamseer L., Clarke M., Ghersi D., Liberati A., Petticrew M., et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wells G, Shea B, O’Connell D, Robertson J, Peterson J, Welch V, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta- Analysis.
- 23.Higgins J.P.T., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Keller K., Geyer M., Hobohm L., Tamm A.R., Kreidel F., Ruf T.F., et al. Survival benefit of overweight patients undergoing MitraClip® procedure in comparison to normal-weight patients. Clin Cardiol. 2022;45(12):1236–1245. doi: 10.1002/clc.23897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Agarwal S., Bansal A., Krishan S., Akhtar K., Khosla J., Baber U. Impact of obesity on outcomes in patients undergoing transcatheter mitral valve repair with MitraClip. Am J Cardiol. 2023;1(200):47–49. doi: 10.1016/j.amjcard.2023.04.015. [DOI] [PubMed] [Google Scholar]
- 26.Shamaki GR, Markson F, Idemudia O, Murphy A, Bob-Manuel T, Antia A, et al. The prevalence and impact of obesity on the outcomes of patients undergoing transcatheter mitral valve repair using MitraClip - a national inpatient sample analysis 2016 to 2020. Adv. Clin. Med. Res. Healthc Deliv. [Internet]. 2023 Nov 27 3(4). Available from: https://scholar.rochesterregional.org/advances/vol3/iss4/5.
- 27.Park D., Lee J.H., Han S. Underweight: another risk factor for cardiovascular disease?: a cross-sectional 2013 Behavioral Risk Factor Surveillance System (BRFSS) study of 491,773 individuals in the USA. Medicine (Baltimore). 2017;96(48):e8769. doi: 10.1097/MD.0000000000008769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chrysant S.G., Chrysant G.S. New insights into the true nature of the obesity paradox and the lower cardiovascular risk. J. Am. Soc. Hypertens JASH. 2013;7(1):85–94. doi: 10.1016/j.jash.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 29.Gurm H.S., Whitlow P.L., Kip K.E., Investigators B.A.R.I. The impact of body mass index on short- and long-term outcomes inpatients undergoing coronary revascularization. Insights from the bypass angioplasty revascularization investigation (BARI) J Am Coll Cardiol. 2002;39(5):834–840. doi: 10.1016/s0735-1097(02)01687-x. [DOI] [PubMed] [Google Scholar]
- 30.Mehta L., Devlin W., McCullough P.A., O’Neill W.W., Skelding K.A., Stone G.W., et al. Impact of body mass index on outcomes after percutaneous coronary intervention in patients with acute myocardial infarction. Am J Cardiol. 2007;99(7):906–910. doi: 10.1016/j.amjcard.2006.11.038. [DOI] [PubMed] [Google Scholar]
- 31.Romero-Corral A., Montori V.M., Somers V.K., Korinek J., Thomas R.J., Allison T.G., et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. LancetLond Engl. 2006;368(9536):666–678. doi: 10.1016/S0140-6736(06)69251-9. [DOI] [PubMed] [Google Scholar]
- 32.Konigstein M., Havakuk O., Arbel Y., Finkelstein A., Ben-Assa E., Leshem Rubinow E., et al. The obesity paradox in patients undergoing transcatheter aortic valve implantation. Clin Cardiol. 2015;38(2):76–81. doi: 10.1002/clc.22355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Horwich T.B., Fonarow G.C., Hamilton M.A., MacLellan W.R., Woo M.A., Tillisch J.H. The relationship between obesity and mortality in patients with heart failure. J Am Coll Cardiol. 2001;38(3):789–795. doi: 10.1016/s0735-1097(01)01448-6. [DOI] [PubMed] [Google Scholar]
- 34.Lavie C.J., Alpert M.A., Arena R., Mehra M.R., Milani R.V., Ventura H.O. Impact of obesity and the obesity paradox on prevalence and prognosis in heart failure. JACC Heart Fail. 2013;1(2):93–102. doi: 10.1016/j.jchf.2013.01.006. [DOI] [PubMed] [Google Scholar]
- 35.Caneiro-Queija B., Raposeiras-Roubin S., Adamo M., Freixa X., Arzamendi D., Benito-González T., et al. Prognostic impact of nutritional status after transcatheter edge-to-edge mitral valve repair: the MIVNUT registry. J. Am. Heart Assoc. 2022;11(20):e023121. doi: 10.1161/JAHA.121.023121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Keller K., Hobohm L., Geyer M., Münzel T., Lavie C.J., Ostad M.A., et al. Obesity paradox in peripheral artery disease. Clin Nutr Edinb Scotl. 2019;38(5):2269–2276. doi: 10.1016/j.clnu.2018.09.031. [DOI] [PubMed] [Google Scholar]
- 37.Bucholz EM, Beckman AL, Krumholz HA, Krumholz HM, Dr. Bucholz was affiliated with the Yale School of Medicine and Yale School of Public Health during the time that the work was conducted. Excess weight and life expectancy after acute myocardial infarction: The obesity paradox reexamined. Am. Heart J. 2016 172:173–81. [DOI] [PMC free article] [PubMed]
- 38.Angerås O., Albertsson P., Karason K., Råmunddal T., Matejka G., James S., et al. Evidence for obesity paradox in patients with acute coronary syndromes: a report from the Swedish Coronary Angiography and Angioplasty Registry. Eur Heart J. 2013;34(5):345–353. doi: 10.1093/eurheartj/ehs217. [DOI] [PubMed] [Google Scholar]
- 39.Lavie C.J., De Schutter A., Parto P., Jahangir E., Kokkinos P., Ortega F.B., et al. Obesity and prevalence of cardiovascular diseases and prognosis-the obesity paradox updated. Prog Cardiovasc Dis. 2016;58(5):537–547. doi: 10.1016/j.pcad.2016.01.008. [DOI] [PubMed] [Google Scholar]
- 40.Keller K., Münzel T., Ostad M.A. Sex-specific differences in mortality and the obesity paradox of patients with myocardial infarction ages >70 y. Nutr. Burbank Los Angel City Calif. 2018;46:124–130. doi: 10.1016/j.nut.2017.09.004. [DOI] [PubMed] [Google Scholar]
- 41.El-Andari R., Bozso S.J., Kang J.J.H., Bedard A.M.A., Adams C., Wang W., et al. Heart valve surgery and the obesity paradox: a systematic review. Clin. Obes. 2022;12(2):e12506. doi: 10.1111/cob.12506. [DOI] [PubMed] [Google Scholar]
- 42.Sweatt K., Garvey W.T., Martins C. Strengths and limitations of BMI in the diagnosis of obesity: what is the path forward? Curr. Obes. Rep. 2024;13(3):584–595. doi: 10.1007/s13679-024-00580-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Das S.R., Alexander K.P., Chen A.Y., Powell-Wiley T.M., Diercks D.B., Peterson E.D., et al. Impact of body weight and extreme obesity on the presentation, treatment, and in-hospital outcomes of 50,149 patients with ST-Segment elevation myocardial infarction results from the NCDR (National Cardiovascular Data Registry) J Am Coll Cardiol. 2011;58(25):2642–2650. doi: 10.1016/j.jacc.2011.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McAuley P.A., Beavers K.M. Contribution of cardiorespiratory fitness to the obesity paradox. Prog Cardiovasc Dis. 2014;56(4):434–440. doi: 10.1016/j.pcad.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 45.Metze C., Matzik A.S., Scherner M., Körber M.I., Michels G., Baldus S., et al. Impact of frailty on outcomes in patients undergoing percutaneous mitral valve repair. JACC Cardiovasc Interv. 2017;10(19):1920–1929. doi: 10.1016/j.jcin.2017.07.042. [DOI] [PubMed] [Google Scholar]
- 46.Fried L.P., Tangen C.M., Walston J., Newman A.B., Hirsch C., Gottdiener J., et al. Frailty in older adults: evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001;56(3) doi: 10.1093/gerona/56.3.m146. M146 M156. [DOI] [PubMed] [Google Scholar]
- 47.Bally M.R., Blaser Yildirim P.Z., Bounoure L., Gloy V.L., Mueller B., Briel M., et al. Nutritional support and outcomes in malnourished medical inpatients: a systematic review and meta-analysis. JAMA Intern. Med. 2016;176(1):43–53. doi: 10.1001/jamainternmed.2015.6587. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.