Abstract
Background
In Shenzhen of China, the continuous increase of syphilis infections threatens the safety of blood transfusion. In 2020, COVID-19 was discovered and spread rapidly around the world, and affected the prevalence of syphilis among blood donors.
Methods
From 2013 to 2020, there were 839,161 blood samples collected in the Shenzhen Blood Center. Blood samples were screened by ELISA tests and confirmed by the TPPA (Treponema pallidum particle agglutination) tests and the TRUST (toluidine red unheated serum tests). All data was analyzed by the chi-square test.
Results
From 2013 to 2020, the positive rate of syphilis among blood donors varied significantly among individuals in different ages, educational backgrounds, regions, and blood donation histories (P<0.001). In 2020, It was the first time that there were more repeat blood donors than first-time blood donors and more blood donors with a higher education level than those with a lower education level, and the lowest reactive and positive rate of syphilis among blood donors was observed. Compared to 2019, the prevalence of syphilis among female and repeat blood donors decreased significantly in 2020 (P<0.01).
Conclusion
The prevalence of syphilis in blood donors is related to the characteristics of blood donors (in addition to gender) and the COVID-19 epidemic. COVID-19 can affect the prevalence of syphilis among blood donors by influencing the composition of blood donors and the number of syphile-positive donors in certain blood donors, including female and repeat blood donors.
Keywords: syphilis, COVID-19, blood donors
Introduction
COVID-19 (Coronavirus disease 2019) is a new type of respiratory disease with high morbidity and mortality rates. It first occurred in Wuhan, China, and quickly spread to more than 200 countries.1,2 Many countries have taken action to close non-essential business, prohibit non-essential rallies, and limit the use of public transportation to reduce the spread of SARS-CoV-2.3 To control the spread of COVID-19, Chinese government had implemented strict lockdown measures, which resulted in a large reduction in anthropogenic activities and found it difficult to carry out volunteer blood donation activities. Currently, little research has focused on the influence of the COVID-19 on blood donation,4,5 and the prevalence of transfusive-transmitted infectious diseases, such like syphilis.6–8
Syphilis is known to be a contagious disease caused by T. pallidum (Treponema pallidum) and can be transmitted through sexual contact, blood transfusion, or vertical transmission during pregnancy. Syphilis continues to be a pervasive global public health problem with a high prevalence.9,10 In 2020, the incidence and mortality of syphilis in China were 33.0831/100 000 and 0.0038/100 000, respectively.11 Syphilis infections are a major health concern in terms of the accessibility, quality, and safety of blood transfusion. It have been reported that the prevalence of syphilis among blood donors is related to a number of factors.
Here, we observed the positive rate of syphilis among blood donors in Shenzhen from 2013 to 2020 to explore the related factors, which can provide the basis for reducing the risk of syphilis transmission through blood transfusion especially when there’s a pandemic.
Materials and Methods
From 2013 to 2020, there were 635,836 blood donors in the Shenzhen Blood Center participating in this project, and the inclusion and exclusion criteria was shown in the Supplementary Figure 1. Whole blood was collected in a 5mL dipotassium ethylenediaminetetraacetate anticoagulation tube. All specimens were stored at 4°C and the plasma was tested the next day. This study complied with the Declaration of Helsinki was approved by the Medical Ethics Committee of Shenzhen Blood Center (SZBC-2020-0011, Date of approval: November 9, 2020). The informed consent was obtained from all subjects, and all methods were carried out in accordance with relevant guidelines and regulations.
Initial tests for syphilis were performed on 839,161 samples in the Shenzhen Blood Center using two ELISA kits (Diagnostic Kit for Antibody to Treponema pallidum, Diasorin S.p.A. UK Branch. Diagnostic Kit for Antibody to Treponema pallidum, Beijing Wantai Biological Pharmacy Enterprise Co., Ltd). Non-reactive samples were confirmed as syphilis-negative samples. Samples tested reactive underwent TPPA and the TRUST tests for confirmation in the Shenzhen Chronic Disease Prevention Center. Some samples which the results of TPPA and the TRUST tests showed positive were confirmed as syphilis-positive samples and the others tested non-reactive were confirmed as initial screening reactive samples. In summary, samples tested positive for syphilis when ELISA, TPPA and TRUST tests all showed reactivity.
The reactive rate was that the number of samples which were reactivity in any of ELISA experiments divided by the number of samples. The positive rate was that the number of blood donors who tested positive in ELISA, TPPA and TRUST experiments divided by the number of blood donors.
The prevalence of one group was that the number of blood donors who tested positive for syphilis in this group divided by the total number of this group. All data were analyzed by the chi-squared test for independence in SPSS 25.0 software.
Results
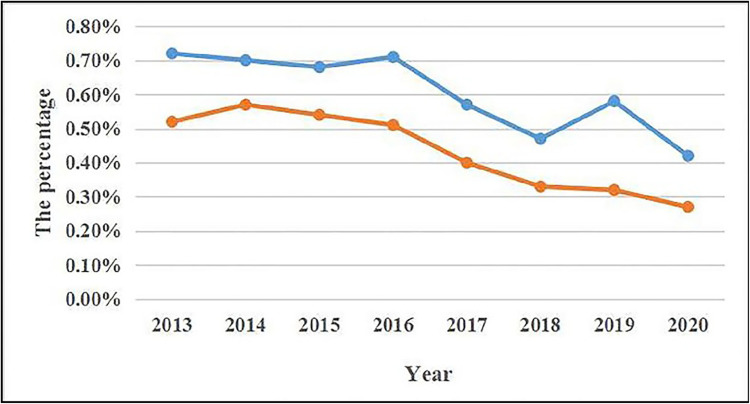
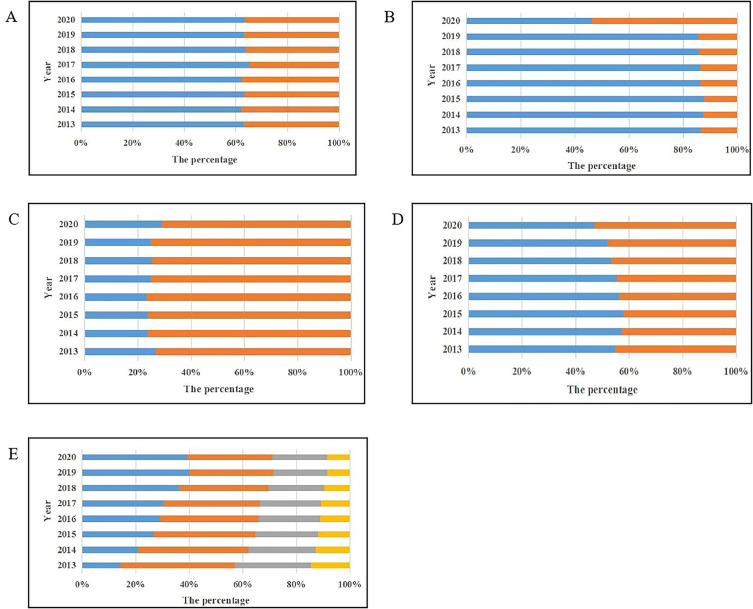
In Figure 1, we can see that from 2013 to 2020, the lowest reactive and positive rate of syphilis is observed in 2020, which may be due to changes in the composition of the blood donors in 2020. In Figure 2, from 2013 to 2019, male, non-local, younger than 40 years old, less than university education, first-time blood donors accounted for a higher percentage (>50%) of the total number of blood donors. The highest proportion of blood donors with a higher education level, local blood donors and repeat blood donors was observed in 2020. For the first time, the proportion of repeat blood donors or blood donors with a higher education level exceeded 50%. This may prove that COVID-19 may affect the positive rate of syphilis in blood donors by influencing the composition of blood donors.
Figure 1.
The reactive and positive rate of syphilis from 2013 to 2020. The blue line shows the reactive rate of syphilis from 2013 to 2020, and the orange line shows the positive rate of syphilis from 2013 to 2020.
Figure 2.
The percentage of blood donors with different characteristics from 2013 to 2020. (A) The percentage of female and male blood donors from 2013 to 2020. Blue represents male blood donors and orange represents female blood donors. (B) The percentage of first-time and repeat blood donors from 2013 to 2020. Blue represents first-time blood donors and orange represents repeat blood donors. (C) The percentage of local and foreign blood donors from 2013 to 2020. Blue represents local blood donors and orange represents foreign blood donors. (D): The percentage of blood donors with different education level from 2013 to 2020. Blue represents blood donors with a lower education level and orange represents blood donors with a higher education level. (E) The percentage of blood donors aged 18–60 years old from 2013 to 2020. Blue represents donors aged 18 to 29 years old, orange represents donors aged 30 to 39 years old, grey represents donors aged 40 to 49 years old, and yellow represents donors aged 50 to 60 years old.
In the past eight years (Table 1), the prevalence of syphilis among foreigners was higher than that of locals (P<0.001), blood donors with a lower education level higher than those with a higher education level (P<0.001), and first-time blood donors higher than that of repeat blood donors (P<0.001). In addition, the prevalence of syphilis varied among different age groups significantly (P<0.001). However, for three years, there was no difference in the positive rate of syphilis between male and female blood donors (P>0.05). It indicates that in addition to gender, the blood donation history, educational background and age of blood donors are related to syphilis infection among blood donors.
Table 1.
The Prevalence of Syphilis Among Blood Donors
| Group | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Gender | Male | Positive | 187 | 222 | 228 | 235 | 187 | 172 | 159 | 165 |
| Total | 40384 | 42,363 | 46,024 | 48,304 | 54,322 | 53,969 | 58,035 | 59,092 | ||
| Prevalence | 0.46% | 0.52% | 0.50% | 0.49% | 0.34% | 0.32% | 0.27% | 0.28% | ||
| Female | Positive | 149 | 165 | 166 | 157 | 141 | 105 | 133 | 89 | |
| Total | 23678 | 25,967 | 26,883 | 29,297 | 28,649 | 30,824 | 34,060 | 33,980 | ||
| Prevalence | 0.63% | 0.64% | 0.62% | 0.54% | 0.49% | 0.34% | 0.39% | 0.26% | ||
| χ2 | 7.904 | 3.546 | 4.707 | 0.885 | 10.423 | 0.261 | 9.219 | 0.237 | ||
| P value | 0.005 | 0.060 | 0.030 | 0.347 | 0.001 | 0.609 | 0.002 | 0.626 | ||
| Region | Local | Positive | 45 | 50 | 45 | 66 | 55 | 43 | 36 | 37 |
| Total | 17073 | 16,207 | 17,417 | 17,969 | 20,667 | 21,393 | 22,759 | 26,967 | ||
| Prevalence | 0.26% | 0.31% | 0.26% | 0.37% | 0.27% | 0.20% | 0.16% | 0.14% | ||
| Foreign | Positive | 291 | 337 | 349 | 326 | 273 | 234 | 256 | 217 | |
| Total | 46860 | 52,034 | 55,396 | 59,488 | 62,193 | 63,377 | 69,262 | 66,110 | ||
| Prevalence | 0.62% | 0.65% | 0.63% | 0.55% | 0.44% | 0.37% | 0.37% | 0.33% | ||
| χ2 | 30.579 | 25.207 | 34.006 | 8.950 | 11.752 | 13.896 | 24.210 | 25.685 | ||
| P value | <0.001 | <0.001 | <0.001 | 0.003 | 0.001 | <0.001 | <0.001 | <0.001 | ||
| Donation history | First-time | Positive | 311 | 361 | 370 | 370 | 302 | 260 | 273 | 229 |
| Total | 55358 | 59,699 | 63,858 | 66,965 | 71,651 | 72,771 | 78,802 | 43,012 | ||
| Prevalence | 0.56% | 0.60% | 0.58% | 0.55% | 0.42% | 0.36% | 0.35% | 0.53% | ||
| Repeat | Positive | 25 | 26 | 24 | 22 | 26 | 17 | 19 | 25 | |
| Total | 8704 | 8631 | 9049 | 10,636 | 11,320 | 12,022 | 13,293 | 50,065 | ||
| Prevalence | 0.29% | 0.30% | 0.27% | 0.21% | 0.23% | 0.14% | 0.14% | 0.05% | ||
| χ2 | 10.868 | 12.331 | 14.556 | 21.822 | 9.134 | 14.767 | 14.904 | 197.891 | ||
| P value | 0.001 | <0.001 | <0.001 | <0.001 | 0.003 | <0.001 | <0.001 | <0.001 | ||
| Education level | Lower | Positive | 233 | 288 | 308 | 295 | 248 | 207 | 218 | 191 |
| Total | 35061 | 38,983 | 42,131 | 43,670 | 44,792 | 45,103 | 47,924 | 43,447 | ||
| Prevalence | 0.80% | 0.98% | 1.00% | 0.87% | 0.65% | 0.52% | 0.45% | 0.44% | ||
| Higher | Positive | 103 | 99 | 86 | 97 | 80 | 70 | 74 | 63 | |
| Total | 28972 | 29,337 | 30,772 | 33,913 | 38,164 | 39,685 | 44,160 | 49,304 | ||
| Prevalence | 0.29% | 0.25% | 0.20% | 0.22% | 0.18% | 0.16% | 0.17% | 0.13% | ||
| χ2 | 29.025 | 47.868 | 67.465 | 57.665 | 61.936 | 51.760 | 60.020 | 82.235 | ||
| P value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||
| Age | 18–29 | Positive | 82 | 102 | 101 | 93 | 64 | 74 | 66 | 65 |
| Total | 9124 | 14,208 | 19,309 | 22,431 | 25,174 | 30,674 | 36,741 | 36,381 | ||
| Prevalence | 0.90% | 0.72% | 0.52% | 0.41% | 0.25% | 0.24% | 0.18% | 0.18% | ||
| 30–39 | Positive | 138 | 147 | 137 | 132 | 107 | 83 | 82 | 65 | |
| Total | 27513 | 28,234 | 27,840 | 28,718 | 29,815 | 28,374 | 28,997 | 29,751 | ||
| Prevalence | 0.50% | 0.52% | 0.49% | 0.46% | 0.36% | 0.29% | 0.28% | 0.22% | ||
| 40–49 | Positive | 100 | 118 | 128 | 139 | 122 | 89 | 95 | 90 | |
| Total | 18126 | 17,193 | 17,159 | 17,842 | 18,898 | 17,652 | 18,444 | 18,914 | ||
| Prevalence | 0.55% | 0.69% | 0.75% | 0.78% | 0.65% | 0.50% | 0.52% | 0.48% | ||
| 50–60 | Positive | 16 | 20 | 28 | 28 | 35 | 31 | 49 | 34 | |
| Total | 9299 | 8695 | 8599 | 8610 | 9084 | 8093 | 7913 | 7995 | ||
| Prevalence | 0.17% | 0.23% | 0.33% | 0.33% | 0.39% | 0.38% | 0.62% | 0.43% | ||
| χ2 | 47.163 | 28.702 | 22.187 | 37.024 | 43.812 | 25.765 | 68.773 | 50.532 | ||
| P value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||
Notes: The prevalence among different groups of blood donors= Positive number of this group/Total number of this group.
When the COVID-19 epidemic in Shenzhen (in 2020), the prevalence of syphilis among female blood donors and repeat blood donors decreased compared with 2019 (Table 2, P<0.01), and the prevalence of syphilis among first-time blood donors in 2020 increased (Table 2, P<0.001). However, when comparing 2019 with 2020, we did not find any significant differences in the prevalence of syphilis among blood donors of different ages, education backgrounds and regions (Table 2, P>0.05). It suggests that in addition to the factors mentioned above, syphilis infection rates in certain groups of blood donors can be affected when there is a new epidemic.
Table 2.
The Prevalence of Syphilis among Different Blood Donors from 2019 to 2020
| Group | Syphilis Status | 2019 | 2020 | P value | χ2 | OR | 95% CI | |
|---|---|---|---|---|---|---|---|---|
| Gender | Male | Positive | 159 | 165 | 0.864 | 0.029 | ||
| Negative | 57876 | 58,927 | ||||||
| Prevalence | 0.27% | 0.28% | ||||||
| Female | Positive | 133 | 89 | 0.003 | 8.646 | 0.670 | 0.512–0.877 | |
| Negative | 33927 | 33,891 | ||||||
| Prevalence | 0.39% | 0.26% | ||||||
| Region | Local | Positive | 36 | 37 | 0.543 | 0.370 | ||
| Negative | 22723 | 26,930 | ||||||
| Prevalence | 0.16% | 0.14% | ||||||
| Foreign | Positive | 256 | 217 | 0.197 | 1.663 | |||
| Negative | 69006 | 65,893 | ||||||
| Prevalence | 0.37% | 0.33% | ||||||
| Donation history | First-time | Positive | 273 | 229 | <0.001 | 23.448 | 1.540 | 1.291–1.836 |
| Negative | 78529 | 42,783 | ||||||
| Prevalence | 0.35% | 0.53% | ||||||
| Repeat | Positive | 19 | 25 | <0.001 | 13.090 | 0.349 | 0.192–0.634 | |
| Negative | 13274 | 50,040 | ||||||
| Prevalence | 0.14% | 0.05% | ||||||
| Education level | Lower | Positive | 218 | 191 | 0.730 | 0.119 | ||
| Negative | 47706 | 43,256 | ||||||
| Prevalence | 0.45% | 0.44% | ||||||
| Higher | Positive | 74 | 63 | 0.112 | 2.520 | |||
| Negative | 44086 | 49,241 | ||||||
| Prevalence | 0.17% | 0.13% | ||||||
| Age | 18–29 | Positive | 66 | 65 | 0.975 | 0.001 | ||
| Negative | 36675 | 36,316 | ||||||
| Prevalence | 0.18% | 0.18% | ||||||
| 30–39 | Positive | 82 | 65 | 0.119 | 2.433 | |||
| Negative | 28915 | 29,686 | ||||||
| Prevalence | 0.28% | 0.22% | ||||||
| 40–49 | Positive | 95 | 90 | 0.589 | 0.292 | |||
| Negative | 18349 | 18,824 | ||||||
| Prevalence | 0.52% | 0.48% | ||||||
| 50–60 | Positive | 49 | 34 | 0.090 | 2.883 | |||
| Negative | 7864 | 7961 | ||||||
| Prevalence | 0.62% | 0.43% | ||||||
In conclusion, the positive rate of syphilis was influenced not only by the characteristics of blood donors (in addition to gender), but also by COVID-19. One of the reasons for the impact of COVID-19 on the positive rate of syphilis may be that the composition of blood donors changed during the COVID-19 epidemic The other reason may be the decrease in syphilitic-positive blood donors in certain types of blood donors, including female blood donors and repeat blood donors. So, the overall positive rate of syphilis among blood donors was changed.
Discussion
In 2020, with the COVID-19 outbreak worldwide, the blood supply and blood donation activities were severely impacted.4,5 As usual, the reasons for not donating blood may be concerned about sterilization of equipment, unknown fears, and feeling weakness after donation.12 But with the outbreak of infectious diseases, people may be afraid of contracting infected diseases during blood donations, which makes blood donations more difficult than usual. In 2020, there was a decline in blood donations in many cities.13,14 But in our study, we found that the number of blood donors increased in 2020, but the characteristics of volunteer blood donors were different from that of the past several years. It may be related to the changes in the motivation of blood donation. Many blood donors may hope to contribute to the fight against the epidemic through blood donation.15
COVID-19 affected the number of blood donors with different characteristics, which can be found in our findings. It was the first time in 2020 that there were more repeat blood donors than first-time blood donors, more blood donors with a higher education level than those with a lower education level. It indicates that recruiting repeat blood donors and individuals with a higher-educated background can be easier when there is an infectious disease epidemic. In fact, COVID-19 can change not only the composition of blood donors, but also the prevalence of transfusion-transmitted diseases among blood donors.6–8
In Rome, the number of positive diagnoses of syphilis in 2020 decreased compared to 2017–2019.8 But in Brazil, the incidence rates of syphilis per million populations increased significantly during the COVID-19 pandemic.7 In Shenzhen, the prevalence of syphilis among volunteer blood donors declined in 2020. All of these suggest that COVID-19 has a different impact on syphilis prevalence in different countries.
In our study, the prevalence of syphilis among first-time blood donors showed a downward trend from 2013 to 2019 but rose from 0.35% in 2019 to 0.53% in 2020. It may indicate that COVID-19 affect the prevalence of syphilis among first blood donors. The reason may be that syphilis-infected individuals may worry that going to the hospital puts them at risk of contracting COVID-19.16,17 Therefore, they opted to participate in the blood donation to screen for syphilis, which was considered to be safer than go to the hospital. So, during the epidemic, hospitals should also pay attention to patients with other infectious diseases. It is very important to reinforce the advertising on the safety of the medical treatment and to ensure that these patients seek medical treatment in an orderly fashion.
However, repeat blood donors had the advantage of the lower prevalence of syphilis compared to first-time blood donors (P<0.01), which is consistent with studies in other countries.18 Especially for the 2020, the lowest prevalence of syphilis among repeat blood donors was observed. It may prove that the history of blood donations can be associated with the prevalence of syphilis and COVID-19 has an impact on the prevalence of syphilis among blood donors with different blood donation history. During the COVID-19 pandemic, the increase in the number of repeat blood donors and the decrease in the prevalence of syphilis could ensure blood supply and blood safety. Since repeat blood donations have certain limitations on the time of blood donation, it is necessary to recruit individuals with a higher education level to be blood donors.
It was reported that blood donors with a higher-educated level were more likely to overcome their fears and felt comfortable donating blood.12 The higher the educational experience, the more they can understand the importance of blood safety and self-protection. In our results, blood donors with a higher-educated level had a lower prevalence of syphilis compared to non-college-educated donors (P<0.001). The educational background of blood donors is a related factor affecting the positive rate of syphilis. Although the proportion of blood donors with different educational backgrounds changed in 2020, COVID-19 did not affect the positive rate of syphilis among blood donors with different educational backgrounds.
Many researchers found that the prevalence of syphilis among males was higher than females.19 But in our study, expect for 2016, 2018 and 2020, the prevalence of syphilis among females was higher than males in Shenzhen (P<0.05). Compared to that in 2019, the prevalence of syphilis in female blood donors in 2020 was lower (P<0.05). There is not enough evidence that the positive rate of syphilis is related to gender, but the positive rate of syphilis among female blood donors is indeed affected by COVID-19.
In recent years, the aging population has been a major threat to the blood supply in several countries,20,21 and the incidence of sexually transmitted diseases among the elderly has shown an increasing trend.22 In our study, we found that from 2013 to 2020, the positive rate of syphilis in blood donors of different ages was different, but the positive rate of syphilis in blood donors of different ages did not change significantly by the COVID-19. The age of the blood donor is indeed a relevant factor in the positive rate of syphilis, however, COVID-19 did not cause changes in syphilis positive rates among blood donors of different ages.
Since blood services are influenced by the specific environment, institutions of the country, and factors, such as epidemics, culture, and traditions.23,24 In Shenzhen, from 2013 to 2019, male blood donors, young blood donors, first-time blood donors, lower-educated blood donors, and foreign blood donors were the main components of volunteer blood donors, which was related to the demographic characteristics of Shenzhen. Owing to the ongoing demographic changes in Shenzhen, regular monitoring of the characteristics of blood donors should be implemented to allow for the better strategies in blood transfusion services. At present, the recruitment strategy for blood donors in Shenzhen is based on the characteristics of the population. Nevertheless, in our study, we believe that the recruitment strategy for blood donors will be adapted depending on the characteristics of transfusion-transmitted infections. Especially during the COVID-19 epidemic, the conversion of recruitment policy is more conducive to ensuring blood supply and safety. Therefore, it is necessary to study the related factors of infectious diseases in blood donors.
In conclusion, the prevalence of syphilis in blood donors is related to the characteristics of blood donors (in addition to gender) and the COVID-19 epidemic. COVID-19 can affect the prevalence of syphilis among blood donors by influencing the composition of blood donors and the number of syphile-positive donors in certain blood donors, including female and repeat blood donors. So, we believe that in general, the prevalence of syphilis is lower among repeat blood donors, highly educated individuals, and local individuals. Recruiting repeat blood donors, highly educated individuals, and local individuals is more conducive to preventing syphilis from entering the blood supply chain. When the COVID-19 epidemic, increased the number of repeat blood donors can reduce the prevalence of syphilis, which is more conducive to ensuring blood supply and blood safety.
Acknowledgments
We wish to acknowledge the Medical Ethics Committee of Shenzhen Blood Center for reviewing and approving all the procedures involved in this study. Special thanks to the staff of Tangshan Qiao Technology Co., Ltd. for helping us collect data. In addition, we thank Tong Li for her contribution to the experiment in this article. We also take this opportunity to thank all members of this project, for their commitment and contribution during the performance of this study. All authors thank the Shenzhen blood center for the permission to publish the finding.
Funding Statement
This study was financially supported by Shenzhen Key Discipline Project of Blood Transfusion Medicine (NO. SZXK070), the Sanming Project of Medicine in Shenzhen (NO. SZSM202311032) and the National Natural Science Foundation of China (NO. 82261138630).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflict of interest.
References
- 1.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Novel Coronavirus (2019-nCoV): situation Report, 3. 2020. Available online: https://apps.who.int/iris/bitstream/handle/10665/330762/nCoVsitrep23Jan2020-eng.pdf. accessed December 23,2020.
- 3.Kelso J, Milne G, Kelly H. Simulation suggests that rapid activation of social distancing can arrest epidemic development due to a novel strain of influenza. BMC Public Health. 2009;9(1):117. doi: 10.1186/1471-2458-9-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stanworth S, New H, Apelseth T, et al. Effects of the COVID-19 pandemic on supply and use of blood for transfusion. Lancet Haematol. 2020;7(10):e756–e764. doi: 10.1016/S2352-3026(20)30186-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rackimuthu S, Hunain R, Babar MS, Santos Costa AC D, Essar MY. Ramifications of coronavirus disease 2019 (COVID-19) on blood donation in Africa: challenges and solutions. Infect Control Hosp Epidemiol. 2022;43(12):1968–1969. doi: 10.1017/ice.2021.425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Braunstein S, Slutsker J, Lazar R, et al. Epidemiology of reported HIV and other sexually transmitted infections during the COVID-19 pandemic. J Infect Dis. 2021;224(5):798–803. doi: 10.1093/infdis/jiab319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maia C, Marques N, Dias V, et al. Epidemiological trends in notified syphilis diagnoses during the COVID-19 pandemic in Brazil. Sex Transm Infect. 2022;98(6):458. doi: 10.1136/sextrans-2021-055240 [DOI] [PubMed] [Google Scholar]
- 8.Latini A, Magri F, Giuliani E, et al. Continuing evidence that COVID-19 has influenced syphilis epidemiology in Rome. Sex Transm Infect. 2022;98(1):72. doi: 10.1136/sextrans-2021-055250 [DOI] [PubMed] [Google Scholar]
- 9.GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1211–1259. doi: 10.1016/S0140-6736(17)32154-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Newman L, Rowley J, Vander Hoorn S, et al. Global estimates of the prevalence and incidence of four curable sexually transmitted infections in 2012 based on systematic review and global reporting. PLoS One. 2015;10(12):e0143304. doi: 10.1371/journal.pone.0143304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Health Committee of People’s Republic of China. Epidemic situation of notifiable infectious diseases in China in 2020. Gazette Natl Health Comm PRC. 2021;3:18–20. [Google Scholar]
- 12.Baig M, Habib H, Haji AH, et al. Knowledge, misconceptions and motivations towards blood donation among university students in KSA. Pak J Med Sci. 2013;29(6):1295–1299. doi: 10.12669/pjms.296.4137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Loua A, Kasilo O, Nikiema J, et al. Impact of the COVID-19 pandemic on blood supply and demand in the WHO African Region. Vox Sang. 2021;116(7):774–784. doi: 10.1111/vox.13071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang Y, Han W, Pan L, et al. Impact of COVID-19 on blood centers in Zhejiang province China. Vox Sang. 2020;115(6):502–506. doi: 10.1111/vox.12931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weidmann C, Derstroff M, Klüter H, Oesterer M, Müller-Steinhardt M. Motivation, blood donor satisfaction and intention to return during the COVID-19 pandemic. Vox Sang. 2022;117(4):488–494. doi: 10.1111/vox.13212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tao J, Napoleon SC, Maynard MA, et al. Impact of the COVID-19 pandemic on sexually transmitted infection clinic visits. Sex Transm Dis. 2021;48(1):e5–e7. doi: 10.1097/OLQ.0000000000001306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Soares P, Leite A, Esteves S, et al. Factors associated with the patient’s decision to avoid healthcare during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(24):13239. doi: 10.3390/ijerph182413239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O’Brien SF, Drews SJ, Yi QL, et al. Monitoring syphilis serology in blood donors: is there utility as a surrogate marker of early transfusion transmissible infection behavioral risk? Transfusion. 2023;63(6):1195–1203. doi: 10.1111/trf.17393 [DOI] [PubMed] [Google Scholar]
- 19.Nawaz Z, Rasool M, Siddique A, et al. Prevalence and risk factors of Syphilis among blood donors of Punjab, Pakistan. Tropical Biomed. 2021;38(1):106–110. doi: 10.47665/tb.38.1.019 [DOI] [PubMed] [Google Scholar]
- 20.Roh J, Choi S, Kim S, et al. Blood Supply and demand in Korea: what is in store for the future? Yonsei Med Jl. 2020;61(5):400–405. doi: 10.3349/ymj.2020.61.5.400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu WJ, Chen YY, Hsu LI, Chen JW, Wei ST, Hou SM. An imbalance in blood collection and demand is anticipated to occur in the near future in Taiwan. J Formos Med Assoc. 2022;121(8):1610–1614. doi: 10.1016/j.jfma.2021.07.027 [DOI] [PubMed] [Google Scholar]
- 22.Wu X, Guan Y, Ye J, et al. Association between syphilis seroprevalence and age among blood donors in Southern China: an observational study from 2014 to 2017. BMJ open. 2019;9(11):e024393. doi: 10.1136/bmjopen-2018-024393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li L, Li K, Yan K, et al. The history and challenges of blood donor screening in China. Transfus Med Rev. 2017;31(2):89–93. doi: 10.1016/j.tmrv.2016.11.001 [DOI] [PubMed] [Google Scholar]
- 24.Dei-Adomakoh Y, Asamoah-Akuoko L, Appiah B, Yawson A, Olayemi E. Safe blood supply in sub-Saharan Africa: challenges and opportunities. Lancet Haematol. 2021;8(10):e770–e776. doi: 10.1016/S2352-3026(21)00209-X [DOI] [PubMed] [Google Scholar]