Abstract
Persistent air leak may complicate malignant disease of the thorax, causing significant morbidity and mortality. A 51‐year‐old male with a 30‐pack‐year history of smoking was diagnosed with metastatic esophageal carcinoma with invasion into the right upper lobe of the lung. He developed a large right hydropneumothorax complicated by empyema leading to persistent air leak despite the insertion of two chest drains. Computed Tomography imaging with 3‐dimensional reconstruction showed severe tracheal compression from the enlarging esophageal tumour as well as bronchopleural fistulas in the right upper lobe. Rigid bronchoscopy with metallic tracheal stenting was performed. This was followed by localization and quantification of air leak with an endobronchial collateral ventilation assessment system and a digital chest drain to guide endobronchial valve placement, in a single operative procedure. This novel combination of interventional bronchoscopy techniques enabled successful transition to an ambulatory chest drain and subsequent hospital discharge.
Keywords: collateral ventilation assessment system, digital chest drainage system, endobronchial valve, persistent air leak, tracheal stenting
We describe a novel technique of simultaneous tracheal stenting followed by localization and quantification of air leak with an endobronchial collateral ventilation assessment system and digital chest drain system to guide endobronchial valve placement in a single operative procedure. This successfully addressed a persistent air leak in a patient with metastatic esophageal carcinoma complicated by invasion into the lung, persistent air leak and empyema, allowing him to be discharged home successfully.
INTRODUCTION
Persistent air leak (PAL) complicating thoracic malignancy portends significant morbidity and mortality. 1 Surgery may be considered if initial management with chest tube drainage and pleurodesis fails. However, patients with advanced thoracic malignancy have limited physiological reserves and are often poor surgical candidates. 1 We describe our novel interventional management of a challenging case of metastatic esophageal carcinoma with bronchopleural fistula complicated by PAL and tracheal stenosis.
CASE REPORT
A 51‐year‐old Chinese male with a 30‐pack year smoking history presented with progressive dysphagia and weight loss. Esophagogastroduodenoscopy revealed an esophageal tumour 22 cm from the incisors, and biopsy confirmed squamous cell carcinoma. Fluorodeoxyglucose positron emission tomography‐computed tomography (FDG PET‐CT) scan revealed a hyper‐metabolic upper esophageal tumour invading into the right upper lobe (RUL) of the lung (Figure 1), with a thick‐walled cavity and multiple mediastinal‐hilar lymph nodes, confirming Stage IV (T4N1M1) esophageal carcinoma. He underwent palliative chemotherapy and esophageal stenting. He was planned for radiotherapy but developed worsening dyspnea, hypoxemia, and swinging fevers. CT Thorax revealed a new large right sided hydropneumothorax and chest drains were inserted. Pleural fluid demonstrated polymicrobial growth and he received broad‐spectrum antibiotics for empyema. This was complicated by PAL requiring prolonged chest tube drainage. Further evaluation with flexible bronchoscopy demonstrated purulent RUL secretions but no mucosal irregularities to suggest tracheoesophageal fistula (TEF). Repeat CT with three‐dimensional reconstruction demonstrated an enlarging esophageal tumour with severe tracheal compression, and bronchopleural fistulas (BPF) in the apical and anterior segments of the RUL (Figure 1). He then underwent rigid bronchoscopy with jet ventilation under general anaesthesia for tracheal stenting followed by deployment of endobronchial valves (EBV) to simultaneously address the tracheal stenosis and PAL. Pre‐operatively, a digital chest drainage system was connected, with air leak of 4000 mLs/min noted at −15 cmH20 of suction, which was maintained pre and intra‐operatively. Rigid bronchoscopy demonstrated severe long segment tracheal stenosis predominantly due to extrinsic compression from the esophageal mass. The endoluminal tumour was mechanically debulked with laser application for haemostasis, and a partially covered self‐expandable metallic stent was deployed (Figure 2). The rigid scope was then exchanged for an endotracheal tube, and ventilation switched to volume‐controlled mode via the anaesthetic machine. The balloon from the endobronchial collateral ventilation (CV) assessment system was used to sequentially occlude the RUL orifice (air leak decreased to 1000 mLs/min, cessation of airflow and negative pressure waveform noted), UL apical (air leak 2000 mLs/min, continuous negative pressure waveform noted), anterior (air leak 3000 mLs/min, ventilation waveform noted), and posterior segments (air leak 3000 mLs/min, ventilation waveform noted). This localized the air leak to the RUL, with significant contribution from the apical segment, demonstrated by airflow cessation and negative pressure waveform on the CV assessment system console (Figure 2) with corresponding drop in air leak on the digital chest drainage system. Four EBVs were sized and sequentially inserted into the apical (air leak decreased to 2300 mLs/min), anterior (air leak further decreased to 1800 mLs/min) and posterior segments (air leak further decreased to 620 mLs/min), achieving an overall improvement in air leak from 4000 to 600 mLs/min at −15 cmH20 of suction. The patient was extubated uneventfully, and the minimal residual air leak remained stable on chest drainage without suction. He was successfully transitioned to an ambulatory chest drain and discharged with home palliative care services as per his last wishes. He demised 2 months later without requiring further hospitalizations (Video 1).
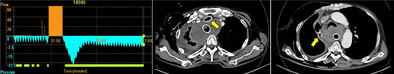
FIGURE 1.
From left to right: Axial cut of computed tomography of the thorax showing malignant fistulation between esophageal tumour and lung parenchyma (yellow arrow), followed by lung window images demonstrating suspicion of bronchopleural fistula at the apical subsegmental and anterior subsegmental branches of the right upper lobe bronchus (yellow arrows).
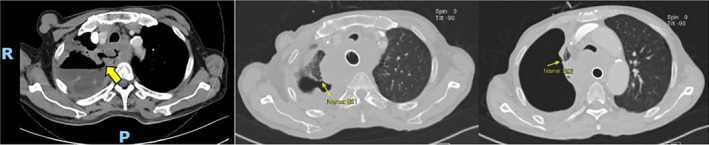
FIGURE 2.
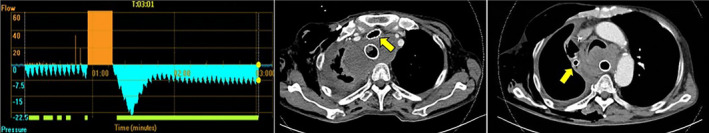
From left to right: Collateral ventilation system diagram demonstrating that intra‐operative occlusion of the right upper lobe orifice led to cessation of airflow and negative pressure waveform generated by inspiration and pleural suction, indicating air leak from the right upper lobe; followed by post‐operative computed tomography cuts demonstrating metallic tracheal stent and endobronchial valve in situ (yellow arrows).
VIDEO 1.
Intra‐operative video post metallic tracheal stenting demonstrating the use of the endobronchial collateral ventilation system to localize and quantify sites of air leak, followed by sizing and deployment of endobronchial valves. Embedded Video Placeholder: Post‐operative axial CT cut demonstrating metallic tracheal stent as well as endobronchial valve (yellow arrow) in‐situ.
DISCUSSION
Currently, there are a lack of guidelines to inform management of PAL. 1 Non‐surgical treatments including pleurodesis, autologous blood patch, sealants (e.g., fibrin spray and tissue glue injection), spigots and metal coils have had inconsistent results. 1 Bronchial valves (BV) include endobronchial valves and intrabronchial valves. These one‐way valves were first developed for bronchoscopic lung volume reduction (BLVR), but their use has expanded to encompass the management of PAL occurring after thoracic surgery, spontaneous secondary pneumothorax, empyema and advanced thoracic malignancy. 1 BV placement is an attractive minimally invasive and reversible option for non‐surgical candidates with PAL, significantly reducing air leak duration and length of stay compared to conservative management. 1 A recent meta‐analysis of BV for PAL found a pooled success rate of 82% (95% confidence intervals, 75–88; 95% prediction intervals, 64–92). The overall complication rate was 9.1%, with granulation tissue being the most common complication, followed by valve migration or expectoration and hypoxemia. 2 The endobronchial CV assessment system was initially developed to assess collateral ventilation during BLVR, 3 and has shown efficacy in shortening the time to air leak resolution during EBV placement for PAL in a recent case series. 4 The digital chest drainage system presents an objective method of air leak quantification compared to visual inspection of the bubble rate in a traditional underwater seal pleural drainage system. It demonstrated significant reduction in the duration of chest tube placement and length of hospital stay in post thoracic surgery patients with PAL compared with the traditional chest drainage system. 5 Quantifying air leak reduction intra‐operatively during selective occlusion of the target lobe provides further objective evidence of the site of air leak. Synergistic use of the endobronchial CV and digital chest drainage systems, together with pre‐operative chest CT, allows triangulation of the site of air leaks, contributing to successful sealing of PALs. This is the first case to our knowledge combining multiple technologies in interventional pulmonology to successfully perform sequential tracheal stenting followed by EBV placement.
AUTHOR CONTRIBUTIONS
Eugene MingJin Gan and Carrie Kah‐Lai Leong were involved in the care of the patient, and contributed to the conceptualization, writing and editing of the manuscript.
FUNDING INFORMATION
Eugene MingJin Gan and Carrie Kah‐Lai Leong do not have any funding to declare.
CONFLICT OF INTEREST STATEMENT
None declared.
ETHICS STATEMENT
The authors declare that appropriate written informed consent was obtained for the publication of this manuscript and accompanying images.
Gan EM, Leong CK‐L. A novel case of simultaneous tracheal stenting and endobronchial valve (EBV) deployment for tracheal stenosis and persistent air leak guided by an endobronchial collateral ventilation assessment system and digital chest drain in malignant esophageal carcinoma. Respirology Case Reports. 2024;12(10):e70041. 10.1002/rcr2.70041
Associate Editor: David Lam
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
REFERENCES
- 1. Fiorelli A, D'Andrilli A, Cascone R, Occhiati L, Anile M, Diso D, et al. Unidirectional endobronchial valves for management of persistent air‐leaks: results of a multicenter study. J Thorac Dis. 2018;10(11):6158–6167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Damaraju V, Sehgal IS, Muthu V, Prasad KT, Dhooria S, Aggarwal AN, Agarwal R. Bronchial valves for persistent air leak: A systematic review and meta‐analysis. J Bronchol Intervent Pulmonol. 2024;31(3):e0964. [DOI] [PubMed] [Google Scholar]
- 3. Saccomanno J, Hübner R‐H, Witzenrath M, Doellinger F, Susanne Dittrich A, Kontogianni K, et al. Bronchoscopic measurement of collateral ventilation: state of the art. Respiration. 2023;102(4):296–307. [DOI] [PubMed] [Google Scholar]
- 4. Omballi M, Noori Z, Alanis RV, Imel RL, Kheir F. Chartis‐guided endobronchial valves placement for persistent air leak. J Bronchol Intervent Pulmonol. 2023;30(4):398–400. [DOI] [PubMed] [Google Scholar]
- 5. Pompili C, Detterbeck F, Papagiannopoulos K, Sihoe A, Vachlas K, Maxfield MW, et al. Multicenter international randomized comparison of objective and subjective outcomes between electronic and traditional chest drainage systems. Ann Thorac Surg. 2014;98(2):490–497. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.


