Highlights
-
•
Radiation for anal cancer is complex, stressful and can cause side effects.
-
•
Pre-consult videos improve patient understanding on key content.
-
•
Patient satisfaction was high and distress scores at content were low.
Abstract
We hypothesized that pre-consult patient education videos can improve patient understanding about their diagnosis, lead to high satisfaction and low distress. In this pilot study, we developed a patient education video curriculum for patients with newly-diagnosed anal cancer. Comprehension of key content was evaluated by comparing pre- and post-test scores. Patient satisfaction scores were collected. Patient distress scores (0–10) were collected at the beginning of their consult visit prior to seeing the physician. We found that patient education videos prior to consult improved patient understanding, resulted in high patient satisfaction, and low patient distress at the time of consult.
Introduction
Squamous cell carcinoma of the anus (SCCA) is a rare malignancy, and pelvic radiation therapy (RT) with concurrent chemotherapy is curative for the majority of patients [1], [2]. However, treatment is intensive and the potential short- and long-term toxicities of pelvic RT can be quality of life (QOL)-limiting. In our prior work surveying 112 survivors of anal cancer characterizing patient experience and QOL after pelvic RT, we found a majority of patients (82 %) reported persistent RT-related toxicity that impacted their QOL [3], [4]. As such, discussions about the benefits versus the risks of treatment are uniquely complex, and 56 % of patients in our survey cohort reported they were not given adequate information regarding their cancer diagnosis, the process of receiving RT and the potential side effects of treatment. A majority of patients (64 %) strongly agreed or somewhat agreed that further educational materials in the form of video and/or written materials would have been helpful prior to starting radiation therapy [5].
The purpose of this brief report is to outline our experience developing, implementing and testing a diagnosis- and institution-specific pre-consult patient education video curriculum for patients with newly-diagnosed SCCA. In this pilot, hypothesized that pre-consult patient education videos would improve patient understanding of key concepts about SCCA and its treatment, result in high patient satisfaction and contribute to low patient distress at the time of their initial clinic visit.
Methods
We received institutional review board approval for this pilot study. Starting in September 2022, we screened all patients with a diagnosis of newly-diagnosed, non-metastatic SCCA and invited them to participate in a prospective protocol collecting patient-reported outcomes (PRO). Patients were excluded from participating if they had received prior pelvic radiation. Patients were contacted by phone 12–72 h prior to their initial radiation oncology consult and invited to participate in the pilot testing of our patient education intervention.
Developing the patient education intervention
The content for the patient education curriculum was developed by a panel of experts including eight radiation oncologists who specialize in gastrointestinal malignancies, two registered nurses, one physician assistant, two nurse practitioners and two survivors of anal cancer. The content agreed upon by consensus was then developed into five video modules: 1.) Anal Cancer Basics, 2.) Anal Cancer Treatment Overview, 3.) Anal Cancer Radiation Logistics, 4.) Early Side Effects and their Management and 5.) Late Side Effects and their Management. The final treatment videos were then recorded with input from physician, nurse practitioner, registered nurse, radiation therapist and patient team members.
Implementing/testing the educational intervention
Patients were contacted by telephone 12–72 h prior to their initial radiation oncology consultation visit and informed consent was obtained if they elected to participate. Then, a link to the pretest assessment in REDCap electronic data capture tools [6] was sent to the participant. The pretest included introductory questions about what sources of information patients had used to learn about their diagnosis and five questions on information covered in each of the five video modules (Supplementary File1). After submitting the pretest, patients were shown five video modules lasting five to ten minutes each. Once the videos completed, patients completed the posttest which included the same twenty-five content questions as well as questions assessing their level of satisfaction with the videos, how likely they were to recommend the videos to other patients and any additional comments on the videos and/or the experience. At the beginning of patient’s clinic visit before seeing the physician, they were asked to rate their level of distress using the National Comprehensive Cancer Network Distress Thermometer on a scale of 0 to 10 as part of the patient needs screen performed by our nursing team at the very beginning of the consult visit before meeting with the physician, resident or advanced practice provider [7].
Statistical analysis
Descriptive statistics were used to report demographic and tumor-related characteristics for patients in this study. Pretest and posttest key content comprehension scores were compared using the paired sample t-test. Distress scores on a scale of 0 to 10 reported at the beginning of the patients’ initial consultation visit were reported using descriptive statistics. P-values <0.05 were considered significant. Statistical analysis was performed using JMP®, Version Pro 17. SAS Institute Inc., Cary, NC, 1989–2023.
Results
Between 9/1/2022 and 1/1/2024, 52 patients with newly-diagnosed, non-metastatic anal squamous cell carcinoma were enrolled onto our prospective PRO-collection protocol and were offered participation in this patient education pilot study. Of the 52 eligible patients, 30 patients (57.7 %) agreed to participate. The most common reasons for the 22 patients not participating in the patient education pilot included being unable to reach the patient by phone prior to consult (N=18) and patient choice (N=4). One patient specifically mentioned that they were overwhelmed right now and just wanted to hear this information from their doctor in person.
Patient demographics
The median [IQR] age of patients participating in this pilot was 61 years [56–69]). Participants were also predominantly female (83.3 %), white (93.3 %), Non-Hispanic/Latino (96.7 %), heterosexual (86.7 %) and HIV-negative (86.7 %). There were no significant differences in patient characteristics between patients who did and did not view the pre-consult patient education videos (Table 1).
Table 1.
Patient demographic information for those who did and did not view pre-consult patient educational videos.
|
Participated in the education cohort N=30 (57.7 %) |
Did not participate in the education cohort N=22 (42.3 %) |
P-value* | |
|---|---|---|---|
| Age in years; median [IQR] | 61 [56–69] | 63 [50–68] | 0.99 |
| Gender; N (%) Men Women |
5 (16.7 %) 25 (83.3 %) |
1 (4.5 %) 21 (95.5 %) |
0.18 |
| Race; N (%) Asian Black Native American/Alaska Native Native Hawaiian/Pacific Islander White |
0 (0 %) 1 (3.3 %) 1 (3.3 %) 0 (0 %) 28 (93.3 %) |
0 (0 %) 1 (4.5 %) 0 (0 %) 0 (0 %) 21 (95.5 %) |
0.67 |
| Ethnicity; N (%) Hispanic/Latino Non-Hispanic/Latino |
1 (3.3 %) 29 (96.7 %) |
2 (9.1 %) 20 (90.9 %) |
0.38 |
| HIV Status; N (%) Negative Positive Unknown |
26 (86.7 %) 3 (10 %) 1 (3.3 %) |
21 (95.5 %) 0 (0 %) 1 (4.5 %) |
0.31 |
| Sexual Orientation; N (%) Heterosexual Homosexual Bisexual Other Prefer not to say |
26 (86.7 %) 2 (6.7 %) 0 (0 %) 0 (0 %) 2 (6.7 %) |
20 (90.9 %) 2 (9.1 %) 0 (0 %) 0 (0 %) 0 (0 %) |
0.45 |
| T-Stage; N (%) T1 T2 T3 T4 |
8 (26.7 %) 14 (46.7 %) 6 (20 %) 2 (6.7 %) |
4 (18.2 %) 11 (50 %)2 (9.1 %) 5 (22.7 %) |
0.28 |
| N-Stage; N (%) N0 N1a N1b N1c |
19 (63.3 %) 9 (30 %) 0 (0 %) 2 (6.7 %) |
7 (31.8 %) 13 (59.1 %) 0 (0 %) 2 (9.1 %) |
0.08 |
| Radiation Dose; N (%) 50 Gray 54 Gray 58 Gray Other |
10 (33.3 %) 12 (40 %) 7 (23.3 %) 1 (3.3 %) |
3 (13.6 %) 10 (45.5 %) 9 (40.9 %) 0 (0 %) |
0.25 |
*Pearson Chi-square test for categorical variables and Kruskal-Wallis test for continuous variables. HIV=human immunodeficiency virus; T = tumor, N=nodal.
Efficacy in communicating key content
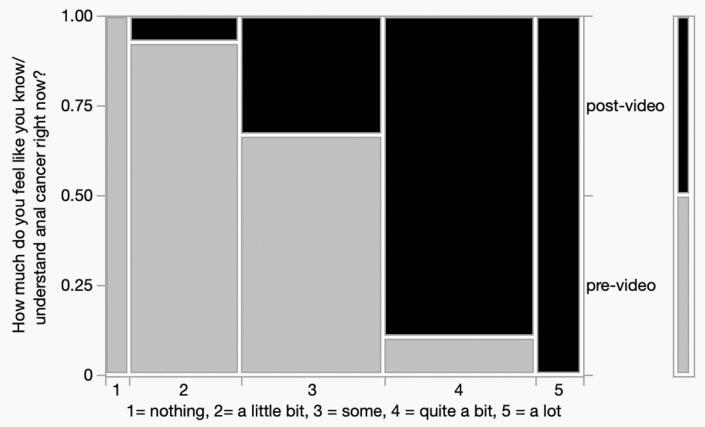
Prior to viewing the pre-consult patient education videos, most patients (N=26, 87 %) reported that they had spent time researching their diagnosis. Eighteen (60 %) had spoken to their primary care physician about it, six (20 %) had spoken to friends or family about it, 21 (70 %) had researched it on the internet, eight (27 %) had viewed the hospital webpage, two (7 %) had joined an online cancer support group and two (7 %) had searched social media sites for information. The mean ± SD score was significantly higher on the post- vs. pre-education intervention assessment (89 %±12 % vs 67 %±17 %; P<.01). Scores were higher on each of the five modules post-intervention compared with pre-intervention (Table 2). More patients reported they understood anal cancer and its treatment better on the post- vs. pre-education intervention assessment (P<.01, Fig. 1), as compared to reporting they know nothing/a little bit. After viewing the patient education videos, most patients reported they found them very/quite a bit helpful (93 %) and were very/quite a bit likely to recommend the videos to other patients (97 %).
Table 2.
Average patient scores for each module before and after viewing the patient education videos.
| Instrument |
Pre-test (Score out of 100 %) |
Post-test (Score out of 100 %) |
P-value* |
|---|---|---|---|
| Total Percent Correct; Mean ± SD Median [IQR] |
67 %±17 % 68 % [60–76 %] |
89 %±12 % 92 % [84–96 %] |
0<.01 |
| Module 1: Anal Cancer Basics; Mean ± SD Median [IQR] |
71 %±17 % 60 % [60–80 %] |
83 %±16 % 80 % [80–100 %] |
0<.01 |
| Module 2: Anal Cancer Treatment Overview Mean ± SD Median [IQR] |
75 %±21 % 80 % [60–100 %] |
92 %±11 % 100 % [80–100 %] |
0<.01 |
| Module 3: Anal Cancer Radiation Logistics Mean ± SD Median [IQR] |
49 %±24 % 50 % [35–60 %] |
91 %±19 % 100 % [95–100 % |
0<.01 |
| Module 4: Early Side Effects and their Management Mean ± SD Median [IQR] |
69 %±19 % 80 % [60–80 %] |
91 %±21 % 100 % [95 %-100 %] |
0<.01 |
| Module 5: Late Side Effects and their Management Mean ± SD Median [IQR] |
61 %±24 % 60 % [40–80 %] |
83 %±19 % 80 % [60–100 %] |
0<.01 |
*Paired sample t-test. SD=standard deviation; IQR=interquartile range.
Fig. 1.
Patient-reported knowledge and understanding about anal cancer before and after watching pre-consult patient education videos. (Pearson Chi-square < 0.01).
Patient Distress Score at the Consultation Visit- Of the 30 patients who watched the pre-consult education videos, 13/33 patients (43.3 %) reported a distress score of 0 (no distress) at the time of their consult visit, and 5/30 (16.7 %) reported a distress score of 5 or greater. Of the 22 patients enrolled in the prospective PRO-collection protocol who did not watch the pre-consult education videos, 7/22 (31.8 %) reported a distress score of 0 at the time of their consult visit, and 10/22 (45.5 %) reported a distress score of 5 of greater.
Discussion
In this pilot study, we showed that a series of pre-consult patient education videos can improve patient understanding of key concepts related to SCCA and its treatment, deliver high patient satisfaction and contribute to low patient distress at the time of their initial oncology consultation.
In this cohort of 30 patients that viewed pre-consult patient education videos, nearly 90 % had spent time researching their diagnosis prior to their first oncology appointment. This is in line with data showing increasing numbers of newly diagnosed patients with cancer and survivors of cancer seek information about their cancer and its treatment outside of what they learn in a physician’s office [8]. Although there are excellent patient-facing resources specific to SCCA on website such as the Anal Cancer Foundation (www.analcancerfoundation.org) and the International Anal Neoplasia Society (https://iansoc.org), the quality of patient education materials online are highly variable, are often incomplete and may be biased towards unproven or alternative therapies [9], [10]. Information about radiation treatment and its side effects can be even more difficult for the public to comprehend. Information provided on radiation oncology department websites is often written at a collegiate reading level rather than the target sixth-grade reading level for patient-facing information [11]. These data emphasize the need for accurate, appropriate and specific patient education information, particularly for rare and potentially stigmatized diagnoses such as SCCA.
At our institution, we previously provided written educational handouts after the patient met with their radiation oncologist during initial consultation. However, we elected to use videos as the method of patient education given the increasing importance of internet-hosted videos when consuming medical information and advice [12]. Additionally, there are many published studies suggesting patients benefit from reviewing education materials in a non-written format. A recent systematic review and meta-analysis of the diagnostic procedure literature showed that education videos are more effective than other forms of information dissemination and may help improve anxiety related to unfamiliarity with procedures such as invasive vascular procedures, positron emission tomography, magnetic resonance imaging, colonoscopy and endoscopic retrograde cholangiopancreatograpy [13].
Additionally, we elected to show patients the patient educational videos prior to their initial consultation rather than afterwards because we hypothesized we could contribute to low patient distress at the time of the clinic visit by giving them reliable information about their disease and its treatment ahead of time. This is consistent with data from patients with breast or gynecologic cancers that show two thirds preferred education materials being given first followed by discussion with their health care provider [14]. Indeed, we received unstructured feedback from patients and physicians that consult visits were more efficient and productive as patients were able to have a baseline understanding and come with specific questions and concerns after watching the pre-consult patient education videos. Additionally, patients who watched the videos reported low distress scores at the start of their consultation visit.
Our study adds to the existing body of literature suggesting patient education content can be effectively communicated to patients and their loved ones prior to the initial consultation visit with their radiation oncologist. Matsuyama et al published a pivotal study in 2013 showing proof of concept that a pre-consult patient education video could improve patients’ understanding of how radiation works and result in high patient satisfaction [15]. While Matsuyama’s twenty-two minute patient education DVD was broadly applicable to all cancer types, we aimed to create diagnosis and treatment-specific content for patients with anal cancer, acknowledging that the rationale, logistics and especially the potential toxicities are unique. Indeed, Kumar et al published a randomized study testing the impact of general and breast-cancer specific web-hosted patient education videos administered to patients prior to their initial consultation. In the group of patients with breast cancer who were randomized to watch the patient education videos, 46.8 % reported decreased anxiety, and 66.0 % felt more comfortable coming to a consult [16]. These results are similar to the low distress scores reported by our patients who watched the anal cancer-specific patient education videos.
This study provides useful data about one method to improve patient education and satisfaction; however, this study has several limitations. First, the pre- and post-video test questions were the same, and repetition could have contributed to the observed increase in scores. We cannot draw any definitive conclusions from this pilot whether or not the patient education videos were the cause of low patient distress compared with patients who did not watch the pre-consult patient education videos because of the non-randomized design of this study. There are likely differences between those who elected to participate in the pilot and those who did not that contribute to the observed differences in distress scores. As such, this observation is hypothesis generating only and supports the need for a larger randomized study to evaluate intervention to reduce patient distress. Finally, the patient education videos created for this pilot were somewhat “institution-specific” in that they contained detailed information about our workflows, locations and personnel. Patient feedback indicated patients appreciated that the videos were tailored to their specific experience, undergoing treatment for anal cancer at our institution. However, our group plans to partner with national and international organizations to adapt our video series for a more general audience beyond our institution, particularly the modules on anal cancer basics and side effects. We also plan to incorporate even more feedback and input from our radiation therapy, nursing and patient advocate team members.
In conclusion, viewing diagnosis- and institution-specific patient education videos before consultation improved patient understanding of SCCA and its treatment, resulted in high patient satisfaction, and may reduce patient distress at the time of their initial oncology consultation visit. After this successful pilot study, we plan on making these videos available to all our patients with newly-diagnosed SCCA at our institution.
Informed patient consent
The author(s) confirm that written informed consent has been obtained from the involved patient(s) or if appropriate from the parent, guardian, power of attorney of the involved patient(s); and, they have given approval for this information to be published in this case report (series).
Funding
This work was funded by a Radiation Oncology Strategic Initiatives seed grant to Dr. Corrigan from the Division of Radiation Oncology at UT MD Anderson Cancer center.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We would like to acknowledge and thank the patients and their loved ones who participated in this pilot study and shared their thoughts and opinions regarding optimizing patient education materials.
Footnotes
Supplementary material to this article can be found online at https://doi.org/10.1016/j.tipsro.2024.100271.
Appendix A. Supplementary material
The following are the Supplementary material to this article:
References
- 1.Kachnic L.A., Winter K., Myerson R.J., Goodyear M.D., Willins J., Esthappan J., et al. RTOG 0529: a phase 2 evaluation of dose-painted intensity modulated radiation therapy in combination with 5-fluorouracil and mitomycin-C for the reduction of acute morbidity in carcinoma of the anal canal. Int J Radiat Oncol Biol Phys. 2013;86:27–33. doi: 10.1016/j.ijrobp.2012.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kachnic L.A., Winter K., Myerson R.J., Goodyear M.D., Abitbol A.A., Streeter O.E., et al. Long term outcomes of NRG oncology/RTOG 0529: a phase ii evaluation of dose-painted intensity modulated radiation therapy (DP-IMRT) in combination with 5-fluorouracil and mitomycin-c for the reduction of acute morbidity in anal canal cancer. Int J Radiat Oncol Biol Phys. 2021 doi: 10.1016/j.ijrobp.2021.08.008. S0360 –3016(21)02647-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.De B., Corrigan K.L., Rooney M.K., Ludmir E.B., Das P., Smith G.L., et al. Patient-reported bowel and urinary function in long-term survivors of squamous cell carcinoma of the anus treated with definitive intensity modulated radiation therapy and concurrent chemotherapy. Int J Radiat Oncol Biol Phys. 2022;S0360–3016(22):00417. doi: 10.1016/j.ijrobp.2022.05.009. [DOI] [PubMed] [Google Scholar]
- 4.Corrigan K.L., Rooney M.K., De B., Ludmir E.D., Das P., Smith G.L., et al. Patient-reported sexual function in long-term survivors of anal cancer treated with definitive intensity modulated radiation therapy and concurrent chemotherapy. Pract Radiat Oncol. 2022;12:e397–e405. doi: 10.1016/j.prro.2022.05.006. [DOI] [PubMed] [Google Scholar]
- 5.Corrigan K.L., De B., Rooney M.K., Ludmir E.B., Das P., Smith G.L., et al. Patient-reported outcomes after chemoradiation in patients with anal cancer: a qualitative analysis. Adv Radiat Oncol. 2022;7 doi: 10.1016/j.adro.2022.100986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ownby K.K. Use of the distress thermometer in clinical practice. J Adv Pract Oncol. 2019;10:175–179. [PMC free article] [PubMed] [Google Scholar]
- 8.Finney Rutten L.J., Agunwamba A.A., Wilson P., Chawla N., Vieux S., Blanch-Hartigan D., et al. Cancer-related information seeking among cancer survivors: trends over a decade (2003–2013) J Cancer Educ. 2016;31:348–357. doi: 10.1007/s13187-015-0802-7. [DOI] [PubMed] [Google Scholar]
- 9.Wasserman M., Baxter N.N., Rosen B., Burnstein M., Halverson A.L. Systematic review of internet patient information on colorectal cancer surgery. Dis Colon Rectum. 2014;57:64–69. doi: 10.1097/DCR.0000000000000011. [DOI] [PubMed] [Google Scholar]
- 10.Kim D.Y., Lee H.R., Nam E.M. Assessing cancer treatment related information online: unintended retrieval of complementary and alternative medicine web sites. Eur J Cancer Care (Engl) 2009;18:64–68. doi: 10.1111/j.1365-2354.2008.00944.x. [DOI] [PubMed] [Google Scholar]
- 11.Rosenberg S.A., Francis D.M., Hullet C.R., Morris Z.S., Brower J.V., Anderson B.M., et al. Online patient information from radiation oncology departments is too complex for the general population. Pract Radiat Oncol. 2017;7:57–62. doi: 10.1016/j.prro.2016.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Langford A., Loeb S. Perceived patient-provider communication quality and sociodemographic factors associated with watching health-related videos on youtube: a cross-sectional analysis. J Med Internet Res. 2019;21:e13512. doi: 10.2196/13512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Monteiro Grilo A., Ferreira A.C., Pedro Ramos M., Carolino E., Filipa Pires A., Vieira L. Effectiveness of educational videos on patient’s preparation for diagnostic procedures: Systematic review and Meta-Analysis. Prev Med Rep. 2022;28 doi: 10.1016/j.pmedr.2022.101895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stabile C., Goldfarb S., Baser R.E., Goldfrank D.J., Abu-Rustum N.R., Barakat R.R., et al. Sexual health needs and educational intervention preferences for women with cancer. Breast Cancer Res Treat. 2017;165:77–84. doi: 10.1007/s10549-017-4305-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matsuyama R.K., Lyckholm L.J., Molisani A., Moghanaki D. The value of an educational video before consultation with a radiation oncologist. J Cancer Educ. 2013;28:306–313. doi: 10.1007/s13187-013-0473-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kumar K.A., Balazy K.E., Gutkin P.M., Jacobson C.E., Chen J.J., Karl J.J., et al. Association between patient education videos and knowledge of radiation treatment. Int J Radiat Oncol Biol Phys. 2021;109:1165–1175. doi: 10.1016/j.ijrobp.2020.11.069. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.