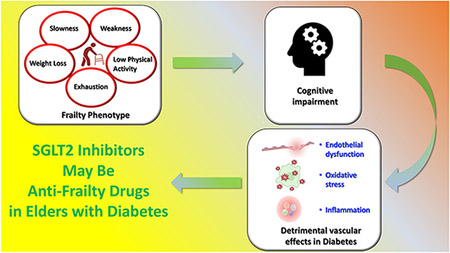
Frailty, one of the most commonly diagnosed conditions in older individuals (>65 years), increases the risk of adverse events.1 Of note, comorbidities, including type 2 diabetes, represent a considerable burden in the pathophysiology of frailty. Additionally, managing diabetes becomes more complex with age, as frailty becomes a crucial factor in adjusting glycaemic goals and medication choices, particularly in older individuals.2 Nevertheless, there is currently no accepted treatment for frailty.
SGLT2 inhibitors (also known as gliflozins) and GLP-1 receptor agonists are, of late, attracting substantial research attention for their benefits beyond glycaemic control, including for both macrovascular and microvascular complications, thereby suggesting their potential as anti-frailty drugs.2-4 However, much of the existing research is based on placebo-controlled clinical trials, which underscores the need for real-world evidence and direct head-to-head comparisons to validate clinical practices and address safety concerns.
In The Lancet Healthy Longevity, Fei-Yuan Hsiao and colleagues evaluated the effects of SGLT2 inhibitors and GLP-1 receptor agonists.5 The study focused on examining the effects of both drugs in frailty subgroups and showed overall similar beneficial results in terms of cardiovascular outcomes. These findings are in line with previous reports that provided evidence on the cardioprotective and nephroprotective effects of SGLT2 inhibitors.6 Hsiao and colleagues5 showed that both drugs have beneficial effects on cardiovascular outcomes in frail individuals with diabetes. These findings are consistent with those of a study by Kutz and colleagues,3 which showed that SGLT-2 inhibitors and GLP-1 receptor agonists improved cardiovascular outcomes and all-cause mortality in a safe manner, with the highest absolute benefits observed among frail people. However, users of GLP-1 receptor agonists presented an increased risk of end-stage renal disease (ie, dialysis and renal transplantation) compared with users of SGLT2 inhibitors.5
Our research group has extensively studied the functional role of SGLT2 inhibition in frailty. In particular, we have provided evidence for the positive effects of SGLT2 inhibitors on cognitive and physical impairment in frail older individuals, with a salutary effect of empagliflozin treatment on the frailty levels in older individuals with diabetes and hypertension.7
Nonetheless, the side effects of both SGLT2 inhibitors and GLP-1 receptor agonists should also be emphasised. SGLT2 inhibitors have been shown to be associated with genitourinary infections and diabetic ketoacidosis; however, a recent investigation showed that none of these adverse events were more frequent among older adults (≥75 years) than among younger adults (<75 years).8 GLP-1 receptor agonists have non-negligible effects on weight loss and the feeling of hunger, with an increased risk of nausea, vomiting, and diarrhoea. Thus, GLP-1 receptor agonists could simulate a sarcopenic effect in frail older individuals.
These observations could lead to the use of SGLT2 inhibitors being favoured over GLP-1 receptor agonists in frail older individuals; however, these aspects need to be evaluated in dedicated randomised investigations with a long follow-up and using additional GLP-1 receptor agonists (including semaglutide, which was not integrated in the investigation by Hsiao and colleagues5). This last aspect is particularly relevant considering the recent publication of the FLOW trial,9 which showed that semaglutide reduces the risk of kidney disease-related events in individuals with type 2 diabetes and chronic kidney disease.
Future studies on frail individuals should also distinguish between the anorexic-malnourished phenotype (characterised by low bodyweight, malnutrition, low glycated haemoglobin [HbA1c], and increased risk of hypoglycaemia) and sarcopenic-obese phenotype (characterised by an elevated bodyweight and high HbA1c).10
In conclusion, even though the results obtained by Hsiao and colleagues5 are in line with the literature, especially the observed effects on cardiovascular and renal protection, the essential role of SGLT2 inhibition in the possible reduction of frailty levels needs to be expanded upon (appendix), especially the pleiotropic effects of SGLT2 inhibitors independent of their action on glycaemia.
Footnotes
We declare no conflicting interests.
Contributor Information
Pasquale Mone, Department of Medicine and Health Sciences “Vincenzo Tiberio”, Campobasso, 86100, Italy; Department of Medicine, Division of Cardiology, Wilf Family Cardiovascular Research Institute, Einstein Institute for Aging Research, Einstein-Mount Sinai Diabetes Research Center (ES-DRC), Einstein Institute for Neuroimmunology and Inflammation (INI), Fleischer Institute for Diabetes and Metabolism (FIDAM), Albert Einstein College of Medicine, New York, NY, USA; Casa di Cura Montevergine, Mercogliano (Avellino), Italy.
Michele Ciccarelli, Department of Medicine, Surgery, and Dentistry, University of Salerno, Baronissi (Salerno), Italy.
Stanislovas S Jankauskas, Department of Medicine, Division of Cardiology, Wilf Family Cardiovascular Research Institute, Einstein Institute for Aging Research, Einstein-Mount Sinai Diabetes Research Center (ES-DRC), Einstein Institute for Neuroimmunology and Inflammation (INI), Fleischer Institute for Diabetes and Metabolism (FIDAM), Albert Einstein College of Medicine, New York, NY, USA.
Germano Guerra, Department of Medicine and Health Sciences “Vincenzo Tiberio”, Campobasso, 86100, Italy; International Translational Research and Medical Education Consortium (ITME), Academic Research Unit, Naples, Italy.
Carmine Vecchione, Department of Medicine, Surgery, and Dentistry, University of Salerno, Baronissi (Salerno), Italy.
Valeria Visco, Department of Medicine, Surgery, and Dentistry, University of Salerno, Baronissi (Salerno), Italy.
Gaetano Santulli, Department of Medicine, Division of Cardiology, Wilf Family Cardiovascular Research Institute, Einstein Institute for Aging Research, Einstein-Mount Sinai Diabetes Research Center (ES-DRC), Einstein Institute for Neuroimmunology and Inflammation (INI), Fleischer Institute for Diabetes and Metabolism (FIDAM), Albert Einstein College of Medicine, New York, NY, USA; International Translational Research and Medical Education Consortium (ITME), Academic Research Unit, Naples, Italy; Department of Advanced Biomedical Sciences, University of Naples “Federico II”, Naples, Italy.
References
- 1.Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet 2013; 381: 752–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mone P, Lombardi A, Gambardella J, et al. Empagliflozin improves cognitive impairment in frail older adults with type 2 diabetes and heart failure with preserved ejection fraction. Diabetes Care 2022; 45: 1247–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kutz A, Kim DH, Wexler DJ, et al. Comparative cardiovascular effectiveness and safety of SGLT-2 inhibitors, GLP-1 receptor agonists, and DPP-4 inhibitors according to frailty in type 2 diabetes. Diabetes Care 2023; 46: 2004–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Santulli G, Varzideh F, Forzano I, et al. Functional and clinical importance of SGLT2-inhibitors in frailty: from the kidney to the heart. Hypertension 2023; 80: 1800–09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hsiao FY, Tan EC, Meng LC, et al. Impact of frailty on effectiveness and safety of GLP-1 receptor agonist and SGLT2 inhibitor in people with type 2 diabetes: a nationwide longitudinal study. Lancet Healthy Longev 2024. 10.1016/j.lanhl.2024.07.004 (in press). [DOI] [PubMed] [Google Scholar]
- 6.Heerspink HJL, Stefánsson BV, Correa-Rotter R, et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med 2020; 383: 1436–46. [DOI] [PubMed] [Google Scholar]
- 7.Mone P, Varzideh F, Jankauskas SS, et al. SGLT2 inhibition via empagliflozin improves endothelial function and reduces mitochondrial oxidative stress: insights from frail hypertensive and diabetic patients. Hypertension 2022; 79: 1633–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goldman A, Fishman B, Twig G, et al. The real-world safety profile of sodium-glucose co-transporter-2 inhibitors among older adults (≥75 years): a retrospective, pharmacovigilance study. Cardiovasc Diabetol 2023; 22: 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Perkovic V, Tuttle KR, Rossing P, et al. Effects of semaglutide on chronic kidney disease in patients with type 2 diabetes. N Engl J Med 2024; 391:109–21. [DOI] [PubMed] [Google Scholar]
- 10.Sinclair AJ, Abdelhafiz AH. Metabolic impact of frailty changes diabetes trajectory. Metabolites 2023; 13: 295. [DOI] [PMC free article] [PubMed] [Google Scholar]


