Abstract
Purpose Sonography training has become an important part of university medicine courses. This study explores the impact of digital and analog teaching resources on learning outcomes, knowledge retention, and student preferences and motivation in a flipped classroom setting.
Materials and Methods This prospective controlled study involving two groups of third-year medical students included a voluntary three-day compact ultrasound course given in a flipped classroom, comprising 26 teaching units of 45 minutes each. Hardcopy lecture notes (control group) and E-learning (study group) were used as teaching resources. Evaluations were conducted before (pre) and during the preparation phase (intermediate), and after (post) the face-to-face course. Likert scale responses, written theory tests with very short answer questions (Theorypre, Theoryinter, Theorypost), and practical examinations (Practiceinter, Practicepost) were used for student self-assessment and to measure attitude, motivation, as well as theoretical and practical skills.
Results A total of N=236 complete data sets (study group n=136; control group n=100) were analyzed. Both groups showed an equivalent initial level of, and a continuous and significant (p<0.01) increase in, subjective and objective skills over the evaluated time frame. The study group achieved significantly (p<0.05) better results in Theoryinter, Theorypost, Practiceinter, and Practicepost. The study group evaluated their teaching resource and the training concept significantly (p<0.05) better.
Conclusion The integration of digital resources into sonography education provides comparable learning outcomes to traditional analog materials, enhancing the preparatory phase. In the future, digitally supported training should be used more.
Keywords: ultrasound education, blended learning, flipped classroom, E-Learning, ultrasound training
Introduction
Ultrasound technology can be used for medical diagnosis and interventions by providing real-time visualization of anatomical structures and physiological processes, thus enhancing clinical decision-making and patient care 1 . Technical advancements in terms of new image modes and constantly improving hand-held ultrasound devices have also contributed to this 2 3 4 5 . As the demand for proficient ultrasound practitioners has risen, the need to impart theoretical knowledge and practical skills in the field of medicine has become increasingly evident. Traditional didactic teaching methods have undergone a transformation to incorporate innovative approaches aligned with the requirements of modern education and technology. Notably, the flipped classroom concept, a practical application of blended learning, has gained prominence, emphasizing active learning and engagement 6 7 8 .
The flipped classroom is an instructional strategy and educational approach that reverses traditional teaching methods. In the conventional setting, students acquire new content through lectures or presentations in the classroom and then solidify their understanding with homework outside of class. In a flipped classroom, this sequence is inverted 9 10 .
In comparison, blended learning integrates traditional face-to-face instruction with online or digital learning experiences. This approach entails a combination of in-person and virtual activities, providing a flexible and personalized learning experience. The overarching objective is to harness the strengths of both traditional classroom teaching and digital resources to enhance the overall educational outcome.
Ultrasound education traditionally entailed didactic lectures followed by hands-on practice sessions. However, the rapid evolution of ultrasound technology, the complexities of anatomy and pathology, and the higher number of trainees require a more dynamic educational approach 11 . The flipped classroom model, with students accessing instructional content before class and engaging in collaborative activities during class, has the potential to enhance student engagement, critical thinking, and problem-solving skills 12 . This approach is particularly promising for ultrasound education, as it can facilitate a deeper understanding of complex concepts and allow more time for practical application and experimental learning. International professional societies recommend the integration of blended learning in ultrasound teaching methodologies 13 14 15 16 17 . Therefore, national and international professional societies such as the German Society for Ultrasound in Medicine (DEGUM) and the European Federation of Societies for Ultrasound in Medicine and Biology are also currently discussing possibilities for digitalization within medical ultrasound training 11 15 18 .
The advancement of digital technologies has ushered in a new era of educational possibilities, providing access to a wealth of multimedia resources such as online lectures, interactive simulations, virtual anatomy models, and self-assessment tools 19 20 21 . These resources offer students opportunities for self-paced learning and personalized exploration of ultrasound principles. Nevertheless, these should supplement, not replace, traditional methods in ultrasound teaching. These “analog” resources, encompassing traditional textbooks, instructor-led demonstrations, and practical training on physical models, offer tangible, tactile learning experiences and direct interaction with instructors, and thus are essential to robust, holistic education in medicine 22 .
Current ultrasound teaching has begun to adopt this “blended” approach, in which flipped classrooms facilitated by digital learning tools supplement analog learning methods. Yet relatively few studies have directly compared the effectiveness of digital and analog resources in ultrasound education in a flipped classroom approach 23 . This DIvAN (Digital vs. Analog) study was developed to investigate how resource types influence learning outcomes, knowledge retention, and student preferences in a flipped ultrasound classroom. The study assesses both subjective and objective measures by which student competence develops, and, in doing so, provides evidence-based optimization of ultrasound educational resources for undergraduates.
Materials and Methods
Study Design and Recruiting
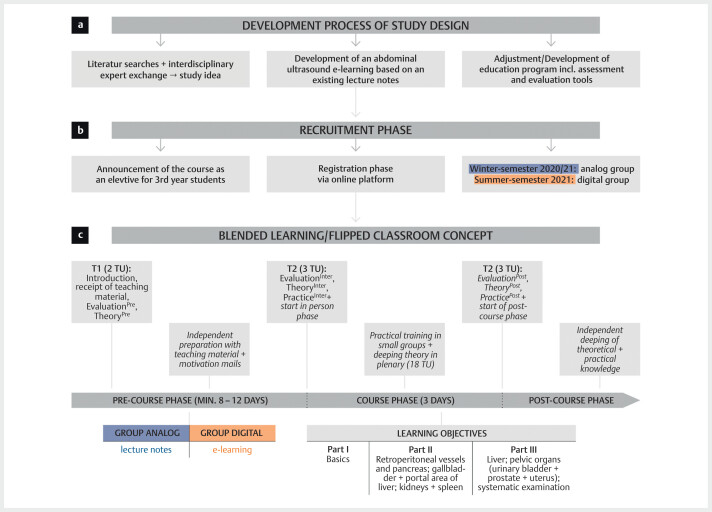
This controlled intervention study was conducted prospectively 24 . Fig. 1 provides further details about study development and study design. The study was performed as part of a voluntary 8-course program at a medical university, and participants were medical students in their third year of medical studies divided into two groups: the winter semester 2020/2021 cohort, which formed the control group taught through lecture notes, and the summer semester 2021, which formed the study group taught through e-learning. Students registered via a university online portal. Inclusion criteria of individual students were consent to participate in the study; completion of all parts of the study; and use of teaching materials 25 . Evaluations were carried out at three points: before the start of the training, i. e., before receiving the teaching material (T 1 =pre), before the face-to-face course phase, i. e., after the preparation period, and after the face-to-face course phase (T 3 =post). Evaluations were complemented by written theory tests (Theory pre , Theory inter , Theory post ) 25 . Additionally, practical examinations with three 120-point work assignments took place at T 2 and T 3 (Practice inter , Practice post ) 25 .
Fig. 1.
Development process and design of the DIvAN study including the measurement times and assessment tools as well as teaching content. After the study was developed ( a ), the recruitment phase ( b ) followed, which was followed by the blended learning/flipped classroom-based training concept ( c ); Evaluation (Evaluationpre, Evaluationinter, Evaluationpost), theoretical tests (Theorypre, Theoryinter, Theorypost), and practical tests (Practiceinter, Practicepost) were carried out at different times (T1–T3). Randomization takes place by semester (winter semester-analog/control group, summer semester-digital/study group); TU=teaching units.
Teaching Concept and Learning Materials
The flipped classroom and blended learning stage was divided into three phases (see Fig. 1 ) and was developed based on preliminary work 26 . An introductory event was followed by the 8–12-day preparation phase, in which students learned independently using either an analog or digital teaching medium. In this study, students learned through hardcopy lecture notes or e-learning modules. The subsequent three-day, modular, face-to-face course phase consisted of 26 teaching units with 45 minutes devoted to each unit. During this phase, several pedagogical approaches were alternated: students observed practical applications of taught content; practiced in small groups under teacher guidance; further practiced under the guidance of peer tutors; independently repeated practice; and then deepened their knowledge of theoretical content. The follow-up phase was used to further explore and independently apply what had been learned. The learning objectives of the training concept (see Supplementary Table 1 ) determined both the content of the teaching media and later examinations and were based on the DEGUM Basic catalog for abdominal sonography developed jointly by sonography experts and didactics 27 . A comparison of the teaching media lecture notes and e-learning is listed in Supplementary Table 2 and Supplementary Figures 1 and 2 . The scope of the content of both teaching media was approximately the same. The participants also received equivalent work assignments in the form of a workbook for preparation and post-course processing follow-up.
Lecture Notes
The hardcopy lecture notes were divided into ten modules and three excursions. Each module contained, in continuous text form, the transducer positions, cross-sectional images (cross-sections), and examination procedures that are important for the organ and image series. The most common pathologies of the organ systems were then described in bullet points and indicated in the images. Checklists after each module encouraged self-assessment.
E-Learning
The e-learning that was developed was based on the hardcopy lecture notes. The e-learning could be accessed online. The same basic structure was used for a total of 10 organ-specific modules. The learning content was conveyed using flashcards (“slides”) with continuous text, bullet points, images, and/or video clips. Links to additional online atlases were also provided 21 . The interactive click functions included resolving questions, filling in empty tables, or labelling ultrasound images or graphics. The same checklists as in the hardcopy lecture notes were used for self-assessment after each module.
Assessment
Evaluations (Evaluation pre , Evaluation inter , Evaluation post )
Evaluations around 10 minutes in length asked about various topics using multiple items. These include “Personal Data”, “Previous Experience”, “Usage Behavior”, “Motivation”, “Subjective Competence Assessment”, “Teaching Material”, and “Training Concept”. The answers were recorded using a seven-point Likert answer scale (1=completely true/very good; 7=not at all true/very bad), dichotomous choice answers, or free text questions.
Theoretical Assessments (Theory pre , Theory inter , Theory post )
The theory tests of 50 minutes and 199 points assessed the following competencies: “Basics” (33 points); “Normal findings/structure recognition in orientational cross-sections” (118 points); and “Pathology recognition” (48 points). The tests used free-text questions based on the defined learning objectives (see Supplementary Figures 3–5 for example questions) 28 .
Practical Assessment (Practice inter , Practice post )
At T 2 and T 3 , practical skills were tested by standardized and validated objective structured clinical examination (OSCE) 29 . The competencies “Transducer handling”, “Patient guidance”, “Examination”, “Picture explanation”, and “Overall performance” were assessed in the defined combinations of three competencies outlined in 2.3.2 (see Supplementary Figure 6 ). Each 7-minute OSCE was worth a maximum of 40 points, totaling 120 overall available points.
Statistical Analysis
Data were for the evaluations as well as theoretical and practical learning success checks were manually evaluated using Microsoft Excel before analysis in R studio (RStudio Team [2020]. RStudio: Integrated Development for R. RStudio, PBC, http://www.rstudio.com , last accessed 11/30/2023) with R 4.0.3 (A Language and Environment for Statistical Computing, R Foundation for Statistical Computing, http://www.R-project.org ; last accessed 11/30/2023). Binary and categorical baseline parameters are expressed as absolute numbers and percentages. Continuous data are expressed as median and interquartile range (IQR) or as mean and standard deviation (SD). Categorical parameters were compared using Fisher’s exact test and continuous parameters using the Mann-Whitney test. In addition, pairwise correlations of metric variables were obtained, and the correlation effect sizes and significances were calculated. Furthermore, Mann-Whitney tests were constructed to compare the influence of individual factors on the results of the theoretical and practical tests. Finally, a multivariate linear regression model was produced to compare the influence of individual factors. P-values<0.05 were considered statistically significant.
Results
Study Population
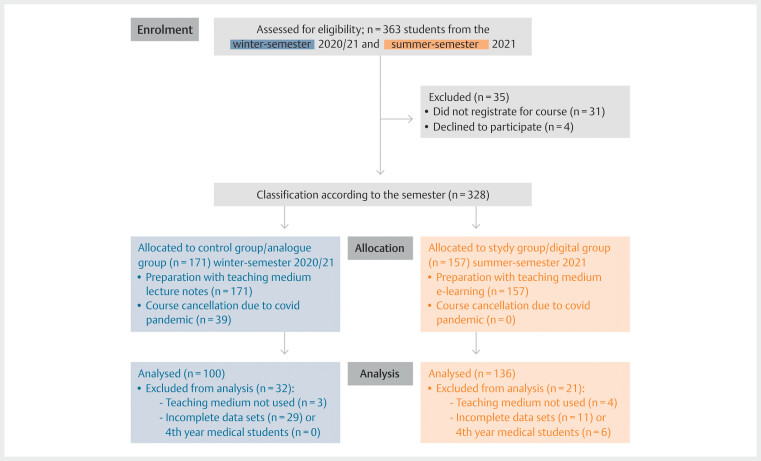
A total of n=236 complete data sets (see Fig. 2 ) from a study group of n=136 and a control group of n=100 were statistically analyzed.
Fig. 2.
Flow diagram for participant inclusion and data analysis according to CONSORT.
Table 1 lists the baseline characteristics of the study and control groups. The average age of the study group was higher than that of the control group (study 25.8±3.2 vs. control 24.6±3.6; p<0.01). In addition, significantly more participants in the study group stated that they had previous training in the medical field (study 74.3% vs. control 55.0%; p<0.01).
Table 1 Comparison of baseline characteristics of the control versus study group.
| Item | Control group | Study group | p-value | |
|---|---|---|---|---|
| n | 100 | 136 | ||
| Age (years) | <0.01 | |||
| Mean±standard deviation | 24.6±3.6 | 25.8±3.2 | ||
| Gender | n | n | % | 1.00 |
| Female | 68 | 92 | 68 | |
| Male | 32 | 44 | 33 | |
| Training before medical studies | ||||
| Medical sector | <0.01 | |||
| Yes | 55 | 101 | 74 | |
| None | 45 | 35 | 26 | |
| Non-medical sector | 0.74 | |||
| Yes | 3 | 6 | 4 | |
| None | 97 | 130 | 96 | |
| Experience with cross-sectional imaging | 0.13 | |||
| None | 76 | 115 | 85 | |
| Yes. Format of training | 24 | 21 | 15 | |
| Non-university courses | 7 | 7 | 5 | |
| University courses | 9 | 3 | 2 | |
| Self-study | 8 | 11 | 8 | |
| Total duration (units of 45 min) | ||||
| <10 units | 16 | 10 | 7 | |
| 10–20 units | 5 | 5 | 4 | |
| >20 units | 3 | 6 | 4 | |
| Previous sonography courses | 0.41 | |||
| No | 96 | 134 | 99 | |
| Yes | 4 | 2 | 1 | |
| Total duration (units of 45 min) | ||||
| <10 units | 3 | 2 | 2 | |
| 10–20 units | 1 | 0 | 0 | |
| >20 units | 0 | 0 | 0 | |
| Observed ultrasound examinations | 0.42 | |||
| None | 18 | 31 | 23 | |
| Yes | 82 | 105 | 77 | |
| Performed ultrasound examinations | 0.07 | |||
| None | 75 | 115 | 115 | |
| Yes | 25 | 21 | 21 | |
| Number | ||||
| <5 | 21 | 18 | 18 | |
| 5–10 | 3 | 2 | 2 | |
| 10–15 | 1 | 1 | 1 | |
| >15 | 0 | 0 | 0 | |
Otherwise, no significant differences were found in the groups, especially not in their self-reporting of previous experience in interpreting cross-sectional images (p=0.13) or having ultrasound knowledge (all p-values>0.05).
Evaluations
Evaluation of the “use of teaching media” and “satisfaction with digital teaching offerings” queries
The evaluation results of the items “use of teaching media” and “satisfaction with digital teaching offerings” are listed in Supplementary Table 3 . Most participants in both groups stated that they used digital media privately (study 97% vs. control 100%; p=0.14) and in their studies (study 99% vs. control 100%; p=0.51), though they had not yet used any digital (study 93% vs. control 98%; p=0.08) or analog media (study 96% vs. control 95%; p=0.74) for ultrasound teaching at time T 1 .
In Evaluation inter at T 2 , no significant differences were found between the two groups in the chapters of the teaching media that they had worked on. However, the study group reported a significantly higher level of preparation (p<0.01).
Evaluation of the “motivation” query
The results of the “motivation” query are presented in Supplementary Table 4 . Both groups had a high motivation to take part in the course at T 1 (study 1.6±0.7 vs. control 1.6±0.7; p=0.42). The groups also reported that the format and presentation of a teaching medium have a major influence on their motivation to participate in courses (study 1.9±1.0 vs. control 2.0±1.0; p=0.58). In addition, both groups showed the greatest motivation for the dual use of e-learning and textbooks (study 77% vs. control 80%; p=0.42). At the start of the face-to-face course/after preparation at T 2 , the control group reported significantly strong agreement with the use of a digital or another teaching medium (control 3.9±2.4 vs. study 5.1±2.1; p<0.01), or for the use of a combination of several media to increase course motivation (control 3.1±2.1 vs. study 4.1±2.2; p<0.01).
After the face-to-face course at T 3 , the motivation to continue working with ultrasound was very high in both groups but was significantly higher within the study group (study 1.4±0.8 vs. control 1.7±0.8; p<0.01). Groups significantly differed with respect to reported motivation when asked about the teaching medium used for follow-up (study 2.0±1.3 vs. control: 2.6±1.7; p<0.01). The motivation of the control group to use a different teaching medium for course follow-up was significantly higher (study 4.7±2.4 vs. control 3.6±2.5; p<0.01).
Evaluation of the “teaching concept and learning materials” query
The evaluation results of the “training concept”, “preparation”, and “teaching materials” are listed in Supplementary Tables 5 and 6 .
The study group rated the training concept and their satisfaction with it significantly better for all items (p<0.01). The competencies of the tutors were rated very positive in both groups, both regarding their practical skills (study 1.1±0.3 vs. control 1.1±0.2; p=0.15) and their didactic skills (study 1.1±0.33 vs. control mean 1.2±0.5; p=0.68).
The study group rated the item “best possible use of the practical sessions during the preparation time” significantly better than the control group (control 3.3±1.7 vs. study 2.4±1.2; p<0.01). The study group also evaluated the content of work assignments more positively (control 2.9±1.6 vs. study 2.4±1.2; p=0.03).
After the preparation period at T 2 , both groups rated their respective teaching medium very positively for all items (study mean 1.5–2.1 scale points vs. control mean 1.5–2.4 scale points). The e-learning was evaluated significantly more positively in the overall score than the lecture notes (study 1.8±0.7 vs. control 2.0±0.8; p=0.047).
The evaluations of the teaching media tended to improve in both groups at T 3 for almost all items (study mean 1.4–1.9 scale points vs. control mean 1.5–2.2 scale points).
Evaluation of subjective estimation of competencies
The participantsʼ subjective assessment of competencies at the different time points T 1 –T 3 are listed in Supplementary Table 7 . In both groups, a continuous and significant (p<0.01) increase in subjective skills for all items was observed both during the preparation period (T 1 –T 2 ) and the face-to-face course time (T 2 –T 3 ). There were no significant differences between the groups at all time points for all items except for “patient management during the examination” at T 3 , with the study group rating themselves significantly better (study 2.0±1.8 vs. control 2.6±1.7 p<0.01).
Theoretical and Practical Assessments
Theoretical Assessments
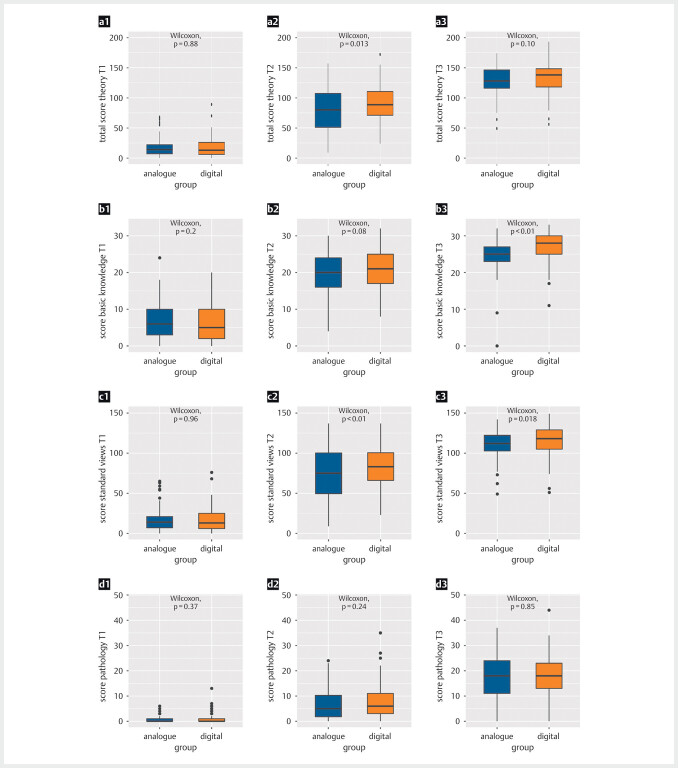
The results of the theoretical tests can be found in Fig. 3 , Supplementary Figure 7 , and Supplementary Tables 8 and 9. For both groups, significant increases (p<0.001) in overall scores and the respective areas of competency were recorded over the course (T 1 –T 2 and T 2 –T 3 ). Based on equivalent results from Theory pre (study group 18±15 vs. control 17±15; p=0.88), the study group achieved both a significantly higher increase in competencies and a significantly higher total score than the control group (study 91±30 vs. control 79±37; p=0.013) in Theory inter at T 2 . The control group, on the other hand, achieved a significantly higher gain from T 2 –T 3 , leading to no significant differences in attainment between the two groups in Theory post (study 133±24 vs. control 28±25; p=0.10). These tendencies can also be seen within almost all competencies except for pathology detection.
Fig. 3.
Boxplot representation of the theoretical test results Results at times T1 (a1–d1), T2 (a2–d2), and T3 (a3–d3) in relation to the total score (a1–a3), basic knowledge (b1–b3), standard cross-sections (c1–c3), and pathologies (d1–d3). The study group using e-learning is shown in orange and the control group using lecture notes is shown in blue.
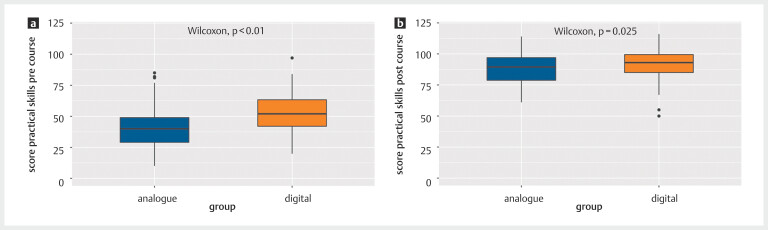
Practical Assessments
The results of the practical tests are shown in Fig. 4 . After the preparation phase, the study group achieved significantly higher scores in Practice inter than the control group (study 53±14 vs. control 41±17; p<0.01). At the end of the face-to-face phase in Practice post , the performance of the study group was also significantly higher (study 92±12 vs. control 88±12; p=0.03). Within both groups, there was also a significant increase in competence from T 2 to T 3 (p<0.01).
Fig. 4.
Boxplot representation of the test results of the practical tests Practical assessment results at times T2 ( a ) and T3 ( b ) in relation to the overall score of the study group (digital-orange) and control group (analog-blue).
Correlations and Influencing Factors
The correlations between the subjective assessment of competencies with the objective competencies as well as the theoretical and practical competencies showed weak-moderate but statistically significant relationships (R 0.17–0.35; p<0.05 in each case).
A multivariate linear regression analysis of the results of the theory tests at T 1 and T 2 as well as the practical examination T 2 , defined “Gender”, “Training before studying the medical field”, “Previous experience in interpreting cross-sectional images”, “Ultrasound examination followed/seen”, and “Ultrasound examination carried out independently” as influencing factors. In the overall T 1 theory assessment, only “Ultrasound examination followed/seen” (standardized regression coefficient β=7.44; p=0.002) had a significant influence.
The subgroup analyses of the preparation times of the theoretical and practical tests at T 2 are shown in Supplementary Figure 8 and Supplementary Table 10 . In Practice Inter , the study group significantly outperformed the control group regardless of preparation time. With respect to theoretical skills, the study group achieved significantly higher scores with a preparation time of<10 hours, but with preparation times of 10 to 20 hours or>20 hours, no significant differences were observed between the groups.
Discussion
Ultrasound education is a critical component of medical training, enabling future physicians to develop essential diagnostic and procedural skills. As medical education evolves in the digital age, the integration of technology with innovative teaching methodologies has increased in importance. This prospective controlled interventional study was conducted to assess the effectiveness of digital versus analog teaching resources via a blended learning/flipped classroom approach in ultrasound education. The results show that the study group, which utilized the e-learning module, outperformed the control group relying on analog lecture notes with respect to various aspects.
A notable observation was that, despite a higher average age and stronger medical background in the study group compared to the control group, both groups exhibited comparable basic knowledge regarding the interpretation of cross-sectional images and ultrasound. The results of the regression analysis suggest that prior knowledge of ultrasound and related fields had no effect, implying that the e-learning module was beneficial independent of prior education 21 30 31 . The motivation of the participants played a crucial role in the use of the respective medium. The study group demonstrated higher motivation during the preparation phase, possibly attributed to the interactive and diverse nature of the e-learning module. It is well-established that motivation strongly influences learning outcomes, as motivated learners are often more engaged and receptive 32 33 .
The evaluation of teaching materials revealed that the study group rated the e-learning module more positively overall than the control group rated their analog lecture notes 6 . Particularly, aspects such as “design” and “optimal utilization of practical sessions due to preparation time” received higher ratings from the study group. These results highlight the advantages of e-learning in visual and interactive learning, especially in an imaging field like sonography. Several studies have shown that e-learning might be an alternative to classroom lectures as it offers the possibility to maximize the time spent on hands-on training and seems to be a feasible method of learning in addition to hands-on ultrasound training 34 35 .
Blended learning, combined with the flipped classroom concept, is a dynamic educational model that capitalizes on the strengths of both traditional and digital learning methods 7 36 37 38 39 . This concept applies modern pedagogical theories that suggest active learning, engagement, and learner-centered education are vital for effective instruction 37 . In this study, e-learning modules offered students the opportunity for independent study before face-to-face sessions, which ensured that students entered practical sessions with solid theoretical knowledge. This in turn allowed instructors to focus on practical applications, skill refinement, and interactive discussions in the classroom 40 . An interesting finding in our study was that the study group consistently performed significantly better with regard to practical skills, regardless of the preparation time. This suggests that the e-learning module effectively enhances practical skill acquisition, emphasizing its utility in hands-on medical training 41 .
The comparison between the digital and analog teaching materials used in our study showed that there was no significant difference in terms of learning outcomes. Participants using the e-learning achieved similar theoretical and practical competencies as those who relied on analog materials. This suggests that well-designed and integrated digital resources can effectively communicate complex medical concepts. During the COVID-19 pandemic, the flexibility of digital resources was particularly beneficial, as e-learning materials remained accessible and suitable for remote learning 42 . In pandemic situations, hand-held ultrasound training has also become established, not least because of the good hygiene of the ultrasound heads 43 . The increased satisfaction with digital resources during the pandemic highlights their potential to address unexpected disruptions in traditional learning environments 44 45 . Since technology cannot entirely replace traditional face-to-face teaching, online instruction has the potential to complement and enrich medical education efforts 46 .
Despite the positive outcomes associated with e-learning, some challenges and opportunities warrant consideration. While the study demonstrated the non-inferiority of e-learning compared to lecture notes, technology is not a one-size-fits-all solution. Learners vary in their preferences, learning styles, and comfort levels with digital tools. Therefore, a comprehensive educational strategy should incorporate a range of resources, tailored to diverse learning preferences.
It would be beneficial to explore the effectiveness of digital resources across different healthcare fields and among students at varying levels of medical training or physicians as part of an ultrasound rotation in interdisciplinary ultrasound training centers or during participation in certified courses 11 39 47 . Moreover, the long-term retention of knowledge and skills acquired through digital learning in comparison to pure analog learning also warrants investigation 48 .
In the future, e-learning could and should be continuously developed to reflect the current state of ultrasound technology and to include other multiparametric procedures such as “fusion” or the use of handheld ultrasound devices 2 43 . In addition, the integration of e-learning into clinical ultrasound training, e. g. in the context of interdisciplinary ultrasound centers or through certified courses, should be pursued in the future in order to meet the high training standards recommended by professional associations even more effectively 11 47 49 50 . This also applies to implementation in student ultrasound training, where greater standardization could be achieved through the use of certified e-learning where appropriate 13 14 51 52 . In addition to the development of ultrasound-specific skills, an improvement in visual-spatial ability, knowledge of anatomical spatial relationships, and radiological cross-sectional image understanding could also be achieved 53 .
Limitations
The evaluation of non-inferiority was focused on immediate learning outcomes and did not address potential differences in long-term retention or real-world clinical application of skills. The study has a potential bias in self-reported data and the lack of a control group receiving neither digital nor analog instruction. Another limitation is the different prior experience of individual study participants. However, this had no significant effect on exam performance, according to the regression calculation.
The scope of the teaching media was not completely the same since videos were shown in e-learning. The random assignment of participants to groups was only performed by semester and not within a semester.
Furthermore, the studyʼs focus on undergraduate medical students raises questions concerning the transferability of findings to other educational levels or healthcare disciplines.
The studyʼs implications extend beyond ultrasound education. As medical education continues to adapt to technological advancements, there is a broader need to investigate the integration of digital resources in various medical specialties. The findings support the incorporation of e-learning in medical curricula, especially in blended learning pedagogy. Educators can apply digital tools to promote active learning, enhance engagement, and provide students with opportunities for self-paced exploration.
Furthermore, our study suggests that a blended learning approach addresses the evolving demands of modern medical education 19 . Medical professionals are expected to be adept at utilizing technology for diagnosis, patient care, and continuous learning. By integrating digital resources into medical curricula, educational institutions contribute to the development of technologically competent healthcare practitioners 54 55 . A further limitation of the study is that not all test instruments were validated. Continued investigation is needed for a comprehensive understanding of the optimal implementation of online teaching. Benchmarks must be developed to define the structure of skill assessment alongside the curriculum. In cases of limited resources, a careful assessment is warranted to ascertain whether online instruction should function as the primary teaching modality or be positioned as a complementary component to hands-on training.
Conclusion
The study provides critical insight into the effectiveness of digital versus analog teaching resources in undergraduate ultrasound education within a flipped classroom model. This prospective controlled study revealed that both digital and analog methods significantly enhanced studentsʼ theoretical and practical ultrasound skills throughout the study period. Notably, the study group, utilizing digital resources, not only achieved higher scores in intermediate and post-course theoretical and practical examinations compared to the control group but also demonstrated a significantly better evaluation of their teaching resources and the training concept as a whole.
A particularly valuable conclusion is that the digital group was able to achieve a similar level of preparedness for practical sessions with a lesser investment in preparation time compared to the analog group. This finding is of paramount importance in the context of a densely packed medical curriculum, where efficient use of time is crucial. The ability of digital resources to provide a more efficient learning pathway without compromising educational outcomes offers a compelling argument for their integration into medical education. This efficiency, coupled with the interactive and flexible nature of e-learning, likely contributed to the higher engagement and motivation observed among learners in the study group. By highlighting the comparative advantages of digital learning resources, including their potential to save time while maintaining or enhancing learning outcomes, this research supports the shift towards more digitally integrated and adaptable learning environments in medical education.
Acknowledgements
This study includes parts of the doctoral thesis of one of the authors (L.H.). We thank all participating students and lecturers for supporting our study. We would like to also thank C. Christe and C. Ille for their help in revising the figures.
Conflict of Interest The authors declare that they have no conflict of interest.
These authors contributed equally to this work and share first authorship
These authors contributed equally to this work and share senior authorship
Supplementary Material
References
- 1.Dietrich C F, Bolondi L, Duck F, Evans D H, Ewertsen C, Fraser A G et al. History of Ultrasound in Medicine from its birth to date (2022), on occasion of the 50 Years Anniversary of EFSUMB. A publication of the European Federation of Societies for Ultrasound In Medicine and Biology (EFSUMB), designed to record the historical development of medical ultrasound. Med Ultrason. 2022;24:434–450. doi: 10.11152/mu-3757. [DOI] [PubMed] [Google Scholar]
- 2.Höpfner M, Weskott H P.Fusion imaging – ein neues Verfahren zur Bildfusion sonografischer und radiologischer Schnittbildverfahren Ultraschall Med 200930V18_02.
- 3.Clevert D A, Beyer G, Nieß H, Schlenker B. Ultrasound—New Techniques Are Extending the Applications. Dtsch Arztebl Int. 2023;120:41–47. doi: 10.3238/arztebl.m2022.0380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weimer J M, Beer D, Schneider C, Yousefzada M, Gottwald M, Züllich T F et al. Inter-System Variability of Eight Different Handheld Ultrasound (HHUS) Devices— A Prospective Comparison of B-Scan Quality and Clinical Significance in Intensive Care. Diagnostics. 2024;14:54. doi: 10.3390/diagnostics14010054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Merkel D, Züllich T F, Schneider C, Yousefzada M, Beer D, Ludwig M et al. Prospective Comparison of Handheld Ultrasound Devices from Different Manufacturers with Respect to B-Scan Quality and Clinical Significance for Various Abdominal Sonography Questions. Diagnostics. 2023;13:3622. doi: 10.3390/diagnostics13243622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hempel D, Sinnathurai S, Haunhorst S, Seibel A, Michels G, Heringer F et al. Influence of case-based e-learning on studentsʼ performance in point-of-care ultrasound courses: a randomized trial. European journal of emergency medicine : official journal of the European Society for. Emergency Medicine. 2016;23:298–304. doi: 10.1097/MEJ.0000000000000270. [DOI] [PubMed] [Google Scholar]
- 7.Röhrig S, Hempel D, Stenger T, Armbruster W, Seibel A, Walcher F et al. [Which learning methods are expected for ultrasound training? Blended learning on trial] Anaesthesist. 2014;63:745–752. doi: 10.1007/s00101-014-2370-3. [DOI] [PubMed] [Google Scholar]
- 8.Gillispie V. Using the Flipped Classroom to Bridge the Gap to Generation Y. Ochsner J. 2016;16:32–36. [PMC free article] [PubMed] [Google Scholar]
- 9.Stockwell B R, Stockwell M S, Cennamo M, Jiang E. Blended Learning Improves Science Education. Cell. 2015;162:933–936. doi: 10.1016/j.cell.2015.08.009. [DOI] [PubMed] [Google Scholar]
- 10.Tolks D, Schäfer C, Raupach T, Kruse L, Sarikas A, Gerhardt-Szép S et al. An Introduction to the Inverted/Flipped Classroom Model in Education and Advanced Training in Medicine and in the Healthcare Professions. GMS J Med Educ. 2016;33:Doc46. doi: 10.3205/zma001045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blank V, Strobel D, Karlas T. Digital Training Formats in Ultrasound Diagnostics for physicians: What options are available and how can they be successfully integrated into current DEGUM certified course concepts? Ultraschall Med. 2022;43:428–434. doi: 10.1055/a-1900-8166. [DOI] [PubMed] [Google Scholar]
- 12.McLaughlin J E, Roth M T, Glatt D M, Gharkholonarehe N, Davidson C A, Griffin L M et al. The flipped classroom: a course redesign to foster learning and engagement in a health professions school. Acad Med. 2014;89:236–243. doi: 10.1097/ACM.0000000000000086. [DOI] [PubMed] [Google Scholar]
- 13.Hoffmann B, Blaivas M, Abramowicz J, Bachmann M, Badea R, Braden B et al. Medical Student Ultrasound Education, a WFUMB Position Paper, Part II. A consensus statement of ultrasound societies. Med Ultrason. 2020;22:220–229. doi: 10.11152/mu-2599. [DOI] [PubMed] [Google Scholar]
- 14.Dietrich C F, Hoffmann B, Abramowicz J, Badea R, Braden B, Cantisani V et al. Medical Student Ultrasound Education: A WFUMB Position Paper, Part I. Ultrasound Med Biol. 2019;45:271–281. doi: 10.1016/j.ultrasmedbio.2018.09.017. [DOI] [PubMed] [Google Scholar]
- 15.Cantisani V, Dietrich C, Badea R, Dudea S, Prosch H, Cerezo E et al. EFSUMB Statement on Medical Student Education in Ultrasound [long version] Ultrasound International Open. 2016;02:E2–E7. doi: 10.1055/s-0035-1569413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hoppmann R A, Mladenovic J, Melniker L, Badea R, Blaivas M, Montorfano M et al. International consensus conference recommendations on ultrasound education for undergraduate medical students. The Ultrasound Journal. 2022;14:31. doi: 10.1186/s13089-022-00279-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dettmer S, Barkhausen J, Volmer E, Mentzel H J, Reinartz S, Voigt F et al. White Paper: Radiology Curriculum for Undergraduate Medical Education in Germany and Integration into the NKLM 2.0. Rofo. 2021;193:1294–1303. doi: 10.1055/a-1586-3372. [DOI] [PubMed] [Google Scholar]
- 18.Bundesvereinigung K.Mehr Flexibilität bei Teilnahme an Ultraschallkursen KBV.de2021 [cited 2024 12.02]. Available from:https://www.kbv.de/html/1150_54959.php
- 19.Ruiz J G, Mintzer M J, Leipzig R M. The impact of E-learning in medical education. Acad Med. 2006;81:207–212. doi: 10.1097/00001888-200603000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Soni V D. Global Impact of E-learning during COVID 19. SSRN Electronic Journal. 2020;12 doi: 10.2139/ssrn.3630073. [DOI] [Google Scholar]
- 21.Lien W C, Lin P, Chang C H, Wu M C, Wu C Y. The effect of e-learning on point-of-care ultrasound education in novices. Med Educ Online. 2023;28:2.152522E6. doi: 10.1080/10872981.2022.2152522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rampton V, Mittelman M, Goldhahn J. Implications of artificial intelligence for medical education. The Lancet Digital Health. 2020;2:e111–e112. doi: 10.1016/S2589-7500(20)30023-6. [DOI] [PubMed] [Google Scholar]
- 23.Tarique U, Tang B, Singh M, Kulasegaram K M, Ailon J. Ultrasound Curricula in Undergraduate Medical Education: A Scoping Review. J Ultrasound Med. 2018;37:69–82. doi: 10.1002/jum.14333. [DOI] [PubMed] [Google Scholar]
- 24.Moher D, Hopewell S, Schulz K F, Montori V, Gøtzsche P C, Devereaux P J et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. Bmj. 2010;340:c869. doi: 10.1136/bmj.c869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Höhne E, Recker F, Dietrich C F, Schäfer V S. Assessment Methods in Medical Ultrasound Education. Front Med (Lausanne) 2022;9:871957. doi: 10.3389/fmed.2022.871957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weimer J, Dionysopoulou A, Strelow K-U, Buggenhagen H, Weinmann-Menke J, Dirks K et al. Undergraduate ultrasound training: prospective comparison of two different peer assisted course models on national standards. BMC Medical Education. 2023;23:513. doi: 10.1186/s12909-023-04511-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.DEGUM e. V. & Keim et al. Curriculum Abdomen DEGUM.de: DEGUM; 2013 [cited 2022 10.10.]. Available from:https://www.degum.de/fachgebiete/sektionen/innere-medizin/kurse/curriculum-abdomen.html
- 28.Puthiaparampil T, Rahman M M. Very short answer questions: a viable alternative to multiple choice questions. BMC Medical Education. 2020;20:141. doi: 10.1186/s12909-020-02057-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hofer M, Kamper L, Sadlo M, Sievers K, Heussen N. Evaluation of an OSCE assessment tool for abdominal ultrasound courses. Ultraschall Med. 2011;32:184–190. doi: 10.1055/s-0029-1246049. [DOI] [PubMed] [Google Scholar]
- 30.Arroyo-Morales M, Cantarero-Villanueva I, Fernández-Lao C, Guirao-Piñeyro M, Castro-Martín E, Díaz-Rodríguez L. A blended learning approach to palpation and ultrasound imaging skills through supplementation of traditional classroom teaching with an e-learning package. Man Ther. 2012;17:474–478. doi: 10.1016/j.math.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 31.Stoehr F, Yang Y, Müller L, Gerstenmeier P, Pinto dos Santos D, Dietz P A blended learning approach for teaching thoracic radiology to medical students: a proof-of-concept study. Front Med. p. 1.272893E6. [DOI] [PMC free article] [PubMed]
- 32.Kusurkar R A, Ten Cate T J, van Asperen M, Croiset G. Motivation as an independent and a dependent variable in medical education: A review of the literature. Medical Teacher. 2011;33:e242–e262. doi: 10.3109/0142159X.2011.558539. [DOI] [PubMed] [Google Scholar]
- 33.Weimer J M, Rink M, Vieth T, Lauff J, Weimer A, Müller L et al. Development and evaluation of a point-of-care ocular ultrasound curriculum for medical students – a proof-of-concept study. BMC Med Educ. 2023;23:723. doi: 10.1186/s12909-023-04723-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hempel D, Haunhorst S, Sinnathurai S, Seibel A, Recker F, Heringer F et al. Social media to supplement point-of-care ultrasound courses: the “sandwich e-learning” approach. A randomized trial. Crit Ultrasound J. 2016;8:3. doi: 10.1186/s13089-016-0037-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Beaulieu Y, Laprise R, Drolet P, Thivierge R L, Serri K, Albert M et al. Bedside ultrasound training using web-based e-learning and simulation early in the curriculum of residents. Critical Ultrasound Journal. 2015;7:1. doi: 10.1186/s13089-014-0018-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Heiberg J, Hansen L S, Wemmelund K, Sørensen A H, Ilkjaer C, Cloete E et al. Point-of-Care Clinical Ultrasound for Medical Students. Ultrasound Int Open. 2015;1:E58–E66. doi: 10.1055/s-0035-1565173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vallée A, Blacher J, Cariou A, Sorbets E. Blended Learning Compared to Traditional Learning in Medical Education: Systematic Review and Meta-Analysis. J Med Internet Res. 2020;22:e16504. doi: 10.2196/16504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nagaraj C, Yadurappa S B, Anantharaman L T, Ravindranath Y, Shankar N. Effectiveness of blended learning in radiological anatomy for first year undergraduate medical students. Surg Radiol Anat. 2021;43:489–496. doi: 10.1007/s00276-020-02572-x. [DOI] [PubMed] [Google Scholar]
- 39.Weimer A M, Berthold R, Schamberger C et al. Digital Transformation in Musculoskeletal Ultrasound: Acceptability of Blended Learning. Diagnostics (Basel) 2023;13:3272. doi: 10.3390/diagnostics13203272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Michael D, Renate M-P. The role of structure, patterns, and people in blended learning. The Internet and Higher Education. 2005;8:111–130. [Google Scholar]
- 41.Bylieva D, Lobatyuk V, Safonova A, Rubtsova A. Correlation between the Practical Aspect of the Course and the E-Learning Progress. Education Sciences. 2019;9:167. [Google Scholar]
- 42.Almarzooq Z I, Lopes M, Kochar A. Virtual Learning During the COVID-19 Pandemic: A Disruptive Technology in Graduate Medical Education. J Am Coll Cardiol. 2020;75:2635–2638. doi: 10.1016/j.jacc.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kaiser U, Dropco I, Reuthner K, Ertl M, Schlitt H J, Herr W et al. Wireless handheld focused ultrasound in student teaching during the COVID-19 pandemic: Initial results of a pilot study 1. Clinical Hemorheology and Microcirculation. 2023;85:297–305. doi: 10.3233/CH-229104. [DOI] [PubMed] [Google Scholar]
- 44.Stoehr F, Müller L, Brady A, Trilla A, Mähringer-Kunz A, Hahn F et al. How COVID-19 kick-started online learning in medical education-The DigiMed study. PLoS One. 2021;16:e0257394. doi: 10.1371/journal.pone.0257394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stoehr F, Müller L, Brady A P, Catalano C, Mildenberger P, Mähringer-Kunz A et al. Online teaching in radiology as a pilot model for modernizing medical education: results of an international study in cooperation with the ESR. Insights Imaging. 2021;12:141. doi: 10.1186/s13244-021-01092-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Höhne E, Recker F, Schmok E, Brossart P, Raupach T, Schäfer V S. Conception and Feasibility of a Digital Tele-Guided Abdomen, Thorax, and Thyroid Gland Ultrasound Course for Medical Students (TELUS study) Ultraschall Med. 2023;44:194–202. doi: 10.1055/a-1528-1418. [DOI] [PubMed] [Google Scholar]
- 47.Clevert D A, Jung E M, Weber M A, Lerchbaumer M H, Willinek W, Fischer T. Concepts in the Establishment of Interdisciplinary Ultrasound Centers: The Role of Radiology. Rofo. 2022;194:1322–1332. doi: 10.1055/a-1853-7443. [DOI] [PubMed] [Google Scholar]
- 48.Weimer J M, Widmer N, Strelow K-U, Hopf P, Buggenhagen H, Dirks K et al. Long-Term Effectiveness and Sustainability of Integrating Peer-Assisted Ultrasound Courses into Medical School – A Prospective Study. Tomography. 2023;9:1315–1328. doi: 10.3390/tomography9040104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wüstner M, Radzina M, Calliada F, Cantisani V, Havre R F, Jenderka K V et al. Professional Standards in Medical Ultrasound – EFSUMB Position Paper (Long Version) – General Aspects. Ultraschall Med. 2022;43:e36–e48. doi: 10.1055/a-1857-4435. [DOI] [PubMed] [Google Scholar]
- 50.Cantisani V, Jenssen C, Dietrich C F, Ewertsen C, Piscaglia F. Clinical Practice Guidance and Education in Ultrasound: Evidence and experience are two sides of one coin! Ultraschall Med. 2022;43:7–11. doi: 10.1055/a-1699-7473. [DOI] [PubMed] [Google Scholar]
- 51.Neubauer R, Bauer C J, Dietrich C F, Strizek B, Schäfer V S, Recker F.Evidence-based Ultrasound Education? – A Systematic Literature Review of Undergraduate Ultrasound Training Studies Ultrasound Int Open 2024. 10(continuous publication).
- 52.Dietrich C F, Sirli R L, Barth G, Blaivas M, Daum N, Dong Y Student ultrasound education – current views and controversies. Ultraschall Med. 2024. [DOI] [PubMed]
- 53.Weimer J, Ruppert J, Vieth T, Weinmann-Menke J, Buggenhagen H, Künzel J et al. Effects of undergraduate ultrasound education on cross-sectional image understanding and visual-spatial ability – a prospective study. BMC Med Educ. 2024;24:619. doi: 10.1186/s12909-024-05608-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Carstensen SM D, Just S A, Velander M, Konge L, Hubel M S, Rajeeth Savarimuthu T E-learning and practical performance in musculoskeletal ultrasound: a multicenter randomized study. Rheumatology (Oxford) 2023. pp. 3547–3554. [DOI] [PubMed]
- 55.Haskins S C, Feldman D, Fields K G, Kirksey M A, Lien C A, Luu T H et al. Teaching a Point-of-Care Ultrasound Curriculum to Anesthesiology Trainees With Traditional Didactic Lectures or an Online E-Learning Platform: A Pilot Study. J Educ Perioper Med. 2018;20:E624. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.