Sir,
Traumatic pulmonary pseudocyst also described as pulmonary pneumatocele is an uncommon clinical entity with the available literature restricted to mostly case reports. These results from lung parenchyma are violated by a blunt or penetrating injury to the chest. The concussion force applied on the chest causes shearing of lung parenchyma creating cysts that get filled with blood or air until there is equalisation of pressures.[1] The most commonly reported mode of injury for the development of pulmonary pseudocysts is road traffic accidents; rare etiologies like guide wire manipulation, chest tube insertion, and barotrauma have also been described in the medical literature. These are called pseudocysts as their walls are formed by interlobar interstitial connective tissue and lack bronchial elements, while on the other hand, true cysts are enclosed by epithelial tissue.[2] We herein describe our experience in managing one of these rare entities.
A 40-year-old male with no known co-morbidities was brought to the emergency department of our centre after sustaining a road traffic accident. He was fully conscious and oriented and had stable hemodynamics except for tachypnea. On examination, he had contusion over the right upper chest wall. Systemic examination revealed crepitus over the right hemithorax on palpation along with reduced breath sounds in the right infraclavicular region and occasional scattered crackles over the bilateral lung field (right > left). He had an elevated white blood cell count of 12,350/cumm with neutrophilia (89%) and abnormal liver function (aspartate transaminase/alanine aminotransferase: 564/469 U/L). Chest radiography showed non-homogeneous opacity limited by the horizontal fissure in the right lung [Figure 1]. Computed tomography (CT) of the chest revealed a right-sided pneumothorax, subcutaneous emphysema, and pneumomediastinum. A large consolidation was visualised in the right upper lobe with an irregular cavity within, and consolidation with small cavitary lesions was visualised in bilateral lower lobe superior and posterior-basal segments [Figure 2]. A diagnosis of traumatic pneumatocele was made, and he was managed conservatively with wound care, analgesics, high-flow oxygen therapy, and close observation. His condition gradually improved and was discharged after 2 weeks. A follow-up CT chest after 4 weeks showed resolution of pneumothorax, subcutaneous emphysema, and pneumomediastinum. The large pneumatocele in the right upper lobe showed a reduction in size and had an air-fluid level [Figure 3]. The patient remained asymptomatic, and a follow- up chest CT done at 3 months showed near complete resolution with the right upper lobe pneumatocele replaced by a fibronodular scar [Figure 4].
Figure 1.
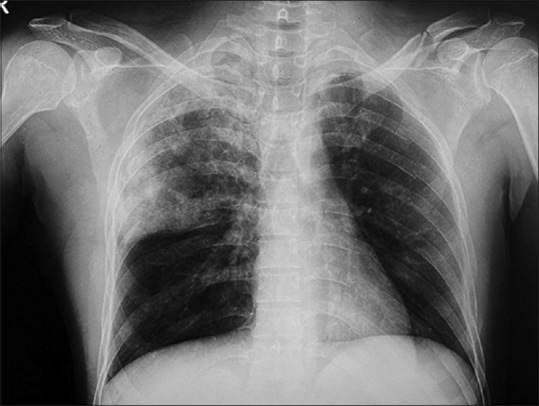
Chest radiograph PA view showing non-homogeneous opacity in right upper and mid zone limited by horizontal fissure below
Figure 2.
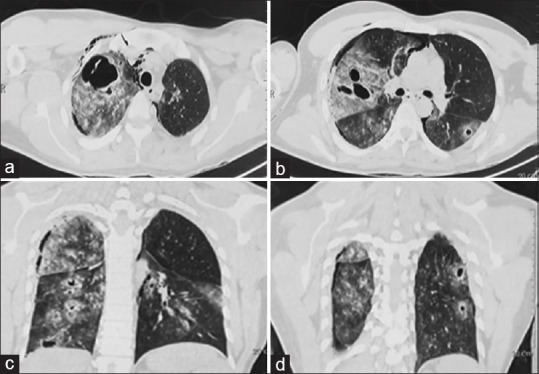
CT of the chest (a and b) Axial section showing subcutaneous emphysema with pneumomediastinum, pneumothorax along with large consolidation and cavity of the right upper and cystic lesion in the superior segment of left lower lobe. (c and d) Coronal section showing multiple cystic lesions in bilateral lungs
Figure 3.
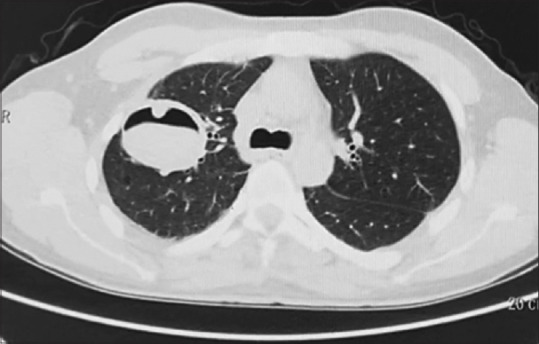
CT of the chest taken 4 weeks post injury - axial section shows residual large cyst with air-fluid level inside along with the resolution of the smaller cystic lesion
Figure 4.
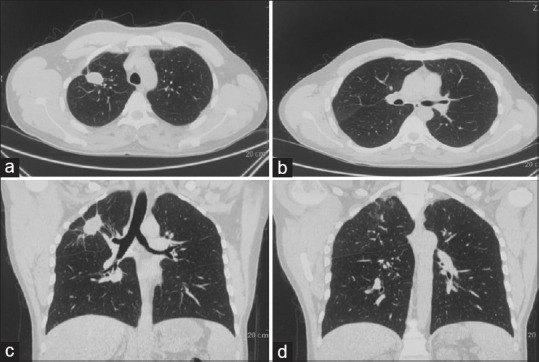
Follow-up CT of the chest taken after 3 months (a and b) Axial section (c and d) Coronal section showing showing near complete resolution with fibro nodular opacity in right upper lobe
Traumatic pulmonary pseudocysts are mostly seen in children and young adults.[3] This subset of the population has significant chest wall compliance, leading to better transmission of compressive forces to the lung parenchyma. In older adults, compressive blunt injury to the chest results mostly in rib and sternal fractures rather than a pulmonary pseudocyst. A male predominance might be because of disproportionately more males suffering from trauma. There is a proposed two-step mechanism in development of pulmonary pseudocyst. The first step is the compressive force applied to the chest, causing an increase in intra-parenchymal pressure, leading to lung laceration. The second step involves decompression of the chest, which allows the elastic tissue of the lung to recoil; the negative pressure created inside the cavity draws in air and blood till the pressure inside the cavity equals the surrounding parenchyma.[4] Traumatic pulmonary pseudocyst usually manifests within 24–48 hours following blunt chest trauma, and its clinical manifestation can range from the patient being asymptomatic to developing acute respiratory distress syndrome.[2] Chest pain, dyspnoea, cough, and hemoptysis have been reported in these patients.[5] The diagnosis is based on history and imaging findings. These pseudocysts have a lower lobe predominance with a relative sparing of apices. Chest radiography is less sensitive when taken on the day of injury; the sensitivity improves after day 5 of injury due to resolution of lung contusion, making the pseudocyst more evident.[2] CT has a very high sensitivity and helps to make an early diagnosis and visualise associated injuries like rib fractures and lung contusions. The typical appearance on CT is that of a thin-walled cavity with associated lung contusion. The management is mostly conservative with video-assisted thoracoscopic surgery (VATS) done in the case of persistent air leak, extensive bleeding causing hemothorax, or an unexpanded lung.
In conclusion, traumatic pulmonary pseudocysts should be kept as a differential by treating physicians when they encounter lung cavities post-chest trauma. Though the treatment is mostly conservative, close follow-up must be kept to identify complications and select patients who would benefit from surgical intervention.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Moore FA, Moore EE, Haenel JB, Waring BJ, Parsons PE. Post-traumatic pulmonary pseudocyst in the adult: Pathophysiology, recognition, and selective management. J Trauma Acute Care Surg. 1989;29:1380–5. doi: 10.1097/00005373-198910000-00016. [DOI] [PubMed] [Google Scholar]
- 2.Phillips B, Shaw J, Turco L, McDonald D, Carey J, Balters M, et al. Traumatic pulmonary pseudocyst: An underreported entity. Injury. 2017;48:214–20. doi: 10.1016/j.injury.2016.12.006. [DOI] [PubMed] [Google Scholar]
- 3.Chon SH, Lee CB, Kim H, Chung WS, Kim YH. Diagnosis and prognosis of traumatic pulmonary psuedocysts: A review of 12 cases. Eur J Cardiothorac Surg. 2006;29:819–23. doi: 10.1016/j.ejcts.2006.01.054. [DOI] [PubMed] [Google Scholar]
- 4.Khan FA, Phillips W, Khan A, Seriff NS. Unusual unilateral blunt chest trauma without rib fractures leading to pulmonary laceration requiring pneumonectomy. Chest. 1974;66:211–4. doi: 10.1378/chest.66.2.211. [DOI] [PubMed] [Google Scholar]
- 5.Yang PJ, Tsai IT, Liu TH. Traumatic pulmonary pseudocyst. J Pediatr. 2015;167:777. doi: 10.1016/j.jpeds.2015.06.025. [DOI] [PubMed] [Google Scholar]


