Abstract
Spontaneous lateral sphenoid cephalocele (SLSC) is the herniation of intracranial contents through a bony defect in the lateral sphenoid, without predisposing factors. SLSC pathogenesis is associated with idiopathic intracranial hypertension (IIH); however, the relationship between IIH and SLSC is not fully understood due to the limited number of published case reports. Here, we report a unique case of SLSC in a 39-year-old female who presented with a combination of a lateral sphenoid cephalocele and multiple radiologic findings indicative of IIH, some of which have never been described in previously published case reports. This case highlights the possibility that chronically elevated intracranial pressure may be a determining factor in SLSC development.
Keywords: Cephalocele, Sphenoid Bone, Idiopathic Intracranial Hypertension, Computed Tomography, Magnetic Resonance Imaging
Abstract
자발성 측면 접형골형 뇌류는 어떠한 선행 요인 없이 측면 접형골의 결손을 통하여 두개 내 구조물이 탈출하는 것을 의미한다. 자발성 측면 접형골형 뇌류의 발병 원인은 특발성 두개 내 고혈압이 동반되어 발생하는 것으로 여겨지고 있다. 그러나, 이에 대한 연구는 제한적으로, 추가적인 이해와 연구가 필요하다. 이에 우리는 39세 여성에서 발생한 특이한 자발성 측면 접형골형 뇌류 증례를 보고하고자 한다. 이 증례 환자의 뇌 영상 사진에서 측면 접형골형 뇌류와 특발성 두개 내 고혈압을 시사하는 여러 영상학적 소견들의 조합을 확인할 수 있으며, 이 중 일부는 이전에 보고된 다른 증례에서는 함께 기술된 적이 없는 소견이다. 이는 만성적으로 상승한 두개 내 압력이 자발적 측면 접형골형 뇌류의 발생에 결정적인 영향을 준다는 가설을 더욱 지지해 준다.
INTRODUCTION
Spontaneous lateral sphenoid cephalocele (SLSC) is the herniation of intracranial contents through a bony defect in the lateral sphenoid in the absence of predisposing factors such as trauma, prior surgery, tumors, or congenital malformations (1,2). SLSC pathogenesis has been proposed to be a rare manifestation of idiopathic intracranial hypertension (IIH) resulting from an anatomic predisposition (3). However, the understanding of this phenomenon is incomplete owing to a limited number of studies. This report presents a unique case of SLSC in a 39-year-old female who presented with an acute headache and chronic watery rhinorrhea. The accompanying radiological hallmarks were suggestive of elevated intracranial pressure (ICP) and a lateral sphenoid cephalocele was identified on brain CT and MR. This case report strengthens the proposed association between SLSC and IIH by describing lateral sphenoid cephalocele and radiological findings indicative of IIH, some of which have not been previously addressed together.
CASE REPORT
A 39-year-old female patient visited the emergency department with a sudden onset headache and a one-year history of intermittent watery rhinorrhea from the right nostril. During the previous three weeks, the patient had experienced cold-like symptoms and had been taking antibiotics for approximately two weeks. The patient presented no history of surgery, trauma, tumors, or congenital malformations. A physical examination revealed left-sided temporal hemianopia and neck stiffness. Laboratory blood tests reported a white blood cell (WBC) count of 22.20 k/uL, a high neutrophil percentage of 86.2%, and an elevated level of C-reactive protein at 2.1 mg/dL. Cerebrospinal fluid (CSF) analysis revealed an opening pressure of 32 cmH2O and the CSF appeared turbid. The CSF WBC count was 580/uL with a high protein value of 167 mg/dL and a decreased CSF/blood glucose ratio of 0.33, clinically suggestive of bacterial meningitis.
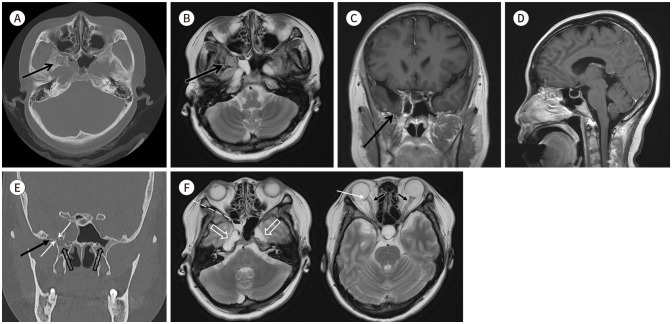
Multilobulated bony erosion in the greater wing of the right sphenoid bone, indicative of an arachnoid pit, was detected on the initial brain CT (Fig. 1A). Within the lesion, a soft-tissue mass-like lesion was noted, which appeared isodense with the brain parenchyma on CT and followed the signal intensity (SI) of the brain parenchyma on MR (Fig. 1B). The lesion showed continuity with the adjacent temporal lobe parenchyma on multiplanar imaging (Fig. 1B, C), suggesting herniation of the right temporal lobe. This accounted for the asymmetric widening of the right Sylvian fissure and downward displacement of the right temporal lobe compared to the left side. Brain MR revealed a CSF collection in the right sphenoid sinus (Fig. 1F). Coronal bone algorithm CT revealed a bony defect at the lateral recess of the right sphenoid sinus that communicated with the arachnoid pit (Fig. 1E). Accordingly, the CSF collection observed in the right sphenoid sinus was suggested to be due to CSF leakage.
Fig. 1. Spontaneous lateral sphenoid cephalocele in a 39-year-old female patient, presenting radiologic features indicative of intracranial hypertension.
A. Axial brain CT image in the bone window shows a multilobulated shaped bony erosion (arrow) in the greater wing of the right sphenoid bone.
B. T2-weighted axial brain MRI shows an isodense lesion (arrow) with brain parenchyma within the space. The lesion also shows continuity with the adjacent temporal lobe parenchyma.
C. T1 enhanced coronal brain MRI shows a lesion (arrow) contiguous with the adjacent temporal lobe parenchyma.
D. T1 enhanced sagittal brain MRI shows sella turcica widening and a partially empty sella.
E. Coronal bone algorithm CT demonstrating pneumatization of bilateral sphenoid sinuses extending to the lateral recess, the right side of which is opacified with CSF (empty arrows). Additionally, it reveals a bony defect (white arrows), which communicates between the lateral recess of the right sphenoid sinus and the arachnoid pit (black arrow).
F. T2 axial brain MRI (left) shows the air-fluid level in the right sphenoid sinus (dashed line) and bilateral widening of Meckel’s cave (open arrows). T2 axial brain MRI (right) shows a small amount of CSF accumulation within the bilateral optic nerve sheaths (black arrows) and sclera flattening of the right posterior globe (white arrow).
CSF = cerebrospinal fluid
In addition, brain MR revealed widening of the sella turcica and a partially empty sella (Fig. 1D). Brain CT revealed pneumatization of the bilateral sphenoid sinuses extending to the lateral recesses, the right side of which was opacified with cerebrospinal fluid (CSF) (Fig. 1E). Brain MR also identified widening of the Meckel’s cave as well as a small amount of bilateral perioptic CSF accumulation and scleral flattening of the right posterior globe (Fig. 1F). Based on these findings, including the arachnoid pit, we postulated that the ICP was chronically elevated. There was no evidence of hydrocephalus, mass, or other underlying deformities that increased the likelihood of an IIH diagnosis. Furthermore, MR revealed a focal T1 high-SI lesion in the right frontal lobe accompanied by mild perilesional edema and focal adjacent parenchymal enhancement. Brain MR also revealed adjacent dural thickening with enhancement in both frontal lobes and diffuse leptomeningeal enhancement. These radiological findings suggest meningoencephalitis in the right frontal lobe and combined hemorrhage as complications of SLSC.
The patient underwent endoscopic transsphenoidal surgery. Bony erosion with herniated brain tissue and CSF leakage in the greater wing of the right sphenoid were observed. The identified cephalocele was repaired without any intra- or postoperative events.
This study was approved by the Institutional Review Board of our institution (IRB No. ISPAIK 2023-11-005). Informed consent was waived due to the retrospective nature of the study.
DISCUSSION
SLSCs are rare encephaloceles that extend into the lateral sphenoid bone without any predisposing factors (1,2). SLSC pathogenesis was previously assumed to be congenital in the early phase but has changed in many retrospective cohort studies (4). SLSC development is recognized as an interaction between altered CSF hemodynamics (chronically elevated or largely fluctuating CSF pressure) and predisposing anatomical factors (3). In this case, CT and MR revealed an arachnoid pit, pneumatization of the lateral recess of the sphenoid sinus (SS), and an empty or partially empty sella. Concerning demographic and clinical aspects, SLSCs develop predominantly in female, middle-aged, and obese patients. These postulated contributing factors to SLSC development, notably, were found to mirror the characteristics of IIH in some retrospective cohort studies. Therefore, SLSCs have been presumed to be a rare manifestation of IIH (1,5,6,7,8,9,10).
In this case report, the patient’s brain CT and MR images described these shared characteristics, including an SLSC of the right greater sphenoid wing, with the following findings: an underlying arachnoid pit, pneumatization of the bilateral lateral recess of the SS, and a partially empty sella. The patient was a 39-year-old female with a BMI of 27.0. In addition, we identified other important radiological markers of IIH using brain imaging: sella turcica widening, posterior scleral flattening, CSF accumulation within the optic nerve sheath, and widening of both Meckel’s caves (9). This case report did not include some radiographic signs of elevated ICP, such as vertical tortuosity of the optic nerve sheath, or slit-like ventricles. However, to the best of our knowledge, this case described the largest number of the findings compared to previous reports. Moreover, this case study presents a novel combination of radiographic findings suggesting elevated ICP in that neither increased perioptic CSF nor Meckel’s cave widening has been radiologically illustrated with pneumatization of the lateral recess of the SS in previous SLSC cases. This strengthens the hypothesis that SLSC development is attributable to underlying IIH.
This case provides definitive evidence for both radiologists and clinicians that patients presenting with SLSC on brain imaging should be suspected of having IIH. This also implies that doctors need to be fully aware of the radiologic findings indicating underlying IIH, as well as the possible manifestations of SLSC. Patients with IIH should be regularly monitored for the development of SLSC, a potential complication that is prevented through ICH control. The importance of ICH management can be emphasized by the SLSC complications associated with CSF leakage, including ascending infection, seizure, or hemorrhage, some of which were also confirmed in our case by brain imaging.
In conclusion, we discuss a rare case of SLSC that radiologically presented with the co-existence of IIH. The detailed and novel radiological findings in this patient emphasize that IIH plays a pivotal role in inducing osseous erosion, predisposing particular cranial regions to subsequent encephalocele development. Recognizing these radiological signs can provide insights into the pathogenesis of these rare entities and may guide therapeutic interventions targeting the underlying intracranial hypertension.
Footnotes
- Conceptualization, L.B.
- data curation, L.B.
- investigation, L.B.
- methodology, L.B.
- project administration, L.B.
- supervision, L.B.
- validation, L.B., H.Y.J.
- visualization, K.D.W., L.B.
- writing—original draft, K.D.W.
- writing—review & editing, L.B., H.Y.J.
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
Funding: None
References
- 1.Shetty PG, Shroff MM, Fatterpekar GM, Sahani DV, Kirtane MV. A retrospective analysis of spontaneous sphenoid sinus fistula: MR and CT findings. AJNR Am J Neuroradiol. 2000;21:337–342. [PMC free article] [PubMed] [Google Scholar]
- 2.Woodworth BA, Palmer JN. Spontaneous cerebrospinal fluid leaks. Curr Opin Otolaryngol Head Neck Surg. 2009;17:59–65. doi: 10.1097/MOO.0b013e3283200017. [DOI] [PubMed] [Google Scholar]
- 3.Settecase F, Harnsberger HR, Michel MA, Chapman P, Glastonbury CM. Spontaneous lateral sphenoid cephaloceles: anatomic factors contributing to pathogenesis and proposed classification. AJNR Am J Neuroradiol. 2014;35:784–789. doi: 10.3174/ajnr.A3744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barañano CF, Curé J, Palmer JN, Woodworth BA. Sternberg’s canal: fact or fiction? Am J Rhinol Allergy. 2009;23:167–171. doi: 10.2500/ajra.2009.23.3290. [DOI] [PubMed] [Google Scholar]
- 5.Lloyd KM, DelGaudio JM, Hudgins PA. Imaging of skull base cerebrospinal fluid leaks in adults. Radiology. 2008;248:725–736. doi: 10.1148/radiol.2483070362. [DOI] [PubMed] [Google Scholar]
- 6.Schuknecht B, Simmen D, Briner HR, Holzmann D. Nontraumatic skull base defects with spontaneous CSF rhinorrhea and arachnoid herniation: imaging findings and correlation with endoscopic sinus surgery in 27 patients. AJNR Am J Neuroradiol. 2008;29:542–549. doi: 10.3174/ajnr.A0840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schlosser RJ, Bolger WE. Significance of empty sella in cerebrospinal fluid leaks. Otolaryngol Head Neck Surg. 2003;128:32–38. doi: 10.1067/mhn.2003.43. [DOI] [PubMed] [Google Scholar]
- 8.Schlosser RJ, Woodworth BA, Wilensky EM, Grady MS, Bolger WE. Spontaneous cerebrospinal fluid leaks: a variant of benign intracranial hypertension. Ann Otol Rhinol Laryngol. 2006;115:495–500. doi: 10.1177/000348940611500703. [DOI] [PubMed] [Google Scholar]
- 9.Silver RI, Moonis G, Schlosser RJ, Bolger WE, Loevner LA. Radiographic signs of elevated intracranial pressure in idiopathic cerebrospinal fluid leaks: a possible presentation of idiopathic intracranial hypertension. Am J Rhinol. 2007;21:257–261. doi: 10.2500/ajr.2007.21.3026. [DOI] [PubMed] [Google Scholar]
- 10.Woodworth BA, Prince A, Chiu AG, Cohen NA, Schlosser RJ, Bolger WE, et al. Spontaneous CSF leaks: a paradigm for definitive repair and management of intracranial hypertension. Otolaryngol Head Neck Surg. 2008;138:715–720. doi: 10.1016/j.otohns.2008.02.010. [DOI] [PubMed] [Google Scholar]