Abstract
Background
Rapid public defibrillation with automated external defibrillators (AEDs) is critical to improving out-of-hospital cardiac arrest survival. Concerns about AED theft and vandalism have led to implementing security measures, including locked cabinets. This scoping review, conducted as part of the evidence review for the International Liaison Committee on Resuscitation, explores the impact of securing AEDs in locked cabinets.
Methods
Searches of Medline, Embase, Cochrane, CINAHL (from database inception to 25/5/2024) and Google Scholar (first 200 articles). Studies of any type or design, published with an English abstract, examining the impact of locked AED cabinets were included. The included studies were grouped by outcomes, and an iterative narrative synthesis was performed.
Results
We screened 2,096 titles and found 10 relevant studies: 8 observational studies (4 published as conference abstracts) and 2 simulation studies. No study reported patient outcomes. Studies reported data on between 36 and 31,938 AEDs. Most studies reported low rates (<2%) of theft/missing/vandalism, including AEDs that were accessible 24/7. The only study comparing unlocked and locked cabinets showed minimal difference in theft and vandalism rates (0.3% vs. 0.1%). Two simulation studies showed significantly slower AED retrieval when additional security measures, included locked cabinets, were used. A survey of first responders reported half (25/50) were injured while accessing an AED that required breaking glass to access.
Conclusion
The limited literature suggests that vandalism and the loss of AEDs are rare and occur in locked and unlocked cabinets. Research on this topic is needed that focuses on real-life retrieval and patient outcomes.
Keywords: Heart arrest, Out-of-hospital cardiac arrest, Defibrillation, Public access defibrillation, Automated external defibrillators, Security, Access
Introduction
Out-of-hospital cardiac arrest (OHCA) outcomes remain poor, with most reported survival rates in treated patients less than 10 %.1 Rapid defibrillation is critical to improving patient outcomes, as each minute of delay in attempting defibrillation reduces the chances of survival and good functional outcomes.2, 3 Automated external defibrillators (AEDs) are portable, easy-to-use devices intended for use by laypersons and first responders. Patients who receive defibrillation from bystanders have the greatest chance of survival,4 yet public rates of AED use are usually below 3 %.1 Ensuring AED accessibility to rescuers is essential for maximising their effectiveness, with a study in Denmark showing a tripling of bystander defibrillation and an almost doubling of survival when the nearest AED was accessible at the time of OHCA.5
Ensuring an AED’s accessibility and 24/7 availability during emergencies poses significant challenges.6, 7, 8, 9 Concerns about theft, vandalism, and misuse of AEDs have led to the implementation of security measures, including the use of locked cabinets to house these devices in public areas.10, 11, 12 Field visits to AED locations, as recorded in registries or apps, have shown high proportions of AEDs in key-locked cabinets in some regions.13 While locked cabinets aim to protect AEDs, they may also cause delays in AED access during emergencies. Given the lack of a comprehensive review on this approach, this topic was prioritised by the Basic Life Support (BLS) Task Force of the International Liaison Committee on Resuscitation (ILCOR) for investigation.
To address this gap, a scoping review was chosen to broadly explore the extent of the literature, identify the types of evidence available, and inform the development of more focused research questions that could later be addressed in a systematic review. By mapping the current state of evidence, this review seeks to identify both the challenges and potential benefits associated with locked AED cabinets and to highlight gaps in current knowledge. The primary research question of this scoping review is what is known in the literature about the impact of locked AED cabinets on the protection, accessibility and effectiveness of AEDs.
Methods
This scoping review followed the Joanna Briggs method14 and the ILCOR process for evidence review,15, 16 including a prespecified plan approved by the ILCOR BLS Task Force (Supplementary materials 1). The reporting followed the PRISMA scoping review guidelines (Checklist available in the Supplementary materials 2).17
Eligibility criteria
Studies of any type or design (e.g., experimental, observational, qualitative, conference abstracts, letters to the Editor) that were published with an English abstract and examined the impact of locked AED cabinets were included. Studies examining the accessibility of AEDs in locked buildings were not included. Any outcome, including AED outcomes (e.g. AED use, time to AED use, AED vandalism or theft) were accepted. Systematic reviews were initially included to review reference lists for missed studies. Authors of conference abstracts were contacted where possible to ascertain whether full results were published. We also contacted the authors of studies that reported rates of theft or vandalism without details of security measures, and these studies were included if any of the AEDs studied were contained in locked cabinets. Reports were excluded if they reported 1) on the general accessibility of AEDs without rates of theft or vandalism or 2) other outcomes (e.g. the results of surveys of what was considered in the placement of an AED).
Information sources
A search of Medline, Embase, Cochrane, CINAHL and Google Scholar (title search of first 200 articles for keywords) was performed from database inception to May 25th 2024. The search strategy was developed with the assistance of an information specialistand included a combination of keywords and phrases related to the topic, including: “Automated External Defibrillator”, “AED”, “Locked cabinet”, “Public access defibrillation”, “Emergency response”, “Sudden cardiac arrest”. The Medline search is provided supplementary materials and the full search is available from the authors. We also searched the reference lists of related reviews and included papers for missed studies. Finally, we searched the first 20 pages in Google Scholar (∼200 titles performed on July 17th 2024) and also examined the papers that cited the included studies (as per Google Scholar search on July 25th 2024) for inclusion.
Title and full-text rscreening and assessments were performed using COVIDENCE software. Two reviewers from the review team (GDP, CMS, CV, JEB) independently screened titles and abstracts for inclusion, and then assessed the full text of these studies against prespecified inclusion criteria. Where the authors of this review were also authors of primary papers, other review team members decided whether to include studies and extracted the data. Disagreements were resolved by discussion. No critical appraisal of individual sources was planned or performed.
Data charting process, items and synthesis
Data charting was iterative. After reading all of the included studies, the studies were grouped by the outcomes. We present a narrative synthesis to summarise the findings of the impact of locked AED cabinets with or without other security measures. One reviewer (JEB) extracted the data, which was then checked by two reviewers (LO and CMS). Due to the small number of studies, which were mostly conference abstracts, no piloting of data extraction was performed. Disagreements were resolved by discussion or further adjudication from a fourth reviewer (GDP). We extracted the following data from each included study: publication type, study design and methodology, population and setting, years of the study, and key findings related to AED security and accessibility.
Results
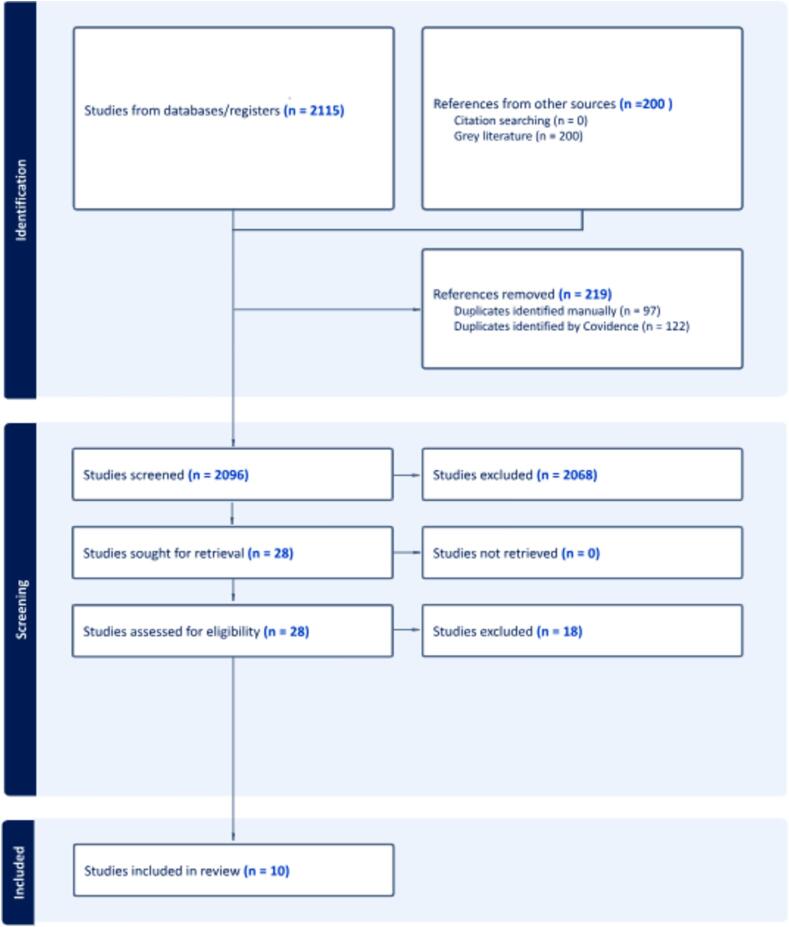
The literature search yielded a total of 2,096 titles, and 18 full-texts were deemed relevant and reviewed (Fig. 1). Subsequently, ten articles fulfilled our eligibility criteria and were included (nine found in the database search18, 19, 20, 21, 22, 23, 24, 25, 26 and one from Google Scholar27). A review of the systematic reviews, advisory statements,7 and the reference lists and citing studies (Google Scholar) of included studies found no additional study.
Fig. 1.
The PRISMA flowchart.
Characteristics of the included articles
A description of included studies is provided in Table 1. All included studies were published after the year 2000. Studies were conducted in the United States of America (USA),23 Canada,21, 23 Australia,22 United Kingdom (UK),25 Switzerland,24 Poland,19 South Korea,18 Singapore27 and Spain.26 Seven of the publications were retrospective observational studies reporting rates of theft and vandalism,18, 19, 20, 21, 22, 23, 24, 25, 26 one paper reported on harm to rescuers,27 and two papers were AED retrieval simulation studies.18, 19 Four papers were only published as conference abstracts,23, 24, 25, 26 two were letters to the Editor,20, 22 and four were peer-reviewed research articles.18, 19, 21, 27 No study reported on the impact of locked AED cabinets on patient outcomes.
Table 1.
Study Characteristics of included studies.
| Study |
Publication type Study design Study dates |
Country | Number of AEDs | Results |
|---|---|---|---|---|
| Theft, vandalism and harm to rescuers of AEDs in locked or unlocked cabinets | ||||
| Cheema 2022 | Conference abstract AED registry 2019–2022 |
United Kingdom | 31,938 AEDs | Vandalism/theft AEDs in locked cabinets vs unlocked AED cabinets (0.34% vs. 0.12%, P < 0.01). Vandalism/theft was lower in areas with restricted access AEDs compared to public accessible AEDs (0.07% vs 0.28%, P = 0.003) |
| Page 2024 | Letter to the Editor AED Registry 2022–2023 |
Australia | 279 AEDs in public locations and in unlocked cabinets | Theft AEDs in unlocked cabinets (1.8%) vandalism (n=2, <1%). Three stolen AEDs were recovered through the tracking device. |
| Yu 2022 | Online survey first responders | Singapore | 50 attempts to retrieve an AED | Injuries were sustained by 24 first responders while breaking glass to access AED. AEDs were successfully retrieved in 45 cases.Injury impacted on 1 responder’s willingness to retrieve an AED in the future. |
| Theft or vandalism of AEDs when locked or unlocked cabinets were not detailed | ||||
| Benvenuti 2013 | Conference abstract not described 2008–2012 |
Switzerland | 142 AEDs in public locations | No theft.One report of tampering with an AED battery (0.7%) and two reports of tampering with cabinets (1.4%). |
| Brugda 2014 | Conference abstract not described | Spain | 508 in public spaces with 24-hour access | No reports of theft. |
| Ludgate 2012 | Conference abstract not described 2012 |
USA | 36 AEDs | 1 (3%) reported stolen 1 (3%) reported as missing |
| Peberdy 2005 | Peer-reviewed paper AEDmonitoring as part of RCT 2000–2003 |
USA and Canada | 1,716 AEDs in public and multi-family residential facilities. | 20/1716 (1.3%) thefts (the “majority” of stolen devices were removed from locked locations as opposed to those kept unlocked and visible) |
| Salerno 2019 | Letter to the Editor Survey PAD program 2015–2018 |
32 cities in USA with an AED registry | Unknown | 9 cases of AED theft were reported in 7 different cities. No reports of AED vandalism |
| AED delivery time related to accessibility | ||||
| Uhm 2008 | Survey of AED sites | South Korea | 233 AEDs in 138 apartment complexes (included AEDs in locked and unlocked cabinets) | Estimate delivery time of an AED was significantly longer in AEDs that were in locked locations (times not provided, p < 0.001), 49 (35.5%) apartment complexes had their AEDs locked away for safe keeping with insufficient notice regarding the keys |
| Telec 2018 | Simulation at AED site | Poland | 78 AED sites (included AEDs in locked and unlocked cabinets) | Delivery time of AED was significantly longer in AEDs that were required assistance of a staff member for AED access compared to those with freely accessible: median 42 s (IQR 12–49) vs. 0 s (IQR 0–0) (p < 0.001) |
AED theft and vandalism
Seven studies reported rates of AED theft and vandalism,20, 21, 22, 23, 24, 25, 26 although only two reported this data by whether the AED cabinets were locked or unlocked.22, 25 The number of AEDs examined in these studies varied widely, ranging from 36 to 31,938 AEDs (Table 1). One study surveyed public access defibrillation (PAD) programs in 51 cities in the USA and reported AED theft and vandalism, but did not report the number of AEDs within these programs or security measures.23 The period studied was not reported in two studies, with the remainder conducted between two to six years.
Overall rates of theft and/or vandalism in studies in which AEDs were located in public spaces and accessible 24/7 ranged from 0% in Spain27 to 1.8 % in Australia.22 A government-run public access defibrillation program in Spain, which reported 129 uses and no vandalism to 508 AEDs located in public spaces, included a public AED awareness campaign.26 A conference abstract from the USA about 36 AEDs, with their access and security not described, reported one as stolen (3 %) and one as ‘missing’ (3%).23 A study from Switzerland, published as a conference abstract on 142 AEDs located in public spaces, reported no theft, one AED with its battery detached, one episode of vandalism relating to the earthing of the AED cabinet and one episode of graffiti.24 A four-year follow-up of 1,716 AEDs placed in public and residential communities as part of a trial in North America, reported 690 uses and 20 (1.3%) AED thefts, with the majority of stolen devices removed from locked locations (not described) as opposed to those kept unlocked and visible (exact number not reported).21 This trial also reported no harm to rescuers related to the AED.21 Another study surveying PAD programs in the USA, reported low rates of theft (n=7) with AEDs stolen from a bike trail, two police vehicles, and various publicly accessible buildings.20
Only one study, published as a conference abstract, compared locked and unlocked AED cabinets across the UK.25 This study of 31,938 AEDs over a four-year period reported very low rates of theft and vandalism, which were slightly higher when AEDs were in unlocked cabinets (0.3% vs. 0.1%, p < 0.01) and in public locations compared to restricted access locations (0.3% vs 0.1%, p = 0.003). Australian data reported in a letter to the Editor examined 279 AEDs in unlocked cabinets in public locations (e.g. outside supermarkets, on main roads) and reported five (2%) were stolen and two (<1%) were vandalised over a two-year period.22 Three stolen AEDs in this study were recovered through a tracking device.
Accessibility
Two OHCA studies examined the delivery time of AEDs in locked (including locked cabinets19) and unlocked sites.18, 19 The South Korean study conducted in-person surveys of 138 apartment complexes with 500 households or more where AED placement is mandatory.18 In these complexes, 35.5% of AEDs were described as ‘locked’ and this was associated with a longer estimated AED delivery time (times not provided, p < 0.001). While the delivery time calculation is poorly described (e.g. no starting point is provided), it appears they added six minutes to an estimated walking distance to the AED for locked cabinets. The Polish study conducted a simulation at 78 buildings known to have AEDs inside.19 Participants, who were blinded to the exact location of the AED in the building, were asked to retrieve the AED from and back to the main entrance of the building. The AED was located in open-access cabinets for unrestricted use in 36 sites, the remainder required staff assistance to retrieve either from locked or unlocked cabinets (detail provided by authors). The median retrieval time was 96s (IQR 52–144), with very wide ranges seen when staff assistance was required (estimated IQR: freely accessible 20 to 250s; staff assistance 30–580s); however, data comparing locked and unlocked AED cabinets were not provided.
Harm associated with locked AED cabinets
An online survey of 88 first responders reported injuries sustained during AED retrieval from locked cabinets in Singapore.27 There were 45 attempts to access an AED (40 were successfully retrieved and brought to the cardiac arrest scene), with the majority (n=38) requiring breaking glass to obtain a key to unlock the AED cabinet. Over half (n=24, 53%) of the first responders surveyed reported sustaining injuries, with most injured (62.5%) using body parts to break the glass. One injured responder reported they would not be willing to access an AED in the future as a result of the sustained injuries.
Discussion
AEDs are critical to improving OHCA survival rates, but their availability and accessibility is likely to significantly impact their effectiveness. We conducted a scoping review to identify literature concerning the impact of additional security, specifically locked cabinets, on AED accessibility and effectiveness. We identified a paucity of research examining this issue, with most studies published as conference abstracts or letters to the Editor, and thus were not peer-reviewed and provided limited information on methods. The ten included studies examined a broad range of outcomes, including rates of theft and vandalism, harm to rescuers and accessibility. No study compared the impact of locked versus unlocked cabinets on patient outcomes, and none of the included studies mentioned that some AEDs may have been taken for use in emergencies and not returned.
Overall, the reported rates of theft or vandalism were very low (<2%), even when examined in highly accessible public locations, and were reported in both locked and unlocked cabinets. In one study, most of the stolen AEDs were recovered through the use of tracking devices.22 The evidence from two simulation studies conducted in Poland19 and South Korea18 suggests that the location and security of AED cabinets impacts the time to access them, although the presentation of these data was very difficult to understand and interpret. Open access AEDs located in public spaces had significantly shorter times to access than those that needed keys or personnel to access them. This finding is important to guide the location and ease of access of AEDs if they are to be easily accessed for use in OHCA situations.
An ILCOR Scientific Statement published in 2022, which focuses on optimising public access defibrillation, advises against using locked cabinets.7 If locked cabinets are used, it recommends that instructions for unlocking them be clear and ensure no delays in access. Although further research is needed to understand the impact of locked AEDs on patient outcomes, data from this scoping review supports these recommendations.
Research gaps
Peer-reviewed research and human studies are needed on this topic, particularly studies focusing on real-life retrieval and the impact of security strategies on delivery times, injuries to rescuers and patient outcomes.
Limitations
Our scoping review has some limitations. We only included literature from studies published in English, and our grey literature search was limited to Google Scholar. We did not feel any additional benefit would be gained in examining further grey literature (e.g., news, case or police reports), as the underlying denominator of AEDs is not likely to be reported.
Conclusion
Overall, the existing evidence suggests that theft and vandalism of AEDs are rare occurrences and that they occur in both locked and unlocked cabinets. Research is needed to explore the impact of locked cabinets on delays in AED access, injuries to rescuers, and patient outcomes.
Non-author Task Force member Collaborators
The authors acknowledge the contributions of the non-author members of the ILCOR BLS Task Force: Michael Smyth, Rebecca Cash, Julie Considine, Sung Phil Chung, Vihara Dassanayake, Katie Dainty, Guillaume Debaty, Maya Dewan, Bridget Dicker, Fredrik Folke, Anthony Lagina, George Lucas, Carolina Malta Hansen, Takanari Ikeyama, Nicholas J. Johnson, Siobhán Masterson, Laurie Morrison, Chika Nishiyama, Ziad Nehme, Tatsuya Norii, Violetta Raffary, Giuseppe Ristagno, Tetsuya Sakamoto, Aloka Samantaray, Baljit Singh, Peter Morley.
Funding
This scoping review was funded by the American Heart Association, on behalf of The International Liaison Committee on Resuscitation (ILCOR). JEB received a fellowship from the Heart Foundation of Australia (#104751).
CRediT authorship contribution statement
Lawrence Oonyu: Writing – original draft, Visualization, Resources, Investigation, Data curation. Gavin D. Perkins: Writing – review & editing, Methodology, Investigation, Funding acquisition, Data curation, Conceptualization. Christopher M. Smith: Writing – original draft, Visualization, Methodology, Data curation. Christian Vaillancourt: Writing – review & editing, Methodology, Data curation. Theresa M. Olasveengen: Writing – review & editing, Supervision, Methodology. Janet E. Bray: Writing – original draft, Visualization, Supervision, Project administration, Methodology, Investigation, Data curation, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. GDP is Editor-in-Chief and JEB is an Associate Editor of Resusciation Plus.
Acknowledgement
We thank Natasha Dodge and Lorena Romero for their assistance with the search strategy.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resplu.2024.100791.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Nishiyama C., Kiguchi T., Okubo M., et al. Three-year trends in out-of-hospital cardiac arrest across the world: Second report from the International Liaison Committee on Resuscitation (ILCOR) Resuscitation. 2023;186 doi: 10.1016/j.resuscitation.2023.109757. [DOI] [PubMed] [Google Scholar]
- 2.Drennan I.R., Lin S., Thorpe K.E., Morrison L.J. The effect of time to defibrillation and targeted temperature management on functional survival after out-of-hospital cardiac arrest. Resuscitation. 2014;85:1623–1628. doi: 10.1016/j.resuscitation.2014.07.010. [DOI] [PubMed] [Google Scholar]
- 3.De Maio V.J., Stiell I.G., Wells G.A., Spaite D.W. Optimal defibrillation response intervals for maximum out-of-hospital cardiac arrest survival rates. Ann Emerg Med. 2003;42:242–250. doi: 10.1067/mem.2003.266. [DOI] [PubMed] [Google Scholar]
- 4.Nehme Z., Andrew E., Bernard S., Haskins B., Smith K. Trends in survival from out-of-hospital cardiac arrests defibrillated by paramedics, first responders and bystanders. Resuscitation. 2019;143:85–91. doi: 10.1016/j.resuscitation.2019.08.018. [DOI] [PubMed] [Google Scholar]
- 5.Karlsson L., Malta Hansen C., Wissenberg M., et al. Automated external defibrillator accessibility is crucial for bystander defibrillation and survival: A registry-based study. Resuscitation. 2019;136:30–37. doi: 10.1016/j.resuscitation.2019.01.014. [DOI] [PubMed] [Google Scholar]
- 6.Smith C.M., Griffiths F., Fothergill R.T., Vlaev I., Perkins G.D. Identifying and overcoming barriers to automated external defibrillator use by GoodSAM volunteer first responders in out-of-hospital cardiac arrest using the Theoretical Domains Framework and Behaviour Change Wheel: a qualitative study. BMJ Open. 2020;10:e034908. doi: 10.1136/bmjopen-2019-034908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brooks S.C., Clegg G.R., Bray J., et al. Optimizing outcomes after out-of-hospital cardiac arrest with innovative approaches to public-access defibrillation: A scientific statement from the International Liaison Committee on Resuscitation. Resuscitation. 2022;172:204–228. doi: 10.1016/j.resuscitation.2021.11.032. [DOI] [PubMed] [Google Scholar]
- 8.Smith C.M., Lim Choi Keung S.N., Khan M.O., et al. Barriers and facilitators to public access defibrillation in out-of-hospital cardiac arrest: a systematic review. Eur Heart J Qual Care Clin Outcomes. 2017;3:264–273. doi: 10.1093/ehjqcco/qcx023. [DOI] [PubMed] [Google Scholar]
- 9.Dainty K.N., Yng Ng Y., Pin Pek P., Koster R.W., Ong E.H.M. Wolf creek XVII part 4: Amplifying lay-rescuer response. Resusc Plus. 2024;17 doi: 10.1016/j.resplu.2023.100547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O’Callaghan P.A., Swampillai J., Stiles M.K. Availability of automated external defibrillators in Hamilton, New Zealand. N Z Med J. 2019;132:75–82. [PubMed] [Google Scholar]
- 11.Lac D., Wolters M.K., Leung K.H.B., MacInnes L., Clegg G.R. Factors affecting public access defibrillator placement decisions in the United Kingdom: A survey study. Resusc Plus. 2023;13 doi: 10.1016/j.resplu.2022.100348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fortington L.V., Bekker S., Finch C.F. Integrating and maintaining automated external defibrillators and emergency planning in community sport settings: a qualitative case study. Emerg Med J. 2020;37:617–622. doi: 10.1136/emermed-2019-208781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang L., Li B., Zhao X., et al. Public access of automated external defibrillators in a metropolitan city of China. Resuscitation. 2019;140:120–126. doi: 10.1016/j.resuscitation.2019.05.015. [DOI] [PubMed] [Google Scholar]
- 14.Khalil H., Peters M., Godfrey C.M., McInerney P., Soares C.B., Parker D. An Evidence-Based Approach to Scoping Reviews. Worldviews Evid Based Nurs. 2016;13:118–123. doi: 10.1111/wvn.12144. [DOI] [PubMed] [Google Scholar]
- 15.Berg K.M., Bray J.E., Ng K.C., et al. 2023 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations: Summary From the Basic Life Support; Advanced Life Support; Pediatric Life Support; Neonatal Life Support; Education, Implementation, and Teams; and First Aid Task Forces. Circulation. 2023;148:e187–e280. doi: 10.1161/CIR.0000000000001179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berg K.M., Bray J.E., Ng K.C., et al. International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations: Summary From the Basic Life Support; Advanced Life Support; Pediatric Life Support; Neonatal Life Support; Education, Implementation, and Teams; and First Aid Task Forces. Resuscitation. 2023;2023 [Google Scholar]
- 17.Tricco A.C., Lillie E., Zarin W., et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 18.Uhm T.H., Kim J.H. Factors affecting delivery time of public access defibrillator in apartment houses. Indian Journal of Public Health Research and Development. 2018;9(9):534–540. [Google Scholar]
- 19.Telec W., Baszko A., Dabrowski M., et al. Automated external defibrillator use in public places: a study of acquisition time. Kardiol Pol. 2018;76:181–185. doi: 10.5603/KP.a2017.0199. [DOI] [PubMed] [Google Scholar]
- 20.Salerno J., Willson C., Weiss L., Salcido D. Myth of the stolen AED. Resuscitation. 2019;140:1. doi: 10.1016/j.resuscitation.2019.04.036. [DOI] [PubMed] [Google Scholar]
- 21.Peberdy M.A., Ottingham L.V., Groh W.J., et al. Adverse events associated with lay emergency response programs: the public access defibrillation trial experience. Resuscitation. 2006;70:59–65. doi: 10.1016/j.resuscitation.2005.10.030. [DOI] [PubMed] [Google Scholar]
- 22.Page G., Bray J. Unlocking the key to increasing survival from out-of-hospital cardiac arrest - 24/7 accessible AEDs. Resuscitation. 2024;110227 doi: 10.1016/j.resuscitation.2024.110227. [DOI] [PubMed] [Google Scholar]
- 23.Ludgate M.B., Kern K.B., Bobrow B.J., Ewy G.A. Donating automated external defibrillators may not be enough. Circulation. 2012;126 [Google Scholar]
- 24.Benvenuti C., Burkart R., Mauri R. Public defibrillators and vandalism: Myth or reality? Resuscitation. 2013;1:S69. [Google Scholar]
- 25.Cheema K., O'Connell D., Herz N., et al. The influence of locked automated external defibrillators (AEDs) cabinets on the rates of vandalism and theft. Resuscitation. 2022;175(Supplement 1):S80. [Google Scholar]
- 26.Brugada R., Morales A., Ramos R., Heredia J., De Morales E.R., Girona B.P. cardio-protected territory. Resuscitation. 2014;1:S57. [Google Scholar]
- 27.Ng J.S.Y., Ho R.J.S., Yu J., Ng Y.Y. Factors influencing success and safety of AED Retrieval in out of Hospital Cardiac Arrests in Singapore. Korean J Emerg Med Serv. 2022;26:97–111. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.