Abstract
Background
Various surgical techniques have been devised for the surgical cosmetic enhancement of female outer genitalia. The selection of an optimal method should be based on satisfaction rates and safety; however, comprehensive, contemporary systematic assessment of these factors has been limited in the literature.
Objectives
Our aim was to conduct a comprehensive systematic review and meta-analysis to evaluate the overall satisfaction rates and risk factors associated with various labiaplasty techniques and tools.
Methods
The authors performed a systematic literature search in 3 medical databases: PubMed, Elsevier, and Cochrane (Central) with the closing date of October 2023. Original articles with quantitative satisfaction rates and frequencies of the most common complications (hematoma, dehiscence, swelling, bleeding, and infection) were included.
Results
Systematic search provided a total of 3954 records. After selection and review of the articles, 86 eligible, peer-reviewed studies were identified, of which 53 provided quantitative data. High overall satisfaction rate was found for all methods (proportion [prop] 94%; confidence interval [CI] 93%-95%), with highest satisfaction for deepithelialization (prop 97%; CI, 85%-99%). Complications were generally rare, with elevated incidences for some techniques (wedge resection: dehiscence, prop, 8%, CI 5%-13%; and composite reduction: swelling, prop 13%, CI 2%-54%). Scalpel technique had significantly higher incidence of complications than laser, namely for bleeding, swelling, and hematoma.
Conclusions
Labiaplasty can be considered a generally effective approach to outer female genitalia beautification, with low associated risks. Surgeons must tailor their approach to the patients’ needs and anatomy to achieve maximal satisfaction, given the differences in the frequency of complications for each method.
Level of Evidence: 3

In contemporary society, the self-image of females is increasingly tied to perceptions of their genitalia, a trend that significantly influences relationship dynamics and psychological health. The media's ubiquitous presence and influence serve to amplify the perceived importance of genitalia appearance, often showing a biased portrayal.1,2 Contemporary trends, such as the decrease in pubic hair, further emphasize the expectation of symmetrical, normometric labia, thereby influencing females’ perceptions of their bodies.3,4 Beyond the realm of aesthetics, variations in the female genitalia, such as labia minora hypertrophy, can carry functional implications.5,6 This can manifest as discomfort when wearing tight-fitting clothes, exercising, or during sexual intercourse.7 Consequently, an increasing number of females are turning to labiaplasty as a solution to these physical and psychological challenges.8 The indications for these procedures have also expanded, now addressing not only hypertrophic labia minora but also labia majora volume loss, typically associated with aging and in some cases as a result of other medical interventions.9,10
According to statistical data released by the American Society for Aesthetic Plastic Surgery, there has been a significant rise in the demand for labiaplasty, marked by an upswing of 217.2% from 2012 to 2017.11 This upward trend continued into the subsequent period, with a further increase of 20% observed between 2017 and 2021 and a minor downward turn of 26% in 2022.12,13 Concurrently, vaginal rejuvenation surgery emerged as a new category in the field, with over 71,000 procedures recorded within this time frame. In response to this demand, a burgeoning array of techniques have been developed, expanding the options available to both patients and surgeons. Emerging techniques, such as allogeneic and autologous fillers, hyaluronic acid, and fat grafting, offer opportunities to treat both labia minora and majora.14 Overall, these procedures boast high satisfaction rates (90%) and low complication rates.15,16 The objective of this study was to systematically review the literature on surgical techniques and tools (scalpel vs laser) for female genital beautification and perform a meta-analysis to assess satisfaction rates and common complications, such as swelling, bleeding, hematoma, dehiscence, and infection.
METHODS
The study was performed according to the Cochrane Handbook for Systematic Reviews of Interventions, version 6.3.17 The study was registered with PROSPERO (registration no. CRD42022380481) and adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA-P) guidelines.18
Literature Search, Inclusion, and Exclusion Criteria
A comprehensive search across 3 databases—MEDLINE (PubMed; National Institutes of Health, Bethesda, MD), Embase (Elsevier, Amsterdam, the Netherlands), and Cochrane (Central Register of Trials; Wiley, Hoboken, NJ)—was conducted up to and including October 2023. The following search key was applied: “(labiaplasty OR labia minora reduction OR labia majora augmentation OR female genital plastic surgery OR female genital beauty OR female genital beautification) AND (outcome OR complication OR satisfaction OR psychological).” Case reports, commentaries, and conference letters were excluded from the analysis due to their low patient numbers, limited data, and subjective quality. Additionally, prospective or retrospective studies providing data on aesthetic surgeries of the labia minora and labia majora were included. The primary outcome was patient-reported satisfaction rates for all known genital beautification techniques, including labiaplasty and complex surgical approaches, which occasionally involved surgical alteration of the labia majora as well as the surgical tool, namely scalpel or laser (when applicable). Literature published in English, Spanish, or French was included. The secondary outcomes included complication rates (bleeding, hematoma, dehiscence, swelling, infection).
Selection and Data Extraction
Duplicates were removed with EndNote version 20 (Clarivate, Philadelphia, PA). The research team conducted a title-abstract assessment with Rayyan, with 2 independent reviewers (A.M.G. and R.V.) overseeing the screening process for eligible studies. In the case of the disagreement, a third independent party (T.V.) resolved it. The following data were extracted from studies that met the inclusion criteria: author, number of patients, indication for labia minora plasty, surgical techniques, supplementary procedures, satisfaction rate, and follow-up, as well as specified complications. The data we reviewed and extracted encompassed patient numbers, indications, techniques or combination of techniques, complications, and patient satisfaction. Classification of interventions was based on the recommendations of Motakef et al, however, because numerous subtypes of techniques emerged, we established 10 major categories based on the original method: deepithelialization, direct excision/edge resection, W-plasty, Z-plasty, butterfly technique, wedge resection, wedge resection with preserved blood vessels and neural supply, composite reduction, combined techniques with labia majora alteration, and radiofrequency.19
Risk of Bias Assessment
The evaluation of outcome quality was independently conducted by 2 independent reviewers (A.M.G., R.V.). Disagreements were resolved by a third reviewer (T.V.). Quality was assessed based on the Methodological Index For Non-Randomized Studies (MINORS) system.20 Studies were included if they reached a score of 9 for noncomparative studies and 18 for comparative studies. Evaluation results of included studies are presented in Supplemental Table 1, available online at www.aestheticsurgeryjournal.com.
Statistical Analysis
The statistical analyses were performed with the software R (R Core Team 2020, version 4.0.3); calculations and plots were performed with the meta (version 6.1-0) package.21 Proportion with 95% confidence interval (CI) was employed for the effect size measure. To calculate the study proportions and pooled proportion, the total number of patients and those with the event of interest were extracted from each study. To pool the effect size the random effect model was applied; the logit transformation of proportions was implemented to calculate an overall proportion.22
To estimate the heterogeneity variance measure (τ2), the Paule-Mandel method was utilized.23 The confidence interval for τ2 and τ were calculated with the Q-Profile method.24 A Hartung-Knapp adjustment was performed for CIs to avoid false positive conclusions.25,26 To quantify the degree of heterogeneity I2 statistics by Higgins and Thompson were applied.27 An I2 above 75% represented considerable heterogeneity based on Cohrane's recommendations. Prediction interval calculations were based on t distribution. For all studies, irrespective of 0 cell counts, the individual study proportion with 95% CI was calculated by adding 0.5 as a continuity correction (only for visualization on the forest plot). In the case of subgroup analysis, we assumed different τ2 values in the subgroups. Forest plots graphically summarized the results. For all outcomes, statistical significance was defined as P<.05.
RESULTS
Literature Search
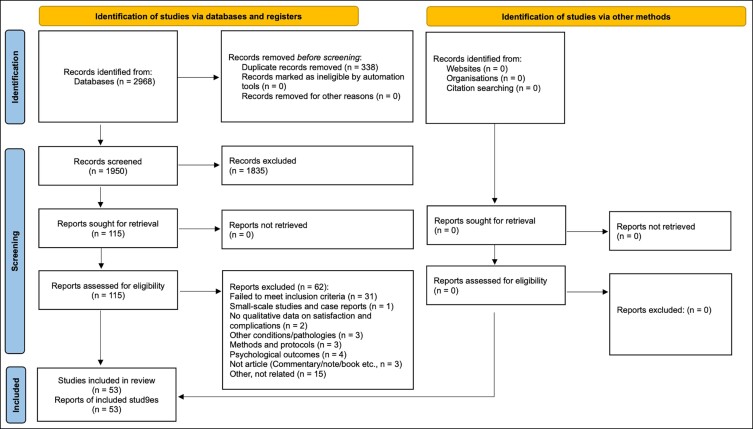
Primary literature search provided 2968 results. After duplicate removal there remained 1950 articles; 1835 were excluded based on title and abstract. From the remaining 115 articles 87 studies fulfilled the inclusion criteria based on full-text review, with 53 studies finally that provided adequate quality data.3,15,19,28-76 The details of the selection process are summarized in Figure 1. The reason for further exclusion was the imprecise or incompletely executed sequestration of techniques, which made it impossible to make statistical comparisons. The characteristics of the included studies can be found in Supplemental Table 1.
Figure 1.
PRISMA flow diagram of the study selection process.
This meta-analysis included 3954 patients, all females between the age of 10 and 72, with an average age of 29.44. The most common indications for labia minora plasty were aesthetic dissatisfaction; discomfort in clothing, while practicing sports, or during sexual activity; hygiene problems; recurrent infections; and sexual dysfunction.
Risk of Bias Assessment
Our meta-analysis incorporated numerous studies, each meticulously evaluated for risk of bias with the Methodological Index for Non-Randomized Studies (MINORS) criteria.20 From the analysis, it was evident that most studies were comprehensive in reporting of the study aims, patient inclusion, data collection methods, and appropriateness of their endpoints. However, variability in the scores was observed in the areas of unbiased assessment of study endpoints and prospective calculation of the study size. A majority of the studies had an appropriate follow-up period relevant to the aim of the study. Comparative studies overwhelmingly had adequate control groups, contemporary groups, and statistical analyses, however, scores varied in the baseline equivalence of groups.
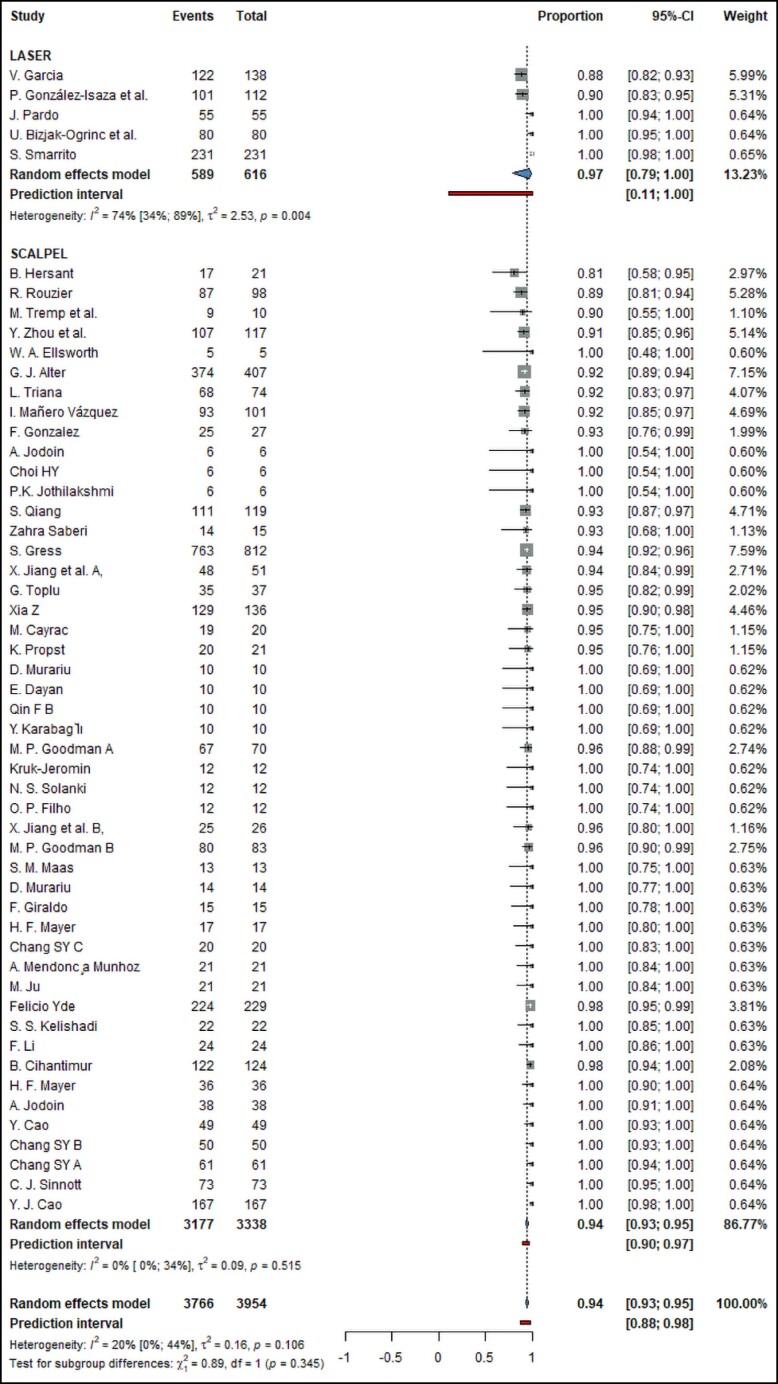
Satisfaction
The analysis involved the synthesis of 53 studies with a total of 3766 observations, accounting for 3954 events. The pooled satisfaction proportion calculated with a random effects model was 0.9443 (CI: 0.9316-0.9548, I2 = 20%). The results regarding satisfaction are summarized in Figure 2.
Figure 2.
Forest plot showing a summary of the overall satisfaction rates of different labiaplasty methods.
Subgroup analyses were conducted based on the technique applied in the individual studies. For studies that utilized a combination of techniques (n = 2), the pooled satisfaction proportion was 0.9394 (CI: 0-1, I2 = 88.5%). For studies utilizing wedge resection (n = 15), the pooled satisfaction proportion was 0.9573 (CI: 0.9286-0.9748, I2 = 23%). Furthermore, in studies in which wedge resection was performed with preserved blood vessels and neural supply (n = 2) satisfaction proportion was 0.9414 (CI: 0.0267-0.9999, I2 = 0%). In studies that included the butterfly technique (n = 6), the pooled satisfaction proportion was 0.9441 (CI: 0.7428-0.99, I2 = 0%). For studies involving deepithelialization (n = 5), the pooled satisfaction proportion was 0.971 (CI: 0.8549-0.9948, I2 = 0%). Edge resection yielded a combined satisfaction proportion of 0.9589 (n = 13, CI: 0.9301-0.9761, I2 = 46.6%), composite reduction a pooled proportion of 0.9293 (n = 10, CI 0.9163-0.9403, I2 = 0%). Last, for the single studies implementing radiofrequency (n = 1), the satisfaction proportion was 0.9545 (CI: 0.5517-0.9972, I2 not applicable due to only 1 study); for W-shape resection (n = 1) it was 0.9643 (CI: 0.6161-0.9978, I2 not applicable); and for Z-plasty (n = 1) it was 0.9688 (CI: 0.6497-0.9981, I2 not applicable). The differences between subgroups were not statistically significant (χ2 = 10.33, degrees of freedom [df] = 9, P < .325). In addition to the surgical technique, we compared satisfaction with laser and satisfaction with the scalpel as surgical tools. Of the 53 studies, the scalpel was employed in 48 and laser in 5, with a pooled satisfaction proportion of 0.9437 (CI: 0.7893-0.9972, I2 = 73.6%) and 0.9734 (CI: 0.9323-0.9534, I2 = 0%) respectively, with no significant difference between the 2 groups (P = .3448). Results regarding the surgical tool are presented in Supplemental Figure 1, available online at www.aestheticsurgeryjournal.com.
Complications
For hematoma incidence, 44 studies with 2090 observations and 38 events were combined, yielding a proportion of 0.0331 (CI: 0.0234-0.0465, I2 = 33.1%). Subgroup analysis demonstrated no significant difference in hematoma incidence across the surgical techniques, such as combination of techniques, laser-assisted labiaplasty, and wedge resection (χ2 = 10.5, df = 9, P = .312). However, when comparing surgical tools, laser showed a significantly lower overall proportion of hematoma (χ2 = 17.7, df = 1, P < .0001) of 0.0135 (CI: 0.006-0.03, I2 = 32.9%) compared to the scalpel, with a proportion of 0.0494 (CI: 0.006-0.03, I2 = 0%). Incidence of hematoma is summarized in Supplemental Figure 2 for surgical techniques and Supplemental Figure 3 for surgical tools, available online at www.aestheticsurgeryjournal.com.
Upon examining the incidence of dehiscence across 41 studies, significant variation was observed based on the different surgical techniques utilized (χ2 = 32.9, df = 9, P = .0001) (Supplemental Figure 4 for surgical techniques and Supplemental Figure 5 for surgical tools, available online at www.aestheticsurgeryjournal.com). The approach involving Z-plasty had the highest incidence, with a proportion of 0.1333 (CI: 0.0336-0.4054, I2 = nonapplicable), and wedge resection had the second highest incidence at 0.084 (CI: 0.0542-0.128, I2 = 27.8%). Notably, when wedge resection was performed preserving blood vessels and neural supply, the incidence of dehiscence became 0.042 (CI: 0.0082-0.1883, I2 = 0%), a 50% drop compared to the original method. In stark contrast, the technique involving composite reduction displayed the lowest incidence, with a proportion of 0.0271 (CI: 0.0171-0.0429, I2 = 0%). In the aggregate, dehiscence incidence was 0.0591 (CI: 0.0424-0.0817, I2 = 48.5%), with substantial variability across studies. The quantification of heterogeneity revealed a high level of inconsistency among the studies, suggesting a greater variability in study outcomes than would be anticipated by chance, potentially owing to divergences in surgical techniques or other study-specific factors. When comparing the laser and scalpel, there was no significant difference for the incidence of dehiscence (χ2 = 1.53, df = 1, P = .216).
Analysis of the incidence of swelling based on 30 studies with a total of 1476 observations and 44 events showed considerable variation among different techniques. Overall incidence was 0.0395 (CI: 0.0244-0.0633, I2 = 56%) with high heterogeneity. Among the techniques evaluated, composite reduction had a higher reported proportion of swelling at 0.131 (CI: 0.019-0.5405, I2 = 23.3%). This was followed by the butterfly technique at 0.0567 (CI: 0.0-1, I2 = 53.2%); radiofrequency at 0.0455 (CI: 0.0028-0.4483, I2 = nonapplicable); W-shape resection at 0.0357 (CI: 0.0022-0.3839, I2 = nonapplicable); Z-plasty at 0.0312 (CI: 0.0019-0.3503, I2 = nonapplicable); wedge resection at 0.0302 (CI: 0.0071-0.1188, I2 = 65.3%); and edge resection labiaplasty at 0.0292 (CI: 0.0097-0.0844, I2 = 62.2%) Again, wedge resection with preserved vessels and neural supply showed lower overall proportion of only 0.021 for swelling (CI: 0.0043-0.0894, I2 = 0%). A test for subgroup differences was significant (χ2 = 17.82, df = 9, P = .0373), indicating that the technique had a significant effect on the incidence of swelling. Regarding surgical tools, laser showed a significantly lower incidence of swelling (χ2 = 35.63, df = 1, P < .0001). Summary of the incidence of swelling is shown in Supplemental Figure 6 for techniques and in Supplemental Figure 7 for tools, available online at www.aestheticsurgeryjournal.com.
In the evaluation of bleeding proportions, 31 studies with 2323 observations and 18 events were combined, resulting in a pooled proportion of 0.0215 (CI: 0.0141-0.0325, I2 = 18.4%) and moderate heterogeneity between studies. Subgroup analysis showed no significant differences in bleeding proportions between the subgroups (χ2 = 5.92, df = 9, P = .748). However, the choice of surgical tool again had a significant impact on the incidence of bleeding (χ2 = 8.3, df = 1, P = .004). Whereas for laser the overall proportion was 0.0093 (CI: 0.0032-0.0269, I2 = 0%), for the scalpel it was 0.0297 (CI: 0.0187-0.0469, I2 = 35%). Incidence of bleeding is shown in Supplemental Figure 8 for techniques and in Supplemental Figure 9 for surgical tools, available online at www.aestheticsurgeryjournal.com.
The analysis of infection incidence incorporated 35 studies with 2122 observations and 20 events, revealing an overall pooled proportion of 0.0301 (CI: 0.019-0.0474, I2 = 42.2%). Subgroup analyses based on surgical techniques demonstrated no significant difference in infection proportions between the subgroups (χ2 = 7, df = 9, P = .6369). Similarly, the choice of surgical tool had no effect on the incidence of infections (χ2 = 0.25, df = 1, P = .6155). The results showing incidence of infection are summarized in Supplemental Figure 10 for surgical techniques and Supplemental Figure 11 for surgical tools, available online at www.aestheticsurgeryjournal.com.
Last, the total number of complications were compared between surgical techniques and the scalpel vs laser. Thirty-six studies were included in both comparisons. The overall pooled proportion for complications was 0.0888 for all methods, with 170 events out of 1914 observations (CI 0.0586-0.1326, I2 = 73.9). However, no significant difference was observed between subgroups (χ2 = 5.91, df = 9, P = .7489), with overall high levels of heterogeneity between studies. When comparing scalpel against laser, we also saw that although laser had a lower proportion of complications (0.0727 to 0.0894), this difference was not significant (P = .6931), most likely due to the low number of observations in the laser group to date. Supplemental Figure 12, available online at www.aestheticsurgeryjournal.com, details the total number of complications.
DISCUSSION
Given the cautious approach of the American College of Obstetricians and Gynecologists (ACOG) to labiaplasty, primarily due to a perceived lack of medical indication and the substantial risks it may entail, many clinicians share the belief that labia minora hypertrophy does not necessitate medical intervention, but rather should be considered a matter of educating females about anatomical variation.77,78 This sentiment is perhaps reinforced by the fact that gynecologists generally lack the specialized training for this procedure, which can often lead to suboptimal outcomes. Yet, this perspective may not be entirely comprehensive, because there is still a lack of consensus on what precisely constitutes labial hypertrophy, and strict thresholds for defining normal labia size might not always be clinically helpful.79 Indeed, the motives behind requests for labiaplasty are not solely aesthetic, but often include functional and psychological considerations as well.8
Over recent years, with the rise in societal awareness and changing trends, the demand for labiaplasty has seen a substantial increase.11-13 In response to this, a variety of techniques have emerged, each aiming to best cater to the individual needs of patients. The decision to adopt a particular surgical approach is a critical one, ideally informed by the patient's unique anatomy, their functional and aesthetic aspirations, and of course, a thorough appraisal of safety concerns and potential complications.80 Currently, we do not have a universally ideal surgical method that balances all these factors perfectly for every patient.28,81 However, it is encouraging to note that the range of techniques in use today have generally exhibited relatively high patient satisfaction rates and safety profiles, suggesting their potential effectiveness across a broad range of scenarios, and this continues based on this latest meta-analysis.16
The wedge resection technique represents a prominent choice within the array of available approaches for labiaplasty, gaining considerable utilization within the field. The distinguishing facet of this method is its inherent allowance for precise determination of the excision line's size and boundaries. Forming a triangular configuration, this provision facilitates fine-tuned adjustments to the tissue volume intended for removal, all while ensuring preservation of the original labial contour.3,29,54,56,82,83 Nevertheless, noteworthy considerations accompany this technique, including a statistically significant risk of dehiscence (0.08, CI: 0.05-0.13). This potential complication can be ascribed to the inherent characteristics of this approach, particularly the extensive excision area, which surpasses that in alternative methods, leading to heightened tension along the newly created suture lines.28,56,83 Furthermore, it is important to mention that despite its relatively low incidence flap necrosis constitutes a possible adverse event following application of this technique.40,56,83 In efforts to augment the outcome, a fusion of fundamental techniques may be employed, yielding enhanced results. Owing to the composite nature of these methods, we have elected to classify them within the composite reduction surgical approach category.43,46 An improved wedge-resection technique was also developed, with the aim of preserving blood vessels and neural supply to mitigate potential adverse effects.32,40 This method has comparable satisfaction, with a notable 50% decrease in the occurrence of dehiscence (0.04, CI: 0.01-0.19) and similarly low levels of other complications. Given the novelty of this approach, a wider application will show the reproducibility of these favorable results from other specialists.
The deepithelialization technique represents a minimally invasive approach within the realm of labiaplasty, featuring preservation of the original labial edge and minimal tissue, nerve, and vascular damage, facilitating a more natural postoperative appearance.28,41,70 However, this method may impose limitations on the volume of tissue that can be safely excised, thereby potentially constraining its applicability in instances of more pronounced hypertrophy.28 Notwithstanding this, these techniques have been linked with remarkably high patient satisfaction rates (0.96, CI: 0.93-0.97) and a notably low incidence of complications.19,28,41,70 Under optimally suitable circumstances, namely in the absence of severe hypertrophy, the application of this technique can be confidently endorsed as a sound clinical decision. The butterfly technique, a combination of wedge resection and deepithelialization, was created to mitigate potential drawbacks of both methods, namely distal flap necrosis and the limited associated volume decrease, respectively, and to produce a more aesthetic outcome.58 However, it still shows a moderately higher probability of dehiscence (0.06, CI: 0-0.88), albeit to a lower extent than wedge resection. The occurrence of bleeding and infection is also among the highest of the different methods, but not to a statistically significant level (0.06, CI: 0.01-0.19 and 0.05, CI: 0-1 respectively).
The simplicity and expediency of the edge resection approach maintains its status as a popular choice among surgeons performing labiaplasty procedures. With a direct linear incision, it offers an efficient method for labial protrusion reduction.44,52,74,84 However, it is crucial to note that this approach entails a direct and longitudinal incision line, often encompassing the entirety of the excess tissue. Consequently, this may result in the loss of the labia minora's original edge, which can exhibit variations in pigmentation and morphology. This method shows only moderate risk of complications, making it a well-rounded choice, especially given its simplicity, with the only recurring complication being potential rise to scar contracture at the site of the wound.74
The recent trend in labiaplasty procedures is a bespoke combination of techniques and approaches, tailored to address the unique requirements of each patient. Over the years, the popularity of this approach has grown significantly, contributing to a wealth of data for this group. Such procedures are designed to augment the patient's aesthetic self-perception, treating the outer genitalia as an integrated aesthetic unit. A gamut of techniques can be employed, including labia minora reduction, labia majora augmentation or reduction, clitoral hood reduction, clitoropexy, mons pubis liposuction, vaginoplasty, and perineoplasty.15,36,46,75 These approaches can be classified in 2 major groups based on the surgical targets beyond the labia minora (labia majora and clitoral hood respectively), combined techniques with labia majora alteration and composite reduction. Both show comparably high satisfaction, with composite reduction having a slightly higher occurrence of hematoma (0.05, CI: 0.01-0.19) and a significantly higher probability of swelling (0.13, CI: 0.02-0.54), and combined techniques showing a higher chance of dehiscence (0.08, CI: 0.01-0.4).
In our meta-analysis, we evaluated several surgical techniques for labia minora reduction, highlighting a few less common but innovative approaches. These methods, although not widely utilized, offer distinct advantages and warrant consideration for their unique contributions to aesthetic and functional outcomes. The bipolar radiofrequency approach stands out for its short recovery time, minimal risk of flap necrosis, and absence of scarring, hematoma, or overresection.76 Its primary drawback is the potential for burns due to heat generation. Despite limited data, patient satisfaction is reported at 100%, with no complications observed.76 However, the scarcity of studies suggests that broader application may reveal more adverse effects.
The W-shape (zigzag) resection, developed to improve upon edge and wedge resection techniques, aims to prevent complications like stiff suture lines and continuous scars that distort the labia's natural appearance.45 Although it achieves a 100% satisfaction rate, it has the highest incidence of hematoma and dehiscence (0.08, CI: 0-0.36 and 0.08, CI: 0-0.36 respectively) among the techniques evaluated, without other significant complications. Last, the Z-plasty approach modifies the wedge resection technique with 2 90° Z-plasties to excise prominent tissue, minimizing morbidities.31 It too has a 100% satisfaction rate, with dehiscence (0.13, CI: 0.02-0.4) being the major complication. Its wider adoption could offer further insights into its efficacy and complication rates. These specialized techniques, although not broadly adopted, enrich the surgical repertoire for labia minora reduction, highlighting the importance of ongoing research and careful clinical application to enhance patient care and outcomes.
Finally, surgical tools for labia minora reduction were compared. Although the scalpel is currently the preferred tool of choice for most specialists, laser-assisted labiaplasty has become more prominent in recent years. Compared to the scalpel, lower observed probability of bleeding (P = .004), swelling (P < .0001), and hematoma (P < .0001) were observed with laser, while maintaining similar levels of patient satisfaction. As laser becomes more available, we may see a significant upturn in laser for labia minora reduction due to these advantages.
Strengths
This study stands out for its comprehensiveness, involving a broader array of studies and data and more fine-grained view on methodologies employed than any previous endeavors on this topic. Additionally, we took steps to ensure the quality of the studies considered by excluding case reports and studies with inadequate data. Our new approach to stratification of studies based on their methodology and surgical tool also contributes to a more comprehensive picture, serving as a meaningful guideline for practicing clinicians.
Limitations
Despite our efforts, the available data on this subject remain scarce and heterogeneous. The present landscape could be significantly enriched by the contribution of new retrospective and prospective studies. However, the lack of standardized indicators and outcome measurements presents a formidable challenge to effective comparisons. Additionally, comparisons between surgical tools other than scalpel and laser were hindered by the lack of available information to date.
Clinical Implications
As a whole, the study indicates a high level of patient satisfaction across the various labiaplasty techniques, with a pooled satisfaction proportion of 0.9443. This demonstrates that these surgical interventions can effectively meet patients’ needs and expectations, with laser in the labiaplasty procedure being associated with a lower number of complications and similarly high patient satisfaction.
The study allows for a better understanding of which technique might best suit a given patient. Satisfaction rates remained high across all techniques, suggesting that the choice of technique may be best determined by the specifics of the individual patient's anatomy and desires, as well as the surgeon's expertise. One noteworthy finding from the study was that high satisfaction rates and low complication rates can be considered standard, but each technique has advantages and drawbacks. This suggests that a tailored approach to labiaplasty that takes into account the specific needs and anatomy of each patient may be the best approach. Due to varying levels of complications associated with different techniques, it is also clear from these results that a “1 size fits all” approach to labiaplasty is not suitable, and individualization of technique selection is necessary for optimal results. Notably, there are still new and emerging techniques for labiaplasty, warranting further study for their promising high satisfaction and low overall complication rates.
The study's findings can serve as a resource for specialized training and continuing medical education for gynecologists and other surgeons who may be performing labiaplasty. Understanding the satisfaction rates, complication rates, and other outcomes associated with various techniques and tools can help improve surgical practice and ultimately lead to better patient outcomes. Finally, these results can also assist with patient education, helping patients understand the different techniques available, their associated satisfaction rates and potential complications, and the importance of individualized treatment planning. This can empower patients to make informed decisions about their care.
Research Implications
Because the field is lacking in standardized definitions and outcome metrics, patient satisfaction questionnaires remain the most popular method for assessing the success of these operations. However, in the absence of a unified, standardized scoring system, these outcome measurements remain largely subjective, making comparison a challenging task.
CONCLUSIONS
Our results demonstrate that labiaplasty is generally safe and has high patient satisfaction rates. Notably, among the most popular techniques, composite reduction and wedge resection have a higher overall complication rate. To achieve the highest patient satisfaction, surgeons must acquire a comprehensive repertoire of techniques, treating each patient as a unique case. It is crucial to perceive the outer female genitalia as an aesthetic unit rather than isolated structures.
Supplemental Material
This article contains supplemental material located online at www.aestheticsurgeryjournal.com.
Supplementary Material
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
REFERENCES
- 1. Koning M, Zeijlmans IA, Bouman TK, van der Lei B. Female attitudes regarding labia minora appearance and reduction with consideration of media influence. Aesthet Surg J. 2009;29(1):65–71. doi: 10.1016/j.asj.2008.12.003 [DOI] [PubMed] [Google Scholar]
- 2. Yang JS, Chen WW, Skolnick J, Shakhnovich EI. All-atom ab initio folding of a diverse set of proteins. Structure. 2007;15(1):53–63. doi: 10.1016/j.str.2006.11.010 [DOI] [PubMed] [Google Scholar]
- 3. Rouzier R, Louis-Sylvestre C, Paniel BJ, Haddad B. Hypertrophy of labia minora: experience with 163 reductions. Am J Obstet Gynecol. 2000;182(1 Pt 1):35–40. doi: 10.1016/S0002-9378(00)70488-1 [DOI] [PubMed] [Google Scholar]
- 4. Veale D, Eshkevari E, Ellison N, et al. Psychological characteristics and motivation of women seeking labiaplasty. Psychol Med. 2014;44(3):555–566. doi: 10.1017/S0033291713001025 [DOI] [PubMed] [Google Scholar]
- 5. Miklos JR, Moore RD. Labiaplasty of the labia minora: patients’ indications for pursuing surgery. J Sex Med. 2008;5(6):1492–1495. doi: 10.1111/j.1743-6109.2008.00813.x [DOI] [PubMed] [Google Scholar]
- 6. Bramwell R, Morland C, Garden AS. Expectations and experience of labial reduction: a qualitative study. BJOG. 2007;114(12):1493–1499. doi: 10.1111/j.1471-0528.2007.01509.x [DOI] [PubMed] [Google Scholar]
- 7. Pardo J, Solà V, Ricci P, Guilloff E. Laser labioplasty of labia minora. Int J Gynecol Obstet. 2006;93(1):38–43. doi: 10.1016/j.ijgo.2006.01.002 [DOI] [PubMed] [Google Scholar]
- 8. Sharp G, Tiggemann M, Mattiske J. Factors that influence the decision to undergo labiaplasty: media, relationships, and psychological well-being. Aesthet Surg J. 2016;36(4):469–478. doi: 10.1093/asj/sjv270 [DOI] [PubMed] [Google Scholar]
- 9. Goodman MP, Placik OJ, Matlock DL, et al. Evaluation of body image and sexual satisfaction in women undergoing female genital plastic/cosmetic surgery. Aesthet Surg J. 2016;36(9):1048–1057. doi: 10.1093/asj/sjw061 [DOI] [PubMed] [Google Scholar]
- 10. Lapalorcia LM, Podda S, Campiglio G, Cordellini M. Labia majora labioplasty in HIV-related vaginal lipodystrophy: technique description and literature review. Aesthetic Plast Surg. 2013;37(4):711–714. doi: 10.1007/s00266-013-0159-4 [DOI] [PubMed] [Google Scholar]
- 11. ASAP (American Society for Aesthetic Plastic Surgery). Cosmetic Surgery National Data Bank Statistics 2017; 2017. Accessed October 2023. www.surgery.org
- 12. International Society of Aesthetic Plastic Surgery. ISAPS International Survey on Aesthetic/Cosmetic Procedures Performed in 2021; 2021. Accessed October 2023. www.isaps.org
- 13. Aesthetic Plastic Surgery National Databank Statistics 2022. Aesthet Surg J. 2023;43(Supplement_2):1–19. doi: 10.1093/asj/sjad354 [DOI] [PubMed] [Google Scholar]
- 14. Hamori CA. Aesthetic surgery of the female genitalia: labiaplasty and beyond. Plast Reconstr Surg. 2014;134(4):661–673. doi: 10.1097/PRS.0000000000000516 [DOI] [PubMed] [Google Scholar]
- 15. Alter GJ. Aesthetic labia minora and clitoral hood reduction using extended central wedge resection. Plast Reconstr Surg. 2008;122(6):1780–1789. doi: 10.1097/PRS.0b013e31818a9b25 [DOI] [PubMed] [Google Scholar]
- 16. Escandón JM, Duarte-Bateman D, Bustos VP, et al. Maximizing safety and optimizing outcomes of labiaplasty: a systematic review and meta-analysis. Plast Reconstr Surg. 2022;150(4):776e–788e. doi: 10.1097/PRS.0000000000009552 [DOI] [PubMed] [Google Scholar]
- 17. Higgins JPT, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (Updated February 2022). Cochrane; 2022. www.training.cochrane.org/handbook
- 18. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Motakef S, Rodriguez-Feliz J, Chung MT, Ingargiola MJ, Wong VW, Patel A. Vaginal labiaplasty: current practices and a simplified classification system for labial protrusion. Plast Reconstr Surg. 2015;135(3):774–788. doi: 10.1097/PRS.0000000000001000 [DOI] [PubMed] [Google Scholar]
- 20. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. doi: 10.1046/j.1445-2197.2003.02748.x [DOI] [PubMed] [Google Scholar]
- 21. R Core Team . R: A language and environment for statistical computing; 2021. Accessed November 2023. https://www.r-project.org/
- 22. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1(2):97–111. doi: 10.1002/jrsm.12 [DOI] [PubMed] [Google Scholar]
- 23. Paule RC, Mandel J. Consensus values, regressions, and weighting factors. J Res Natl Inst Stand Technol. 1989;94(3):197–203. doi: 10.6028/jres.094.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Viechtbauer W. Confidence intervals for the amount of heterogeneity in meta-analysis. Stat Med. 2007;26(1):37–52. doi: 10.1002/sim.2514 [DOI] [PubMed] [Google Scholar]
- 25. Knapp G, Hartung J. Improved tests for a random effects meta-regression with a single covariate. Stat Med. 2003;22(17):2693–2710. doi: 10.1002/sim.1482 [DOI] [PubMed] [Google Scholar]
- 26. Inthout J, Ioannidis JPA, Borm GF. The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Med Res Methodol. 2014;14:25. doi: 10.1186/1471-2288-14-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Higgins J, Thompson S, Deeks J, Altman D. Statistical heterogeneity in systematic reviews of clinical trials: a critical appraisal of guidelines and practice. J Health Serv Res Policy. 2002;7(1):51–61. doi: 10.1258/1355819021927674 [DOI] [PubMed] [Google Scholar]
- 28. Ellsworth WA, Rizvi M, Lypka M, et al. Techniques for labia minora reduction: an algorithmic approach. Aesthetic Plast Surg. 2010;34(1):105–110. doi: 10.1007/s00266-009-9454-5 [DOI] [PubMed] [Google Scholar]
- 29. Filho OP, Ely JB, Lee KH, Paulo EMH. Labiaplasty with stable labia minora retraction-butterfly-like approach. Plast Reconstr Surg Glob Open. 2020;8(4):e2664. doi: 10.1097/GOX.0000000000002664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Garcia V, Rodriguez Z, Rivera K, Fernandez CJP. Functional and esthetic satisfaction in patients treated with diode laser by hypertrophic labia minor. Am Soc Laser Med Surg Abstr. 2013;45(S25):1-93. doi: 10.1155/2017/8675814 [DOI] [Google Scholar]
- 31. Giraldo F, González C, De Haro F. Central wedge nymphectomy with a 90-degree Z-plasty for aesthetic reduction of the labia minora. Plast Reconstr Surg. 2004;113(6):1820–1825. doi: 10.1097/01.PRS.0000117304.81182.96 [DOI] [PubMed] [Google Scholar]
- 32. Gonzalez F, Dass D, Almeida B. Custom flask labiaplasty. Ann Plast Surg. 2015;75(3):266–271. doi: 10.1097/SAP.0000000000000048 [DOI] [PubMed] [Google Scholar]
- 33. González-Isaza P, Lotti T, França K, et al. Carbon dioxide with a new pulse profile and shape: a perfect tool to perform labiaplasty for functional and cosmetic purpose. Open Access Maced J Med Sci. 2018;6(1):25–27. doi: 10.3889/oamjms.2018.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Goodman MP, Placik OJ, Benson RH 3rd, et al. A large multicenter outcome study of female genital plastic surgery. J Sex Med. 2010;7(4_Pt_1):1565–1577. doi: 10.1111/j.1743-6109.2009.01573.x [DOI] [PubMed] [Google Scholar]
- 35. Gress S. Composite reduction labiaplasty. Aesthetic Plast Surg. 2013;37(4):674–683. doi: 10.1007/s00266-013-0149-6 [DOI] [PubMed] [Google Scholar]
- 36. Hersant B, Jabbour S, Noel W, et al. Labia majora augmentation combined with minimal labia minora resection: a safe and global approach to the external female genitalia. Ann Plast Surg. 2018;80(4):323–327. doi: 10.1097/SAP.0000000000001435 [DOI] [PubMed] [Google Scholar]
- 37. Jiang X, Chen S, Qu S, et al. A new modified labiaplasty combined with wedge de-epithelialization on the medial side and edge resection. Aesthetic Plast Surg. 2021;45(4):1869–1876. doi: 10.1007/s00266-021-02137-2 [DOI] [PubMed] [Google Scholar]
- 38. Jodoin A, Dubuc E. Labia minora surgery in the adolescent population: a cross-sectional satisfaction study. J Sex Med. 2021;18(3):623–631. doi: 10.1016/j.jsxm.2020.12.003 [DOI] [PubMed] [Google Scholar]
- 39. Jothilakshmi PK, Salvi NR, Hayden BE, Bose-Haider B. Labial reduction in adolescent population–a case series study. J Pediatr Adolesc Gynecol. 2009;22(1):53–55. doi: 10.1016/j.jpag.2008.03.008 [DOI] [PubMed] [Google Scholar]
- 40. Ju M, Wang W, Ma N, Chen W. Reduction of hypertrophic labia minora by posterior-lateral wedge resection with preservation of the central blood vessels and nerve bundle. Aesthetic Plast Surg. 2019;43(3):742–749. doi: 10.1007/s00266-019-01326-4 [DOI] [PubMed] [Google Scholar]
- 41. Karabağlı Y, Kocman EA, Velipaşaoğlu M, et al. Labia majora augmentation with de-epithelialized labial rim (minora) flaps as an auxiliary procedure for labia minora reduction. Aesthetic Plast Surg. 2015;39(3):289–293. doi: 10.1007/s00266-015-0474-z [DOI] [PubMed] [Google Scholar]
- 42. Kelishadi SS, Elston JB, Rao AJ, Tutela JP, Mizuguchi NN. Posterior wedge resection: a more aesthetic labiaplasty. Aesthet Surg J. 2013;33(6):847–853. doi: 10.1177/1090820X13494755 [DOI] [PubMed] [Google Scholar]
- 43. Li F, Li Q, Zhou Y, et al. L-shaped incision in composite reduction labiaplasty. Aesthetic Plast Surg. 2020;44(5):1854–1858. doi: 10.1007/s00266-020-01867-z [DOI] [PubMed] [Google Scholar]
- 44. Lista F, Mistry BD, Singh Y, Ahmad J. The safety of aesthetic labiaplasty: a plastic surgery experience. Aesthet Surg J. 2015;35(6):689–695. doi: 10.1093/asj/sjv002 [DOI] [PubMed] [Google Scholar]
- 45. Maas SM, Hage JJ. Functional and aesthetic labia minora reduction. Plast Reconstr Surg. 2000;105(4):1453–1456. doi: 10.1097/00006534-200004040-00030 [DOI] [PubMed] [Google Scholar]
- 46. Vázquez IM, Buendía GG, Vega AR, Oña CGR. Labiaplasty with clitoropexy. Plast Reconstr Surg Glob Open. 2019;7(5):e2239. doi: 10.1097/GOX.0000000000002239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Mayer HF, De Elizalde MLB, Duh N, Loustau HD. Bidimensional labia minora reduction. Eur J Plast Surg. 2011;34(5):345–350. doi: 10.1007/s00238-010-0487-4 [DOI] [Google Scholar]
- 48. Alter GJ. A new technique for aesthetic labia minora reduction. Ann Plast Surg. 1998;40(3):287–290. doi: 10.1097/00000637-199803000-00016 [DOI] [PubMed] [Google Scholar]
- 49. Mayer HF. Vaginal labiaplasty: current practices and a simplified classification system for labial protrusion. Plast Reconstr Surg. 2015;136(5):705e–706e. doi: 10.1097/PRS.0000000000001663 [DOI] [PubMed] [Google Scholar]
- 50. Munhoz AM, Filassi JR, Ricci MD, et al. Aesthetic labia minora reduction with inferior wedge resection and superior pedicle flap reconstruction. Plast Reconstr Surg. 2006;118(5):1237–1247. doi: 10.1097/01.prs.0000237003.24294.04 [DOI] [PubMed] [Google Scholar]
- 51. Pardo JS, Solà VD, Ricci PA, Guiloff EF, Freundlich OK. Colpoperineoplasty in women with a sensation of a wide vagina. Acta Obstet Gynecol Scand. 2006;85(9):1125–1127. doi: 10.1080/00016340600622544 [DOI] [PubMed] [Google Scholar]
- 52. Propst K, Ferrando CA. Outcomes of labiaplasty in women with labial hypertrophy. Int Urogynecol J. 2021;32(5):1247–1251. doi: 10.1007/s00192-020-04621-w [DOI] [PubMed] [Google Scholar]
- 53. Qiang S, Li F, Zhou Y, et al. A new concept for central wedge resection in labiaplasty. Gynecol Obstet Invest. 2021;86(3):257–263. doi: 10.1159/000513402 [DOI] [PubMed] [Google Scholar]
- 54. Sinnott CJ, Glickman LT, Natoli NB, Dobryansky M, Veeramachaneni HB. Outcomes, techniques, and risk factors for dehiscence in central wedge labiaplasty. Ann Plast Surg. 2020;85(S1):S68–S75. doi: 10.1097/SAP.0000000000002342 [DOI] [PubMed] [Google Scholar]
- 55. Smarrito S. Lambda laser nymphoplasty: retrospective study of 231 cases. Plast Reconstr Surg. 2014;133(2):231e–232e.. doi: 10.1097/01.prs.0000437239.53671.6f [DOI] [PubMed] [Google Scholar]
- 56. Solanki NS, Tejero-Trujeque R, Stevens-King A, Malata CM. Aesthetic and functional reduction of the labia minora using the Maas and Hage technique. J Plast Reconstr Aesthet Surg. 2010;63(7):1181–1185. doi: 10.1016/j.bjps.2009.05.053 [DOI] [PubMed] [Google Scholar]
- 57. Toplu G, Altinel D. Genital beautification and rejuvenation with combined use of surgical and non-surgical methods. Aesthetic Plast Surg. 2021;45(2):758–768. doi: 10.1007/s00266-020-01980-z [DOI] [PubMed] [Google Scholar]
- 58. Tremp M, Oranges CM, Schaefer DJ, Waldkircher NJ, Schleh AC, Kalbermatten DF. The butterfly technique: a retrospective study for labia minora reduction using an integrated approach. Plast Reconstr Surg Glob Open. 2021;9(9):e3810. doi: 10.1097/GOX.0000000000003810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Bizjak-Ogrinc U, Senčar S. Sutureless laser labiaplasty of labia minora. Sex Med. 2021;9(5):100406. doi: 10.1016/j.esxm.2021.100406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Triana L, Robledo AM. Refreshing labioplasty techniques for plastic surgeons. Aesthetic Plast Surg. 2012;36(5):1078–1086. doi: 10.1007/s00266-012-9916-z [DOI] [PubMed] [Google Scholar]
- 61. Turini T, Weck Roxo AC, Serra-Guimarães F, et al. The impact of labiaplasty on sexuality. Plast Reconstr Surg. 2018;141(1):87–92. doi: 10.1097/PRS.0000000000003921 [DOI] [PubMed] [Google Scholar]
- 62. Yang E, Hengshu Z. Individualized surgical treatment of different types of labia minora hypertrophy. Aesthetic Plast Surg. 2020;44(2):579–585. doi: 10.1007/s00266-019-01545-9 [DOI] [PubMed] [Google Scholar]
- 63. Zhou Y, Li Q, Li S, et al. Trilobal methods for composite reduction labiaplasty. Aesthetic Plast Surg. 2022;46(3):1472–1480. doi: 10.1007/s00266-022-02841-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Murariu D, Jackowe DJ, Parsa AA, Parsa FD. Comparison of wedge versus straight-line reduction labioplasty. Plast Reconstr Surg. 2010;125(3):1046–1047. doi: 10.1097/PRS.0b013e3181cb61c3 [DOI] [PubMed] [Google Scholar]
- 65. Choi HY, Kim KT. A new method for aesthetic reduction of labia minora (the deepithelialized reduction of labioplasty). Plast Reconstr Surg. 2000;105(1):419–422. doi: 10.1097/00006534-200001000-00069 [DOI] [PubMed] [Google Scholar]
- 66. Saberi Z. Simultaneous labia minora and clitoral hood reduction by introducing a new laser-assisted technique : a pilot study. Canon J Med. 2022;3(2):22–24. doi: 10.30477/CJM.2022.332366.1034 [DOI] [Google Scholar]
- 67. Qin F, Xia Z, Yang Y, et al. Labiaplasty in adolescents: indications and treatment protocol. Aesthet Surg J. 2023;43(7):NP516–NP527. doi: 10.1093/asj/sjad049 [DOI] [PubMed] [Google Scholar]
- 68. Xia Z, Liu C-Y, Yu N, et al. Three-step excision: an easy way for composite labia minora and lateral clitoral hood reduction. Plast Reconstr Surg. 2021;148(6):928e–935e. doi: 10.1097/PRS.0000000000008589 [DOI] [PubMed] [Google Scholar]
- 69. Kruk-Jeromin J, Zieliński T. Hypertrophy of labia minora–pathomorphology and surgical treatment. Ginekol Pol. 2010;81(4):298–302. [PubMed] [Google Scholar]
- 70. Cao YJ, Li FY, Li SK, et al. A modified method of labia minora reduction: the de-epithelialised reduction of the central and posterior labia minora. J Plast Reconstr Aesthet Surg. 2012;65(8):1096–1102. doi: 10.1016/j.bjps.2012.03.025 [DOI] [PubMed] [Google Scholar]
- 71. Chang S-Y, Kao S-W, Shih Y-C, Huang J-J. Labiaplasty in Asian women: motivation, technique feasibility, and patient reported outcomes. J Plast Reconstr Aesthet Surg. 2023;85:217–225. doi: 10.1016/j.bjps.2023.07.002 [DOI] [PubMed] [Google Scholar]
- 72. Felicio YDA. Labial surgery. Aesthet Surg J. 2007;27(3):322–328. doi: 10.1016/j.asj.2007.03.003 [DOI] [PubMed] [Google Scholar]
- 73. Cao Y, Li Q, Li F, et al. Aesthetic labia minora reduction with combined wedge-edge resection: a modified approach of labiaplasty. Aesthetic Plast Surg. 2015;39(1):36–42. doi: 10.1007/s00266-014-0428-x [DOI] [PubMed] [Google Scholar]
- 74. Cayrac M, Rouzier R. Traitement de l’hypertrophie des petites lèvres. Évaluation de la nymphoplastie de réduction par résection longitudinale. Gynecol Obstet Fertil. 2012;40(10):561–565. doi: 10.1016/j.gyobfe.2011.08.004 [DOI] [PubMed] [Google Scholar]
- 75. Cihantimur B, Herold C. Genital beautification: a concept that offers more than reduction of the labia minora. Aesthetic Plast Surg. 2013;37(6):1128–1133. doi: 10.1007/s00266-013-0211-4 [DOI] [PubMed] [Google Scholar]
- 76. Dayan E, Ramirez H, Theodorou S. Radiofrequency treatment of labia minora and majora: a minimally invasive approach to vulva restoration. Plast Reconstr Surg Glob Open. 2020;8(4):e2418. doi: 10.1097/GOX.0000000000002418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Schnatz P, Boardman LA; Committee on Gynecologic Practice . ACOG committee opinion #795—elective female genital cosmetic surgery. Obstet Gynecol. 2020;135(1):e36–e42. doi: 10.1097/AOG.0000000000003616 [DOI] [PubMed] [Google Scholar]
- 78. Spriggs M, Gillam L. “I don ‘ t see that as a medical problem”: clinicians ‘ attitudes and responses to requests for cosmetic genital surgery by adolescents. J Bioeth Inq. 2018;15(4):535–548. doi: 10.1007/s11673-018-9878-1 [DOI] [PubMed] [Google Scholar]
- 79. Widschwendter A, Riedl D, Freidhager K, et al. Perception of labial size and objective measurements-is there a correlation? A cross-sectional study in a cohort not seeking labiaplasty. J Sex Med. 2020;17(3):461–469. doi: 10.1016/j.jsxm.2019.11.272 [DOI] [PubMed] [Google Scholar]
- 80. Lange M, Hage JJ, Amant F. An algorithm for labia minora reduction based on a review of anatomical, configurational, and individual considerations. Arch Plast Surg. 2023;50(1):17–25. doi: 10.1055/a-1938-0991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Oranges CM, Sisti A, Sisti G. Labia minora reduction techniques: a comprehensive literature review. Aesthet Surg J. 2015;35(4):419–431. doi: 10.1093/asj/sjv023 [DOI] [PubMed] [Google Scholar]
- 82. Surroca MM, Miranda LS, Ruiz JB. Labiaplasty: a 24-month experience in 58 patients: outcomes and statistical analysis. Ann Plast Surg. 2018;80(4):316–322. doi: 10.1097/SAP.0000000000001395 [DOI] [PubMed] [Google Scholar]
- 83. Mirzabeigi MN, Moore JH Jr, Mericli AF, et al. Current trends in vaginal labioplasty: a survey of plastic surgeons. Ann Plast Surg. 2012;68(2):125–134. doi: 10.1097/SAP.0b013e31820d6867 [DOI] [PubMed] [Google Scholar]
- 84. Hodgkinson DJ, Hait G. Aesthetic vaginal labioplasty. Plast Reconstr Surg. 1987;74(3):414–416. doi: 10.1097/00006534-198409000-00015 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.