Abstract
Exercise mechanical efficiency typically falls within the range of approximately 20 to 25%. This means that a great part of the metabolic energy converted to generate movement is released as heat. Therefore, the rise in core temperature during endurance exercise in humans is proportional to generated work. Cutaneous vasodilation occurs when the core temperature threshold is reached. The rise in heart rate in response to thermal stress is a cardiovascular response that increases cardiac output and skin blood flow. The cardiovascular response during endurance exercise is a complex phenomenon potentially influenced by the involvement of nitric oxide in active thermoregulatory vasodilation. Excessive exercise can create high oxidative stress by disrupting the balance between free radicals’ production and scavenging, resulting in impaired cardiovascular function. The above considerations are related to the severity and duration of endurance exercise. The first focus of this narrative review is to provide an updated understanding of cardiovascular function during endurance exercise. We aim to explore the potential role of oxidative stress in causing cardiovascular dysfunction during endurance exercise from a fresh perspective. Additionally, we aim to identify the primary factors contributing to cardiovascular risk during strenuous prolonged exercise by highlighting recent progress in this area, which may shed light on previously unexplained physiological responses. To ascertain the effect of endurance exercise on cardiovascular function and dysfunction, a narrative review of the literature was undertaken using PubMed, ScienceDirect, Medline, Google Scholar, and Scopus. The review highlighted that high oxidative stress (due to high levels of catecholamines, shear stress, immune system activation, and renal dysfunction) leads to a rise in platelet aggregation during endurance exercise. Importantly, we clearly revealed for the first time that endothelial damage, vasoconstriction, and blood coagulation (inducing thrombosis) are potentially the primary factors of cardiovascular dysfunction and myocardial infarction during and/or following endurance exercise.
Keywords: Cardiovascular responses, Catecholamine, Exercise, Inflammation, Heat stress, Oxidative stress, Platelet aggregation, Thermoregulation
INTRODUCTION
Prolonged exercise in hot conditions induces an important increase in body temperature that can result in impaired physical and mental performances in humans [1, 2]. The rise in core temperature depends upon exercise duration and/or intensity [3, 4]. Competition for blood flow develops between thermoregulatory and metabolic processes [5] and this may become problematic during conditions where cardiac output and arterial blood pressure are reduced due to dehydration and/or severe hyperthermia [6]. Blood flow to the active muscles is required to satisfy metabolic needs, while simultaneous blood flow to the skin ensures thermoregulatory control [5]. The major cardiovascular adjustment to heat stress is an increase in skin blood flow (SkBF) in response to the increase in cardiac output [7]. Severe heat stress conditions lead to a substantial increase in resting SkBF due to thermoregulatory vasodilation [8, 9]. However, during exercise, SkBF fails to reach high levels compared to the resting state, as active skeletal muscles require a significant increase in blood flow [7]. Furthermore, prolonged exercise under warm or neutral conditions is accompanied by a complex phenomenon known as “cardiovascular drift” [10]. Cardiovascular drift manifests as a gradual increase in heart rate over time, accompanied by a decrease in both stroke volume and mean arterial pressure [10]. Traditionally, it has been suggested that cardiovascular drift reflects cardiac fatigue [11], serving as a marker of cardiovascular dysfunction and/or limitation [7]. However, we have previously proposed a novel phenomenon that can potentially explain cardiovascular drift [10], extending beyond the realm of cardiovascular fatigue alone. We posited that cardiovascular drift, characterized by changes in the force-frequency relationship, may serve as a protective strategy against potential damage induced by strong myocardial contractions [10]. It is important to note that the focus of this current narrative review does not revolve around cardiovascular drift and dehydration. Instead, our aim was to provide an updated (until December 2023) understanding of the molecules involved in mediating cutaneous vasodilation during strenuous endurance exercise in the heat and/or normothermia, along with potential risk factors contributing to cardiovascular dysfunction and fatigue. The present narrative review of the literature was undertaken using PubMed, ScienceDirect, Medline, Google Scholar, and Scopus.
MATERIALS AND METHODS
In this narrative review we searched databases including PubMed, ScienceDirect, Medline, Google Scholar, and Scopus for studies published up to 2023. The search focused on keywords such as “endurance exercise”, “cardiovascular function & dysfunction”, “thermoregulatory control”, “oxidative stress”, and “free radicals”. Inclusion criteria targeted studies relevant to the thermoregulatory control and cardiovascular responses to strenuous endurance exercise in the heat, particularly emphasizing the role of free radicals in cardiovascular function and dysfunction. Exclusion criteria encompassed non-English publications. Data extraction emphasized study design, participant details, exercise protocols, and cardiovascular measures. The quality of each study was assessed based on its design, methodology, and analytical rigor. Findings were synthesized to align with the review’s objectives, focusing on the cardiovascular responses to strenuous endurance exercise and the identified risk factors.
Thermoregulatory control during exercise
During heat exposure and/or prolonged exercise, body temperature elevation induces a rise in the diameter of cutaneous blood vessels and therefore a reduction in vascular resistance [12]. Heart rate increases to restore peripheral blood pressure. Consequently, SkBF and skin temperature increase, which enhances heat dissipation via convection [8, 13]. Moreover, heat dissipation by evaporation of sweat needs heat transfer to the skin via cutaneous vasodilation [14, 15]. Indeed, the large increase in SkBF requires a significant elevation in cardiac output and a reduction of blood flow to renal and splanchnic circulations [16]. These adjustments could be sufficient to match the demand for increased SkBF at rest [8]. However, during prolonged exercise (of moderate or high intensity) in the heat or thermoneutral conditions [4, 17, 18], the heat loss remains inferior to heat generation. Therefore, in such conditions, the body cannot stop temperature elevation or maintain steady-state core temperature. Thus, the body temperature continues to rise even after an adequate thermoregulatory response, but at a lower rate compared to when prolonged exercise was started [17, 18]. The increase in core temperature depends on both exercise intensity and duration [3, 4]. It has been identified that power output capability and integrated electromyographic activity of the muscles decrease during prolonged exercise under heat stress [19, 20]. It has been reported that the neural recruitment of skeletal muscle motor units is reduced when core body temperature rises to “critical” levels [19, 20]. The critical temperature might be one of the major factors limiting muscular function [21]. Indeed, the efferent command to active muscles is attenuated when a high core temperature is reached (e.g. ∼39-40°C) [2]. The critical temperature may function as a signal for the central nervous system, which will then inhibit motor unit recruitment to protect the brain against severe hyperthermia [2, 20, 22, 23]. We confirm that the central nervous system may reduce neural drive and attenuate skeletal muscular function to prevent overheating. On the other hand, we suggest that the decrease in myocardial function cannot be considered as a strategy for preventing overheating as it may disturb the thermoregulatory control and increase the risk of heat stroke [17]. Interestingly, it is still unknown whether the decrease in cardiac performance (i) is simply due to an alteration in preload/afterload, and/or cardiac fatigue and/or cardiac damage, or (ii) it may be partially related to a protective strategy against the potential damage that could be induced by a permanent strong myocardial contraction [10].
Cutaneous vasodilation during exercise
It is well known that cutaneous vasodilation is attenuated during exercise relative to the rest condition [5, 24]. Exercise initiation induces competition between the vasoconstrictor and vasodilator cutaneous systems [5]. Cutaneous vasoconstriction occurs in response to the initiation of exercise in heat-stressing conditions [5]. Exercise places several limits on the ability of the skin to dilate, due to an increased vasoconstrictor tone and decreased vasodilator capacity [5]. Furthermore, exercise influences the temperature threshold (which tends to rise) at which cutaneous vasodilation starts [5, 25]. Consequently, the central temperature increases brusquely in the first few minutes of exercise. Otherwise, despite further significant core temperature increases particularly in severe heat stress conditions, the rise in SkBF is attenuated when the central temperature approaches 38°C [26].
It has been reported in the literature that the exercise effect is intensity- dependent; low intensity does not alter thermoregulatory cutaneous vasodilation, whereas high intensity shifts the temperature threshold (which tends to rise) for cutaneous vasodilation [27–29]. However, the stimulus behind the exercise-induced shift in the temperature threshold for cutaneous vasodilation remains unclear [26], Interestingly, since it has been observed that cutaneous vasodilation during high-intensity exercise in the heat is attenuated relative to that during low-intensity exercise due to increased oxidative stress [30, 31], we speculate that oxidative stress is a potential factor explaining the shift in the temperature threshold.
There are several agents that have recently been found to act as vasodilators during exercise. Louie et al. [32] reported that ATP-sensitive potassium, calcium-activated potassium channels, and voltage- gated potassium channels contribute to the control of cutaneous vasodilation during exercise in heat stress conditions. Furthermore, Fujii et al. [33] highlighted that heat shock protein 90 contributed to cutaneous vasodilation during exercise via nitric oxide (NO) synthase (NOS)-dependent mechanisms. Importantly, Fujii et al. [33] also stated that NOS contributes to ∼40-50% of total cutaneous vasodilation during prolonged exercise in healthy humans. This finding reflects the major role of NOS in the thermoregulatory control (vasodilation response) during endurance exercise [33–36]. The vasodilation response to heat stress appears to be potentiated by NO production at rest and during exercise. Charkoudian et al. [37] identified that the cutaneous vasodilation response to a local warming (i.e. 30 minutes at 42°C) stimulus is biphasic and NO plays an important role in both the initiation and the maintenance of the second slower phase.
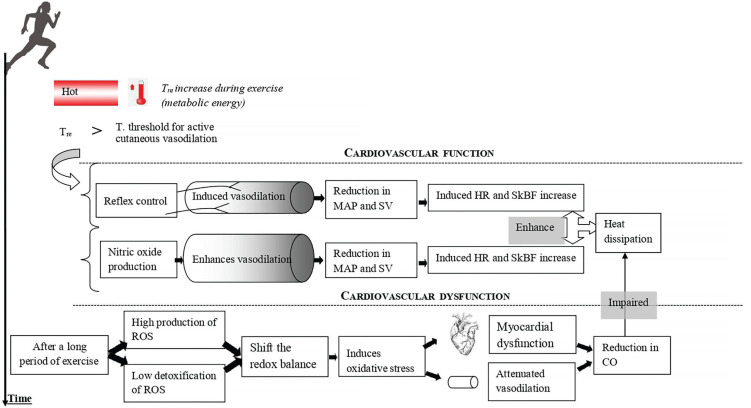
Mechanisms mediating cutaneous vasodilation differ between whole-body and local skin heating [38]. However, it appears that there are some common points between them (e.g. NO-induced vasodilation) [33–36]. The skin vasodilation response to endurance exercise depends on reflex control (i.e. sensory nerve-mediated vasodilation) and free radicals (cutaneous endothelial NO-dependent vasodilation) (Figure 1). It has been demonstrated that skin vasodilation in heat stress depends on NO at rest and during exercise, with sensory nerves mediating an initial transient vasodilatory “peak” followed by a prolonged vasodilatory “plateau” mediated primarily by NO production [33, 39, 40]. We highlight that it is still unknown whether the source of NO during “local heating” is the same as the one released during exercise where the heat generation comes from the muscular work. Future research should pay more attention to such issues.
FIG. 1.
Simplified representation of the cardiovascular response to prolonged exercise. CO: cardiac output. HR: heart rate. MAP: mean arterial pressure. ROS: reactive oxygen species. SkBF: skin blood flow. SV: stroke volume. T: temperature. Tre: rectal temperature.
Cardiovascular fatigue related to oxidative stress during endurance exercise
Multiple factors contribute to cardiovascular fatigue during prolonged exercise and make it a complex phenomenon [41–43]. Meta-analyses revealed a reduction in left ventricular function following 24-h exercise [42, 43]. During prolonged exercise, the large displacement of blood flow toward the skin appears to play a key role in the development of cardiovascular fatigue [17].
Exercise results in an increase in heart rate, which increases the mechanical forces of blood flow on the vascular wall (i.e. shear stress and blood pressure) [44]. Shear stress has been shown to increase endothelial superoxide generation in conductance arteries in vivo [45]. Similarly, high levels of shear stress during prolonged exercise have been found to stimulate vascular superoxide and hydrogen peroxide production [46]. Exercise-induced oxidative stress has recently been well confirmed [47–51], and it is well established that the increased production of reactive oxygen species (ROS) during exercise has both positive and negative physiological effects [47, 51–53]. The latter may shift the redox balance to a pro-oxidant state and impair thermoregulatory vasodilation [47, 49, 51]. According to this fact, studies indicated that NOS-dependent cutaneous vasodilation during high-intensity exercise in the heat is attenuated relative to that during moderate-intensity exercise due to increased oxidative stress [30, 31].
Nicotinamide adenine dinucleotide phosphate oxidase enzyme (NADPH) is the major source of ROS in the heart [54, 55], and also well known for its role in myocardial dysfunction [55]. Interestingly, a significant link between NADPH oxidase-dependent oxidative stress and myocardial dysfunction has been identified after prolonged strenuous exercise in rats [56–58]. This might potentially represent a new trigger in the understanding of exercise-induced myocardial dysfunction. High oxidative stress was proposed to depress cardiac function through protein kinase G and cyclic monophosphate-mediated desensitization of cardiac myofilaments [59].
Furthermore, a long period of exercise increases catecholamine and pro-inflammatory markers such as tumour necrosis factor and interleukin- 6 (IL-6) [60–62]. Excess catecholamines contribute to an increase in ROS formation [61], and attenuation of β-adrenergic inotropic responsiveness [63–66]. A previous study highlighted that cardiac stress induced by exercise activates both oxidative stress, inflammation and β-adrenergic pathways [67]. It is well known that oxidative stress and inflammation are potentially involved in the pathogenesis of heart failure and impaired left ventricular function [56–58, 68, 69]. Interestingly, the administration of IL-1 and tumour necrosis factor is associated with a decline in contractile function in rats’ hearts, this being partially improved by treatment with an NOS inhibitor [70]. Moreover, antioxidant supplementation may attenuate the decline in myocardial function during exercise [67, 71, 72].
Does inflammation cause cardiovascular risk during endurance exercise?
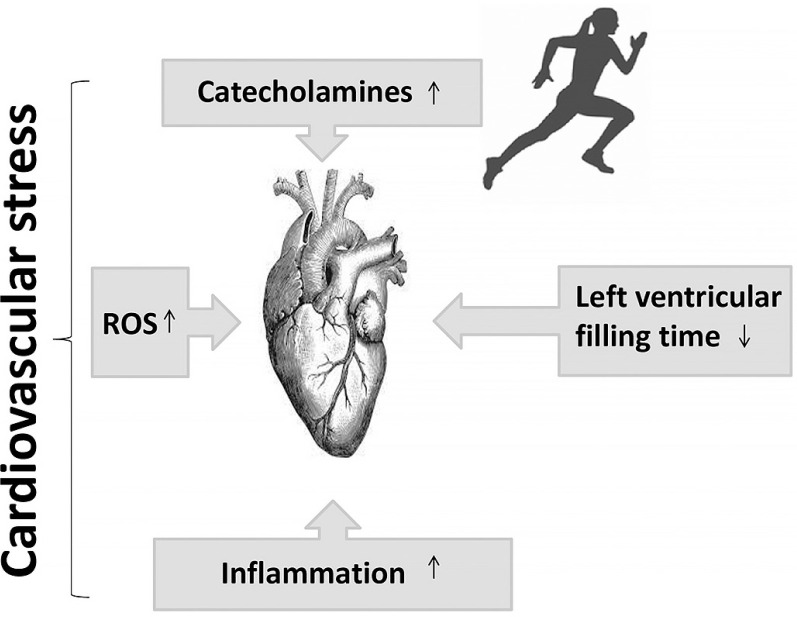
For a considerable period, the notion of cardiovascular risk has been associated with increased cardiovascular stress leading to alterations (decline) in cardiovascular function [12, 17] (Figure 2). Recent studies have attributed the decline in cardiac function during exercise to adrenergic desensitization (βj and β2 receptors), [10, 73, 74], which attenuates cardiac function and provides cardioprotection against acute stressors induced by exercise, such as mechanical stress, cellular damage, and mitochondrial damage [10, 42, 75]. Interestingly, alongside the controlled mechanisms of β-adrenergic receptor desensitization and β3 activation, high levels of oxidative stress linked to inflammation [10, 62, 76, 77] may also contribute to the attenuation of cardiac function.
FIG. 2.
Putative mechanisms leading to cardiovascular stress during exercise. ROS: reactive oxygen species.
In fact, studies have demonstrated that inhibition of endogenous NO leads to an enhancement of the effects of catecholamines [78–80], indicating that NO may play a cardio-protective role by attenuating the effect of catecholamines, potentiating the positive inotropic effect in normal hearts. Accordingly, it has been confirmed that the increase in NO concentrations attenuates the positive inotropic effect of catecholamines [81]. Furthermore, certain molecules associated with inflammation, such as IL-10, brain-derived neurotrophic factor, and follistatin-like protein, which increase during or after exercise, may also play a cardio-protective role by facilitating tissue repair and regeneration [82]. These findings raise a crucial question regarding the initial causes of cardiovascular risk. The primary focus of the present narrative review is to elucidate our current understanding of cardiovascular dysfunction during prolonged exercise with respect to inflammation and oxidative stress. Additionally, we aim to identify the primary cause of cardiovascular risk.
Cardio-renal association and immune response activation Renal vasoconstriction and NADPH oxidase activation
The large increase in SkBF during endurance exercise requires a significant reduction of renal blood flow [16]. The decrease in renal blood flow [16] constitutes a potential factor for the decline in renal function. Sustained levels of sympathetic activity and dehydration may contribute to the increase in plasma renin activity and circulating angiotensin II [83, 84]. Then, the activation of angiotensin II type 1 receptors (i) elevates ROS production through NADPH oxidase activation [85–87], and (ii) stimulates aldosterone secretion [88, 89]. In turn, aldosterone can directly stimulate ROS production through the activation of NADPH oxidase [90]. Importantly, the stimulation of aldosterone release is linked to an increase in galectin-3 concentration in the heart and kidney [77, 91]. Galectin-3 and other markers of cardiac damage (e.g. troponin I, suppression of tumorigenicity 2 (ST2)) increase following strenuous physical effort [92, 93]. Interestingly, as at December 2023, there remains no explanation of the reason for this increase, which has been suggested to be physiological [94, 95]. This narrative review seeks to clarify our comprehension of the factors contributing to the elevation of galectin-3 levels in reaction to strenuous endurance exercise.
Galectin-3 and inflammatory biomarkers
When cardiovascular tissues are physically damaged, the immune system is activated in order to remove the damaged cells and maintain homeostasis in the body [96]. Galectin-3 seems to play an important role in immune response activation [97] by stimulating hyperoxide secretion from neutrophils through NADPH activation [98, 99]. Neutrophils are generated and sent to the site of injury within minutes and are the hallmark of acute inflammation [100]. Suzuki [101] highlighted the protective role of neutrophils in the exercise-induced muscle damage associated with high production of ROS. Hence, neutrophil levels have been shown to double during prolonged strenuous exercise and remain elevated for at least 24 h [102].
Galectin-3 is actually considered a reasonable cardiovascular inflammatory biomarker [97]. Although galectin-3 is identified as a risk predictor of adverse events and cardiac arrest [103, 104], its levels correlate also with tissue repair [105, 106]. Galectin-3 should not be considered a pathogenic molecule inducing cardiovascular damage, since it contributes to activation of the immune system, playing a cardioprotective role during exercise. Interestingly, it was observed that the blood levels of galectin-3 in endurance athletes were more elevated than in sedentary healthy humans at the beginning and the end of exercise [107], confirming that galectin-3 can play a cardioprotective role in athletes. A 2020 review suggested that galectin-3 could be used as a novel treatment for atherosclerosis [97]. In fact, galectin-3 can play an anti-inflammatory role and exert a beneficial effect on atherosclerosis by activating M2 macrophage differentiation, via the CD98/ phosphoinositide 3-kinase pathway [108]. On the other hand, we highlight that a clinical 2022 study found that galectin-3 accumulation potentiates platelet aggregation via dectin-1 activation [109], which can promote thrombosis during/or following exercise.
Aldosterone, fibroblast growthfactor 23 and parathyroid hormone
It is well established that fibroblast growth factor 23 (FGF-23), a newly discovered hormone, and parathyroid hormone (PTH) are markers of chronic kidney injury and cardiovascular impairment (i.e. ventricular hypertrophy, vascular calcification, and arterial stiffness) [110]. The literature revealed that high-intensity endurance exercise training is associated with arterial stiffness [111], ventricular hypertrophy [112], and coronary artery calcification [113, 114]. Importantly, the increase in PTH level depends on exercise severity (intensity and duration), suggesting a complex cause-and-effect relationship between PTH and coronary artery calcification [113]. Currently (December 2023), the mechanism explaining PTH elevation during exercise is not yet well understood. In fact, RAS is activated during prolonged exercise [115], indicating a decline in renal function and then an impairment in calcium and phosphate regulation. Therefore, PTH and FGF-23 are both secreted to restore calcium and decrease phosphate levels [116].
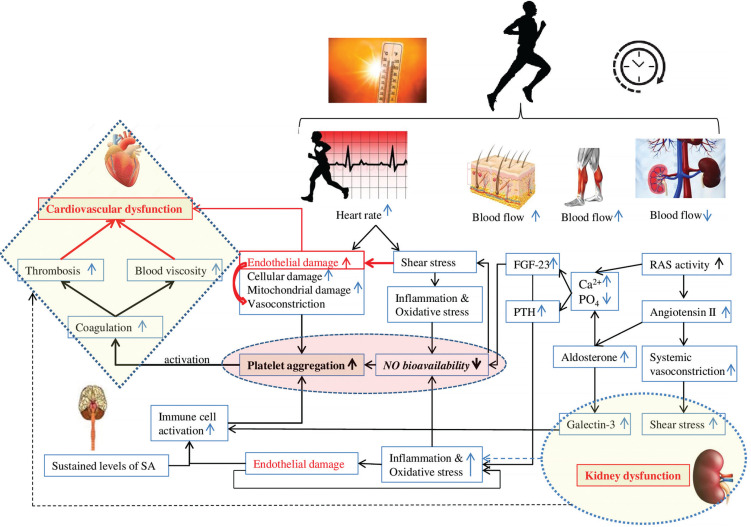
We hypothesize that aldosterone, PTH and FGF-23 play a key role in the development of cardiovascular fatigue during exercise: Aldosterone increases oxidative stress, reduces NO levels, and promotes platelet adhesion possibly by potentiating collagen production [117, 118], triggering a cascade of coagulation. We believe that aldosterone can play a crucial role in the development of thrombosis, resulting in cardiovascular dysfunction during and following endurance exercise. FGF23 directly alters endothelial vasodilation function by reducing NO bioavailability [119] (Figure 3). Importantly, clinical studies identified a strong correlation between PTH elevation and hypercoagulability [120]. One could speculate that PTH can contribute to blood coagulation and cardiovascular dysfunction during prolonged exercise possibly by affecting calcium levels and potentiating oxidative stress [121].
FIG. 3.
Potential factors contributing to coagulation and cardiovascular dysfunction during prolonged exercise. FGF-23: fibroblast growth factor 23. PTH: parathyroid hormone. RAS: renin-angiotensin-aldosterone system. SA: sympathetic activity.
Toll-like receptor 4 (tlr4) and coagulation
The analysis of TLR4 is a promising advanced orientation in the search for understanding cardiovascular dysfunction [122]. Indeed, a single bout of exercise induces TLR4 activation, promoting endoplasmic reticulum stress [122, 123], an inflammatory response [122–124], and increased markers of cardiac injury [122, 123] and apoptosis [122] (i.e. heart-damaging events), which are necessary mechanisms for remodelling and adaptation [122]. Interestingly, it has been recently suggested that nuclear factor- kappa B (NF-kβ) activation by TLR4 is a necessary mechanism for cardiovascular adaptations induced by physical effort [122]. According to Gordon et al. [125], NF-kP can promote desirable adaptive responses. Cardioprotection is triggered during or immediately after exercise when cells are under oxidative stress [126]
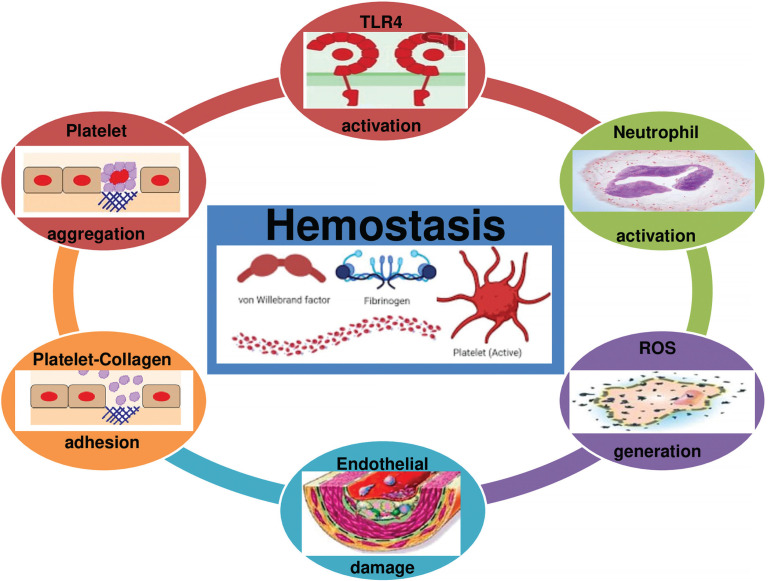
Although TLR4 is a physiological response favouring apoptosis and tissue regeneration to assure beneficial adaptive responses to exercise, evidence suggests that TLR4 promotes acute coagulation [127] via NF-kβ activation, neutrophil activation, ROS generation, and platelet aggregation [127, 128] (Figure 4). Therefore, we highlight that TLR4 activation by acute strenuous exercise can result in undesirable cardiac events (myocardial infarction or sudden death), particularly in people with cardiovascular diseases [41].
FIG. 4.
Toll-like receptor 4 (TLR4) promotes acute coagulation via neutrophil activation, ROS generation and platelet aggregation. ROS: Reactive oxygen species.
What is the primary cause of cardiovascular risk?
To date (December 2023), inflammation has traditionally been regarded as the primary cause of cardiovascular dysfunction during endurance exercise. However, there is abundant evidence indicating that the inflammatory response is not the primary cause of dysfunction [129]. Importantly, some anti-inflammatory cytokines (e.g. IL-10) inhibit activation of coagulation and regulate thrombosis [130, 131]. Furthermore, it is well established that the IL-33/ST2 axis exhibits a cardioprotective role, reducing fibrosis and cardiomyocyte hypertrophy, and improving myocardial function in both chronic and acute heart failure [132]. Moreover, creatine kinase is traditionally considered an indicator of tissue damage and subsequent fatigue. Creatine kinase’s function is intriguing. Its role in cardioprotection, particularly through the inhibition of ADP-triggered platelet activation [133], underscores the imperative for researchers to recalibrate and deepen their perspectives on the multifaceted biological responses to exercise.
White blood cells and platelet counts are reported to be elevated after prolonged strenuous exercise [134–136]. It was reported that inhibition of platelet aggregation by NO was decreased following acute prolonged strenuous exercise. The attenuated response of platelets to NO during exercise results in thrombotic complications [137]. Moreover, NADPH plays a crucial role in ROS generation and platelet activation [138]. Indeed, such activation despite its protective role through haemostasis-inducing coagulation can result in thrombosis, myocardial infarction, and cardiac arrest [139].
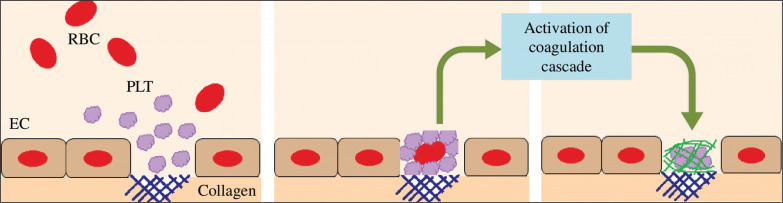
Moreover, it is well established that strenuous exercise induces endothelial damage/vascular injury [10]. The damage of endothelial cells results in vasoconstriction and exposes the collagen substratum to the blood circulating at high shear rates [128]. Therefore, platelets circulating at high velocity will adhere to collagen. The adherent platelets then aggregate. Platelets are then activated (by secreting ADP, serotonin and TxA2) which promotes a cascade of coagulation [128] (Figure 5). Therefore, endothelial damage can further trigger haemostasis, resulting in a high level of blood viscosity, potentiating thrombosis and cardiovascular dysfunction during and/or following exercise.
FIG. 5.
Platelets are activated when binding to the collagen substratum, which promotes a cascade of coagulation. EC: endothelial cell. PLT: platelet. RBC: red blood cell.
In summary, our review suggests that the primary causes of cardiovascular risk during acute endurance exercise are two-fold. Firstly, cell damage (involving endothelial and mitochondrial cells) emerges as a significant contributor. The stress imposed during exercise can lead to damage in these cells and result in vasoconstriction, potentially impacting cardiovascular function and overall risk. Secondly, blood coagulation (due to cell damage, inflammation, renal dysfunction, and high oxidative stress) leading to thrombosis and an increase in blood viscosity, plays a crucial role in cardiovascular risk. These factors can affect blood flow dynamics and potentially lead to adverse cardiovascular events. Additionally, it is important to consider coronary artery calcification as a risk factor that may be exacerbated after high-load training. This calcification process can further contribute to the overall cardiovascular risk profile.
In conclusion, the combination of several factors –(i) shear stressinduced endothelial damage promoting coagulation cascade and then thrombosis, (ii) oxidative stress, inflammation, renal dysfunction, and immune activation promoting blood coagulation and then thrombosis, and (iii) vasoconstriction (due to endothelial damage, oxidative stress, and haemostasis) promoting thrombosis – contributes to the increased cardiovascular fatigue and risk (myocardial infarction) during and/or following strenuous endurance exercise. Finally, we highlight that dehydration can potentiate cardiovascular fatigue and the risk of cardiovascular infarction.
Perspective and limitations
Our hypothesis revolves around the notion that excessive oxidative stress, potentially linked to shear stress, cellular damage, renal dysfunction, and activation of the immune response, contributes to cardiovascular dysfunction through the promotion of platelet aggregation. This hypothesis is firmly grounded, supported by compelling evidence indicating that vigorous exercise leads to a significant rise in platelet aggregation and activation [140, 141]. Additionally, there exist various other molecules associated with impaired energetic metabolism and cardiovascular dysfunction (such as free fatty acids, cholesterol, low-density lipoprotein, catecholamines, and serotonin) [142] that may further exacerbate coagulation during and/or following exercise [143, 144]. Investigating the complex association of these variables with coagulation warrants comprehensive exploration in future studies. Of particular interest, the use of antithrombotic therapy holds promising potential in counteracting coagulation-induced cardiovascular fatigue. However, caution must be exercised due to the inherent risk of bleeding complications. Markers of cardiac/renal damage (e.g. galectin-3) increase during and/or following exercise; however, there has been no explanation of the reason for this response, which has been suggested to be physiological (i.e. non-pathological), though it remains unexplained to date. Notably, this increase in markers is potentially associated with activation of TLR4. TLR4 activation promotes an inflammatory response and increases markers of cardiac injury, which are crucial for remodelling. Immune activation and inflammatory responses to acute exercise are both adequate physiological responses, ensuring a cardioprotective role by optimizing cardiovascular adaptation to physical effort (i.e. training). However, excessive immune system activation and inflammation during exercise are associated with a heightened risk of cardiac events. Although evidence suggests that galectin-3 is secreted to promote physiological cardiac remodelling and immune system activation, it is not yet clear whether galectin-3 contributes to cardiovascular dysfunction by promoting platelet activation and thrombosis (i.e. by activating dectin-1/spleen tyrosine kinase signalling). This narrative review serves as a call to researchers to explore and investigate this potential pathway for a better understanding of cardiovascular risk prevention through exercise.
The present narrative review, while providing valuable insights, does have additional perspectives. We acknowledge that not all biomarkers of inflammation (e.g. IL-6 and IL-17), iron deficiency, and numerous other factors potentially exacerbating coagulation during exercise have been discussed. Furthermore, our focus centred on oxidative stress during exercise, while neglecting the influence of other factors, including alterations in pH, calcium levels, and energy metabolism, which can also contribute to cardiovascular dysfunction [145]. We encourage further exploration in this field to enhance our understanding of cardiovascular dysfunction during prolonged exercise by incorporating additional information and complementing our current knowledge base.
CONCLUSIONS
The thermoregulatory vasodilation during prolonged exercise primarily relies on reflex control and nitric oxide production. However, extensive evidence from the literature indicates that cutaneous vasodilation during strenuous exercise is impaired by excessive ROS production and increased oxidative stress. Furthermore, reducing the inhibitory effects of nitric oxide on platelet aggregation during prolonged strenuous exercise may result in potentially dangerous thrombotic complications.
Prolonged strenuous exercise has been shown to increase NADPH oxidase activity, shift the redox balance to a pro-oxidant state, and impair renal and cardiovascular function. NADPH plays a critical role in the formation of ROS, as well as immune and platelet activation. Although such activation serves an immune-protective function, it can lead to coagulation and myocardial infarction.
Acknowledgments
Open access was provided by the Heart Failure Laboratory of Research (LR12SP09), Farhat HACHED Hospital, Sousse, Tunisia.
Funding Statement
Funding This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interests
The authors declare that they have no competing interests.
Declaration
In order to correct and improve the academic writing of our paper, we have used the language model ChatGPT 3.5 [146, 147].
REFERENCES
- 1.MacDougall JD, Reddan WG, Layton CR, Dempsey JA. Effects of metabolic hyperthermia on performance during heavy prolonged exercise. J Appl Physiol. 1974;36(5):538–44. Epub 1974/05/01. doi: 10.1152/jappl.1974.36.5.538. PubMed PMID: 4826315. [DOI] [PubMed] [Google Scholar]
- 2.Nielsen B, Nybo L. Cerebral changes during exercise in the heat. Sports Med. 2003;33(1):1–11. doi: 10.2165/00007256-200333010-00001. PubMed PMID: 12477374. [DOI] [PubMed] [Google Scholar]
- 3.Kenny GP, Niedre PC. The effect of exercise intensity on the post-exercise esophageal temperature response. Eur J Appl Physiol. 2002;86(4):342–6. doi: 10.1007/s00421-001-0538-4. PubMed PMID: 11990748. [DOI] [PubMed] [Google Scholar]
- 4.Souissi A, Yousfi N, Dabboubi R, Aloui G, Haddad M, Souissi N. Effect of acute melatonin administration on physiological response to prolonged exercise. Biol Rhythm Res. 2020;51(6):980–7. doi: 10.1080/09291016.2019.1573462. [DOI] [Google Scholar]
- 5.Kellogg D Jr, Johnson J, Kosiba W. Competition between cutaneous active vasoconstriction and active vasodilation during exercise in humans. Am J Physiol. 1991. Oct; 261(4 Pt 2):H1184–9. doi: 10.1152/ajpheart.1991.261.4.H1184. PMID: 1928401. [DOI] [PubMed] [Google Scholar]
- 6.Murray R. Dehydration, hyperthermia, and athletes: science and practice. J Athl Train. 1996;31(3):248–52. PubMed PMID: 16558408; PubMed Central PMCID: . [PMC free article] [PubMed] [Google Scholar]
- 7.Rowell LB. Human cardiovascular adjustments to exercise and thermal stress. Physiol Rev. 1974;54(1):75–159. doi: 10.1152/physrev.1974.54.1.75. PubMed PMID: 4587247. [DOI] [PubMed] [Google Scholar]
- 8.Johnson, JM and Proppe DW. Cardiovascular adjustments to heat stress. In Comprehensive Physiology, Terjung R. (Ed.). 2011. https://doi.org/10.1002/cphy.cp040111. doi: https://doi.org/10.1002/cphy.cp040111. [Google Scholar]
- 9.Taylor WF, Johnson JM, O’Leary D, Park MK. Effect of high local temperature on reflex cutaneous vasodilation. J Appl Physiol Respir Environ Exerc Physiol. 1984;57(1):191–6. doi: 10.1152/jappl.1984.57.1.191. PubMed PMID: 6469780. [DOI] [PubMed] [Google Scholar]
- 10.Souissi A, Haddad M, Dergaa I, Ben Saad H, Chamari K. A new perspective on cardiovascular drift during prolonged exercise. Life Sci. 2021;287:120109. Epub 20211027. doi: 10.1016/j.lfs.2021.120109. PubMed PMID: 34717912. [DOI] [PubMed] [Google Scholar]
- 11.Saltin B, Stenberg J. Circulatory response to prolonged severe exercise. J Appl Physiol. 1964;19(5):833–8. doi: 10.1152/jappl.1964.19.5.833. PubMed PMID: 14207729. [DOI] [PubMed] [Google Scholar]
- 12.Crandall CG, Gonzalez-Alonso J. Cardiovascular function in the heat-stressed human. Acta Physiol (Oxf). 2010;199(4):407–23. Epub 20100324. doi: 10.1111/j.1748-1716.2010.02119.x. PubMed PMID: 20345414; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnson JM. Exercise and the cutaneous circulation. Exerc Sport Sci Rev. 1992;20:59–97. PMID: 1623893. [PubMed] [Google Scholar]
- 14.Hargreaves M. Physiological limits to exercise performance in the heat. J Sci Med Sport. 2008;11(1):66–71. Epub 20070827. doi: 10.1016/j.jsams.2007.07.002. PubMed PMID: 17720623. [DOI] [PubMed] [Google Scholar]
- 15.Galloway SD, Maughan RJ. Effects of ambient temperature on the capacity to perform prolonged cycle exercise in man. Med Sci Sports Exerc. 1997;29(9):1240–9. doi: 10.1097/00005768-199709000-00018. PubMed PMID: 9309637. [DOI] [PubMed] [Google Scholar]
- 16.Kenney MJ, Fels RJ. Sympathetic nerve regulation to heating is altered in senescent rats. Am J Physiol Regul Integr Comp Physiol. 2002. Aug; 283(2):R513–20. doi: 10.1152/ajpregu.00683.2001. PMID: 12121865. [DOI] [PubMed] [Google Scholar]
- 17.Periard JD, Caillaud C, Thompson MW. The role of aerobic fitness and exercise intensity on endurance performance in uncompensable heat stress conditions. Eur J Appl Physiol. 2012;112(6):1989–99. Epub 20110923. doi: 10.1007/s00421-011-2165-z. PubMed PMID: 21947407. [DOI] [PubMed] [Google Scholar]
- 18.Souissi A, Dergaa I, Musa S, Saad HB, Souissi N. Effects of daytime ingestion of melatonin on heart rate response during prolonged exercise. Mov Sport Sci/Sci Mot. 2022(115):25–32. doi: 10.1051/sm/2021020. [DOI] [Google Scholar]
- 19.Tucker R, Rauch L, Harley YX, Noakes TD. Impaired exercise performance in the heat is associated with an anticipatory reduction in skeletal muscle recruitment. Pflugers Arch. 2004. Jul; 448(4):422–30. doi: 10.1007/s00424-004-1267-4. Epub 2004 May 8. PMID: 15138825. [DOI] [PubMed] [Google Scholar]
- 20.Gordon R, Tillin NA, Tyler CJ. The effect of head and neck per-cooling on neuromuscular fatigue following exercise in the heat. Appl Physiol Nutr Metab. 2020;45(11):1238–46. Epub 20200521. doi: 10.1139/apnm-2020-0079. PubMed PMID: 32437624. [DOI] [PubMed] [Google Scholar]
- 21.Racinais S, Periard JD, Karlsen A, Nybo L. Effect of heat and heat acclimatization on cycling time trial performance and pacing. Med Sci Sports Exerc. 2015;47(3):601–6. doi: 10.1249/MSS.0000000000000428. PubMed PMID: 24977692; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gonzalez-Alonso J, Teller C, Andersen SL, Jensen FB, Hyldig T, Nielsen B. Influence of body temperature on the development of fatigue during prolonged exercise in the heat. J Appl Physiol (1985). 1999. Mar; 86(3):1032–9. doi: 10.1152/jappl.1999.86.3.1032. PMID: 10066720. [DOI] [PubMed] [Google Scholar]
- 23.Morrison SF. Central control of body temperature. F1000Res. 2016. May 12; 5: F1000 Faculty Rev-880. doi: 10.12688/f1000research.7958.1. PMID: 27239289; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johnson JM, Park MK. Effect of heat stress on cutaneous vascular responses to the initiation of exercise. J Appl Physiol Respir Environ Exerc Physiol. 1982;53(3):744–9. doi: 10.1152/jappl.1982.53.3.744. PubMed PMID: 7129999. [DOI] [PubMed] [Google Scholar]
- 25.Charkoudian N. Mechanisms and modifiers of reflex induced cutaneous vasodilation and vasoconstriction in humans. J Appl Physiol (1985). 2010. Oct; 109(4):1221–8. doi: 10.1152/japplphysiol.00298.2010. Epub 2010 May 6. PMID: 20448028; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kenney WL, Johnson JM. Control of skin blood flow during exercise. Med Sci Sports Exerc. 1992;24(3):303–12. PubMed PMID: 1549024. [PubMed] [Google Scholar]
- 27.Mack GW, Nose H, Takamata A, Okuno T, Morimoto T. Influence of exercise intensity and plasma volume on active cutaneous vasodilation in humans. Med Sci Sports Exerc. 1994;26(2):209–16. doi: 10.1249/00005768-199402000-00011. PubMed PMID: 8164538. [DOI] [PubMed] [Google Scholar]
- 28.Smolander J, Saalo J, Korhonen O. Effect of work load on cutaneous vascular response to exercise. J Appl Physiol (1985). 1991. Oct; 71(4):1614–9. doi: 10.1152/jappl.1991.71.4.1614. PMID: 1757390. [DOI] [PubMed] [Google Scholar]
- 29.Taylor WF, Johnson JM, Kosiba WA, Kwan CM. Graded cutaneous vascular responses to dynamic leg exercise. J Appl Physiol (1985). 1988. May; 64(5):1803–9. doi: 10.1152/jappl.1988.64.5.1803. PMID: 3391884. [DOI] [PubMed] [Google Scholar]
- 30.Fujii N, McGinn R, Stapleton JM, Paull G, Meade RD, Kenny GP. Evidence for cyclooxygenase-dependent sweating in young males during intermittent exercise in the heat. J Physiol. 2014;592(23):5327–39. Epub 20141017. doi: 10.1113/jphysiol.2014.280651. PubMed PMID: 25326453; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Meade RD, Fujii N, Alexander LM, Paull G, Louie JC, Flouris AD, et al. Local infusion of ascorbate augments NO-dependent cutaneous vasodilatation during intense exercise in the heat. J Physiol. 2015;593(17):4055–65. Epub 20150728. doi: 10.1113/JP270787. PubMed PMID: 26110415; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Louie JC, Fujii N, Meade RD, Kenny GP. The interactive contributions of Na(+) /K(+) -ATPase and nitric oxide synthase to sweating and cutaneous vasodilatation during exercise in the heat. J Physiol. 2016;594(12):3453–62. Epub 20160329. doi: 10.1113/JP271990. PubMed PMID: 26852741; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fujii N, Zhang SY, McNeely BD, Nishiyasu T, Kenny GP. Heat shock protein 90 contributes to cutaneous vasodilation through activating nitric oxide synthase in young male adults exercising in the heat. J Appl Physiol (1985). 2017. Oct 1; 123(4):844–850. doi: 10.1152/japplphysiol.00446.2017. Epub 2017 Jul 27. PMID: 28751373; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McNamara TC, Keen JT, Simmons GH, Alexander LM, Wong BJ. Endothelial nitric oxide synthase mediates the nitric oxide component of reflex cutaneous vasodilatation during dynamic exercise in humans. J Physiol. 2014;592(23):5317–26. Epub 20140925. doi: 10.1113/jphysiol.2014.272898. PubMed PMID: 25260636; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Welch G, Foote KM, Hansen C, Mack GW. Nonselective NOS inhibition blunts the sweat response to exercise in a warm environment. J Appl Physiol (1985). 2009. Mar; 106(3):796–803. doi: 10.1152/japplphysiol.90809.2008. Epub 2009 Jan 8. PMID: 19131481; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fujii N, Meade RD, Alexander LM, Akbari P, Foudil-Bey I, Louie JC, et al. iNOS-dependent sweating and eNOS-dependent cutaneous vasodilation are evident in younger adults, but are diminished in older adults exercising in the heat. J Appl Physiol (1985). 2016. Feb 1; 120(3):318–27. doi: 10.1152/japplphysiol.00714.2015. Epub 2015 Nov 19. PubMed PMID: 26586908; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Charkoudian N, Eisenach JH, Atkinson JL, Fealey RD, Joyner MJ. Effects of chronic sympathectomy on locally mediated cutaneous vasodilation in humans. J Appl Physiol (1985). 2002. Feb; 92(2):685–90. doi: 10.1152/japplphysiol.00758.2001. PubMed PMID: 11796682. [DOI] [PubMed] [Google Scholar]
- 38.Kellogg DL, Jr., Zhao JL, Wu Y. Roles of nitric oxide synthase isoforms in cutaneous vasodilation induced by local warming of the skin and whole body heat stress in humans. J Appl Physiol (1985). 2009. Nov; 107(5):1438–1444. doi: 10.1152/japplphysiol.00690.2009. Epub 2009 Sep 10. PubMed PMID: 19745188; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kellogg DL, Jr., Liu Y, Kosiba IF, O’Donnell D. Role of nitric oxide in the vascular effects of local warming of the skin in humans. J Appl Physiol (1985). 1999. Apr; 86(4):1185–1190. doi: 10.1152/jappl.1999.86.4.1185. PubMed PMID: 10194201. [DOI] [PubMed] [Google Scholar]
- 40.Minson CT, Berry LT, Joyner MJ. Nitric oxide and neurally mediated regulation of skin blood flow during local heating. Nitric Oxide. [DOI] [PubMed] [Google Scholar]
- 41.Eijsvogels TM, Fernandez AB, Thompson PD. Are there deleterious cardiac effects of acute and chronic endurance exercise? Physiol Rev. 2016. Jan; 96(1):99–125. doi: 10.1152/physrev.00029.2014. PubMed PMID: 26607287; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lord RN, Utomi V, Oxborough DL, Curry BA, Brown M, George KP. Left ventricular function and mechanics following prolonged endurance exercise: an update and meta-analysis with insights from novel techniques. Eur J Appl Physiol. 2018;118(7):1291–1299. Epub 20180605. doi: 10.1007/s00421-018-3906-z. PubMed PMID: 29869711; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Middleton N, Shave R, George K, Whyte G, Hart E, Atkinson G. Left ventricular function immediately following prolonged exercise: A meta-analysis. Med Sci Sports Exerc. 2006;38(4):681–687. doi: 10.1249/01.mss.0000210203.10200.12. PubMed PMID: 16679983. [DOI] [PubMed] [Google Scholar]
- 44.Kojda G, Hambrecht R. Molecular mechanisms of vascular adaptations to exercise. Physical activity as an effective antioxidant therapy? Cardiovasc Res. 2005. Aug 1; 67(2):187–197. doi: 10.1016/j.cardiores.2005.04.032. PMID: 15935334. [DOI] [PubMed] [Google Scholar]
- 45.Laurindo FR, Pedro Mde A, Barbeiro HV, Pileggi F, Carvalho MH, Augusto O, et al. Vascular free radical release. Ex vivo and in vivo evidence for a flow-dependent endothelial mechanism. Circ Res. 1994. Apr; 74(4):700–709. doi: 10.1161/01.res.74.4.700. PMID: 7511072. [DOI] [PubMed] [Google Scholar]
- 46.Lauer N, Suvorava T, Ruther U, Jacob R, Meyer W, Harrison DG, et al. Critical involvement of hydrogen peroxide in exercise-induced up-regulation of endothelial NO synthase. Cardiovasc Res. 2005. Jan 1; 65(1):254–262. doi: 10.1016/j.cardiores.2004.09.010. PMID: 15621054. [DOI] [PubMed] [Google Scholar]
- 47.Trinity JD, Broxterman RM, Richardson RS. Regulation of exercise blood flow: Role of free radicals. Free Radic Biol Med. 2016;98:90–102. Epub 2016 Feb 10. doi: 10.1016/j.freeradbiomed.2016.01.017. PubMed PMID: 26876648; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kruk J, Aboul-Enein BH, Duchnik E. Exercise-induced oxidative stress and melatonin supplementation: current evidence. J Physiol Sci. 2021;71(1):27. Epub 2021 Sep 1. doi: 10.1186/s12576-021-00812-2. PubMed PMID: 34470608; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Powers SK, Deminice R, Ozdemir M, Yoshihara T, Bomkamp MP, Hyatt H. Exercise-induced oxidative stress: Friend or foe? J Sport Health Sci. 2020;9(5):415–425. Epub 2020 May 4. doi: 10.1016/j.jshs.2020.04.001. PubMed PMID: 32380253; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Powers SK, Nelson WB, Hudson MB. Exercise-induced oxidative stress in humans: cause and consequences. Free Radic Biol Med. 2011;51(5):942–950. Epub 2010 Dec 16. doi: 10.1016/j.freeradbiomed.2010.12.009. PubMed PMID: 21167935. [DOI] [PubMed] [Google Scholar]
- 51.Kawamura T, Muraoka I. Exercise-induced oxidative stress and the effects of antioxidant intake from a physiological viewpoint. Antioxidants (Basel). 2018;7(9):119. Epub 2018 Sep 5. doi: 10.3390/antiox7090119. PubMed PMID: 30189660; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Souissi A, Ben Maaouia G, Dergaa I, Ghram A, Ben Saad H. The fat burning ability of melatonin during submaximal exercise. Biol Rhythm Res. 2023;54(3):307–321. doi: 10.1080/09291016.2022.2157531. [DOI] [Google Scholar]
- 53.Souissi A, Dergaa I, Chtourou H, Ben Saad H. The effect of daytime ingestion of melatonin on thyroid hormones responses to acute submaximal exercise in healthy active males: A pilot study. Am J Mens Health. 2022;16(1):15579883211070383. doi: 10.1177/15579883211070383. PubMed PMID: 35060417; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lambeth JD. NOX enzymes and the biology of reactive oxygen. Nat Rev Immunol. 2004;4(3):181–189. doi: 10.1038/nri1312. PubMed PMID: 15039755. [DOI] [PubMed] [Google Scholar]
- 55.Murdoch CE, Zhang M, Cave AC, Shah AM. NADPH oxidase-dependent redox signalling in cardiac hypertrophy, remodelling and failure. Cardiovasc Res. 2006. Jul 15; 71(2):208–215. doi: 10.1016/j.cardiores.2006.03.016. Epub 2006 Mar 27. PubMed PMID: 16631149. [DOI] [PubMed] [Google Scholar]
- 56.Vitiello D, Boissière J, Doucende G, Gayrard S, Polge A, Faure P, et al. β-Adrenergic receptors desensitization is not involved in exercise-induced cardiac fatigue: NADPH oxidase-induced oxidative stress as a new trigger. J Appl Physiol (1985). 2011. Nov; 111(5):1242–1248. doi: 10.1152/japplphysiol.00449.2011. Epub 2011 Jun 30. PubMed PMID: 21719731. [DOI] [PubMed] [Google Scholar]
- 57.Nie J, Close G, George KP, Tong TK, Shi Q. Temporal association of elevations in serum cardiac troponin T and myocardial oxidative stress after prolonged exercise in rats. Eur J Appl Physiol. 2010;110(6):1299–303. Epub 20100814. doi: 10.1007/s00421-010-1604-6. PubMed PMID: 20711602. [DOI] [PubMed] [Google Scholar]
- 58.Vitiello D. Connexin 43 dephosphorylation: a potential underlying mechanism involved in exercise-induced cardiac fatigue. Austin Biol. 2016;1(4):1018. [Google Scholar]
- 59.Tavernier B, Li JM, El-Omar MM, Lanone S, Yang ZK, Trayer IP, et al. Cardiac contractile impairment associated with increased phosphorylation of troponin I in endotoxemic rats. FASEB J. 2001;15(2):294–296. Epub 20001208. doi: 10.1096/fj.00-0433fje. PubMed PMID: 11156941. [DOI] [PubMed] [Google Scholar]
- 60.Jee H, Jin Y. Effects of prolonged endurance exercise on vascular endothelial and inflammation markers. J Sports Sci Med. 2012;11(4):719–726. Epub 20121201. PubMed PMID: 24150084; PubMed Central PMCID: . [PMC free article] [PubMed] [Google Scholar]
- 61.Kruk J, Kotarska K, Aboul-Enein BH. Physical exercise and catecholamines response: benefits and health risk: possible mechanisms. Free Radic Res. 2020;54(2–3):105–125. Epub 20200218. doi: 10.1080/10715762.2020.1726343. PubMed PMID: 32020819. [DOI] [PubMed] [Google Scholar]
- 62.Krzeminski K, Buraczewska M, Miskiewicz Z, Dabrowski J, Steczkowska M, Kozacz A, et al. Effect of ultra-endurance exercise on left ventricular performance and plasma cytokines in healthy trained men. Biol Sport. 2016;33(1):63–69. Epub 20151231. doi: 10.5604/20831862.1189767. PubMed PMID: 26985136; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Massion PB, Feron O, Dessy C, Balligand JL. Nitric oxide and cardiac function: ten years after, and continuing. Circ Res. 2003. Sep 5; 93(5):388–398. doi: 10.1161/01.RES.0000088351.58510.21. PMID: 12958142. [DOI] [PubMed] [Google Scholar]
- 64.Shah AM, MacCarthy PA. Paracrine and autocrine effects of nitric oxide on myocardial function. Pharmacol Ther. 2000. Apr; 86(1):49–86. doi: 10.1016/s0163-7258(99)00072-8. PMID: 10760546. [DOI] [PubMed] [Google Scholar]
- 65.Cotton JM, Kearney MT, MacCarthy PA, Grocott-Mason RM, McClean DR, Heymes C, et al. Effects of nitric oxide synthase inhibition on Basal function and the force-frequency relationship in the normal and failing human heart in vivo. Circulation. 2001;104(19):2318–2323. Epub 2001/11/07. doi: 10.1161/hc4401.098515. PubMed PMID: 11696472. [DOI] [PubMed] [Google Scholar]
- 66.Ziolo MT, Katoh H, Bers DM. Positive and negative effects of nitric oxide on Ca(2+) sparks: influence of beta-adrenergic stimulation. Am J Physiol Heart Circ Physiol. 2001;281(6):H2295–H2303. doi: 10.1152/ajpheart.2001.281.6.H2295. PubMed PMID: 11709395. [DOI] [PubMed] [Google Scholar]
- 67.Chakouri N, Reboul C, Boulghobra D, Kleindienst A, Nottin S, Gayrard S, et al. Stress-induced protein S-glutathionylation and phosphorylation crosstalk in cardiac sarcomeric proteins - Impact on heart function. Int J Cardiol. 2018;258:207–216. doi: 10.1016/j.ijcard.2017.12.004. PubMed PMID: 29544934. [DOI] [PubMed] [Google Scholar]
- 68.Lord KC, Shenouda SK, McIlwain E, Charalampidis D, Lucchesi PA, Varner KJ. Oxidative stress contributes to methamphetamine-induced left ventricular dysfunction. Cardiovasc Res. 2010. Jul 1; 87(1):111–118. doi: 10.1093/cvr/cvq043. Epub 2010 Feb 5. PMID: 20139112; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Souissi A, Dergaa I, Romdhani M, Ghram A, Irandoust K, Chamari K, et al. Can melatonin reduce the severity of post-COVID-19 syndrome? EXCLI J. 2023. Feb 2; 22:173–187. doi: 10.17179/excli2023-5864. PMID: 36998709; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Schulz R, Panas DL, Catena R, Moncada S, Olley PM, Lopaschuk GD. The role of nitric oxide in cardiac depression induced by interleukin-1 beta and tumour necrosis factor-alpha. Br J Pharmacol. 1995. Jan; 114(1):27–34. doi: 10.1111/j.1476-5381.1995.tb14901.x. PMID: 7536096; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Emami A, Tofighi A, Asri-Rezaei S, Bazargani-Gilani B. The effect of short-term coenzyme Q10 supplementation and pre-cooling strategy on cardiac damage markers in elite swimmers. Br J Nutr. 2018;119(4):381–390. doi: 10.1017/S0007114517003774. PubMed PMID: 29498347. [DOI] [PubMed] [Google Scholar]
- 72.Souissi A, Dergaa I. An overview of the potential effects of melatonin supplementation on athletic performance. Int J Sport Stud Hlth. 2021;4(1):e121714. doi: 10.5812/intjssh.121714. [DOI] [Google Scholar]
- 73.Hart E, Dawson E, Rasmussen P, George K, Secher NH, Whyte G, et al. Beta-adrenergic receptor desensitization in man: insight into post-exercise attenuation of cardiac function. J Physiol. 2006. Dec 1; 577(Pt 2):717–725. doi: 10.1113/jphysiol.2006.116426. Epub 2006 Sep 14. PMID: 16973702; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Banks L, Sasson Z, Busato M, Goodman JM. Impaired left and right ventricular function following prolonged exercise in young athletes: influence of exercise intensity and responses to dobutamine stress. J Appl Physiol (1985). 2010. Jan; 108(1):112–119. doi: 10.1152/japplphysiol.00898.2009. Epub 2009 Nov 5. PMID: 19892922. [DOI] [PubMed] [Google Scholar]
- 75.Coates AM, King TJ, Currie KD, Tremblay JC, Petrick HL, Slysz JT, et al. Alterations in cardiac function following endurance exercise are not duration dependent. Front Physiol. 2020;11:581797. Epub 2020 Sep 18. doi: 10.3389/fphys.2020.581797. PubMed PMID: 33071833; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Silva SD, Jr., Jara ZP, Peres R, Lima LS, Scavone C, Montezano AC, et al. Temporal changes in cardiac oxidative stress, inflammation and remodeling induced by exercise in hypertension: Role for local angiotensin II reduction. PLoS One. 2017;12(12):e0189535. Epub 2017 Dec 12. doi: 10.1371/journal.pone.0189535. PubMed PMID: 29232407; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Burtscher J, Vanderriele P-E, Legrand M, Predel H-G, Niebauer J, O’Keefe JH, et al. Could repeated cardio-renal injury trigger late cardiovascular sequelae in extreme endurance athletes? Sports Med. 2022. Dec; 52(12):2821–2836. doi: 10.1007/s40279-022-01734-8. Epub 2022 Jul 18. PubMed PMID: 35851948; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Muller-Strahl G, Kottenberg K, Zimmer HG, Noack E, Kojda G. Inhibition of nitric oxide synthase augments the positive inotropic effect of nitric oxide donors in the rat heart. J Physiol. 2000;522 Pt 2(Pt 2):311–320. doi: 10.1111/j.1469-7793.2000.00311.x. PubMed PMID: 10639106; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Balligand JL, Kelly RA, Marsden PA, Smith TW, Michel T. Control of cardiac muscle cell function by an endogenous nitric oxide signaling system. Proc Natl Acad Sci U S A. 1993;90(1):347–351. doi: 10.1073/pnas.90.1.347. PubMed PMID: 7678347; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Keaney JF, Jr., Hare JM, Balligand JL, Loscalzo J, Smith TW, Colucci WS. Inhibition of nitric oxide synthase augments myocardial contractile responses to beta-adrenergic stimulation. Am J Physiol. 1996;271(6 Pt 2):H2646–H2652. doi: 10.1152/ajpheart.1996.271.6.H2646. PubMed PMID: 8997327. [DOI] [PubMed] [Google Scholar]
- 81.Reading S, Barclay J. The inotropic effect of nitric oxide on mammalian papillary muscle is dependent on the level of beta1-adrenergic stimulation. Can J Physiol Pharmacol. 2002. Jun; 80(6):569–577. doi: 10.1139/y02-085. PubMed PMID: 12117306. [DOI] [PubMed] [Google Scholar]
- 82.Sierra APR, Martinez Galan BS, de Sousa CAZ, de Menezes DC, Branquinho JLO, Neves RL, et al. Exercise induced-cytokines response in marathon runners: Role of ACE I/D and BDKRB2 +9/-9 polymorphisms. Front Physiol. 2022;13:919544. Epub 2022-09-02. doi: 10.3389/fphys.2022.919544. PubMed PMID: 36117688; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tidgren B, Hjemdahl P, Theodorsson E, Nussberger J. Renal neurohormonal and vascular responses to dynamic exercise in humans. J Appl Physiol (1985). 1991. May; 70(5):2279–2286. doi: 10.1152/jappl.1991.70.5.2279. PubMed PMID: 1677937. [DOI] [PubMed] [Google Scholar]
- 84.Aldigier J, Huang H, Dalmay F, Lartigue M, Baussant T, Chassain A, et al. Angiotensin-converting enzyme inhibition does not suppress plasma angiotensin II increase during exercise in humans. J Cardiovasc Pharmacol. 1993. Feb; 21(2):289–295. doi: 10.1097/00005344-199302000-00015. PubMed PMID: 7679164. [DOI] [PubMed] [Google Scholar]
- 85.Griendling KK, Ushio-Fukai M. Reactive oxygen species as mediators of angiotensin II signaling. Regul Peptides. 2000;91(1–3):21–27. doi: 10.1016/s0167-0115(00)00136-1. PubMed PMID: 10967199. [DOI] [PubMed] [Google Scholar]
- 86.Hanna IR, Taniyama Y, Szöcs K, Rocic P, Griendling KK. NAD(P)H oxidase-derived reactive oxygen species as mediators of angiotensin II signaling. Antioxid Redox Signal. 2002. Dec; 4(6):899–914. doi: 10.1089/152308602762197443. PubMed PMID: 12573139. [DOI] [PubMed] [Google Scholar]
- 87.Harrison DG, Cai H, Landmesser U, Griendling KK. Interactions of angiotensin II with NAD(P)H oxidase, oxidant stress and cardiovascular disease. J Renin Angiotensin Aldosterone Syst. 2003;4(2):51–61. doi: 10.3317/jraas.2003.014. PubMed PMID: 12806586. [DOI] [PubMed] [Google Scholar]
- 88.Lastra-Lastra G, Sowers JR, Restrepo-Erazo K, Manrique-Acevedo C, Lastra-Gonzalez G. Role of aldosterone and angiotensin II in insulin resistance: an update. Clin Endocrinol (Oxf). 2009;71(1):1–6. Epub 2008 Dec 5. doi: 10.1111/j.1365-2265.2008.03498.x. PubMed PMID: 19138313. [DOI] [PubMed] [Google Scholar]
- 89.Li LH, Kao WF, Chiu YH, Hou SK, Meng C, How CK. Impact of renin-angiotensin-aldosterone system activation and body weight change on N-terminal pro-B-type natriuretic peptide variation in 100-km ultramarathon runners. J Chin Med Assoc. 2020;83(1):48–54. doi: 10.1097/JCMA.0000000000000227. PubMed PMID: 31770190. [DOI] [PubMed] [Google Scholar]
- 90.Miyata K, Rahman M, Shokoji T, Nagai Y, Zhang G-X, Sun G-P, et al. Aldosterone stimulates reactive oxygen species production through activation of NADPH oxidase in rat mesangial cells. J Am Soc Nephrol. 2005. Oct; 16(10):2906–2912. doi: 10.1681/ASN.2005040390. Epub 2005 Aug 31. PubMed PMID: 16135774. [DOI] [PubMed] [Google Scholar]
- 91.Giam B, Kaye DM, Rajapakse NW. Role of renal oxidative stress in the pathogenesis of the cardiorenal syndrome. Heart Lung Circ. 2016;25(8):874–880. Epub 2016 Apr 16. doi: 10.1016/j.hlc.2016.02.022. PubMed PMID: 27132623. [DOI] [PubMed] [Google Scholar]
- 92.Hättasch R, Spethmann S, de Boer RA, Ruifrok WP, Schattke S, Wagner M, et al. Galectin-3 increase in endurance athletes. Europ J Prev Cardiol. 2014. Oct; 21(10):1192–1199. doi: 10.1177/2047487313492069. Epub 2013 May 30. PubMed PMID: 23723328. [DOI] [PubMed] [Google Scholar]
- 93.Shaheen HAA, Mohamed MA, Basset FHA, Rashed MH, Theruvan NB, Mosbah SA. Heart failure prediction in athletic heart remodeling among long distance runners. World J Cardiovasc Dis. 2022;12(1):1–10. doi: 10.4236/wjcd.2022.121001. [DOI] [Google Scholar]
- 94.Wilson M, O’Hanlon R, Prasad S, Oxborough D, Godfrey R, Alpendurada F, et al. Biological markers of cardiac damage are not related to measures of cardiac systolic and diastolic function using cardiovascular magnetic resonance and echocardiography after an acute bout of prolonged endurance exercise. Br J Sports Med. 2011;45(10):780–784. Epub 2009 Oct 23. doi: 10.1136/bjsm.2009.064089. PubMed PMID: 19854761. [DOI] [PubMed] [Google Scholar]
- 95.Donnellan E, Phelan D. Biomarkers of cardiac stress and injury in athletes: What do they mean? Curr Heart Fail Rep. 2018;15(2):116–122. doi: 10.1007/s11897-018-0385-9. PubMed PMID: 29520707. [DOI] [PubMed] [Google Scholar]
- 96.Park SA, Hyun YM. Neutrophil extravasation cascade: What can we learn from two-photon intravital imaging? Immune Netw. 2016. Dec; 16(6):317–321. doi: 10.4110/in.2016.16.6.317. Epub 2016 Dec 22. PubMed PMID: 28035206; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Gao Z, Liu Z, Wang R, Zheng Y, Li H, Yang L. Galectin-3 is a potential mediator for atherosclerosis. J Immunol Res. 2020. Feb 14; 2020:5284728. doi: 10.1155/2020/5284728. PubMed PMID: 32149158; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Karlsson A, Follin P, Leffler H, Dahlgren C. Galectin-3 activates the NADPH-oxidase in exudated but not peripheral blood neutrophils. Blood. 1998;91(9):3430–3438. PubMed PMID: 9558402. [PubMed] [Google Scholar]
- 99.Almkvist J, Faldt J, Dahlgren C, Leffler H, Karlsson A. Lipopolysaccharide-induced gelatinase granule mobilization primes neutrophils for activation by galectin-3 and formylmethionyl-Leu-Phe. Infect Immun. 2001;69(2):832–837. doi: 10.1128/IAI.69.2.832-837.2001. PubMed PMID: 11159975; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Cohen S, Burns R. Pathways of the pulp, 8th ed. St. Louis: CV Mosby Co; St. Louis, Missouri. 2002;64146. [Google Scholar]
- 101.Suzuki K. Involvement of neutrophils in exercise-induced muscle damage and its modulation. Gen Intern Med Clin Innov. 2018;3:1–8. doi: 10.15761/GIMCI.1000170. [DOI] [Google Scholar]
- 102.Pedersen BK, Toft AD. Effects of exercise on lymphocytes and cytokines. Br J Sports Med. 2000;34(4):246–251. doi: 10.1136/bjsm.34.4.246. PubMed PMID: 10953894; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Gehlken C, Suthahar N, Meijers WC, de Boer RA. Galectin-3 in heart failure: An update of the last 3 years. Heart Fail Clin. 2018;14(1):75–92. doi: 10.1016/j.hfc.2017.08.009. PubMed PMID: 29153203. [DOI] [PubMed] [Google Scholar]
- 104.Suthahar N, Meijers WC, Sillje HHW, Ho JE, Liu FT, de Boer RA. Galectin-3 Activation and inhibition in heart failure and cardiovascular disease: An update. theranostics. 2018;8(3):593–609. Epub 20180101. doi: 10.7150/thno.22196. PubMed PMID: 29344292; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Akimoto Y, Ikehara S, Yamaguchi T, Kim J, Kawakami H, Shimizu N, et al. Galectin expression in healing wounded skin treated with low-temperature plasma: Comparison with treatment by electronical coagulation. Arch Biochem Biophys. 2016;605:86–94. Epub 20160128. doi: 10.1016/j.abb.2016.01.012. PubMed PMID: 26827730. [DOI] [PubMed] [Google Scholar]
- 106.González GE, Cassaglia P, Truant SN, Fernández MM, Wilensky L, Volberg V, et al. Int J Cardiol. 2014. Oct 20; 176(3):1423–5. doi: 10.1016/j.ijcard.2014.08.011. Epub 2014 Aug 8. PMID: 25150483. [DOI] [PubMed] [Google Scholar]
- 107.Hättasch R, Spethmann S, de Boer RA, Ruifrok WP, Schattke S, Wagner M, et al. Galectin-3 increase in endurance athletes. Eur J Prev Cardiol. 2014;21(10):1192–9. Epub 20130530. doi: 10.1177/2047487313492069. PubMed PMID: 23723328. [DOI] [PubMed] [Google Scholar]
- 108.MacKinnon AC, Farnworth SL, Hodkinson PS, Henderson NC, Atkinson KM, Leffler H, et al. Regulation of alternative macrophage activation by galectin-3. J Immunol. 2008;180(4):2650–8. doi: 10.4049/jimmunol.180.4.2650. PubMed PMID: 18250477. [DOI] [PubMed] [Google Scholar]
- 109.Chen Y, Fu W, Zheng Y, Yang J, Liu Y, Qi Z, et al. Galectin 3 enhances platelet aggregation and thrombosis via Dectin-1 activation: a translational study. Europ Heart J. 2022;43(37):3556–74. doi: 10.1093/eurheartj/ehac034. PubMed PMID: 35165707; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Schefold JC, Filippatos G, Hasenfuss G, Anker SD, von Haehling S. Heart failure and kidney dysfunction: epidemiology, mechanisms and management. Nat Rev Nephrol. 2016;12(10):610–23. Epub 20160830. doi: 10.1038/nrneph.2016.113. PubMed PMID: 27573728. [DOI] [PubMed] [Google Scholar]
- 111.Calleja-Romero A, Vicente-Rodriguez G, Garatachea N. Acute effects of long-distance races on heart rate variability and arterial stiffness: A systematic review and meta-analysis. J Sports Sci. 2022;40(3):248–70. Epub 20211031. doi: 10.1080/02640414.2021.1986276. PubMed PMID: 34720045. [DOI] [PubMed] [Google Scholar]
- 112.Ohman EM, Teo KK, Johnson AH, Collins PB, Dowsett DG, Ennis JT, et al. Abnormal cardiac enzyme responses after strenuous exercise: alternative diagnostic aids. Br Med J (Clin Res Ed). 1982;285(6354):1523–6. doi: 10.1136/bmj.285.6354.1523. PubMed PMID: 6814629; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Zambrano A, Tintut Y, Demer LL, Hsu JJ. Potential mechanisms linking high-volume exercise with coronary artery calcification. Heart. 2023;109(15):1139–45. Epub 20230712. doi: 10.1136/heartjnl-2022-321986. PubMed PMID: 36702539; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.DeFina LF, Radford NB, Barlow CE, Willis BL, Leonard D, Haskell WL, et al. Association of all-cause and cardiovascular mortality with high levels of physical activity and concurrent coronary artery calcification. JAMA Cardiol. 2019;4(2):174–81. doi: 10.1001/jamacardio.2018.4628. PubMed PMID: 30698608; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Luger A, Deuster PA, Debolt JE, Loriaux DL, Chrousos GP. Acute exercise stimulates the renin-angiotensin-aldosterone axis: adaptive changes in runners. Horm Res. 1988;30(1):5–9. doi: 10.1159/000181017. PubMed PMID: 2851526. [DOI] [PubMed] [Google Scholar]
- 116.Kovesdy CP, Quarles LD. The role of fibroblast growth factor-23 in cardiorenal syndrome. Nephron Clin Pract. 2013;123(3–4):194–201. Epub 20130806. doi: 10.1159/000353593. PubMed PMID: 23942553; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Gromotowicz A, Szemraj J, Stankiewicz A, Zakrzeska A, Mantur M, Jaroszewicz E, et al. Study of the mechanisms of aldosterone prothrombotic effect in rats. J Renin Angiotensin Aldosterone Sys. 2011;12(4):430–439. [DOI] [PubMed] [Google Scholar]
- 118.Brilla CG. Renin–angiotensin–aldosterone system and myocardial fibrosis. Cardiovasc Research. 2000;47(1):1–3. [DOI] [PubMed] [Google Scholar]
- 119.Silswal N, Touchberry CD, Daniel DR, McCarthy DL, Zhang S, Andresen J, et al. FGF23 directly impairs endothelium-dependent vasorelaxation by increasing superoxide levels and reducing nitric oxide bioavailability. Am J Physiol Endocrinol Metab. 2014;307(5):E426–E436. Epub 20140722. doi: 10.1152/ajpendo.00264.2014. PubMed PMID: 25053401; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Squizzato A, Van Zaane B, Gerdes VE, Büller HR. The influence of pituitary, adrenal, and parathyroid hormones on hemostasis and thrombosis. Semin Thromb Hemost. 2011. Feb; 37(1):41–48. doi: 10.1055/s-0030-1270070. Epub 20110119. PMID: 21249603. [DOI] [PubMed] [Google Scholar]
- 121.Lombardi G, Ziemann E, Banfi G, Corbetta S. Physical activity-dependent regulation of parathyroid hormone and calcium-phosphorous metabolism. Int J Mol Sci. 2020;21(15):5388. Epub 20200729. doi: 10.3390/ijms21155388. PubMed PMID: 32751307; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.de Vicente LG, Pinto AP, Munoz VR, Rovina RL, da Rocha AL, Gaspar RC, et al. TLR4 participates in the responses of markers of apoptosis, inflammation, and ER stress to different acute exercise intensities in mice hearts. Life Sci. 2020;240:117107. Epub 20191127. doi: 10.1016/j.lfs.2019.117107. PubMed PMID: 31785241. [DOI] [PubMed] [Google Scholar]
- 123.Cristi-Montero C, Sanchez-Collado P, Veneroso C, Cuevas MJ, Gonzalez-Gallego J. Effect of an acute exercise bout on Toll-like receptor 4 and inflammatory mechanisms in rat heart. Rev Med Chil. 2012;140(10):1282–1288. doi: 10.4067/S0034-98872012001000007. PubMed PMID: 23559285. [DOI] [PubMed] [Google Scholar]
- 124.Wang R-p, Yao Q, Xiao Y-b, Zhu S-b, Yang L, Feng J-m, et al. Toll-like receptor 4/nuclear factor-kappa B pathway is involved in myocardial injury in a rat chronic stress model. Stress. 2011. Sep; 14(5):567–575. doi: 10.3109/10253890.2011.571729. Epub 2011 Jun 15. PMID: 21675862. [DOI] [PubMed] [Google Scholar]
- 125.Gordon JW, Shaw JA, Kirshenbaum LA. Multiple facets of NF-κB in the heart: to be or not to NF-κB. Circ Res. 2011. Apr 29; 108(9):1122–1132. doi: 10.1161/CIRCRESAHA.110.226928. PMID: 32932194. [DOI] [PubMed] [Google Scholar]
- 126.de Vicente LG, Pinto AP, da Rocha AL, Pauli JR, de Moura LP, Cintra DE, et al. Role of TLR4 in physical exercise and cardiovascular diseases. Cytokine. 2020;136:155273. Epub 20200912. doi: 10.1016/j.cyto.2020.155273. PubMed PMID: 32932194. [DOI] [PubMed] [Google Scholar]
- 127.Ding N, Chen G, Hoffman R, Loughran PA, Sodhi CP, Hackam DJ, et al. Toll-like receptor 4 regulates platelet function and contributes to coagulation abnormality and organ injury in hemorrhagic shock and resuscitation. Circ Cardiovasc Genet. 2014;7(5):615–624. Epub 20140721. doi: 10.1161/CIRCGENETICS.113.000398. PubMed PMID: 25049041; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Semple JW, Italiano JE Jr., Freedman J. Platelets and the immune continuum. Nat Rev Immunol. 2011;11(4):264–274. doi: 10.1038/nri2956. PubMed PMID: 21436837. [DOI] [PubMed] [Google Scholar]
- 129.Coates AM, Petrick HL, Millar PJ, Burr JF. Exercise alters cardiac function independent of acute systemic inflammation in healthy men. Am J Physiol Heart Circ Physiol. 2021;320(5):H1762–H73. Epub 20210312. doi: 10.1152/ajpheart.00809.2020. PubMed PMID: 33710926. [DOI] [PubMed] [Google Scholar]
- 130.Downing LJ, Strieter RM, Kadell AM, Wilke CA, Austin JC, Hare BD, et al. IL-10 regulates thrombus-induced vein wall inflammation and thrombosis. J Immunol. 1998;161(3):1471–1476. PubMed PMID: 9686613. [PubMed] [Google Scholar]
- 131.Pajkrt D, van der Poll T, Levi M, Cutler DL, Affrime MB, van den Ende A, et al. Interleukin-10 inhibits activation of coagulation and fibrinolysis during human endotoxemia. Blood. 1997;89(8):2701–2705. PubMed PMID: 9108387. [PubMed] [Google Scholar]
- 132.Villacorta H, Maisel AS. Soluble ST2 Testing: A Promising biomarker in the management of heart failure. Arq Bras Cardiol. 2016;106(2):145–152. Epub 20160115. doi: 10.5935/abc.20150151. PubMed PMID: 26761075; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Horjus DL, Nieuwland R, Boateng KB, Schaap MC, van Montfrans GA, Clark JF, et al. Creatine kinase inhibits ADP-induced platelet aggregation. Sci Rep. 2014;4(1):6551. Epub 20141009. doi: 10.1038/srep06551. PubMed PMID: 25298190; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Kratz A, Lewandrowski KB, Siegel AJ, Chun KY, Flood JG, Van Cott EM, et al. Effect of marathon running on hematologic and biochemical laboratory parameters, including cardiac markers. Am J Clin Pathol. 2002;118(6):856–863. doi: 10.1309/14TY-2TDJ-1X0Y-1V6V. PubMed PMID: 12472278. [DOI] [PubMed] [Google Scholar]
- 135.Reid SA, Speedy DB, Thompson JM, Noakes TD, Mulligan G, Page T, et al. Study of hematological and biochemical parameters in runners completing a standard marathon. Clin J Sport Med. 2004;14(6):344–353. doi: 10.1097/00042752-200411000-00004. PubMed PMID: 15523206. [DOI] [PubMed] [Google Scholar]
- 136.Bird SR, Linden M, Hawley JA. Acute changes to biomarkers as a consequence of prolonged strenuous running. Ann Clin Biochem. 2014. Mar; 51(2):137–150. doi: 10.1177/0004563213492147. Epub 2013 Sep 2. [DOI] [PubMed] [Google Scholar]
- 137.Sakita S, Kishi Y, Numano F. Acute vigorous exercise attenuates sensitivity of platelets to nitric oxide. Thromb Res. 1997;87(5):461–71. doi: 10.1016/s0049-3848(97)00162-x. PubMed PMID: 9306620. [DOI] [PubMed] [Google Scholar]
- 138.Delaney MK, Kim K, Estevez B, Xu Z, Stojanovic-Terpo A, Shen B, et al. Differential roles of the NADPH-Oxidase 1 and 2 in Platelet activation and thrombosis. Arterioscler Thromb Vasc Biol. 2016;36(5):846–854. Epub 2016 Mar 17. doi: 10.1161/ATVBAHA.116.307308. PubMed PMID: 26988594; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Smith JE. Effects of strenuous exercise on haemostasis. Br J Sports Med. 2003;37(5):433–435. doi: 10.1136/bjsm.37.5.433. PubMed PMID: 14514536; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Kestin AS, Ellis PA, Barnard MR, Errichetti A, Rosner BA, Michelson AD. Effect of strenuous exercise on platelet activation state and reactivity. Circulation. 1993;88(4 Pt 1):1502–1511. doi: 10.1161/01.cir.88.4.1502. PubMed PMID: 8403298. [DOI] [PubMed] [Google Scholar]
- 141.el-Sayed MS. Effects of exercise on blood coagulation, fibrinolysis and platelet aggregation. Sports Med. 1996;22(5):282–298. doi: 10.2165/00007256-199622050-00002. PubMed PMID: 8923646. [DOI] [PubMed] [Google Scholar]
- 142.Dawson E, George K, Shave R, Whyte G, Ball D. Does the human heart fatigue subsequent to prolonged exercise? Sports Med. 2003;33(5):365–380. doi: 10.2165/00007256-200333050-00003. PMID: 12696984. [DOI] [PubMed] [Google Scholar]
- 143.Poole JC. The effect of certain fatty acids on the coagulation of plasma in vitro. Br J Exp Pathol. 1955;36(3):248–253. PubMed PMID: 13239980; PubMed Central PMCID: . [PMC free article] [PubMed] [Google Scholar]
- 144.El-Sayed MS, Ali N, El-Sayed Ali Z. Aggregation and activation of blood platelets in exercise and training. Sports Med. 2005;35(1):11–22. doi: 10.2165/00007256-200535010-00002. PubMed PMID: 15651910. [DOI] [PubMed] [Google Scholar]
- 145.Gresslien T, Agewall S. Troponin and exercise. Int J Cardiol. 2016;221:609–621. Epub 2016 Jun 28. doi: 10.1016/j.ijcard.2016.06.243. PubMed PMID: 27420587. [DOI] [PubMed] [Google Scholar]
- 146.Dergaa I, Chamari K, Zmijewski P, Ben Saad H. From human writing to artificial intelligence generated text: examining the prospects and potential threats of ChatGPT in academic writing. Biol Sport. 2023;40(2):615–622. Epub 2023 Mar 15. doi: 10.5114/biolsport.2023.125623. PubMed PMID: 37077800; PubMed Central PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Dergaa I, Zakhama L, Dziri C, Saad HB. Enhancing scholarly discourse in the age of artificial intelligence: A guided approach to effective peer review process. Tunis Med 2023;101(10):721–6. [PMC free article] [PubMed] [Google Scholar]