Abstract
Background
The aim of this study is to assess the clinical effectiveness of the 3-step hand hygiene (HH) technique (3-HT) compared with the 6-step HH technique (6-HT; World Health Organization 6-step technique) using an alcohol-based hand rub.
Methods
A randomized controlled crossover trial was conducted from November to December 2023 in 10 wards of a tertiary A-level hospital according to CONSORT guidelines. The 240 healthcare workers (HCWs) were randomly divided into the 3-HT intervention group or the 6-HT control group. The trial was conducted in 2 stages, and the effectiveness of each indicator in the 2 groups was compared after a washout period of 2 weeks.
Results
Compared with the 6-HT, the 3-HT has demonstrated significant superiority in all indicators of HH compliance as well as the accuracy rate of HH practices. The total HH median times for the 3-HT and 6-HT were 16.00 (interquartile range, 15.00–20.00) and 32.50 (30.00–40.00) seconds, respectively (P < .05). The reduction factors for bacterial colony-forming unit counts did not differ and the colony-forming unit counts were not significantly different. Bacillus, Staphylococcus, and Micrococcus were detected before and after the use of hand rubs. HCWs preferred the 3-HT over the 6-HT. There were no significant difference in healthcare-associated infections rate between the 2 techniques.
Conclusions
The 3-HT was significantly superior to the 6-HT in terms of the HH eligibility rate, compliance, and HH time. The safety and feasibility of the 3-HT were verified by assessing microorganism count.
Keywords: compliance, hand hygiene, randomized cross-over trial, technique
According to data from the World Health Organization (WHO), healthcare-associated infections (HAIs) cause approximately 40 000 deaths per year, which translates to a prevalence of HAIs as high as 25% in developing countries and 5%–15% in developed countries [1, 2]. The average total hospital cost per patient with HAIs is $137 963 [3], resulting in huge losses to hospitals and patients. A consensus has been reached that hand hygiene (HH) is the best and most cost-effective measure to reduce the cross-transmission of pathogenic microorganisms in medical institutions, thereby reducing the accessibility of HAIs. Effective HH can reduce HAIs by 30% [4]. However, the overall HH compliance (HHC) remains unsatisfactory. The average HHC is reportedly 40% in high-income countries and <20% in low-income countries [5, 6].
One of the main reasons for the low HHC is the time factor. The current 6-step HH technique (6-HT) is recommended by the WHO to take 20–30 seconds [4]. However, a study in a Finnish hospital found that a quarter of healthcare workers (HCWs) washed their hands for only 13 seconds [7]. A study in a surgical ward found that the average HH time among nurses was 4.7–5.3 seconds [8]. One study showed that the HHC of HCWs in the emergency department was only 29%, and one of the influencing factors was lack of time due to too many patients [9]. HCWs in clinical settings are faced with ever-increasing numbers of emergencies, patients, and HH indications; therefore, it is difficult to balance completing the 6-HT with clinical diagnosis and treatment-related activities.
In recent years, many scholars have explored the use of simplified HH steps to improve HHC. Tschudin-Sutter et al [10] simplified the 6-HT into a 3-step HH technique (3-HT) through a cluster randomized trial and compared the differences in HHC, number of bacterial colonies cleared, and microbial assessment between the 2 techniques. They found that the 3-HT had higher HHC and the reduction factors for bacterial colony-forming unit (CFU) counts did not differ between techniques. Reilly et al [11] compared the difference between the 2 techniques in covering the hand area and reducing the number of bacterial colonies. Their results revealed that although the 6-HT could cover more hand area, it extended the HH time of HCWs, and the size of the covered area was not correlated with a greater reduction in bacterial load.
Previous studies have preliminarily verified the effect and feasibility of HH with the 3-HT; however, a more in-depth evaluation is lacking. Therefore, the current study aimed to comprehensively compare the application effects of the 6-HT and the 3-HT through indicators such as HH eligibility rate, HHC, accuracy, HH time, colony clearance rate, microbial detection rate, HCW preference, and HAI rate, thus providing evidence for the clinical application of the 3-HT.
METHODS
Trial Design
From November to December 2023, we performed a cross-controlled trial at the Zhongnan Hospital of Wuhan University—a 3300-bed tertiary hospital. Ten departments were randomly selected from the 46 clinical departments in the hospital. The 10 departments (high-risk departments: respiratory and critical care medicine, infectious diseases, cardiovascular surgery, thoracic surgery, geriatric medicine, transplantation medical center; medium-risk departments: hepatobiliary and pancreatic surgery, urology surgery, and colorectal and anal surgery; low-risk departments: gastroenterology [12–14]) were then randomly divided into either the intervention group (3-HT) or the control group (6-HT) at a 50% ratio.
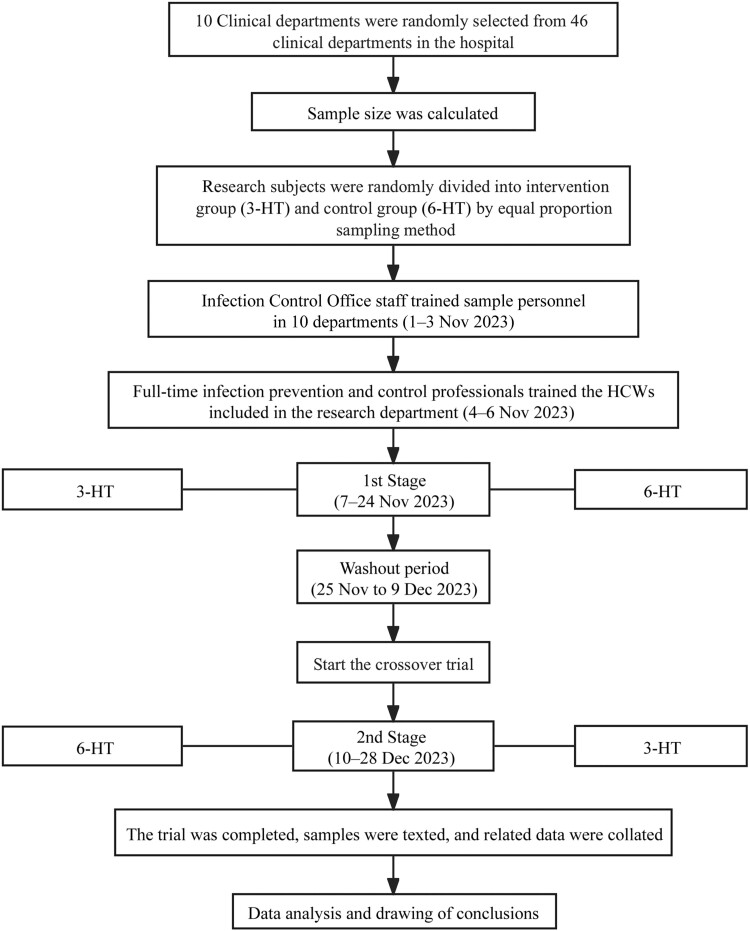
The HCWs in the study department were trained by full-time infection prevention and control professionals. After the end of the first stage, a 2-week washout period was observed, after which the 2 groups were switched to start the second-stage trial (Figure 1). This study was approved by the Clinical Research Ethics Committee of the Zhongnan Hospital of Wuhan University (approval no. 2023136K), and a waiver of informed consent was obtained. The study followed the CONSORT reporting guidelines.
Figure 1.
Randomized crossover trial procedure. Abbreviations: 3-HT, 3-step hand hygiene technique; 6-HT, 6-step hand hygiene technique; HCWs, healthcare workers.
Participants
The inclusion criteria were as follows: (1) HCW with working time ≥3 months, including internship, refresher, and regulated training; (2) skin of the hand not damaged during the study period; and (3) provision of informed consent. The exclusion criteria were (1) resignation; (2) hand skin inflammation or ulceration; and (3) allergy to alcohol-based hand rub (ABHR).
Intervention
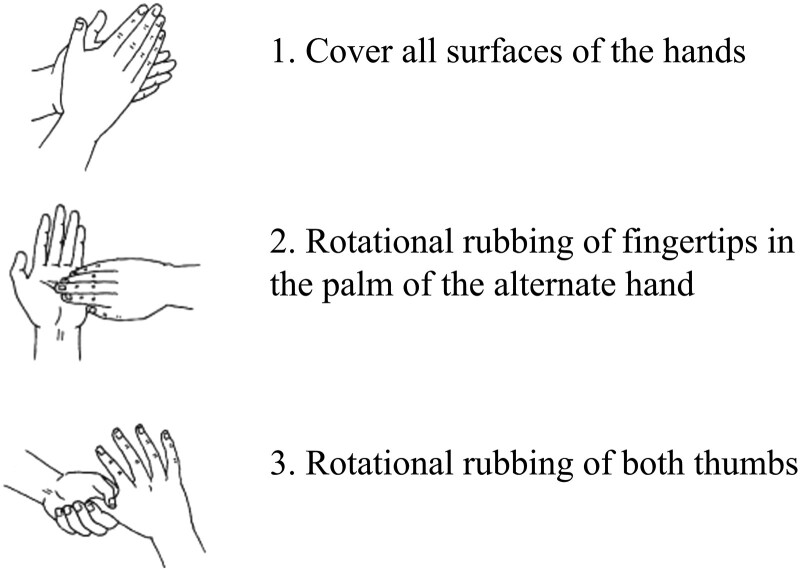
In the 3-HT group, the 3 steps in the technique consisted of (1) covering all surfaces of the hands (based on one's own judgment), (2) rotationally rubbing the fingertips on the palm of the alternate hand, and (3) rotationally rubbing both thumbs [15] (Figure 2). Our study used an ABHR provided by the hospital, produced by Shandong Lierkang Medical Technology. The main active ingredients and content were 80% ± 5% ethanol (vol/vol) and 1.3 ± 0.13 g/L hydrogen peroxide. The participants fully pressed the liquid extraction device twice to obtain a total of about 3.2 mL of the ABHR. After the HH is finished, the HCWs need to dry their hands for 1 minute. This 1-minute time is used to wait for the hands to dry and for the HH observation to be recorded [16, 17].
Figure 2.
Three-step hand hygiene technique.
Control
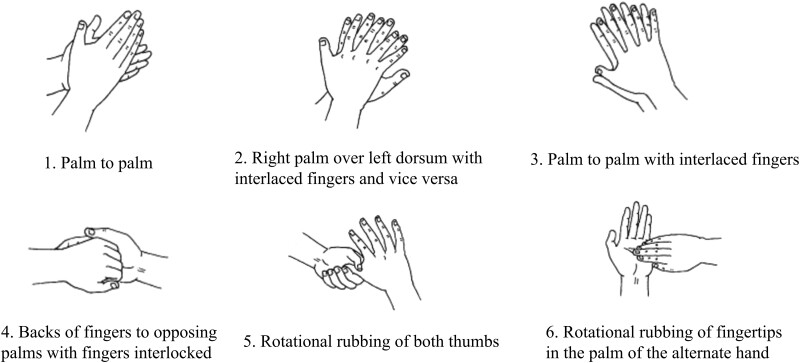
The HH technique of the control group was in accordance with the 6-HT, as recommended by the WHO (Figure 3) [18]. The control group also used the ABHR provided by the hospital and fully pressed the liquid device twice each time to obtain a total of about 3.2 mL of the ABHR. The steps after HH were consistent with those in the intervention group.
Figure 3.
Six-step hand hygiene technique.
Presampling Preparation and Sampling Procedure
The researcher responsible for sampling used a sterile eluent tube containing the appropriate neutralizer, sterile cotton swab, alcohol lamp, and light. The HH sampling process was as follows. First, the participants’ 5 fingers for both hands were placed together, and the researcher used a sterile cotton swab soaked with the neutralizer to rub the curved surface of the participant's fingers twice, from the root to the tip. The rubbing area of one hand was approximately 30 cm2, and the cotton swab was turned during the rubbing process. The part of the swab that was in contact with the researcher was cut off, and the remaining swab was placed into a 10-mL sterile test tube [16].
Microbiological Assessments
All samples were tested within 24 hours after sampling, oscillated with an oscillator for no less than 10 seconds, and thoroughly mixed. A total of 0.5 mL of the samples to be tested were absorbed with a sterile straw, added to a common nutrient agar plate, and incubated in a 36℃ ± 1℃ incubator for 48 hours for microbial count. The detected microbial samples were classified and sequenced for identification [19].
Total community genomic DNA extraction was performed using a E.Z.N.ATM MagBind Soil DNA Kit (Omega; M5635-02), following the manufacturer's instructions. Our target was the V3–V4 hypervariable region of the bacterial 16S ribosomal RNA gene. DNA extraction from polymerase chain reaction amplification fragments and Internal Transcribed Spacer product testing, sequencing, and sequence alignment are performed according to the instructions provided by DNA Extraction Kit. After sequencing, the effective tags were clustered into operational taxonomic units with a similarity threshold of ≥97% using Usearch software (version 11.0.667) [20], following the recommended pipeline and parameters. Microbial taxonomy annotation was performed using the latest RDP database at the genus level to ensure better validity and reliability.
Outcome
The main purpose of this study was to compare the HH eligibility rate, HHC, accuracy, HH time, colony clearance rate, microbial detection rate, HCW preference, and HAI rate between the 2 techniques.
HH Eligibility Rate
HH eligibility means that HH is considered qualified only when the number of bacterial colonies on the hands is ≤10 CFUs/cm2 after HH. HH eligibility rate is defined as the percentage of eligible hands with a bacterial count ≤10 CFUs/cm2 of the total hands sampled [19]. The eligibility rate was calculated using Equation 1:
| (1) |
HHC
HHC is calculated as the number of HH episodes performed per opportunities [21]. After the observed HCWs washed their hands, a researcher recorded the number of HH actions and the number of HH opportunities in an observation table. The extent of the HHC was calculated using Equation 2:
| (2) |
HH Accuracy Rate
The HH accuracy rate is a critical indicator, reflecting the extent to which HCWs meticulously follow the complete HH procedure with each HH action. It captures the percentage of times that the HH is performed in strict compliance with the standard steps. The HH accuracy rate was calculated using Equation 3:
| (3) |
HH Time
Whenever an HCW was ready to wash their hands, a researcher prepared a stopwatch and measured the total HH time. The time from the beginning of rubbing the ABHR to the completion of HH was recorded in seconds in an observation table.
Colony Clearance Rate
The extent of the colony clearance rate was calculated using Equation 4:
| (4) |
Microbial Detection Rate
Samples containing microorganisms were classified and sequenced to identify the microorganisms present in the hand samples of HCWs and their total frequencies among all hand samples. The extent of microbial detection was calculated using Equation 5:
| (5) |
HCW Preference Rates
After the observed HCWs in both groups used the 3-HT, the sample personnel orally asked which technique they preferred to use and recorded the results in an observation table. The HCW preference rate was calculated using Equations 6 and 7:
| (6) |
| (7) |
HAI Rates
A total of 240 observed HCWs were assigned to work in 10 departments, and there was no case of observed HCWs working in multiple departments during the study period. If the patient receives a diagnosis of as, it needs to be further reported in the information system. Subsequently, the infection prevention and control department will receive the reported information for verification and data registration.
In our study, the first stage of the study was conducted from 7 to 24 November 2023, and the second stage from 10 to 28 December 2023. Considering issues such as the incubation period, the data on HAI rate for the month of the study period in each department were queried using the Xinglin system of the Zhongnan Hospital of Wuhan University. The HAI rate was calculated using Equation 8:
| (8) |
Sample Size
Sample size was calculated using the formula applicable for randomized controlled trials [22] and is detailed in the Supplementary Materials.
Blinding
We implemented a blinding process for the team responsible for microbial culture and data analysis, thereby eliminating potential subjectivity in the analytical and data handling processes.
Statistical Analyses
We used χ2 and Fisher exact tests (where appropriate) to compare the proportions. To calculate the HH time and distribution of bacterial colonies, statistical differences were calculated using the Wilcoxon signed-rank test. Medians and interquartile ranges (IQRs) were used to describe the measurement data. Statistical significance was set at P < .05. Analyses were performed using SPSS software (SPSS version 16; SPSS).
RESULTS
HH Eligibility Rate of 2 Techniques
The eligibility rate for the 3-HT and the 6-HT were 95.83% (230 of 240) and 89.17% (214 of 240), respectively (P < .05). Observed HCWs were grouped according to sex, age, post, length of service, title, position, department, and different risk departments. Except for observed HCWs aged >55 years, the overall eligibility rate for HH with the 3-HT was higher than that with the 6-HT, but the difference was not statistically significant (P > .05). The eligibility rates for HH in the 2 techniques for HCWs aged 46–55 years old (100.00% vs 62.50%, respectively) and physicians (96.00% vs 84.00%) were significantly different. The eligibility rate for the 3-HT was significantly higher than that for the 6-HT (Table 1).
Table 1.
Eligibility Rates of Hand Hygiene With the 2 Techniques Used by Healthcare Workers
| Observed HCWs | Eligibility Rateb, No. Eligible/Total No. (%) | χ2 Value | P Valuea | |
|---|---|---|---|---|
| 3-HT (n = 240) | 6-HT (n = 240) | |||
| Sex | ||||
| Male | 45/49 (91.84) | 44/49 (89.80) | 0.069 | .79 |
| Female | 185/191 (96.86) | 170/191 (89.01) | ||
| Age, y | ||||
| <26 | 44/45 (97.78) | 43/45 (95.56) | 0.834 | .95 |
| 26–35 | 134/141 (95.04) | 124/141 (87.94) | ||
| 36–45 | 41/42 (97.62) | 38/42 (90.48) | ||
| 46–55 | 8/8 (100.00) | 5/8 (62.50) | ||
| >55 | 3/4 (75.00) | 4/4 (100.00) | ||
| Post | ||||
| Physician | 48/50 (96.00) | 42/50 (84.00) | 0.106 | .75 |
| Nurse | 182/190 (95.79) | 172/190 (90.53) | ||
| Length of service, y | ||||
| <5 | 73/75 (97.33) | 69/75 (92.00) | 0.094 | >.99 |
| 5–10 | 92/98 (93.88) | 85/98 (86.73) | ||
| 11–15 | 41/42 (97.62) | 38/42 (90.48) | ||
| 16–20 | 13/13 (100.00) | 11/13 (84.62) | ||
| >20 | 11/12 (91.67) | 11/12 (91.67) | ||
| Title | ||||
| Primary | 133/138 (96.38) | 126/138 (91.30) | 0.156 | .93 |
| Intermediate | 79/82 (96.34) | 70/82 (85.37) | ||
| Senior | 18/20 (90.00) | 18/20 (90.00) | ||
| Position | ||||
| Head nurse | 9/10 (90.00) | 9/10 (90.00) | 0.039 | .98 |
| Director | 5/5 (100.00) | 5/5 (100.00) | ||
| Other | 216/225 (96.00) | 200/225 (88.89) | ||
| Department | ||||
| Internal medicine | 99/104 (95.19) | 91/104 (87.50) | 0.012 | .91 |
| Surgery | 131/136 (96.32) | 123/136 (90.44) | ||
| Different risk departments | ||||
| High risk | 130/133 (97.74) | 123/133 (92.48) | 0.150 | .93 |
| Medium risk | 67/71 (94.37) | 63/71 (88.73) | ||
| Low risk | 33/36 (91.67) | 28/36 (77.78) | ||
Abbreviations: 3-HT, 3-step hand hygiene technique; 6-HT, 6-step hand hygiene technique; HCWs, healthcare workers.
aOverall P < .05 (based on χ2 test).
bHH eligibility rate is defined as the percentage of eligible hands with a bacterial count ≤10 Cfu/cm2 out of total hands sampled.
HHC With the 2 Techniques
Overall, 5720 HH indicators were observed in 240 HCWs. The HHC of observed HCWs using the 3-HT was 84.88% (2402 of 2830), and that of observed HCWs using the 6-HT was 76.85% (2221 of 2890; P < .05). There was a significant difference in the HHC between the 2 techniques with different lengths of service, position, departments, and different risk departments (P < .05). The HHC was significantly higher with the 3-HT than with the 6-HT for HCWs in the following categories: physicians, observed HCWs with 5–10 years of service, those with no position, and those in the surgery department or medium-risk departments; these differences were statistically significant (Table 2; P < .05).
Table 2.
Hand Hygiene Compliance With the 2 Techniques Used by Healthcare Workers
| Observed HCWs | HHC, No./Total (%) | 3-HT vs 6-HT | Intragroup Comparisonsa | |||
|---|---|---|---|---|---|---|
| 3-HT (n = 2830) | 6-HT (n = 2890) | χ2 Value | P Valueb | χ2 Value | P Valueb | |
| Sex | ||||||
| Male | 475/561 (84.67) | 439/606 (72.44) | 3.114 | .08 | 1.802 | .62 |
| Female | 1927/2269 (84.93) | 1782/2284 (78.02) | 3.673 | .055 | ||
| Age, y | ||||||
| <26 | 432/523 (82.60) | 456/563 (80.99) | 0.047 | .83 | 16.830 | .051 |
| 26–35 | 1442/1676 (86.04) | 1311/1694 (77.39) | 4.246 | .04 | ||
| 36–45 | 425/498 (85.34) | 346/484 (71.49) | 3.370 | .07 | ||
| 46–55 | 73/91 (80.22) | 81/103 (78.64) | 0.008 | .93 | ||
| >55 | 30/42 (71.43) | 27/46 (58.70) | 0.333 | .56 | ||
| Post | ||||||
| Physician | 459/560 (81.96) | 376/588 (63.95) | 7.413 | .006 | 3.705 | .054 |
| Nurse | 1943/2270 (85.59) | 1845/2320 (80.15) | 2.238 | .14 | ||
| Length of service | ||||||
| <5 | 719/863 (83.31) | 760/940 (80.85) | 0.183 | .67 | 25.914 | .002 |
| 5–10 | 989/1157 (85.48) | 824/1162 (70.91) | 8.845 | .003 | ||
| 11–15 | 458/524 (87.40) | 423/502 (84.26) | 0.159 | .71 | ||
| 16–20 | 134/157 (85.35) | 103/142 (72.54) | 0.866 | .35 | ||
| >20 | 102/129 (79.07) | 111/144 (77.08) | 0.019 | .89 | ||
| Title | ||||||
| Primary | 1404/1622 (86.56) | 1346/1693 (79.50) | 2.716 | .10 | 5.793 | .45 |
| Intermediate | 825/992 (83.17) | 761/1025 (74.24) | 2.856 | .09 | ||
| Senior | 173/216 (80.09) | 161/248 (64.92) | 2.138 | .14 | ||
| Position | ||||||
| Head nurse | 101/113 (89.38) | 95/116 (81.90) | 0.202 | .65 | 12.989 | .04 |
| Director | 38/46 (82.61) | 59/74 (79.73) | 0.016 | .90 | ||
| Other | 2263/2671 (84.72) | 2067/2700 (76.56) | 6.156 | .01 | ||
| Department | ||||||
| Internal medicine | 831/1176 (70.66) | 886/1163 (76.18) | 1.399 | .24 | 48.266 | <.001 |
| Surgery | 1571/1654 (94.98) | 1181/1537 (76.84) | 16.426 | <.001 | ||
| Different risk departments | ||||||
| High risk | 1171/1496 (78.28) | 1229/1616 (76.05) | 0.281 | .60 | 46.460 | <.001 |
| Medium risk | 846/878 (96.36) | 606/818 (74.08) | 13.323 | <.001 | ||
| Low risk | 385/456 (84.43) | 374/444 (84.23) | 0.001 | .98 | ||
Abbreviations: 3-HT, 3-step hand hygiene technique; 6-HT, 6-step hand hygiene technique; HCWs, healthcare workers; HHC, hand hygiene compliance.
aIntragroup comparisons for 3-HT and 6-HT.
bOverall P < .05 (based on χ2 test).
Accuracy Rates for the 2 Techniques
The accuracy rate of HH in the 3-HT group (98.06% [706 of 720]) was higher than that in the 6-HT group (88.47% [1274 of 1440]; P > .05). The observed HCWs were grouped according to sex, age, post, length of service, title, position, department, and different risk departments. It was found that the accuracy rate of HH in the 3-HT group was higher than that in the 6-HT group, but the difference was not significant (Table 3; P > .05).
Table 3.
Accuracy Rates of Hand Hygiene With the 2 Techniques Used by Healthcare Workers
| Observed HCWs | Accuracy Rateb, No./Total (%) | χ2 Value | P Valuea | |
|---|---|---|---|---|
| 3-HT (n = 720) | 6-HT (n = 1440) | |||
| Sex | ||||
| Male | 145/147 (98.64) | 252/294 (85.71) | 0.247 | .97 |
| Female | 561/573 (97.91) | 1022/1146 (89.18) | ||
| Age, y | ||||
| <26 | 133/135 (98.52) | 246/270 (91.11) | 1.034 | >.99 |
| 26–35 | 414/434 (95.39) | 752/846 (88.89) | ||
| 36–45 | 125/126 (99.21) | 220/252 (87.30) | ||
| 46–55 | 23/24 (95.83) | 39/48 (81.25) | ||
| >55 | 11/12 (91.67) | 17/24 (70.83) | ||
| Post | ||||
| Physician | 147/150 (98.00) | 233/300 (77.67) | 1.879 | .17 |
| Nurse | 559/570 (98.07) | 1041/1140 (91.32) | ||
| Length of service | ||||
| <5 | 221/225 (98.22) | 403/450 (89.56) | 1.312 | >.99 |
| 5–10 | 286/294 (97.28) | 504/588 (85.71) | ||
| 11–15 | 126/126 (100.00) | 239/252 (94.84) | ||
| 16–20 | 38/39 (97.44) | 69/78 (88.46) | ||
| >20 | 35/36 (97.22) | 59/72 (81.94) | ||
| Title | ||||
| Primary | 406/414 (98.07) | 744/828 (89.86) | 1.062 | .98 |
| Intermediate | 240/246 (97.56) | 435/492 (88.41) | ||
| Senior | 60/60 (100.00) | 95/120 (79.17) | ||
| Position | ||||
| Head nurse | 30/30 (100.00) | 49/60 (81.67) | 1.217 | .98 |
| Director | 15/15 (100.00) | 21/30 (70.00) | ||
| Other | 661/675 (97.93) | 1204/1350 (89.19) | ||
| Department | ||||
| Internal medicine | 304/312 (97.44) | 556/624 (89.10) | 0.067 | >.99 |
| Surgery | 402/408 (98.53) | 718/816 (87.99) | ||
| Different risk departments | ||||
| High risk | 387/399 (96.99) | 681/798 (85.34) | 2.405 | .88 |
| Medium risk | 211/213 (99.06) | 377/426 (88.50) | ||
| Low risk | 108/108 (100.00) | 216/216 (100.00) | ||
Abbreviations: 3-HT, 3-step hand hygiene technique; 6-HT, 6-step hand hygiene technique; HCWs, healthcare workers.
aOverall P > .05 (based on χ2 test).
bThe HH accuracy rate reflects the extent to which HCWs meticulously follow the complete HH procedure with each HH action.
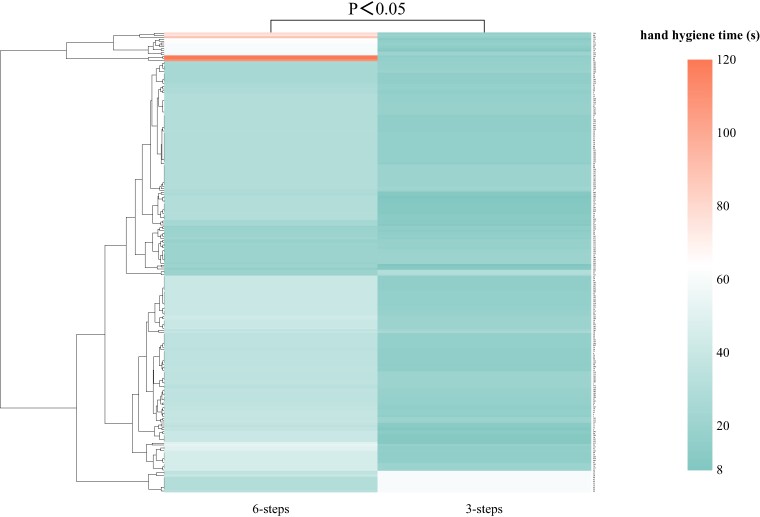
HH Times for the 2 Techniques
The median total HH time (IQR) was 16.00 (15.00–20.00) seconds for the 3-HT and 32.50 (30.00–40.00) seconds for the 6-HT (Table 4), and the difference was statistically significant. The cluster graph in Figure 4 is intended to show that the time of the 3-HT is significantly lower than that of the 6-HT (Figure 4; P < .05). The HH time of observed HCWs using the 3-HT was shorter than that using the 6-HT in different groups, except for the group aged >55 years, and the difference was significant (P < .05).
Table 4.
Hand Hygiene Time With the 2 Techniques Used by Healthcare Workers
| Observed HCWs | 3-HT(s) | 6-HT(s) | z Value | P Value |
|---|---|---|---|---|
| Total | 16.00 (15.00–20.00) | 32.50 (30.00–40.00) | −11.098 | <.001 |
| Sex | ||||
| Male | 16.00 (15.00–18.00) | 31.00 (30.00–37.50) | −5.588 | <.001 |
| Female | 16.00 (15.00–20.00) | 33.00 (30.00–40.00) | −9.632 | <.001 |
| Age, y | ||||
| <26 | 17.00 (15.00–20.00) | 30.00 (30.00–40.50) | −4.011 | <.001 |
| 26–35 | 16.00 (15.00–19.00) | 32.00 (30.00–40.00) | −8.335 | <.001 |
| 36–45 | 15.00 (11.50–20.00) | 35.00 (30.00–40.00) | −5.583 | <.001 |
| 46–55 | 16.00 (15.25–19.25) | 30.00 (22.50–34.50) | −2.392 | .02 |
| >55 | 18.00 (16.00–20.00) | 32.50 (30.00–38.75) | −1.841 | .07 |
| Post | ||||
| Physician | 16.00 (15.00–20.00) | 35.00 (30.00–38.00) | −5.480 | <.001 |
| Nurse | 16.00 (15.00–20.00) | 30.50 (30.00–40.00) | −9.676 | <.001 |
| Length of service | ||||
| <5 | 17.00 (15.00–20.00) | 30.00 (30.00–40.00) | −4.715 | <.001 |
| 5–10 | 16.00 (15.00–18.00) | 31.00 (30.00–38.50) | −8.167 | <.001 |
| 11–15 | 16.00 (15.00–20.00) | 35.00 (30.00–40.00) | −4.677 | <.001 |
| 16–20 | 16.00 (12.00–20.00) | 35.00 (30.00–38.50) | −3.062 | .002 |
| >20 | 16.00 (15.00–19.25) | 35.50 (30.00–40.00) | −2.981 | .003 |
| Title | ||||
| Primary | 16.00 (15.00–20.00) | 30.00 (30.00–40.00) | −7.723 | <.001 |
| Intermediate | 15.50 (15.00–18.00) | 35.00 (30.00–40.00) | −7.441 | <.001 |
| Senior | 16.50 (15.25–20.00) | 30.00 (30.00–35.75) | −3.062 | .002 |
| Position | ||||
| Head nurse | 15.50 (10.00–20.00) | 34.00 (27.50–40.00) | −2.689 | .007 |
| Director | 17.00 (15.50–19.00) | 30.00 (25.00–39.00) | −2.023 | .04 |
| Other | 16.00 (15.00–20.00) | 32.00 (30.00–40.00) | −10.643 | <.001 |
| Department | ||||
| Internal medicine | 17.00 (15.00–18.00) | 35.00 (30.00–40.00) | −8.616 | <.001 |
| Surgery | 16.00 (15.00–20.00) | 30.00 (30.00–37.75) | −7.108 | <.001 |
| Different risk departments | ||||
| High risk | 16.00 (15.00–16.00) | 30.00 (30.00–35.00) | −7.421 | <.001 |
| Medium risk | 15.00 (15.00–20.00) | 35.00 (29.00–38.00) | −7.167 | <.001 |
| Low risk | 18.00 (17.25–20.00) | 30.00 (25.00–35.00) | −5.016 | <.001 |
Abbreviations: 3-HT, 3-step hand hygiene technique; 6-HT, 6-step hand hygiene technique; HCWs, healthcare workers.
Figure 4.
Hand hygiene (HH) time cluster graph. Abbreviations: 3-HT, 3-step hand hygiene technique; 6-HT, 6-step hand hygiene technique.
Colony Clearance Rates of the 2 Techniques
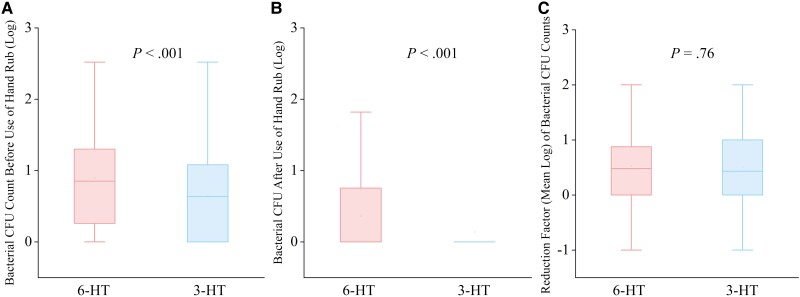
A comparison of the number of bacterial CFU counts before and after use of the hand rub, the reduction factors of the bacterial CFU counts, and the clearance rate for the 2 techniques showed that the bacterial CFU counts before and after use of the hand rub were smaller with the 3-HT than that with the 6-HT, and this difference was statistically significant (P < .05; Table 5). The median reduction factors of bacterial CFU counts (IQR) were 0.48 (0.00–0.88) log10 CFUs for the 3-HT and 0.43 (0.00–1.00) log10 CFUs for the 6-HT; this difference was not significant (P > .05; Figure 5).
Table 5.
Colony Clearance Rates in the 2 Techniques Used by Healthcare Workers
| Observed HCWs | 3-HT | 6-HT | z Value | P Valuea | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Bacterial colony-forming unit (CFU) counts (Log) | The reduction factor (RF) of CFU Counts (Log) | Clearance Rate,% | Bacterial colony-forming unit (CFU) counts (Log) | The reduction factor (RF) of CFU Counts (Log) | Clearance Rate, % | |||||
| Before Use of Hand Rub | After Use of Hand Rub | Before Use of Hand Rub | After Use of Hand Rub | |||||||
| Total | 0.85 (0.24–1.30) | 0.00 (0.00–0.77) | 0.48 (0.00–0.88) | 78.46 | 0.64 (0.00–1.08) | 0.00 (0.00–0.00) | 0.43 (0.00–1.00) | 59.22 | −0.300 | .76 |
| Sex | ||||||||||
| Male | 1.00 (0.40–1.43) | 0.00 (0.00–0.22) | 0.52 (0.13–1.26) | 79.08 | 1.12 (0.52–1.52) | 0.00 (0.00–0.71) | 0.60 (0.06–1.17) | 66.07 | −0.233 | .82 |
| Female | 0.52 (0.00–1.00) | 0.00 (0.00–0.00) | 0.30 (0.00–0.82) | 78.20 | 0.82 (0.22–1.22) | 0.00 (0.00–0.78) | 0.40 (0.00–0.82) | 56.85 | −0.574 | .57 |
| Age, y | ||||||||||
| <26 | 0.80 (0.06–1.10) | 0.00 (0.00–0.26) | 0.43 (0.00–0.88) | 72.03% | 0.73 (0.00–1.22) | 0.00 (0.00–0.82) | 0.30 (0.00–0.65) | 53.99% | −0.531 | .60 |
| 26–35 | 0.60 (0.00–1.00) | 0.00 (0.00–0.00) | 0.43 (0.00–1.00) | 79.01 | 0.97 (0.39–1.36) | 0.00 (0.00–0.70) | 0.52 (0.11–1.00) | 62.14 | −1.040 | .30 |
| 36–45 | 0.43 (0.00–0.87) | 0.00 (0.00–0.00) | 0.37 (0.00–0.82) | 82.61 | 0.92 (0.09–1.43) | 0.00 (0.00–0.82) | 0.30 (0.00–0.88) | 55.37 | −0.543 | .59 |
| 46–55 | 1.17 (0.78–1.50) | 0.00 (0.00–0.39) | 0.95 (0.24–1.50) | 83.25 | 0.93 (0.56–1.62) | 0.26 (0.00–1.35) | 0.54 (0.21–0.69) | 43.06 | −1.690 | .09 |
| >55 | 1.48 (0.36–2.27) | 0.00 (0.00–0.84) | 0.91 (0.08–2.27) | 79.44 | 0.80 (0.20–2.10) | 0.00 (0.00–0.75) | 0.80 (0.20–1.35) | 75.76 | −0.730 | .47 |
| Post | ||||||||||
| Physician | 1.00 (0.40–1.33) | 0.00 (0.00–0.00) | 0.82 (0.18–1.24) | 85.63 | 1.32 (0.63–1.75) | 0.11 (0.00–1.00) | 0.52 (0.12–1.05) | 57.80 | −0.879 | .38 |
| Nurse | 0.52 (0.00–1.00) | 0.00 (0.00–0.00) | 0.30 (0.00–0.82) | 75.46 | 0.82 (0.22–1.22) | 0.00 (0.00–0.65) | 0.39 (0.00–0.83) | 59.80 | −0.911 | .36 |
| Length of service, y | ||||||||||
| <5 | 0.82 (0.12–1.12)b | 0.00 (0.00–0.00) | 0.43 (0.00–1.00) | 78.18 | 0.82 (0.22–1.30) | 0.00 (0.00–0.82) | 0.48 (0.00–0.82) | 56.48 | −0.477 | .63 |
| 5–10 | 0.80 (0.12–1.12) | 0.00 (0.00–0.00) | 0.43 (0.00–1.00) | 77.73 | 0.99 (0.30–1.45) | 0.00 (0.00–0.82) | 0.50 (0.11–1.00) | 62.06 | −1.270 | .20 |
| 11–15 | 0.52 (0.00–1.00) | 0.00 (0.00–0.00) | 0.37 (0.00–0.70) | 78.23 | 0.94 (0.28–1.22) | 0.00 (0.00–0.65) | 0.48 (0.00–0.93) | 55.92 | −0.679 | .50 |
| 16–20 | 0.60 (0.37–0.97) | 0.00 (0.00–0.15) | 0.52 (0.06–0.82) | 100 | 0.30 (0.00–1.48) | 0.00 (0.00–0.71) | 0.24 (0.00–0.50) | 46.83 | −0.890 | .37 |
| >20 | 1.06 (0.00–1.43) | 0.00 (0.00–0.00) | 0.64 (0.00–1.38) | 83.38 | 0.73 (0.24–0.82) | 0.00 (0.00–0.00) | 0.54 (0.19–0.78) | 77.44 | −0.979 | .33 |
| Title | ||||||||||
| Primary | 0.72 (0.00–1.04) | 0.00 (0.00–0.00) | 0.39 (0.00–1.00) | 79.10 | 0.82 (0.22–1.30) | 0.00 (0.00–0.72) | 0.51 (0.00–0.86) | 61.50 | −0.111 | .91 |
| Intermediate | 0.64 (0.00–1.02) | 0.00 (0.00–0.00) | 0.45 (0.00–0.82) | 76.75 | 0.96 (0.30–1.30) | 0.00 (0.00–0.82) | 0.30 (0.00–0.91) | 53.16 | −0.463 | .64 |
| Senior | 0.6 (0.03–1.43) | 0.00 (0.00–0.00) | 0.48 (0.00–1.20) | 80.23 | 0.91 (0.13–1.52) | 0.00 (0.00–0.60) | 0.60 (0.08–0.98) | 69.38 | −0.087 | .93 |
| Position | ||||||||||
| Head nurse | 0.48 (0.09–0.82) | 0.00 (0.00–0.00) | 0.48 (0.00–0.82) | 75.40 | 0.60 (0.00–1.45) | 0.00 (0.00–0.54) | 0.30 (0.00–0.93) | 58.61 | −0.255 | .80 |
| Director | 0.00 (0.00–0.82) | 0.00 (0.00–0.00) | 0.00 (0.00–0.82) | 100.00 | 0.78 (0.00–1.17) | 0.00 (0.00–0.11) | 0.78 (-0.11–1.17) | 92.87 | −0.730 | .47 |
| Other | 0.70 (0.00–1.10) | 0.00 (0.00–0.00) | 0.43 (0.00–1.00) | 78.31 | 0.87 (0.30–1.30) | 0.00 (0.00–0.82) | 0.48 (0.03–0.88) | 58.73 | −0.163 | .87 |
| Department | ||||||||||
| Internal medicine | 0.60 (0.00–1.00) | 0.00 (0.00–0.00) | 0.32 (0.00–0.82) | 73.11 | 0.82 (0.30–1.22) | 0.00 (0.00–0.82) | 0.30 (0.00–0.82) | 51.95 | −0.128 | .90 |
| Surgery | 0.78 (0.00–1.12) | 0.00 (0.00–0.00) | 0.52 (0.00–1.06) | 81.92 | 0.97 (0.15–1.43) | 0.00 (0.00–0.70) | 0.52 (0.03–0.97) | 64.15 | −0.496 | .62 |
| Different risk departments | ||||||||||
| High risk | 0.43 (0.00–1.00) | 0.00 (0.00–0.00) | 0.30 (0.00–0.88) | 83.57 | 0.70 (0.00–1.22) | 0.00 (0.00–0.48) | 0.31 (0.00–0.82) | 64.27 | −0.274 | .78 |
| Medium risk | 0.82 (0.12–1.12) | 0.00 (0.00–0.00) | 0.52 (0.00–1.00) | 78.23 | 1.12 (0.52–1.52) | 0.22 (0.00–0.82) | 0.52 (0.12–1.00) | 61.83 | −0.843 | .40 |
| Low risk | 0.82 (0.60–1.12) | 0.00 (0.00–0.56) | 0.56 (0.15–0.82) | 66.62 | 1.02 (0.69–1.50) | 0.37 (0.00–1.00) | 0.41 (0.06–0.80) | 41.75 | −1.089 | .28 |
Abbreviations: 3-HT, 3-step hand hygiene technique; 6-HT, 6-step hand hygiene technique; CFU, colony-forming unit; HCWs, healthcare workers; RF, reduction factor.
aOverall P > .05 (based on χ2 test).
bThe medians and interquartile ranges (INR) were used to describe the CFU counts.
Figure 5.
Bacterial colony-forming unit (CFU) counts (Cfu·cm2) before (A) and after (B) use of hand rub and reduction factors (Cfu·cm2) of bacterial CFU counts (C) for both hand hygiene (HH) techniques. Abbreviations: 3-HT, 3-step hand hygiene technique; 6-HT, 6-step hand hygiene technique.
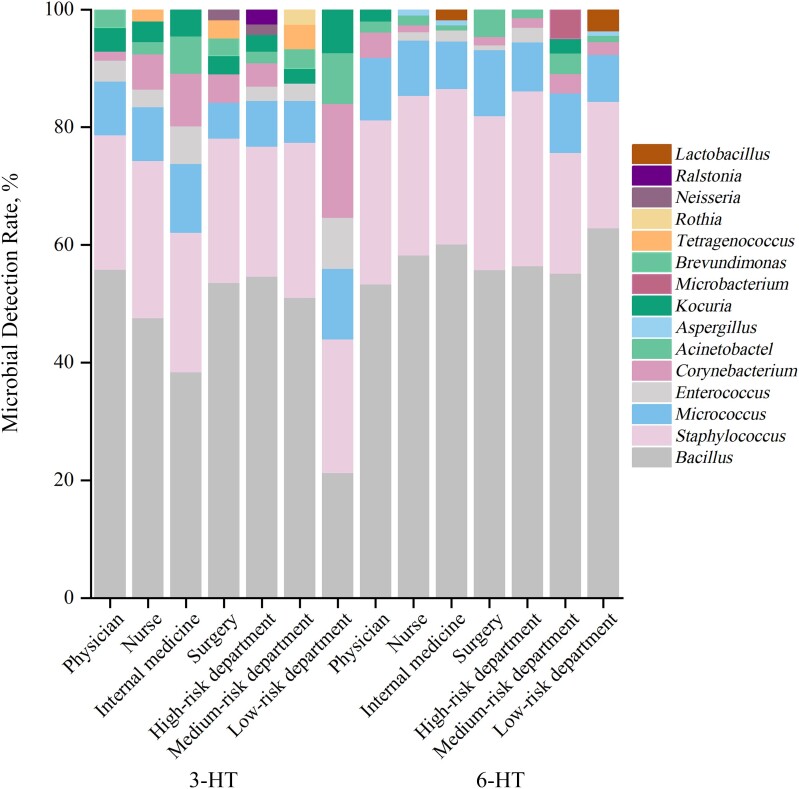
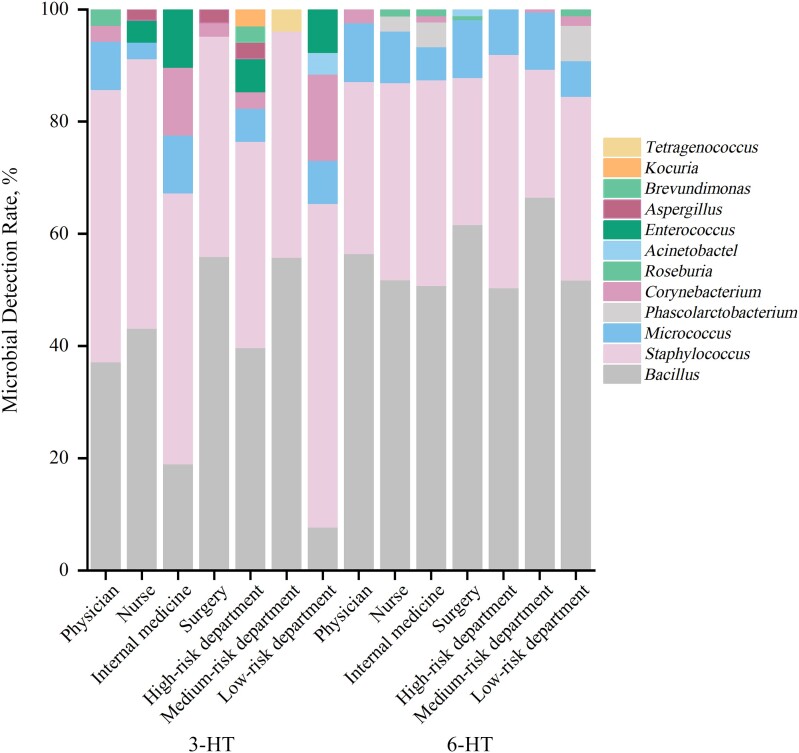
Microbial Detection Rates of 2 Techniques
A comparison of hand microbial samples from observed HCWs before HH showed that the hands of HCWs using the 2 techniques were mainly contaminated by Bacillus, Staphylococcus, and Micrococcus. The top 3 types of bacteria detected were gram-positive cocci/bacilli (Figure 6 and Table 6; P > .05). The top 3 microbes detected in the hands after HH with the 2 techniques were Bacillus, Staphylococcus, and Micrococcus, consistent with the findings of hand microbial detection before HH (Figure 7 and Table 6; P < .05). Bacillus, Staphylococcus, and Micrococcus are components of the normal skin flora [10].
Figure 6.
Top 3 bacterial species detected in the hand microbial samples from the 2 groups of healthcare workers before hand hygiene (HH). Abbreviations: 3-HT, 3-step HH technique; 6-HT, 6-step HH technique.
Table 6.
Top 3 Microbials Detected Before and After Hand Hygiene With the 2 Techniques
| Microbial Detected | Detection Rate Before HH, No./Total (%) | χ2 Value | P Value | Detection Rate After HH, No./Total (%) | χ2 Value | P Value | ||
|---|---|---|---|---|---|---|---|---|
| 3-HT | 6-HT | 3-HT | 6-HT | |||||
| Bacillus | 1165/2423 (48.08) | 1796/3112 (57.71) | 3.870 | .14 | 173/425 (40.71) | 850/1530 (55.56) | 36.106 | <.001 |
| Staphylococcus | 591/2423 (24.39) | 808/3112 (25.96) | 188/425 (44.24) | 492/1530 (32.16) | ||||
| Micrococcus | 210/2423 (8.67) | 290/3112 (9.32) | 18/425 (4.24) | 132/1530 (8.63) | ||||
Abbreviations: 3-HT, 3-step HH technique; 6-HT, 6-step HH technique; HH, hand hygiene.
Figure 7.
Top 4 bacterial species detected in the hand microbial samples from the 2 groups of healthcare workers after hand hygiene (HH). Abbreviations: 3-HT, 3-step HH technique; 6-HT, 6-step HH technique.
HCWs’ Preferences Between the 2 Techniques
Except for low-risk departments, more observed HCWs (66.67%) chose the 3-HT than the 6-HT (33.33%). The same conclusion was reached on further grouping, indicating that observed HCWs preferred the 3-HT over the 6-HT (Table 7).
Table 7.
Hand Hygiene Preference in 2 Groups of Healthcare Workers
| Observed HCWs | 3-HT | 6-HT | ||
|---|---|---|---|---|
| HCWs, No. | Preference, % | HCWs, No. | Preference, % | |
| Total | 160 | 66.67 | 80 | 33.33 |
| Sex | ||||
| Male | 34 | 69.39 | 15 | 30.61 |
| Female | 126 | 65.97 | 65 | 34.03 |
| Age, y | ||||
| <26 | 30 | 66.67 | 15 | 33.33 |
| 26–35 | 90 | 63.83 | 51 | 36.17 |
| 36–45 | 32 | 76.19 | 10 | 23.81 |
| 46–55 | 5 | 62.50 | 3 | 37.50 |
| >56 | 3 | 75.00 | 1 | 25.00 |
| Post | ||||
| Physician | 32 | 64.00 | 18 | 36.00 |
| Nurse | 128 | 67.37 | 62 | 32.63 |
| Length of service, y | ||||
| <5 | 46 | 61.33 | 29 | 38.67 |
| 5–10 | 69 | 70.41 | 29 | 29.59 |
| 11–15 | 28 | 66.67 | 14 | 33.33 |
| 16–20 | 9 | 69.23 | 4 | 30.77 |
| >20 | 149 | 66.82 | 74 | 33.18 |
| Title | ||||
| Primary | 89 | 64.49 | 49 | 35.51 |
| Intermediate | 55 | 67.07 | 27 | 32.93 |
| Senior | 16 | 80.00 | 4 | 20.00 |
| Position | ||||
| Head nurse | 7 | 70.00 | 3 | 30.00 |
| Director | 3 | 60.00 | 2 | 40.00 |
| Other | 150 | 66.67 | 75 | 33.33 |
| Department | ||||
| Internal medicine | 64 | 61.54 | 40 | 38.46 |
| Surgery | 96 | 70.59 | 40 | 29.41 |
| Different risk departments | ||||
| High risk | 105 | 78.95 | 28 | 21.05 |
| Medium risk | 49 | 69.01 | 22 | 30.99 |
| Low risk | 6 | 16.67 | 30 | 83.33 |
Abbreviations: 3-HT, 3-step hand hygiene technique; 6-HT, 6-step hand hygiene technique; HCWs, healthcare workers.
HAI Rates for the 2 Techniques
During the study period, we monitored the HAI rates in all departments, and the results showed no significant differences in HAI rate between the 2 groups (P > .05; Table 8).
Table 8.
Comparison of Healthcare-Associated Infection Rates Between the 2 Groups
| Observed HCWs by Department | 3-HT Group | 6-HT Group | P Value | ||||
|---|---|---|---|---|---|---|---|
| New Infections in the Same Period, No. | Hospitalized Patients, Total No. | HAI Rate, % | New Infections in the Same Period, No. | Hospitalized Patients, Total No. | HAI Rate,% | ||
| Pulmonary and critical care medicine | 12 | 173 | 1.68 | 10 | 333 | 1.58 | .05 |
| Infectious diseases | 2 | 398 | 0.50 | 5 | 203 | 2.46 | .05 |
| Cardiovascular surgery | 34 | 568 | 6.69 | 40 | 558 | 7.17 | .45 |
| Thoracic surgery | 11 | 302 | 3.64 | 15 | 319 | 4.70 | .53 |
| Geriatric medicine | 2 | 232 | 0.86 | 9 | 233 | 3.86 | .06 |
| Transplantation medical center | 13 | 307 | 4.23 | 14 | 238 | 5.88 | .40 |
| Hepatobiliary and pancreatic Surgery | 7 | 513 | 1.36 | 9 | 586 | 1.54 | .82 |
| Urology surgery | 7 | 714 | 0.98 | 13 | 699 | 1.86 | .17 |
| Colorectal and anal surgery | 3 | 470 | 0.64 | 8 | 506 | 1.58 | .23 |
| Gastroenterology | 6 | 1742 | 0.34 | 6 | 1886 | 0.32 | .89 |
Abbreviations: 3-HT, 3-step hand hygiene technique; 6-HT, 6-step hand hygiene technique; HAI, healthcare-associated infection; HCWs, healthcare workers.
DISCUSSION
The WHO Hand Hygiene Research Agenda for 2023–2030 underscores the need to advance HH research and emphasizes the importance of HH over the next 2 decades. HHC is widely recognized as a highly challenging task. While HCWs are required to develop HH habits, adequate time to perform HH correctly is an important factor. In this study, the clinical application effects of the 6-HT and the 3-HT were comprehensively compared through HH eligibility rate, HHC, accuracy, HH time, colony clearance rate, microbial detection rate, HCW preference, and HAI rate, and the findings revealed that the application effects of the 3-HT outperformed the 6-HT in terms of HH eligibility rate, HHC, and HH time.
In terms of the HH eligibility rate, except for observed HCWs aged >55 years, the eligibility rate for the 3-HT was generally higher than that for the 6-HT. The HH eligibility rate of physicians using the 3-HT was 96.00%, significantly higher than that using the 6-HT (84.00%) in all groups. One study reported that triage services had an overall eligibility rate of 86.70% for 6-HT [23]. We speculate that the 6-HT is complicated and difficult for physicians to complete when there are many patients and HH indicators, resulting in a poor HH effect. The 3-HT saves HH time and compliance is higher; therefore, the HH eligibility rate is better.
The current study found that, except for observed HCWs in internal medicine, compliance with the 3-HT was higher than with the 6-HT. Likewise, Tschudin-Sutter et al [10] randomly divided 12 wards in the hospital into 3-HT and 6-HT and found that the HHC in the wards using the 3-HT was 75.9% (1151 of 1516), compared with 65.0% (915 of 1407) in the wards using the 6-HT. Jiang et al [24] randomly assigned 4 departments to the study group and the control group and found that the HHC was 69.68% for the 3-HT and 52.45% for the 6-HT. HH is a high-frequency action faced by HCWs, and a more concise and simplified HH technique is beneficial for daily implementation by HCWs, especially in medical scenarios, such as intensive care units and emergency departments, where HH opportunities are more frequent [9]. A concise HH technology is needed to ensure the safety of the diagnostic and treatment processes and reduce the burden of HH for HCWs.
Furthermore, in terms of the accuracy rate for HH, the 3-HT offers certain advantages due to its fewer steps, ease of operation, strong operability, and low memory load. These attributes directly contribute to its higher accuracy rate. Jiang et al [24] found that the accuracy rate of HH with the 3-HT was 74.20%, higher than that with the 6-HT (57.38%). The accuracy rate of HH among the physicians was 56.26% for the 3-HT, higher than that for the 6-HT (44.85%).
In terms of HH time, one study has shown that the optimal duration of HH with the ABHR to ensure adequate hand decontamination is ≥15 seconds [25, 26], and our study found that the average time of HH with the 3-HT was 16 seconds, which met the requirements of the ABHR. Reilly et al [11] found that the 6-HT usually took a longer time (42.5 seconds), while the 3-HT took 35.0 seconds and the 6-HT took 15% longer. Chow et al [27] found that the HH time of the 3-HT was 26 seconds, which was less than the 38.5 seconds for the 6-HT. Therefore, within the time that the ABHR can be applied, a shorter HH technique should be considered to reduce the burden on HCWs, save time, and improve clinical efficiency.
In terms of the comparison of colony clearance rate, this study found no significant differences between the 2 techniques in terms of the efficacy of killing microorganisms. Consistent with the findings of the current study, an Austrian study of 20 volunteers found that the 3-HT at 15 seconds was no less effective at reducing the number of bacteria on the hands than the 3-HT at 30 seconds [15]. An experimental study showed that the average bacterial count for the 3-HT had a significant logarithmic decline (median [IQR], 4.45 [4.04–5.15] log10 CFUs), even higher than that for the 6-HT [(3.91 [3.69–4.62] log10 CFUs; P = .02)] [15]. Another study, which observed 2923 HH moments in >20 hospital wards, found that the HHC of the 3-HT is higher than that of the 6-HT, with no difference in bacterial count reduction factors between the 2 techniques [10]. Both techniques have been shown to be equally effective in reducing the number of microbes, but the 3-HT is easier to remember and generalize [10, 11, 28].
Similar to this study, when comparing the 2 HH techniques, Tschudin-Sutter et al [10] identified coagulase-negative Staphylococcus, Micrococcus, Corynebacterium spp, Bacillus spp, Staphylococcus aureus, and gram-negative bacteria, which is consistent with the results of Staphylococcus, Micrococcus, and Bacillus identified in our study. These 3 bacteria are common components of normal skin flora. In addition, a small number of potential pathogenic bacteria, such as Enterococcus, were also detected. Experiments have shown that hypochlorous acid solutions can significantly reduce contamination of the skin [29].
In addition, we sought to understand the preference of the 3-HT from the perspective of observed HCWs. More than half of the observed HCWs preferred the 3-HT, and an observational study at the University Hospital of Basel reported that the compliance rate of HCWs in performing HH was 93.2%, whereas compliance with the full 6-HT was only 8.5% [30]. Therefore, more observed HCWs prefer the 3-HT. We monitored the HAI rate in 10 departments during the study period and found no significant differences between the 2 groups, which verified the feasibility of the 3-HT.
Our study had several limitations. All the hand samples of observed HCWs sampled in this study were collected in a clinical but nonsurgical environment, such as after giving an injection, doing an electrocardiogram, and before and after contact with patients. There is still a gap in the comparison of the effects of the 2 HH techniques in other clinical environments, such as surgery. This may impede generalizability to other settings. In addition, the ABHR used in this study uses alcohol as the main component; therefore, this study represents only the use of an ABHR with alcohol as the main component, and the effects of other types of hand disinfectants are unknown.
In conclusion, compared with the 6-HT, the 3-HT has outstanding advantages in terms of HH eligibility rate, HHC, and HH time. This is particularly useful for physicians, surgeons, and HCWs in high-risk departments who are faced with multiple medical operations on a daily basis. The traditional 6-HT can be safely replaced with a 3-HT for a higher HHC. Future studies should further explore the efficacy of the 3-HT in surgical settings and with the use of other types of ABHRs.
Supplementary Material
Acknowledgments
Author contributions. B. F. and Y. W. designed the study and protocol development. Y. L. and X. Cheng were responsible for data collection. N. C. and W. H. were responsible for data analysis. N. C. and Y. W. wrote the manuscript, F. C., X. Chen., W. Z., Y. T., and W. W. critically revised the manuscript, and L. W. and F. Q. provided final approval for this version to be published. All authors agreed to be accountable for all aspects of the work, ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Financial support. This work was supported by the National Natural Science Foundation of China (grants 52178080 and 52408127); the National Institute of Hospital Administration Management of China (grant GY2023049); the Discipline Cultivation Fund (Nursing) of Zhongnan Hospital of Wuhan University (grant ZNXKPY2022005); the special fund for medicine and nursing technology and management of Zhongnan Hospital of Wuhan University (grant CXPY2023105); and the 2022–2023 Nursing Research project of Chinese Medical Journals Publishing House (grant CMAPH-NRI2022007).
Contributor Information
Nuo Chen, School of Public Health, Hubei University of Medicine, Shiyan, Hubei, China; Department of Healthcare-associated Infection Prevention and Control, Zhongnan Hospital of Wuhan University, Hubei, China.
Yan Li, Department of Healthcare-associated Infection Prevention and Control, Zhongnan Hospital of Wuhan University, Hubei, China.
Wenbin He, Nursing Department of Zhongnan Hospital of Wuhan University, Hubei, China.
Xiaoyan Chen, Nursing Department of Zhongnan Hospital of Wuhan University, Hubei, China.
Fan Cheng, Department of Healthcare-associated Infection Prevention and Control, Zhongnan Hospital of Wuhan University, Hubei, China.
Xiaolin Cheng, Department of Healthcare-associated Infection Prevention and Control, Zhongnan Hospital of Wuhan University, Hubei, China.
Weilong Zhou, Department of Infection Prevention and Control, West China Women's and Children's Hospital, Chengdu, China.
Yibin Tan, Department of Healthcare-associated Infection Prevention and Control, Zhongnan Hospital of Wuhan University, Hubei, China.
Wenwen Wu, School of Public Health, Hubei University of Medicine, Shiyan, Hubei, China; Sinopharm Dongfeng General Hospital (Hubei Clinical Research Center of Hypertension), Hubei University of Medicine, Shiyan, Hubei, China.
Lingling Wu, Department of Information, Zhongnan Hospital of Wuhan University, Hubei, China.
Fu Qiao, Infection Prevention and Control Department, West China Hospital, Sichuan University, Chengdu, China.
Bilong Feng, Nursing Department of Zhongnan Hospital of Wuhan University, Hubei, China; Hubei Engineering Center for Infectious Disease Prevention, Control and Treatment, Hubei, China.
Ying Wang, Department of Healthcare-associated Infection Prevention and Control, Zhongnan Hospital of Wuhan University, Hubei, China; Hubei Engineering Center for Infectious Disease Prevention, Control and Treatment, Hubei, China.
Supplementary Data
Supplementary materials are available at Open Forum Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
References
- 1. Larypoor M, Frsad S. Evaluation of nosocomial infections in one of hospitals of Qom, 2008. Iran J Med Microbiol Persian 2011; 5:7–17. [Google Scholar]
- 2. Olise CC, Simon-Oke IA. Fomites: possible vehicle of nosocomial infections. J Pub Health Catalog 2018; 1:16. [Google Scholar]
- 3. Shepard J, Frederick J, Wong F, Madison S, Tompkins L, Hadhazy E. Could the prevention of health care-associated infections increase hospital cost? The financial impact of health care-associated infections from a hospital management perspective. Am J Infect Control 2020; 48:255–60. [DOI] [PubMed] [Google Scholar]
- 4. World Health Organization . WHO guidelines for hand hygiene in health care. Geneva, Switzerland: World Health Organization, 2009. [Google Scholar]
- 5. Allegranzi B, Bagheri Nejad S, Combescure C, et al. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet 2011; 377:228–41. [DOI] [PubMed] [Google Scholar]
- 6. Erasmus V, Daha TJ, Brug H, et al. Systematic review of studies on compliance with hand hygiene guidelines in hospital care. Infect Control Hosp Epidemiol 2010; 31:283–94. [DOI] [PubMed] [Google Scholar]
- 7. Ojanperä H, Kanste OI, Syrjala H. Hand-hygiene compliance by hospital staff and incidence of health-care-associated infections, Finland. Bull World Health Organ 2020; 98:475–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gould D, Chamberlain A. The use of a ward-based educational teaching package to enhance nurses’ compliance with infection control procedures. J Clin Nurs 1997; 6:55–67. [DOI] [PubMed] [Google Scholar]
- 9. Muller MP, Carter E, Siddiqui N, Larson E. Hand hygiene compliance in an emergency department: the effect of crowding. Acad Emerg Med 2015; 22:1218–21. [DOI] [PubMed] [Google Scholar]
- 10. Tschudin-Sutter S, Sepulcri D, Dangel M, Ulrich A, Frei R, Widmer AF. Simplifying the World Health Organization protocol: 3 steps versus 6 steps for performance of hand hygiene in a cluster-randomized trial. Clin Infect Dis 2019; 69:614–20. [DOI] [PubMed] [Google Scholar]
- 11. Reilly JS, Price L, Lang S, et al. A pragmatic randomized controlled trial of 6-step vs 3-step hand hygiene technique in acute hospital care in the United Kingdom. Infect Control Hosp Epidemiol 2016; 37:661–6. [DOI] [PubMed] [Google Scholar]
- 12. Su X, Zong CX, Wang X, Sun XG, Lv FY, Sun L. Application of risk assessment system in classified management of healthcare-associated infection in different departments. Chin J Infect Control 2022; 21:844–52. [Google Scholar]
- 13. Peng C, Jiang BZ. Risk assessment in the management of healthcare-associated infection in primary care hospitals. Modern Nurse 2022; 21:844–52. [Google Scholar]
- 14. Gan YJ, Lu YY, Liang DY. Risk assessment on healthcare-associated infection in different clinical departments based on rank-sum ratio method. Chin J Infect Control 2018; 17:418–22. [Google Scholar]
- 15. Tschudin-Sutter S, Rotter ML, Frei R, et al. Simplifying the WHO ‘how to hand rub’ technique: three steps are as effective as six-results from an experimental randomized crossover trial. Clin Microbiol Infect 2017; 23:409.e1–e4. [DOI] [PubMed] [Google Scholar]
- 16. World Health Organization . WHO guidelines on hand hygiene in health care, first global patient safety challenge clean care is safer care. France: World Health Organization, 2009. [PubMed] [Google Scholar]
- 17. Suchomel M, Leslie RA, Parker AE, Macinga DR. How long is enough? Identification of product dry-time as a primary driver of alcohol-based hand rub efficacy. Antimicrob Resist Infect Control 2018; 7:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Specification of hand hygiene for healthcare workers WS/T 313-2019. Chin J Infect Control 2020; 19: 93–8. [Google Scholar]
- 19. People's Republic of China health industry standard. Standard for hand hygiene for healthcare workers in healthcare settings. WS/T 313-2009[S]. China, Ministry of Health of the People's Republic of China, 2009; 4.
- 20. Edgar RC. UPARSE: highly accurate OTU sequences from microbial amplicon reads. Nat Methods 2013; 10:996–8. [DOI] [PubMed] [Google Scholar]
- 21. Wang Y, Yang J, Qiao F, et al. Compared hand hygiene compliance among healthcare providers before and after the COVID-19 pandemic: a rapid review and meta-analysis. Am J Infect Control 2022; 50:563–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tam W, Lo K, Woo B. Reporting sample size calculations for randomized controlled trials published in nursing journals: a cross-sectional study. Int J Nurs Stud 2020; 102:103450. [DOI] [PubMed] [Google Scholar]
- 23. Chen J, Hope MA, Lin Z, et al. Interactions of oxide surfaces with water revealed with solid-state NMR spectroscopy. J Am Chem Soc 2020; 142:11173–82. [DOI] [PubMed] [Google Scholar]
- 24. Jiang DP, Li YX, Hui Y, Gu CW. The application effect of simplifying “three-step handwashing method” in general departments. J Med Inf 2021; 34:123–5, 136. [Google Scholar]
- 25. Vermeil T, Peters A, Kilpatrick C, Pires D, Allegranzi B, Pittet D. Hand hygiene in hospitals: anatomy of a revolution. J Hosp Infect 2019; 101:383–92. [DOI] [PubMed] [Google Scholar]
- 26. Pires D, Soule H, Bellissimo-Rodrigues F, Gayet-Ageron A, Pittet D. Hand hygiene with alcohol-based hand rub: how long is long enough? Infect Control Hosp Epidemiol 2017; 38:547–52. [DOI] [PubMed] [Google Scholar]
- 27. Chow A, Arah OA, Chan SP, et al. Alcohol handrubbing and chlorhexidine handwashing protocols for routine hospital practice: a randomized clinical trial of protocol efficacy and time effectiveness. Am J Infect Control 2012; 40:800–5. [DOI] [PubMed] [Google Scholar]
- 28. Pires D, Bellissimo-Rodrigues F, Soule H, Gayet-Ageron A, Pittet D. Revisiting the WHO “How to Handrub” hand hygiene technique: fingertips first? Infect Control Hosp Epidemiol 2017; 38:230–3. [DOI] [PubMed] [Google Scholar]
- 29. Nerandzic MM, Rackaityte E, Jury LA, Eckart K, Donskey CJ. Novel strategies for enhanced removal of persistent Bacillus anthracis surrogates and Clostridium difficile spores from skin. PLoS One 2013; 8:e68706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Tschudin-Sutter S, Sepulcri D, Dangel M, Schuhmacher H, Widmer AF. Compliance with the World Health Organization hand hygiene technique: a prospective observational study. Infect Control Hosp Epidemiol 2015; 36:482–3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.