Abstract
Background
Despite coalition resection being the preferred treatment for talocalcaneal coalition (TCC), postoperative complications, suboptimal functional recovery, and recurrence risks remain challenges. Although current TCC classification systems guide personalized surgical plans, the impact of middle and posterior facet coalitions on TCC resection surgery’s effectiveness is still poorly understood. Therefore, this study aims to compare the clinical outcomes of TCC patients with and without involvement of the subtalar joint’s (STJ) middle and posterior facets undergoing coalition resection to explore the potential impact of these coalitions on surgical outcomes.
Methods
We conducted a retrospective study on 115 patients who underwent coalition resection surgery due to symptomatic TCC between November 2009 and February 2023. According to preoperative CT scan results, patients were divided into an isolated posterior facet coalition (P-type) group and a middle-posterior facet coalition (MP-type) group. Demographic characteristics (including age, sex, body mass index (BMI), follow-up time, and medical history duration), pre-and postoperative assessments (including Visual Analog Scale (VAS), American Orthopaedic Foot & Ankle Society (AOFAS) score, Pain Interference (PI) and Physical Function (PF) scores from the Patient-Reported Outcomes Measurement Information System (PROMIS)), as well as postoperative self-assessment of efficacy (excellent, good, fair, poor) and hindfoot stiffness, were compared between the two groups. Postoperatively, TCC recurrence was evaluated through imaging follow-up examinations.
Results
69 patients meeting the inclusion criteria were included, with 30 patients in the P-type group and 39 in the MP-type group. There were no statistically significant differences between the two groups in demographic characteristics (P<0.05). There were also no statistically significant differences between the two groups in preoperative VAS score, AOFAS score, PI score, and PF score. However, postoperatively, there were statistically significant differences between the two groups in VAS score (1(1,1.5) vs. 2(1,2), P<0.01), AOFAS score (92.5(87,96.5) vs. 82(69.5,87), P<0.01), PI score (39(39,43) vs. 39(39,51), P = 0.014), PF score (73(61,73) vs. 55(51,73), P = 0.001), fair or poor outcome (4(13%) vs. 14(35.9%), P = 0.034), and hindfoot stiffness (3(10.3%) vs. 16(37.2%), P = 0.011). There was no statistically significant differences in the recurrence rate between the two groups postoperatively (0(0%) vs. 3(7.69%), P = 0.252).
Conclusion
Even with complete coalition resection during surgery and rehabilitation following standardized protocols, the surgical outcomes in MP-type TCC patients are still inferior to those in P-type patients.
Keywords: Talocalcaneal coalition, Coalition resection, Subtalar joint, Clinical outcome
Introduction
Talocalcaneal coalition (TCC) refers to foot congenital anomaly caused by the abnormal connection between two or more tarsal bones due to the failure of original mesenchymal differentiation and segmentation during foot development, a common cause of flatfoot in older children or adolescents [1, 2]. For younger patients with high physical activity demands and without widespread degenerative changes in the subtalar joint (STJ), it is recommended to consider surgical treatment after conservative treatment has failed.
Coalition resection is a recognized technique for treating TCC, including open and arthroscopic resections. Arthroscopic surgery has the advantage of smaller incisions and a lower incidence of complications when compared to open surgery. However, open surgery outperforms surgical field visibility, the extent of resection, and reduced risk of recurrence. Notably, arthroscopic and open surgeries share common issues, including postoperative irritation of nerves and tendons, scar adhesion, lower functional scores, and the risk of recurrence. Drawing on past research experience, we have implemented stringent selection controls for surgical indications, established reasonable resection boundaries, and used bone wax for postoperative filling. However, despite the potential of surgery to alleviate pain effectively, postoperative functional scores may still not meet the desired level. Existing studies suggest that this may be associated with an inability of the foot to regain a regular movement pattern following coalition resection or with peroneal spasm, as well as more severe degenerative changes of the STJ [3–5]. However, many potential risk factors remain to be further elucidated.
In 2010, Rozansky et al. introduced a classification method for the TCC, utilizing three-dimensional CT to precisely describe the location, size, nature, and direction of different bone bridges, which is extremely helpful for designing surgical plans [6]. Following Rozansky, Guo and colleagues proposed a new classification system that details the coalition conditions of STJ facets to provide more precise surgical planning guidance, highlighting isolated posterior facet coalition (P-type) and a middle-posterior facet coalition (MP-type) as the most common types in TCC [7]. Although these classification methods have significantly advanced treatment strategies, more empirical research still needs to be conducted on the relationship between coalition of the middle and posterior facets involvement and the outcomes of coalition resection surgery and this may be one of the reasons for suboptimal outcomes of coalition resection procedures. In light of this, our study is dedicated to investigating the potential impact of the MP-type coalition on the results of TCC resection surgery, aiming to improve foot and ankle surgeons’ ability to assess patients’ postoperative prognosis accurately.
Methods
Patients
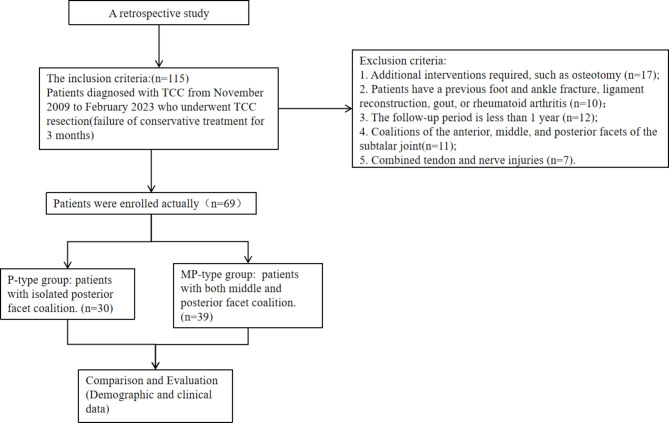
This study was approved by the ethical review of the First Affiliated Hospital of the Army Medical University ((B)KY2023064). We included patients who were diagnosed with TCC at our hospital between November 2009 and February 2023 and underwent TCC resection surgeries operated by the same surgical team. The inclusion and exclusion criteria, as well as details of the grouping, are presented in Fig. 1.
Fig. 1.
Research process diagram
Surgery method
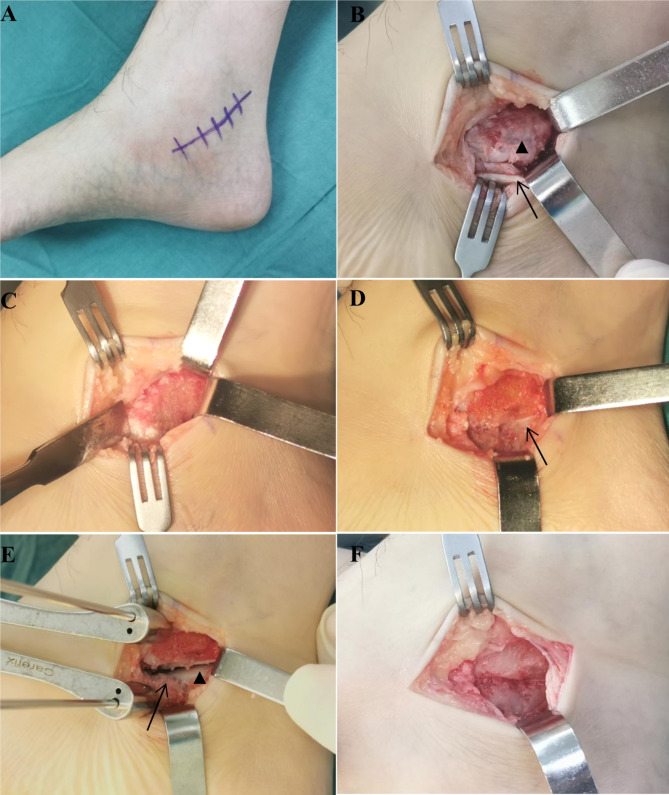
The anesthetic is general anesthesia or nerve-block anesthesia. A tourniquet was applied to the lower limb under a pressure of 40 kPa. Make an approximately 4 cm incision below the posterior tibial tendon (Fig. 2A). Cut through the skin and subcutaneous tissue to expose the flexor digitorum longus. Carefully pull the tendon proximally, being cautious not to damage the posterior tibial nerve. Open the joint capsule, expose the TCC, and reveal the coalition (Fig. 2B). Gently dissect the surrounding soft tissues and use the osteotome to make an osteotomy along the posterior aspect of the sustentaculum tali until the subtalar cartilage is visible (Fig. 2C-D). Then, a K-wire was placed in the sustentaculum tali, and other one was placed in the posterior aspect of the calcaneus. Use a Hintermann K-wire distractor to open the STJ (Fig. 2. E). With the K-wire as a reference, mobilize the calcaneus and assess the range of motion (ROM) of the STJ (Fig. 3A-B). Fill the osteotomy site with bone wax and insert a drainage tube (Fig. 2F). Finally, close the incision.
Fig. 2.
A. Diagram of the incision; B. The black arrows head indicate the TCC, while the black arrows represent the flexor digitorum longus; C. Use an osteotome to resection the TCC; D. Expose the articular cartilage of the subtalar joint (black arrows); E. Hintermann K-wire distractor to open the subtalar joint (black arrows head), sustentaculum tali (black arrow); F. Fill the osteotomy site with bone wax
Fig. 3.
Insert the K-wires parallel to each other into the calcaneus and talus (black arrow). A. When calcaneus is inversion, if the K-wires are parallel, the TCC has not been fully resected, or the joint remains adhered; B. If the K-wires intersect, the range of motion of STJ has been restored
Postoperative rehabilitation
To prevent recurrence, we have adopted a relatively aggressive rehabilitation approach. Specifically, on the first-day post-surgery, we encourage patients to engage in toe movements, dorsiflexion, and ankle joint plantarflexion. The drainage tube is removed when one of the following criteria is met: the drainage volume decreases to less than 10 milliliters or the time exceeds 48 h. Subsequently, we encourage patients to start crutch-assisted weight-bearing exercises, and most patients can reach this stage within 72 h post-surgery. Based on the patient’s tolerance to pain, we encourage full weight-bearing two weeks post-surgery and a gradual return to daily activities.
Demographic and clinical data evaluation
Patient preoperative medical history, operative reports, X-ray, and CT were reviewed to determine several information, including variables such as sex, age, Body Mass Index (BMI), follow-up time, and medical history duration, and the type of coalition, we meticulously reprocessed the preoperative CT data of two patient groups with the aid of Mimics Research 19.0 software to accurately determine the presence of coalition in the middle-posterior facets of the STJ. Postoperative follow-up data were primarily obtained from outpatient clinic records and telephone interviews. The recorded data includes patient self-assessment of surgical outcomes (categorized as excellent, good, fair, poor), as well as Pain Interference (PI) and Physical Function (PF) scores recorded using the Patient-Reported Outcomes Measurement Information System (PROMIS), Visual Analog Scale (VAS) scores, and evaluations based on the American Orthopedic Foot and Ankle Society (AOFAS) scoring system. It also includes recordings of whether patients experience noticeable hindfoot stiffness and pain when walking on uneven surfaces.
Imaging evaluation
Patients from each group underwent a foot X-ray in dorsoplantar and lateral images at various postoperative time points (one day, three months, six months post-surgery, and at the last follow-up). This was to assess the TCC resection condition and monitor for any recurrence. For patients suspected of having a recurrence of TTC or poor function, we will use 3D CT reconstruction for reassessment.
Statistical methods
The data were analyzed using IBM SPSS version 22.0 (IBM, Armonk, NY, USA). The Kolmogorov‒Smirnov test was used to confirm a normal distribution. The mean ± standard deviation represents data conforming to a normal distribution. The comparison between two groups of data was conducted using either a t-test or a t’ test. The nonnormally distributed measurement data are represented by M (Q1, Q3) or N(%) and were compared using the Mann-Whitney U test or Chi-square test (R × C contingency table).
Result
A total of 69 individuals met the inclusion criteria, with 30 in P-type group (12 males and 18 females) aged 22 (21.5, 28) years, BMI of 26.09 ± 3.62, medical history duration of 18 (6, 24) months, and follow-up time of 62.63 ± 44.35; and 39 in MP-type group (24 males and 15 females) aged 28.5 (21, 29) years, BMI of 25.16 ± 3.34, medical history duration of 12 (6, 78) months, and follow-up time of 61.54 ± 28.49. The two groups had no statistically significant differences regarding age, BMI, gender distribution, follow-up time, and medical history duration (P<0.05) (Table 1).
Table 1.
Demographic comparison between two groups
| Group | Number | Age (year) | Male sex(%) | BMI(kg/m2) | Medical history duration (months) | Follow-up time (months) |
|---|---|---|---|---|---|---|
| P-type group | 30 | 22(21.5,28) | 12(40%) | 26.09 ± 3.62 | 18(6,24) | 62.63 ± 44.35 |
| MP-type group | 39 | 28.5(21,29) | 24(61.54%) | 25.16 ± 3.34 | 12(6,78) | 61.54 ± 28.49 |
| Statistic value | -0.492 | 3.327 | 1.102 | -0.858 | 0.118 | |
| P | 0.623 | 0.076 | 0.274 | 0.391 | 0.907 |
The preoperative data of P-type group showed a VAS score of 3(2, 3), an AOFAS score of 76.70 ± 8.70, a PI score of 54.03 ± 3.79, and a PF score of 49(44, 53). MP-type group had a preoperative VAS score of 3(2, 4), an AOFAS score of 78.46 ± 5.83, a PI score of 53.92 ± 3.70, and a PF score of 50(46, 53). The two groups had no statistically significant differences in the preoperative data (Table 2).
Table 2.
Preoperative comparison of clinical data between two groups
| Group | VAS | AOFAS | PI | PF |
|---|---|---|---|---|
| P-type group | 3(2,3) | 76.70 ± 8.70 | 54.03 ± 3.79 | 49(44,53) |
| MP-type group | 3(2,4) | 78.46 ± 5.83 | 53.92 ± 3.70 | 50(46,53) |
| Statistic value | -0.3 | -0.956 | 0.121 | -1.536 |
| P | 0.764 | 0.344 | 0.904 | 0.125 |
All patients had good incision healing after surgery. In the MP-type group, 3 patients developed mild clinical symptoms of tibial nerve injury, such as weakened ankle inversion strength and reduced sensation in the plantar skin. We consider this to be caused by intraoperative traction, and the symptoms improved after one month of oral mecobalamin treatment.
In the postoperative clinical evaluation, P-type group had a VAS score of 1(1,1.5), AOFAS score of 92.5(87,96.5), PI score of 39(39,43), and PF score of 73(61,73); four cases (13%) of patients rated the postoperative efficacy as fair or poor; three cases (10.3%) reported stiffness or pain in the hindfoot when walking on uneven surfaces and there were no cases of recurrent conditions at the last follow-up. MP-type group had a VAS score of 2(1,2), AOFAS score of 82(69.5,87), PI score of 39(39,51), and PF score of 55(51,73); fourteen cases (35.9%) of patients rated the postoperative efficacy as fair or poor; sixteen patients (37.2%) reported stiffness or pain in the hindfoot when walking on uneven surfaces and there were three cases (7.69%) of recurrence at the last follow-up. The two groups had statistically significant differences regarding postoperative VAS, AOFAS, PI, PF scores, efficacy evaluation, and hindfoot stiffness. At the same time, there was no statistical significance in terms of recurrent joint conditions postoperatively (Table 3).
Table 3.
Postoperative comparison of clinical data between two groups
| Group | VAS | AOFAS | PI | PF | Fair or poor outcome |
Stiffness of hindfoot | Recurrence |
|---|---|---|---|---|---|---|---|
| P-type group | 1(1,1.5) | 92.5(87,96.5) | 39(39,43) | 73(61,73) | 4(13%) | 3(10.3%) | 0(0%) |
| MP-type group | 2(1,2) | 82(69.5,87) | 39(39,51) | 55(51,73) | 14(35.9%) | 16(37.2%) | 3(7.69%) |
| Statistic value | -3.575 | -4.318 | -2.46 | -3.169 | 4.477 | 6.435 | * |
| P | <0.01 | <0.01 | 0.014 | 0.001 | 0.034 | 0.011 | 0.252 |
*In SPSS, Fisher’s exact probability method does not provide the chi-square statistic.
Discussion
This study demonstrates that for patients with or without the involvement of the middle and posterior facet of the STJ in TCC, coalition resection surgery has achieved certain clinical outcomes. However, the clinical efficacy and improvement in STJ function were more pronounced in the P-type group. Moreover, there was no statistically significant differences in recurrence rates between the two groups at the last follow-up.
The present categorization of TCC mainly relies on the morphology and location of the coalition, with the most representative classification method being Rozansky’s classification [6]. However, this classification method does not consider the involvement of joint surfaces. Guo et al. expanded the classification of the joint facet coalition based on Rozansky’s classification, providing information on the location and orientation of TCC, which is more conducive to guiding surgery. In Guo’s study, it was found through CT three-dimensional reconstruction that P-type revealed the opening of the tarsal canal. In contrast, the MP-type did not show the tarsal canal opening [8]. It is worth noting that our study also discovered similar findings. Moreover, through analysis using Mimics software, We found that the coalition of MP-type can affect the internal structure of the tarsal canal, suggesting that simply removing the surface coalition of MP-type may not be thorough (Figs. 4 and 5). Extensive research indicates that the complex shape of the joint drives the normal function of the STJ, and alterations in the articular surfaces of the STJ can affect the axis of motion [9]. Bruckner stated that sustenteculum tali facet variations are clinically significant because they influence STJ stability [10]. Agarwal S found that the type of anterior-middle articular surface coalition was likely to lead to abnormal STJ activity, and the anterior, middle, and posterior articular surface separation was the optimal type of STJ function [11]. Mosca and Bevan reported that despite pain relief after coalition resection, the STJ continued to have a limited range of motion. In addition, kinematic and dynamic studies before and after surgery have shown that normal plantar pressure cannot be restored after surgery [12]. From a biomechanical perspective, in MP-type TCC, if the coalition within the tarsal canal cannot be completely cleared, it will still hinder the normal sliding and rotation of the STJ complex, resulting in degenerative joint disease, joint contracture, and hindfoot valgus deformity [13–15]. This condition is analogous to a car losing its independent suspension system and being unable to adapt to bumpy road surfaces [12, 15]. This may be the reason for the poor postoperative clinical outcomes and hindfoot stiffness in MP-type TCC patients. For patients with poor postoperative clinical outcomes, it is necessary to conduct a comprehensive evaluation of both overall and local conditions. In addition to assessing the overall situation of the rearfoot alignment and arch height, consideration should also be given to whether there is incomplete clearance of the coalition within the tarsal canal.
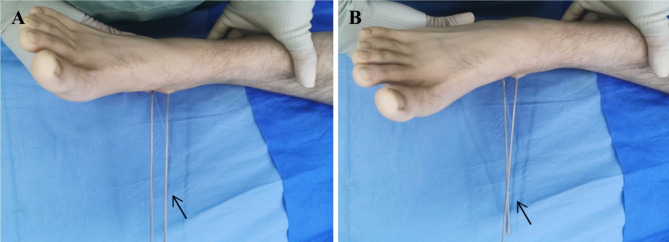
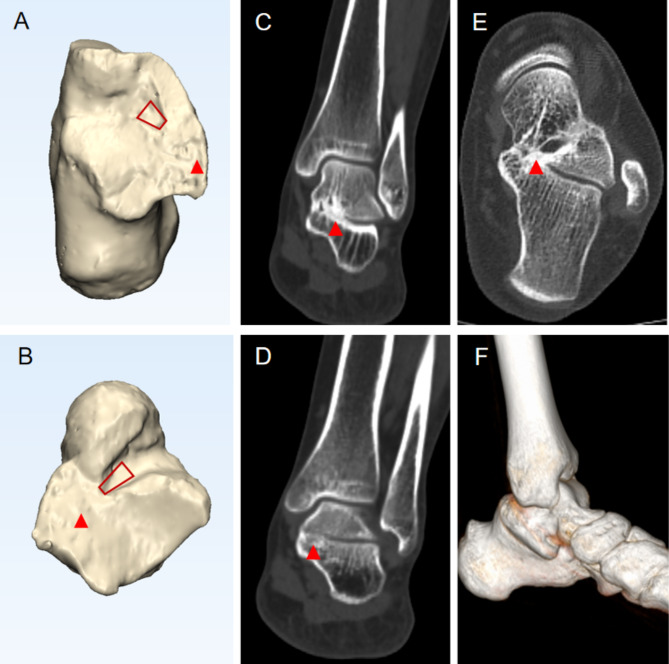
Fig. 4.
27-year-old male with a left foot MP-type TCC. The tubular structure of the tarsal canal is present, maintaining its rectangular morphology (red rectangle), but coalition is observed within the canal upon examination (red arrow head). A-B. Images after MIMICS processing; A. Aspect of calcaneus; B. Aspect of talus; C. The middle anterior part of the tarsal canal (partial disappearance); D. The middle posterior part of the tarsal canal (complete disappearance); E. CT horizontal plane suggesting bad morphology of the tarsal canal; F. CT three-dimensional reconstruction of MP-type TCC
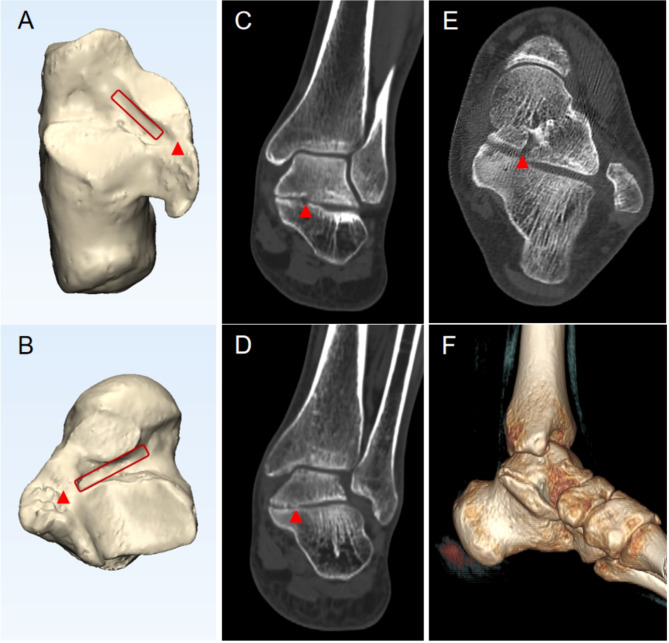
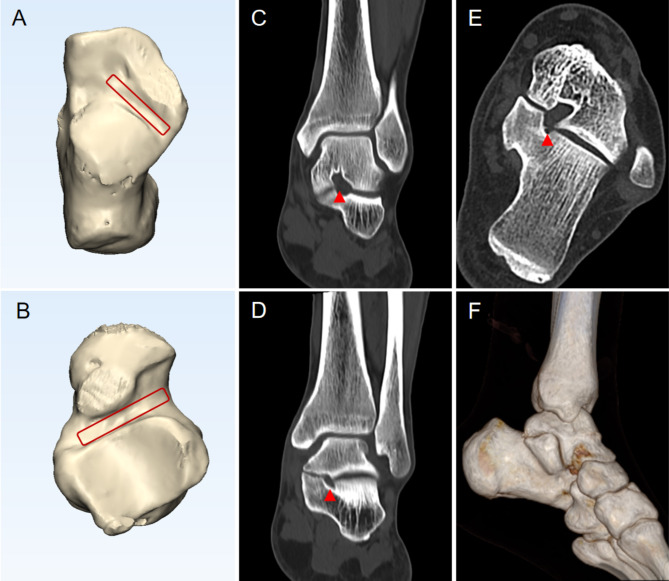
Fig. 5.
35-year-old male with a left foot MP-type TCC. The tubular structure of the tarsal canal disappears, presenting a trapezoidal shape (red trapezoid), with complete coalition of the lumen (red arrow head). A-B. Images after MIMICS processing; A. Aspect of calcaneus; B. Aspect of talus; C. The middle anterior part of the tarsal canal (disappearance); D. The middle posterior part of the tarsal canal (disappearance); E. CT horizontal plane suggesting bad morphology of the tarsal canal; F. CT three-dimensional reconstruction of MP-type TCC
We observed two exciting phenomena in the MP and P types of TCC: (1) a prevalent intra-articular coalition in the MP-type of TCC patients. In contrast, this phenomenon is rare in the P-type of TCC patients (Figs. 6). According to the research by J. Linklater [16], when TCC involves the middle STJ facets, the coalition typically affects the STJ internally. In contrast, an isolated coalition of the posterior STJ facets is rarely associated with internal STJ involvement. This phenomenon may be related to the enlargement of the middle STJ surface in TCC patients. Agarwal S and Garg R [11] noted that the morphology of the STJ facet is influenced by ethnicity and genetics, and indeed, a large STJ facet may result in excessive anterior and inferior rotation of the talus, leading to eversion of the calcaneus and downward tilt of the talar head; (2) Previous studies have shown that TCC typically occurs between the ages of 12 and 16, with symptoms often manifesting in adulthood, exhibiting a noticeable delay. Kevin E et al. [17]. found that, unlike adult TCC patients, adolescent TCC patients are relatively less likely to have calcaneal eversion and flatfoot, and their clinical symptoms are milder. Additionally, Alexander A. Dermanis [18] proposed that with increasing patient age, the coalition gradually ossifies, suggesting a correlation between age and the degree of coalition. Our research also observed this phenomenon, as although there was no statistically significant difference in age between the MP and P type group. In the MP -type group, elderly patients exhibited a more severe coalition within the tarsal canal (Figs. 4 and 5). Moreover, BMI may also be a key factor affecting postoperative outcomes. Although we found no statistically significant difference in BMI between the two groups in this study, it does not rule out the possibility that patients with higher BMI may have more severe degenerative joint changes and poorer execution of postoperative rehabilitation exercises. Although our study did not explicitly investigate the correlation between age, BMI, and the degree of coalition within the tarsal canal, these factors remain key considerations in the evaluation of postoperative outcomes.
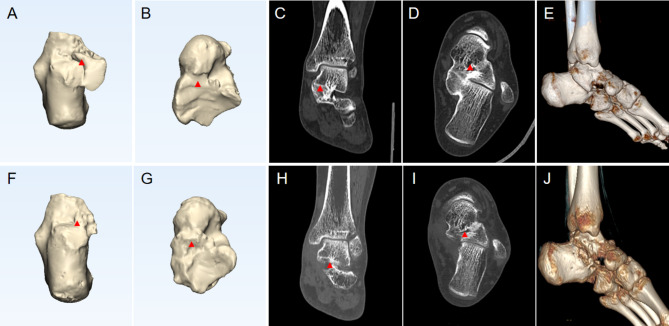
Fig. 6.
25-year-old male with a left foot P-type TCC. The tarsal canal maintains its tubular structure, presenting a rectangular morphology (red arrow head). A-B. Images after MIMICS processing; A. Aspect of calcaneus; B. Aspect of talus; C. The middle anterior part of the tarsal canal; D. The middle posterior part of the tarsal canal; E. CT horizontal plane suggesting good morphology of the tarsal canal; F. CT three-dimensional reconstruction of P-type TCC
TCC resection surgery is a widely recognized surgical approach for treating this condition; however, it is essential to acknowledge that there can be significant variation in surgical outcomes. Mahan et al. reviewed patients who underwent TCC resection and observed that 27% had a poor outcome [19]. Julian et al. evaluated 1284 patients with TCC resection, and 21% of patients had poor outcomes [20]. It has also been suggested that in order to minimize the recurrence rate in patients with TCC resection, tissue grafts or materials, such as extensor digitorum brevis (EDB) or fat graft, bone wax, and fibrin glue, should be tamponade at the resection site, as well as early active weight bearing to avoid re-fusion [21, 22]. Mubarak considered that it might be due to the failure to return to normal plantar pressure after TCC resection or improper selection of surgical methods [23]. In our study, bone wax filling was employed in all surgeries to ensure consistency in surgical procedures. In addition, for patients with MP-type TCC, we will appropriately extend the incision to the medial opening of the tarsal canal to expose the coalition fully. Furthermore, after coalition excision, we will use two parallel Kirschner wires to assess the mobility of the STJ (Fig. 3). However, follow-up assessments indicated that a vast majority of patients in the MP-type group still experienced hindfoot stiffness (Table 3; Fig. 7). Therefore, we suspect that the incomplete resection of the coalition within the tarsal canal is a crucial factor contributing to poor clinical outcomes, as it hinders the restoration of the original range of motion in the STJ.
Fig. 7.
25-year-old male with a left foot MP-type TCC. A-E. The preoperative Mimics and CT imaging data; F-J. The postoperative 12-month Mimics and CT imaging data. The red arrow indicates a coalition within the tarsal canal
It is important to note that our study has certain limitations. Firstly, regarding surgical techniques, we have yet to devise a method to clear the coalition within the tarsal canal completely. Secondly, although there was no statistically significant difference in postoperative coalition recurrence between the MP and P types, we attribute this to potentially insufficient sample size. Thus, further accumulation of clinical samples is necessary for validation. Lastly, the STJ, as a micro-movement joint, has a ROM that is not as easily measured as that of larger joints like the ankle or knee. Since the movement of the STJ involves three planes and is a complex motion, measuring it in a single plane is both inaccurate and challenging. Therefore, during surgery, we often use crossed Kirschner wires as a reference to assess the recovery of STJ mobility. However, this reference standard may lack sufficient persuasiveness in certain situations because it lacks more effective and objective indicators. Moreover, our study did not clearly evaluate whether the preoperative hindfoot alignment and the degree of joint degeneration were consistent between the two groups of patients, which constitutes a limitation of this study.
Conclusion
TCC treatment aims to restore sufficient recreational activities while simultaneously reducing foot load and torque to prevent degenerative changes in the subtalar and adjacent joints [18]. Theoretically, coalition resection can enhance the mobility of the hindfoot and midfoot joints and improve clinical symptoms in patients. However, in MP-type TCC, the effect of coalition resection alone is less effective compared to P-type TCC. This suggests that for MP-type TCC, it may be necessary to incorporate additional treatment methods to improve clinical outcomes for patients.
Acknowledgements
Not applicable.
Author contributions
Zhenyu Wang wrote the main manuscript text; Xiaoli Gou Fangcheng Yang and Yonghua Chen collected and analyzed data; Guo Zheng and Xu Tao reviewed the manuscript.
Funding
This work was supported by [Chongqing Science and Health Joint Medical Research Project (2023MSXM121)] and [Sports injury repair and reconstruction research innovation group (cstc2020jcyj-cxttX0004)].
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the First Affiliated Hospital of Army Medical University ((B)KY2023064).
Consent for publication
Written informed consent for publication was obtained from the participant.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xiaoli Gou, Fangcheng Yang, Yonghua Chen are co-first authors
Contributor Information
Xu Tao, Email: taoux@hotmail.com.
Guo Zheng, Email: zhenguo880501@tmmu.edu.cn.
References
- 1.Flynn JF, Wukich DK, Conti SF, Hasselman CT, Kline AJ. Subtalar coalitions in the adult. Foot Ankle Clin North Am. 2015;20(2):283–91. [DOI] [PubMed] [Google Scholar]
- 2.H W, Bohne. Tarsal coalition. Current opinion in pediatrics 2001. [DOI] [PubMed]
- 3.Varner KE, Michelson JD. Tarsal coalition in adults. Foot & ankle international / American Orthopaedic Foot and Ankle Society and Swiss. Foot Ankle Soc. 2000;21(8):669. [DOI] [PubMed] [Google Scholar]
- 4.Cass AD, Camasta CA. A review of Tarsal Coalition and Pes Planovalgus: clinical examination, Diagnostic Imaging, and Surgical Planning. J foot Ankle Surgery: Official Publication Am Coll Foot Ankle Surg. 2010;49(3):274–93. [DOI] [PubMed] [Google Scholar]
- 5.Brown RR, Rosenberg ZS, Thornhill BA. The C sign: more specific for flatfoot deformity than subtalar coalition. Skeletal Radiol. 2001;30(2):84–7. [DOI] [PubMed] [Google Scholar]
- 6.Rozansky A, Varley E, Moor M, Wenger DR, Mubarak SJ. A radiologic classification of talocalcaneal coalitions based on 3D reconstruction. J Childrens Orthop. 2010;4(2):129–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang A, Shi W, Gao L, Chen L, Xie X, Zhao F, et al. A new classification of talocalcaneal coalitions based on computed tomography for operative planning. BMC Musculoskelet Disord. 2021;22(1):678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang A, Shi W, Gao L, Chen L, Guo Q. A new classification of talocalcaneal coalitions based on computed tomography for operative planning. BMC Musculoskelet Disord 2021;22(1). [DOI] [PMC free article] [PubMed]
- 9.Zhang L, Peng X, He S, Zhou X, Yi G, Tang X et al. Association between subtalar articular surface typing and flat foot deformity: which type is more likely to cause flat foot deformity. BMC Musculoskeletal Disorders 2021(1). [DOI] [PMC free article] [PubMed]
- 10.Bruckner J. Variations in the human subtalar joint. J Orthop Sports Phys Therapy. 1987;8(10):489. [DOI] [PubMed] [Google Scholar]
- 11.Agarwal S, Garg S, Vasudeva N. Subtalar Joint Instability and Calcaneal Spurs Associated with the configuration of the articular facets of Adult Human Calcaneum in Indian Population. J Clin Diagn Res Jcdr. 2016;10(9):AC05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mosca VS, Bevan WP. Talocalcaneal tarsal coalitions and the calcaneal lengthening osteotomy: the role of deformity correction. J Bone Joint Surgery-american Volume. 2012;94(17):1584–94. [DOI] [PubMed] [Google Scholar]
- 13.Bhowmik AD, Ramakumaran VS, Dalal A. Tarsal-carpal coalition syndrome: report of a novel missense mutation in NOG gene and phenotypic delineation. Am J Med Genet Part A 2018;176(1). [DOI] [PubMed]
- 14.Jackson TJ, Larson AN, Mathew SE, Milbrandt TA. Incidence of Symptomatic Pediatric Tarsal Coalition in Olmsted County: A Population-Based Study. JBJS 2020;latest articles. [DOI] [PMC free article] [PubMed]
- 15.Leonard MA. The inheritance of tarsal coalition and its relationship to spastic flat foot. J Bone Join Surg B. 1974;56(3):520–6. [PubMed] [Google Scholar]
- 16.Linklater J, Hayter C, Vu D, Tse K. Anatomy of the subtalar joint and imaging of talo-calcaneal coalition. Skeletal Radiol. 2009;38(5):437–49. [DOI] [PubMed] [Google Scholar]
- 17.Varner K, Michelson J. Tarsal coalition in adults. Foot Ankle Int. 2000;21(8):669–72. [DOI] [PubMed] [Google Scholar]
- 18.Dermanis A, Elmajee M, Duffaydar H, Aljawadi A, Hussain S, Pillai A. Talocalcaneal Coalition Resection in the Adult Population. Syst Rev Cureus. 2022;14(10):e30581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mahan ST, Spencer SA, Vezeridis PS, Kasser JR. Patient-reported outcomes of tarsal coalitions treated with Surgical Excision. J Pediatr Orthop 2014;Publish Ahead of Print(6):583. [DOI] [PubMed]
- 20.Hollander J, Dusoswa Q, Dahmen J, Sullivan N, Kerkhoffs G, Stufkens S. 8 out of 10 patients do well after surgery for tarsal coalitions: a systematic review on 1284 coalitions. Foot Ankle Surgery: Official J Eur Soc Foot Ankle Surg. 2022;28(7):1110–9. [DOI] [PubMed] [Google Scholar]
- 21.Cowell HR. Tarsal coalition–review and update. Instr Course Lect. 1982;31(1):264. [PubMed] [Google Scholar]
- 22.Masquijo J, Allende V, Torres-Gomez A, Dobbs MB. Fat Graft and Bone Wax Interposition Provides Better Functional Outcomes and Lower Reossification Rates Than Extensor Digitorum Brevis after Calcaneonavicular Coalition Resection. J Pediatr Orthop. 2017;37(7):e427. [DOI] [PubMed] [Google Scholar]
- 23.Mubarak S, Patel P, Upasani V, Moor M, Wenger D. Calcaneonavicular coalition: treatment by excision and fat graft. J Pediatr Orthop. 2009;29(5):418–26. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.