Abstract
Background
The direct anterior approach (DAA) for total hip arthroplasty (THA) has gained popularity due to perceived advantages in achieving better early outcomes. However, the theoretical benefits such as precise implant positioning and accurate leg length restoration are still inconsistent. In this study, we compared implant position and leg length discrepancy (LLD) of the DAA and posterolateral approach (PLA) conducted by a single surgeon who had mastered both approaches.
Methods
This study retrospectively reviewed the medical records and radiographic images of 244 patients who underwent THA between 2012 and 2021 by a single experienced surgeon using either the DAA (n = 120) or PLA (n = 124). Postoperative pelvic anteroposterior radiographs at 6 months follow-up were used to assess acetabular component inclination and anteversion, as well as LLD. Mann-Whitney U tests and Chi-squared test were performed to compare outcomes between the two approaches.
Results
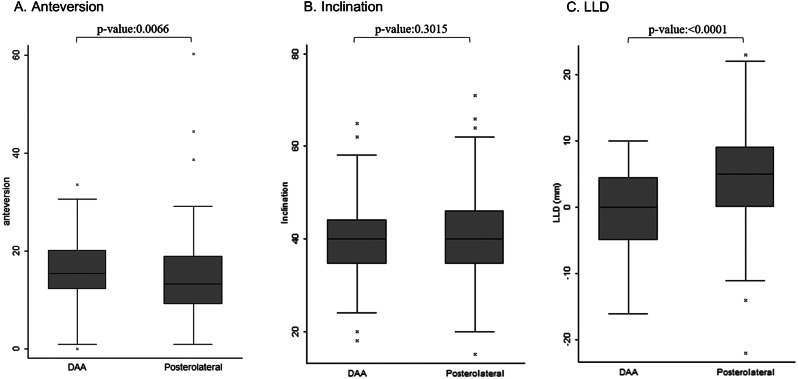
No significant differences were observed in patient demographics between the two groups. The DAA group demonstrated significantly lower postoperative LLD (0.00 mm) compared to the PLA group (5.00 mm, p < 0.0001). No significant difference was observed in the Lewinnek zone for cup anteversion and inclination angles between the two groups.
Conclusions
For experienced surgeons in other approaches, our findings suggest transferring to the DAA may not substantially improve cup positioning, but it might slightly enhance limb length measurement. For surgeons already proficient in other approaches and deciding to maintain those approaches, their primary concern for optimal THA outcome should be striving for leg length equivalence.
Keywords: Total hip arthroplasty, Direct anterior approach, Posterolateral approach, Acetabular position, Leg length discrepancy
Introduction
The historical context of total hip arthroplasty encompasses various surgical approaches. In recent decades, the DAA to THA has garnered significant attention, owing to its perceived advantages in achieving better early outcomes, precise implant positioning, and ergonomic leg length measurement. Numerous studies have emphasized the rapid recovery associated with DAA, attributing it to the muscle-sparing nature of the approach and the accuracy achieved in implant placement and leg length measurement through intraoperative fluoroscopy and comparison with the contralateral limb [1, 2]. A noteworthy trend has emerged in the United States, where a substantial percentage of surgeons have transitioned from employing different approaches to embracing the DAA [3].
While the benefits of expedited recovery have been extensively explored, comparative precision of implant positioning between the direct anterior approach and alternative methods was less thoroughly discovered. Theoretically, the DAA enhances precision in implant placement and leg length measurement due to the supine position that allows for intraoperative fluoroscopy. Studies even demonstrate that the freehand technique also demonstrate comparable implant positioning, irrespective of fluoroscopy utilization [4–6]. This raises the question: Does the DAA offer better prosthesis positioning and limb length measurement when performed by surgeons already experienced in alternative surgical approaches? Consequently, does a surgeon proficient in an alternative technique need to transition to the DAA to improve prosthesis positioning?
In this study, we seek to evaluate whether the advantages associated with the DAA extend beyond early recovery to encompass a statistically significant improvement in the precision of implant positioning. Our investigation will scrutinize the nuanced aspects of implant placement, including the cup inclination, anteversion and postoperative LLD, comparing the DAA with the PLA within the same surgeon cohort—a group with prior experience in both techniques.
Materials and methods
Patient population
This retrospective study reviewed the medical records and radiographic images of 244 patients who received total hip arthroplasty. All the patients underwent the operation at a single medical center between 2012 and 2021. The inclusion criteria were (1) patients older than 20-year-old, (2) patients receiving unilateral THR for hip osteoarthritis or osteonecrosis of femoral head, (3) follow-up duration greater than 6 months. The exclusion criteria were (1) patients receiving revision surgery, (2) patients with history of developmental dysplasia of the hip (3) patients with preoperative leg length discrepancy greater than 2 centimeters, (4) hip joint deformity related to malignancy, trauma or infection. This study was approved by the Ethics Committee and Institutional Review Board of Chi Mei Medical Center (No CE21228A).
Surgical procedures
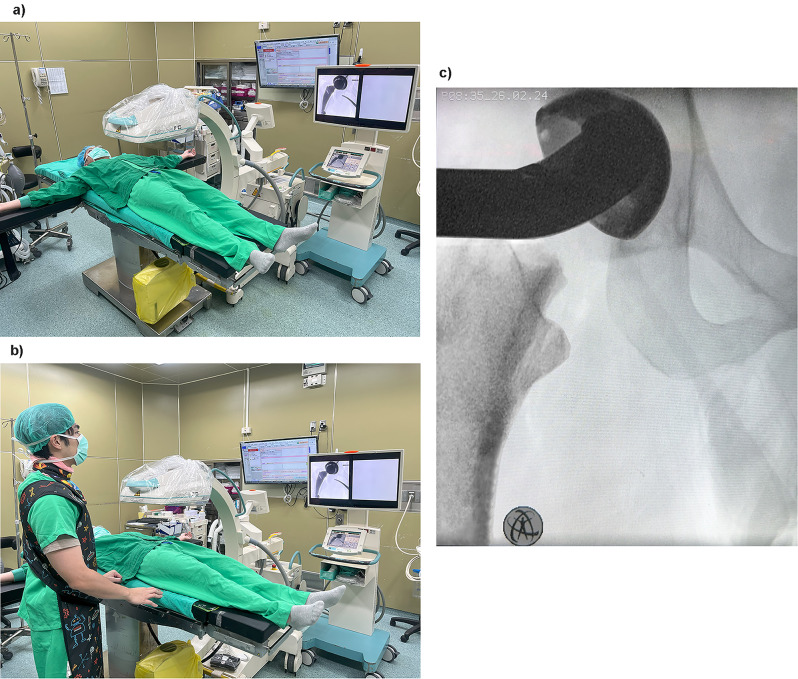
A single senior hip surgeon performed all total hip arthroplasty procedures, utilizing either a direct anterior approach or posterolateral approach. All the implants used in our study were Zimmer Kinetiv (Zimmer Biomet, Washington D.C., USA) implants. Before 2016, this surgeon used the posterolateral approach. After 2016, he switched to using the DAA approach. In the direct anterior group, patients were placed in a supine position (Fig. 1a, b). The preparation of the acetabulum component was completed under intraoperative fluoroscopic guidance (Fig. 1c). Once the surgeon was satisfied with the cup position, the acetabular component was impacted and secured with screws. Subsequently, the femoral canal was reamed, and a trial femoral component was inserted. Leg length discrepancy can be assessed by comparing both limbs due to the supine position or by measuring the bilateral trochanteric height difference under fluoroscopy. After determining the appropriate femoral stem size, the definitive femoral stem was inserted, and the hip joint was reduced. In the posterolateral approach group, patients were placed in a lateral decubitus position. Due to the overlapping of skeletal shadows, no fluoroscopy were taken in the posterolateral group during the study. Prosthesis positioning relied solely on the surgeon’s clinical judgement and experience without imaging guidance.
Fig. 1.
a., b. In the direct anterior group, patients were placed in a supine position. c. The preparation of the acetabulum component was completed under intraoperative fluoroscopic guidance
Radiological assessment
Postoperative pelvic anteroposterior radiographs at 6 months follow-up were utilized to assess acetabular component inclination and anteversion, as well as LLD after THA. We measured the LLD according to the lesser trochanter height difference between both hips (Fig. 2). We used the ellipse method to measure Liaw’s anteversion (Fig. 3). The radiographic anteversion angle is calculated as the arcsine of the ratio of the short axis to the long axis of the ellipse formed by the acetabular cup on an anteroposterior X-ray image [7]. The cup inclination was directly measured by the angle formed between the long axis of the cup and the horizontal line. To compare the accuracy of cup positioning in THA, we utilized Lewinnek’s safe zone. According to this standard, the cup should ideally be oriented at 40 ± 10 degrees of inclination and 15 ± 10 degrees of anteversion to enhance outcomes following THA [8].
Fig. 2.

A pelvis anterior-posterior radiograph demonstrates examples of LLD cup inclination measurement. Line A represents the interteardrop line. Line segment B signifies the distance between line A and the lower edge of the right lesser trochanter, while line segment C denotes the distance between line A and the lower edge of the left lesser trochanter. LLD is determined by the disparity in length between line segments B and C. Cup inclination is defined as the angle between line A and line D
Fig. 3.
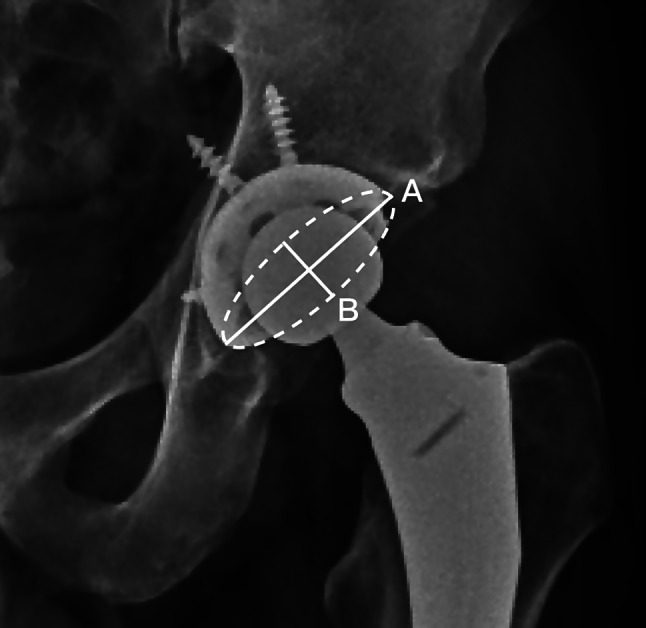
A pelvis anterior-posterior radiograph illustrates the application of the ellipse method for measuring Liaw’s anteversion. Angle β is defined as the angle between the major axis of the ellipse and the connection of the two endpoints (points A and B) of the major and minor axes. The calculation of cup anteversion is determined by the arc sine of the tangent of β
Data analyses
The descriptive statistic was used in this study. The categorical variables were presented as frequency with percentage and analyzed using Pearson’s chi-square test for comparing the difference between two groups. In addition, the Kolmogorov-Smirnov test was used to assess the normality of continuous variables. Since the continuous variables did not follow a normal distribution, they were expressed as the median and interquartile range (IQR). The difference in these continuous variables between two groups was compared using the Wilcoxon rank-sum test. Statistical analyses were performed using the IBM SPSS Statistics software package (version 24.0, IBM Corp, Armonk, NY, USA). Statistically significant was set as P-values less than 0.05.
Results
Demographics and characteristics of patients
From 2012 to 2021, a total of 244 patients underwent THA at our institution, performed by an experienced surgeon. Among them, 120 patients underwent the DAA, while 124 patients underwent the PLA. All patients in both groups achieved successful THA at their latest follow-up. The basic demographic data for both groups are presented in Table 1, showing no significant differences between the two groups.
Table 1.
Patient’s demographic data
| DAA group(n = 120) | Posterior group(n = 124) | P-value | |
|---|---|---|---|
| Age, median(Q1,Q3) | 65.00(59.00,71.00) | 61.00(52.00,73.00) | 0.0975 |
| Gender | 0.4631 | ||
| Male | 43(36.75) | 39(32.23) | |
| Female | 74(63.25) | 82(67.77) | |
| BMI, median(Q1,Q3) | 25.80(23.20,29.10) | 25.60(23.40,27.90) | 0.4083 |
Radiographic outcome
The radiographic data is summarized in Tables 2 and 3. Post-operative anteversion is 15.54 (12.27, 20.14) degrees in the DAA group and 13.35(9.11, 18.96) degrees in the PLA group (P value ≤ 0.01). In 85.8% of cases within the DAA group, the cup anteversion angle fell within the Lewinnek zone, compared to 81.5% in the PLA group (P = 0.355). Inclination of the cup is 40.00 (34.50, 44.00) degrees in the DAA group and 40.00 (34.50, 46.00) degrees in the PLA group (P value > 0.05). 80.8% of cases in the DAA group had the cup inclination angle within the Lewinnek zone, compared to 78.2% in the PLA group (P = 0.614). Notably, no significant difference was observed in cup anteversion and inclination angles within the Lewinnek safe zone between groups. The LLD after the operation is 0.00 (-5.00, 4.50) mm in the DAA group and 5.00 (0.00, 9.00) mm in the PLA group, with significant difference (P value ≤ 0.0001).
Table 2.
The box plot
Table 3.
Lewinnek safe zone
| overall (n = 244) |
DAA group (n = 120) |
Posterior lateral group (n = 124) |
P-value* | |
|---|---|---|---|---|
| Anteversion, n(%) | 0.3553 | |||
| in zone(5–25 degrees) | 204(83.61) | 103(85.83) | 101(81.45) | |
| out of zone | 40(16.39) | 17(14.17) | 23(18.55) | |
| Inclination, n(%) | 0.6139 | |||
| in zone(30–50 degrees) | 194(79.51) | 97(80.83) | 97(78.23) | |
| out of zone | 50(20.49) | 23(19.17) | 27(21.77) |
*Chi-Squared Test
Discussion
A key technical advantage of the DAA is its performance with the patient in a supine position. This positioning facilitates convenient access for fluoroscopy, potentially minimizing component placement errors and aiding in the optimization of hip biomechanics during THA [9, 10]. Fluoroscopy, however, comes with certain drawbacks. It can extend operative time due to image acquisition and raises concerns about potential contamination of the fluoroscopy arm’s sterile covering during surgery [11, 12]. Moreover, if not used correctly, fluoroscopy can be misleading in cases of morphological variants or when there are discrepancies in pelvic or fluoroscopy arm positioning. In our hospital, we employ two key strategies to avoid discrepancies in pelvic or fluoroscopy arm positioning. First, we use standardized patient positioning, ensuring consistent and precise positioning of the patient. This standardization helps maintain uniform pelvic orientation. Second, we implement careful C-arm setup, focusing on two critical aspects: aligning the beam center with the area of interest to ensure the target anatomical region is properly centered in the fluoroscopic image, and positioning the C-arm perpendicular to the patient’s long axis. By adhering to these practices, we aim to minimize positioning errors, enhance image quality during the operation.
An appropriately positioned acetabular cup is crucial for optimal hip joint mechanics and mobility after total hip arthroplasty. Proper cup inclination and anteversion angles minimize wear, loosening, impingement, and dislocation risks, while ensuring smooth joint motion and reducing premature implant failure [13]. Excessive cup anteversion increases dislocation risk, while excessive cup inclination accelerates bearing surface wear, edge-loading, and elevated metal ion levels - factors that compromise implant longevity. Conversely, insufficient cup inclination decreases range of motion and raises impingement risk [14–17]. Accurate cup positioning also optimizes leg length and offset restoration, improving overall biomechanics and functional outcomes after surgery. In our study, there were no significant differences in the percentage of cases within the Lewinnek zone for cup anteversion and inclination between groups. Although there were significant differences in the median values of cup anteversion and inclination between the groups, it might be a slight adjustment necessary between approaches. For example, when using the DAA, the lip of the THR insert is usually positioned anteriorly to prevent anterior dislocation. Mercer et al. shared the experience of a single surgeon who switched from PLA to DAA, suggesting that different approaches may require a different safe zone for the cup and size because the PLA might need to prevent posterior dislocation while the DAA had the risk of anterior dislocation [18].
However, the findings of our study revealed a statistically significant reduction in LLD within the DAA group compared to the PLA group. The median LLD was 0 mm (range: -5.00 to 4.50 mm) in the DAA group and 5 mm (range: 0.00 to 9.00 mm) in the PLA group. This suggests even in the hands of an experienced surgeon, the DAA posed an enhanced ability to achieve more precise leg length adjustment. Besides the benefits of the surgeon being able to compare the bilateral lesser trochanteric height via the intraoperative anteroposterior view, the supine position itself also makes determining the proper LLD easier [19]. In approaches utilizing the lateral decubitus position, surgeons can assess proper leg length intraoperatively through assessment of knee and ankle levels [20, 21], mechanical guides and calipers that directly measure the operative leg length [22, 23], or computer navigation systems that provide accurate leg length data based on imaging and tracking [24]. However, it is clinically difficult to put the patient’s legs in the true neutral position under lateral decubitus position. Intraoperative computer navigation can achieve more precise LLD compared to conventional freehand techniques, but it is more expensive and time-consuming [25]. Although we usually consider LLD lesser than 10 mm a forgivable range [26], it is crucial to acknowledge that even minor leg length differences can have a notable impact, potentially leading to low back pain, altered gait, or other symptoms in certain patients [13, 27]. For certain individuals with specific functional requirements, such as athletes or those engaged in activities with strict biomechanical demands, minimizing LLD may be a priority.
Recent attention has focused on the concept of combined version (CV) of acetabular and femoral components, aiming to enhance impingement-free range of motion and reduce instability and impingement in THA [28–30]. A study by Benjamin et al. revealed that combined anteversion within the “safe zone” was achieved 79% of the time with the DAA. Interestingly, the outliers seemed to mostly result from failure to place the cup within the Lewinnek zone [31]. A recent study by Dimitriou et al. showed that for DAA to avoid anterior dislocation, the CV should be placed under 60 degree [32]. Our study did not measure femoral anteversion placement, thus, unable to form the CV value for comparison.
A systematic review conducted by Stolarczyk et al. in 2021 analyzed six RCTs that compared radiographic cup positioning between the DAA and other surgical approaches, suggesting the DAA may allow for better control of cup anteversion compared to other approaches, especially the lateral approach. Inconsistent findings on cup inclination and LLD, coupled with a lack of sufficient high-quality trials, make it difficult to draw definitive conclusions about the radiological outcomes of the DAA compared to other approaches in total hip replacement [33]. Our study limited the procedures to be performed by a single surgeon with well-established expertise. By having one surgeon perform all the procedures, we reduced inter-operator variability factors such as operative skills, surgical philosophy, and anticipated implant positioning. The results indicate that for an experienced surgeon in PLA, the percentage of cases falling within the Lewinnek zone are comparable to himself performing DAA. However, study by Debi et al. demonstrated that surgeon switched from anterolateral approach to DAA not only revealed a better leg length equivalence but also in cup position [34].
There are several limitations to our study. First, the retrospective nature of the study design inherently has limitations, such as potential selection bias, incomplete data, and reliance on previously recorded information which may not have been collected for the specific research question. Second, the study was conducted at a single medical center, which may limit the generalizability of the findings to other healthcare settings or patient populations. Third, the study design of our research focused entirely on radiographic parameters, evaluating cup inclination and anteversion angles as well as leg length discrepancy after THA procedures, without including any clinical outcome measures. Lastly, while having a single experienced surgeon perform all procedures helps control for inter-operator variability, the results may not be generalizable to surgeons with different levels of experience with the DAA and PLA techniques. It is possible that the single surgeon performing all cases in this study was highly proficient in both the DAA and PLA approaches. To establish a broader perspective, additional comparisons among different surgeons may be necessary.
In summary, for an experienced PLA surgeon, mastering the DAA does not necessarily enable more precise positioning of cup anteversion and inclination within the ideal range of Lewinnek zone. However, the DAA might offer advantages in minimizing LLD. These findings emphasize that for surgeons highly skilled in alternative surgical approaches, the primary concern to optimize the THA outcome could be lied within how to achieved the leg length equivalence.
Abbreviations
- DAA
Direct anterior approach
- THA
Total hip arthroplasty
- LLD
Leg length discrepancy
- PLA
Posterolateral approach
Author contributions
TM.W. brought up the conception and design of the work; PK.W. did the acquistion of data; TM.W. and PK.W. wrote the main manuscript text; PK.W. and WS.C. prepared the figures; PK.W. and KT.C. prepared the tables; CH.H. performed the formal data analysis; PC.H. and CS.C. supervised the direction and revised the manuscript; All authors have reviewed and approved the submitted version.
Funding
No funding was received for this research.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Himnaera Hospital Institutional Review Board of Human Study Committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by Himnaera Hospital Institutional Review Board of Human Study Committee. Informed consent was obtained from all participants or their legal guardians prior to their participation in the study, in accordance with the ethical guidelines.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sibia US, Turner TR, MacDonald JH, King PJ. The impact of Surgical technique on patient reported outcome measures and early complications after total hip arthroplasty. J Arthroplasty. 2017;32(4):1171–5. [DOI] [PubMed] [Google Scholar]
- 2.Matta JM, Shahrdar C, Ferguson T. Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthop Relat Res. 2005;441:115–24. [DOI] [PubMed] [Google Scholar]
- 3.Patel NN, Shah JA, Erens GA. Current trends in clinical practice for the Direct Anterior Approach Total Hip Arthroplasty. J Arthroplasty. 2019;34(9):1987–93. e1983. [DOI] [PubMed] [Google Scholar]
- 4.Soderquist MC, Scully R, Unger AS. Acetabular Placement Accuracy with the Direct Anterior Approach Freehand technique. J Arthroplasty. 2017;32(9):2748–54. [DOI] [PubMed] [Google Scholar]
- 5.Holst DC, Levy DL, Angerame MR, Yang CC. Does the use of intraoperative fluoroscopy improve postoperative radiographic component positioning and implant size in total hip arthroplasty utilizing a direct anterior approach? Arthroplast Today. 2020;6(1):94–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bingham JS, Spangehl MJ, Hines JT, Taunton MJ, Schwartz AJ. Does intraoperative Fluoroscopy Improve limb-length discrepancy and Acetabular Component Positioning during Direct Anterior Total Hip Arthroplasty? J Arthroplasty. 2018;33(9):2927–31. [DOI] [PubMed] [Google Scholar]
- 7.Lin CH, Chen WC, Weng PW, Huang YM, Liaw CK. Liaw’s Ellipse Anteversion Method for distinguishing Acetabular Component Retroversion from Anteversion on plain radiographs. Orthop Surg. 2024;16(1):276–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60(2):217–20. [PubMed] [Google Scholar]
- 9.Lin TJ, Bendich I, Ha AS, Keeney BJ, Moschetti WE, Tomek IM. A comparison of Radiographic outcomes after total hip arthroplasty between the posterior Approach and Direct Anterior Approach with Intraoperative Fluoroscopy. J Arthroplasty. 2017;32(2):616–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alvarez AM, Suarez JC, Patel P, Benton EG. Fluoroscopic imaging of acetabular cup position during THA through a direct anterior approach. Orthopedics. 2013;36(10):776–7. [DOI] [PubMed] [Google Scholar]
- 11.Gershkovich GE, Tiedeken NC, Hampton D, Budacki R, Samuel SP, Saing M. A comparison of three C-Arm draping techniques to minimize contamination of the Surgical Field. J Orthop Trauma. 2016;30(10):e351–356. [DOI] [PubMed] [Google Scholar]
- 12.Peters PG, Laughlin RT, Markert RJ, Nelles DB, Randall KL, Prayson MJ. Timing of C-arm drape contamination. Surg Infect (Larchmt). 2012;13(2):110–3. [DOI] [PubMed] [Google Scholar]
- 13.Fujita K, Kabata T, Kajino Y, Tsuchiya H. Optimizing leg length correction in total hip arthroplasty. Int Orthop. 2020;44(3):437–43. [DOI] [PubMed] [Google Scholar]
- 14.Leslie IJ, Williams S, Isaac G, Ingham E, Fisher J. High cup angle and microseparation increase the wear of hip surface replacements. Clin Orthop Relat Res. 2009;467(9):2259–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.De Haan R, Pattyn C, Gill HS, Murray DW, Campbell PA, De Smet K. Correlation between inclination of the acetabular component and metal ion levels in metal-on-metal hip resurfacing replacement. J Bone Joint Surg Br. 2008;90(10):1291–7. [DOI] [PubMed] [Google Scholar]
- 16.Coventry MB, Beckenbaugh RD, Nolan DR, Ilstrup DM. 2,012 total hip arthroplasties. A study of postoperative course and early complications. J Bone Joint Surg Am. 1974;56(2):273–84. [PubMed] [Google Scholar]
- 17.Dorr LD, Malik A, Dastane M, Wan ZN. Combined anteversion technique for total hip arthroplasty. Clin Orthop Relat R. 2009;467(1):119–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mercer N, Hawkins E, Menken L, Deshmukh A, Rathod P, Rodriguez JA. Optimum anatomic socket position and sizing for the direct anterior approach: impingement and instability. Arthroplast Today. 2019;5(2):154–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Murphy SB, Ecker TM. Evaluation of a new leg length measurement algorithm in hip arthroplasty. Clin Orthop Relat Res. 2007;463:85–9. [DOI] [PubMed] [Google Scholar]
- 20.Brodt S, Schulze M, Jacob B, Wassilew G, Nowack D, Rohe S, Matziolis G. Validity of leg length measurement in the supine and standing position compared with pelvic survey X-ray after total hip arthroplasty. Arch Orthop Trauma Surg. 2024;144(1):433–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rubash HE, Parvataneni HK. The pants too short, the leg too long: leg length inequality after THA. Orthopedics. 2007;30(9):764–5. [DOI] [PubMed] [Google Scholar]
- 22.Shiramizu K, Naito M, Shitama T, Nakamura Y, Shitama H. L-shaped caliper for limb length measurement during total hip arthroplasty. J Bone Joint Surg Br. 2004;86(7):966–9. [DOI] [PubMed] [Google Scholar]
- 23.Takigami I, Itokazu M, Itoh Y, Matsumoto K, Yamamoto T, Shimizu K. Limb-length measurement in total hip arthroplasty using a calipers dual pin retractor. Bull NYU Hosp Jt Dis. 2008;66(2):107–10. [PubMed] [Google Scholar]
- 24.Wixson RL. Computer-assisted total hip navigation. Instr Course Lect. 2008;57:707–20. [PubMed] [Google Scholar]
- 25.Manzotti A, Cerveri P, De Momi E, Pullen C, Confalonieri N. Does computer-assisted surgery benefit leg length restoration in total hip replacement? Navigation versus conventional freehand. Int Orthop. 2011;35(1):19–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Konyves A, Bannister GC. The importance of leg length discrepancy after total hip arthroplasty. J Bone Joint Surg Br. 2005;87(2):155–7. [DOI] [PubMed] [Google Scholar]
- 27.Desai AS, Dramis A, Board TN. Leg length discrepancy after total hip arthroplasty: a review of literature. Curr Rev Musculoskelet Med. 2013;6(4):336–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Widmer KH, Zurfluh B. Compliant positioning of total hip components for optimal range of motion. J Orthop Res. 2004;22(4):815–21. [DOI] [PubMed] [Google Scholar]
- 29.Renkawitz T, Haimerl M, Dohmen L, Gneiting S, Lechler P, Woerner M, Springorum HR, Weber M, Sussmann P, Sendtner E, et al. The association between femoral tilt and impingement-free range-of-motion in total hip arthroplasty. BMC Musculoskelet Disord. 2012;13:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplasty. 2002;17(3):282–8. [DOI] [PubMed] [Google Scholar]
- 31.Jackson JB, Martin JR, Christal A, Masonis JL, Springer BD, Mason JB. The Direct Anterior Approach Total Hip Arthroplasty reliably achieves safe zones for combined anteversion. Arthroplasty Today. 2020;6(4):651–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dimitriou D, Zindel C, Winkler E, Cornaz F, Mazel P, Zingg PO. Combined anteversion threshold to avoid anterior dislocation in primary total hip arthroplasty performed through the Direct Anterior Approach. J Arthroplast. 2024;39(1):145–50. [DOI] [PubMed] [Google Scholar]
- 33.Stolarczyk A, Stolarczyk M, Stepinski P, Dorocinska MK, Swiercz M, Szymczak J, Zarnovsky K, Zuchniewicz A, Maciag BM. The Direct Anterior Approach to primary total hip replacement: Radiological Analysis in comparison to other approaches. J Clin Med 2021, 10(11). [DOI] [PMC free article] [PubMed]
- 34.Debi R, Slamowicz E, Cohen O, Elbaz A, Lubovsky O, Lakstein D, Tan Z, Atoun E. Acetabular cup orientation and postoperative leg length discrepancy in patients undergoing elective total hip arthroplasty via a direct anterior and anterolateral approaches. BMC Musculoskelet Disord. 2018;19(1):188. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.