Abstract
Background: Cardiac arrest is a critical condition affecting approximately 1 in every 1000 people in Europe. Feedback devices have been developed to enhance the quality of chest compressions during CPR, but their clinical impact remains uncertain. This study aims to evaluate the effect of feedback devices on key clinical outcomes in adult patients experiencing both out-of-hospital (OHCA) and in-hospital cardiac arrest (IHCA). The primary objective is to assess their impact on the return of spontaneous circulation (ROSC); secondary objectives include the evaluation of neurological status and survival to discharge. Methods: A systematic review was conducted following PRISMA guidelines, utilizing databases including PubMed, Scopus, Web of Science, and Embase. Studies published between 2000 and 2023 comparing CPR with and without the use of feedback devices were included. A fixed-effects network meta-analysis was performed for ROSC and survival, while a frequentist meta-analysis was conducted for neurological outcomes. Results: Twelve relevant studies met the inclusion criteria. The meta-analysis results showed that the use of audiovisual feedback devices significantly increases the likelihood of ROSC (OR 1.26, 95% CI 1.13–1.41, p < 0.0001) and survival (OR 1.52, 95% CI 1.27–1.81, p < 0.0001) compared to CPR without feedback. However, the effect of metronomes did not reach statistical significance. Conclusions: Feedback devices, particularly audiovisual ones, are associated with improved clinical outcomes in cardiac arrest patients. Their use should be encouraged in both training settings and real-life emergency scenarios to enhance survival rates and ROSC. However, further studies are needed to confirm long-term impacts and to explore the potential benefits of metronomes.
Keywords: feedback devices, cardiopulmonary resuscitation, return of spontaneous circulation, OHCA, IHCA
1. Introduction
Cardiac arrest is a very relevant pathology, affecting about 1 in every 1000 people in Europe [1,2]. Studies in recent years have focused predominantly on analyzing cardiac arrests in the out-of-hospital setting (OHCA) [3,4], whereas studies on events in the in-hospital setting (IHCA) are less numerous and show very different epidemiology and outcomes from pre-hospital [5,6].
To improve patient survival, advanced cardiovascular life support (ACLS) algorithms [2,7] and the adherence that healthcare professionals follow in their management have been reported to play a relevant role [8]. The algorithm should be promptly started by all healthcare professionals attending a cardiac arrest; in fact, deviations in terms of timing [9] and the clinical algorithm have been shown to play a negative role in patient outcomes [10,11].
Cardiac arrest guidelines have emphasized the importance of the rapid initiation of CPR and proper maintenance of a standard rate [12] to guarantee proper perfusion to the critical organs. Indeed, despite the role of advanced maneuvers such as ACLS, rapid and effective BLS is necessary for the proper management of advanced maneuvers [13,14]. For this purpose, feedback devices [15] have been developed to help healthcare professionals maintain an adequate rhythm and feedback [16,17]. These devices proved effective during simulation [18] and also during the management of cardiac arrests on the ward [15].
Although the devices have shown their effectiveness [19], they are not yet commonly used in hospital settings and emergencies [20] or even in training settings where healthcare workers become familiar with devices for managing cardiac arrest [21].
The study aims to provide an evaluation of the effect of feedback devices on clinical outcomes in the adult human population during both out-of-hospital cardiac arrest (OHCA) and in-hospital cardiac arrest (IHCA). The primary objective of the study is to evaluate their effect on return to spontaneous circulation (ROSC); the secondary objective is to evaluate the effect on neurological status and survival to discharge.
2. Materials and Methods
We conducted a systematic review following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [22].
2.1. Eligibility Criteria
Studies published between 2000 and 2023 that examined cardiopulmonary resuscitation performed with the use of feedback devices by both healthcare personnel and lay bystanders were included, including both in-hospital and out-of-hospital cardiac arrests. In addition, the studies were to compare two interventions: feedback device-assisted CPR and conventional CPR (without the use of feedback devices). The language was limited to English, French, and Italian. As our research focused on the human population, studies involving dummy simulations and animal studies were excluded. Commentaries, case reports, case series, posters, narrative reviews, systematic reviews, and meta-analyses were excluded.
2.2. Search String
The PICO format was used to construct the search string:
Population: patients in cardiac arrest.
Intervention: use of feedback devices for chest compressions during CPR.
Control: CPR without the use of CPR feedback.
Outcomes: ROSC (primary outcome); survival to discharge, neurological status at discharge (secondary outcomes).
The search was conducted on 30 June 2024. Multiple databases were consulted, as recommended by the main practical guidelines for the synthesis of scientific evidence: PubMed, Scopus, Web Of Science, and Embase.
The entire working group defined and shared the search string and can be found in Supplementary Materials in Table S1 (Research strategy).
2.3. Selection of Studies
Search strings were entered into the respective databases with publication after 1 January 2000 as the limit. Papers were uploaded to Rayyan (http://rayyan.qcri.org, last access 30 June 2023), a free web and mobile app used by researchers to speed up the initial screening of articles [23]. The software was used at all stages of paper selection, up to the article inclusion stage.
Data selection was performed independently by four authors (SB, DFC, MM, and DMS), and discrepancies were resolved by consulting a fifth (LG) and a sixth (PD) author.
The LG and PD reviewers extracted data independently from the included studies. Discrepancies were resolved through discussion until a consensus was reached.
The main outcome considered in the research was the rate of return to spontaneous circulation (ROSC). Data on neurological status and survival to discharge were also extracted where available.
Publication bias risk assessment was conducted by LG using funnel plots.
2.4. Effect Measurement
For the evaluation of the effect of feedback devices on the return to spontaneous circulation, the odds ratio of ROSC between CPR using feedback devices and conventional CPR was used; the odds ratio between the survival rate of patients in cardiac arrest on whom CPR with feedback devices was performed and the odds ratio between favorable and unfavorable neurological outcomes in patients in cardiac arrest who underwent CPR with feedback devices and without was used to assess the effect of feedback devices on neurological outcomes.
2.5. Synthesis Method
We conducted a network meta-analysis with a fixed-effects model for ROSC and survival and a frequentist meta-analysis (again with a fixed-effects model) for neurological outcomes.
This type of statistical approach thus allowed us to evaluate a network of evidence in which we have more than two different interventions. In our case, the studies examined present the application of different feedback devices and their absence during CPR. In the fixed-effects model, it is assumed that the effect of interest is constant between the included studies; therefore, fixed weights are used to combine the results.
We also created networks, forest plots, and funnel plot plots for each analysis. Statistical analysis was performed with R 4.2.1 version with ‘meta’ and ‘netmeta’ packages [24].
3. Results
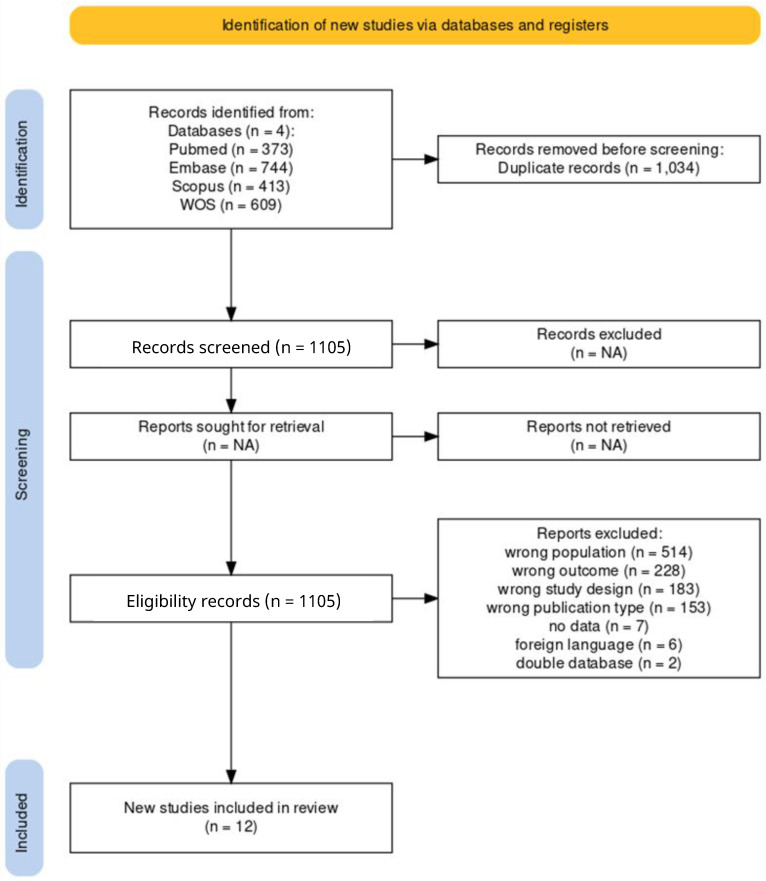
The search strings were entered into the respective databases by setting publication after 1 January 2000 as the limit. As shown in Figure 1, the search generated a total of 2139 articles of which 373 were in Pubmed, 744 were in Embase, 413 were in Scopus, and 609 were in Web of Science. All documents were uploaded to Rayyan (http://rayyan.qcri.org) to speed up the initial screening of articles [23]. The software, therefore, allowed the group to perform an initial step of eliminating duplicates, which turned out to be 1034, resulting in a total of 1105 unduplicated articles. Following further screening of articles, 12 studies were included in the meta-analysis [15,16,24,25,26,27,28,29,30,31,32,33]. Figure 1 shows the selection process flow diagram.
Figure 1.
Selection process flow diagram.
Of the 1105 potentially eligible unduplicated studies, 12 met our inclusion criteria. These 12 studies are shown in Table 1.
Table 1.
Included studies.
| Author | Year | Sample | Outcome | Feedback Type |
|---|---|---|---|---|
| Vahedian-Azimi et al. [25] | 2016 | 80 | -ROSC | Audiovisual |
| Couper et al. [26] | 2015 | 634 | -ROSC -SURVIVAL -NEUROLOGICAL OUTCOME |
Audiovisual |
| Kramer-Johansen et al. [27] | 2006 | 358 | -ROSC -SURVIVAL |
Audiovisual |
| Goharani et al. [28] | 2019 | 900 | -ROSC -SURVIVAL |
Audiovisual |
| Obling et al. [29] | 2022 | 325 | -ROSC -SURVIVAL |
Audiovisual, Metronome |
| Hostler et al. [15] | 2011 | 1586 | -ROSC -SURVIVAL -NEUROLOGICAL OUTCOME |
Audiovisual |
| Lukas et al. [30] | 2012 | 638 | -ROSC | Audiovisual |
| Abella et al. [31] | 2007 | 156 | -ROSC -SURVIVAL |
Audiovisual |
| Botelho et al. [32] | 2016 | 111 | -ROSC -SURVIVAL |
Metronome |
| Camacho Leis et al. [33] | 2012 | 892 | -ROSC | Audiovisual |
| Lakomek et al. [16] | 2020 | 292 | -ROSC | Audiovisual |
| Agerskov et al. [34] | 2017 | 196 | -ROSC -SURVIVAL |
Audiovisual |
Table 2 shows the included studies (Study) with the respective outcomes analyzed (Outcome), the type of intervention applied (Feedback), the number of events that achieved the outcome considered (Event), and the total number of events included in the intervention/control group (Total). Several outcomes were analyzed from each study (good neurological status, survival to discharge, and ROSC). For each outcome, an intervention group (feedback devices) and a control group (no feedback devices) were selected.
Table 2.
Selected studies with the respective outcomes analyzed, type of intervention/control, number of events meeting the outcome per intervention/control, and the total number of events in the intervention/control group.
| Study | Outcome | Feedback | Event | Total |
|---|---|---|---|---|
| Couper et al., 2015 [26] | GOOD NEUROLOGICAL OUTCOME | Audiovisual | 82 | 513 |
| Couper et al., 2015 [26] | GOOD NEUROLOGICAL OUTCOME | No Feedback | 17 | 121 |
| Hostler et al., 2011 [15] | GOOD NEUROLOGICAL OUTCOME | Audiovisual | 35 | 815 |
| Hostler et al., 2011 [15] | GOOD NEUROLOGICAL OUTCOME | No Feedback | 29 | 771 |
| Couper et al., 2015 [26] | SURVIVAL | No Feedback | 21 | 121 |
| Couper et al., 2015 [26] | SURVIVAL | Audiovisual | 90 | 513 |
| Kramer-Johansen et al., 2006 [27] | SURVIVAL | No Feedback | 7 | 241 |
| Kramer-Johansen et al., 2006 [27] | SURVIVAL | Audiovisual | 5 | 117 |
| Goharani et al., 2019 [28] | SURVIVAL | No Feedback | 128 | 450 |
| Goharani et al., 2019 [28] | SURVIVAL | Audiovisual | 243 | 450 |
| Hostler et al., 2011 [15] | SURVIVAL | No Feedback | 96 | 771 |
| Hostler et al., 2011 [15] | SURVIVAL | Audiovisual | 92 | 815 |
| Abella et al., 2007 [31] | SURVIVAL | No Feedback | 5 | 55 |
| Abella et al., 2007 [31] | SURVIVAL | Audiovisual | 9 | 101 |
| Botelho et al., 2016 [32] | SURVIVAL | No Feedback | 4 | 60 |
| Botelho et al., 2016 [32] | SURVIVAL | Metronome | 4 | 51 |
| Agerskov et al., 2017 [34] | SURVIVAL | No Feedback | 53 | 134 |
| Agerskov et al., 2017 [34] | SURVIVAL | Audiovisual | 24 | 62 |
| Vahedian-Azimi et al., 2016 [25] | ROSC | Audiovisual | 29 | 40 |
| Vahedian-Azimi et al., 2016 [25] | ROSC | No Feedback | 14 | 40 |
| Couper et al., 2015 [26] | ROSC | Audiovisual | 262 | 513 |
| Couper et al., 2015 [26] | ROSC | No Feedback | 61 | 121 |
| Kramer-Johansen et al., 2006 [27] | ROSC | Audiovisual | 27 | 117 |
| Kramer-Johansen et al., 2006 [27] | ROSC | No Feedback | 42 | 241 |
| Goharani et al., 2019 [28] | ROSC | Audiovisual | 300 | 450 |
| Goharani et al., 2019 [28] | ROSC | No Feedback | 191 | 450 |
| Obling et al., 2022 [29] | ROSC | Audiovisual | 51 | 155 |
| Obling et al., 2022 [29] | ROSC | Metronome | 38 | 77 |
| Obling et al., 2022 [29] | ROSC | No Feedback | 38 | 93 |
| Hostler et al., 2011 [15] | ROSC | Audiovisual | 361 | 815 |
| Hostler et al., 2011 [15] | ROSC | No Feedback | 345 | 771 |
| Lukas et al., 2012 [30] | ROSC | Audiovisual | 165 | 319 |
| Lukas et al., 2012 [30] | ROSC | No Feedback | 151 | 319 |
| Abella et al., 2007 [31] | ROSC | Audiovisual | 45 | 101 |
| Abella et al., 2007 [31] | ROSC | No Feedback | 22 | 55 |
| Botelho et al., 2016 [32] | ROSC | Metronome | 28 | 51 |
| Botelho et al., 2016 [32] | ROSC | No Feedback | 36 | 60 |
| Camacho Leis et al., 2012 [33] | ROSC | Audiovisual | 50 | 104 |
| Camacho Leis et al., 2012 [33] | ROSC | No Feedback | 319 | 788 |
| Lakomek et al., 2020 [16] | ROSC | Audiovisual | 37 | 103 |
| Lakomek et al., 2020 [16] | ROSC | No Feedback | 69 | 189 |
| Agerskov et al., 2017 [34] | ROSC | Audiovisual | 34 | 62 |
| Agerskov et al., 2017 [34] | ROSC | No Feedback | 72 | 134 |
3.1. ROSC
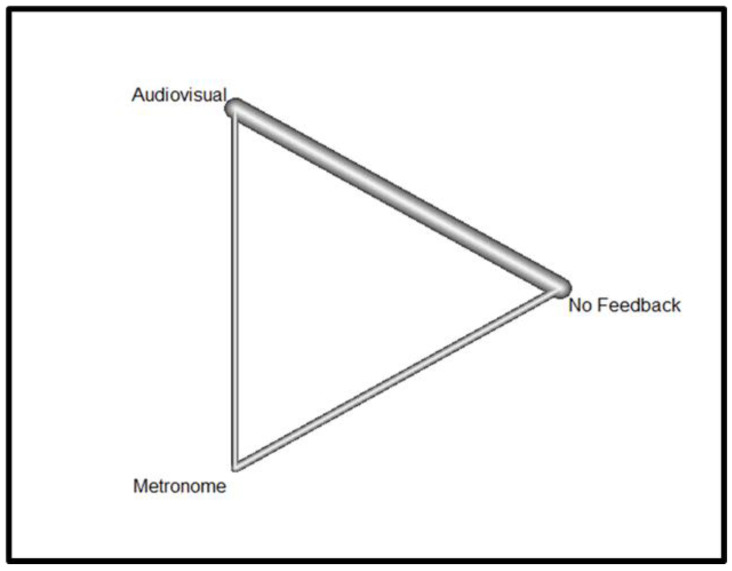
Concerning the ROSC outcome, Figure 2 shows the Netgraph linking direct comparisons of three interventions applied during cardiopulmonary resuscitation in the ROSC studies considered in this meta-analysis: the use of audiovisual feedback devices compared with the use of metronomes, the use of audiovisual feedback devices compared with the absence of feedback devices, and finally the use of metronomes compared with the absence of feedback devices.
Figure 2.
Netgraph For ROSC.
The thickness of the line connecting the different interventions represents the overall amount of comparisons between the interventions in the different studies considered; the thicker the line, the greater the number of comparisons between the two interventions. The graph shows that there are more comparisons between the use of audio-visual feedback devices and the non-use of feedback devices during cardiopulmonary resuscitation.
Table 3 summarizes the results of the comparisons between different interventions within their respective studies.
Table 3.
Summary of effect sizes (common effect model).
| Study | Treatment 1 | Treatment 2 | OR | 95% CI | Leverage |
|---|---|---|---|---|---|
| Vahedian-Azimi et al., 2016 [25] | Audiovisual | No feedback | 1.26 | [1.13–1.41] | 0.01 |
| Couper et al., 2015 [26] | Audiovisual | No feedback | 1.26 | [1.13–1.41] | 0.08 |
| Kramer-Johansen et al., 2006 [27] | Audiovisual | No feedback | 1.26 | [1.13–1.41] | 0.04 |
| Goharani et al., 2019 [28] | Audiovisual | No feedback | 1.26 | [1.13–1.41] | 0.17 |
| Obling et al., 2022 [29] | Audiovisual | Metronome | 0.84 | [0.55–1.30] | 0.00 |
| Obling et al., 2022 [29] | Audiovisual | No feedback | 1.26 | [1.13–1.41] | 0.00 |
| Obling et al., 2022 [29] | Metronome | No feedback | 1.50 | [0.98–2.30] | 0.00 |
| Hostler et al., 2011 [15] | Audiovisual | No feedback | 1.26 | [1.13–1.41] | 0.32 |
| Lukas et al., 2012 [30] | Audiovisual | No feedback | 1.26 | [1.13–1.41] | 0.13 |
| Abella et al., 2007 [31] | Audiovisual | No feedback | 1.26 | [1.13–1.41] | 0.03 |
| Botelho et al., 2016 [32] | Metronome | No feedback | 1.50 | [0.98–2.30] | 0.32 |
| Camacho Leis et al., 2012 [33] | Audiovisual | No feedback | 1.26 | [1.13–1.41] | 0.08 |
| Lakomek et al., 2020 [16] | Audiovisual | No feedback | 1.26 | [1.13–1.41] | 0.05 |
| Agerskov et al., 2017 [34] | Audiovisual | No feedback | 1.26 | [1.13–1.41] | 0.03 |
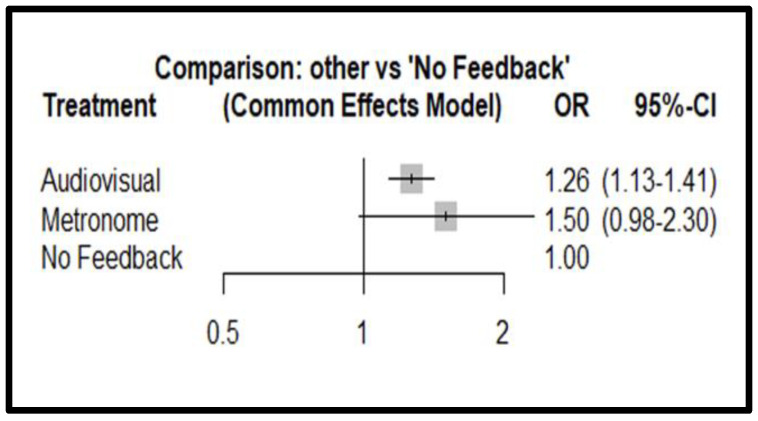
The analysis of the overall effect relative to the applied interventions for ROSC shows OR 1.26 (IC 95% 1.13–1.41, p < 0.0001) for audiovisual feedback and an OR of 1.50 (IC 95% 0.98–2.30, p = 0.064) for metronome compared to patients managed without feedback.
Figure 3 shows the forest plot for ROSC, while the funnel plot with the distribution of effects versus standard error can be found in Supplementary Materials in Figure S1, Funnel plot for ROSC.
Figure 3.
Forest plot for ROSC; Tau = 0.42, Tau2 = 0.17, I2 = 80.3% (66.4–88.4%).
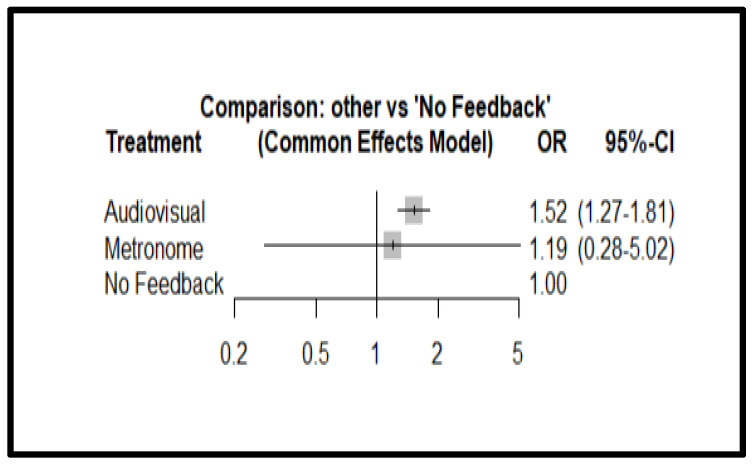
3.2. Survival
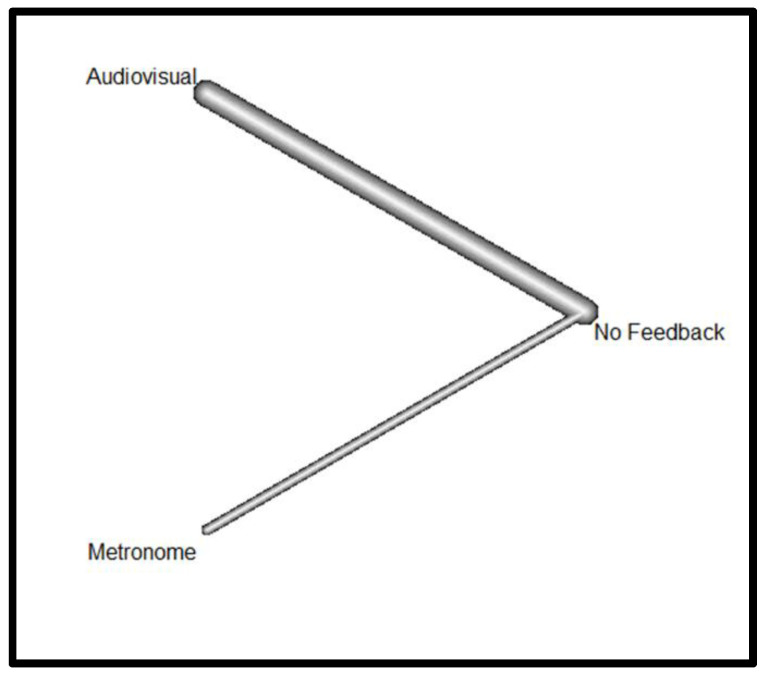
Figure 4 presents the Netgraph showing the different types of feedback devices (FDs) compared in terms of survival.
Figure 4.
Netgraph for survival.
The Netgraph shows that there is a considerable comparison between audiovisuals and the absence of feedback devices (thick line), little comparison between the metronome and the absence of feedback devices (thin line), and no direct comparison between metronome and audiovisuals (absence of line). Therefore, the comparison between metronome and audiovisual devices is made indirectly through the feedback device.
Table 4 summarizes the results of the comparisons between different interventions within their respective studies.
Table 4.
Summary of effect sizes (common effects model).
| Study | Treatment 1 | Treatment 2 | OR | 95% CI | Leverage |
|---|---|---|---|---|---|
| Couper et al., 2015 [26] | Audiovisual | No feedback | 1.52 | [1.27–1.81] | 0.12 |
| Kramer-Johansen et al., 2006 [27] | Audiovisual | No feedback | 1.52 | [1.27–1.81] | 0.02 |
| Goharani et al., 2019 [28] | Audiovisual | No feedback | 1.52 | [1.27–1.81] | 0.41 |
| Hostler et al., 2011 [15] | Audiovisual | No feedback | 1.52 | [1.27–1.81] | 0.34 |
| Abella et al., 2007 [31] | Audiovisual | No feedback | 1.52 | [1.27–1.81] | 0.02 |
| Botelho et al., 2016 [32] | Metronome | No feedback | 1.19 | [0.28–5.02] | 1.00 |
| Agerskov et al., 2017 [34] | Audiovisual | No feedback | 1.52 | [1.27–1.81] | 0.08 |
The analysis of the overall effect relative to the applied interventions on survival shows OR 1.52 (IC 95% 1.27–1.81, p < 0.0001) for the audiovisual feedback and an OR of 1.19 (IC 95% 00.28–5.02, p = 0.81) for the metronome compared to patients managed without feedback.
Figure 5 shows the forest plot for ROSC, while the funnel plot with the distribution of effects concerning the standard error can be found in Supplementary Materials in Figure S2, Funnel plot for survival.
Figure 5.
Forest plot for survival: Tau = 0.63, Tau2 = 0.40, I2 = 87.1% (74.3–93.5%).
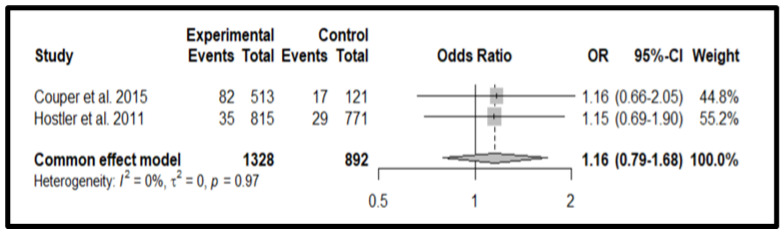
3.3. Good Neurological Outcomes
Figure 6 summarizes the results of the comparisons between audiovisual devices and unassisted CPR. The analysis of the overall effect relative to the applied interventions on survival shows OR 1.16 (95% CI 0.79–1.68, p = 0.45) for the audiovisual feedback.
Figure 6.
The funnel plot with the distribution of effects concerning the standard error can be found in Supplementary Materials in Figure S3, Funnel plot for good neurological outcome.
4. Discussion
The present meta-analysis, through direct and indirect comparisons, analyzed the impact of the use of feedback devices during cardiopulmonary resuscitation. In particular, the effects of audiovisual and metronome devices on ROSC, survival, and neurological outcomes were observed.
First, studies concerning the influence of audiovisual devices on the return to spontaneous circulation (ROSC) were analyzed. Analysis of the results regarding ROSC showed that compared to no devices in canonical CPR, the use of audiovisual feedback devices leads to an increase in ROSC (OR 1.26, 95% confidence interval [CI] 1.13–1.41%, p < 0.0001). In contrast, comparing classical CPR without device support to cardiopulmonary resuscitation supported by the use of metronomes, in the same way, showed that the latter did not lead to a significant increase in ROSC (OR 1.5, 95% confidence interval [CI] 0.98–2.23%, p = 0.06); however, it is possible that the use of the metronome was not significant due to a lack of studies or the inclusion of lower-level studies.
In the funnel plot we derived for ROSC, it could be observed that Egger’s statistical test did not show publication bias between studies that reported the incidence of ROSC in the use of the different feedback devices or their absence.
Secondly, the effects of audiovisual and metronome feedback devices on survival were observed. During the meta-analysis, several studies emerged comparing the use of audiovisual devices versus non-use and asking questions about their impact on survival. In contrast, there is a poor comparison in the literature of the impact of metronomes versus non-use concerning survival. Concerning the impact on survival, no direct comparison was found between the use of audiovisual feedback devices and metronomes, which could affect the results obtained. The meta-analysis showed that the support of audio-visual feedback devices has a positive impact on survival. The forest plot confidence interval indicates statistical significance (OR 1.52; 95% Confidence Interval [CI] 1.27–1.81).
In contrast, metronomes did not prove to have any impact on the outcome analyzed. This is justified by the very wide confidence interval, which highlights the statistical non-significance of their use (OR 1.19; 95% Confidence Interval [CI] 0.28–5.02). Thus, in contrast to ROSC, for which there are no significant data as there are statistically few studies using the metronome, it is likely that survival is not improved by the use of the metronome (p-value 0.81).
Finally, the effects of audiovisual feedback and metronomes on neurological outcomes were analyzed. In this regard, the literature presented a small number of studies analyzing the impact of devices on neurological outcomes. Specifically, these studies only observed the use of audiovisual devices and not metronomes. As a method of analysis, a non-network frequentist fixed-effect meta-analysis was performed. In this case, the effects are not distributed between the samples but there is only one true effect, and the differences between the studies are due to errors inherent in taking real-world measurements.
The meta-analysis showed that audio-visual device support did not significantly improve neurological status OR 1.16 (95% CI 0.79–1.68, p = 0.45) Looking at the forest plot in Figure 6, we can therefore state that the total effect is not significant as the tip of the cumulative effects diamond touches the baseline.
To assess the heterogeneity of studies within the meta-analysis, Kendall’s tau correlation coefficient, which quantifies the relationship between two variables, and the statistical I2, used to quantify heterogeneity between studies, were used. The I2 is based directly on the Cochran Q method and is defined as the percentage of variability in effect size that is not caused by sampling error.
In the cases of ROSC and survival, the percentages of I2 are in the range of 75% to 100%; more precisely, 80.3% for ROSC and 87.1% for survival. These percentages, according to the Cochrane Manual, are attributable to considerable heterogeneity. Concerning the result on neurological outcome, 0.0% indicates low heterogeneity.
It has been observed that in many cases, sub-optimal cardiopulmonary resuscitation is practiced both during resuscitation attempts in real cases and during simulated scenarios (guidelines for CPR and ECC, s.d.). Current guidelines consider correct cardiac massage, in terms of frequency, depth, and release, to be the principal standard for good CPR resulting in a return to spontaneous circulation and favorable outcomes [35]. To meet these standards, healthcare professionals need more and more training to maintain the ability to apply resuscitation skills. However, constant training may not be enough as the psychomotor skills of CPR delivery deteriorate rapidly [36,37].
A potential tool to ensure the maintenance of CPR skills, especially in those operators who practice basic life support infrequently, could be the use of stand-alone feedback devices or those connected to automated external defibrillators (AEDs) [38].
This meta-analysis showed that the support of feedback devices during cardiopulmonary resuscitation may lead to a positive impact on the return to spontaneous circulation and survival. In particular, audio-visual feedback devices may lead to better outcomes on the outcomes studied. However, studies supporting the use of metronomes are not numerous in the current literature.
Based on the available evidence, it can be affirmed that the use of audio-visual feedback devices should be encouraged both during training and during cases of cardiac arrest in real-life scenarios. These devices may prove to be a useful and supportive tool for the performer, especially if he/she does not work in emergency/urgent settings where it may be easier to maintain practical and theoretical skills over time.
The use of feedback devices would therefore ensure the better acquisition of skills during training and their maintenance during CPR in real time with a consequent improvement in patient outcomes. Furthermore, we must point out that the cost of the devices is not excessive and could be a useful tool to increase the survival of patients affected by IHCA by improving CPR.
We must underline that our analysis showed that there is a need for more studies on the OHCA setting, because pre-hospital systems, which often have to manage cardiac arrest in inaccessible and complicated situations, could benefit more from the use of these devices. In addition, studies should be set up to analyze the good neurological outcomes of patients, with a longer follow-up than simply ROSC; in fact, in the event of a return to spontaneous circulation, it does not guarantee that the patient will survive in the long term.
5. Conclusions
The meta-analysis showed that feedback devices are a valid support for increasing the probability of ROSC and survival for patients. Long-term survival data are lacking, however, so we would like to hope for increased interest in the scientific world. The effect of these devices is very efficient; thus, one could envisage their routine use within wards together with all the necessary devices for the management of IHCA.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm13195989/s1, Table S1: Research strategy; Figure S1: Funnel plot for ROSC; Figure S2: Funnel plot for survival; Figure S3: Funnel plot for good neurological outcome.
Author Contributions
Conceptualization, L.G. and G.S.; methodology, L.G. and G.S.; software, L.G.; validation, P.D.F., S.B., M.M. and D.M.S.; formal analysis, L.G.; investigation, P.D.F. and S.B.; resources, S.B., M.M. and D.M.S.; data curation, writing—original draft preparation, G.S.; writing—review and editing, visualization, all authors; supervision G.R. and L.G. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The original data presented in the study are available in the manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Stirparo G., Andreassi A., Sechi G.M., Signorelli C. Spring, It’s Time to ROSC. J. Prev. Med. Hyg. 2023;64:E87–E91. doi: 10.15167/2421-4248/jpmh2023.64.1.2782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bellini L., Fagoni N., Andreassi A., Sechi G.M., Bonora R., Stirparo G. Effectiveness of Cardiopulmonary Resuscitation at the Workplace. Med. Lav. Work Environ. Health. 2023;114:e2023010. doi: 10.23749/mdl.v114i3.13995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gräsner J.-T., Lefering R., Koster R.W., Masterson S., Böttiger B.W., Herlitz J., Wnent J., Tjelmeland I.B.M., Ortiz F.R., Maurer H., et al. EuReCa ONE-27 Nations, ONE Europe, ONE Registry: A Prospective One Month Analysis of out-of-Hospital Cardiac Arrest Outcomes in 27 Countries in Europe. Resuscitation. 2016;105:188–195. doi: 10.1016/j.resuscitation.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 4.Gräsner J.-T., Wnent J., Herlitz J., Perkins G.D., Lefering R., Tjelmeland I., Koster R.W., Masterson S., Rossell-Ortiz F., Maurer H., et al. Survival after Out-of-Hospital Cardiac Arrest in Europe—Results of the EuReCa TWO Study. Resuscitation. 2020;148:218–226. doi: 10.1016/j.resuscitation.2019.12.042. [DOI] [PubMed] [Google Scholar]
- 5.Andersen L.W., Holmberg M.J., Berg K.M., Donnino M.W., Granfeldt A. In-Hospital Cardiac Arrest: A Review. JAMA. 2019;321:1200–1210. doi: 10.1001/jama.2019.1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barros A.J., Enfield K.B. In-Hospital Cardiac Arrest. Emerg. Med. Clin. N. Am. 2023;41:455–464. doi: 10.1016/j.emc.2023.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Honarmand K., Mepham C., Ainsworth C., Khalid Z. Adherence to Advanced Cardiovascular Life Support (ACLS) Guidelines during in-Hospital Cardiac Arrest Is Associated with Improved Outcomes. Resuscitation. 2018;129:76–81. doi: 10.1016/j.resuscitation.2018.06.005. [DOI] [PubMed] [Google Scholar]
- 8.McEvoy M.D., Field L.C., Moore H.E., Smalley J.C., Nietert P.J., Scarbrough S.H. The Effect of Adherence to ACLS Protocols on Survival of Event in the Setting of In-Hospital Cardiac Arrest. Resuscitation. 2014;85:82–87. doi: 10.1016/j.resuscitation.2013.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grunau B., Kawano T., Scheuermeyer F., Tallon J., Reynolds J., Besserer F., Barbic D., Brooks S., Christenson J. Early Advanced Life Support Attendance Is Associated with Improved Survival and Neurologic Outcomes after Non-Traumatic out-of-Hospital Cardiac Arrest in a Tiered Prehospital Response System. Resuscitation. 2019;135:137–144. doi: 10.1016/j.resuscitation.2018.12.003. [DOI] [PubMed] [Google Scholar]
- 10.Nehme Z., Andrew E., Bernard S., Smith K. Impact of Cardiopulmonary Resuscitation Duration on Survival from Paramedic Witnessed Out-of-Hospital Cardiac Arrests: An Observational Study. Resuscitation. 2016;100:25–31. doi: 10.1016/j.resuscitation.2015.12.011. [DOI] [PubMed] [Google Scholar]
- 11.Larribau R., Deham H., Niquille M., Sarasin F.P. Improvement of Out-of-Hospital Cardiac Arrest Survival Rate after Implementation of the 2010 Resuscitation Guidelines. PLoS ONE. 2018;13:e0204169. doi: 10.1371/journal.pone.0204169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berg K.M., Bray J.E., Ng K.-C., Liley H.G., Greif R., Carlson J.N., Morley P.T., Drennan I.R., Smyth M., Scholefield B.R., et al. 2023 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations: Summary From the Basic Life Support; Advanced Life Support; Pediatric Life Support; Neonatal Life Support; Education, Implementation, and Teams; and First Aid Task Forces. Resuscitation. 2024;195:109992. doi: 10.1016/j.resuscitation.2023.109992. [DOI] [PubMed] [Google Scholar]
- 13.Kurz M.C., Schmicker R.H., Leroux B., Nichol G., Aufderheide T.P., Cheskes S., Grunau B., Jasti J., Kudenchuk P., Vilke G.M., et al. Advanced vs. Basic Life Support in the Treatment of Out-of-Hospital Cardiopulmonary Arrest in the Resuscitation Outcomes Consortium. Resuscitation. 2018;128:132–137. doi: 10.1016/j.resuscitation.2018.04.031. [DOI] [PubMed] [Google Scholar]
- 14.Picard C., Yang B.G., Norris C., McIntosh S., Douma M.J. Cardiopulmonary Resuscitation Feedback: A Comparison of Device-Measured and Self-Assessed Chest Compression Quality. J. Emerg. Nurs. 2021;47:333–341.e1. doi: 10.1016/j.jen.2020.10.003. [DOI] [PubMed] [Google Scholar]
- 15.Hostler D., Everson-Stewart S., Rea T.D., Stiell I.G., Callaway C.W., Kudenchuk P.J., Sears G.K., Emerson S.S., Nichol G. Resuscitation Outcomes Consortium Investigators Effect of Real-Time Feedback during Cardiopulmonary Resuscitation Outside Hospital: Prospective, Cluster-Randomised Trial. BMJ. 2011;342:d512. doi: 10.1136/bmj.d512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lakomek F., Lukas R.-P., Brinkrolf P., Mennewisch A., Steinsiek N., Gutendorf P., Sudowe H., Heller M., Kwiecien R., Zarbock A., et al. Real-Time Feedback Improves Chest Compression Quality in out-of-Hospital Cardiac Arrest: A Prospective Cohort Study. PLoS ONE. 2020;15:e0229431. doi: 10.1371/journal.pone.0229431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martin P., Theobald P., Kemp A., Maguire S., Maconochie I., Jones M. Real-Time Feedback Can Improve Infant Manikin Cardiopulmonary Resuscitation by up to 79%—A Randomised Controlled Trial. Resuscitation. 2013;84:1125–1130. doi: 10.1016/j.resuscitation.2013.03.029. [DOI] [PubMed] [Google Scholar]
- 18.Kiyohara K., Kitamura Y., Ayusawa M., Nitta M., Iwami T., Nakata K., Sobue T., Kitamura T. Dissemination of Chest Compression-Only Cardiopulmonary Resuscitation by Bystanders for Out-of-Hospital Cardiac Arrest in Students: A Nationwide Investigation in Japan. J. Clin. Med. 2022;11:928. doi: 10.3390/jcm11040928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nassar B.S., Kerber R. Improving CPR Performance. Chest. 2017;152:1061–1069. doi: 10.1016/j.chest.2017.04.178. [DOI] [PubMed] [Google Scholar]
- 20.Leo W.Z., Chua D., Tan H.C., Ho V.K. Chest Compression Quality and Patient Outcomes with the Use of a CPR Feedback Device: A Retrospective Study. Sci. Rep. 2023;13:19852. doi: 10.1038/s41598-023-46862-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stirparo G., Di Fronzo P., Solla D., Bottignole D., Gambolò L. Are Italian Newly Licensed Nurses Ready? A Study on Self-Perceived Clinical Autonomy in Critical Care Scenarios. Healthcare. 2024;12:809. doi: 10.3390/healthcare12080809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ouzzani M., Hammady H., Fedorowicz Z., Elmagarmid A. Rayyan—A Web and Mobile App for Systematic Reviews. Syst. Rev. 2016;5:210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.R Core Team . R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; Vienna, Austria: 2021. [Google Scholar]
- 25.Vahedian-Azimi A., Hajiesmaeili M., Amirsavadkouhi A., Jamaati H., Izadi M., Madani S.J., Hashemian S.M.R., Miller A.C. Effect of the Cardio First AngelTM Device on CPR Indices: A Randomized Controlled Clinical Trial. Crit. Care. 2016;20:147. doi: 10.1186/s13054-016-1296-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Couper K., Kimani P.K., Abella B.S., Chilwan M., Cooke M.W., Davies R.P., Field R.A., Gao F., Quinton S., Stallard N., et al. The System-Wide Effect of Real-Time Audiovisual Feedback and Postevent Debriefing for In-Hospital Cardiac Arrest: The Cardiopulmonary Resuscitation Quality Improvement Initiative. Crit. Care Med. 2015;43:2321–2331. doi: 10.1097/CCM.0000000000001202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kramer-Johansen J., Myklebust H., Wik L., Fellows B., Svensson L., Sørebø H., Steen P.A. Quality of Out-of-Hospital Cardiopulmonary Resuscitation with Real Time Automated Feedback: A Prospective Interventional Study. Resuscitation. 2006;71:283–292. doi: 10.1016/j.resuscitation.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 28.Goharani R., Vahedian-Azimi A., Pourhoseingholi M.A., Amanpour F., Rosano G.M.C., Sahebkar A. Survival to Intensive Care Unit Discharge among In-hospital Cardiac Arrest Patients by Applying Audiovisual Feedback Device. ESC Heart Fail. 2021;8:4652–4660. doi: 10.1002/ehf2.13628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Obling L., Hassager C., Blomberg S.N., Folke F. Inverse Association Between Bystander Use of Audiovisual Feedback From an Automated External Defibrillator and Return of Spontaneous Circulation. J. Am. Heart Assoc. 2022;11:e023232. doi: 10.1161/JAHA.121.023232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lukas R.-P., Gräsner J.T., Seewald S., Lefering R., Weber T.P., Van Aken H., Fischer M., Bohn A. Chest Compression Quality Management and Return of Spontaneous Circulation: A Matched-Pair Registry Study. Resuscitation. 2012;83:1212–1218. doi: 10.1016/j.resuscitation.2012.03.027. [DOI] [PubMed] [Google Scholar]
- 31.Abella B.S., Edelson D.P., Kim S., Retzer E., Myklebust H., Barry A.M., O’Hearn N., Hoek T.L.V., Becker L.B. CPR Quality Improvement during In-Hospital Cardiac Arrest Using a Real-Time Audiovisual Feedback System. Resuscitation. 2007;73:54–61. doi: 10.1016/j.resuscitation.2006.10.027. [DOI] [PubMed] [Google Scholar]
- 32.de Oliveira Botelho R.M., Campanharo C.R.V., Lopes M.C.B.T., Okuno M.F.P., de Góis A.F.T., Batista R.E.A. The Use of a Metronome during Cardiopulmonary Resuscitation in the Emergency Room of a University Hospital. Rev. Lat. Am. Enferm. 2016;24:e2829. doi: 10.1590/1518-8345.1294.2829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leis C.C., González V.A., Hernández R.D.E., Sánchez Ó.E., Martín J.L.M., Hermosa E.J.M., Torres E.C. Feedback on Chest Compression Quality Variables and Their Relationship to Rate of Return of Spontaneous Circulation. Emergencias. 2013;25:99–104. [Google Scholar]
- 34.Agerskov M., Hansen M.B., Nielsen A.M., Møller T.P., Wissenberg M., Rasmussen L.S. Return of Spontaneous Circulation and Long-Term Survival According to Feedback Provided by Automated External Defibrillators. Acta Anaesthesiol. Scand. 2017;61:1345–1353. doi: 10.1111/aas.12992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Idris A.H., Guffey D., Pepe P.E., Brown S.P., Brooks S.C., Callaway C.W., Christenson J., Davis D.P., Daya M.R., Gray R., et al. Chest Compression Rates and Survival Following Out-of-Hospital Cardiac Arrest. Crit. Care Med. 2015;43:840–848. doi: 10.1097/CCM.0000000000000824. [DOI] [PubMed] [Google Scholar]
- 36.Oermann M.H., Kardong-Edgren S.E., Odom-Maryon T. Competence in CPR. AJN Am. J. Nurs. 2012;112:43–46. doi: 10.1097/01.NAJ.0000414320.71954.34. [DOI] [PubMed] [Google Scholar]
- 37.Stirparo G., Bellini L., Solla D., Stirparo P., Fagoni N., Gambolò L. Should Basic Life Support–Defibrillator Training Be Compulsory for Newly Licensed Italian Physicians? An Observational Study. J. Cardiovasc. Med. 2024;25:632–636. doi: 10.2459/JCM.0000000000001645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gugelmin-Almeida D., Tobase L., Polastri T.F., Peres H.H.C., Timerman S. Do Automated Real-Time Feedback Devices Improve CPR Quality? A Systematic Review of Literature. Resusc. Plus. 2021;6:100108. doi: 10.1016/j.resplu.2021.100108. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original data presented in the study are available in the manuscript.