Abstract
Objective: To investigate the anesthetic and analgesic effects of combining general anesthesia with an anterior quadratus lumborum block at the lateral supra-arcuate ligament (SA-AQLB) in elderly patients undergoing laparoscopic radical resection for colorectal cancer (CRC). Methods: In this prospective study, 92 elderly patients scheduled for radical CRC resection were randomly divided into three groups: ultrasound-guided SA-AQLB group (SA group, n=31), ultrasound-guided subcostal AQLB (SC-AQLB) group (SC group, n=31), and a general anesthesia-only group (GA group, n=30). Measurements included mean arterial pressure (MAP) and heart rate (HR) at predefined time points, ranging from pre-operation to the end of surgery. Visual analog scale (VAS) pain scores were recorded at multiple postoperative time points up to 48 hours. Additional data collected included intraoperative drug dosages, anesthetic recovery times, patient-controlled intravenous analgesia (PCIA) usage, Lovett muscle strength scores, and early postoperative recovery indicators. Results: The SA group consistently showed lower MAP and HR compared to the SC group, which in turn was lower than the GA group during the monitored time points (all P<0.05). Sensory block levels were significantly higher in the SA group than that in the SC group (P<0.05). Postoperative VAS scores were also significantly lower in the SA group compared to the other groups at all recorded times (all P<0.05). The SA group required lower doses of propofol, remifentanil, and sufentanil, but higher doses of ephedrine compared to the SC and GA groups (all P<0.05). Anesthesia recovery time was shorter in the SA group, and the total number of PCIA pump presses was least in the SA group (P<0.05). Early ambulation was achieved sooner in the SA and SC groups (P<0.05), and the incidence of nausea and vomiting was reduced in these groups compared to the GA group (P<0.05). Conclusion: General anesthesia combined with ultrasound-guided SA-AQLB provides superior outcomes to general anesthesia alone in elderly patients undergoing laparoscopic CRC surgery. This approach significantly reduces general anesthesia drug dosage, decreases postoperative pain, minimizes perioperative adverse events, and accelerates patient recovery.
Keywords: Ultrasound guidance, anterior quadratus lumborum block at the lateral supra-arcuate ligament, subcostal anterior quadratus lumborum block, radical resection of colorectal cancer, perioperative analgesia
Introduction
Colorectal cancer (CRC) is a prevalent malignant tumor within the digestive system, notably among elderly populations [1]. Radical resection for CRC in these patients carries an increased risk of perioperative cardiovascular and cerebrovascular events due to pre-existing conditions, diminished physiological resilience, and postoperative pain. Furthermore, the extended duration of laparoscopic procedures for CRC necessitates substantial quantities of general anesthetics, raising concerns over perioperative management. High doses of opioid analgesics during this period can suppress respiratory function and exacerbate the risk of adverse events like nausea and vomiting in elderly patients. Consequently, minimizing the dosage of anesthetics, reducing postoperative pain, and facilitating rapid patient recovery remain critical challenges in clinical anesthesia [2,3].
The advent of enhanced recovery after surgery protocols has popularized multimodal analgesia in managing postoperative pain. A combined approach of nerve blockades and intravenous opioids is increasingly adopted to alleviate perioperative discomfort in patients undergoing radical CRC resection [4-8]. Among the various techniques, the quadratus lumborum block (QLB) is favored in abdominal surgeries due to its effective pain control and lower complication rates [9-13]. Nevertheless, the clinical application of QLB is sometimes limited by its delayed onset and inconsistent blockade levels. It is hypothesized that the arcuate ligament below the diaphragm may obstruct the diffusion of anesthetic agents, thereby impacting the efficacy of the nerve block [14-19].
Therefore, clinical researchers are actively investigating methods to enhance the efficacy of the traditional ultrasound-guided QLB while retaining its benefits. In 2020, Professor Yun Wang and colleagues introduced a novel QLB technique known as the AQLB at the lateral supra-arcuate ligament (SA-AQLB), also referred to as the supra-arcuate ligament QLB or supra-QLB [20]. This technique involves injecting local anesthetic into the quadratus plane above the lateral arcuate ligament, targeting the space below the quadratus lumborum muscle between the lateral supra-arcuate ligament and the fascia extending from the 12th rib to the L1 transverse process [21]. This strategic placement of the injection site near the lower thoracic paravertebral space facilitates enhanced diffusion of the anesthetic into the paravertebral space, potentially broadening the block’s range and improving its precision [22-24]. From an anatomical standpoint, SA-AQLB is theorized to provide a more extensive and targeted blockade [25-27]. However, research on SA-AQLB is still emerging, with a notable lack of comparative studies on its clinical efficacy against traditional QLB techniques in elderly patients undergoing laparoscopic surgery of CRC. Consequently, this study aims to evaluate the anesthetic and analgesic effects of combining SA-AQLB with general anesthesia in this patient demographic.
Materials and methods
General data
Research object
This prospective study initially included 119 elderly patients scheduled for elective laparoscopic radical resection of CRC at Changsha Central Hospital from May 2022 to February 2023. Following application of inclusion, exclusion, and elimination criteria, 10 patients were deemed ineligible, and 17 were excluded due to refusal to participate (n=5), loss to follow-up (n=5), conversion to open surgery (n=5), and inadequate ultrasound imaging (n=2). Consequently, 92 patients were included in the final analysis (Figure 1). These participants were randomly assigned to one of three groups using a random number method: ultrasound-guided SA-AQLB group (SA group, n=31), ultrasound-guided subcostal AQLB (SC-AQLB) group (SC group, n=31), and general anesthesia-only group (GA group, n=30). The study protocol was approved by the Ethics Committee of Changsha Central Hospital (approval number 2022-S0038), and all participants or their authorized representatives provided informed consent. The study was registered with the Chinese Clinical Trial Registry (ChiCTR2200063811).
Figure 1.
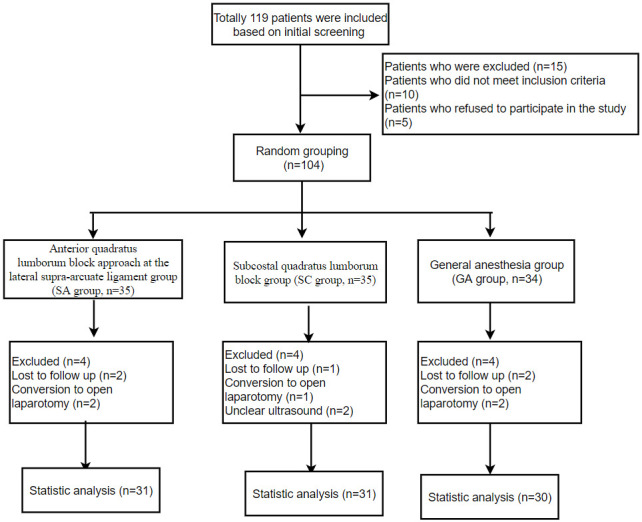
Flow chart of the clinical trial.
Inclusion and exclusion criteria for patients
(1) Inclusion criteria: classified as ASA II-III; diagnosed based on established criteria [28]; aged 65 to 80 years with a body mass index (BMI) between 16 and 29 kg/m2; possessing complete clinical data; and capable of effective communication and compliance. (2) Exclusion criteria: patients recently receiving analgesic treatment; with cognitive impairments impacting pain assessment; with diabetes, mental illnesses, severe cardiovascular or cerebrovascular diseases, abnormal liver or kidney functions, coagulation disorders, infections or tumor lesions at the puncture site, shock, endocrine disorders, or allergies to local anesthetics.
Case elimination criteria
Patients with incomplete intraoperative data or lost to follow-up postoperatively. Patients undergoing a change from laparoscopic to open surgical approach. Patients with poor ultrasound visualization of anatomical structures, resulting in unsuccessful nerve blocks.
Study grouping and procedure
Using PASS 11 software, the sample size was initially calculated based on the preliminary dose of remifentanil, requiring 24 cases per group. Accounting for an anticipated 20% attrition rate, the required sample size was adjusted to 30 per group, totaling 90 participants (Figure 1). All groups received uniform general anesthesia. The SA and SC groups underwent bilateral nerve blocks before general anesthesia induction, whereas the GA group did not receive any nerve block. All nerve blocks were administered by the same anesthesiologist, and surgeries were performed by the same surgical team. The study maintained blinding for patients, anesthesia providers, surgeons, ward staff, caregivers, and postoperative evaluators, except for the anesthesiologist administering the nerve blocks. This anesthesiologist did not participate in other aspects of the study.
Preparation before anesthesia
Upon admission, all groups received peripheral venous access for the intravenous administration of Ringer’s sodium acetate. Monitoring included percutaneous oxygen saturation (SpO2), electrocardiogram (ECG), bispectral index (BIS), axillary temperature, and end-tidal carbon dioxide pressure (PETCO2). Mean arterial pressure (MAP) was monitored via left radial artery cannulation.
Nerve block
SA-AQLB
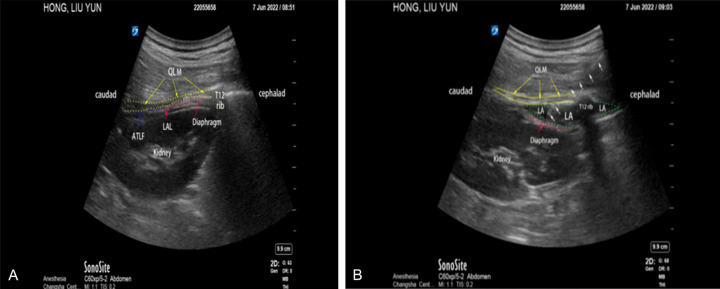
In the SA group, bilateral SA-AQLB [29] was performed before the induction of general anesthesia. Using a portable color ultrasound device, patients were positioned prone with elevated lumbar backs facilitated by a tilted operating table or a thin pillow under the lumbar area to expose the target site for the nerve block. After identifying the bilateral costovertebral angles, the area was sterilized and draped, and a sterile cover was applied to the ultrasound probe. A low-frequency (1-5 MHz) ultrasound probe was used for sagittal scanning, positioned vertically at the bilateral costovertebral angles and parallel to the spine. The probe was slightly tilted outward toward the spine for a midline long-axis paravertebral scan. The “L1 transverse process disappearance” method helped identify the L1 and L2 transverse processes alongside the brightly illuminated T12 rib. Patients were instructed to breathe deeply, aiding the “curtain method” in identifying two high-echogenicity structures sandwiching a low-echogenicity structure, indicative of the diaphragm, pleura, deep layers of the kidney, and the “pod-shaped” quadratus lumborum above the diaphragm. The target area for puncture was identified between the T12 rib and L1, between the quadratus lumborum and diaphragm (Figure 2A). Using an in-plane ultrasound-guided technique, the needle was inserted from the posterior superior direction to the lower inner side until it reached the anterior layer of the quadratus lumborum, where a subtle breakthrough sensation was noted. Correct placement was confirmed by the absence of blood or air upon aspiration, followed by injection of 0.3 ml/kg of 0.4% ropivacaine hydrochloride. Successful injection was confirmed by observing the diaphragm being pushed downward and the medication spreading towards both ends (Figure 2B). The procedure was replicated on the opposite side. Sensory block levels were assessed through ice block testing at 5 and 15 minutes post-block; reduced abdominal skin sensation or segmental block indicated successful nerve block.
Figure 2.
Ultrasound-guided SA-AQLB with a low-frequency probe. A: Pre-nerve block image. B: Post-nerve block image. Notes: T12 rib = 12th rib, Diaphragm = diaphragm, QLM = quadratus lumborum muscle, LAL = ligamentum arteriosum laterale, ATLF = Anterior thoracolumbar fascia, LA = local anesthetic. White arrow indicates the nerve block needle insertion. SA-AQLB: Anterior quadratus lumborum block at the lateral supra-arcuate ligament.
SC-AQLB
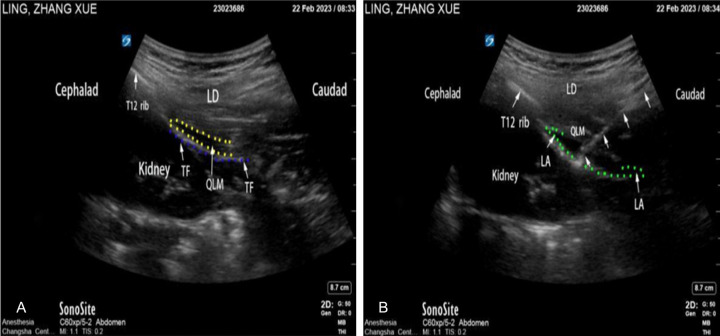
In the SC group, a bilateral ultrasound-guided SC-AQLB [30] was performed prior to the induction of general anesthesia. Using a portable color ultrasound device, patients were placed in a prone position to expose the lumbar back skin. The operating table was adjusted to elevate the lumbar region, either by lowering the head and feet or by placing a thin pillow under the lumbar area to improve access to the anatomical site. After locating the bilateral costovertebral angles, the area was sterilized, and drapes were applied. A sterile cover was placed on the ultrasound probe, which used a low-frequency (1-5 MHz) setting for sagittal scanning. The “L1 transverse process disappearance” technique identified the L1 and L2 transverse processes and the prominently illuminated T12 rib. The probe was then positioned at the L1-L2 level, 6-8 cm lateral to the L1 spinous process, and oriented with an inward tilt at both the head and tail ends for oblique sagittal plane scanning. This technique delineated the latissimus dorsi muscle, quadratus lumborum (QL), the anterior layer of the thoracolumbar fascia (TF), perirenal fat, and the kidney sequentially. Employing a long-axis in-plane technique, the needle was advanced through these layers until a distinct breakthrough sensation was felt as it penetrated the anterior layer of the quadratus lumborum, indicating the needle was positioned between the QL and the anterior layer of the TF. Successful placement was confirmed by the absence of blood or air upon aspiration, followed by the administration of 0.3 ml/kg of 0.4% ropivacaine hydrochloride. The injection was visualized on ultrasound as a depression of the anterior layer of the TF (Figure 3), signifying a successful puncture and injection. This method was replicated on the opposite side. Sensory block levels were evaluated using ice block testing at 5 and 15 minutes post-block, with reduced sensation or segmental block of the abdominal skin confirming a successful nerve block.
Figure 3.
Ultrasound-guided SC-AQLB with a low-frequency probe. A: Pre-nerve block image. B: Post-nerve block image. Notes: T12 rib = 12th rib, QLM = quadratus lumborum muscle, LD = Latissimus dorsi, TF = transversalis fascia, LA = local anesthetic. White arrow indicates the nerve block needle insertion. SA-AQLB: Anterior quadratus lumborum block at the lateral supra-arcuate ligament; SC-AQLB: subcostal anterior quadratus lumborum block.
Anesthesia induction
Induction of anesthesia followed a uniform protocol across all three groups. Intravenous administration included 0.3 mg of pentobarbital sodium (H20193271, Huasen Pharmaceutical), 1 mg/kg of propofol (H20200013, Liaoning Hienke Pharmaceutical), 0.3 μg/kg of sufentanil (H20054171, Yichang Renfu Pharmaceutical), and 0.3 mg/kg of rocuronium. Following a 3-5 minutes oxygenation period, an appropriately sized reinforced endotracheal tube was selected based on each patient’s weight and gender. Tube placement was confirmed and secured, followed by the initiation of mechanical ventilation set to a tidal volume of 6-8 ml/kg and maintaining endtidal carbon dioxide (PETCO2) between 35-45 mmHg. The ventilation rate was adjusted between 10-16 breaths per minute.
Anesthesia maintenance
Anesthesia was maintained with a combination of inhalation and intravenous methods: (1) Inhalation Anesthesia: Continuous administration of sevoflurane at 0.6 MAC. (2) Intravenous Anesthesia: Remifentanil was infused at 0.05-0.2 μg/(kg·min), propofol at 4-12 mg/(kg·h), and cisatracurium at 0.1 mg/(kg·h). Anesthesia depth was monitored using the BIS, maintaining it between 40 and 60. The rates of propofol and remifentanil were adjusted according to variations in BIS, MAP, and heart rate (HR). All medications were discontinued at skin closure, with cessation of cisatracurium 30 minutes prior to the end of surgery. (3) Intraoperative Anesthesia: Continuous intravenous infusion of Ringer’s acetate, a balanced electrolyte solution, or Ringer’s lactate was used to manage blood volume. Blood pressure was kept within 20% of baseline values. For decreases in MAP below 80% of baseline, ephedrine hydrochloride (3-6 mg) was administered. Increases in MAP above 120% of baseline prompted deepening anesthesia or an additional dose of sufentanil (5 µg). Sinus bradycardia (HR≤45 beats/min for more than 1 minute) was treated with anisodamine (2 mg), and tachycardia (HR≥100 beats/min for more than 1 minute) with landiolol (5 mg). Following surgery, spontaneous respiration was awaited before administering neostigmine (0.5 mg), and the endotracheal tube was removed upon meeting extubation criteria.
Postoperative analgesia scheme
Following surgery, patients from all groups were transferred to the post-anesthesia care unit where they received patient-controlled intravenous analgesia (PCIA). The PCIA pump was loaded with a mixture containing sufentanil (50 μg), nalbuphine (80 mg), and normal saline up to a total volume of 95 ml. The pump was programmed to deliver a self-administered dose of 0.5 ml with a lockout interval of 15 minutes and a continuous infusion rate of 2 ml/h.
Outcome measures
Primary outcome measures [28]
(1) Hemodynamic Parameters: The MAP and HR were recorded at specific intervals: upon arrival in the operating room (T0), 5 minutes before surgical incision (T1), during surgical incision (T2), 30 minutes after the start of surgery (T3), at the end of surgery (T4), and during extubation in the postoperative period (T5). Additionally, for the SA and SC groups, MAP and HR were compared before, and 5 and 15 minutes after the nerve blocks were administered. (2) Postoperative Visual Analog Scale (VAS) Score: VAS scores for resting and during activity were recorded at multiple time points: during extubation (T5), upon transfer from the post-anesthesia care unit to the ward (T6), and at 6 (T7), 12 (T8), 24 (T9), and 48 hours (T10) postoperatively. The VAS scale ranges from 0 (no pain) to 10 (maximum pain). (3) Intraoperative Anesthetic Drug Dosage and PCIA Usage: The doses of sufentanil, remifentanil, and propofol used during the operation were recorded. Additionally, the total number of PCIA pump presses within the first 48 hours postoperatively was documented. (4) Sensory Block Level Assessment: In the SA and SC groups, the level of sensory block was evaluated at 5 and 15 minutes post-block. This assessment was performed using an ice cube test along the midline of the abdomen, sternal line, anterior axillary line, and mid-axillary line. A detectable sensory block segment or decreased sensation indicated a successful nerve block.
Secondary outcome measures
(1) Dosage of Vasoactive Drugs: This includes the usage of ephedrine, anisodamine, and landiolol during surgery across the three groups. (2) Postoperative Lovett Muscle Strength Score: The Lovett muscle strength score is a scale from 0 to 5, where 0 indicates no muscle contraction and higher scores reflect increasing strength. A score of 5 denotes full resistance against gravity and the ability to perform complete joint movements. (3) Anesthetic Recovery Time and Early Postoperative Recovery Outcomes: These outcomes for the three groups include the time to first ambulation post-surgery, the length of hospital stay, and the incidence of adverse events within 48 hours postoperatively. Adverse events monitored include dizziness, local anesthetic toxicity, nausea and vomiting, pneumothorax, renal injury, and nerve damage.
Statistical analyses
With a significance level set at α=0.05 and power (1-β)=0.9, the initial sample size was calculated as 24 participants per group using PASS 11 software, with adjustments for an anticipated 20% dropout rate increasing this to 30 participants per group, for a total of 90 participants. Data were analyzed using SPSS 28.0. For normally distributed variables, results are presented as mean ± standard deviation. Group comparisons were made using one-way analysis of variance (ANOVA), with repeated measures ANOVA used for within-group comparisons over time. Hemodynamic indices, VAS scores, and Lovett muscle strength assessments were analyzed using repeated measures ANOVA. For non-normally distributed variables, results are presented as median and interquartile range (M [P25, P75]), and compared using the Kruskal-Wallis test. Categorical data were presented as counts (%) and analyzed using the chi-square test (X2). A P-value <0.05 was considered statistically significant.
Results
Comparison of general characteristics among the three groups
Analysis of general characteristics, including gender, ASA classification, age, BMI, and surgery duration, revealed no significant differences among the groups (all P>0.05, Table 1).
Table 1.
Comparison of general characteristics among the three groups (x̅ ± s)
| Items | SA group (n=31) | SC group (n=31) | GA group (n=30) | F/χ2 | P value |
|---|---|---|---|---|---|
| Sex ratio (male/female) | 14/17 | 15/16 | 17/13 | 1.571 | 0.652 |
| ASA ratio (II/III) | 11/20 | 14/17 | 15/15 | 0.616 | 0.511 |
| Age (years) | 71.21±6.09 | 71.56±5.61 | 71.30±6.94 | 1.289 | 0.842 |
| BMI (kg/m2) | 22.74±4.12 | 23.33±4.13 | 22.03±2.63 | 1.561 | 0.650 |
| Surgery duration | 277.00±79.45 | 265.33±95.50 | 230.35±78.45 | 2.098 | 0.154 |
| Mean preoperative blood pressure | 87.82±1.01 | 90.01±0.95 | 88.55±1.10 | 1.996 | 0.319 |
| Preoperative oxygen saturation | 97.58±1.85 | 97.24±1.33 | 98.04±1.03 | 0.901 | 0.428 |
| Preoperative heart rate | 75.01±2.10 | 71.33±2.02 | 76.56±2.35 | 0.798 | 0.821 |
| Blood loss | 81.01±49.32 | 79.32±39.00 | 76.78±49.61 | 0.401 | 0.950 |
| Transfusion volume | 1852.00±781.29 | 1736.00±484.15 | 1603.32±450.00 | 1.987 | 0.367 |
Notes: ASA: American Society of Anesthesiologists; BMI: Body mass index.
Comparison of hemodynamics in three groups at different time points
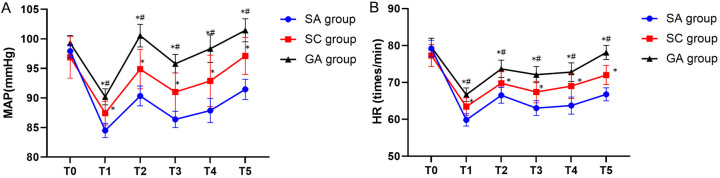
Comparison of MAP and HR of three groups at different time points
At T0, there were no significant differences in MAP and HR among the three groups (P>0.05). From T1 to T5, the SA group exhibited lower MAP and HR compared to the GA group, and the SC group also displayed lower MAP and HR when compared to the GA group (all P<0.05, Table 2 and Figure 4).
Table 2.
Comparison of MAP and HR at different time points among the three groups (x̅ ± s)
| Indices | Time points | SA group (n=31) | SC group (n=31) | GA group (n=30) | χ2 | P value |
|---|---|---|---|---|---|---|
| MAP (mmHg) | T0 | 97.92±1.05 | 96.89±1.79 | 99.75±1.20 | 0.441 | 0.344 |
| T1 | 84.50±1.07 | 87.11±1.82* | 90.70±1.22*,# | 24.678 | 0.002 | |
| T2 | 89.15±1.64 | 94.89±2.79* | 100.55±1.87*,# | 39.891 | <0.001 | |
| T3 | 86.39±1.37 | 91.00±2.34* | 95.80±1.57*,# | 42.019 | <0.001 | |
| T4 | 87.89±2.01 | 93.67±3.42* | 98.35±2.29*,# | 23.897 | 0.005 | |
| T5 | 89.85±1.46 | 96.67±2.47* | 103.70±1.66*,# | 39.019 | <0.001 | |
| HR (times/minute) | T0 | 79.21±2.20 | 77.33±3.02 | 79.56±2.40 | 0.750 | 0.847 |
| T1 | 59.84±1.59 | 63.44±2.31* | 68.44±1.73*,# | 19.876 | 0.003 | |
| T2 | 64.47±1.64 | 72.11±2.39* | 78.94±1.79*,# | 42.109 | <0.001 | |
| T3 | 63.05±1.88 | 67.44±2.73* | 73.50±2.04*,# | 26.785 | 0.002 | |
| T4 | 64.16±2.10 | 69.00±3.05* | 75.50±2.29*,# | 18.786 | 0.003 | |
| T5 | 66.05±1.68 | 73.11±2.44* | 84.19±1.83*,# | 40.198 | <0.001 |
indicates P<0.05 vs. the SA group at the same time point;
indicates P<0.05 vs. the SC group at the same time point.
SA group: ultrasound-guided anterior quadratus lumborum block at the lateral supra-arcuate ligament group; SC group: ultrasound-guided subcostal anterior quadratus lumborum block group; GA group: general anesthesia-only group; T0: upon arrival in the operating room; T1: 5 minutes before surgical incision; T2: during surgical incision; T3: 30 minutes after the start of surgery; T4: at the end of surgery; T5: during extubation in the postoperative period; MAP: Mean arterial pressure; HR: Heart rate.
Figure 4.
Comparison of MAP and HR in three groups at different time points during operation. A: Comparison of MAP in three groups during operation. B: Comparison of HR in three groups during operation. Notes: * indicates P<0.05 vs. the SA group at the same time point; # indicates P<0.05 vs. the SC group at the same time point. MAP: Mean arterial pressure; HR: Heart rate; SA group: ultrasound-guided anterior quadratus lumborum block at the lateral supra-arcuate ligament group; SC group: ultrasound-guided subcostal anterior quadratus lumborum block group; GA group: general anesthesia-only group.
Comparison of MAP and HR before and after nerve block in SA and SC groups
The comparisons of MAP and HR before, 5 and 15 minutes after nerve block in both the SA and SC groups showed no significant differences either between or within the groups (all P>0.05, Table 3 and Figure 5).
Table 3.
Comparison of MAP and HR before and after SA-AQLB and SC-AQLB (x̅ ± s)
| Indices | Time points | SA group (n=31) | SC group (n=31) | χ2 | P value |
|---|---|---|---|---|---|
| MAP (mmHg) | Before block | 95.60±1.94 | 94.83±3.07 | 1.178 | 0.835 |
| 5 min after block | 94.60±3.15 | 94.33±4.98 | 0.534 | 0.964 | |
| 10 min after block | 93.60±2.52 | 93.67±3.98 | 0.498 | 0.989 | |
| HR (times/minute) | Before block | 78.27±2.71 | 78.64±4.69 | 0.610 | 0.947 |
| 5 min after block | 75.94±2.56 | 76.64±4.43 | 1.310 | 0.892 | |
| 10 min after block | 73.758±2.52 | 75.00±4.36 | 0.991 | 0.806 |
Notes: MAP: Mean arterial pressure; HR: Heart rate; SA-AQLB: anterior quadratus lumborum block at the lateral supra-arcuate ligament; SC-QLB: subcostal anterior quadratus lumborum block; SA group: ultrasound-guided anterior quadratus lumborum block at the lateral supra-arcuate ligament group; SC group: ultrasound-guided subcostal anterior quadratus lumborum block group; GA group: general anesthesia-only group.
Figure 5.
Changes in MAP and HR at the time of admission to the operating room and skin incision in the SA and SC groups. A: Comparison of MAP between the two groups before and after nerve block. B: Comparison of HR between the two groups before and after nerve block. Notes: SA group: ultrasound-guided anterior quadratus lumborum block at the lateral supra-arcuate ligament group; SC group: ultrasound-guided subcostal anterior quadratus lumborum block group; GA group: general anesthesia-only group; MAP: Mean arterial pressure; HR: Heart rate.
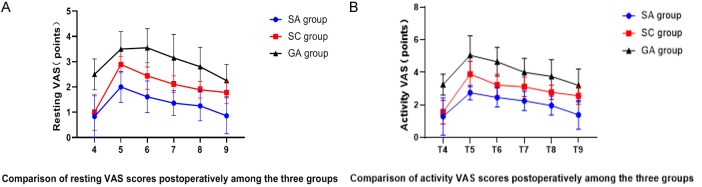
Comparison of VAS scores at different time points after surgery among the three groups
At T5, both the SA and SC groups reported significantly lower VAS scores at rest and during activity compared to the GA group (P<0.05). There was no significant difference between the SA and SC groups (P>0.05). From T6 to T9, the SA group continued to exhibit lower VAS scores at rest and during activity than the SC group, and the SC group reported lower scores than the GA group (all P<0.05). At T10, the SA group maintained lower VAS scores in comparison to both the SC and GA groups (P>0.05); however, no significant difference was observed between the SC and GA groups (P>0.05, Table 4 and Figure 6).
Table 4.
Comparison of resting and activity VAS scores at different time points postoperatively among the three groups (x̅ ± s, points)
| Indices | Time points | SA group (n=31) | SC group (n=31) | GA group (n=30) | χ2 | P value |
|---|---|---|---|---|---|---|
| Resting VAS | T5 | 0.83±0.82 | 1.00±0.71 | 2.5±0.61*,# | 42.015 | <0.001 |
| T6 | 2.00±0.61 | 2.89±0.33* | 3.95±0.69*,# | 41.217 | <0.001 | |
| T7 | 1.61±0.63 | 2.44±0.53* | 3.55±0.76*,# | 40.287 | <0.001 | |
| T8 | 1.36±0.49 | 2.11±0.33* | 3.15±0.93*,# | 41.001 | <0.001 | |
| T9 | 1.25±0.59 | 1.89±0.33* | 2.80±0.77*,# | 40.277 | <0.001 | |
| T10 | 0.86±0.71 | 1.78±0.44* | 2.25±0.64* | 41.201 | <0.001 | |
| Activity VAS | T5 | 1.29±1.15 | 1.56±0.73 | 3.25±0.64*,# | 41.231 | <0.001 |
| T6 | 2.75±0.44 | 3.89±0.78* | 5.05±1.20*,# | 40.010 | <0.001 | |
| T7 | 2.46±0.58 | 3.22±0.67* | 4.65±0.88*,# | 43.012 | <0.001 | |
| T8 | 2.25±0.59 | 3.11±0.60* | 4.00±0.86*,# | 41.098 | <0.001 | |
| T9 | 1.96±0.58 | 2.78±0.44* | 3.75±1.02*,# | 40.190 | <0.001 | |
| T10 | 1.39±0.88 | 2.56±0.53* | 3.20±1.01* | 39.098 | <0.001 |
indicates P<0.05 vs. the SA group at the same time point;
indicates P<0.05 vs. the SC group at the same time point.
SA group: ultrasound-guided anterior quadratus lumborum block at the lateral supra-arcuate ligament group; SC group: ultrasound-guided subcostal anterior quadratus lumborum block group; GA group: general anesthesia-only group; T5: during extubation in the postoperative period; T6: upon transfer from the post-anesthesia care unit to the ward; T7: 6 hours after surgery; T8: 12 hours after surgery; T9: 24 hours after surgery; T10: 48 hours after surgery; VAS: Visual analog scale.
Figure 6.
Comparison of resting and active VAS scores among three groups at different time points. A: Comparison of resting VAS scores postoperatively among the three groups. B: Comparison of activity VAS scores postoperatively among the three groups. Notes: * indicates P<0.05 vs. the SA group at the same time point; # indicates P<0.05 vs. the SC group at the same time point. SA group: ultrasound-guided anterior quadratus lumborum block at the lateral supra-arcuate ligament group; SC group: ultrasound-guided subcostal anterior quadratus lumborum block group; GA group: general anesthesia-only group; VAS: Visual analog scale.
Comparison of intraoperative anesthetic drug dosages and total PCIA presses within 48 hours postoperatively
The intraoperative dosage of sufentanil was lower in both the SA and SC groups compared to the GA group (P<0.05), with no significant difference between the SA and SC groups (P>0.05). The SA group used less remifentanil than both the SC and GA groups (P<0.05), while no significant difference was found between the SC and GA groups (P>0.05). Similarly, propofol usage was lower in the SA and SC groups compared to the GA group (P<0.05), with the SA group using less than the SC group (P<0.05). Within 48 hours postoperatively, both the SA and SC groups recorded fewer total PCIA presses than the GA group, with the SA group showing the fewest (P<0.05, Table 5 and Figure 7).
Table 5.
Comparison of intraoperative anesthetic drug dosages and total presses of PCIA within 48 hours postoperatively among the three groups (x̅ ± s)
| Items | SA group (n=31) | SC group (n=31) | GA group (n=30) | χ2 | P value |
|---|---|---|---|---|---|
| Sufentanil (ug) | 39.29±6.04 | 45.56±7.27 | 52.75±14.73*,# | 43.009 | P<0.001 |
| Remifentanil (ug) | 1233.15±529.67 | 1612.22±223.26* | 1676.00±379.23* | 20.001 | 0.003 |
| Propofol (mg) | 444.57±80.36 | 552.22±62.81* | 719.50±168.035*,# | 42.019 | P<0.001 |
| Total presses of PCIA within 48 h postoperatively (times) | 5.79±3.43 | 8.33±1.50* | 11.60±2.33*,# | 8.910 | 0.039 |
indicates P<0.05 vs. the SA group at the same time point;
indicates P<0.05 vs. the SC group at the same time point.
SA group: ultrasound-guided anterior quadratus lumborum block at the lateral supra-arcuate ligament group; SC group: ultrasound-guided subcostal anterior quadratus lumborum block group; GA group: general anesthesia-only group; PCIA: Patient-controlled intravenous analgesia.
Figure 7.
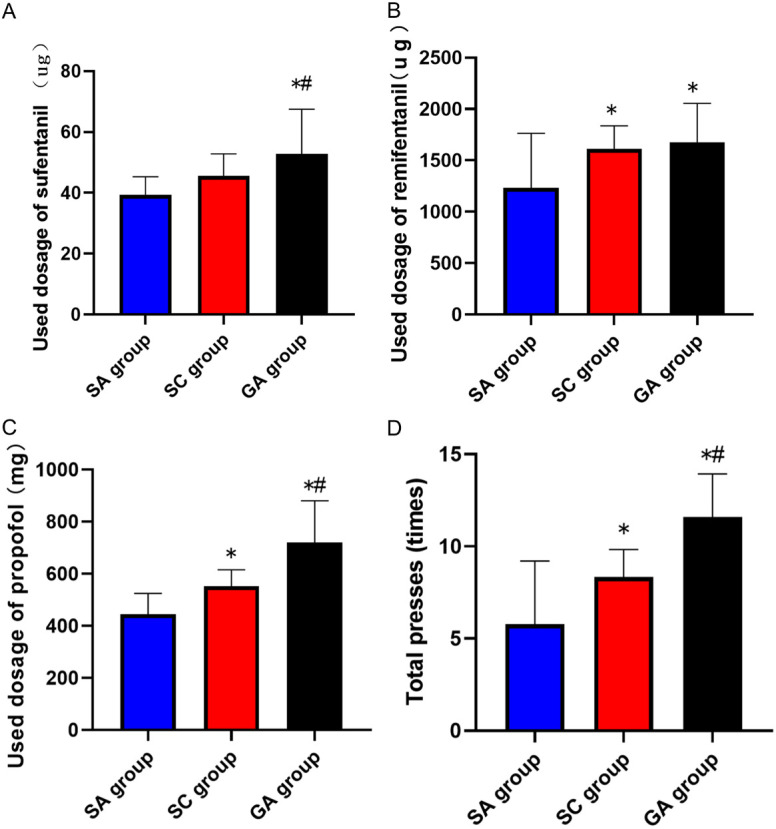
Comparison of intraoperative used dosages of anesthetic drug and postoperative analgesic presses among the three groups. A: Comparison of intraoperative used dosage of sufentanil among the three groups. B: Comparison of intraoperative used dosage of remifentanil among the three groups. C: Comparison of intraoperative used dosage of propofol among the three groups. D: Comparison of the total presses of PCIA within 48 hours postoperatively among the three groups. Notes: * indicates P<0.05 vs. the SA group at the same time point; # indicates P<0.05 vs. the SC group at the same time point. SA group: ultrasound-guided anterior quadratus lumborum block at the lateral supra-arcuate ligament group; SC group: ultrasound-guided subcostal anterior quadratus lumborum block group; GA group: general anesthesia-only group; PCIA: patient-controlled intravenous analgesia.
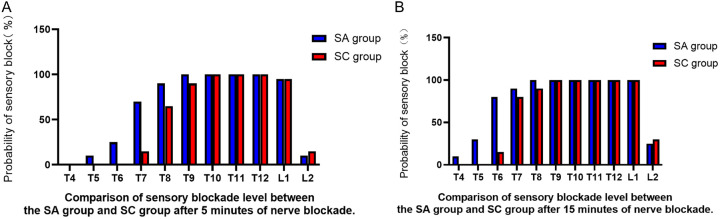
Comparison of sensory block levels at 5 minutes and 15 minutes after SA-AQLB and SC-AQLB
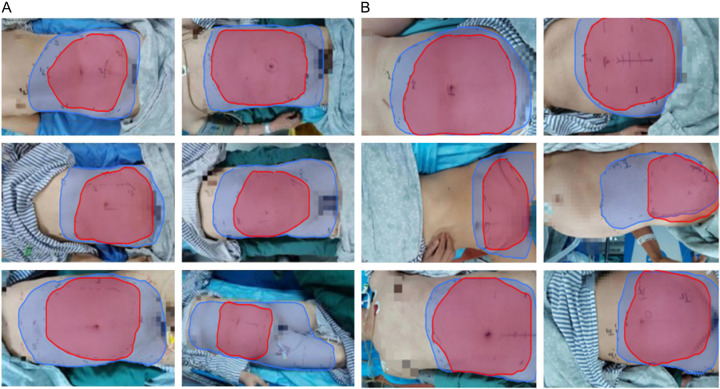
Five minutes after SA-AQLB, the highest sensory block level was at T5 and the lowest at L2. After 15 minutes, the highest and lowest levels were at T4 and L2, respectively. All patients achieved sensory block levels between T9-T12 and T8-L1 after 15 minutes. Following SC-AQLB, the highest and lowest sensory block levels at 5 minutes were at T7 and L2, respectively, and at T6 and L2 after 15 minutes. All patients reached sensory block levels between T10-T12 and T9-L1 within 5 minutes. The SA group exhibited significantly higher sensory block levels than the SC group (P<0.05, Figures 8 and 9).
Figure 8.
Sensory block levels at 5 minutes and 15 minutes after ultrasound-guided SA-AQLB (A) and SC-AQLB (B). (A) Sensory block levels at 5 minutes and 15 minutes after ultrasound-guided SA-AQLB. (B) Sensory block levels at 5 minutes and 15 minutes after SC-AQLB. Notes: The red area represents the block range at 5 minutes, and the blue area represents the block range at 15 minutes. SA-AQLB: Anterior quadratus lumborum block at the lateral supra-arcuate ligament; SC-AQLB: subcostal anterior quadratus lumborum block.
Figure 9.
Sensory block levels and probability maps of ultrasound-guided SA-AQLB and SC-AQLB. A: Comparison of sensory blockade level between the SA group and SC group after 5 minutes of nerve blockade. B: Comparison of sensory blockade level between the SA group and SC group after 15 minutes of nerve blockade. Notes: SA-AQLB: Anterior quadratus lumborum block at the lateral supra-arcuate ligament; SC-AQLB: subcostal anterior quadratus lumborum block.
Comparison of intraoperative usage of vasoactive medications among the three groups
Both the SA and SC groups used more ephedrine than the GA group (P<0.05), with the SA group using more than the SC group (P<0.05). No significant differences were noted in the use of anisodamine and landiolol across the three groups (P>0.05, Table 6).
Table 6.
Comparison of intraoperative usage of vasoactive medications among the three groups (x̅ ± s)
| Items | SA group (n=31) | SC group (n=31) | GA group (n=30) | χ2 | P value |
|---|---|---|---|---|---|
| Ephedrine (mg) | 6.0 (4.5, 10.5) | 3.0 (0.0, 12.0)* | 0.0 (0.0, 4.5)*,# | 17.901 | 0.030 |
| Anisodamine (mg) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.0 (0.0, 2.0) | 6.512 | 0.053 |
| Landirol (mg) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.401 | 0.378 |
indicates P<0.05 vs. the SA group at the same time point;
indicates P<0.05 vs. the SC group at the same time point.
SA group: ultrasound-guided anterior quadratus lumborum block at the lateral supra-arcuate ligament group; SC group: ultrasound-guided subcostal anterior quadratus lumborum block group; GA group: general anesthesia-only group.
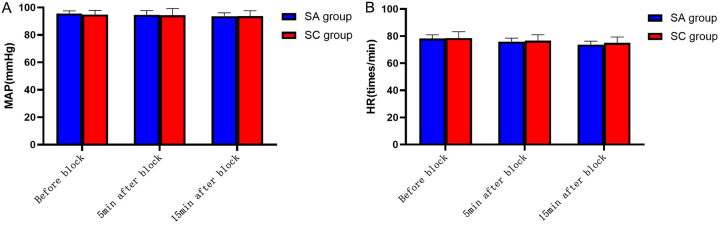
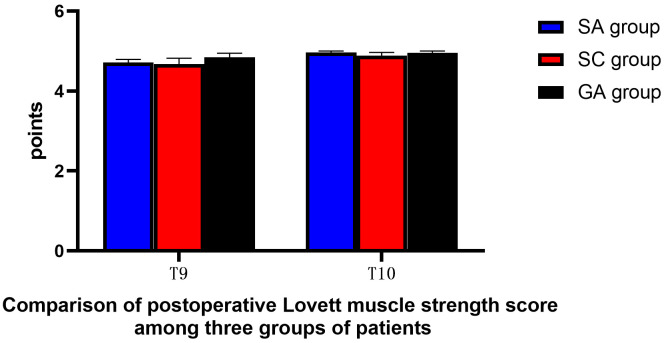
Comparison of postoperative Lovett muscle strength scores among the three groups
At T9 and T10, there were no significant differences in Lovett muscle strength scores among the three groups (both P>0.05, Table 7 and Figure 10).
Table 7.
Comparison of postoperative Lovett muscle strength scores among the three groups (x̅ ± s, score)
| Time | SA group (n=31) | SC group (n=31) | GA group (n=30) | χ2 | P value |
|---|---|---|---|---|---|
| T9 | 4.71±0.08 | 4.67±0.15 | 4.85±0.10 | 0.321 | 0.463 |
| T10 | 4.96±0.04 | 4.89±0.08 | 4.95±0.05 | 1.678 | 0.689 |
Notes: SA group: ultrasound-guided anterior quadratus lumborum block at the lateral supra-arcuate ligament group; SC group: ultrasound-guided subcostal anterior quadratus lumborum block group; GA group: general anesthesia-only group; T9: 24 hours after surgery; T10: 48 hours after surgery.
Figure 10.
Comparison of postoperative Lovett muscle strength scores among the three groups. Notes: T9: 24 hours after surgery; T10: 48 hours after surgery; SA group: ultrasound-guided anterior quadratus lumborum block at the lateral supra-arcuate ligament group; SC group: ultrasound-guided subcostal anterior quadratus lumborum block group; GA group: general anesthesia-only group.
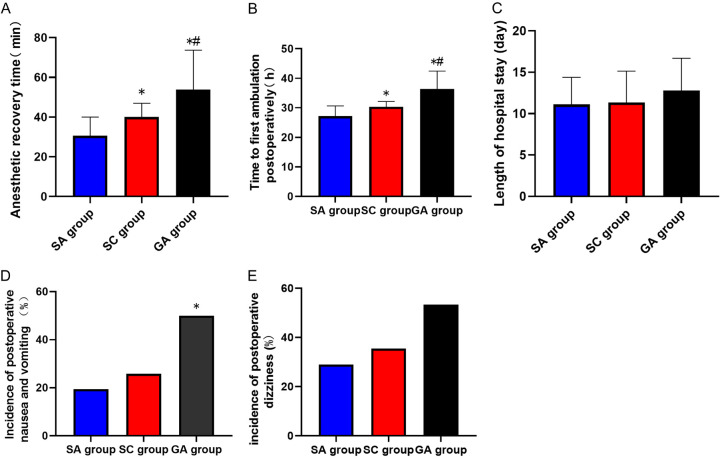
Comparison of anesthetic recovery time and early postoperative recovery outcomes among the three groups
The SA group had shorter anesthetic recovery times and earlier ambulation compared to the SC group, which in turn showed better outcomes than the GA group (both P<0.05). The incidence of postoperative nausea and vomiting was lower in the SA and SC groups compared to the GA group (P<0.05), but there was no significant difference between the SA and SC groups (P>0.05). No significant differences were observed in the length of hospital stay and incidence of postoperative dizziness among the groups (P>0.05). No complications such as pneumothorax, renal injury, or infection at the injection site were reported in any group (Table 8 and Figure 11).
Table 8.
Comparison of anesthetic recovery time and early postoperative recovery outcomes among the three groups (x̅ ± s)
| Items | SA group (n=31) | SC group (n=31) | GA group (n=30) | χ2 | P value |
|---|---|---|---|---|---|
| Anesthesia recovery time (min) | 30.61±9.43 | 40.11±6.88* | 53.80±17.21*,# | 43.009 | P<0.001 |
| Time to first ambulation (h) | 30.61±9.43 | 40.11±6.88* | 53.80±17.21*,# | 42.098 | P<0.001 |
| Length of hospital stay (d) | 26.18±3.48 | 30.33±1.80* | 36.35±6.08*,# | 41.098 | P<0.001 |
| Incidence of nausea and vomiting [n (%)] | 6 (19.35) | 8 (25.81) | 15 (50.00)*,# | 16.001 | 0.031 |
| Incidence of dizziness [n (%)] | 9 (29.03) | 11 (35.48) | 16 (53.33) | 0.298 | 0.261 |
indicates P<0.05 vs. the SA group at the same time point;
indicates P<0.05 vs. the SC group at the same time point.
SA group: ultrasound-guided anterior quadratus lumborum block at the lateral supra-arcuate ligament group; SC group: ultrasound-guided subcostal anterior quadratus lumborum block group; GA group: general anesthesia-only group.
Figure 11.
Comparison of anesthetic recovery time and early postoperative recovery outcomes among three groups. A: Comparison of anesthetic recovery time among three groups. B: Comparison of time to first ambulation among three groups. C: Comparison of length of hospital stay among three groups. D: Comparison of the incidence of postoperative nausea and vomiting among three groups. E: Comparison of the incidence of postoperative dizziness among three groups. Notes: * indicates P<0.05 vs. the SA group at the same time point; # indicates P<0.05 vs. the SC group at the same time point. SA group: ultrasound-guided anterior quadratus lumborum block at the lateral supra-arcuate ligament group; SC group: ultrasound-guided subcostal anterior quadratus lumborum block group; GA group: general anesthesia-only group.
Discussion
CRC is currently among the top five malignant tumors in China [31], with surgery playing a crucial role in its treatment. Laparoscopic radical resection of CRC often involves a midline approach, requiring navigation of a complex array of visceral structures. This complexity necessitates reducing general anesthesia dosage and enhancing postoperative pain management, presenting significant challenges for anesthesiologists. Commonly, a combination of ultrasound-guided nerve blocks and general anesthesia is employed in abdominal surgeries, with techniques such as the QLB and the transversus abdominis plane block (TAPB) being prevalent. TAPB is known to decrease adverse intraoperative stimuli, enhance perioperative analgesia, and stabilize hemodynamics [32]. However, QLB has been reported to offer more prolonged analgesia and a wider blockade area compared to TAPB [33].
Introduced by Blanco in 2007, QLB involves the injection of local anesthetics into or around the quadratus lumborum muscle, potentially extending into the paravertebral space to block various neural segments, thereby alleviating somatic pain [34-37]. The efficacy of this diffusion, however, is contingent on the volume and timing of the anesthetic used. The SC-AQLB, proposed by Elsharkawy in 2016, involves injecting anesthetics anterior to the quadratus lumborum, near the 12th rib at the L1-L2 level [38]. This method allows the anesthetic to spread cephalad beneath the arcuate ligament, reaching the lower paravertebral space behind the thoracic fascia. Nonetheless, the lateral arcuate ligament can impede complete diffusion into the paravertebral space, often limiting the block range to between T6 and L2 [13,39,40]. Moreover, distinguishing between the thoracolumbar fascia, anterior QL fascia, and posterior renal fascia on ultrasound can be challenging, occasionally leading to inaccurate injections and reduced block success rates [21,38].
Ultrasound-guided SA-AQLB, introduced by Professor Wang Y in 2020 [21], has yet to be extensively compared in clinical applications with other QLB approaches in elderly patients undergoing laparoscopic CRC surgery. Our study noted significantly more stable intraoperative and extubation hemodynamics in the SA group compared to the SC and GA groups, suggesting better analgesic effects and enhanced management of intraoperative anesthesia. The local anesthetic in SA-AQLB bypasses muscle fascia losses by directly traversing the arcuate ligament into the lower thoracic paravertebral space, enabling a broader spinal nerve and sympathetic trunk blockade, akin to a paravertebral nerve block. This extensive block not only provides effective analgesia but also mitigates the stress response from electrocautery during surgery [22-27]. Despite these advantages, patients in the SA group required higher ephedrine doses during surgery compared to those in the SC and GA groups. No significant differences were found in hemodynamic fluctuations post-block implementation between the SA and SC groups, underscoring the safety and efficacy of the supraarch lumbar quadratus muscle block. Furthermore, the SA group exhibited significantly lower dosages of sufentanil, remifentanil, and propofol, indicating stronger intraoperative analgesia. This potent analgesia contributed to shorter postoperative recovery times and no reported intraoperative awareness, ultimately enhancing surgical turnover rates.
VAS pain scores during extubation were significantly lower in the SA and SC groups compared to the GA group, with the SA group maintaining significantly reduced scores up to 48 hours postoperatively. This suggests that ultrasound-guided SA-AQLB not only diminishes pain intensity early postoperatively but also sustains long-lasting analgesia, echoing findings by Shi et al. [27]. Okmen et al. [41,42] reported that SC-AQLB, despite providing effective analgesia within the first 24 hours, tends to offer reduced pain control after this period due to the obstructive effect of the lateral arcuate ligament and the resultant anesthetic dispersion issues. This is consistent with our findings where the SC group showed improved VAS scores within 24 hours postoperatively compared to the GA group, but similar scores at the 48-hour mark.
Furthermore, the GA group exhibited significantly higher total PCIA presses than the SC group, implying that the timing of postoperative pain assessments may align with temporary analgesic interventions, providing only transient pain relief [43]. Postoperative follow-ups indicated that patients undergoing SA-AQLB typically experienced mild wound pain characterized by swelling, validating the efficacy of the analgesia.
This study confirmed that SA-AQLB achieves a block range from T5 to L2 within 5 minutes, narrowing slightly to T4 to L2 by 15 minutes, aligning with the onset, extent, and duration of analgesia documented by Professor Wang Y’s team [21]. Similarly, the initial block range for SC-AQLB was between T7 and L2, extending up to T6 to L2 after 15 minutes, as suggested by Elsharkawy [13]. The “QL triangle”, a critical anatomical target for SA-AQLB, is positioned between the diaphragm and QL muscle, adjacent to the lower thoracic paravertebral space. This strategic placement minimizes medication loss and enhances the spread towards the upper thoracic area, potentially blocking more thoracic spinal nerves, intercostal nerves, and sympathetic ganglia [21-24].
SA-AQLB’s fast onset, extensive coverage, and sustained analgesic effect make it highly suitable for various abdominal surgeries [26,27]. However, sensory blind spots in the bilateral rectus abdominis areas were noted in some cases, possibly due to the intricate nerve structures and embryonic layer cells around the umbilicus [44]. This highlights the complexity of achieving comprehensive sensory blockades and underscores the need for precise anatomical understanding and technique refinement in abdominal nerve blocks.
The time to first ambulation post-surgery was earlier in the SA and SC groups compared to the GA group, with the SA group achieving the earliest mobilization. This suggests that ultrasound-guided SA-AQLB effectively reduces postoperative pain, enhances patient comfort, promotes early mobilization, and accelerates patients’ recovery. However, no significant differences were observed in postoperative discharge times among the three groups, likely due to discharge criteria focusing primarily on the recovery of the anastomotic site in CRC patients. The integrity of the anastomotic site, which influences intestinal function and dietary resumption, directly impacts hospital stay duration.
Nausea and vomiting were less prevalent in the SA and SC groups compared to the GA group, likely due to reduced opioid use during surgery. The incidence of dizziness was similar across all groups, possibly influenced by the use of nabumetone in postoperative PCIA pumps. Despite concerns about postoperative quadriceps femoris weakness - a known complication of QLB - a recent study reported a 65% incidence following anterior QLB surgery [45]. In our study, no significant reduction in lower limb muscle strength was noted, which might be attributed to the lower concentration of local anesthetics used and the study’s relatively small sample size.
The typical dosage range for ropivacaine in QLB is 0.2 to 0.4 mL/kg of 0.2% to 0.5% ropivacaine, requiring careful consideration during bilateral blocks in elderly patients [46]. This study utilized 0.3 mL/kg of 0.4% ropivacaine for each preoperative nerve block in elderly CRC patients, achieving rapid onset and extensive spread of anesthesia. Local anesthetics’ slow absorption within the fascial plane contributes to prolonged postoperative analgesia. Throughout the study, no complications such as local anesthetic toxicity, allergies, pneumothorax, or renal injury were observed, underscoring the procedure’s safety.
The study’s limitations include a small sample size and single-time-point data collection, which may have introduced observational gaps. Furthermore, postoperative analgesia was uniformly administered using 50 μg of sufentanil, not tailored to individual body weight, potentially affecting the accuracy of postoperative pain assessments and other outcomes. The ice block method, used to gauge block level, might also vary in effectiveness due to individual temperature sensitivity differences.
In conclusion, general anesthesia combined with ultrasound-guided SA-AQLB provides superior outcomes to general anesthesia alone in elderly patients undergoing laparoscopic CRC surgery. This approach significantly reduces general anesthesia drug dosage, decreases postoperative pain, minimizes perioperative adverse events, and accelerates patient recovery.
Acknowledgements
This work was supported by 2021, 2022 Changsha Central Hospital Scientific Research Project (Nos. YNKY202102, YNKY202232); Hunan Medical Technology Innovation Guidance Project (No. 2021SK53404); and Natural Science Foundation of Changsha (No. kq2202046).
Disclosure of conflict of interest
None.
References
- 1.Xia C, Dong X, Li H, Cao M, Sun D, He S, Yang F, Yan X, Zhang S, Li N, Chen W. Cancer statistics in China and United States, 2022: profiles, trends, and determinants. Chin Med J (Engl) 2022;135:584–590. doi: 10.1097/CM9.0000000000002108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sato B, Kanda M, Tanaka C, Kobayashi D, Iwata N, Hattori N, Suenaga M, Hayashi M, Yamada S, Murotani K, Fujiwara M, Kodera Y. Significance of preoperative systemic inflammation score in short-term and long-term outcomes of patients with pathological T2-4 gastric cancer after radical gastrectomy. World J Surg. 2018;42:3277–3285. doi: 10.1007/s00268-018-4597-7. [DOI] [PubMed] [Google Scholar]
- 3.Boggett S, Chahal R, Griffiths J, Lin J, Wang D, Williams Z, Riedel B, Bowyer A, Royse A, Royse C. A randomised controlled trial comparing deep neuromuscular blockade reversed with sugammadex with moderate neuromuscular block reversed with neostigmine. Anaesthesia. 2020;75:1153–1163. doi: 10.1111/anae.15094. [DOI] [PubMed] [Google Scholar]
- 4.Blanco R, Ansari T, Riad W, Shetty N. Quadratus lumborum block versus transversus abdominis plane block for postoperative pain after cesarean delivery: a randomized controlled trial. Reg Anesth Pain Med. 2016;41:757–762. doi: 10.1097/AAP.0000000000000495. [DOI] [PubMed] [Google Scholar]
- 5.Cui XL, Li X, Li MN, Zhang YL, Xie Y, Yan WG, Zhang YS, Ji ZG, Huang YG. Ultrasound-guided transmuscular quadratus lumbar block reduces opioid consumption after laparoscopic partial nephrectomy. Chin Med Sci J. 2020;35:289–296. doi: 10.24920/003759. [DOI] [PubMed] [Google Scholar]
- 6.Li J, Wei C, Huang J, Li Y, Liu H, Liu J, Jin C. Efficacy of quadratus lumborum block for pain control in patients undergoing hip surgeries: a systematic review and meta-analysis. Front Med (Lausanne) 2021;8:771859. doi: 10.3389/fmed.2021.771859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shahid Z, Burns B. Anatomy, abdomen and pelvis: diaphragm. StatPearls. Treasure Island (FL) ineligible companies; Disclosure: Bracken Burns declares no relevant financial relationships with ineligible companies.: StatPearls Publishing Copyright © 2024, StatPearls Publishing LLC.; 2024. [PubMed] [Google Scholar]
- 8.Kokatnur L, Vashisht R, Rudrappa M. Diaphragm disorders. StatPearls. Treasure Island (FL) ineligible companies; Disclosure: Rishik Vashisht declares no relevant financial relationships with ineligible companies. Disclosure: Mohan Rudrappa declares no relevant financial relationships with ineligible companies.: StatPearls Publishing Copyright © 2024, StatPearls Publishing LLC.; 2024. [Google Scholar]
- 9.Dam M, Moriggl B, Hansen CK, Hoermann R, Bendtsen TF, Børglum J. The pathway of injectate spread with the transmuscular quadratus lumborum block: a cadaver study. Anesth Analg. 2017;125:303–312. doi: 10.1213/ANE.0000000000001922. [DOI] [PubMed] [Google Scholar]
- 10.Tamura T, Yokota S, Ito S, Shibata Y, Nishiwaki K. Local anesthetic spread into the paravertebral space with two types of quadratus lumborum blocks: a crossover volunteer study. J Anesth. 2019;33:26–32. doi: 10.1007/s00540-018-2578-5. [DOI] [PubMed] [Google Scholar]
- 11.Chen Q, Liang C, Liang J, Qiu J, Yang B. An image study on local anesthetic spread in healthy volunteers receiving subcostal exterior semilunaris transversus abdominis plane (SE-TAP) block. J Pain Res. 2021;14:2013–2019. doi: 10.2147/JPR.S316582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Colli Neto JA, Udelsmann A, Barreto G, Tincani AJ. Experimental model for local anesthetic spread in spinal anesthesia: application to medical education. Braz J Anesthesiol. 2022;72:428–431. doi: 10.1016/j.bjane.2021.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Elsharkawy H, Ahuja S, DeGrande S, Maheshwari K, Chan V. Subcostal approach to anterior quadratus lumborum block for pain control following open urological procedures. J Anesth. 2019;33:148–154. doi: 10.1007/s00540-018-02605-1. [DOI] [PubMed] [Google Scholar]
- 14.Diwan S, Blanco R, Kulkarni M, Patil A, Nair A. The supine coronal midaxillary approach to anterior quadratus lumborum block: case report. Braz J Anesthesiol. 2020;70:443–447. doi: 10.1016/j.bjane.2020.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahmed A, Fawzy M, Nasr MAR, Hussam AM, Fouad E, Aboeldahb H, Saad D, Osman S, Fahmy RS, Farid M, Waheb MM. Ultrasound-guided quadratus lumborum block for postoperative pain control in patients undergoing unilateral inguinal hernia repair, a comparative study between two approaches. BMC Anesthesiol. 2019;19:184. doi: 10.1186/s12871-019-0862-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mitchell KD, Smith CT, Mechling C, Wessel CB, Orebaugh S, Lim G. A review of peripheral nerve blocks for cesarean delivery analgesia. Reg Anesth Pain Med. 2019 doi: 10.1136/rapm-2019-100752. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li H, Shi R, Shi D, Wang R, Liu Y, Wang Y. Anterior quadratus lumborum block at the lateral supra-arcuate ligament versus transmuscular quadratus lumborum block for postoperative analgesia in patients undergoing laparoscopic nephrectomy: a randomized controlled trial. J Clin Anesth. 2021;75:110561. doi: 10.1016/j.jclinane.2021.110561. [DOI] [PubMed] [Google Scholar]
- 18.Lu Y, Zhang J, Xu X, Chen W, Zhang S, Zheng H, Xia Y, Papadimos TJ, Xu X, Chen H. Sensory assessment and block duration of transmuscular quadratus lumborum block at L2 versus L4 in volunteers: a randomized controlled trial. Minerva Anestesiol. 2019;85:1273–1280. doi: 10.23736/S0375-9393.19.13656-5. [DOI] [PubMed] [Google Scholar]
- 19.Wikner M. Unexpected motor weakness following quadratus lumborum block for gynaecological laparoscopy. Anaesthesia. 2017;72:230–232. doi: 10.1111/anae.13754. [DOI] [PubMed] [Google Scholar]
- 20.Li H, Liang J, Shao P, Zheng J, Shi R, Wang Y. Supra-arcuate ligament blocks: anatomy, mechanisms, and techniques. J Pain Res. 2021;14:3837–3848. doi: 10.2147/JPR.S347071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li H, Ma D, Liu Y, Wang Y. A transverse approach for ultrasound-guided anterior quadratus lumborum block at the lateral supra-arcuate ligament. Anaesthesia. 2020;75:1400–1401. doi: 10.1111/anae.15058. [DOI] [PubMed] [Google Scholar]
- 22.Hussain N, Brull R, Speer J, Hu LQ, Sawyer T, McCartney CJL, Abdallah FW. Analgesic benefits of the quadratus lumborum block in total hip arthroplasty: a systematic review and meta-analysis. Anaesthesia. 2022;77:1152–1162. doi: 10.1111/anae.15823. [DOI] [PubMed] [Google Scholar]
- 23.Koschwanez HE, Broadbent E. The use of wound healing assessment methods in psychological studies: a review and recommendations. Br J Health Psychol. 2011;16:1–32. doi: 10.1348/135910710X524633. [DOI] [PubMed] [Google Scholar]
- 24.Liu X, Song T, Chen X, Zhang J, Shan C, Chang L, Xu H. Quadratus lumborum block versus transversus abdominis plane block for postoperative analgesia in patients undergoing abdominal surgeries: a systematic review and meta-analysis of randomized controlled trials. BMC Anesthesiol. 2020;20:53. doi: 10.1186/s12871-020-00967-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wu Z, Wang Y. Development of guidance techniques for regional anesthesia: past, present and future. J Pain Res. 2021;14:1631–1641. doi: 10.2147/JPR.S316743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li H, Shi R, Wang Y. A modified approach below the lateral arcuate ligament to facilitate the subcostal anterior quadratus lumborum block. J Pain Res. 2021;14:961–967. doi: 10.2147/JPR.S306696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shi R, Li H, Wang Y. Dermatomal coverage of single-injection ultrasound-guided parasagittal approach to anterior quadratus lumborum block at the lateral supra-arcuate ligament. J Anesth. 2021;35:307–310. doi: 10.1007/s00540-021-02903-1. [DOI] [PubMed] [Google Scholar]
- 28.Guo T, Xie L, Zhao J, Song W, Dai W, Liu F, Zheng Y, Xu Y. Trend analysis of morbidity and mortality of colorectal cancer in China from 1988 to 2009. Zhonghua Wei Chang Wai Ke Za Zhi. 2018;21:33–40. [PubMed] [Google Scholar]
- 29.Tan HS, Taylor C, Weikel D, Barton K, Habib AS. Quadratus lumborum block for postoperative analgesia after cesarean delivery: a systematic review with meta-analysis and trial-sequential analysis. J Clin Anesth. 2020;67:110003. doi: 10.1016/j.jclinane.2020.110003. [DOI] [PubMed] [Google Scholar]
- 30.Elsharkawy H, Ahuja S, Sessler DI, Maheshwari K, Mao G, Sakr Esa WA, Soliman LM, Ayad S, Khoshknabi D, Khan MZ, Raza S, DeGrande S, Turan A. Subcostal anterior quadratus lumborum block versus epidural block for analgesia in open nephrectomy: a randomized clinical trial. Anesth Analg. 2021;132:1138–1145. doi: 10.1213/ANE.0000000000005382. [DOI] [PubMed] [Google Scholar]
- 31.Kondo A, Okano K, Kumamoto K, Kobara H, Nagahara T, Wato M, Shibatoge M, Minato T, Masaki T, Suzuki Y Kagawa Gastroenterology Forum. Surgical management and outcomes of obstructive colorectal cancer in elderly patients: a multi-institutional retrospective study. Surgery. 2022;172:60–68. doi: 10.1016/j.surg.2021.12.007. [DOI] [PubMed] [Google Scholar]
- 32.Wang D, Liao C, Tian Y, Zheng T, Ye H, Yu Z, Jiang J, Su J, Chen S, Zheng X. Analgesic efficacy of an opioid-free postoperative pain management strategy versus a conventional opioid-based strategy following open major hepatectomy: an open-label, randomised, controlled, non-inferiority trial. EClinicalMedicine. 2023;63:102188. doi: 10.1016/j.eclinm.2023.102188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Milone M, Di Minno MN, Musella M, Maietta P, Salvatore G, Iacovazzo C, Milone F. Outpatient inguinal hernia repair under local anaesthesia: feasibility and efficacy of ultrasound-guided transversus abdominis plane block. Hernia. 2013;17:749–755. doi: 10.1007/s10029-012-1022-2. [DOI] [PubMed] [Google Scholar]
- 34.Blanco R. 271. Tap block under ultrasound guidance: the description of a “no pops” technique. Reg Anesth Pain Med. 2007;32:130. [Google Scholar]
- 35.Adhikary SD, El-Boghdadly K, Nasralah Z, Sarwani N, Nixon AM, Chin KJ. A radiologic and anatomic assessment of injectate spread following transmuscular quadratus lumborum block in cadavers. Anaesthesia. 2017;72:73–79. doi: 10.1111/anae.13647. [DOI] [PubMed] [Google Scholar]
- 36.Chin KJ, Lirk P, Hollmann MW, Schwarz SKW. Mechanisms of action of fascial plane blocks: a narrative review. Reg Anesth Pain Med. 2021;46:618–628. doi: 10.1136/rapm-2020-102305. [DOI] [PubMed] [Google Scholar]
- 37.Balocco AL, López AM, Kesteloot C, Horn JL, Brichant JF, Vandepitte C, Hadzic A, Gautier P. Quadratus lumborum block: an imaging study of three approaches. Reg Anesth Pain Med. 2021;46:35–40. doi: 10.1136/rapm-2020-101554. [DOI] [PubMed] [Google Scholar]
- 38.Elsharkawy H. Quadratus lumborum block with paramedian sagittal oblique (subcostal) approach. Anaesthesia. 2016;71:241–242. doi: 10.1111/anae.13371. [DOI] [PubMed] [Google Scholar]
- 39.Elsharkawy H, Bajracharya GR, El-Boghdadly K, Drake RL, Mariano ER. Comparing two posterior quadratus lumborum block approaches with low thoracic erector spinae plane block: an anatomic study. Reg Anesth Pain Med. 2019 doi: 10.1136/rapm-2018-100147. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 40.Zhu M, Qi Y, He H, Lou J, Pei Q, Mei Y. Analgesic effect of the ultrasound-guided subcostal approach to transmuscular quadratus lumborum block in patients undergoing laparoscopic nephrectomy: a randomized controlled trial. BMC Anesthesiol. 2019;19:154. doi: 10.1186/s12871-019-0825-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ökmen K, Metin Ökmen B, Topal S. Ultrasound-guided posterior quadratus lumborum block for postoperative pain after laparoscopic cholecystectomy: a randomized controlled double blind study. J Clin Anesth. 2018;49:112–117. doi: 10.1016/j.jclinane.2018.06.027. [DOI] [PubMed] [Google Scholar]
- 42.Gu B, Zhou H, Lian Y, Zhou Y, He S, Xie K, Jiang H. Ultrasound-guided anterior quadratus lumborum block at lateral supra-arcuate ligament vs. thoracic epidural analgesia after open liver surgery: a randomized, controlled, noninferiority trial. J Am Coll Surg. 2022;235:871–878. doi: 10.1097/XCS.0000000000000354. [DOI] [PubMed] [Google Scholar]
- 43.Mao Y, Zhao W, Hao M, Xing R, Yan M. Ultrasound-guided quadratus lumborum block at the lateral supra-arcuate ligament versus subcostal transversus abdominis plane block for postoperative analgesia following open hepatectomy: a randomized controlled trial. J Pain Res. 2023;16:1429–1440. doi: 10.2147/JPR.S404810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cui XL, Li X, Li MN, Zhang YL, Xie Y, Yan WG, Zhang YS, Ji ZG, Huang YG. Ultrasound-guided transmuscular quadratus lumbar block reduces opioid consumption after laparoscopic partial nephrectomy. Chin Med Sci J. 2020;35:289–296. doi: 10.24920/003759. [DOI] [PubMed] [Google Scholar]
- 45.Ueshima H, Hiroshi O. RETRACTED: Incidence of lower-extremity muscle weakness after quadratus lumborum block. J Clin Anesth. 2018;44:104. doi: 10.1016/j.jclinane.2017.11.020. [DOI] [PubMed] [Google Scholar]
- 46.Wang J, Zhao G, Song G, Liu J. The efficacy and safety of local anesthetic techniques for postoperative analgesia after cesarean section: a bayesian network meta-analysis of randomized controlled trials. J Pain Res. 2021;14:1559–1572. doi: 10.2147/JPR.S313972. [DOI] [PMC free article] [PubMed] [Google Scholar]