Abstract
Background
Complementary and alternative medicine (CAM) use is common in inflammatory bowel disease (IBD) patients and impacts compliance with conventional treatment. Gastroenterologists should understand the motivational factors of CAM use—factors that push patients away from standard therapy or pull towards CAM. Our study describes the motivations behind CAM use for IBD and evaluates differences between Crohn’s disease (CD) and ulcerative colitis (UC) patients.
Methods
Retrospective cohort survey of patients over 18 years old with IBD, evaluated by gastroenterologists at a tertiary care referral centre from January 1 to December 31, 2019. Only patients who reported CAM use were included. Chi-square and independent t-tests were performed and P-value <0.05 was significant.
Results
Of the 230 completed surveys, 193 reported CAM use (CD: 57.5% vs UC: 42.5%). Demographics, disease duration, and hospitalizations were similar, but CD patients had lower SIBDQ scores (CD: 48.1 vs UC: 53.5, P < 0.001). Both groups were largely influenced by their social network to use CAM (CD: 33% vs UC: 31.3%) and did not feel well informed about CAM (87.4%). CD and UC patients had similar push and pull factors. Push factors included lack of improvement (39%) and side effects (20%) with conventional treatment. Pull factors included the desire for a holistic approach (21%) and to improve mood (35%). UC patients wanted a natural approach to treat their IBD, which nearly reached significance (P = 0.049). Most patients hoped fatigue 62.7%, and diarrhoea 61.7% would improve with CAM, but more CD patients wanted to improve their appetite (P = 0.043).
Conclusion
Despite differences in QoL, push and pull motivations for CAM use did not differ between CD and UC patients. Most users do not feel well informed of CAM and ongoing dialogue is important for patient-centred care.
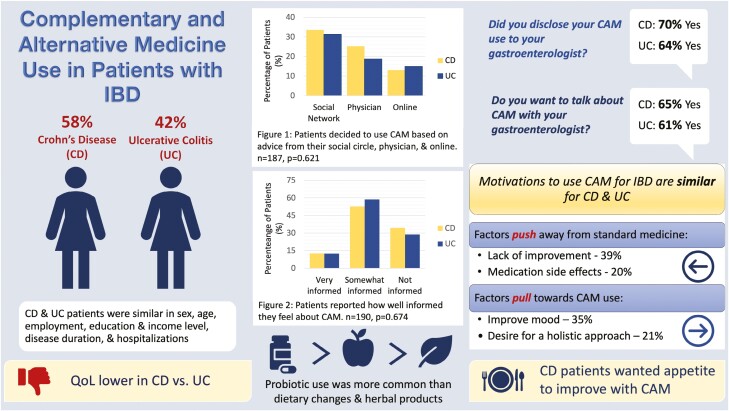
Graphical Abstract
Graphical Abstract.
Introduction
Inflammatory bowel disease (IBD) is an immune-mediated, chronic disease with a relapsing and remitting pattern characterized by abdominal pain, diarrhoea, and rectal bleeding. It may negatively impact quality of life (QoL) and require hospitalization and surgery.1 While treatment targets have evolved and newer advanced therapies are approved, patients focus on symptom management and improvement in QoL.1
The WHO defines complementary and alternative medicine (CAM) as “…a broad set of health care practices that are not part of a country’s own tradition nor part of conventional medicine, and are not fully integrated into the dominant healthcare system.”2 CAM is especially prevalent in patients with chronic disease, but given the variety of therapies and practices that are considered CAM, it is challenging to evaluate the motivations behind its use.3,4
Canada has one of the highest rates of CAM use, 21%–56%5–7 and British Columbia, has increasingly positive attitudes toward natural therapies compared to other provinces.8 Globally, 40%–50% of IBD patients use CAM and 18%–33% use CAM specifically for IBD.5,7,9,10 Predictors of CAM use in the general population include female gender, higher income, and urban dwelling.7,11 Initial enquiries identified various motivations behind CAM use, which are characterized as push or pull factors in this current study. Push & pull factors are an extension of Lee’s theory of physician migration and have been applied to physician, nurse, and medical trainee career choice, as well as patient healthcare utilization.12,13 Broadly, negative forces push patients away from their current situation or treatment and positive forces pull towards a new destination or treatment.14 Portela et al. were the first to characterize push and pull factors involved in CAM use by patients with IBD.11Push factors, which include side effects or dissatisfaction with standard care, push patients away from conventional treatment; whereas pull factors, such as the desire to have a holistic or natural approach, pull patients towards CAM.11 Earlier literature evaluates these factors using a broad characterization of CAM and not for IBD specifically.
The literature on specific CAM therapies is sparse, creating issues around safety and efficacy. Similarly, CAM may interact or impact compliance with standard treatment.5,11,15 It is imperative that gastroenterologists understand the motivations behind CAM use for IBD as addressing CAM use is integral to patient-centred care and improves outcomes.16 The primary aim of this study is to identify the push and pull factors that drive patients to use CAM for IBD.
Materials and methods
Study design
This survey-based, retrospective cohort study was conducted at the Pacific Gastroenterology Associates tertiary care, referral, outpatient clinic located in Vancouver, British Columbia and included patients with a diagnosis of IBD that were seen by a gastroenterologist between January 1, 2019 to December 31, 2019. The patients had consented to be contacted via email for future research.
Patients who met the inclusion criteria were notified by email with a detailed description of the study and a link to the survey. Prior to accessing the survey, the description clearly stated that completion of the survey provided consent to have their responses used for the study. Data from all attempted surveys was stored and electronically extracted from Qualtrics, a secure survey tool available for research through the University of British Columbia. Quality of Life (QoL) was assessed using the Short IBD Questionnaire (SIBDQ), a licensed, 10 question survey validated in both UC and CD patients that scores on bowel, systemic, social, and emotional domains.17 Each question contains a 7-point scale and a cut-off of <50 was used to define poor QoL. Ethics approval was obtained through the University of British Columbia Research Ethics Board.
Inclusion/exclusion criteria
Patients met inclusion criteria if they were 18 years or older, diagnosed with IBD, and evaluated at the Pacific Gastroenterology Associates tertiary care clinic between January 1, 2019 and December 31, 2019. Patients had provided consent for email correspondence for research purposes. Due to delays in study and license approval during the COVID pandemic, the survey was sent to patients in August 2022. Patients were excluded if they did not meet the above criteria and if they did not return the survey or returned an incomplete survey. A completed survey required 70% completion of the questions, which included the completed SIBDQ and demographics.
Data extraction and definitions
Patients meeting the inclusion criteria had the following demographic data collected in the survey: age, sex, education, employment, income, disease duration, current medication prescribed for IBD, surgical history, IBD-related hospitalizations and SIBDQ score. Participants were asked if they were currently taking medication for their IBD, which included steroids, 5-ASA products, azathioprine, methotrexate, infliximab, adalimumab, vedolizumab, ustekinumab, and tofacitinib. Participants chose predefined survey answers with a free text option if their answer were not available.
Questions about use of CAM were drawn from a national health survey on the use of Complementary and Alternative Medicine by Canadians.8 CAM was characterized as dietary changes, natural supplements/herbal products, mental health services, and alternative healthcare services. Specific therapies, including herbal products, were chosen for the survey-based on previous reviews on the efficacy and potential mechanism of individual CAM therapies in IBD.15,18,19 Patients were given the option to report additional types of CAM used for IBD, ensuring patients who used non-listed CAM therapies were included in the study. CAM use was determined by asking participants ‘Have you ever used the following therapies for your IBD specifically?’ and the available answers were gluten-free diet, anti-inflammatory diet, other dietary changes, probiotics, curcumin, Andrographis paniculata (Indian Echinacea), Boswellia serrate (Indian frankincense), Artemesia absinthium (wormwood), Cannabis, other herbal formulas, Cognitive Behavioural Therapy, Acupuncture and other. The “other” option provided a free text box to input CAM products or services that were not specifically listed. For each chosen answer, participants were asked to report the IBD symptom(s) that the CAM product or service was used for. The survey asked about monthly expenditure on CAM, motivations for use, source of information, degree of CAM knowledge, and disclosure to their gastroenterologist.
Data analysis
Data was extracted from Qualtrics and analyzed using SPSS 27. Participants were separated and compared based on their IBD type, CD or UC. Continuous variables were described using median, mean, standard deviation, and minimum/maximum values when applicable. Categorical variables were described using absolute frequencies and analyzed using cross tabulations and chi-square test. A significance level of 5% was used for all tests.
Results
Excluded patients
The survey was sent to 910 participants; 11 emails bounced and there were 2 duplicate emails. 293 surveys were started and 253 surveys were submitted. Of these, 230 surveys were completed and 193 patients reported CAM use.
Study demographics
Of the CAM users, 57.5% (111/193) had CD and 42.5% (82/193) had UC. There was no difference in the mean age, sex, education level, employment, income, disease duration, and hospitalizations between the phenotypes (Table 1). CD patients scored lower on the SIBDQ (CD:48.1 vs UC:53.5 P < 0.001), had a greater number of surgeries (CD: 73, 65%, vs UC: 11, 13%, P < 0.001), and increased use of immunosuppression (CD: 9.9% vs UC: 2.4%, P = 0.041) and anti-TNF biologics (CD: 35.1% vs UC 15.9%, P < 0.001) (Table 2). UC patients had a significantly higher rate of 5-ASA derivatives (CD: 9.9% vs UC 37.8%, P < 0.001) (Table 2).
Table 1.
Study demographics of IBD patients that use CAM.
| Gender, n = 193 (%) | |
| Male | 79 (40.9) |
| Female | 113 (58.5) |
| Prefer not to say | 1 (0.9) |
| Age, mean, n = 193 | 46.8 ± 15.8 |
| Employment status, n = 192 (%) | |
| Full time | 101 (52.6) |
| Part time | 16 (10.0) |
| Student | 6 (3.0) |
| Not working | 43 (22.4) |
| Other | 26 (13.5) |
| Education n = 192 (%) | |
| No post-secondary | 20 (10.4) |
| Some post-secondary | 71 (37.0) |
| University | 101 (52.6) |
| Income n = 189 (%) | |
| <40,000 | 45 (23.8) |
| 40-59 000 | 35 (18.5) |
| 60-79 000 | 32 (16.9) |
| >80 000 | 77 (40.7) |
Table 2.
Disease history of IBD patients that use CAM.
| Disease duration n = 193 (%) | |
| <12 months | 1 (1.2) |
| 1-5 years | 18 (9.0) |
| 6-10 years | 45 (23.3) |
| 11-20 years | 71 (36.8) |
| >20 years | 58 (30.1) |
| Medical therapy n = 193 (%) | |
| Steroids (n = 191) | 9 (5.0) |
| 5-ASA derivatives | 42 (21.8) |
| Azathioprine/methotrexate | 9 (5.0) |
| Anti-TNF | 52 (26.9) |
| Newer agents | 79 (40.9) |
| Combination | 6 (3.0) |
| No advanced therapy | 50 (25.9) |
| Hospitalizations n = 158 (%) | |
| None | 51 (32.3) |
| Within past month | 1 (1.0) |
| Within past 12 months | 4 (3.0) |
| Within past 5 years | 36 (22.8) |
| Within past 10 years | 66 (41.8) |
| Surgeries n = 193 (%) | |
| None | 109 (56.5) |
| 1 | 63 (32.6) |
| 2 | 9 (4.6) |
| 3 or more | 12 (10.8) |
Types of CAM use
Overall, probiotics and dietary changes were the most commonly used CAM by IBD patients (Table 3), however, there was no statistical difference between the use of a gluten-free diet, anti-inflammatory diet, probiotics, curcumin, herbal products, cannabis, cognitive behavioural therapy, and acupuncture between the CD and UC groups (Table 3). There was a numerical trend towards increased Cannabis use by CD compared to UC patients (CD: 42, 37.8% vs UC:21 25.6%, P = 0.073). Herbal products were used the least (Table 3).
Table 3.
Characteristics of CAM use.
| CD | UC | P-value | |
|---|---|---|---|
| Have you ever used the following therapies for your IBD? n = 193 (%) | |||
| Gluten-free diet | 44 (39.6) | 36 (43.9) | 0.552 |
| Anti-inflammatory diet | 51 (45.9) | 34 (41.5) | 0.535 |
| Other diet | 53 (47.7) | 37 (45.1) | 0.718 |
| Probiotics | 70 (63.1) | 57 (69.5) | 0.35 |
| Curcumin | 21 (18.9) | 24 (29.3) | 0.093 |
| Andrographis paniculata | 0 | 0 | |
| Boswellia serrate | 4 (3.6) | 3 (3.7) | 0.984 |
| Artemisia absinthium | 5 (4.5) | 0 | 0.052 |
| Cannabis | 42 (37.8) | 21 (25.6) | 0.073 |
| Other herbal formula | 17 (15.3) | 18 (22.0) | 0.237 |
| Cognitive behavioural therapy | 20 (18.0) | 12 (14.6) | 0.532 |
| Acupuncture | 28 (25.2) | 18 (22.0) | 0.598 |
| Other | 25 (22.5) | 16 (19.5) | 0.613 |
| What are the reasons for using CAM? n = 193 (%) | |||
| Conventional medicine did not make me feel better | 46 (41.4) | 29 (35.4) | 0.392 |
| Conventional medicine will not cure my disease | 24 (21.6) | 14 (17.1) | 0.432 |
| Side effects of conventional medicine | 22 (19.8) | 17 (20.7) | 0.876 |
| Final hope | 15 (13.5) | 11 (13.4) | 0.984 |
| Fear of surgery | 20 (18.0) | 9 (11.0) | 0.176 |
| Want to use natural approach | 17 (15.3) | 22 (26.8) | 0.049 |
| Want to use holistic approach | 22 (19.8) | 18 (22.0) | 0.718 |
| Improve mood | 41 (36.9) | 26 (31.7) | 0.451 |
| Other | 47 (42.3) | 30 (36.6) | 0.419 |
| What symptoms were you hoping would improve with CAM? n = 193 (%) | |||
| Abdominal pain | 69 (62.2) | 43 (52.4) | 0.176 |
| Diarrhoea | 64 (57.7) | 55 (67.1) | 0.184 |
| Fatigue | 72 (64.9) | 49 (59.8) | 0.468 |
| Appetite | 28 (25.2) | 11 (13.4) | 0.043 |
| Weight loss | 24 (21.6) | 14 (17.1) | 0.432 |
| Other | 34 (30.6) | 21 (25.6) | 0.445 |
Motivations for CAM use
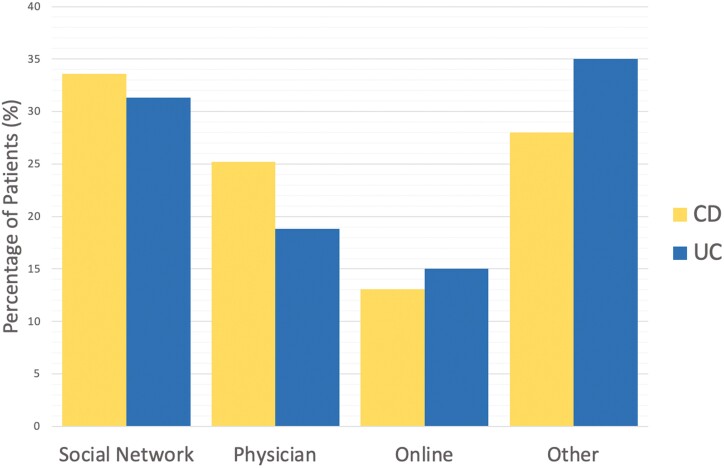
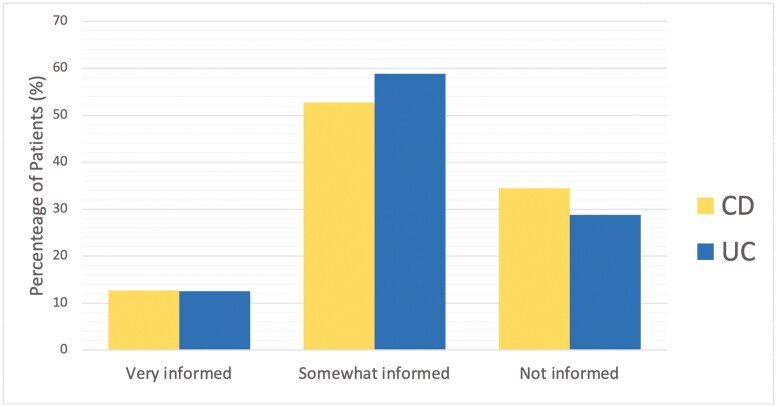
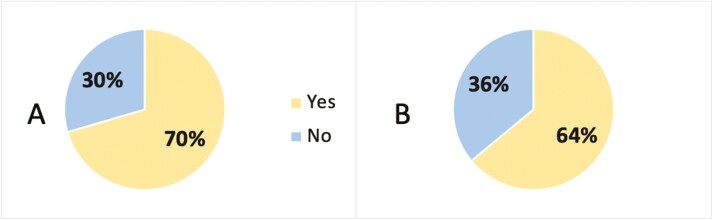
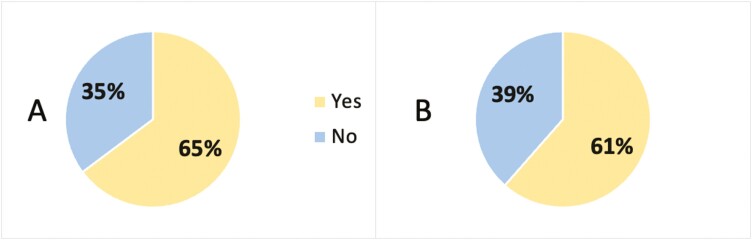
Both groups primarily decided to use CAM based on advice from a colleague, friend, or family member (CD:33% vs UC:31.3%, P = 0.621, Figure 1). CAM users did not feel well informed of CAM therapies (166, 87.4%, P = 0.674, Figure 2), but the majority of participants disclosed their CAM use (CD:74, 70.5% vs UC:48, 64%, P = 0.359, Figure 3) and wanted to discuss CAM (CD: 68, 64.8% vs UC: 48, 61.5%, 0.654, Figure 4) with their gastroenterologist. CD and UC patients had similar push and pull motivational factors; although, nearing significance, more UC patients wanted a natural approach (P = 0.049, Table 3). Push factors included side effects, fear of surgery and that standard medical treatment did not make them feel better and would not cure their disease. Pull factors included the desire to use a holistic approach and to improve mood (Table 3). The primary symptoms that IBD patients wanted to improve with CAM were fatigue 62.7% (121/193), diarrhoea 61.7% (119/193), and abdominal pain 58.0% (112/193), but more CD patients hoped appetite (P = 0.043) would improve (Table 3).
Figure 1.
Percentage of patients that decided to use CAM based on advice from their social circle, physician, online, or other, n = 187, P = 0.621; CD = Crohn’s disease; UC = ulcerative colitis.
Figure 2.
Patients reported how well informed they feel about CAM, n = 190, P = 0.674; CD = Crohn’s disease; UC = ulcerative colitis.
Figure 3.
Percentage of CD and UC patients that disclosed CAM use to their gastroenterologist, n = 180, P = 0.359. (A) = Crohn’s disease; (B) = Ulcerative colitis.
Figure 4.
Percentage of CD and UC patients that wanted to discuss CAM with their gastroenterologist, n = 183, P = 0.654. (A) = Crohn’s disease; (B) = Ulcerative colitis.
Discussion
Motivations
Our study demonstrates that both push and pull factors are responsible for CAM use by IBD patients, to address their condition. The lack of improvement in symptoms with conventional medicine—a push factor—was the most common motivation. This is similar to earlier studies demonstrating lack of efficacy and side effects of conventional treatment as main drivers of CAM use.5,6,11 Improving mood, a pull factor, was the second most common motivation and patients with IBD have increased rates of psychiatric comorbidities.20–22
Both groups used CAM to improve abdominal pain, diarrhoea, and fatigue, similar to an earlier Canadian study, that used a broader definition of CAM.23 Diarrhoea and pain are expected to improve before endoscopic inflammation with treatment and may reflect suboptimal efficacy of medical treatment, or co-existing conditions. Assessment of CAM use may optimize care by identifying persistent symptoms.
Type of CAM use
There was no significant difference in the type of CAM used between CD and UC patients. Similarly, the Manitoba IBD Cohort Study found no significant difference between the IBD phenotypes.7 In the present study, dietary changes and probiotics were the most common type of CAM used by both groups. Probiotics are frequently the most common CAM product used for both general health and IBD in CD and UC patients.5,6 However, Portela et al., found that herbal medicines were most commonly used, relating to regional variations in CAM use.5,6 Cannabis use occurred in 33% (63/193) of the surveyed patients. This is lower than a Canadian study showing significantly increased cannabis use by IBD patients, 74% compared to a non-IBD population 48.3%.24 The higher rates may reflect selection bias and voluntary nature of the survey. In our study, cannabis use was unexpectedly low despite recent legalization in Canada. A possible explanation may be general attitudes of CAM users recognizing cannabis as a recreational substance, rather than medicinal. Cannabis use should be assessed due to unknown long-term effects, safety profile, and medication interactions.
CAM disclosure
Patients used advice from a colleague, friend, or family member 32.6% (61/187) when deciding to use CAM, but did not feel well-informed 87.4% (166/193), which is similar to previous studies.5,11,25,26 Our study reported 63% (122/193) of patients disclosed CAM use to their gastroenterologist, which differs from previous 54%–75% rates of non-disclosure.25 A prospective study of 380 IBD patients demonstrated greater compliance with conventional medicine in those that disclosed CAM use, potentially indicating greater trust with their physician.6 In contrast, patients seek CAM due to dissatisfaction with the patient–doctor relationship25 and poor physician communication.27 CAM use and disclosure may be reflective of the therapeutic relationship.
Strengths
The study population is comparable to an outpatient IBD population. Patients with CD had lower QoL scores and higher anti-TNF use. Unlike previous literature, our study focused on CAM use specifically for IBD, and the motivating factors. This provides a foundation for gastroenterologists to open dialogue with patients and avoid consequences of CAM use, such as drug interactions and non-compliance.5,11 Additionally, our study included specific CAM products and services frequently promoted by alternative practitioners based on limited in vitro and vivo research. Gastroenterologists can become familiar with relevant literature and navigate misconceptions of efficacy, safety, and avoid dismissal of alternative therapies, as patients using CAM tend to incorporate and maintain healthy behaviour changes.28,29
Limitations
A limitation of our study is the survey design and potentially polarizing topic of CAM, which is likely to attract participants with a strong interest in CAM. This may explain the lower response rate, particularly by CAM non-users. Future studies can provide the survey at the initial appointment rather than through email at a later date. Many patients had disease duration greater than a decade, and recall bias may be present. Our study asked about specific CAM products and services, which limits comparison to studies that hold broader CAM definitions. A standardized CAM questionnaire may alleviate study protocol differences, although this has not been adopted in the literature.30
Conclusion
Patients with IBD are motivated to use CAM by both push and pull factors, despite having little knowledge of CAM products and services. Lack of symptom improvement with conventional therapies and mental health concerns are the most common drivers of use. By discussing CAM, gastroenterologists have an opportunity to identify persistent symptoms, optimize treatment and compliance, and improve the therapeutic relationship.
Supplementary Material
Acknowledgments
We would like to acknowledge Maria Ancheta-Schmit for her assistance.
Contributor Information
Natasha Klemm, Department of Gastroenterology, University of British Columbia, Vancouver, BC V6B0C3, Canada.
Roberto Trasolini, Department of Gastroenterology, University of British Columbia, Vancouver, BC V6B0C3, Canada.
Brian Bressler, Department of Gastroenterology, University of British Columbia, Vancouver, BC V6B0C3, Canada; IBD Centre of BC, Vancouver, BC V6Z 2L2, Canada.
Gregory Rosenfeld, Department of Gastroenterology, University of British Columbia, Vancouver, BC V6B0C3, Canada; IBD Centre of BC, Vancouver, BC V6Z 2L2, Canada.
Gina Almasan, IBD Centre of BC, Vancouver, BC V6Z 2L2, Canada.
Yvette Leung, Department of Gastroenterology, University of British Columbia, Vancouver, BC V6B0C3, Canada; IBD Centre of BC, Vancouver, BC V6Z 2L2, Canada.
Author contributions
N.K., R.T., and Y.L.—study design. N.K.—date collection. N.K., B.B., G.R., Y.K.—data analysis. N.K., B.B., G.R., G.A., and Y,L.—manuscript writing.
Funding
Funding was provided by the GI Research Institute.
Conflicts of interest
N.K., R.T., and G.A. have no conflicts of interest. B.B. has served as an advisor/speaker/consultant for Pfizer, Merck, Ferring, Janssen, AbbVie, Takeda, Celgene, Genentech, Novartis, Amgen, Allergan, AMT, Fresenius Kabi, Gilead, Protagonist, Sandoz, Alimentiv, Iterative Scopes, Mylan and BMS; received research support from Janssen, AbbVie, Takeda, Atlantic Pharmaceuticals, GSK, BMS, Amgen, Genentech, Merck, RedHill Biopharma, BI, Qu Biologics, Celgene and Alvine; and had stock options in Qu Biologics. G.R. has served as an advisor/ speaker/ consultant for AbbVie, Ferring Fresnius, Kabi, Janssen, Merck, Pfizer, Eli-Lilly, and Takeda. Y.L. has served as advisor/speaker/consultant for Abbvie, Eli Lilly, Takeda, Bristol Myers, Squibb, Pendopharm, Organon, BioJamp, Janssen, Pfizer, and Amgen.
In addition to this COI statement, ICMJE disclosure forms have been collected for all co-authors and can be accessed as supplementary material.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
- 1. Chen XL, Zhong L, Wen Y, et al. Inflammatory bowel disease-specific health-related quality of life instruments: a systematic review of measurement properties. Health Qual Life Outcomes. 2017;15(1):1–13. 10.1186/s12955-017-0753-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization [WHO]. WHO Global Report on Traditional and Complementary Medicine 2019.; 2019. https://www.who.int/health-topics/traditional-complementary-and-integrative-medicine#tab=tab_1 [Google Scholar]
- 3. Zezos P, Nguyen GC.. Use of complementary and alternative medicine in inflammatory bowel disease around the world. Gastroenterol Clin North Am. 2017;46(4):679–688. 10.1016/j.gtc.2017.08.001 [DOI] [PubMed] [Google Scholar]
- 4. Yanai H, Salomon N, Lahat A.. Complementary therapies in inflammatory bowel diseases. Curr Gastroenterol Rep. 2016;18(12):62. 10.1007/s11894-016-0537-6 [DOI] [PubMed] [Google Scholar]
- 5. Nguyen GC, Croitoru K, Silverberg MS, Steinhart AH, Weizman AV.. Use of complementary and alternative medicine for inflammatory bowel disease is associated with worse adherence to conventional therapy: the compliant study. Inflamm Bowel Dis. 2016;22(6):1412–1417. 10.1097/MIB.0000000000000773 [DOI] [PubMed] [Google Scholar]
- 6. Weizman AV, Ahn E, Thanabalan R, et al. Characterisation of complementary and alternative medicine use and its impact on medication adherence in inflammatory bowel disease. Aliment Pharmacol Ther. 2012;35(3):342–349. 10.1111/j.1365-2036.2011.04956.x [DOI] [PubMed] [Google Scholar]
- 7. Rawsthorne P, Clara I, Graff LA, et al. The Manitoba inflammatory bowel disease cohort study: a prospective longitudinal evaluation of the use of complementary and alternative medicine services and products. Gut. 2012;61(4):521–527. 10.1136/gutjnl-2011-300219 [DOI] [PubMed] [Google Scholar]
- 8. Esmail N. Complementary and Alternative Medicine: Use and Public Attitudes 1997, 2006, and 2016. Fraser Institute. https://www.fraserinstitute.org/sites/default/files/complementary-and-alternative-medicine-2017.pdf [Google Scholar]
- 9. Bensoussan M, Jovenin N, Garcia B, et al. Complementary and alternative medicine use by patients with inflammatory bowel disease: results from a postal survey. Gastroenterol Clin Biol. 2006;30(1):14–23. 10.1016/s0399-8320(06)73072-x [DOI] [PubMed] [Google Scholar]
- 10. D P. Predictive factors of complementary and alternative medicine use for patients with inflammatory bowel disease in Korea. Complement Ther Med. 2014;22(1):87–93. [DOI] [PubMed] [Google Scholar]
- 11. Portela F, Dias CC, Caldeira P, et al. The who-when-why triangle of CAM use among Portuguese IBD patients. Dig Liver Dis. 2017;49(4):388–396. 10.1016/j.dld.2016.12.031 [DOI] [PubMed] [Google Scholar]
- 12. Sasso L, Bagnasco A, Catania G, Zanini M, Aleo G, Watson R; RN4CAST@IT Working Group. Push and pull factors of nurses’ intention to leave. J Nurs Manag. 2019;27(5):946–954. 10.1111/jonm.12745 [DOI] [PubMed] [Google Scholar]
- 13. Cleland JA, Johnston P, Watson V, Krucien N, Skåtun D.. What do UK medical students value most in their careers? A discrete choice experiment. Med Educ. 2017;51(8):839–851. 10.1111/medu.13257 [DOI] [PubMed] [Google Scholar]
- 14. Nguyen AM, Wood SJ.. The push-pull factors of physician-system integration: a qualitative study of Washington state healthcare executives. J Healthc Manag. 2019;64(1):15–26. 10.1097/JHM-D-17-00219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lin SC, Cheifetz AS.. The use of complementary and alternative medicine in patients with inflammatory bowel disease. Gastroenterol Hepatol. 2018;14(7):415–425. 10.14309/00000434-201802001-00098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Maizes V, Rakel D, Niemiec C.. Integrative medicine and patient-centered care. Explore (New York, N.Y.) 2009;5(5):277–289. 10.1016/j.explore.2009.06.008 [DOI] [PubMed] [Google Scholar]
- 17. Irvine EJ, Zhou Q TA.. The short inflammatory bowel disease questionnaire: a quality of life instrument for community physicians managing inflammatory bowel disease. CCRPT investigators. Canadian Crohn’s relapse prevention trial. Am J Gastroenterol. 1996;91(8):1571–1578. [PubMed] [Google Scholar]
- 18. Langhorst J, Wulfert H, Lauche R, et al. Systematic review of complementary and alternative medicine treatments in inflammatory bowel diseases. J Crohn’s Colitis. 2015;9(1):86–106. 10.1093/ecco-jcc/jju007 [DOI] [PubMed] [Google Scholar]
- 19. Lin Z, Wu H, Fu Y, Dai S.. Application of herbaceous medications for inflammatory bowel disease as a complementary and alternative therapy. Inflamm Bowel Dis. 2019;25(12):1886–1895. 10.1093/ibd/izz190 [DOI] [PubMed] [Google Scholar]
- 20. Arp L, Jansson S, Wewer V, Burisch J.. Psychiatric disorders in adult and paediatric patients with inflammatory bowel diseases—a systematic review and meta-analysis. J Crohns Colitis. 2022;16(12):1933–1945. 10.1093/ecco-jcc/jjac095 [DOI] [PubMed] [Google Scholar]
- 21. Barberio B, Zamani M, Black CJ, Savarino EV, Ford AC.. Prevalence of symptoms of anxiety and depression in patients with inflammatory bowel disease: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2021;6(5):359–370. 10.1016/S2468-1253(21)00014-5 [DOI] [PubMed] [Google Scholar]
- 22. Mikocka-Walus A, Knowles SR, Keefer L, Graff L.. Controversies revisited: a systematic review of the comorbidity of depression and anxiety with inflammatory bowel diseases. Inflamm Bowel Dis. 2015;22(3):752–762. 10.1097/mib.0000000000000620 [DOI] [PubMed] [Google Scholar]
- 23. Burgmann T, Rawsthorne P, Bernstein CN.. Predictors of alternative and complementary medicine use in inflammatory bowel disease: Do measures of conventional health care utilization relate to use? Am J Gastroenterol. 2004;99(5):889–893. 10.1111/j.1572-0241.2004.30033.x [DOI] [PubMed] [Google Scholar]
- 24. Pi S, Rosenfeld G, Enns R, et al. Patterns and motivations of Cannabis use amongst patients with inflammatory bowel disease. GastroHep. 2019;1(3):100–107. 10.1002/ygh2.338 [DOI] [Google Scholar]
- 25. Mountifield R, Andrews JM, Mikocka-Walus A, Bampton P.. Doctor communication quality and friends’ attitudes influence complementary medicine use in inflammatory bowel disease. World J Gastroenterol. 2015;21(12):3663–3670. 10.3748/wjg.v21.i12.3663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Langhorst J, Anthonisen IB, Steder-Neukamm U, et al. Patterns of complementary and alternative medicine (CAM) use in patients with inflammatory bowel disease: perceived stress is a potential indicator for CAM use. Complement Ther Med. 2007;15(1):30–37. 10.1016/j.ctim.2006.03.008 [DOI] [PubMed] [Google Scholar]
- 27. Lindberg A, Fossum B, Karlen P, Oxelmark L.. Experiences of complementary and alternative medicine in patients with inflammatory bowel disease - a qualitative study. BMC Complement Altern Med. 2014;14(1):1–9. 10.1186/1472-6882-14-407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sirois FM. Health-related self-perceptions over time and provider-based Complementary and Alternative Medicine (CAM) use in people with inflammatory bowel disease or arthritis. Complement Ther Med. 2014;22(4):701–709. 10.1016/j.ctim.2014.07.003 [DOI] [PubMed] [Google Scholar]
- 29. Long AF. The potential of complementary and alternative medicine in promoting well-being and critical health literacy: a prospective, observational study of Shiatsu. BMC Complement Altern Med. 2009;9(1):1–11. 10.1186/1472-6882-9-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Quandt SA, Verhoef MJ, Arcury TA, et al. Development of an international questionnaire to measure use of complementary and alternative medicine (I-CAM-Q). J Altern Complement Med. 2009;15(4):331–339. 10.1089/acm.2008.0521 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.