Abstract
Guidelines advocate that the symptomatic management of fever should prioritize alleviating the child's discomfort. We investigated the definition and assessment of discomfort in febrile children within the scientific pediatric literature. A systematic review was conducted in accordance with PRISMA 2020 guidelines and preregistered on the Prospero database (CRD42023471590). Databases including PubMed, Embase, and Cochrane were searched. Studies addressing discomfort in febrile children were eligible. Out of 794 initially identified articles, 27 original studies and seven guidelines specifically used the term ‘discomfort’. Only 14 original articles provided a definition of discomfort, revealing substantial heterogeneity and no clear-cut definition. Discomfort was often assessed subjectively, predominantly through parent or self-report, and only two studies used a scoring system for assessment. The definitions varied widely, with terms such as crying, irritability, shivering and chills, pain and distress, goosebumps commonly used and evaluation of observable modifications such as facial modifications. Overall, no consensus on a single, standardized definition was available.
Conclusions: This systematic review shows the absence of a standardized definition and assessment of discomfort in febrile children. The findings of the present analysis might be the basis for building a consensus and developing a new tool to evaluate discomfort.
|
What is Known: • Discomfort is currently considered the main criterion to guide antipyretic administration in children with fever. • Despite this clear-cut recommendation, it has been questioned whether a commonly accepted understanding and assessment of this condition exists. |
|
What is New: • This systematic review identifies a significant heterogeneity in definitions and assessment of discomfort in children with fever. • Both subjective parameters and observable modifications in physiological parameters should be included in a new and shared characterization of discomfort. |
Supplementary Information
The online version contains supplementary material available at 10.1007/s00431-024-05753-7.
Keywords: Fever, Management, Fever phobia, Comfort, Antipyretics
Introduction
Fever annually affects approximately 70% of preschool-aged children, leading about 40% of these cases to seek medical care [1, 2]. Both national and international guidelines advocate that the management of fever with antipyretics, such as paracetamol or ibuprofen, should prioritize alleviating the child’s general conditions and should be prescribed only when the child presents with discomfort independently form a specific body temperature threshold [3]. Despite this clear-cut recommendation, it has been recently questioned whether a commonly accepted understanding and assessment of discomfort exists in the scientific community [4]. This issue is of paramount importance to favorite a proper management of pediatric patients with fever. For this purpose, we conducted a study to investigate existing definitions of discomfort in febrile children within literature and evaluate how this condition is assessed.
Material and methods
Literature search and study selection
A systematic literature review was conducted according to PRISMA 2020 guidelines. The protocol was preregistered on the Prospero database (CRD42023471590). The search was conducted on November 30, 2023, in three databases (PubMed, Embase, and Cochrane) using the following terms: (child* OR pediatric* OR perinat* OR neonat* OR newborn* OR infan* OR baby OR babies OR toddler* OR juvenil* OR adolescen*) AND (discomfort* OR comfort* AND (fever OR pyrexia OR hyperthermia OR temperature OR febrile OR feverish OR body temperature)). The detailed literature search strategy is provided in the online supplementary material. Eligible reports were original studies providing a definition of discomfort associated with fever in childhood. Studies written in languages other than English, letters, case reports, or case series with a sample size of fewer than ten subjects, and studies conducted in non-human subjects were excluded. Additionally, a search was conducted on guidelines on fever management. The search was carried out on national scientific societies or government organizations’ websites: PubMed; Australian Clinical Practice Guidelines (http://www.clinicalguidelines.gov.au/); Canadian CPG Infobase: Clinical Practice Guidelines Database (http://www.cma.ca/En/Pages/clinical-practice-guidelines.asp); Guidelines International Network (http://www.g-i-n.net/); National Guideline Clearinghouse (http://www.guideline.gov); NICE: National Institute for Health and Care Excellence (http://www.nice.org.uk); Scottish Intercollegiate Guidelines Network (SIGN) (http://www.sign.ac.uk).
Study management, data extraction, and quality assessment
The tool Rayyan, a text mining technology to identify abstracts that are potentially most relevant for a project, allowing those abstracts to be screened first, was used to manage original articles and guidelines. Data were recorded in a predefined electronic database. From the original articles, the following data were extracted: general characteristics of the study (author, year of publication, country), study design, sample size, and definition of discomfort. For guidelines, the information collected included: authorship, publication year, country, type of guidelines and definition of discomfort.
The STROBE guideline for observational studies and the Cochrane Risk of Bias tool for randomized controlled trials (RCTs) were used. AGREE 2 was used to evaluate the quality of guidelines.
Pairs of authors (I.A., A.S., S.G.) independently selected the articles and guidelines, extracted the data, and evaluated the study quality. In instances of discrepancies or disagreements, a collaborative approach was adopted with face-to-face discussions. If controversies persisted, a third senior author was involved (G.P.M. or E.C.)
Results
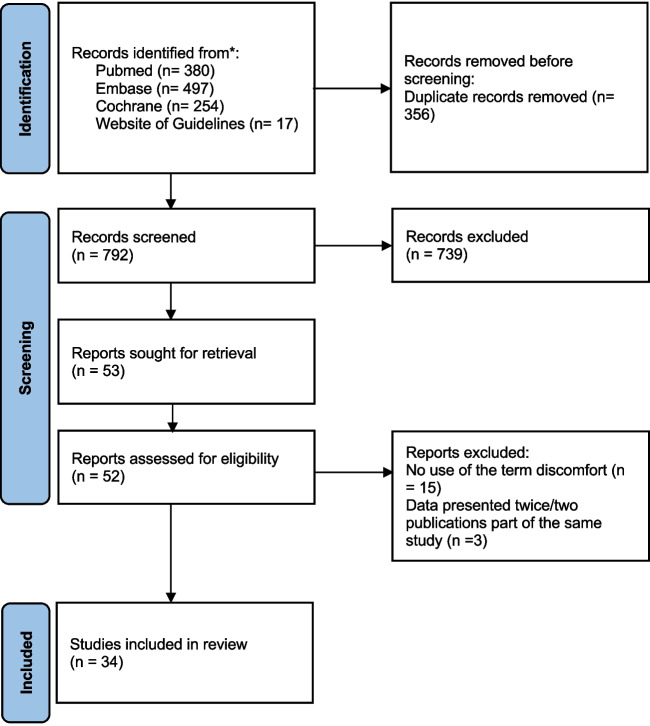
A total of 794 articles (including 13 guidelines) were initially identified (Fig. 1). After the article screening, 27 original articles [5–31] and seven guidelines [32–38] that used the term “discomfort” (or “comfort”) were retrieved. Among these, 14 original articles reported a definition of discomfort [5–18]. The seven guidelines that discussed discomfort did not provide any definition of the term.
Fig. 1.
Flowchart of the literature search
Among the original articles providing a definition of discomfort, eight were randomized clinical trials [5–12] (Table 1) and six were observational studies (four were cross-sectional studies [13, 16–18] and two were cohort studies) [14, 15] (Table 2). All the observational studies were conducted in high-income countries [13–18]. Six studies were conducted to compare the effectiveness of antipyretics, ibuprofen, or cold water sponging in the treatment of fever [5–7, 9, 11, 12]. One article established the efficacy of paracetamol and ibuprofen and their economic impact [10]. Three articles focused on analyzing fever management approaches by caregivers or healthcare providers [13, 17, 18], while one study evaluated how parents approach their children’s illness [16]. Another study analyzed the impact of paracetamol, ibuprofen, or aspirin on comfort [8]. Additionally, one study examined fever discomfort before and after paracetamol administration [14], and another compared sickness behavior and fever [15]. Children enrolled in the studies ranged in age from 6 months to 12 years.
Table 1.
Characteristics of RCTs reporting a definition of discomfort
| Name | Year | Country | Study design | Population | Study objectives | Role of discomfort in the study | Discomfort definition | Score |
|---|---|---|---|---|---|---|---|---|
| Agbolosu N.B. et al. [5] | 1997 | Malawi | RCT, data prospectively collected | 80 children, aged 6 to 60 months | Compare the effects of tepid sponging and paracetamol in reducing fever in children | Discomfort used as primary outcome | Convulsions, crying, irritability, vomiting and shivering | / |
| Aluka T et al. [6] | 2013 | Nigeria | RCT, data prospectively collected | 88 children from 12 to 120 months old | Compare the effectiveness of cold water sponging with that of oral paracetamol in the treatment of fever in children | Discomfort used as primary outcome | Crying, shivering, goose pimples and convulsions | / |
| Alves JG et al. [7] | 2008 | Brazil | RCT, data prospectively collected | 106 children from six months to five years old with axillary temperature greater than 38°C in the emergency ward | Evaluate and compare the effectiveness of tepid sponging plus dipyrone with dipyrone alone in lowering fever in children | Discomfort used as secondary outcome | Crying, irritable or shivering | / |
| Autret E et al. [8] | 1997 | France | RCT, data prospectively collected | 351 children from 6 to 24 months | To assess effectiveness and impact on children’s comfort of ibuprofen, aspirin and paracetamol | Comfort used as a primary outcome |
Comfort valuated using: -Children’s reaction to pain (crying or change in facial expression) -general behaviour -child’s relief |
Child’s reaction to pain: “CHEOPS” scale (child's crying: 0 not crying; 1 fretting; 2 crying or whimpering; 3 crying with sobs or screams. expression on the child's face: 0 smiling, frankly happy expression; 1 peaceful, neutral expression; 2 grimacing, frankly unhappy expression) General behavior: four level rating scale (0 as good as before the illness; 1 slightly abnormal; 2 fairly abnormal;3 very abnormal) and 100-ram horizontal visual scale (from 0 as good as before to 100 very abnormal Child’s relief: five-level rating scale (3 completely relieved; 2 fairly relieved; 1 little relieved; 0 not at all relieved; − 1 aggravated) |
| Chetak KB et al. [9] | 2017 | India | RCT, data prospectively collected | 500 children under the age of 6 months to 12 years | Compare the effectiveness of tepid sponging and antipyretic drug versus antipyretic drug alone in febrile children | Discomfort used as primary outcome | Chills, goose bumps, and irritability | |
| Hay AD et al. [10] | 2009 | England | RCT, data prospectively collected | 156 children Age between 6 months and 6 years | Establish the relative clinical effectiveness and cost-effectiveness of paracetamol plus ibuprofen compared with paracetamol and ibuprofen separately for time without fever and the relief of fever-associated discomfort in young children who can be managed at home | Discomfort used as primary outcome | Some pain—> distress, crying—> very distressed | / |
| Sharber J et al. [11] | 1997 | Arizona | RCT, data prospectively collected | 20 children, front 5 to 68 months of age | Compare fever reduction and with acetaminophen alone and acetaminophen plus a 15-min tepid sponge bath | Discomfort used as primary outcome | Crying, shivering, and goosebumps | / |
| Thomas S et al. [12] | 2009 | India | RCT, data prospectively collected | 150 children from 6 months to 12 years with fever (axillary temperature ≥ 101°F) in a tertiary care hospital | Determine which approach between tepid sponging and antipyretic drug versus only antipyretic drug is more effective in managing fever in children | Discomfort used as secondary outcome | Crying, restlessness and irritability | / |
Table 2.
Characteristics of observational studies reporting a definition of discomfort
| Name | Year | Country | Study design | Population | Study objectives | Role of discomfort in the study | Discomfort definition | Score | |
|---|---|---|---|---|---|---|---|---|---|
| Betz MG et al. [13] | 2005 | United Arab Emirates | Cross-sectional study, data prospectively collected | 264 caregivers identified following the registration and triage of any child who presents with the primary concern or one of several concerns related to “fever” | Examine caregivers’ approach to fever in emergency situations | Discomfort used as primary outcome | Malaise and vomiting | / | |
| Chiappini E et al. [14] | 2023 | Italy | Cohort study, data prospectively collected | 172 febrile children attending Emergency Department (median age 41.7 months) | Evaluate the level of discomfort before and after administration of paracetamol | Degree of discomfort used as a primary outcome | Variations of sleep wake cycle, appetite, motor activity, mood, daily habits, facial expression (using Doria et al., 2019 study) | discomfort evaluated using items defined by Italian experts; level of pain evaluated using Faces Pain Scale-Revised | |
| Corrard F et al. [15] | 2017 | France | Multi-center, observational study, data retrospectively collected | 200 febrile children and 200 non-febrile children aged 6 months to 3 years (changes in child’s behavior was reported by parents) | Evaluate the relation between sickness behavior and fever and SB clinical components | Discomfort (and its association to SB) used as a primary outcome | Tendency to become irritated or angry, to whine or cry, change in facial expression indicative of pain. Decreased activity, lack of initiative, less liveliness, mood disorders with irritability, whimpering and greater tearfulness, reduced social interactions, less interest in the surrounding, distorted expression, decreased appetite, and disturbed sleep) | / | |
| Lagerløv P et al. [16] | 2003 | Norway | Cross-sectional study, data prospectively collected | 24 parents of children accessing 6 Norwegian hospitals | Evaluate how parents identify common childhood illnesses, their perspectives on the importance of fever, the influence of children’s illnesses on the daily life of the family, and how parents handle illnesses by using paracetamol | Discomfort used as primary outcome | Pain and sufferance | / | |
| Lava SAG et al. [17] | 2013 | Switzerland | Cross-sectional study, data prospectively collected | 322 pediatricians | Examine if there are variations in fever management across the three linguistic regions of Switzerland | Discomfort used as primary outcome | Reduced general appearance | / | |
| Leigh S et al. [18] | 2020 | United Kingdom | Multi-center, observational, cross-sectional survey, data prospectively collected | 98 parents of children 0–11 years and 99 healthcare providers (HCP) | Define parental and healthcare providers preferences for childhood fever management in the emergency department | HCP grade of discomfort was asked in the survey | Synonym of pain | / | |
Characteristics of the studies and guidelines which did not provided any definition of discomfort are given in the online supplementary material.
Discomfort definition
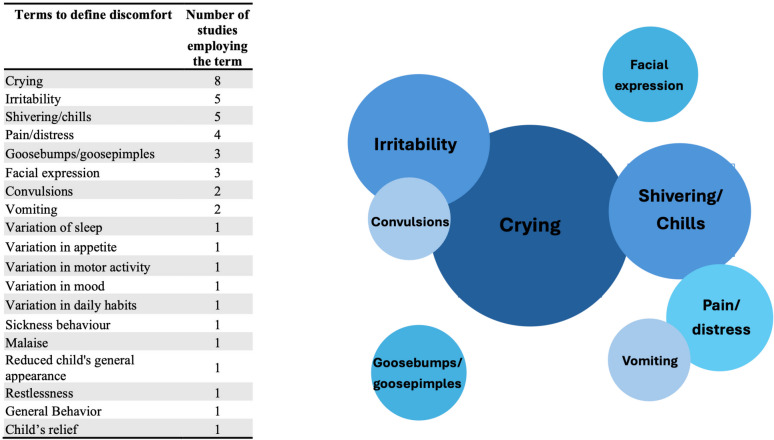
None of the studies provided a clear-cut definition of discomfort. All the studies used a variety of terms, except for one study that used “discomfort” synonymously with “pain” [18] and another that equated it with a “reduced general appearance” [17]. Specifically, eight studies used the term “crying” [5–8, 10–12, 15], five used “irritability” [5, 7, 9, 12, 15], five used “shivering” or “chills” [5–7, 9, 11], three mentioned “goose pimples/bumps” [6, 9, 11], two referenced “convulsions” [5, 6], one used “malaise” [13], three used “change in facial expressions” [14, 15], one mentioned “general behavior” and “child’s relief” [8], and two referred to “vomiting” [5, 13].
One study, conducted in a high-income country, adopted a definition of discomfort from a previous study that evaluated variations in the sleep–wake cycle, motor activity, facial expressions, appetite, mood, and daily habits [14]. Another article linked discomfort to sickness behavior [15]. Additionally, four articles considered “pain” or “distress” as synonyms for discomfort (Fig. 2) [10, 15, 16, 18].
Fig. 2.
Venn diagram depicting the frequency of terms used to report discomfort. The larger the circles, the more frequently the terms to define discomfort have been used in literature. Items reported in < 2 studies were not represented by circles
“Crying” was mentioned in seven RCTs (randomized clinical trials) conducted in Africa [5, 6], Europe [8, 10], Asia [12], North America [11], and South America [7], but it was used exclusively in only one observational study conducted in Europe [15]. “Goose pimples/bumps” and “shivering” were only mentioned in RCTs (one each in North America [11], South America [7], and Asia [9], and two in Africa[5, 6]). “Irritability” appeared in five studies (four RCTs [5, 7, 9, 12] and one observational study [15]) conducted in Africa, South America, and Asia. “Convulsions” was used to define discomfort in two RCTs conducted in Africa [5, 6], while “pain/distress”,”variations in the sleep–wake cycle”, “changes in appetite”, “variations in motor activity”, “changes in daily habits”, “sickness behavior”, and “reduced general appearance” were only used in observational studies conducted in Europe [14, 15, 17]. “Change in facial expression” was used in one RCT [8] and two observational studies conducted in Europe [14, 15].
One study utilized the Faces Pain Scale-Revised scoring system to assess discomfort, [14] while another study used a scoring system that referred to child’s reaction to pain (CHEOPS), general behavior and relief [8]. No studies evaluated vital parameters related to discomfort, and assessments were either self-reported, reported by parents, or conducted through clinical evaluation.
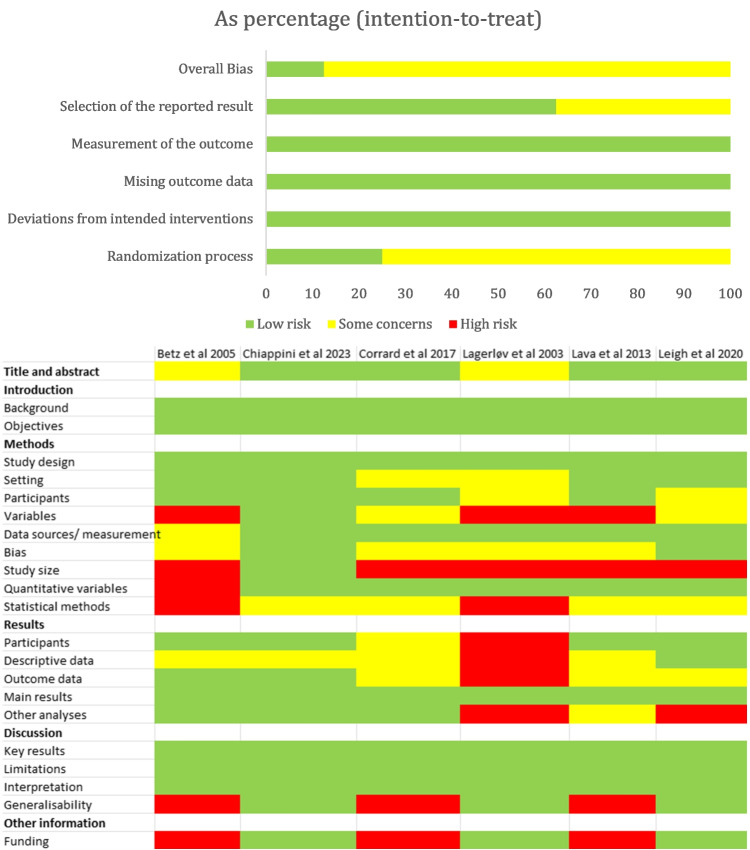
Quality assessment
Among the seven randomized controlled trials providing a definition of discomfort (Fig. 3, upper panel), some concerns were presented in 88% of the studies [5–7, 9, 11, 12], while one exhibited a low risk of bias [10]. All the studies adhered to an intention-to-treat approach. In the case of the six observational studies providing a definition of discomfort (Fig. 3, lower panel), four exhibited a low risk of bias in the title and abstract [14, 15, 17, 18], while two raised some concerns [13, 16]. Across all six studies, there was a low risk of bias identified in the introduction [13–18]. The assessment of methods, which was categorized into study design, setting, participants, variables, data sources/measurement, bias, study size, quantitative variables, and statistical methods, generally presented some concerns. Specifically, study size showed a high risk in all studies except one, which presented a low risk of bias [14]. Results were divided into five sections: participants, descriptive data, outcome data, main results, and other analyses. One study presented a high risk of bias in four sections [16], but overall, all studies showed some concerns. Main results had a low risk of bias in all articles [13–18]. In considering the evaluation of the discussion, all articles presented a low risk of bias in key results, limitations, and interpretation [13–18]. However, three studies had a high risk of bias in generalizability [13, 15, 18], and three had a low risk [14, 16, 17]. Quality assessment of studies and guidelines which did not provide any definition of discomfort is provided in the online supplementary material.
Fig. 3.
Quality assessment of RCTs (ROB) using the term discomfort and providing a definition (upper panel). Quality assessment of observational studies (Strobe) using the term discomfort and providing a definition (lower panel)
Discussion
This is the first systematic review investigating the presence of a shared definition and standardized assessment methods for discomfort in children with fever within the existing literature. The key findings of this analysis can be summarized as follows: (1) a minority of studies addressing this issue provide a definition of discomfort; (2) notably, pediatric guidelines on fever lack a specific definition of discomfort; (3) a lack of consensus regarding the definition of discomfort is evident in the scientific literature and it also includes guidelines on fever management; and (3) standardized methods for assessing discomfort are notably absent.
Given that fever typically holds beneficial effects for children, discomfort arising from fever can engender various challenges such as mental distress, reduced appetite, and disruptions in sleep patterns [39, 40]. Consequently, mitigating discomfort assumes importance in the management of febrile children [41, 42]. However, our review identified a marked heterogeneity in the definition of discomfort across scientific literature, independently from study design and quality. Nearly all studies employing a definition of discomfort utilized a combination of terms, often related to generic clinical manifestations or alterations in the child’s appearance and daily habits. Notably, the level of discomfort was predominantly assessed subjectively by parents or the children themselves, rendering a quantitative evaluation of discomfort challenging. Notably, only two studies incorporated a scoring system for the evaluation of discomfort.
This lack of uniformity in defining discomfort complicates the assessment and management of fever in children, potentially leading to inappropriate interventions. In a few studies, discomfort was used as a synonym of pain. While discomfort is often associated to pain, a child with fever and discomfort may present without any pain [41]. Therefore, we feel that fever, discomfort, and pain should be carefully evaluated and separately assessed.
The absence of a standardized definition of discomfort likely accounts for the dearth of standardized assessment methods in clinical practice. This finding is unexpected given the emphasis placed on treating discomfort in many guidelines, but several factors may contribute to this gap. Unlike fever, discomfort is inherently subjective, posing challenges particularly in non-verbal children such as infants. Furthermore, cultural and contextual factors in defining and assessing discomfort in febrile children might exist. We observed variations in the terminology and conceptualization of discomfort across studies conducted in different regions and settings. It is known that cultural beliefs influence conceptions on fever. Similarly, also how discomfort is perceived and expressed might vary, requiring culturally sensitive approaches to assessment and management.
The definition of discomfort might include the terms most commonly identified in this analysis such as crying, irritability, shivering and chills, pain and distress, and goosebumps. Additionally, incorporating observable alterations in physiological parameters could enhance clinical assessments (e.g., changes in facial expressions). We posit that a robust definition of discomfort should comprehensively encompass subjective experiences and objectively observable modifications in the child’s behavior. Furthermore, to facilitate widespread adoption, any new definition should be easily applicable by caregivers without specialized medical training, considering that fever management often occurs outside medical settings. To this regard, pediatric research in other fields has made several relevant improvements in recent years (e.g. introducing easy to use scales for pain assessment in children).
Prior studies have documented the prevalence of “fever phobia” among caregivers and healthcare providers, which often leads to inappropriate interventions [43–46]. Despite efforts to mitigate this phenomenon, it persists globally [44, 46, 47]. We contend that clarifying the concept of discomfort, rather than focusing solely on high body temperatures, is pivotal in altering approaches to fever management. However, the absence of a clear definition of discomfort may impede such a paradigm shift. We advocate for the creation of an international working group to provide a definition of discomfort using a standardized scientific approach, such as the Delphi process.
A standardized assessment of discomfort in clinical practice might be relevant also to evaluate the effects of pharmacological and non-pharmacological treatment of children with fever. Since most guidelines on management of children with fever highlight the importance of discomfort, future recommendations should incorporate standardized definitions of discomfort and recommend appropriate assessment strategies and interventions. Such guidelines would not only support healthcare providers in delivering optimal care but also empower parents and caregivers to effectively manage fever-related discomfort at home.
This systematic review has several limitations. The search was limited to three databases and other potential sources of articles (e.g. CINAHL) were not evaluated. All the articles considered were in English and we cannot exclude that studies in other languages providing a definition and assessment of discomfort are available. Additionally, the exclusion of narrative review may have overlooked valuable insights, although guidelines, which were expected to contain such definitions, were included. Finally, it was not possible to compare studies’ definitions is a structured way (e.g. testing if some definitions were more common in high-quality studies) due to their heterogeneity.
In conclusion, this systematic review highlights the absence of a universally shared definition and assessment of discomfort in children with fever. The data from this study might be the basis for building a consensus and developing a new tool to evaluate discomfort.
Supplementary Information
Below is the link to the electronic supplementary material.
Abbreviation
- RCT
Randomized controlled trial
Authors’ contributions
All authors contributed to the study design. Ilaria Alberti, Alessia bonetti, Silvia Garattini performed the literature search and data extraction, Antonio Corsello, Paola Marchisio contributed to data interpretation. Gregorio Paolo Milani, Ilaria Alberti, Alessia Bonetti, Silvia Garattini, Elena Chiappini wrote the first draft of the manuscript. Antonio Corsello, Paola Marchisio reviewed the first draft of the manuscript. All authors approved the manuscript as submitted.
Funding
Open access funding provided by Università degli Studi di Milano within the CRUI-CARE Agreement. The study was partially supported by the Italian Ministry of Health (Ricerca Corrente 2023). The funding agencies had no role in study design, data collection, analysis or interpretation, or writing of the report.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Competing interests
Gregorio Paolo Milani received unrestricted grant from Angelini Pharma S.P.A and Reckitt Benckiser Healthcare S.P.A. Furthermore, he received a fee for scientific advice from Angelini Pharma S.P.A. Furthermore, he is one of the editors of European Journal of Pediatrics.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hussain SM, Al-Wutayd O, Aldosary AH, Al-Nafeesah A, AlE’ed A, Alyahya MS, Alfeneekh AS, AlKadi SA, Alghasham GA, Aloyaidi GA (2020) Knowledge, attitude, and practice in management of childhood fever among saudi parents. Glob Pediatr Health 7:2333794x20931613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sakr F, Toufaili Z, Akiki Z, Akel M, Malaeb D, Dabbous M, Salameh P (2022) Fever among preschool-aged children: a cross-sectional study assessing Lebanese parents’ knowledge, attitudes and practices regarding paediatric fever assessment and management. BMJ Open 12:e063013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chiappini E, Bortone B, Galli L, de Martino M (2017) Guidelines for the symptomatic management of fever in children: systematic review of the literature and quality appraisal with AGREE II. BMJ Open 7:e015404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Milani GP, Corsello A, Schulz PJ, Fadda M, Giannì ML, Alberti I, Comotti A, Marchisio P, Chiappini E, Peroni D (2023) Are we confident that we all share a common understanding of discomfort in febrile children? Acta Paediatr 112:2252–2253 [DOI] [PubMed] [Google Scholar]
- 5.Agbolosu NB, Cuevas LE, Milligan P, Broadhead RL, Brewster D, Graham SM (1997) Efficacy of tepid sponging versus paracetamol in reducing temperature in febrile children. Ann Trop Paediatr 17:283–288 [DOI] [PubMed] [Google Scholar]
- 6.Aluka TM, Gyuse AN, Udonwa NE, Asibong UE, Meremikwu MM, Oyo-Ita A (2013) Comparison of cold water sponging and acetaminophen in control of fever among children attending a tertiary hospital in South Nigeria. J Family Med Prim Care 2:153–158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alves JG, Almeida ND, Almeida CD (2008) Tepid sponging plus dipyrone versus dipyrone alone for reducing body temperature in febrile children. Sao Paulo Med J 126:107–111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Autret E, Reboul-Marty J, Henry-Launois B, Laborde C, Courcier S, Goehrs JM, Languillat G, Launois R (1997) Evaluation of ibuprofen versus aspirin and paracetamol on efficacy and comfort in children with fever. Eur J Clin Pharmacol 51:367–371 [DOI] [PubMed] [Google Scholar]
- 9.Chetak K, Gowri P, Ravi M (2018) Effectiveness of antipyretic with tepid sponging versus antipyretic alone in febrile children: a randomized controlled trial. J Nepal Paediatr Soc 37:129–133 [Google Scholar]
- 10.Hay AD, Costelloe C, Redmond NM, Montgomery AA, Fletcher M, Hollinghurst S, Peters TJ (2008) Paracetamol plus ibuprofen for the treatment of fever in children (PITCH): randomised controlled trial. BMJ 337:a1302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sharber J (1997) The efficacy of tepid sponge bathing to reduce fever in young children. Am J Emerg Med 15:188–192 [DOI] [PubMed] [Google Scholar]
- 12.Thomas S, Vijaykumar C, Naik R, Moses PD, Antonisamy B (2009) Comparative effectiveness of tepid sponging and antipyretic drug versus only antipyretic drug in the management of fever among children: a randomized controlled trial. Indian Pediatr 46:133–136 [PubMed] [Google Scholar]
- 13.Betz MG, Grunfeld AF (2006) “Fever phobia” in the emergency department: a survey of children’s caregivers. Eur J Emerg Med 13:129–133 [DOI] [PubMed] [Google Scholar]
- 14.Chiappini E, Bestetti M, Masi S, Paba T, Venturini E, Galli L (2023) Discomfort relief after paracetamol administration in febrile children admitted to a third level paediatric emergency department. Front Pediatr 11:1075449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Corrard F, Copin C, Wollner A, Elbez A, Derkx V, Bechet S, Levy C, Boucherat M, Cohen R (2017) Sickness behavior in feverish children is independent of the severity of fever. An observational, multicenter study. PLoS One 12:e0171670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lagerløv P, Helseth S, Holager T (2003) Childhood illnesses and the use of paracetamol (acetaminophen): a qualitative study of parents’ management of common childhood illnesses. Fam Pract 20:717–723 [DOI] [PubMed] [Google Scholar]
- 17.Lava SA, Simonetti GD, Ferrarini A, Ramelli GP, Bianchetti MG (2013) Regional differences in symptomatic fever management among paediatricians in Switzerland: the results of a cross-sectional web-based survey. Br J Clin Pharmacol 75:236–243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leigh S, Robinson J, Yeung S, Coenen F, Carrol ED, Niessen LW (2020) What matters when managing childhood fever in the emergency department? A discrete-choice experiment comparing the preferences of parents and healthcare professionals in the UK. Arch Dis Child 105:765–771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chiappini E, Cangelosi AM, Becherucci P, Pierattelli M, Galli L, de Martino M (2018) Knowledge, attitudes and misconceptions of Italian healthcare professionals regarding fever management in children. BMC Pediatr 18:194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chiappini E, D’Elios S, Mazzantini R, Becherucci P, Pierattelli M, Galli L, de Martino M (2013) Adherence among Italian paediatricians to the Italian guidelines for the management of fever in children: a cross sectional survey. BMC Pediatr 13:210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Deja E, Peters MJ, Khan I, Mouncey PR, Agbeko R, Fenn B, Watkins J, Ramnarayan P, Tibby SM, Thorburn K, Tume LN, Rowan KM, Woolfall K (2021) Establishing and augmenting views on the acceptability of a paediatric critical care randomised controlled trial (the FEVER trial): a mixed methods study. BMJ Open 11:e041952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ertmann RK, Møller JJ, Waldorff FB, Siersma V, Reventlow S, Söderström M (2012) The majority of sick children receive paracetamol during the winter. Dan Med J 59:A4555 [PubMed] [Google Scholar]
- 23.Khaliq A, Zeb R, Khan S, Ahmad I, Tahir M, Shah SIA (2019) Comparison between antipyretic and cold sponging versus only antipyretic in treatment of fever in pediatrics age group. J Med Sci 27:3–6 [Google Scholar]
- 24.Krafft HS, Raak CK, Jenetzky E, Zuzak TJ, Längler A, Martin DD (2022) Warming up for a better fever: a randomized pilot study in pediatric oncology. Pilot Feasibility Stud 8:183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Martins M, Abecasis F (2016) Healthcare professionals approach paediatric fever in significantly different ways and fever phobia is not just limited to parents. Acta Paediatr 105:829–833 [DOI] [PubMed] [Google Scholar]
- 26.Milani GP, Corsello A, Fadda M, Falvo I, Bianchetti MG, Peroni D, Chiappini E, Cantoni B, Sannino P, Destrebecq A, Marchisio P (2023) Approach to fever in children among final-year nursing students: a multicenter survey. BMC Nurs 22:119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Park YR, Kim H, Park JA, Ahn SH, Chang S, Shin JW, Kim M, Lee JH (2021) Comparative analysis of single and combined antipyretics using patient-generated health data: retrospective observational study. JMIR Mhealth Uhealth 9:e21668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peters MJ, Khan I, Woolfall K, Deja E, Mouncey PR, Wulff J, Mason A, Agbeko R, Draper ES, Fenn B, Gould DW, Koelewyn A, Klein N, Mackerness C, Martin S, O’Neill L, Ramnarayan P, Tibby S, Tume L, Watkins J, Thorburn K, Wellman P, Harrison DA, Rowan KM (2019) Different temperature thresholds for antipyretic intervention in critically ill children with fever due to infection: the FEVER feasibility RCT. Health Technol Assess 23:1–148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Polidori G, Titti G, Pieragostini P, Comito A, Scaricabarozzi I (1993) A comparison of nimesulide and paracetamol in the treatment of fever due to inflammatory diseases of the upper respiratory tract in children. Drugs 46(Suppl 1):231–233 [DOI] [PubMed] [Google Scholar]
- 30.Gupta H, Shah D, Gupta P, Sharma KK (2007) Role of paracetamol in treatment of childhood fever: a double-blind randomized placebo controlled trial. Indian Pediatr 44:903–911 [PubMed] [Google Scholar]
- 31.Tan E, Haskell L, Beck S, MacLean A, Rogan A, Than M, Venning B, White C, Yates K, McKinlay CJ, Dalziel SR (2022) Use of the Theoretical Domains Framework to explore factors influencing paediatric fever management practices and antipyretic use in New Zealand emergency departments. J Paediatr Child Health 58:1847–1854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pantell RH, Roberts KB, Adams WG, Dreyer BP, Kuppermann N, O’Leary ST, Okechukwu K, Woods CR Jr (2021) Evaluation and management of well-appearing febrile infants 8 to 60 days old. Pediatrics 148:e2021052228 [DOI] [PubMed] [Google Scholar]
- 33.Perth Children’s Hospital P. Febrile child. https://www.rch.org.au/clinicalguide/guideline_index/Febrile_child/
- 34.Doniec Z, Jackowska T, Sybilski A, Woroń J, Mastalerz-Migas A (2021) FEVER in children – recommendations for primary care doctors – FEVER COMPASS. Fam Med Prim Care Rev 23:99–115 [Google Scholar]
- 35.Children’s Health Queensland C. Febrile illness – Emergency management in children. https://www.childrens.health.qld.gov.au/for-health-professionals/queensland-paediatric-emergency-care-qpec/queensland-paediatric-clinical-guidelines/febrile-illness
- 36.National Collaborating Centre for Ws, Children’s H (2013) National Institute for Health and Care Excellence: Guidelines. Feverish Illness in children: assessment and initial management in children younger than 5 years. Royal College of Obstetricians and Gynaecologists (UK) [PubMed]
- 37.Chiappini E, Principi N, Longhi R, Tovo PA, Becherucci P, Bonsignori F, Esposito S, Festini F, Galli L, Lucchesi B, Mugelli A, de Martino M (2009) Management of fever in children: summary of the Italian Pediatric Society guidelines. Clin Ther 31:1826–1843 [DOI] [PubMed] [Google Scholar]
- 38.World Health Organization WHO (2013) Pocket book of hospital care for children. Guidelines for the management of common childhood illnesses [PubMed]
- 39.Clinch J, Dale S (2007) Managing childhood fever and pain–the comfort loop. Child Adolesc Psychiatry Ment Health 1:7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barbi E, Marzuillo P, Neri E, Naviglio S, Krauss BS (2017) Fever in children: pearls and pitfalls. Children (Basel) 4:81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Doria M, Careddu D, Ceschin F, Libranti M, Pierattelli M, Perelli V, Laterza C, Chieti A, Chiappini E (2019) Understanding discomfort in order to appropriately treat fever. Int J Environ Res Public Health 16:4487 [DOI] [PMC free article] [PubMed]
- 42.Kelly M, McCarthy S, O’Sullivan R, Shiely F, Larkin P, Brenner M, Sahm LJ (2016) Drivers for inappropriate fever management in children: a systematic review. Int J Clin Pharm 38:761–770 [DOI] [PubMed] [Google Scholar]
- 43.Merlo F, Falvo I, Caiata-Zufferey M, Schulz PJ, Milani GP, Simonetti GD, Bianchetti MG, Fadda M (2022) New insights into fever phobia: a pilot qualitative study with caregivers and their healthcare providers. Eur J Pediatr 182:651–659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Milani GP, Corsello A, Schulz PJ, Fadda M, Giannì ML, Alberti I, Comotti A, Marchisio P, Chiappini E, Peroni D (2023) Childhood fever and medical students: a multicenter, educational intervention. Acta Paediatr 112:1954–1961 [DOI] [PubMed] [Google Scholar]
- 45.Arias D, Chen TF, Moles RJ (2019) Educational interventions on fever management in children: a scoping review. Nurs Open 6:713–721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Milani GP, Corsello A, Fadda M, Falvo I, Giannì ML, Marseglia GL, Cuppari C, Bruzzese E, Bianchetti MG, Schulz PJ, Peroni D, Marchisio P, Chiappini E (2022) Perception, knowledge and attitude towards childhood fever: a survey among final-year medical students. Br J Clin Pharmacol 89:261–267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Clericetti CM, Milani GP, Bianchetti MG, Simonetti GD, Fossali EF, Balestra AM, Bozzini MA, Agostoni C, Lava SAG (2019) Systematic review finds that fever phobia is a worldwide issue among caregivers and healthcare providers. Acta Paediatr 108:1393–1397 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.