Abstract
Purpose of Review
The tibial tubercle osteotomy (TTO) is a versatile surgical technique used to treat a range of patellofemoral disorders, including patellar instability, painful malalignment, focal chondral defects, and patellar maltracking that have failed conservative therapies. TTO is a personalized procedure that can be tailored to the pathoanatomy of the patient based on physical examination and imaging. The complication rate associated with TTO strongly depends on the indication for surgery, the severity of the patient’s condition, and the surgical approach. Despite the literature on TTO, to our knowledge, no single source has addressed the indications, techniques, outcomes, and complications of this procedure. The purpose of this article is to serve as such a valuable resource.
Recent Findings
Highlights from recent studies we would like to emphasize are two-fold. First, maintaining a distal cortical hinge yields lower complication rates than osteotomies involving complete tubercle detachment with classic or standard techniques. Second, based on current evidence, TTO consistently provides symptomatic relief, and most patients can return to work or sport at their pre-operative level within 3 and 6 months, respectively.
Summary
TTO is a personalizable surgical technique that may be utilized for multiple patellofemoral disorders and is associated with good outcomes.
Keywords: Tibial tubercle osteotomy, Knee, Patellofemoral, Instability
Introduction
The tibial tubercle osteotomy (TTO) was first described as a medial and distal relocation of the tibial tubercle to treat patellar instability [1]. Its application has since expanded and has become a well-recognized surgical option for addressing a variety of patellofemoral conditions, including focal patellar and trochlear chondral defects, osteoarthritis, and refractory pain in the setting of patellofemoral malalignment, with or without instability [2, 3]. The goal of the TTO is to improve the biomechanics of the knee by correcting patellar tracking, improving the stability of the patella within the trochlea, and offloading the chondral undersurface of the patella, ultimately reducing pain and improving function [4]. Although numerous clinical studies have highlighted the success of TTO, it is not without complications [5–9]. As such, the addition of TTO should be made on an individual basis with careful consideration of a multitude of factors. The purpose of this article is to present up-to-date indications for TTO, highlight various techniques, outline surgical complications, and assess the reliability of surgery for patients to return to work or sport successfully. A brief summary of relevant pathoanatomy, biomechanics, and clinical assessment will also be reviewed.
Pathoanatomy and Biomechanics
Patients presenting with symptomatic patellofemoral pathology often have abnormal osseous anatomy and/or soft tissue imbalances about the knee. Understanding normal anatomy and biomechanical relationships is foundational to identifying pathoanatomy and ultimately determining appropriate surgical treatment.
The patella is a sesamoid bone located anteriorly in the knee embedded in the quadriceps tendon. As the knee flexes and extends, the patella glides in the trochlear groove, increasing the biomechanical leverage of the quadriceps [10]. The medial patellofemoral ligament (MPFL) provides static stability and is the primary restraint to lateral instability in the first 30 degrees of flexion. The trochlear groove also provides additional static stability essential for deep knee flexion. Dynamic stability comes from surrounding musculature and relies on a balance of forces across the knee [11]. Any morphologic insufficiencies or disruptions to the static and dynamic stabilizers may lead to patellar instability.
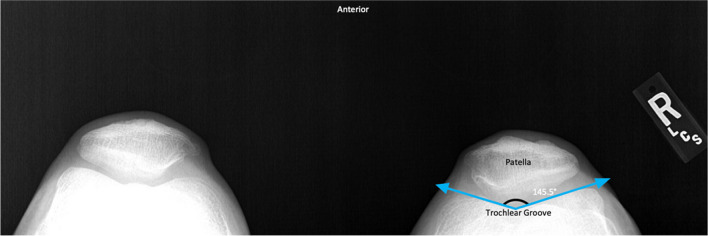
Trochlear dysplasia involves morphologic variation to the trochlear groove that can alter tracking and is defined by a sulcus angle of more than 145 degrees (Fig. 1) [11, 12]. The Dejour classification has been described to characterize trochlear groove morphological abnormality [13]. In brief, this classification comprises Grades A-D, which are determined by the presence of double contour, crossing sign, and/or supratrochlear spurs on lateral radiographs. Overall, this classification system has been heavily scrutinized for poor reliability, reproducibility, and limited clinical utility in treatment decision-making [14]. Notably, a recent study has demonstrated improved reliability when radiographic assessment is combined with advanced imaging such as CT or MRI [14, 15].
Fig. 1.
Sulcus Angle. Merchant view radiograph demonstrating an increased sulcus angle greater than 145° consistent with trochlear dysplasia of the right knee
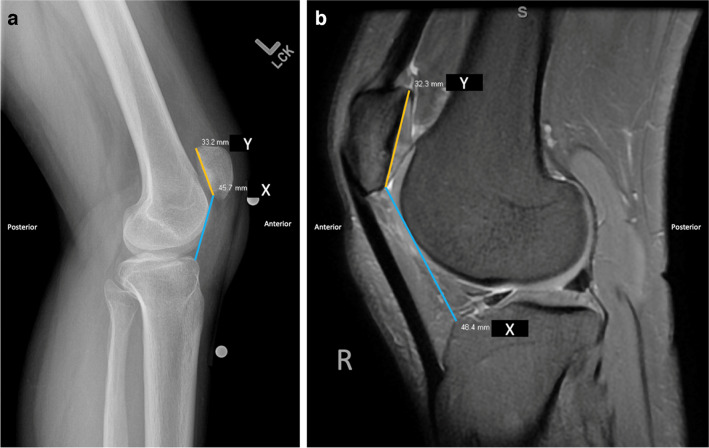
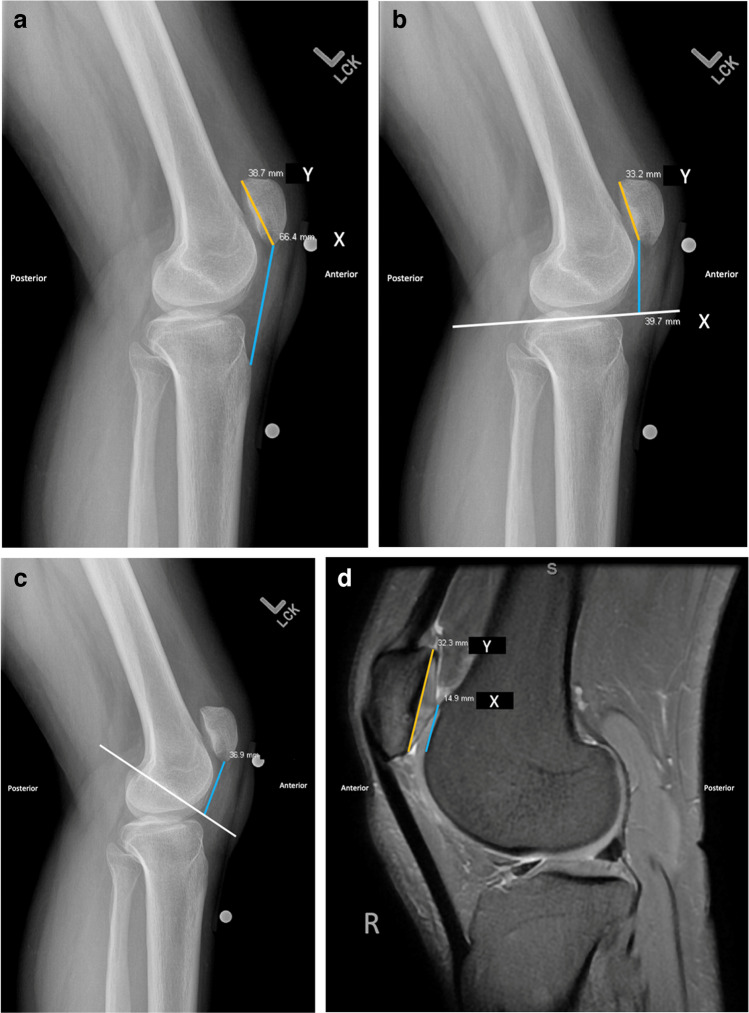
Patella alta also contributes to disrupted patellofemoral kinematics that can affect the angle of flexion at which engagement with the trochlea commences. Effectively decreasing osseous restraint through a larger arc of motion places patients at higher risk for patellar instability [16–18]. Patella alta changes the contact area and increases the mechanical stress of the joint [16, 19]. The preferred method to assess patella alta for the senior authors (RMF, SLS) is the Caton-Deschamps index (CDI) (Fig. 2a and b) [20, 21]. Patella alta is characterized by CDI > 1.2 as measured on an X-ray, computed tomography (CT), or magnetic resonance imaging (MRI) [17, 22]. Alternative patellar height evaluation includes the Insall-Salvati method, Blackburne-Peel method, plateau-patella angle, and extension of Blumensaat’s line using conventional radiographs (Fig. 3a-c). More recently, the patellotrochlear index using sagittal MRI was introduced to assess for true patellotrochlear engagement of the articular cartilage surfaces (Fig. 3D) [23].
Fig. 2.
a Caton-Deschamps Index. Lateral radiograph of a left knee measuring the distance between the inferior patellar articular surface and the anterior angle of the tibial plateau (blue line) compared with the length of the patellar articular surface (yellow line). b: Caton-Deschamps Index. Sagittal T2-weighted MRI of a right knee demonstrating the Caton-Deschamps Index. A ratio (X:Y) greater than 1.2 indicates patella alta
Fig. 3.
a Patellar Height Measurements. Lateral radiograph of a left knee demonstrating the Insall-Salvati Index (X:Y) by measuring the length of the patellar tendon (blue line) compared to the total patella length (yellow line). b: Patellar Height Measurements. Lateral radiograph of a left knee demonstrating the Blackburne-Peel Index (X:Y) by measuring the distance from the horizontal tibial plateau (white line) to the inferior patellar articular surface (blue line) compared to the length of the patellar articular surface (yellow line). c: Patellar Height Measurements. Lateral radiograph of a left knee demonstrating the Blumensaat Line by measuring the perpendicular distance from the intercondylar line of the femur (white line) to the inferior patella (blue line) d: Patellar Height Measurements. Sagittal T2-weighted MRI of a right knee demonstrating the patellotrochlear index by measuring the distance between the superior most trochlear cartilage to the inferior most patellar articular cartilage (blue line) compared to the length of the patellar articular surface (yellow line). A ratio (X:Y) less than 0.18 indicates patella alta
Axial forces applied to the patella are important contributors to patellofemoral alignment. Supraphysiologic lateral forces can predispose to patellofemoral instability, lateral patellar overload, and pain [16]. The Q-angle is the angle created between two intersecting lines measured using the vector of pull by the quadriceps from the middle of the patella to the anterior superior iliac spine and another line from the tibial tubercle through the center of the patella (Fig. 4) [10]. Historically, this angle served as an indicator of the lateral force vector, with normal values reported between 14–16 degrees for men and 16–18 degrees for women [24]. An excessive Q-angle outside this range increases the lateral pull of the quadriceps femoris muscle on the patella and potentiates patellofemoral disorders [25]. Q-angle was previously heavily utilized to guide the necessity for TTO; however, a wide degree of interobserver and intraobserver reliability has made it more clinically obsolete.
Fig. 4.
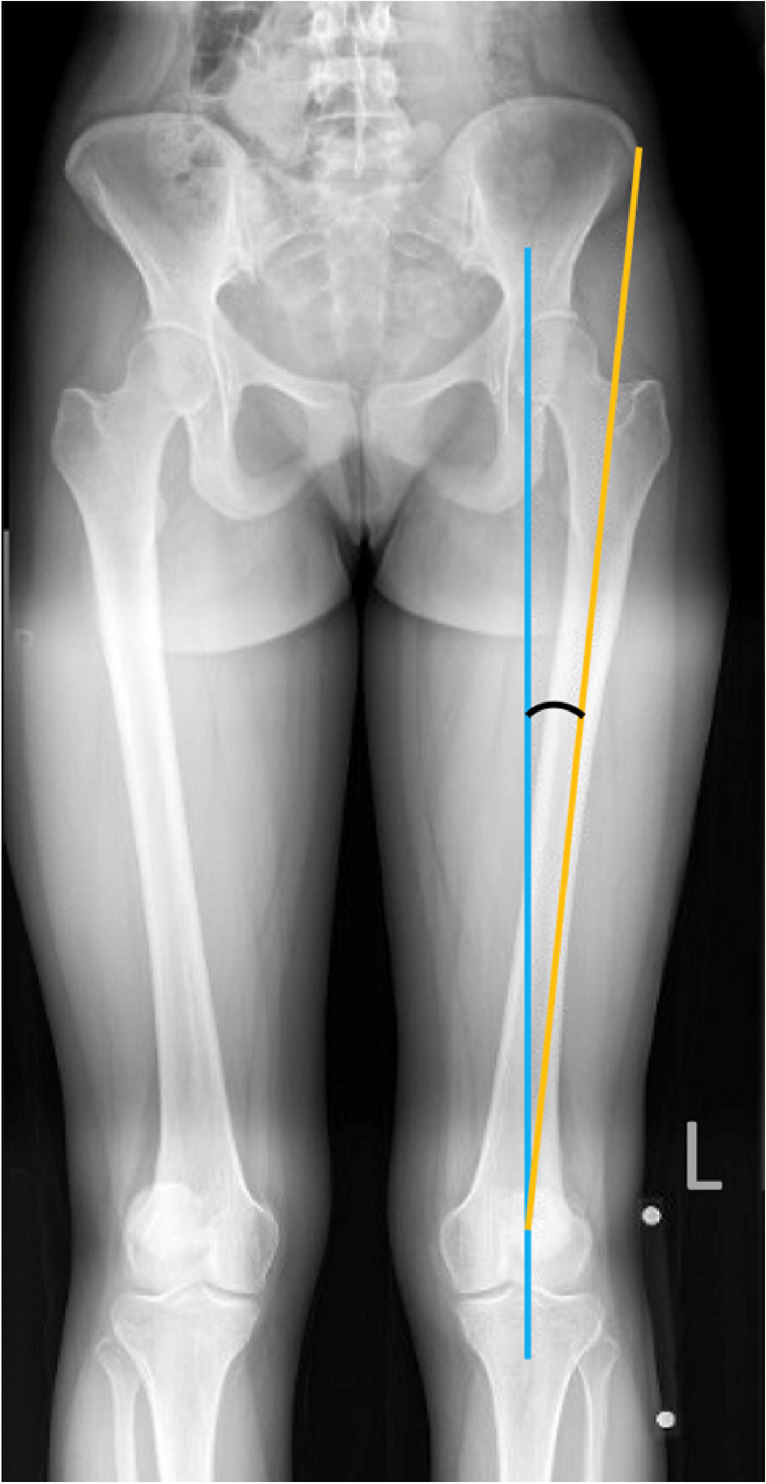
Q-Angle. AP radiograph measuring the angle between a line from the anterior superior iliac spine to the mid-patella and a vertical line connecting the center of the patella with the tibial tubercle. Normal values are between 14–16° for men and 16–18° for women
Q-angle has been replaced by the more sensitive tibial-tuberosity-to-trochlear-groove (TT-TG) distance described by Dejour [20]. Using superimposed axial CT or MRI slices, two parallel lines are drawn, with one line through the deepest point of the trochlear groove and the other through the center of the most proximal portion of the tibial tuberosity [26]. The distance between these parallel lines is measured on another line tangent to the posterior condylar axis. (Fig. 5a and b) [27]. The TT-TG distance in patients without patellofemoral symptoms in full extension is between 10 and 20 mm [21]. A TT-TG distance exceeding 20 mm is considered pathological and is associated with a greater risk of patellar instability, though the measurement of TT-TG is variable based on patient demographics, imaging modality, knee flexion angle, and weightbearing status [21, 27, 28]. Additionally, TT-TG distance depends on the femoral reference point, and caution must be taken for patients with excessive femoral anteversion or tibial external rotation, as these deformities may misrepresent the TT-TG [16, 29].
Fig. 5.
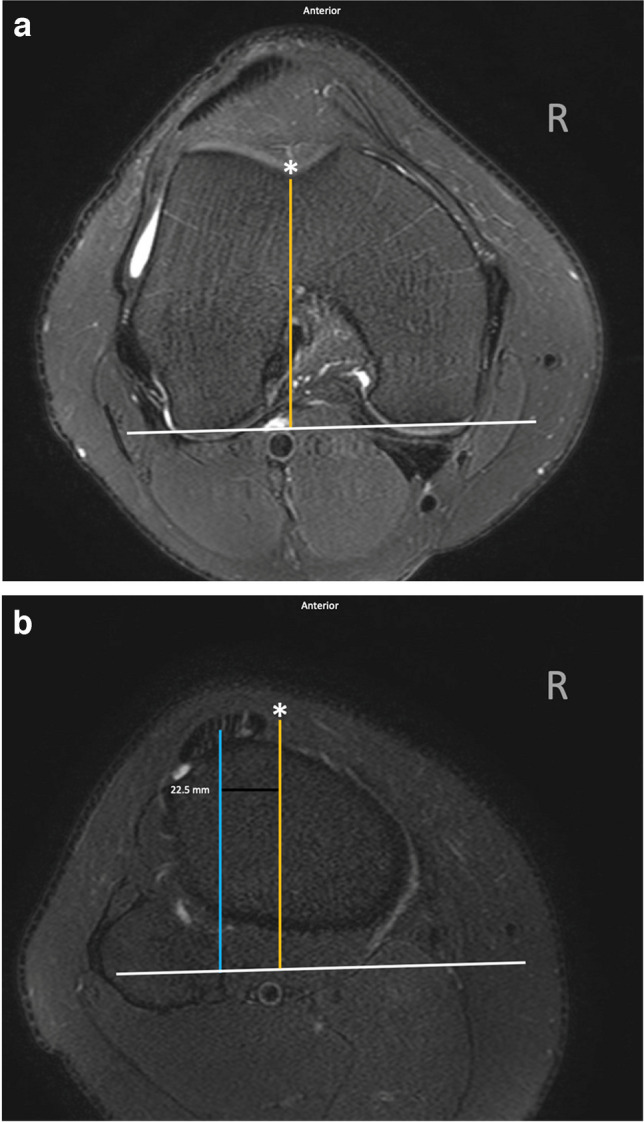
TT-TG. Axial T2-weighted MRI of a right knee demonstrating (a) the measurement between the deepest point of the trochlear groove (asterisk along the yellow line) along a line parallel to the posterior condylar axis (white line) superimposed with (b) the center of the tibial tuberosity (blue line). TT-TG values greater than 20 mm are considered abnormal
Patellar tilt is also measured by superimposing two axial view images of the knee. It can be evaluated on Sunrise/Merchant or lateral radiographs, MRI, and CT [30]. The first image should be through the center of the patella and the second through the reference trochlear cut. Two lines are drawn, the first through the patellar axis and the second through the posterior condylar line. The tilt is the angle between those two lines (Fig. 6). The tilt is measured with and without quadriceps contraction. The tilt of the patella can lead to abnormal forces across the joint, whereas excessive overload can predispose to focal chondral degeneration [30, 31].
Fig. 6.
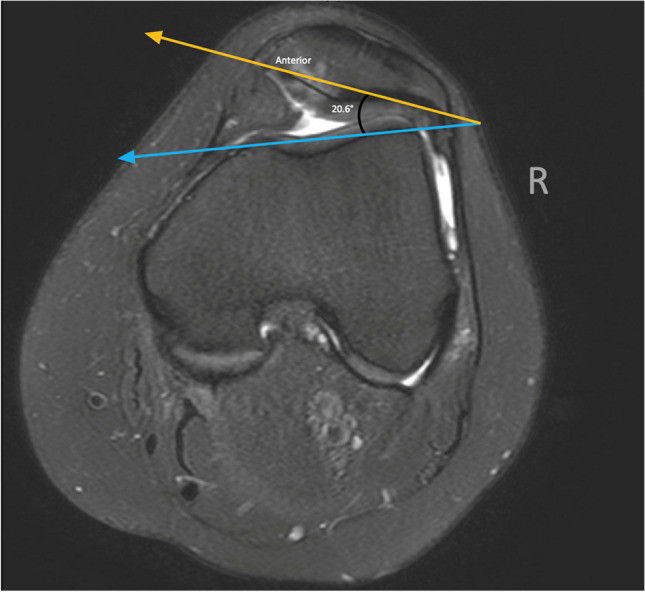
Patellar Tilt. Axial T2-weighted MRI of a right knee demonstrating lateral patellar tilt evaluated by measuring the angle between the anterior condylar line (blue line) and a line through the maximum width of the patella (yellow line). Patellar instability is often associated with a patellar tilt angle greater than 20 degrees
Clinical Evaluation
A complete and thorough history and physical examination should be pursued, encompassing the onset, location, and duration of symptoms. Differentiating symptoms of instability versus pain is particularly important in guiding treatment. In patients who endorse patellofemoral instability, it is important to inquire about the mechanism of injury, frequency of instability events, and underlying medical history that may predispose ligamentous laxity. Reporting of mechanical symptoms or swelling may be suggestive of chondral injury.
Physical examination should involve a complete knee examination, as well as overall limb alignment, gait, and dynamic strength assessment. In the setting of patellar instability, assessment may demonstrate malalignment (e.g., knee valgus), hip and knee malrotation, increased passive patellar translation, patellar apprehension, and/or a J sign [17, 22]. It is important to assess for apprehension with knee flexion angle greater than 30° or the presence of a “jumping” J-sign, as these are poor prognostic indicators for soft tissue stabilization alone, and would warrant a bony procedure such as a TTO [32, 33]. In the instance of cartilage injury, the presence of a knee effusion, a positive compression test, and pain with deep knee flexion with or without crepitus are often present.
Standard radiographic imaging of the knee, including bilateral weightbearing anteroposterior, Rosenberg (posteroanterior view with 45 degrees flexion), low-flexion axial (e.g., Merchant), and lateral radiographs of the affected limb should be utilized to assess for any anatomic pathology contributing to patellar instability, including trochlea dysplasia and patellar malposition. Full-length lower extremity radiographs can be particularly useful in the setting of suspected coronal plane malalignment. Advanced imaging is also useful for preoperative planning. Magnetic resonance imaging (MRI) remains the gold standard for evaluating osteochondral surfaces, soft tissues (e.g., MPFL), and osseous contusions. Computed tomography (CT) is less commonly obtained but can be very helpful for pre-operative planning when rare significant torsional abnormalities are present [16].
Surgical Indications
Acute first-time patella dislocation has traditionally been treated with conservative measures, especially without evidence of a loose body or fracture [4, 34, 35]. These patients are managed with nonsteroidal anti-inflammatory drugs (NSAIDs) for pain and inflammation, activity modification, patellar stabilization utilizing a J-brace or sleeve, and physical therapy emphasizing quadriceps, gluteal, and core strengthening exercises [4, 11, 34, 36, 37]. Surgery is generally indicated for recurrent patella dislocation where anatomical abnormalities contribute to patellar instability or in those who have failed to respond to conservative therapy [4, 11, 34, 36, 37]. Early surgical intervention in the setting of first-time dislocation is typically only considered with unstable chondral injuries or in patients with a high chance of recurrent instability attributed to high-risk anatomy [16].
Well-defined and widely agreed upon surgical indications for tibial tubercle osteotomy remain to be seen. However, this procedure is typically pursued in combination with soft tissue balancing and/or cartilage restoration procedure in the setting of refractory patellofemoral pain/instability with underlying patellofemoral malignment and/or excessive patellar tilt [3, 16, 38]. The technique used for TTO is individualized, often multiplanar, and should be carefully chosen in reference to the clinical picture, position, and biomechanics of the tibial tuberosity, patella, and quadriceps tendon. In general, TTO can be considered in skeletally mature patients with excessive lateralized patellar force vector (TT-TG > 15–20) or excessive patellar height (CDI > 1.2) in order to prevent recurrent patellar instability or to offload patellofemoral cartilage injury [3, 16]. TTO may also be considered with isolated lateral patellofemoral compartment overload that has failed conservative measures or prior arthroscopic intervention (i.e., lateral release) [39].
AMZ is useful in isolation to offload distal or lateral patellar chondral lesions or can be combined with cartilage restoration for medial, central, pan-patellar, and bipolar lesions [40]. In this setting, AMZ is effective in patients with an elevated TT-TG distance measurement (> 15 mm) to correct the lateralized force vector and unload the patellofemoral joint. The aim of TTO AMZ is to achieve a TT-TG distance closer to 10–12 mm or an intra-operative Tibial Tubercle -Sulcus Angle of 0° [40].
The risks of distalization are higher, and so should be the threshold for surgical intervention. With a complete detachment of the tibial tuberosity, damage to local vascularity and increased mechanical stress at the attachment site may lead to an increased risk of complications, including fracture, loss of fixation, delayed union, or nonunion [41, 42]. Most patients with low-grade patella alta can be managed without bony work and tend to do well from a clinical perspective. However, to evenly distribute forces concentrated on the distal aspect of the patellofemoral joint, distalization can be performed. One of the senior authors (SLS) recommends distalization for symptomatic patella alta with a CDI > 1.4 only with a post-surgical CDI correction goal of 1.1–1.2 [40].
Techniques: A Historical Perspective
Roux carried out the first recorded operation for distal realignment, which involved a medial transfer of the lateral half of the patella tendon [20, 36, 43]. Using an osteotome to create a mid-line patella tendon split, the lateral half of the tendon was detached from the tibia while sparing a distal periosteal hinge and slid medially under the intact medial half of the patella tendon. Goldthwait described a similar distal patellar realignment procedure, and thus, medialization of the patellar tendon became known as the Roux-Goldthwait procedure [44–46].
Several modifications to the Roux-Goldthwait procedure have since been described. Elmslie and Trillat popularized the flat axial plane osteotomy of the tibial tubercle for medial transfer aimed to mitigate instability secondary to patellofemoral malalignment and increased lateralized force vector of the patella [36, 47]. Hauser proposed another modification, including a distal and medial patella shift to further increase constraint and reduce the risk of lateral instability [48]. Unfortunately, this procedure was shown to result in a high incidence of late osteoarthritis resulting from increased patellofemoral pressure and has become essentially obsolete [49–51].
For pain associated with patellofemoral arthritis, Maquet first described a straight anteriorization osteotomy, which requires an iliac crest bone graft to allow for the proper degree of anteriorization [52, 53]. Maquet recommended 2–2.5 cm of anterior tibial tubercle elevation to decrease the cartilage contact pressure. Despite early success, this procedure has largely fallen out of favor due to long-term follow-up studies demonstrating high rates of soft tissue and wound complications [54, 55].
Ultimately, Fulkerson popularized the idea of anteromedialization (AMZ) by using an oblique osteotomy to anteriorize (Maquet concept) and medialize (Elmslie-Trillat concept) the tibial tubercle in a multiplanar fashion [56]. In this approach, anteriorization and medialization for the planned correction are considered separately and calculated preoperatively [57]. The AMZ osteotomy is performed either free-hand or with a proprietary cutting jig and the degree of obliquity can be modified depending on the desired amount of AMZ. An oblique cut is extended from the medial origin of the patella tendon to the tibial tuberosity. The tuberosity is fully released using a reciprocating saw for the medial and lateral proximal cuts and osteotomes to release the patella tendon at the distal insertion. The mobile osteotomized tibial tuberosity is translated medially to the desired position using a ruler based on pre-operative calculations. The tuberosity fragment is then secured using screw fixation [16, 57]. This technique has been commonly used to address both instability and offloading pressure in osteoarthritis [58]. The advantage of the Fulkerson combined shift is that it addresses the increased patellofemoral forces with the anteriorization component and then addresses the mechanical alignment issues and efficiency of the patellofemoral mechanism with the medialization component [59]. Biomechanical models have shown that AMZ decreases chondral contact pressure on the lateral patellar facet, which may ultimately alleviate pain in patients with concurrent patellar instability [2, 20, 60]. Additionally, compared to isolated medialized TTO, AMZ TTO demonstrated significantly decreased medial compartment contact pressures in the setting of patellofemoral dysplasia [61]. This technique has the advantage that there is no requirement for bone grafting, and fewer complications arise due to the maintenance of a viable soft tissue envelope [52, 62].
Fulkerson also described an alternative straight anteriorization osteotomy based on the AMZ TTO. This approach does not require bone grafting, which potentially improves fixation and reduces the high complication rate associated with the classic Maquet anteriorization technique. Straight anteriorization osteotomy has been shown to decrease the mean trochlear contact pressures without a medial shift of the center of force [63]. While AMZ osteotomy has broader applications, straight anteriorization can be used in a subset of patients, particularly those with medial patellofemoral chondral defects [63].
Distalization is effective in cases of patella alta. In this procedure, the periosteum is cut 4 cm distally to the patellar tendon insertion, and a periosteal elevator is used to peel the periosteum distally. A V-cut is made, followed by a transverse cut in the proximal part of the tubercle. This tibial tubercle shingle is then moved distally and secured with self-tapping cortical bone screws [41]. Distalization effectively corrects patellar height, reducing the distal load on the patella and providing stabilization through earlier engagement of the patella in the trochlear groove [64]. This is typically performed in conjunction with AMZ to offload painful chondrosis.
Present techniques have evolved to include uniplanar (i.e., isolated anteriorization, distalization, proximalization) and multi-planar corrections as part of the wider armamentarium of TTO subtypes. Depending on patient selection and surgical objectives, multiplanar correction often includes medialization or AMZ combined with distalization [20, 60]. Merchant has developed a multi-directional TTO technique, offering surgeons the ability to precisely and reproducibly move the tibial tubercle in various directions while minimizing the risk of tibial stress fractures [65, 66]. In this technique, a compound wedge cut comprising the tibial tubercle and patellar tendon forms the primary wedge. For corrections involving medialization, a secondary wedge of bone is created just medial to the primary wedge. The primary and secondary bone wedges are then transposed, and the extent of the medialization is equivalent to the width of the secondary wedge. The primary wedge is secured using low-profile 3.5 mm cannulated screws. Anteromedialization TTO incorporates the aforementioned technique along with the placement of bone graft or bone void filler posterior to the primary wedge. Conversely, unidirectional TTO (anteriorization, distalization, or proximalization) involves repositioning the primary bone wedge, eliminating the need for a secondary bone wedge. This ensures a safe approach with minimal soft tissue dissection and reduced cortical violation. Additionally, this technique facilitates intra-operative modularity and offers a reproducible and teachable method to perform otherwise complex and multi-planar corrections. While evidence is mounting, there is still a paucity of midterm and long-term follow-up to support routine use of the Merchant system. Additionally, bone voids require synthetic bone grafting in some cases, which adds cost and can be a major challenge in the setting of postoperative infection.
Outcomes
Generally, TTO has been reported to have favorable outcomes in improving patellar stability, reducing patellofemoral pain, and restoring normal patellar tracking [5, 67]. The outcomes and success rates of TTO can vary depending on several factors, including the specific indication for surgery, the patient population, and the expertise of the surgeon. While it is essential to note the definition of success may vary across studies, the ability to return to work (RTW) or return to sport (RTS) is an important factor for patients undergoing elective procedures and contributes to patient satisfaction [1, 2, 68]. Therefore, physicians must advise their patients on their ability to RTW or RTS following surgery while considering the functional demands of the patient. The timing for RTW and RTS depends on individual healing and the nature of the job or sport [69–71].
Most patients RTW to their pre-operative capacity, although there is a significant difference in the time it takes for physically demanding jobs compared to sedentary professions. In a study evaluating an active military population who underwent TTO, 63% of patients successfully returned to military function. The remaining 37% were unable to return to modified military activity due to knee-related limitations [67]. Zarkadis et al. demonstrated that 78% of military service members were able to return to duty requiring moderate to very heavy occupational demand with significantly decreased patient-reported knee pain [72]. In a limited series of 36 civilian patients undergoing TTO, Buuck and Fulkerson reported that 19% of patients successfully resumed heavy labor, 25% moderate labor, and 50% sedentary occupations [73]. Notably, this study failed to report pre-operative occupational demand categories and included a comparatively heterogeneous patient population. Kingery et al. found over 95% of patients who underwent TTO had returned to work one year post-operatively with an average RTW of 3 months [1]. Patients with physically demanding jobs required slightly more time for recovery, with an average RTW of 4.99 ± 5.33 months [1]. In a retrospective study, Agarwal et al. reported 91.9% of patients were able to RTW by 2.8 ± 2.6 months following TTO [68]. Pestka et al. demonstrated a similar RTW (2.8 months) with a dose-dependent relationship between occupational intensity and time away from work [74].
The standardized TTO postoperative protocol instructs patients to maintain toe-touch weightbearing restrictions in a hinged knee brace locked in full extension for up to six weeks. It is essential to counsel patients regarding the minimum time needed to allow for healing and functional recovery. Advancements are dependent on individual progress, and this may vary depending on a variety of factors, such as occupation, age, and motivation. For example, the rehabilitative course has been shown to be more favorable in patients with sedentary or low-intensity occupations in their ability to RTW at a faster rate compared to those with physically demanding occupations [68]. Zarkadis et al. identified an appreciable connection between age and physical demand on the ability to RTW following TTO in a military population [72]. In this study, risk factors for failure to RTW were age less than 30 years and more physically demanding junior enlisted service positions compared to senior officer ranks. Additionally, socioeconomic status, disability coverage, workers’ compensation, comorbidities, and health insurance coverage are among several other factors that impact motivation for a patient to RTW and should be considered pre-operatively [68].
Another important measure for a large population of patients indicated for TTO is the time to RTS [75–77]. This information is essential for surgeons and patients to establish realistic postoperative expectations. In a systematic review including 85 studies, Koshino et al. reported the most common RTS timeline in patients following TTO is six months postoperatively [69]. In a retrospective case series, Liu et al. found 83.3% of patients returned to at least one sport, and 62.5% of patients were able to resume more than one sport on average 7.8 months postoperatively. Of these, 77.5% believed they returned at the same or higher level. Despite TTO effectively returning athletes to competitive sports, significant strength deficits persist six months after surgery [78]. Physicians can use these results to counsel patients that returning to competitive sports is safe with good clinical outcomes. In a more recent study, Kingery et al. reported a mean time of 9.21 months to return to athletic activity [1]. Athletes should be advised that a slower recovery and extended recovery timeline may necessitate 9–12 months before safely returning to competition-level action.
Complications
Tibial tubercle osteotomy is a complex surgical procedure with a significant risk of complication. The most common complications following TTO include infection, skin necrosis, delayed or nonunion, thromboembolic events, and tibial fracture [5–9]. Previous studies have suggested the rate of complication of TTO depends largely on the surgical approach and the direction of the tibial tubercle transfer [9]. Symptomatic hardware removal is the most frequently reported complication after TTO, with an estimated rate between 12.6% and 36.7%. The overall complication rate, excluding hardware removal and instability events, is estimated to be between 4.6% and 6.2% [9, 52, 79]. However, Johnson et al. found that smaller low-profile screws measuring 3.5-mm were less painful and less likely to need removal compared to larger screws [80]. Bio-integrative compression screws have the potential to reduce symptomatic hardware while improving the strength and stability of an osteotomy construct, though further clinical testing is needed.
It has been well documented that osteotomies involving complete detachment of the tubercle have an increased risk of complication compared with those in which a distal cortical hinge is preserved [9]. Kanamiya et al. suggested that periosteal insult after complete tibial tubercle detachment arrests the blood flow and increases the risk for nonunion [81]. Notably, Luhmann et al. found complications decreased from 5.9% to zero when intact periosteum was left at the distal portion of the osteotomy [82]. Avoiding distal “step cuts” and ensuring a proximal buttress with bone grafting can mitigate the risks of distalization.
Nonunion is a serious complication following tibial tubercle osteotomy [9]. Fortunately, rates of nonunion found within the literature are low and overall reassuring [83]. Choi et al. observed radiographic union in 46/51 TTOs (90.2%) [84], Le Moulec et al. in 59/63 (93.7%) [85], Mendes et al. in 64/67 (95.5%) [86], Young et al. in 41/42 (97.6%) [87], and Zonnenberg et al. found that union was achieved in 22/22 TTOs (100%) [88].
Despite high rates of union, it is essential to consider technique and relocation of the tibial tubercle to minimize the risk of nonunion. It has been hypothesized that distalization of the tibial tubercle may increase stress on the osteotomy site and ultimately contribute to nonunion [35, 73]. A thin bone shingle and small proximal buttress can compromise union rate and lead to fracture [73]. Improper technique resulting in periosteal stripping or thermal necrosis decreases bone perfusion and higher rates of nonunion [73]. Various methods of fixation of the tibial tubercle have been proposed. Regardless of the technique, adequate fixation must be ensured. In a study by Cosgarea et al., it was concluded that insufficient fixation of the TTO consequentially results in nonunion [89]. Hence, care should be taken to place screws perpendicular to the osteotomy site to ensure maximum contact and compression of the two surfaces. Payne and colleagues found that compression screw fixation limits the risk of nonunion at the osteotomy site to 3.7% [9]. Certain patient factors such as obesity, smoking, lack of compliance, and aggressive rehabilitation may also predispose to nonunion [9, 90].
Another recognized risk of tibial tubercle osteotomy is proximal tibia fracture. Similar to the risk of nonunion, the risk of fracture has been related to surgical technique, osteotomy size, osteotomy tools, and rehabilitation protocols [8, 91, 92]. The reported fracture rates of the proximal tibia range from 2.6–8% [20, 92]. Large cortical defects or the improper use of surgical instrumentation can increase the risk of fracture or propagate the osteotomy distally or posteriorly [73]. Rapid and aggressive physical therapy may also increase fracture risk. By allowing patients to weightbear as tolerated, Stetson and Fulkerson et al. reported a higher tibial fracture rate of 8–11% [91]. Alternatively, in a case series by Bellemans and Stetson, there were no reported fractures after 12 weeks post-operatively with the implementation of weightbearing restrictions [92]. This stresses the significance of protected weightbearing, early activity restriction, and progressive rehabilitation to mitigate the risk of tibial fracture [36].
Complications following TTO can be minimized with preoperative assessment and planning, careful attention to detail, technical execution, and postoperative rehabilitation compliance.
Future Direction
Given the complexity of patient presentation, imaging findings, and indication for surgical intervention, TTO remains a highly personalized procedure with multiple high-risk complications and a long postoperative course. Based on patient-specific bony morphology and underlying pathology, TTO can be used in isolation or in conjunction with additional procedures, including cartilage restoration and soft tissue balancing, to address malalignment associated with patellofemoral overload, instability, and/or symptomatic chondral defects. Moving forward, advancements in surgical techniques and tools may lead to more minimally invasive approaches, which reduces the risk of infection and rate of complications. Novel techniques should continue to mitigate soft tissue dissection, optimize bone cut stability, and incorporate improved materials such as bone grafting and fixation devices. Artificial intelligence, machine learning, and improved imaging technology may also refine risk stratification for recurrence or enhance pre-operative planning that allows surgeons to tailor the procedure to each patient's unique anatomy. Furthermore, future research and the development of personalized medicine may focus on predicting patient outcomes and assessing potential risks more accurately. This may ultimately help surgeons better identify suitable candidates for elective TTO and manage patient expectations. It is important to remember that a myriad of approaches exist for various pathologies, and this must be considered to truly compare outcomes across the literature.
Conclusion
Although TTO is a relatively frequently performed procedure amongst orthopedic surgeons, specific guidelines for surgical indication and postoperative management continue to develop. Methods for diagnosis and treatment will continue to vary based on individual patient presentation, pathology, comorbidities, and personal factors. Surgeons should continue to counsel their patients on the risks and benefits of TTO to guide the shared surgical decision-making process and establish realistic patient expectations.
Author Contributions
M.L.C. (Contribution: conceptualization, writing – original draft, writing - review & editing)
D.J.S. (Contribution: conceptualization, writing – original draft, writing – review & editing)
B.P.E. (Contribution: conceptualization, visualization, writing – original draft, writing – review & editing)
Y.R. (Contribution: conceptualization, validation, writing – review & editing)
K.S.M. (Contribution: visualization, writing – review & editing)
S.L.S. (Contribution: conceptualization, resources, supervision, validation, visualization, writing – review & editing)
R.M.F. (Contribution: conceptualization, resources, supervision, validation, visualization, writing – review & editing)
All authors reviewed the manuscript and approved the final version. The authors agree to be accountable for all aspects of the work.
Funding
There were no sources of funding that played a role in this study.
Data Availability
No datasets were generated or analysed during the current study.
Declarations
Competing Interests
RMF reports consultant fees from Allosource, Arthrex, and JRF Ortho; speaking fees from Allosource, Arthrex, JRF Ortho, and Ossur; research support from Aesculap Biologics and Arthrex; publishing royalties from Elsevier. SLS reports consultant fees from Arthrex, BioVentus, CONMED Linvatec, JRF Ortho, Kinamed, Smith & Nephew, and Vericel; speaking fees from Arthrex, CONMED Linvatec, JRF Ortho, Kinamed, Smith & Nephew, and Vericel; research support from JRF Ortho and Ossio; IP royalties from CONMED Linvatec; stock or stock options held in Epic Bio, Reparel, Sarcio, and Vivorte. The other authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kingery MT, Bloom DA, Hoberman A, Fliegel B, Alaia MJ, Jazrawi LM, et al. Return to Work and Sport Following Tibial Tubercle Anteromedialization. Bull Hosp Jt Dis. 2022;80(4):226–9. [PubMed] [Google Scholar]
- 2.Belmont PJ Jr, Fisher TF, Bader JM, Lanzi JT, Owens BD, Waterman BR. Anteromedializing Tibial Tubercle Osteotomy for Patellofemoral Instability: Occupational and Functional Outcomes in U.S. Military Service Members. J Knee Surg. 2018;31(4):306–13. 10.1055/s-0037-1603639. [DOI] [PubMed] [Google Scholar]
- 3.Rosso F, Rossi R, Cottino U, Bonasia DE. Tibial tubercle osteotomy for patellofemoral malalignment and chondral disease provided good outcomes: A systematic review. J isakos. 2022;7(2):78–86. 10.1016/j.jisako.2021.10.002. [DOI] [PubMed] [Google Scholar]
- 4.Grawe B, Stein BE. Tibial Tubercle Osteotomy: Indication and Techniques. J Knee Surg. 2015;28(4):279–84. 10.1055/s-0035-1544973. [DOI] [PubMed] [Google Scholar]
- 5.Burger D, Feucht M, Muench LN, Forkel P, Imhoff AB, Mehl J. Good clinical outcomes after patellar cartilage repair with no evidence for inferior results in complex cases with the need for additional patellofemoral realignment procedures: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2022;30(5):1752–68. 10.1007/s00167-021-06728-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caplan N, Nassar I, Anand B, Kader DF. Why Do Patellofemoral Stabilization Procedures Fail? Keys to Success. Sports Med Arthrosc Rev. 2017;25(1):e1–7. 10.1097/jsa.0000000000000135. [DOI] [PubMed] [Google Scholar]
- 7.Knapik DM, Kunze KN, Azua E, Vadhera A, Yanke AB, Chahla J. Radiographic and Clinical Outcomes After Tibial Tubercle Osteotomy for the Treatment of Patella Alta: A Systematic Review and Meta-analysis. Am J Sports Med. 2022;50(7):2042–51. 10.1177/03635465211012371. [DOI] [PubMed] [Google Scholar]
- 8.Lundeen A, Macalena J, Agel J, Arendt E. High incidence of complication following tibial tubercle surgery. J Isakos. 2022;8:81. 10.1016/j.jisako.2022.11.005. [DOI] [PubMed] [Google Scholar]
- 9.Payne J, Rimmke N, Schmitt LC, Flanigan DC, Magnussen RA. The Incidence of Complications of Tibial Tubercle Osteotomy: A Systematic Review. Arthroscopy. 2015;31(9):1819–25. 10.1016/j.arthro.2015.03.028. [DOI] [PubMed] [Google Scholar]
- 10.Loudon JK. Biomechanics and pathomechanics of the patellofemoral joint. Int J Sports Phys Ther. 2016;11(6):820–30. [PMC free article] [PubMed] [Google Scholar]
- 11.Dejour D, Le Coultre B. Osteotomies in Patello-Femoral Instabilities. Sports Med Arthrosc Rev. 2018;26(1):8–15. 10.1097/jsa.0000000000000183. [DOI] [PubMed] [Google Scholar]
- 12.Malghem J, Maldague B. Depth insufficiency of the proximal trochlear groove on lateral radiographs of the knee: relation to patellar dislocation. Radiology. 1989;170(2):507–10. 10.1148/radiology.170.2.2911676. [DOI] [PubMed] [Google Scholar]
- 13.Perry AK, Maheshwer B, DeFroda SF, Hevesi M, Gursoy S, Chahla J, et al. 2022 Patellar Instability. JBJS Rev 10 (11) 10.2106/jbjs.Rvw.22.00054 [DOI] [PubMed]
- 14.Kazley JM, Banerjee S. Classifications in Brief: The Dejour Classification of Trochlear Dysplasia. Clin Orthop Relat Res. 2019;477(10):2380–6. 10.1097/corr.0000000000000886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mousinho R, Ribeiro JNA, Pedrosa FKS, Lima DA, Gonçalves RK, Leite JAD. Evaluation of the Reproducibility of the Dejour Classification for Femoropatellar Instability. Rev Bras Ortop (Sao Paulo). 2019;54(2):171–7. 10.1016/j.rbo.2017.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sherman SL, Erickson BJ, Cvetanovich GL, Chalmers PN, Farr J 2nd, Bach BR Jr, et al. Tibial Tuberosity Osteotomy: Indications, Techniques, and Outcomes. Am J Sports Med. 2014;42(8):2006–17. 10.1177/0363546513507423. [DOI] [PubMed] [Google Scholar]
- 17.Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19–26. 10.1007/bf01552649. [DOI] [PubMed] [Google Scholar]
- 18.Mayer C, Magnussen RA, Servien E, Demey G, Jacobi M, Neyret P, et al. Patellar tendon tenodesis in association with tibial tubercle distalization for the treatment of episodic patellar dislocation with patella alta. Am J Sports Med. 2012;40(2):346–51. 10.1177/0363546511427117. [DOI] [PubMed] [Google Scholar]
- 19.Luyckx T, Didden K, Vandenneucker H, Labey L, Innocenti B, Bellemans J. Is there a biomechanical explanation for anterior knee pain in patients with patella alta?: influence of patellar height on patellofemoral contact force, contact area and contact pressure. J Bone Joint Surg Br. 2009;91(3):344–50. 10.1302/0301-620x.91b3.21592. [DOI] [PubMed] [Google Scholar]
- 20.Hall MJ, Mandalia VI. Tibial tubercle osteotomy for patello-femoral joint disorders. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):855–61. 10.1007/s00167-014-3388-4. [DOI] [PubMed] [Google Scholar]
- 21.Camp CL, Stuart MJ, Krych AJ, Levy BA, Bond JR, Collins MS, et al. CT and MRI measurements of tibial tubercle-trochlear groove distances are not equivalent in patients with patellar instability. Am J Sports Med. 2013;41(8):1835–40. 10.1177/0363546513484895. [DOI] [PubMed] [Google Scholar]
- 22.Wolfe S, Varacallo M, Thomas JD, Carroll JJ, Kahwaji CI. Patellar Instability. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2023, StatPearls Publishing LLC.; 2023. [PubMed]
- 23.Biedert RM, Albrecht S. The patellotrochlear index: a new index for assessing patellar height. Knee Surg Sports Traumatol Arthrosc. 2006;14(8):707–12. 10.1007/s00167-005-0015-4. [DOI] [PubMed] [Google Scholar]
- 24.Skouras AZ, Kanellopoulos AK, Stasi S, Triantafyllou A, Koulouvaris P, Papagiannis G, et al. Clinical Significance of the Static and Dynamic Q-angle. Cureus. 2022;14(5):e24911. 10.7759/cureus.24911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Emami MJ, Ghahramani MH, Abdinejad F, Namazi H. Q-angle: an invaluable parameter for evaluation of anterior knee pain. Arch Iran Med. 2007;10(1):24–6. [PubMed] [Google Scholar]
- 26.Dong C, Zhao C, Li M, Fan C, Feng X, Piao K, et al. Accuracy of tibial tuberosity-trochlear groove distance and tibial tuberosity-posterior cruciate ligament distance in terms of the severity of trochlear dysplasia. J Orthop Surg Res. 2021;16(1):383. 10.1186/s13018-021-02527-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carlson VR, Boden BP, Shen A, Jackson JN, Yao L, Sheehan FT. The Tibial Tubercle-Trochlear Groove Distance Is Greater in Patients With Patellofemoral Pain: Implications for the Origin of Pain and Clinical Interventions. Am J Sports Med. 2017;45(5):1110–6. 10.1177/0363546516681002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pennock AT, Alam M, Bastrom T. Variation in tibial tubercle-trochlear groove measurement as a function of age, sex, size, and patellar instability. Am J Sports Med. 2014;42(2):389–93. 10.1177/0363546513509058. [DOI] [PubMed] [Google Scholar]
- 29.Tensho K, Akaoka Y, Shimodaira H, Takanashi S, Ikegami S, Kato H, et al. What Components Comprise the Measurement of the Tibial Tuberosity-Trochlear Groove Distance in a Patellar Dislocation Population? J Bone Joint Surg Am. 2015;97(17):1441–8. 10.2106/jbjs.N.01313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barbosa RM, da Silva MV, Macedo CS, Santos CP. Imaging evaluation of patellofemoral joint instability: a review. Knee Surg Relat Res. 2023;35(1):7. 10.1186/s43019-023-00180-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hinckel BB, Gobbi RG, Kihara Filho EN, Demange MK, Pécora JR, Camanho GL. Patellar Tendon-Trochlear Groove Angle Measurement: A New Method for Patellofemoral Rotational Analyses. Orthop J Sports Med. 2015;3(9):2325967115601031. 10.1177/2325967115601031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sappey-Marinier E, Sonnery-Cottet B, O’Loughlin P, Ouanezar H, Reina Fernandes L, Kouevidjin B, et al. Clinical Outcomes and Predictive Factors for Failure With Isolated MPFL Reconstruction for Recurrent Patellar Instability: A Series of 211 Reconstructions With a Minimum Follow-up of 3 Years. Am J Sports Med. 2019;47(6):1323–30. 10.1177/0363546519838405. [DOI] [PubMed] [Google Scholar]
- 33.Colatruglio M, Flanigan DC, Harangody S, Duerr RA, Kaeding CC, Magnussen RA. Identifying Patients With Patella Alta and/or Severe Trochlear Dysplasia Through the Presence of Patellar Apprehension in Higher Degrees of Flexion. Orthop J Sports Med. 2020;8(6):2325967120925486. 10.1177/2325967120925486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Caton JH, Dejour D. Tibial tubercle osteotomy in patello-femoral instability and in patellar height abnormality. Int Orthop. 2010;34(2):305–9. 10.1007/s00264-009-0929-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhou K, Bai P, Sun Z, Jia Y, Wang F, Wang X, et al. Distalization of tibial tubercle osteotomy is not necessary for patients with recurrent patellar dislocation accompanied by patella alta and increased TT-TG distance. BMC Musculoskelet Disord. 2022;23(1):838. 10.1186/s12891-022-05779-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gardner EC, Molho DA, Fulkerson JP. Coronal Malalignment-When and How to Perform a Tibial Tubercle Osteotomy. Clin Sports Med. 2022;41(1):15–26. 10.1016/j.csm.2021.07.008. [DOI] [PubMed] [Google Scholar]
- 37.Weaver JK, Wieder D, Derkash RS. Patellofemoral arthritis resulting from malalignment A long-term evaluation of treatment options. Orthop Rev. 1991;20(12):1075–81. [PubMed] [Google Scholar]
- 38.Farr J. Tibial tubercle osteotomy. Techniques Knee Surg. 2003;2:28–42. [Google Scholar]
- 39.Duchman K, Bollier M. Distal realignment: indications, technique, and results. Clin Sports Med. 2014;33(3):517–30. 10.1016/j.csm.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 40.Atzmon R, Steen A, Vel MS, Pierre K, Murray IR, Sherman SL. Tibial tubercle osteotomy to unload the patellofemoral joint. J Cartilage & Joint Preservation. 2023;3(1):100112. 10.1016/j.jcjp.2023.100112. [Google Scholar]
- 41.Palhares G, Hinkley P, Rizy M, Fletcher C, Gomoll A, Strickland S. Tibial Tubercle Osteotomy With Distalization for the Treatment of Patella Alta. Arthrosc Tech. 2023;12(5):e609–14. 10.1016/j.eats.2022.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rood A, Van Sambeeck J, Koëter S, Van Kampen A, Van De Groes SAW. A detaching, V-shaped tibial tubercle osteotomy is a safe procedure with a low complication rate. Arch Orthop Trauma Surg. 2020;140(12):1867–72. 10.1007/s00402-020-03375-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Roux C. Recurrent dislocation of the patella: operative treatment. Clin Orthop Relat Res. 2006;452:17–20. 10.1097/01.blo.0000238832.88304.0e. [DOI] [PubMed] [Google Scholar]
- 44.Goldthwait JEV. Permanent Dislocation of the Patella The Report of a Case of Twenty Years’ Duration, successfully treated by Transplantation of the Patella Tendons with the Tubercle of the Tibia. Ann Surg. 1899;29(1):62–8. [PMC free article] [PubMed] [Google Scholar]
- 45.Roux C. 1979 The classic. Recurrent dislocation of the patella: operative treatment. Clin Orthop Relat Res 144 4–8 [PubMed]
- 46.Goldthwait JE. Slipping or recurrent dislocation of the patella: with the report of eleven cases. American J Bone Joint Surg Am. 2003;85(12):2489. [PubMed] [Google Scholar]
- 47.Trillat A, Dejour H. Diagnosis And Treatment Of Recurrent Dislocations Of The Patella. Rev Chir Orthop Reparatrice Appar Mot. 1964;50:813–24. [PubMed]
- 48.Hauser ED. Total tendon transplant for slipping patella: a new operation for recurrent dislocation of the patella. Clin Orthop Relat Res. 2006;452:7–16. 10.1097/01.blo.0000238831.50186.87. [DOI] [PubMed] [Google Scholar]
- 49.Chrisman OD, Snook GA, Wilson TC. A long-term prospective study of the Hauser and Roux-Goldthwait procedures for recurrent patellar dislocation. Clin Orthop Relat Res. 1979;144:27–30. [PubMed] [Google Scholar]
- 50.Pidoriano AJ, Weinstein RN, Buuck DA, Fulkerson JP. Correlation of patellar articular lesions with results from anteromedial tibial tubercle transfer. Am J Sports Med. 1997;25(4):533–7. 10.1177/036354659702500417. [DOI] [PubMed] [Google Scholar]
- 51.Juliusson R, Markhede G. A modified Hauser procedure for recurrent dislocation of the patella. A long-term follow-up study with special reference to osteoarthritis. Arch Orthop Trauma Surg. 1984;103(1):42–6. 10.1007/bf00451317. [DOI] [PubMed] [Google Scholar]
- 52.Longo UG, Rizzello G, Ciuffreda M, Loppini M, Baldari A, Maffulli N, et al. Elmslie-Trillat, Maquet, Fulkerson, Roux Goldthwait, and Other Distal Realignment Procedures for the Management of Patellar Dislocation: Systematic Review and Quantitative Synthesis of the Literature. Arthroscopy. 2016;32(5):929–43. 10.1016/j.arthro.2015.10.019. [DOI] [PubMed] [Google Scholar]
- 53.Radin EL. The Maquet procedure–anterior displacement of the tibial tubercle. Indications, contraindications, and precautions. Clin Orthop Relat Res. 1986;213:241–8. [PubMed] [Google Scholar]
- 54.Kadambande SS, Auyeung J, Ghandour A, Mintowt-Czyz W. A review of wound healing following Maquet osteotomy. Knee. 2004;11(6):463–7. 10.1016/j.knee.2003.07.005. [DOI] [PubMed] [Google Scholar]
- 55.Marcacci M, Zaffagnini S, Iacono F, Visani A, Petitto A, Neri NP. Results in the treatment of recurrent dislocation of the patella after 30 years’ follow-up. Knee Surg Sports Traumatol Arthrosc. 1995;3(3):163–6. 10.1007/bf01565476. [DOI] [PubMed] [Google Scholar]
- 56.Fulkerson JP. Anteromedialization of the tibial tuberosity for patellofemoral malalignment. Clin Orthop Relat Res. 1983;177:176–81. [PubMed] [Google Scholar]
- 57.Farr J, Cole BJ, Kercher J, Batty L, Bajaj S. Anteromedial Tibial Tubercle Osteotomy (Fulkerson Osteotomy). In: Sanchis-Alfonso V, editor. Atlas of the Patellofemoral Joint. London: Springer, London; 2013. p. 229–31. [Google Scholar]
- 58.Saranathan A, Kirkpatrick MS, Mani S, Smith LG, Cosgarea AJ, Tan JS, et al. The effect of tibial tuberosity realignment procedures on the patellofemoral pressure distribution. Knee Surg Sports Traumatol Arthrosc. 2012;20(10):2054–61. 10.1007/s00167-011-1802-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Carofino BC, Fulkerson JP. Anteromedialization of the tibial tubercle for patellofemoral arthritis in patients > 50 years. J Knee Surg. 2008;21(2):101–5. 10.1055/s-0030-1247803. [DOI] [PubMed] [Google Scholar]
- 60.Farr J. Autologous chondrocyte implantation improves patellofemoral cartilage treatment outcomes. Clin Orthop Relat Res. 2007;463:187–94. [PubMed] [Google Scholar]
- 61.Lamplot JD, Jahandar A, Meyers KN, Gomoll AH, Maher SA, Strickland SM. Anteromedialization Tibial Tubercle Osteotomy Improves Patellar Contact Forces: A Cadaveric Model of Patellofemoral Dysplasia. Am J Sports Med. 2023;51(2):453–60. 10.1177/03635465221138287. [DOI] [PubMed] [Google Scholar]
- 62.Karamehmetoğlu M, Oztürkmen Y, Azboy I, Caniklioğlu M. Fulkerson osteotomy for the treatment of chronic patellofemoral malalignment. Acta Orthop Traumatol Turc. 2007;41(1):21–30. [PubMed] [Google Scholar]
- 63.Rue JP, Colton A, Zare SM, Shewman E, Farr J, Bach BR Jr, et al. Trochlear contact pressures after straight anteriorization of the tibial tuberosity. Am J Sports Med. 2008;36(10):1953–9. 10.1177/0363546508317125. [DOI] [PubMed] [Google Scholar]
- 64.Leite CBG, Santos TP, Giglio PN, Pécora JR, Camanho GL, Gobbi RG. Tibial Tubercle Osteotomy With Distalization Is a Safe and Effective Procedure for Patients With Patella Alta and Patellar Instability. Orthop J Sports Med. 2021;9(1):2325967120975101. 10.1177/2325967120975101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sarin VK, Camisa W, Leasure JM, Merchant AC. Multidirectional Tibial Tubercle Transfer Technique: Rationale and Biomechanical Investigation. J Surg Orthop Adv. 2016;25(3):157–64. [PubMed] [Google Scholar]
- 66.Matthews LS. Chapman’s Orthopaedic Surgery. Philadelphia: Lippincott Williams & Wilkins; 2001. [Google Scholar]
- 67.Fisher TF, Waterman BR, Orr JD, Holland CA, Bader J, Belmont PJ Jr. Tibial Tubercle Osteotomy for Patellar Chondral Pathology in an Active United States Military Population. Arthroscopy. 2016;32(11):2342–9. 10.1016/j.arthro.2016.03.027. [DOI] [PubMed] [Google Scholar]
- 68.Agarwalla A, Liu JN, Wu H-H, Kalbian IL, Garcia GH, Shubin Stein BE. Return to Work Following Tibial Tubercle Osteotomy for Patellofemoral Osteoarthritis and Pain. Cartilage. 2021;13:1066S-73S. 10.1177/1947603520916544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Koshino Y, Taniguchi S, Kobayashi T, Samukawa M, Inoue M. Protocols of rehabilitation and return to sport, and clinical outcomes after medial patellofemoral ligament reconstruction with and without tibial tuberosity osteotomy: a systematic review. Int Orthop. 2022;46(11):2517–28. 10.1007/s00264-022-05480-4. [DOI] [PubMed] [Google Scholar]
- 70.Vivekanantha P, Kahlon H, Cohen D, de Sa D. Isolated medial patellofemoral ligament reconstruction results in similar postoperative outcomes as medial patellofemoral ligament reconstruction and tibial-tubercle osteotomy: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2022;31:2433. 10.1007/s00167-022-07186-x. [DOI] [PubMed] [Google Scholar]
- 71.Liu JN, Wu HH, Garcia GH, Kalbian IL, Strickland SM, Shubin Stein BE. Return to Sports After Tibial Tubercle Osteotomy for Patellofemoral Pain and Osteoarthritis. Arthroscopy. 2018;34(4):1022–9. 10.1016/j.arthro.2017.09.021. [DOI] [PubMed] [Google Scholar]
- 72.Zarkadis NJ, Belmont PJ Jr, Zachilli MA, Holland CA, Kinsler AR, Todd MS, et al. Autologous Chondrocyte Implantation and Tibial Tubercle Osteotomy for Patellofemoral Chondral Defects: Improved Pain Relief and Occupational Outcomes Among US Army Servicemembers. Am J Sports Med. 2018;46(13):3198–208. 10.1177/0363546518800713. [DOI] [PubMed] [Google Scholar]
- 73.Grimm NL, Lazarides AL, Amendola A. Tibial Tubercle Osteotomies: a Review of a Treatment for Recurrent Patellar Instability. Curr Rev Musculoskelet Med. 2018;11(2):266–71. 10.1007/s12178-018-9482-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pestka JM, Feucht MJ, Porichis S, Bode G, Südkamp NP, Niemeyer P. Return to Sports Activity and Work After Autologous Chondrocyte Implantation of the Knee: Which Factors Influence Outcomes? Am J Sports Med. 2016;44(2):370–7. 10.1177/0363546515614578. [DOI] [PubMed] [Google Scholar]
- 75.Ekhtiari S, Haldane CE, de Sa D, Simunovic N, Musahl V, Ayeni OR. Return to Work and Sport Following High Tibial Osteotomy: A Systematic Review. J Bone Joint Surg Am. 2016;98(18):1568–77. 10.2106/jbjs.16.00036. [DOI] [PubMed] [Google Scholar]
- 76.Tjoumakaris FP, Forsythe B, Bradley JP. Patellofemoral instability in athletes: treatment via modified Fulkerson osteotomy and lateral release. Am J Sports Med. 2010;38(5):992–9. 10.1177/0363546509357682. [DOI] [PubMed] [Google Scholar]
- 77.Hoorntje A, Witjes S, Kuijer P, Koenraadt KLM, van Geenen RCI, Daams JG, et al. High Rates of Return to Sports Activities and Work After Osteotomies Around the Knee: A Systematic Review and Meta-Analysis. Sports Med. 2017;47(11):2219–44. 10.1007/s40279-017-0726-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Krych AJ, O’Malley MP, Johnson NR, Mohan R, Hewett TE, Stuart MJ, et al. Functional testing and return to sport following stabilization surgery for recurrent lateral patellar instability in competitive athletes. Knee Surg Sports Traumatol Arthrosc. 2018;26(3):711–8. 10.1007/s00167-016-4409-2. [DOI] [PubMed] [Google Scholar]
- 79.Taylor MZ, Caldwell PE 3rd, Pearson SE. Failure and Complication Rates in Common Sports and Arthroscopic Procedures: Reality Check. Sports Med Arthrosc Rev. 2022;30(1):10–6. 10.1097/jsa.0000000000000338. [DOI] [PubMed] [Google Scholar]
- 80.Johnson AA, Wolfe EL, Mintz DN, Demehri S, Shubin Stein BE, Cosgarea AJ. Complications After Tibial Tuberosity Osteotomy: Association With Screw Size and Concomitant Distalization. Orthop J Sports Med. 2018;6(10):2325967118803614. 10.1177/2325967118803614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kanamiya T, Naito M, Ikari N, Hara M. The effect of surgical dissections on blood flow to the tibial tubercle. J Orthop Res. 2001;19(1):113–6. 10.1016/s0736-0266(00)00009-7. [DOI] [PubMed] [Google Scholar]
- 82.Luhmann SJ, Fuhrhop S, O’Donnell JC, Gordon JE. Tibial fractures after tibial tubercle osteotomies for patellar instability: a comparison of three osteotomy configurations. J Child Orthop. 2011;5(1):19–26. 10.1007/s11832-010-0311-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Divano S, Camera A, Biggi S, Tornago S, Formica M, Felli L. Tibial tubercle osteotomy (TTO) in total knee arthroplasty, is it worth it? A review of the literature. Arch Orthop Trauma Surg. 2018;138(3):387–99. 10.1007/s00402-018-2888-y. [DOI] [PubMed] [Google Scholar]
- 84.Choi HR, Burke D, Malchau H, Kwon YM. Utility of tibial tubercle osteotomy in the setting of periprosthetic infection after total knee arthroplasty. Int Orthop. 2012;36(8):1609–13. 10.1007/s00264-012-1541-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Le Moulec YP, Bauer T, Klouche S, Hardy P. Tibial tubercle osteotomy hinged on the tibialis anterior muscle and fixed by circumferential cable cerclage in revision total knee arthroplasty. Orthop Traumatol Surg Res. 2014;100(5):539–44. 10.1016/j.otsr.2014.02.012. [DOI] [PubMed] [Google Scholar]
- 86.Mendes MW, Caldwell P, Jiranek WA. The results of tibial tubercle osteotomy for revision total knee arthroplasty. J Arthroplasty. 2004;19(2):167–74. 10.1016/j.arth.2003.08.013. [DOI] [PubMed] [Google Scholar]
- 87.Young CF, Bourne RB, Rorabeck CH. Tibial tubercle osteotomy in total knee arthroplasty surgery. J Arthroplasty. 2008;23(3):371–5. 10.1016/j.arth.2007.02.019. [DOI] [PubMed] [Google Scholar]
- 88.Zonnenberg CB, van den Bekerom MP, de Jong T, Nolte PA. Tibial tubercle osteotomy with absorbable suture fixation in revision total knee arthroplasty: a report of 23 cases. Arch Orthop Trauma Surg. 2014;134(5):667–72. 10.1007/s00402-014-1950-7. [DOI] [PubMed] [Google Scholar]
- 89.Cosgarea AJ, Schatzke MD, Seth AK, Litsky AS. Biomechanical analysis of flat and oblique tibial tubercle osteotomy for recurrent patellar instability. Am J Sports Med. 1999;27(4):507–12. 10.1177/03635465990270041601. [DOI] [PubMed] [Google Scholar]
- 90.Zura R, Mehta S, Della Rocca GJ, Steen RG. Biological Risk Factors for Nonunion of Bone Fracture. JBJS Rev. 2016;4(1):e5. 10.2106/jbjs.Rvw.O.00008. [DOI] [PubMed] [Google Scholar]
- 91.Stetson WB, Friedman MJ, Fulkerson JP, Cheng M, Buuck D. Fracture of the proximal tibia with immediate weightbearing after a Fulkerson osteotomy. Am J Sports Med. 1997;25(4):570–4. 10.1177/036354659702500422. [DOI] [PubMed] [Google Scholar]
- 92.Bellemans J, Cauwenberghs F, Brys P, Victor J, Fabry G. Fracture of the proximal tibia after Fulkerson anteromedial tibial tubercle transfer A report of four cases. Am J Sports Med. 1998;26(2):300–2. 10.1177/03635465980260022401. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.