Abstract
Objective:
In April 2020, the US Centers for Disease Control and Prevention (CDC) recommended community masking to prevent the transmission of SARS-CoV-2. Since then, a total of 39 US states and DC issued mask mandates. Despite CDC recommendations and supporting evidence that masking reduces COVID-19 community transmission, from January to June 2021, 20 states lifted their mask mandates for all individuals. This study examined the association between lifting state-issued mask mandates and mask-wearing behavior in 2021.
Design:
We estimated a difference-in-difference model, comparing changes in the likelihood for individuals to wear a mask in states that lifted their mask mandate relative to states that kept their mandates in place between February and June of 2021.
Setting:
Individuals were surveyed from across the United States.
Participants:
We used masking behavior data collected by the Porter Novelli View 360 + national surveys (N = 3459), and data from state-issued mask mandates obtained by CDC and the University of Nevada, Las Vegas.
Main Outcomes:
The outcome variable of interest was self-reported mask use during the 30 days prior to the survey data collection.
Results:
In the overall population, lifting mask mandates did not significantly influence mask-wearing behavior. Mask wearing did significantly decrease in response to the lifting of mask mandates among individuals living in rural counties and individuals who had not yet decided whether they would receive a COVID-19 vaccine.
Conclusion:
Policies around COVID-19 behavioral mitigation, specifically amongst those unsure about vaccination and in rural areas, may help reduce the transmission of COVID-19 and other respiratory viruses, especially in communities with low vaccination rates.
Keywords: COVID-19, mask mandate, non-pharmaceutical intervention, prevention
Introduction
SARS-CoV-2, the virus that causes COVID-19, is transmitted from person-to-person through the inhalation of aerosolized respiratory droplets, emitted after an infected person coughs, talks, breathes, or sneezes.1 Early observational studies conducted in March 2020 found that after exposure to a confirmed symptomatic case, multi-layered cloth masks, respirators, and face coverings were 70-79% effective at reducing the transmission of SARS-CoV-2.2,3 On April 3, 2020, the US Centers for Disease Control and Prevention (CDC) released guidance recommending the use of masks, especially in areas of significant community-based transmission, as part of a multi-prong behavioral approach to reduce COVID-19-related deaths and hospitalizations.4 In September 2020, CDC established metrics for jurisdictions to use to assess their level of community transmission, based on new COVID-19 cases/100 000 individuals and the percent of positive COVID-19 tests, averaged over the prior seven days.5 In December 2020, CDC reiterated its universal masking recommendation. As part of its guidance amid high levels of community transmission, the CDC identified “policies and mandates” to achieve universal masking as a community-level prevention strategy.6
From April 2020 through the beginning of our study period, January 2021, 39 US states and the District of Columbia issued mask mandates.7 By April 2020, most (62%) US adults reported wearing a face covering when conducting activities outside of their home in the past week.8 By May 2020, this percentage increased to 76.4%.8 Masking polices proved effective, as mask mandates were associated with declines in COVID-19 case counts, hospitalization, and death rates.9, 10, 11 State-issued mask mandates were associated with a 0.5 and 0.7 percentage point decrease in COVID-19 cases and deaths, respectively, just 3 weeks after implementation.9 COVID-associated hospitalization rates declined by 2.4 percentage points as early as three weeks after mandate implementation and by 5.0 percentage points 3 or more weeks after implementation.10 In May 2021, CDC updated its guidance to lift the masking recommendation for people who are considered fully vaccinated for COVID-19 but recommended unvaccinated people to continue to wear masks in public.12 Despite CDC recommendations and supporting evidence that masking reduces COVID-19 community transmission, from January to June 2021, 20 states lifted their mask mandates for all individuals.6
While it is unknown if the lifting of statewide mask mandates affected mask-wearing behavior, prior studies demonstrate associations between the public’s actions before and after lifting mitigation measures. For example, a longitudinal analysis examining the effects of lifting stay-at-home orders on changes in social distancing behaviors, attitudes, and subjective norms between May–June 2020 found that as local orders expired, normative beliefs supporting social distancing and actual social distancing behavior declined.13 Although positive attitudes and intentions to socially distance increased over time, social distancing behavior did not. Findings from this analysis suggest that subjective norms, rather than attitudes and behavioral intentions, are significantly associated with, and predict engagement in, the COVID-19 prevention behaviors over time.13
In this study, we compare self-reported individual mask-wearing behavior before and after states revoked their mask mandates during the survey period. We sought to understand the effect, if any, the lifting of state-issued mask mandates had on individual mask use and to explore differences in effects based on vaccination status. This study seeks to build upon prior research evaluating behavioral responses to COVID-19 non-pharmaceutical interventions. Furthermore, this study fills a critical gap by exploring the heterogeneous impacts of lifting mask mandates on mask-wearing behavior across population subgroups.
Methods
Self-reported data on masking behavior were collected using the Porter Novelli (PN) View 360+ survey, a national, opt-in panel survey administered by ENGINE Insights and Porter Novelli Public Services.* PN View 360+ surveys were licensed and designed by CDC and PN Public Services to assess public engagement in mask wearing, physical distancing, and other COVID-19 prevention behaviors. ENGINE Insights14 utilizes quota sampling to assemble a representative national sample of US adults 18 years and older. PN View 360+ surveys are administered in English over the internet using the Lucid platform, a digital consumer network for survey research.15 The Lucid platform survey methodology and methods of survey administration have been summarized in previous literature.16 PN View 360+ survey data were weighted by age, gender, region, race/ethnicity, and education to mirror US demographic proportions according to the Census Bureau’s Current Population Survey.17 Under CDC’s license with PN View surveys, survey questions on masks use for COVID-19 prevention were fielded every month from April 2020 to July 2021. Our analysis focused on data obtained from 8538 participants from surveys fielded from February 16 to July 20, 2021.
The outcome variable of interest is self-reported mask use during the 30 days prior to data collection, as obtained in the survey question “In the LAST MONTH, how frequently did you do the following?” Participants reported how often they wore a mask around those who they did not live with. Responses were captured on a Likert-scale, ranging from 1 to 4 (never, rarely, often, or always). Participants reporting to often, or always wear a mask, around persons they do not live with were considered mask wearers for these analyses. Participants also reported demographic characteristics including age, race, gender, employment, and education. PN View 360+ surveys fielded starting in February 2021 collected additional information on COVID-19 vaccination status and intentions. Participants reported if they had been vaccinated, had a plan to be vaccinated, were unsure if they would get vaccinated, or if they did not plan to vaccinate.
Data on state-issued mask mandates were obtained from executive and administrative orders identified from state government websites from January to June 2021; included orders were analyzed and coded to extract their effective dates and termination dates.10 State-issued mask mandates were defined as requirements to wear a mask: (1) anywhere outside the home or (2) in retail businesses and restaurants. Responses from individuals residing in states that did not have a statewide mask mandate in place for a least 15 days prior to the first survey date during the study time-frame were removed from the analysis. An individual was coded as residing in a state that lifted a mask mandate in a particular survey month if a prior statewide mask mandate had not been in place for at least 15 days prior to the survey date to factor in the retrospective nature of the PN survey question related to mask-wearing behavior.
Analysis
Associations between the lifting of state-issued mask mandates and mask-wearing behavior were measured using a difference-in-difference (DID) model,18 which is a widely used methodology in public health to study the impact of policy changes on health and behavioral outcomes.19,20 In this study, the DID model used temporal and geographic variation in the lifting of state-issued mask mandates to identify their association with mask-wearing behavior. The model (Model 1) included a variable indicating whether an individual’s state lifted a mask mandate during the specific survey round; included two-way fixed effects (survey-month and state); and controlled for the age, sex, race/ethnicity, education, employment, the urbanicity of their county (urban, suburban, or rural), the COVID-19 vaccination status of respondents, and the statewide COVID-19 community transmission level (low, moderate, substantial, or high)21 at the time of the survey date for the state in which each respondent resided. The inclusion of survey-month fixed effects controlled for the change in CDC mask-wearing guidance for fully vaccinated individuals issued on May 13, 2021.12 The model was estimated with robust standard errors.
Additional specifications of the DID model were estimated potential differential effects of the policy change across a person’s vaccination status, the urbanicity of their residence, and the community transmission level of their residence at the time of the policy change. Furthermore, these specifications included policy interaction terms: Model 2—the mask mandate lifting variable interacted with urbanicity; Model 3—the mask mandate lifting variable interacted with vaccination status; and Model 4—the mask mandate lifting variable interacted with state-wide COVID-19 community transmission levels. Separate models were also estimated to explore the interaction of the policy change, vaccination status, and urbanicity by restricting the sample of each to one type of urbanicity (urban, suburban, or rural) and including the vaccine status/policy change interaction term. Formal presentations of these models are available in the supplement (supplementary material content, appendix, available at: http://links.lww.com/JPHMP/B423).
The underlying assumption of the DID model is the “parallel trend” assumption, which suggest that the trend in mask-wearing behavior for those who reside in states that lifted mask mandates would have been the same as those who reside in states that did not lift such mask mandates in the absence of policy change. Due to the lack of availability of the relevant covariates in PN surveys prior to February 2021, we were unable to indirectly test this parallel trend assumption via an event study model, an approach standard within the DID literature.10,19,20
Beginning in April 2021, some states started to exempt fully vaccinated individuals from mask mandates. As a sensitivity analysis, and to understand how these exemptions may have influenced our results, we estimated an additional DID model defining the date a state lifted a mandate as the earlier of either the date that the indoor mask-wearing exemption for fully vaccinated people took effect or the date the state-issued mask mandate was lifted for all residents.
Results
The final sample used for analysis included 3,459 individuals from the 37† states and the District of Columbia that had a statewide mask mandate in place on February 1,2021. Over the study period, 20 states and the District of Columbia lifted their mask mandates: 2 states lifted prior to the March survey, 6 more by the April survey, 5 more by the May survey, and the final 7 and the District of Columbia by the June survey (Figure 1). Mask-wearing behavior significantly varied by survey month (chi-sq = 56, P < .001), with 86.6% of the February respondents reporting that they wore a mask around people they did not know over the past 30 days, 90.3% of March’s respondents, 87.2% of April’s respondents, 87.9% of May’s respondents, and 78% of June’s respondents (Figure 1).
FIGURE 1.
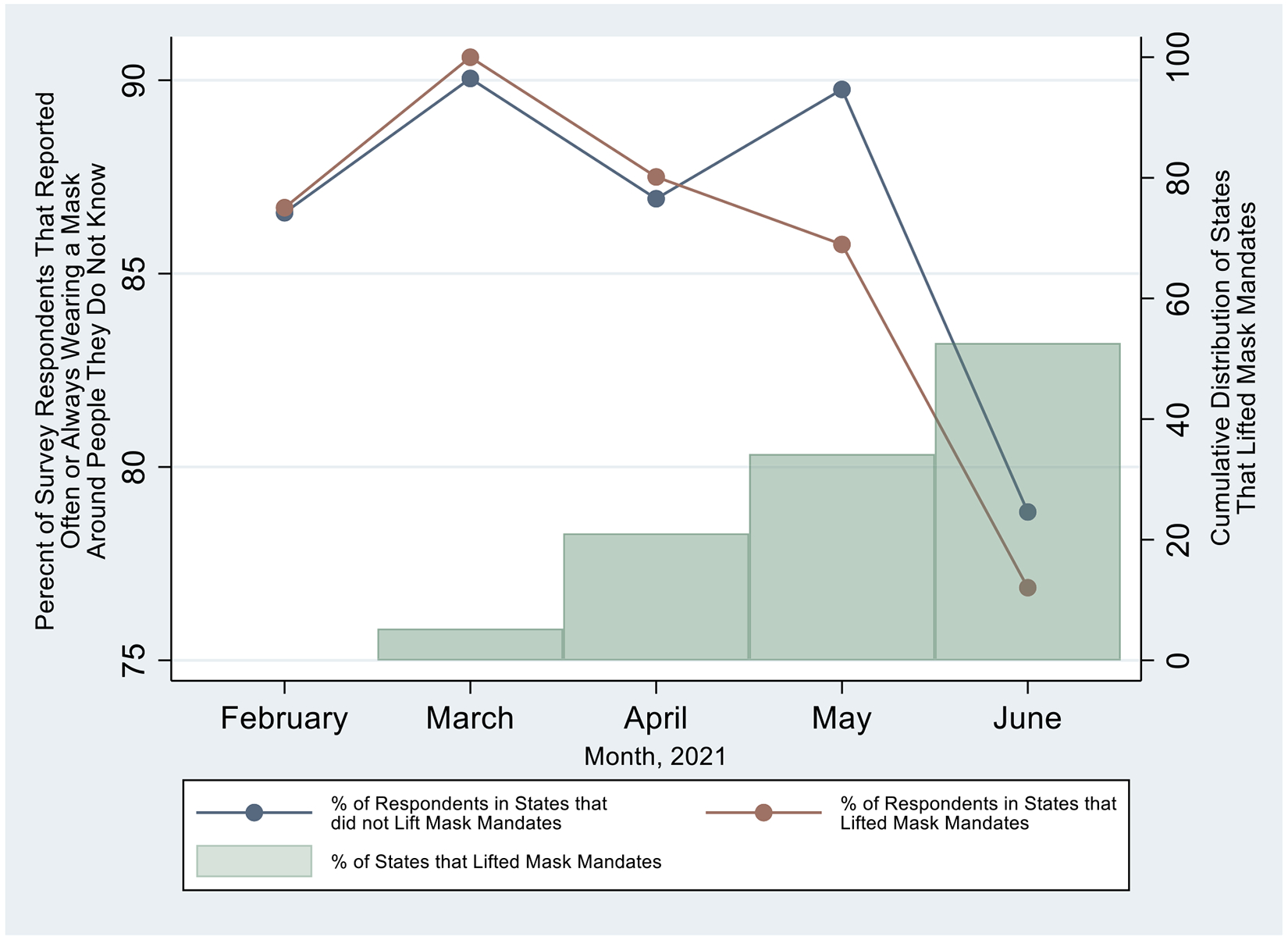
Percent of Survey Respondents Reporting They “Often” or “Always” Wore a Mask around People They Did Not Know and the Cumulative Distribution of States that Lifted State-issued Mask Mandates, February–June 2021.
Data Source: Porter Novelli Emerging Timely Topics, State-issued Prevention Measures, CDC COVID-19 Tracker.Notes: Sample included 3459 individuals from the 37 states and the District of Columbia that had a mask mandate in place on February 1, 2021. Chi-square test shows statistical association between survey month and whether an individual wears a mask around people they do not know (chi-sq = 56, P < .001).
The DID results indicate the lifting of state-issued mask mandates was not associated with overall changes in individuals’ likelihood of wearing a mask around people they did not know (Table 1, Model 1). Model 1 also shows the association between each covariate and mask-wearing behavior; urbanicity and vaccination status were each significantly associated with self-reported mask-wearing behavior. People living in rural counties were 5 percentage points less likely to report wearing a mask around people they did not know compared to people in urban counties (P = .004). Compared to vaccinated individuals, those that planned to get vaccinated were 3 percentage points more likely to report wearing a mask around people they did not know (P = .010), those that were unsure if they would get vaccinated were 4 percentage points less likely to report mask-wearing behavior (P = .041), and those that did not plan to get vaccinated were 25 percentage points less likely to report mask-wearing behavior (P = .001) (Table 1, Model 1).
TABLE 1.
The Association Between Lifting State-Issued Mask Mandates (At Least 15 Days Prior to Survey Date) and Self-Reported Mask-Wearing Behavior: Difference-in-Difference Estimates
| Coefficient Estimates (P-value) | ||||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | |
| Lifting of state-issued mask mandate | ||||
| Overall | −0.03 (.276) | – | – | – |
| For those who live in a rural county | – | −0.11 (.005)a | – | – |
| For those who live in a suburban county | – | −0.01 (.703) | – | – |
| For those who live in an urban county | – | 0.03 (.343) | – | – |
| For those who are vaccinated | – | – | −0.02 (.427) | – |
| For those who plan to get vaccinated | – | – | 0.04 (.289) | – |
| For those who are not sure if they will get vaccinated | – | – | −0.12 (.037)a | – |
| For those who do not plan to get vaccinated | – | – | −0.03 (.544) | – |
| For those who live in a state with low cases | – | – | – | −0.01 (.853) |
| For those who live in a state with moderate cases | – | – | – | −0.05 (.139) |
| For those who live in a state with substantial cases | – | – | – | 0.01 (.940) |
| For those who live in a state with high cases | – | – | – | −0.03 (.688) |
| Urbanicity | ||||
| Urban (reference) | – | – | – | – |
| Suburban | −0.01 (.683) | 0.01 (.937) | −0.01 (.669) | −0.01 (.681) |
| Rural | −0.05 (.004)a | −0.02 (.276) | −0.05 (.005)a | −0.05 (.004)a |
| Vaccination status | ||||
| Vaccinated (reference) | – | – | – | – |
| Plan to get vaccinated | 0.03 (.010)a | 0.03 (.005)a | 0.03 (.052) | 0.03 (.010)a |
| Not sure if 1 plan to get vaccinated | −0.04 (.041)a | −0.04 (.057) | −0.02 (.265) | −0.04 (.041)a |
| Do not plan to get vaccinated | −0.25 (.001)a | −0.24 (.001)a | −0.24 (.001)a | −0.25 (.001) |
| Sex | ||||
| Male (reference) | – | – | – | – |
| Female | 0.03 (.009)a | 0.03 (.008)a | 0.03 (.009)a | 0.03 (.009)a |
| Age group | ||||
| 18-24 (reference) | – | – | – | – |
| 25-34 | −0.01 (.696) | −0.01 (.744) | −0.01 (.731) | −0.01 (.685) |
| 35-44 | 0.01 (.796) | 0.02 (.723) | 0.02 (.686) | 0.01 (.813) |
| 45-54 | 0.10 ( 037)a | 0.11 (.035)a | 0.11 (032)a | 0.10 (.038)a |
| 55-64 | 0.01 (.986) | −0.01 (.982) | 0.01 (.944) | −0.01 (.993) |
| 65 + | 0.08 (.084) | 0.08 (.060) | 0.08 (.064) | 0.08 (.087) |
| Education | ||||
| High school or less (reference) | – | – | – | – |
| College degree | −0.03 (.065) | −0.03 (.073) | −0.03 (.073) | −0.03 (.070) |
| Postgraduate degree | 0.01 (.564) | 0.01 (.456) | 0.01 (.563) | 0.01 (.543) |
| Employment | ||||
| Full-time (reference) | – | – | – | – |
| Part-time | −0.02 (.410) | −0.02 (.375) | −0.02 (.390) | −0.02 (.401) |
| Unemployed | 0.02 (.269) | 0.02 (.286) | 0.02 (.290) | 0.02 (.280) |
| Other | 0.01 (.961) | 0.01 (.946) | −0.01 (.969) | 0.01 (.967) |
| Race/ethnicity | ||||
| White (reference) | – | – | – | – |
| Black | −0.002 (.935) | −0.002 (.988) | −0.002 (.907) | −0.01 (.946) |
| Asian | 0.02 (.473) | 0.02 (.456) | 0.02 (.466) | 0.02 (.472) |
| American Indian/Alaskan Native | −0.05 (.360) | −0.06 (.317) | −0.05 (.380) | −0.05 (.358) |
| Hispanic | 0.02 (.382) | 0.02 (.390) | 0.02 (.375) | 0.02 (.389) |
| Other | 0.07 (.011)a | 0.07 (.009)a | 0.07 (.011)a | 0.07 (.011)a |
| COVID-19 Community Level | ||||
| Low | – | – | – | – |
| Moderate | −0.05 (.198) | −0.04 (.203) | −0.04 (.231) | −0.03 (.523) |
| Substantial | −0.04 (.255) | −0.04 (.261) | −0.04 (.291) | −0.04 (.381) |
| High | −0.06 (.145) | −0.05 (.158) | −0.05 (.165) | −0.05 (.297) |
Note: The dependent variable is a dummy variable indicating whether the respondent often or always wore a mask around people they did not know in the last month. Sample included 3,459 individuals from the 37 states and District of Columbia that had a mask mandate in place on February 1, 2021. Respondents were coded as residing in a state that lifted a mask mandate if their state was subject to the lifted mandate for at least IS days prior to the survey date. Model 1 estimates the average effect of lifting state-issued mask mandates. Model 2 estimates the average effect of lifting state-issued mask mandates by vaccination status. Model 3 estimates the average effect of lifting state-issued mask mandates by urbanicity, and Model 4 estimates the average effect of lifting state-issued mask mandates by state COVID-19 community-level categorization. All models included survey month fixed effects and state fixed effects and were estimated with robust standard errors. Results are reported as coefficient estimate with P-values in parenthesis.
Data Source: Porter Novelli Emerging Timely Topics. Policy data source.
Each cell with an asterisk indicates P < .05.
When stratifying the effect of the policy by urbanicity, the lifting of state-issued mask mandates was associated with an 11-percentage point reduction in the probability of reporting mask-wearing behavior among people living in rural counties (P = .005) (Table 1, Model 2). No significant association was found for those residing in urban or suburban counties (Table 1, Model 2). Stratifying the effect of policy change by individuals’ vaccination status, the lifting of mask mandates was associated with a 12-percentage point reduction in the probability of reporting mask-wearing behavior among those who were unsure if they would get vaccinated (P = .037) (Table 1, Model 3). No significant association was found for those who were vaccinated, planned to get vaccinated, or did not plan on getting vaccinated. Stratifying the effect of the policy change by statewide COVID-19 community transmission levels revealed no significant association between the level of COVID-19 community transmission in the state in which an individual resided and mask-wearing behavior after lifting of mask mandates (Table 1, Model 4).
Stratifying the effect of the policy by both urbanicity and vaccination status (Table 2) shows that the lifting of state-issued mask mandates was associated with a 14-percentage point increase in the probability of reporting mask-wearing behavior among those residing in urban counties who were unsure if they would get vaccinated (P = .010) and a 25-percentage point reduction among those residing in rural counties who were unsure if they would get vaccinated (P = .014) (Table 2).
TABLE 2.
The Association Between Lifting of State-issued Mask Mandates (At Least 15 Days Prior to Survey Date) and Self-reported Mask-Wearing Behavior by Vaccination Status, Sample Stratification by Urbanicity: Difference-in-difference Estimates
| Sample Stratification | |||
|---|---|---|---|
| Urban | Suburban | Rural | |
| Lifting of mask mandate | |||
| For vaccinated | 0.06 (.219) | −0.03 (.385) | −0.08 (.247) |
| For those who plan to get vaccinated | 0.06 (.424) | 0.07 (.143) | −0.01 (.973) |
| For those who are not sure if they will get vaccinated | 0.14 (.010)a | −0.08 (.358) | −0.25 (.014)a |
| For those who do not plan to get vaccinated | 0.10 (.345) | −0.07 (.430) | −0.07 (.510) |
Note: The dependent variable is a dummy variable indicating whether the respondent often or always wore a mask around people they did not know in the last month. Respondents were coded as residing in a state that lifted a mask mandate if their state was subject to the lifted mandate for at least 15 days prior to the survey date. All models were estimated with robust standard errors and included covariates for sex, age, race and ethnicity, education, employment status, vaccination status, sun/ey month fixed effects, and state fixed effects. Results are reported as coefficient estimate with P-values in parenthesis.
Data Source: Porter Novelli Emerging Timely Topics. Policy data source.
Each cell with an asterisk indicates P < .05.
Finally, the sensitivity analysis for states that exempted fully vaccinated individuals from mask mandates did not reveal significantly different results, indicating that exempting fully vaccinated individuals did not affect masking behavior for these individuals after the policy change (Formal results available upon request to corresponding author).
Discussion
Across all states between February and June 2021, including those that lifted state-issued mask mandates, mask use declined over time. The results of this study suggest that the lifting of state-issued mask mandates in this time was not associated with an overall change in mask-wearing behavior in the United States. However, there was a differential effect of the policy change based on the urbanicity of the respondent’s community and the vaccination status of the respondent.
When examining the masking behavior after state mask mandates were lifted based on the urbanicity of respondents, masking decreased by 11-percentage points among residents of rural counties. Yet, no significant behavior change was observed among urban or suburban residents. These findings are consistent with previous studies that found that masking behaviors vary by urbanicity,21 as do the benefits of state mitigation measures such as mask mandates, which had a more pronounced effect in nonmetropolitan areas.22 Additionally, this finding aligns with research suggesting that the lifting of statewide mask mandates increased COVID-19 cases in Iowa (a predominately rural state) due to decreases in mask-wearing behavior.23 Further, previous studies have shown that perceived susceptibility and severity have been significant predictors of prevention behaviors throughout the COVID-19 pandemic,24 as well as in previous outbreaks, such as the 2009 Avian Influenza outbreak in Taiwan.25 In rural counties, which have experienced disproportionately higher rates of community transmission26,27 and low rates of vaccination,28 initiatives to increase the knowledge of disease susceptibility and severity are vital to increase the uptake of masks in the absence of mandates.
Lifting mask mandates was also associated with a significant reduction in the probability of mask wearing among those who were not sure if they would get vaccinated, although there was no association between the policy change and mask-wearing behavior among those who were already vaccinated, planned to get vaccinated, or did not plan to get vaccinated. These findings align with research on social norms surrounding preventive behaviors throughout the pandemic29,30; which appear to differ based on an individual’s willingness to obtain the COVID-19 vaccine.31 Social Identity theory explains that individuals identify with and engage in the normative behaviors reflective of their group membership. Latkin et al31 explains that individuals who regularly engaged in masking and social distancing were more likely to have high intentions to receive a COVID-19 vaccine due to their “COVID-19 social identity.” Those in this group view vaccination as further protection against the virus, consistent with their preventative behavior social identity.31 Consistent with these studies, our results suggest that individuals’ perceptions of one COVID-19 preventive behavior correlate with other preventive behaviors, and those who are decidedly supportive or unsupportive of one preventive behavior are less affected by policy change for other prevention measures. However, those who are unsure or who have not formed strong opinions about a preventive behavior may be more influenced by a change in policy or requirements.
Changes to COVID-19 policy influencing those who are unsure regarding vaccination, who can be viewed as the “movable middle,” may also be the result of impacting the dichotomous social norms that surround COVID-19 prevention behaviors. Studies on COVID-19 prevention behaviors report a correlation between the individual intentions to perform a preventive behavior and the social norms surrounding that behavior.32 For example, if mask mandates had remained, unsure individuals may have continued to engage in preventive behaviors at similarly high rates as vaccinated groups, as masking policies communicate that mask wearing continues to be a normative and beneficial behavior.8
When modeling the urbanicity of respondents who were unsure of vaccination, as shown in Table 2, we observed significant changes in masking behavior. Respondents in urban counties who were still contemplating vaccination, increased their mask-wearing behavior after the state lifted the mandate. This may be, in part, due to those individuals’ awareness of their own susceptibility to infection and the possibility that the likelihood of exposure would increase without a mask mandate as masking behaviors declined in their densely populated communities. On the other hand, respondents living in rural counties exhibited the greatest change in behavior, with a 24-percentage point decrease in masking behavior once state mandates were lifted. For rural respondents, who had worn masks but were yet undecided on vaccination, the removal of the mask mandate represented a turning point in their mitigation behaviors. These individuals who reside in counties with historically low rates of mask wearing21 and vaccination,28 but among the highest rates of COVID-19 transmission and mortality,26,27 represent an ideal target population for communicating the importance of disease prevention strategies.
With the emergence and prevalence of the Delta and Omicron variants, hospitalization and death rates among the unvaccinated far exceeded that of those who had been fully vaccinated.33,34 The CDC recommends wearing a well-fitted mask indoors in areas with a high COVID-19 community level.5 Community-level prevention policies should be relaxed only after a community has sustained several weeks of a continuous decrease in COVID-19 community transmission.35 In areas of high transmission and where COVID-19 vaccinations may lag, mask mandates may provide additional help in protecting those most at risk for severe COVID-19 illness, including those unvaccinated or people who are immunocompromised. To best protect those who remain unvaccinated or not fully vaccinated from serious illness or hospitalization, state and local governments may consider crafting COVID-19 prevention messaging tailored to rural communities and individuals still deciding if they will receive a vaccine. Improving understanding of the role masks and other behavioral prevention strategies play in decreasing individual and community-wide disease risk is needed to prevent and control future respiratory infection epidemics.
This study is subject to several limitations. First, we were unable to indirectly test the parallel trend assumption of the model due to the time horizon of the PN Survey. Second, the retrospective nature of the mask wearing questions may have led to recall bias among respondents. Third, there may be other confounding factors that we were unable to control for that affected the timing of policy change and mask-wearing behavior. Fourth, our analysis did not control for county or city mask mandates. City mask mandates that remained after states lifted their state-wide mandate may explain our finding that the rural communities saw the greatest change in masking behavior after states lifted mask mandates. Lastly, the PN View 360+ survey was conducted via the internet in English only, suggesting that a large portion of non-English speaking individuals may not be captured through the survey design.
Conclusion
While mask wearing decreased over the 5-month study period as states lifted mask mandates across the United States overall, our study found that the lifting of state-issued mask mandates was only associated with decreased mask wearing in rural counties and for individuals unsure if they would get vaccinated. If state-issued mask mandates were not lifted, those individuals may have continued wearing masks. As future waves of COVID-19 are expected, due to the emergence of highly transmissible variants, education, and policies on the use of multi-layered prevention approaches is crucial, especially in rural communities with low vaccination rates.
Supplementary Material
Implications for Policy & Practice.
The lifting of state-issued mask mandates was associated with decreased mask wearing in rural counties and for individuals unsure if they would get vaccinated.
Those who are unsure or who have not formed strong opinions about COVID-19 preventive behaviors may be more influenced by a change in policy or requirements.
As future waves of COVID-19 are expected, due to the emergence of highly transmissible variants, education, and policies on the use of multi-layered prevention approaches is crucial, especially in rural communities with low vaccination rates.
Acknowledgments
We would like to acknowledge CDC 2019 NCoV Response CICP Monitoring and Evaluation Team; Dr Christine Prue, CDC; Dr Fred Fridinger, CDC; Deanne Weber, Porter Novelli for their support.
Footnotes
The findings and conclusions in this publication are those of the authors and do not necessarily represent the official position of funding agencies.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (http://www.JPHMP.com).
This study was reviewed by the Centers for Disease Control and Prevention (CDC) and was conducted consistent with applicable federal law and CDC policies, including 45 Code of Federal Regulations (CFR) part 46, 21 CFR part 56; 42 US Code (USC) §241(d); 5 USC §552a; and 44 USC §3501 et seq.
North Dakota’s mask mandate, issued in November 2020 was rescinded prior to the study period. Survey results from Mississippi were not included in this analysis because Mississippi did not have a statewide mask mandate during the study period (ie, the state’s mask mandate only applied in some counties).
Contributor Information
Aderonke S. Ajiboye, CDC COVID-19 Response, Monitoring and Evaluation Team, Centers for Disease Control and Prevention, Atlanta, GA; Division of Global HIV & TB, Global Health Center, Centers for Disease Control and Prevention, Atlanta, GA.
Christopher Dunphy, CDC COVID-19 Response, Monitoring and Evaluation Team, Centers for Disease Control and Prevention, Atlanta, GA.
Linda Vo, CDC COVID-19 Response, Monitoring and Evaluation Team, Centers for Disease Control and Prevention, Atlanta, GA.
Mara Howard-Williams, CDC COVID-19 Response, Monitoring and Evaluation Team, Centers for Disease Control and Prevention, Atlanta, GA.
Chandresh N. Ladva, CDC COVID-19 Response, Monitoring and Evaluation Team, Centers for Disease Control and Prevention, Atlanta, GA.
Susan J. Robinson, CDC COVID-19 Response, Monitoring and Evaluation Team, Centers for Disease Control and Prevention, Atlanta, GA.
Russell McCord, CDC COVID-19 Response, Monitoring and Evaluation Team, Centers for Disease Control and Prevention, Atlanta, GA.
Maxim Gakh, Environmental and Occupational Health, School of Public Health, University of Nevada, Las Vegas, Nevada.
Regen Weber, CDC COVID-19 Response, Monitoring and Evaluation Team, Centers for Disease Control and Prevention, Atlanta, GA.
Gregory Sunshine, CDC COVID-19 Response, Monitoring and Evaluation Team, Centers for Disease Control and Prevention, Atlanta, GA; Office of Public Health Law Services, Centers for Disease Control and Prevention, Atlanta, GA.
References
- 1.Science brief: community use of masks to control the spread of SAR-CoV-2. CDC. https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/masking-science-sars-cov2.html. Accessed August 2021. [PubMed] [Google Scholar]
- 2.Payne DC, Smith-Jeffcoat SE, Nowak G, et al. SARS-CoV-2 infections and serologic responses from a sample of U.S. navy service members—USS Theodore Roosevelt, April 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):714–721. doi: 10.15585/mmwr.mm6923e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang Y, Tian H, Zhang L, et al. Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection, and social distancing: a cohort study in Beijing, China. BMJ Glob Health. 2020;5(5):e002794. doi: 10.1136/bmjgh-2020-002794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control & Prevention. Recommendation regarding the use of cloth face coverings, especially in areas of significant community-based transmission. CDC Stacks, April 3, 2020. https://stacks.cdc.gov/view/cdc/86440. Accessed July 22, 2022. [Google Scholar]
- 5.Science brief: indicators for monitoring COVID-19 community levels and making public health recommendations. CDC. https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/indicators-monitoring-community-levels.html. Accessed August 2022. [PubMed] [Google Scholar]
- 6.Honein MA, Christie A, Rose DA, et al. Summary of guidance for public health strategies to address high levels of community transmission of SARS-CoV-2 and related deaths, December 2020. MMWR Morb Mortal Wkly Rep. 2020;69(49):1860–1867. doi: 10.15585/mmwr.mm6949e2externalicon. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. State-issued prevention measures at the state-level. CDC COVID data tracker. https://covid.cdc.gov/covid-data-tracker/#state-level-covid-policy. Last visited July 22, 2022. [Google Scholar]
- 8.Fisher KA, Barile JP, Guerin RJ, et al. Factors associated with cloth face covering use among adults during the COVID-19 pandemic—United States, April and May 2020. MMWR Morb Mortal Wkly Rep. 2020;69(28):933–937. doi: 10.15585/mmwr.mm6928e3. [DOI] [PubMed] [Google Scholar]
- 9.Guy GP Jr., Lee FC, Sunshine G, et al. Association of State-issued mask mandates and allowing on-premises restaurant dining with county-level COVID-19 case and death growth rates—United States, March 1-December 31, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(10):350–354. doi: 10.15585/mmwr.mm7010e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Joo H, Miller GF, Sunshine G, et al. Decline in COVID-19 hospitalization growth rates associated with statewide mask mandates—10 States, March-October 2020 [published correction appears in MMWR Morb Mortal Wkly Rep. 2021 Feb 26;70(8):293], MMWR Morb Mortal Wkly Rep. 2021;70(6):212–216. doi: 10.15585/mmwr.mm7006e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lyu W, Wehby GL. Community use of face masks and COVID-19: evidence from a natural experiment of state mandates in the US. Health Affairs. 2020;39(8):1419–1425. doi: 10.1377/hlthaff.2020.00818. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. Interim public health recommendations for fully vaccinated people; May 13, 2021. https://stacks.cdc.gov/view/cdc/106177. Last accessed July 22, 2022.
- 13.Gibson L BA, Magnan R, Kramer E, Bryan A. Theory of planned behavior analysis of social distancing during the COVID-19 pandemic: focusing on the intention-behavior gap. Ann Behav Med. 2021;55(8):805–812. doi: 10.1093/abm/kaab041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.ENGINE’S CARAVAN omnibus surveys ∣ engine-insights.com. https://engine-insights.com/product/caravan/. Accessed October 2021.
- 15.Survey sampling platform ∣ online survey sampling, https://luc.id/marketplace/. Accessed October 2021.
- 16.Coppock A, McClellan OA. Validating the demographic, political, psychological, and experimental results obtained from a new source of online survey respondents. Res Politics. 2019;6(1): 205316801882217. doi: 10.1177/2053168018822174. [DOI] [Google Scholar]
- 17.Current Population Survey (CPS), (n.d.). https://www.census.gov/programs-surveys/cps.html. Accessed February 21, 2022.
- 18.Dunphy C, Miller GF, Rice K, et al. The impact of Covid-19 State closure orders on consumer spending, employment, and business revenue. J Public Health Manag Pract. 2022;28(1):43–49. doi: 10.1097/PHH.0000000000001376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wing C, Simon K, Bello-Gomez RA. Designing difference in difference studies: best practices for public health policy research. Annu Rev Public Health. 2018;39(1):453–469. doi: 10.1146/annurev-publhealth-040617-013507. [DOI] [PubMed] [Google Scholar]
- 20.Dunphy C, Miller GF, Sunshine G, et al. The differential impact of reopening states with and without COVID-19 face mask mandates on county-level consumer spending. Public Health Rep. 2022;137 (5): 1000–1006. doi: 10.1177/00333549221103816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haisher MH, Beilfuss R, Hart M, Opielinski L, Wrucke D. Who is wearing a mask? Gender-, age-, and location-related differences during the COVID-19 pandemic. PLOS ONE. 2020; 15(10): e0240785. doi: 10.1371/journal.pone.0240785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dasgupta S, Kassem A, Sunshine G, Liu T, Rose C. Differences in rapid increases in county-level COVID-19 incidence by implementtation of statewide closures and mask mandates—United States, June 1-September 30, 2020. Ann Epidemiol. 2021;57:46–53. https://www.sciencedirect.com/science/article/pii/S1047279721000211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Petersen F, Errore A, Karaca-Mandic P. Lifting statewide mask mandates and COVID-19 cases: a synthetic control study. Med Care. 2022;60(7):538–544. doi: 10.1097/MLR.0000000000001725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Seale H, Dyer CEF, Abdi I, et al. Improving the impact of non-pharmaceutical interventions during COVID-19: examining the factors that influence engagement and the impact on individuals. BMC Infect Dis. 2020;20(1):607. doi: 10.1186/s12879-020-05340-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kuo PC, Huang JH, Liu MD. Avian influenza risk perception and preventive behavior among traditional market workers and shoppers in Taiwan: practical implications for prevention. PLoS One. 2011;6(9):e24157. doi: 10.1371/journal.pone.0024157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dobis EA, McGranahan D. Rural Residents Appear to Be More Vulnerable to Serious Infection or Death from Coronavirus COVID-19. Washington, DC: U.S. Department of Agriculture; 2021. https://www.ers.usda.gov/amber-waves/2021/february/rural-residents-appear-to-be-more-vulnerable-to-serious-infection-or-death-from-coronavirus-covid-19. Accessed February 6, 2022. [Google Scholar]
- 27.Ullrich F, Mueller K. COVID-19 Cases and Deaths, Metropolitan and Nonmetropolitan Counties over Time (Update). Iowa City, IA: Rural Policy research Institute, Center for Rural Health Policy Analysis; 2022. https://rupri.public-health.uiowa.edu/publications/policybriefs/2020/COVID%20Longitudinal%20Data.pdf. Accessed February 6, 2022. [Google Scholar]
- 28.Saelee R, Zell E, Murthy BP, et al. Disparities in COVID-19 vaccination coverage between urban and rural counties—United States, December 14, 2020-January 31, 2022. MMWR Morb Mortal Wkly Rep. 2022;71 (9):335–340. doi: 10.15585/mmwr.mm7109a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Agranov M, Elliott M, Ortoleva P. The importance of social norms against strategic effects: the case of Covid-19 vaccine uptake. Econ Lett. 2021;206:109979. doi: 10.1016/j.econlet.2021.109979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bokemper SE, Cucciniello M, Rotesi T, et al. Experimental evidence that changing beliefs about mask efficacy and social norms increase mask wearing for COVID-19 risk reduction: results from the United States and Italy. PLoS ONE. 2021;16(10): e0258282. doi: 10.1371/journal.pone.0258282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Latkin CA, Dayton L, Yi G, Colon B, Kong X. Mask usage, social distancing, racial, and gender correlates of COVID-19 vaccine intentions among adults in the US. PLoS ONE. 2021; 16(2): e0246970. doi: 10.1371/journal.pone.0246970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Latkin CA, Dayton L, Kaufman M, Schneider KE, Strickland JC, Konstantopoulos A. Social norms, and prevention behaviors in the United States early in the COVID-19 pandemic. Psychol Health Med. 2022;27(1):162–177. doi: 10.1080/13548506.2021.2004315. [DOI] [PubMed] [Google Scholar]
- 33.Scobie HM, Johnson AG, Suthar AB, et al. Monitoring incidence of COVID-19 cases, hospitalizations, and deaths, by vaccination status—13 U.S. jurisdictions, April 4-July 17, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(37):1284–1290. doi: 10.15585/mmwr.mm7037e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Danza P, Koo TH, Haddix M, et al. SARS-CoV-2 infection and hospitalization among adults aged ≥18 years, by vaccination status, before and during SARS-CoV-2 B.1.1.529 (Omicron) Variant Predominance—Los Angeles County, California, November 7, 2021-January 8, 2022. MMWR Morb Mortal Wkly Rep. 2022;71 (5): 177–181. doi: 10.15585/mmwr.mm7105e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Christie A, Brooks JT, Hicks LA, et al. Guidance for implementing COVID-19 prevention strategies in the context of varying community transmission levels and vaccination coverage. MMWR Morb Mortal Wkly Rep. 2021;70(30):1044–1047. doi: 10.15585/mmwr.mm7030e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


