Abstract
Objectives
Ureterorenoscopy is seeing a bloom of technological advances, one of which is incorporating suction. The objective of this study is to systematically review existing literature regarding suction use in rigid and flexible ureterorenoscopy and perform meta‐analysis of studies comparing suction versus no suction ureteroscopy or mini percutaneous nephrolithotomy (PCNL).
Methods
A literature search was performed (November 2023) in MEDLINE, Embase and Cochrane CENTRAL. Study protocol was registered at PROSPERO (CRD42023482360). Comparative studies (observational and randomized) were eligible for inclusion if they compared suction versus no suction group and reported at least one primary outcome of interest (stone‐free or complication rate).
Results
Sixteen studies (5 randomized and 11 observational), analysing 1086 and 1109 patients in standard and suction groups, respectively, were included. Final stone‐free rates (SFRs), overall and infectious complications and length of hospital stay exhibited significant improvement when suction was used. When mini‐PCNL was compared with flexible ureterorenoscopy with suction, no differences were found in terms of stone‐free and infectious complications rates.
Conclusions
Ureterorenoscopy is a commonly performed endoscopic procedure for urolithiasis treatment, the success of which is defined by SFRs and complication rates. Application of suction via ureteral access sheaths, ureteral catheters or scopes may provide improved SFRs, reduced overall and infectious complication rates, along with a reduction in length of hospital stay. Further randomized studies are needed to validate these findings and standardize indications and protocols.
Keywords: endourology, retrograde intrarenal surgery (RIRS), suction, ureteroscopy (URS), urolithiasis
1. INTRODUCTION
The increasing urolithiasis incidence has led to a bloom of technological advances in the field of endourology; from adoption of the miniaturized, digital and single‐use flexible scopes to high‐power and more efficient laser fibres and machines, 1 , 2 all of them led to an increase in utilization of endoscopic procedures such as percutaneous nephrolithotomy (PCNL) and ureteroscopy (URS)/retrograde intrarenal surgery (RIRS). European Association of Urology Guidelines on Urolithiasis set the clear indication for proper management selection according to stone size, composition and location, with RIRS being a suitable choice for stones up to 2 cm in size in most cases, while the increased efficiency seen with the implementation of new technologies is anticipated to expand these indications. 3 Despite the wide adoption of this technique, RIRS does not come without cost both for patients and healthcare systems; up to 22% of patients may have residual fragments, and infectious complications are not uncommon, while life‐threatening sepsis may be seen in 1.3% of cases. 4
Stone‐free rates (SFRs) are related to surgical expertise, appropriate patient selection, surgical technique (stone dusting, fragmentation and pop‐dusting) and available surgical equipment. 5 There is a scientific debate according to proper size cut‐off to define clinically insignificantly residual fragments (CIRFs), but studies have shown that even stone particles 2–4 mm can lead to recurrence, while those measured >4 mm are related to re‐intervention rates in a significant proportion of patients. 6 Therefore, surgeons are frequently relying on manual extraction of fragments using baskets and/or forceps, which can lead to increased operating time and potentially complications. Infectious complications have been clearly associated with infected urine, increased operating time and raised intrarenal temperature or pressure, which can lead to pyelovenous and pyelolymphatic backflow of urine into systemic circulation. 7 Suction has been initially used in endoscopic stone management for more than 25 years during PCNL, but the emergence of new devices applying suction through patented ureteroscopes, ureteral access sheaths (UAS) and ureteral catheters led to application of suction in URS/RIRS. 8
The aim of this systematic review and meta‐analysis is to appraise existing literature on suction use during URS/RIRS and provide pooled estimates for its safety and effectiveness.
2. MATERIALS AND METHODS
This systematic review and meta‐analysis were conducted according to the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) statement. 9
2.1. Data sources and searches
Two authors (L.T. and P.J.) independently performed the literature search in MEDLINE, Embase and Cochrane Central Register of Controlled Trials (CENTRAL) (via Ovid) from inception to 10 November 2023, using the following search algorithm as provided in Appendix S1 (control vocabulary and text words were searched using terms related to ureterorenoscopy and suction use). Conference abstracts and case reports were excluded in the search. Duplicate studies were removed, while reference lists of included studies were also screened. In case of disagreement between the two authors, a third author (R.G.) was advised to reach consensus. The protocol for the systematic review/meta‐analysis was registered in PROSPERO (CRD42023482360).
2.2. Eligibility criteria, data extraction and outcome of interest
Only English clinical papers were accepted (Table 1). The PICOS model (Patient Intervention Comparison Outcome Study type) was used to frame and answer to the clinical question:
- P:
adult patients with ureteral/kidney stones;
- I:
URS/RIRS using suction;
- C:
URS/RIRS not using suction or PCNL;
- O:
primary: complications and SFR; secondary: operative time (OR time), stone fragmentation time, lasering time, fluoroscopy time, length of hospital stay (LOS), auxiliary procedures, readmission rates, cost, post‐procedural pain scores and quality of life indicators
- S:
prospective and retrospective comparative studies.
TABLE 1.
Baseline patient and study characteristics.
| Author/year | Study design | Control arm | Experimental arm | Details about suction | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Definition | Sample size | Age (± SD) | BMI (± SD) | Energy used for lithotripsy | Definition | Sample size | Age (± SD) | BMI (± SD) | Energy used for lithotripsy | |||
| Sur 2022 | RCT | Flexible URS | 8 | 37 | 23.4 | Ho:YAG lithotripsy (0.6–1.0 J, 6–12 Hz), 270 μm fibre | Flexible URS with suction | 9 | 42 | 22.3 | Ho:YAG lithotripsy (0.6–1.0 J, 6–12 Hz), 270 μm fibre | SURE procedure using the C‐VAC aspiration system, a custom aspiration catheter used to navigate all areas of collecting system under fluoroscopy. The device has a steering control dial to allow deflection and guidance into collecting system, allowing irrigation and aspiration via connection to a vacuum port with suction set at 150–200 mmHg. Fragments up to 2.5 mm can be removed (inner aspiration channel 7.5 Fr) |
| Tang 2023 | RCT | Mini‐PCNL | 87 | 51.3 (8.2) | 22.6 (3.2) | Ho:YAG lithotripsy (15–20 W), 200 or 365 μm fibre | Flexible URS with suction | 86 | 52.7 (9.3) | 23.1 (3.9) | Ho:YAG lithotripsy (0.8–1.0 J, 15–20 Hz), 200 μm fibre | Novel disposable vacuum‐assisted ureteral access sheath (V‐UAS, Y‐type) consisting from an expansion tube, tube connector, sheath tube and operating handle |
| Chen 2019 | Retrospective | Mini‐PCNL | 45 | 39.4 (17.9) | 27.3 (4.4) | Ho:YAG lithotripsy (2.0 J, 20 Hz) | Flexible URS with suction | 44 | 45.7 (11.9) | 28.2 (8.2) | Ho:YAG lithotripsy (0.8 J, 30 Hz) | An intelligent irrigation and suctioning pressure monitoring platform with the integrated pressure‐measuring flexible ureteral access sheath with pressure sensing and suctioning function through pressure feedback control technology |
| Du 2019 | RCT | Semi‐rigid URS | 60 | 47 (15.7) | NR | Ho:YAG lithotripsy (0.6–0.8 J, 25–30 Hz), 550 μm fibre | Semi‐rigid URS with suction | 62 | 47.4 (13.2) | NR | Ho:YAG lithotripsy (0.6–0.8 J, 25–30 Hz), 550 μm fibre | Patented perfusion and suctioning platform consisting of a main control unit, perfusion and suctioning device and pressure feedback device. Platform allows setting perfusion flow rate, control pressure, alarming pressure and maximum pressure level. Ureteral access sheath inner diameter is 12 Fr and outer diameter 14 Fr with a length of 30–45 cm. A pressure sensor lies at the front and two connection channels at the back end, which are connected to the pressure monitoring, feedback device and negative pressure suctioning device. If the pressure of the operation exceeds the alarming pressure, platform gives alarm, while if it exceeds the maximum pressure level the platform stops perfusion automatically |
| Lai 2020 | Retrospective | Mini‐PCNL | 56 | 49.6 (12.2) | 25.3 (4.1) | Ho:YAG lithotripsy or pneumatic lithotripter | Flexible URS with suction | 28 | 45.2 (10.4) | 25 (3.5) | Ho:YAG lithotripsy (1.0–1.5 J, 15–20 Hz), 200 μm fibre | Novel vacuum‐assisted ureteral access sheath (V‐UAS, ClearPetra) with an oblique drainage tube connected to a negative pressure aspirator |
| Zhu 2018 | Retrospective | Flexible URS | 165 | 51.7 (15.8) | 23.1 (3.4) | Ho:YAG lithotripsy (12–16 W for ureter, 12–20 W for kidney, 14–20 Hz), 200 μm fibre | Flexible URS with suction | 165 | 53.9 (13.4) | 22.9 (2.6) | Ho:YAG lithotripsy (12–16 W for ureter, 12–20 W for kidney, 14–20 Hz), 200 μm fibre | Suction system included a modified ureteral access sheath and a vacuum device, connected at the back end of the sheath. An elastic rubber film with a hole on the tail end of the UAS enhanced the efficiency of suction by providing an airproof. Additionally, on the back end of the UAS, another channel covered by a red cap worked as an air door to regulate the negative pressure. Perfusion flow and negative pressure were set at 60–140 ml/min and 3–8 kPa, while to maintain satisfactory suctioning effect, the pressure was dynamically regulated by manually twisting the red cap on the tail end of the sheath. When lithotripsy was completed, the flexible ureteroscope was detracted, a 5F ureteral catheter was inserted into the UAS, its tip was placed in the ureteropelvic junction, and the tail end of the ureteral catheter was injected with saline to create artificial water circulation. The flow of artificial water circulation and the negative pressure were set to approximately 180 ml/min and 5 kPa, respectively, and were maintained for 20–40 s |
| Zhang 2021 | Retrospective | Semi‐rigid URS | 50 | 54.3 (11.6) | 21.8 (3.4) | Ho:YAG lithotripsy, 200 μm fibre | Semi‐rigid URS with suction | 56 | 53.8 (12.1) | 20.8 (3.4) | Ho:YAG lithotripsy, 200 μm fibre | The new vacuum suction ureteroscope consisted of a standard ureteroscope (9.8F), a lithotripsy endoscope (6F), a standard semi‐rigid ureteroscopic access sheath (13F) and a vacuum suction device |
| Zhang 2021 | Retrospective | Flexible URS | 54 | 55.2 (10.2) | 21.9 (3.5) | Ho:YAG lithotripsy, 200 μm fibre | Semi‐rigid URS with suction | 56 | 53.8 (12.1) | 20.8 (3.4) | Ho:YAG lithotripsy, 200 μm fibre | The new vacuum suction ureteroscope consisted of a standard ureteroscope (9.8F), a lithotripsy endoscope (6F), a standard semi‐rigid ureteroscopic access sheath (13F) and a vacuum suction device |
| Lechevallier 2003 | RCT | Semi‐rigid URS | 14 | NR | NR | Pneumatic lithotripter | Semi‐rigid URS with suction | 11 | NR | NR | Pneumatic lithotripter | Automated electronically controlled irrigation/suction system, consisting of an irrigation roller pump with a pressure control that supplies continuous irrigation to the ureteroscope and a suction roller pump with a constant flow rate that removes liquid and stone particles from the cavity. Pressure was set at 150 cm H20 (110.3 mmHg) and suction at 200 ml/min |
| Huang 2023 | Retrospective | Flexible URS | 103 | 54.7 (10.7) | 26.5 (4.9) | Ho:YAG lithotripsy (1.2 J, 20 Hz) | Flexible URS with suction | 103 | 54.5 (11) | 26.3 (4.2) | Ho:YAG lithotripsy (1.2 J, 20 Hz) | Vacuum‐assisted ureteral access sheath (FV‐UAS) was used. Continuous suction was applied through the entire process and after stones were pulverized the intrarenal end of the FV‐UAS sheath was guided into the calyces to suck out the fragments. Vacuum pressure was set at 100–300 cmH20, while intrarenal vacuum pressure was set according to surgeon. Irrigation rate was set at 65‐75 ml |
| Wu 2022 | Retrospective | Semi‐rigid URS | 82 | 44.9 (12.7) | 24.6 (2.8) | Ho:YAG lithotripsy (0.3–0.8 J, 15–30 Hz), 200 μm fibre | Semi‐rigid URS with suction | 76 | 48.5 (12.4) | 23.9 (2) | Ho:YAG lithotripsy (0.3–0.8 J, 15–30 Hz), 200 μm fibre | The vacuum suction device is composed of a 5F ureteral catheter and a tee joint, which can be assembled into a semi‐rigid ureteroscope. The ureteral catheter is linked to the vacuum aspirator |
| Ding 2023 | Retrospective | Flexible URS | 61 | 55.7 (13.1) | 24 (2.6) | Ho:YAG lithotripsy | Flexible URS with suction | 138 | 57.6 (13.7) | 24.6 (3.2) | Ho:YAG lithotripsy | Omnidirectional (flexible) ureteral access sheath (OD UAS) is supported by a metal wire coil to prevent collapse under pressure, the intraluminal channel is coated with Teflon (polyetrafluoroethylene) and the outside layer is coated with hydrophilic polyvinylpyrrolidone. The suction port comprises a nozzle which connects to vacuum suction, a suction switch and a watertight valve. The top 3 mm of the sheath is without a metal wire coil and is soft, while the flexible portion of the sheath is 10 cm. The suction was continuously performed with a pressure around −25 kPa, while the suction intensity could be modulated by tuning the suction switch from weak to strong |
| Zhai 2023 | Retrospective | Semi‐rigid URS | 60 | 46.2 (6.9) | 26.2 (4.1) | Ho:YAG lithotripsy (0.6–1.0 J, 20–30 Hz), 275 μm fibre | Semi‐rigid URS with suction | 60 | 47.2 (6.5) | 25 (3.4) | Ho:YAG lithotripsy (0.6–1.0 J, 20–30 Hz), 275 μm fibre | Use of a ureteral access sheath with negative pressure suctioning |
| Zhai 2023 | Retrospective | Semi‐rigid URS | 60 | 46.2 (6.9) | 26.2 (4.1) | Ho:YAG lithotripsy (0.6–1.0 J, 20–30 Hz), 275 μm fibre | Semi‐rigid URS with suction | 60 | 45.7 (4.5) | 24.9 (3.1) | Ho:YAG lithotripsy (0.6–1.0 J, 20–30 Hz), 275 μm fibre | Use of a negative pressure suctioning integrated semi‐rigid ureteroscope |
| Qian 2022 | Retrospective | Flexible URS | 81 | 50 (10.6) | 24.1 (3.4) | Ho:YAG lithotripsy (12–20 W, 14–20 Hz), 200 μm fibre | Flexible URS with suction | 81 | 50 (11.3) | 24 (3) | Ho:YAG lithotripsy (12–20 W, 14–20 Hz), 200 μm fibre | Suctioning access sheath which was connected with a negative pressure pump whose pressure was maintained at 0.01 Mpa and perfusion flow was set at 50–150 ml/min |
| Zhang 2022 | RCT | Flexible URS | 30 | 55.7 (10.8) | 25.5 (2.9) | Ho:YAG lithotripsy | Semi‐rigid URS with suction (combined with flexible standard URS) | 30 | 53.5 (12.9) | 25.2 (3.2) | Ho:YAG lithotripsy | The Soton ureteroscope was used. It comprises of 5 main components: a standard ureteroscope, a console ureteroscope, a rigid ureteral access sheath, a switch for adjusting the negative pressure and irrigation/suctioning platgorm. Perfusion exists in pulsed and continuous modes easily switched, while setting range for suction negative pressure is −25 to −4 kPa |
| Deng 2022 | Retrospective | Mini‐PCNL | 70 | 47.4 (7.8) | 19.8 (5.7) | Ho:YAG lithotripsy (2.0 J, 25 Hz) | Flexible URS with suction | 57 | 51.9 (10.9) | 20.3 (4.4) | Ho:YAG lithotripsy (0.8 J, 20 Hz), 200 μm fibre | Patented ureteral access sheath (12/14 Fr) with pressure measuring suctioning. Perfusion flow rate was set at 50–150 ml/min, renal pressure control value at −15 to 5 mmHg, renal pressure warning value at 20 mmHg and renal pressure maximum value at 30 mmHg |
| AlSmadi 2019 | Retrospective | Semi‐rigid URS | 60 | 48.2 (11) | 24 (1.7) | Ho:YAG or pneumatic lithotripsy | Semi‐rigid URS with suction | 43 | 51.9 (13.2) | 22.8 (1.5) | Ho:YAG or pneumatic lithotripsy | The modified ureteral access sheath used was a sheath with an additional channel at the proximal end, allowing the sheath to be connected to the suction machine. The sheath consist of a straight distal and proximal bifurcated segment. The distal segment accommodated a semi‐rigid ureteroscope. The suction was connected to the sheath and suction was set in continuous mode at 150–200 mmHg, while flow was adjusted to 60–80 ml/min |
Abbreviations: BMI, body mass index (kg/m2); Ho:YAG, Holmium‐Yttrium‐Aluminium‐Garnet; mini‐PCNL, mini percutaneous nephrolithotripsy; NR, not reported; RCT, randomized controlled trial; SD, standard deviation; SFR, stone‐free rate; URS, ureteroscopy.
Studies including less than 10 patients, those with patients with urinary diversions, ureteral re‐implantation, previous ureteric strictures or urologic malignancy were excluded. Any mode of stone fragmentation was considered eligible (laser, mechanical, ultrasound, extraction using baskets or forceps or combination of these methods). Immediate SFR was defined according to study definition but ranged between 1 and 5 days postoperatively (Table 2), and final SFR ranged between 4 and 12 weeks (Table 2). Secondary outcomes were operative time (OR time), stone fragmentation time, lasering time, fluoroscopy time, length of hospital stay (LOS), auxiliary procedures, readmission rates, cost, post‐procedural pain scores and quality of life indicators.
TABLE 2.
Stone characteristics and stone‐free rate definition.
| Author/Year | Control arm | Experimental arm | SFR Definition | SFR assessment | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Definition | Sample size | Stone size mm (± SD) | Stone surface mm2 (± SD) | HU (± SD) | Stone location (number) | Definition | Sample size | Stone size mm (± SD) | Stone surface mm2 (± SD) | HU (± SD) | Stone location (number) | |||
| Sur 2022 | Flexible URS | 8 | NR | NR | 926 |
Ureter 0 Renal 5 |
Flexible URS with suction | 9 | NR | NR | 786 |
Ureter 0 Renal 7 |
No residual fragments | CT at 1 day and 4 weeks |
| Tang 2023 | Mini‐PCNL | 87 | 15 (5) | NR | NR |
Upper ureter 87 Renal 0 |
Flexible URS with suction | 86 | 16 (4) | NR | NR |
Upper ureter 86 Renal 0 |
Fragments ≤2 mm | CT for radiolucent stones and X‐ray KUB for radiopaque stones at 1 day (immediate), 2 weeks and 4 weeks (final) |
| Chen 2019 | Mini‐PCNL | 45 | NR | NR | NR |
Ureter 0 Upper calyx 16 Middle calyx 16 Lower calyx 13 |
Flexible URS with suction | 44 | NR | NR | NR |
Ureter 0 Upper calyx 17 Middle calyx 18 Lower calyx 11 |
Fragments <3 mm | X‐ray KUB at 4 weeks |
| Du 2019 | Semi‐rigid URS | 60 | 21.4 (3.6) | NR | 985 (227) |
Upper ureter 20 Mid ureter 13 Distal ureter 27 Renal 0 |
Semi‐rigid URS with suction | 62 | 21.9 (4.9) | NR | 1023 (215) |
Upper ureter 21 Mid ureter 15 Distal ureter 26 Renal 0 |
Fragments ≤4 mm | X‐ray KUB at 4 weeks |
| Lai 2020 | Mini‐PCNL | 56 | 38.2 (5.4) | 729 (83.7) | 845 (240) |
Ureter 0 Renal pelvis 56 Upper calyx 22 Middle calyx 28 Lower calyx 22 |
Flexible URS with suction | 28 | 35.3 (6.3) | 676.1 (42.2) | 894 (232) |
Ureter 0 Renal pelvis 28 Upper calyx 13 Middle calyx 15 Lower calyx 11 |
No residual fragments | CT at 1 day and 12 weeks |
| Zhu 2018 | Flexible URS | 165 | 17.4 (4.7) | NR | 1023 (175) |
Ureter NR Renal pelvis 23 Upper calyx 18 Middle calyx 35 Lower calyx 42 |
Flexible URS with suction | 165 | 18.2 (5.2) | NR | 1049 (196) |
Ureter NR Renal pelvis 29 Upper calyx 14 Middle calyx 27 Lower calyx 40 |
Fragments <2 mm | X‐ray KUB at 1 day and X‐ray or CT KUB at 4 weeks |
| Zhang 2021 | Semi‐rigid URS | 50 | 12.5 (4.9) | NR | 665 (310) |
Upper ureter 50 Renal 0 |
Semi‐rigid URS with suction | 56 | 13.9 (4.7) | NR | 709 (344) |
Upper ureter 56 Renal 0 |
No residual fragments | CT at 3–5 days and 4 weeks |
| Zhang 2021 | Flexible URS | 54 | 12.7 (5.5) | NR | 684 (376) |
Upper ureter 54 Renal 0 |
Semi‐rigid URS with suction | 56 | 13.9 (4.7) | NR | 709 (344) |
Upper ureter 56 Renal 0 |
No residual fragments | CT at 3–5 days and 4 weeks |
| Lechevallier 2003 | Semi‐rigid URS | 14 | NR | NR | NR | NR | Semi‐rigid URS with suction | 11 | NR | NR | NR | NR | NR | XR KUB at the end of procedure |
| Huang 2023 | Flexible URS | 103 | 17 (5) | NR | NR | NR | Flexible URS with suction | 103 | 17 (6) | NR | NR | NR | Fragments <3 mm | CT at 1 day and 4 weeks |
| Wu 2022 | Semi‐rigid URS | 82 | NR | 157 (35) | 916 (81) |
Upper ureter 82 Renal 0 |
Semi‐rigid URS with suction | 76 | NR | 165 (33) | 938 (85) |
Upper ureter 76 Renal 0 |
No residual fragments | X‐ray KUB at 1 day and 4 weeks |
| Ding 2023 | Flexible URS | 61 | 13.4 (5.2) | NR | 715 (341) |
Upper ureter 13 Renal pelvis 35 Upper calyx 2 Middle calyx 5 Lower calyx 29 |
Flexible URS with suction | 138 | 13 (6.9) | NR | 752 (429) |
Upper ureter 26 Renal pelvis 98 Upper calyx 3 Middle calyx 11 Lower calyx 64 |
Fragments <2 mm | CT at 4 weeks |
| Zhai 2023 | Semi‐rigid URS | 60 | NR | 132 (25) | 912 (53) |
Upper ureter 13 Mid ureter 17 Distal ureter 30 Renal 0 |
Semi‐rigid URS with suction | 60 | NR | 137 (27) | 907 (64) |
Upper ureter 12 Mid ureter 18 Distal ureter 30 Renal 0 |
Fragments <4 mm | 4 weeks |
| Zhai 2023 | Semi‐rigid URS | 60 | NR | 132 (25) | 912 (53) |
Upper ureter 13 Mid ureter 17 Distal ureter 30 Renal 0 |
Semi‐rigid URS with suction | 60 | NR | 136 (25) | 897 (94) |
Upper ureter 12 Mid ureter 28 Distal ureter 20 Renal 0 |
Fragments <4 mm | 4 weeks |
| Qian 2022 | Flexible URS | 81 | 20 (4.5) | NR | NR |
Ureter 0 Renal 81 |
Flexible URS with suction | 81 | 19.7 (4.5) | NR | NR |
Ureter 0 Renal 0 |
Fragments <4 mm | X‐ray KUB at 1 day and X‐ray/CT KUB at 4 weeks |
| Zhang 2022 | Flexible URS | 30 | 18.5 (5.6) | NR | NR |
Ureter 0 Renal 30 |
Semi‐rigid URS with suction (combined with fURS) | 30 | 18.2 (5.3) | NR | NR |
Ureter 0 Renal 30 |
Fragments ≤3 mm | X‐ray KUB at 1 week |
| Deng 2022 | Mini‐PCNL | 70 | 24.9 (7.9) | NR | NR |
Ureter 0 Renal 70 |
Flexible URS with suction | 57 | 23.1 (6.5) | NR | NR |
Ureter 0 Renal 57 |
Fragments <2 mm | CT at 4 and 12 weeks |
| AlSmadi 2019 | Semi‐rigid URS | 60 | 14.9 (1.8) | NR | 777 (120) |
Upper ureter 60 Renal 0 |
Semi‐rigid URS with suction | 43 | 12.7 (1.2) | NR | 896 (70) |
Upper ureter 43 Renal 0 |
Fragments ≤3 mm | X‐ray KUB at 1–2 days and CT at 4 weeks |
Abbreviations: fURS, flexible ureteroscopy; KUB, kidneys‐ureters‐bladder; mini‐PCNL, mini percutaneous nephrolithotripsy; NR, not reported; RCT, randomized controlled trial; URS, ureteroscopy.
Data extraction was performed using a preset Excel sheet for baseline study and patient characteristics (year, centre, inclusion/exclusion criteria, age, body mass index‐BMI, sample size, stone size/surface/volume and technical characteristics regarding the operation and suction technique) and primary and secondary outcomes. Two authors (L.T. and P.J.) independently extracted data, and in case of disagreement between the two authors, a third author (R.G.) was advised to reach consensus.
2.3. Risk of bias assessment
Two authors (L.T. and P.J.) assessed the risk of bias independently using the Cochrane risk of bias 2 for randomized controlled trials (RCTs) and the risk of bias for non‐randomized trials tool (ROBINS‐I). 10 , 11 In case of disagreement between the two authors, a third author (R.G.) was advised to reach consensus.
2.4. Publication bias assessment
Publication bias was assessed after visual inspection of Funnel plots for outcomes on which at least 10 studies were reporting results.
2.5. Certainty of evidence
The Grading of Recommendation Assessment, Development and Evaluation (GRADE) tool was used to evaluate each of the outcomes for certainty of evidence. 12 The levels of evidence were very low, low, moderate or high; each evidence certainty was ranked as high for RCTs and low for observational studies initially, while after evaluating limitations of risk of bias, imprecision, inconsistency, indirectness and publication bias, the level of certainty was downrated. 12
2.6. Statistical analysis
Statistical analysis was performed in R (R statistical software; R Foundation for Statistical Computing, Vienna, Austria, version 4.3.1). Meta‐analyses were performed using the meta and metafor packages, with plots made using these along with the forestplot package. For continuous variables, the mean difference or standardized mean difference was used with the corresponding 95% confidence intervals (CIs). Relative risks (RRs) were used to estimate binary outcomes with corresponding 95% CIs. For missing data, no imputation was performed. A priori, a fixed effects model was used in case of low heterogeneity (I2 < 50%) and random effects model for high heterogeneity (I2 > 50%). Heterogeneity between studies was assessed using the Chi‐squared Q test and I2 statistics. If I2 > 50% and/or Chi‐squared < 0.10, substantial heterogeneity was considered. Formulas by Sterne et al. 10 , 11 were used to transform medians and interquartile ranges to means and standard deviations when necessary. Subanalyses for study design (RCT only) and type of intervention (semirigid URS, flexible URS and PCNL) were also conducted. For all outcomes, heterogeneity was assessed using I2, tau2 and Cochran's Q. We present risk ratios, according to the random or fixed effects model as above. Publication bias was assessed via visual inspection of Funnel plots. In analyses with n > 2 studies, we performed trim and fill analyses to statistically assess for publication bias. Adjusted values for the trim and fill analysis are presented along with the calculated number of missing studies. We present forest and funnel plots, along with heterogeneity statistics (I2, Cochran's Q and Tau2) if the number of studies included was >2. All analyses are available in Appendix S2, which details the full code.
3. RESULTS
Literature search in 3 databases revealed 230 studies after removal of 145 duplicates. After initial screening by title and abstract, 118 were excluded due to irrelevance, 36 due to analysing PCNL only data, while 13 case reports and 33 reviews were also excluded, leaving 30 studies to be screened by reading the full text. Twelve further studies were excluded due to non‐comparative design and two because they were comparing two different suction techniques. Finally, 16 comparative studies (5 RCTs 13 , 14 , 15 , 16 , 17 and 11 observational 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 ) were included in qualitative and quantitative analysis, including 1086 patients in control and 1109 patients in suction groups (2 of the studies reported 3 groups, 21 , 25 thus in total 18 groups of comparison were extracted). Figure 1 shows the PRISMA flow diagram for study selection. The risk of bias assessment for all studies can be found in Tables S1 and S2, while certainty of evidence for all outcomes based on GRADE system in Table S3. Publication bias assessed by visual inspection of Funnel plots revealed high risk for all outcomes. All analyses are detailed in Appendix S2 including heterogeneity statistics.
FIGURE 1.
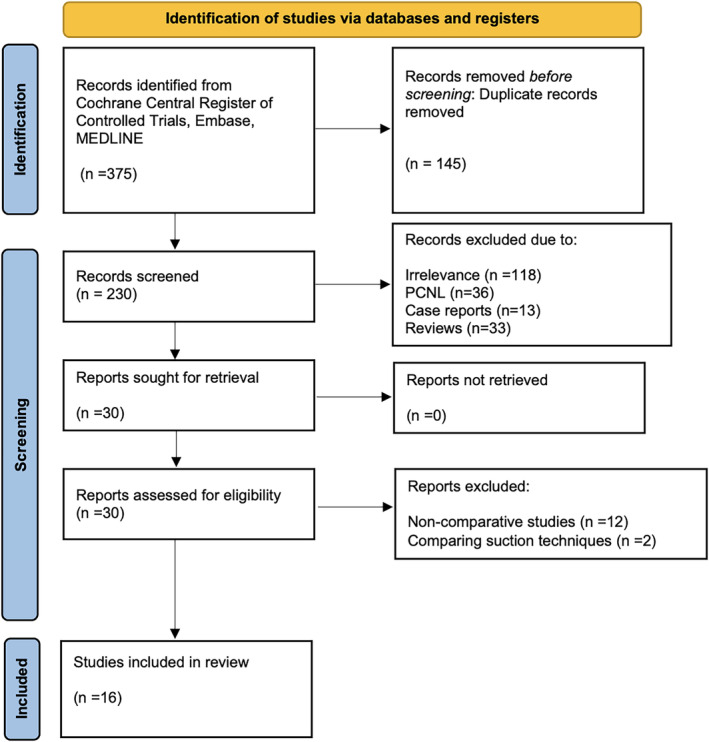
PRISMA flow diagram.
3.1. Overall comparative analysis
Pooled analysis of nine studies revealed a non‐significant difference on immediate SFR between suction and non‐suction groups (RR = 1.15, 95% C.I.: 0.99–1.34, p = 0.08), while analysis of 17 study arms on final SFR showed a significant improvement in favour of suction (RR = 1.12, 95% C.I.: 1.05–1.19, p < 0.001). Auxiliary treatment did not differ significantly. Overall complications as analysed in 17 study arms were significantly lower in suction group (RR = 0.44, 95% C.I.: 0.33–0.57, p < 0.001). Fever (RR = 0.44, 95% C.I.: 0.3–0.64, p < 0.001), infections (RR = 0.43, 95% C.I.: 0.29–0.63, p < 0.001), sepsis (RR = 0.24, 95% C.I.: 0.07–0.75, p = 0.01), pain (RR = 0.22, 95% C.I.: 0.08–0.59, p < 0.001) and transfusion rates (RR = 0.16, 95% C.I.: 0.03–0.88, p = 0.04) were significantly lower in suction group, while no significant differences were detected regarding ureteral stricture formation and embolization. When using Clavien‐Dindo classification, grades I (RR = 0.6, 95% C.I.:0.4–0.9, p = 0.01) and II (RR = 0.37, 95% C.I.: 0.16–0.88, p = 0.02) were significantly lower in suction group (for combined grades I and II, RR = 0.53, 95% C.I.: 0.37–0.76, p < 0.001), while grades III and IV did not differ significantly. Summary forest plots are shown in Figure 2.
FIGURE 2.
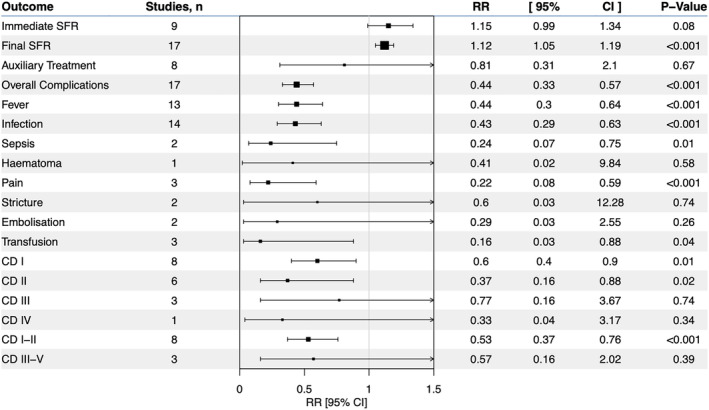
Forest plot for overall comparative analysis of binary outcomes.
Operative time and pain when reported as VAS scores did not differ significantly between the two groups, but LOS was significantly shorter by 1.09 days in suction group (mean difference—1.09, 95% C.I.: −1.9 to −0.28, p = 0.01). Summary forest plots are shown in Figure S1. See Appendix S2, section 4, for individual outcome forest plots and heterogeneity statistics.
3.2. Sensitivity analysis on RCTs only
Pooled analysis of five RCTs revealed no statistically significant difference in both immediate and final SFR, auxiliary treatments, sepsis, stricture formation and Clavien‐Dindo grade I or II complications, although only a single RCT reported results for auxiliary treatments, sepsis and stricture formation. Overall complications (RR = 0.2, 95% C.I.: 0.09–0.41, p < 0.001), infections (RR = 0.22, 95% C.I.: 0.08–0.61, p < 0.001) and fever (RR = 0.22, 95% C.I.: 0.07–0.63, p < 0.001) were significantly lower the suction group. OR time and LOS did not differ significantly between groups. One study analysing pain and VAS score showed results in favour of suction group (RR = 0.16, 95% C.I.: 0.04–0.67, p = 0.01 and MD = −0.34, 95% C.I.: −0.65 to −0.03, p = 0.03). Summary forest plots are shown in Figures S2 and S3. See Appendix S2, section 6, for individual outcome forest plots and heterogeneity statistics.
3.3. Subgroup analysis on semi‐rigid URS only
Pooled analysis of studies comparing suction versus no suction in semi‐rigid URS showed significantly improved final (RR = 1.16, 95% C.I.: 1.07–1.25, p < 0.001) but not immediate SFR in favour of suction group, while rates of auxiliary treatment were also similar. Overall complications (RR = 0.45, 95% C.I.: 0.25–0.83, p = 0.01), fever (RR = 0.29, 95% C.I.: 0.12–0.72, p = 0.01) and infection (RR = 0.29, 95% C.I.: 0.12–0.72, p = 0.01) were significantly lower in suction group, but pain (one study), ureteral stricture formation (one study) and Clavien‐Dindo grades I and II complications were similar between the two groups. LOS was significantly lower in suction group by 0.29 days (MD = −0.29, 95% C.I.: −0.55 to −0.03, p = 0.03), but OR time was similar. Summary forest plots are shown in Figures S4 and S5. See Appendix S2, section 8, for individual outcome forest plots and heterogeneity statistics.
3.4. Subgroup analysis on flexible URS/RIRS only
Pooled analysis of studies comparing suction versus no suction in flexible URS/RIRS revealed significantly improved final SFR (RR = 1.2, 95% C.I.: 1.1–1.3, p < 0.001) but not immediate SFR or auxiliary treatments (one study), in favour of suction group. Overall complications (RR = 0.44, 95% C.I.: 0.29–0.67, p < 0.001), fever (RR = 0.38, 95% C.I.: 0.23–0.65, p < 0.001), infections (RR = 0.38, 95% C.I.: 0.23–0.64, p < 0.001), sepsis at one study (RR = 0.27, 95% C.I.: 0.08–0.96, p = 0.04), Clavien II (RR = 0.28, 95% C.I.: 0.09–0.88, p = 0.03) and I‐II (RR = 0.48, 95% C.I.: 0.29–0.8, p < 0.001) were significantly lower in suction group, while ureteral stricture formation (one study), Clavien‐Dindo I, III, IV and III‐IV (one study) did not differ significantly between the two groups. OR time and LOS did not differ significantly, while VAS score was lower in suction group, as reported in one study. Summary forest plots are shown in Figures S6 and S7. See Appendix S2, section 10, for individual outcome forest plots and heterogeneity statistics.
3.5. Subgroup analysis on mini‐PCNL versus flexible URS/RIRS
Pooled analysis comparing suction in flexible URS/RIRS versus mini‐PCNL revealed no significant differences in both immediate and final SFR, auxiliary treatments, infectious complications (infections, fever and sepsis), hematoma formation (one study), embolization and Clavien‐Dindo I, II, III and IV. However, overall complications (RR = 0.42, 95% C.I.: 0.21–0.81, p = 0.01), pain (RR = 0.21, 95% C.I.: 0.07–0.6, p < 0.001) and transfusion rates (RR = 0.16, 95% C.I.: 0.03–0.88, p = 0.04) were significantly lower in flexible URS/RIRS with the use of suction. OR time did not differ significantly between the two groups, while LOS was significantly shorter by 2.89 days in flexible URS/RIRS group (MD = −2.89, 95% C.I.: −3.55 to −2.23, p < 0.001). VAS score in one study was also significantly lower in flexible URS/RIRS group. Summary forest plots are shown in Figures S8 and S9. See Appendix S2, section 12, for individual outcome forest plots and heterogeneity statistics.
4. DISCUSSION
The two outcomes synthesizing the success of URS/RIRS are SFR and complication rates; suction application seems to be associated with both increased SFRs (mainly final) and substantially reduced complication rates, especially those related to infections. More specifically, final SFR was improved by 12% in suction group, while infectious complications (sepsis, infection and fever) were reduced by 56–76% in suction group when all studies were analysed. In RCTs subgroup analysis, infectious complication rates were also decreased, but SFRs and sepsis rates were similar between suction and non‐suction groups. In further subgroup analysis accordingly to specific types of treatment, in semi‐rigid and flexible URS/ RIRS, final SFRs were improved by 16–20% in suction groups, despite immediate SFRs being similar. Also, in both subanalyses, infectious and overall complications were significantly reduced in suction groups. However, when mini‐PCNL was compared to suction‐aided flexible URS/ RIRS, no significant differences were detected regarding SFRs, auxiliary treatments and infectious complications; reduced rates of overall complications, pain and transfusion rates were seen in suction URS/ RIRS. These findings are probably explained due to suction effectiveness in reducing intrarenal pressure, which can rise during URS/ RIRS from irrigation fluids and lead to pyelovenous and pyelolymphatic backflow and entrance of pathogenic bacteria in systemic circulation. 29 High‐power Holmium and Thulium Fibre laser (TFL) have enhanced the dusting mode of stone disintegration, but vision can be obscured from this ‘cloud of dust’, thus increasing operative time and risk for injuries; when suction is applied, several reports support that vision is not compromised, accounting partially for the reported reduced operative times. 29 Nevertheless, our pooled analysis did not reveal any significant improvement in terms of operative time in any of the groups. The absence of observed significant differences between mini‐PCNL and suction aided URS/RIRS can potentially be explained by the inherent suction component of mini‐PCNL technique itself, due to the ‘Venturi effect’ generated by the dynamic fluid property at the tip of the nephroscope. 30
The first reported RCT evaluating suction in RIRS was by Lechevallier et al., 16 20 years ago, who showed that OR time was significantly reduced, while SFR was higher in suction group (92% vs. 69%, p = 0.048). Du et al. 15 and Chen et al. 18 designed further RCTs to assess suction via a patented perfusion and suction platform in ureteric and renal stones, respectively. The system was connected to a patented ureteral access sheath and was able to maintain a low/negative intrapelvic pressure (5 to −15 mm Hg) with perfusion set at 50–150 ml/min and concluded that its application is effective and safe. A new semi‐rigid ureterorenoscope, the Soton ureterorenoscope, was used by Zhang et al. 17 in comparison with standard ureteroscopy; authors reported improved vision and appropriate control of intrapelvic pressure, leading to reduction of operative time. Aspiration systems have been described also via the scope used for lithotripsy, the so‐called direct in‐scope suction (DISS) technique, as described in the original study. 31 The great advantage of DISS is that the system comprises of a reproducible idea on every ureteroscope. Specifically, two simple three‐way stoppers are attached and allow connection to irrigation and suction tubes according to surgeons' preference during surgery. 31 In the study by Gauhar et al., 31 the DISS technique compared to a traditional suction access sheath led to reduction of LOS and similar residual fragments rates in the cost of increased operative time. Besides ureteral access sheaths and ureteroscopes, ureteral catheters can also serve as a mean of suction application during URS/RIRS. In the study by Wu et al., 23 a modified 5Fr ureteral catheter was connected via a T‐shaped joint to a vacuum system and then introduced into a semi‐rigid ureterorenoscope. This system was tested in patients with impacted ureteral stones in comparison with conventional URS and showed that operative time was significantly lower (38.2 min vs. 46.7 min, P < 0.001), fever rates lower (3.9% vs. 14.6%, p = 0.022) and higher early SFR (88.2% vs. 72%, p = 0.011). 23 In our pooled analysis, immediate SFR was similar, final SFR higher, operative time similar and infectious complications significantly reduced in the group of suction‐aided, semi‐rigid ureteroscopy. An innovative system was described in the pilot study by Sur et al., 13 who used the steerable ureteroscopic renal evacuation catheter (SURE), which was connected to a ureteral access sheath after completing lithotripsy and was guided by fluoroscopy to all calyces in order to apply suction and remove fragmented stone particles. Authors detected a final SFR that was significantly higher in the SURE group compared to basket extraction group (100% vs. 75%, p = 0.20), although number of patients was small. 13
Flexible URS/RIRS is an already costly procedure and adding another technological innovation may reasonably increase the associated costs. Not many studies reported the monetary burden of this technology, but in two studies, Du et al. 15 and Zhang et al. 21 did not show any increased costs; on the contrary, Zhang et al. 21 reported that suction group was associated with significantly lower costs (2622.6 US dollars) compared to rigid URS (2883.6 US dollars) and flexible RIRS (3724.4 US dollars). This was attributed to skipping the use of baskets and forceps and to the reusable design of suction equipment. The trend observed on reduced LOS in suction group may also contribute to cost reduction. Another important limitation of this equipment is its availability since many of the described systems are patented and may not be easy to be acquired. Some of these systems need additional use of fluoroscopy, which may add more hazardous exposure to both patients and operating room staff. 32 , 33
This study is not devoid of limitations. First of all, both observational and randomized studies were collected due to paucity of data derived from RCTs; however, subgroup and sensitivity analysis was also performed for RCTs showing similar results excluding the SFRs and specific types of complications. Existing RCTs analyse small sizes and different stone location/types of suction; thus, we have chosen to include also overall analysis including observational studies. Suction and irrigation settings were also widely variable, contributing to the heterogeneity of the results among studies, while definition and assessment (timepoint and examination used) of SFRs and complications were also variable. Endourological equipment is continuously enriched, and endourologists are blessed and cursed at the same time to have a vast number of choices regarding every step of ureteroscopy; to name some, guidewires, stents, ureteroscopes, access sheaths, laser types and settings, graspers and baskets are only the main categories. Adding to this complexity, several suction devices are already available and tested: semirigid ureteroscopes with incorporated suction, ureteral access sheaths with suction, which can be steerable or not, several suction techniques such as direct‐in‐scope‐technique or the flexible and navigable ureteral suction sheath (FANS). The comparative studies found in literature were heterogeneous regarding suction type, stone type/size and location, technique used for comparison (miniPCNL or non‐suction ureteroscopy), pressure used for suction and irrigation. In order to be able to incorporate suction technology for specific indications, we certainly need sounder and more robust comparative RCTs for specific patient populations and specific suction technology. Despite these limitations, this is the first systematic review with a meta‐analysis on suction use for URS/RIRS and may serve as the basis for designing proper clinical trials to define the indications, protocols, safety and effectiveness of these systems, since paucity of existing data prevents us from comparing which suction mechanism has the best possible potential to improve RIRS in future.
5. CONCLUSIONS
Application of suction via ureteral access sheaths, ureteral catheters or scopes may provide improved SFRs, reduced overall and infectious complication rates, along with a reduction in length of hospital stay. Further randomized studies are needed to validate these findings and standardize indications and protocols.
AUTHOR CONTRIBUTIONS
Lazaros Tzelves: Conception/design of the work; acquisition/analysis/interpretation of data; drafting the manuscript. Robert Geraghty: Acquisition/analysis/interpretation of data; critically reviewing the manuscript for important intellectual content. Patrick Juliebø‐Jones: acquisition/analysis/interpretation of data; critically reviewing the manuscript for important intellectual content. Yuhong Yuan: Acquisition/analysis/interpretation of data; critically reviewing the manuscript for important intellectual content. Konstantinos Kapriniotis: Acquisition/analysis/interpretation of data; critically reviewing the manuscript for important intellectual content. Daniele Castellani: Acquisition/analysis/interpretation of data; critically reviewing the manuscript for important intellectual content. Vineet Gauhar: Acquisition/analysis/interpretation of data; critically reviewing the manuscript for important intellectual content. Andreas Skolarikos: Acquisition/analysis/interpretation of data; critically reviewing the manuscript for important intellectual content. Bhaskar Somani: Conception/design of the work; acquisition/analysis/interpretation of data; critically reviewing the manuscript for important intellectual content.
CONFLICT OF INTEREST STATEMENT
L. Tzelves is an associate member of EAU Guidelines Panel on Urolithiasis, a YAU Member in Endourology Group and a member of ESU Working Group on PCNL. R. Geraghty is an associate member of EAU Guidelines Panel on Urolithiasis. P. Juliebø‐Jones is a YAU Member in Endourology Group. Y. Yuan is a member of EAU Guidelines Methods Office. G. Vineet is a clinical and education research consultant for PUSEN, BIORAD, CLEARPETRA, INNOVEX, ROCAMED and BD and a member of European Section of Urolithiasis (EULIS), EAU Guidelines Dissemination committee; a board member of endourology academy; and a board member of kidney stone academy. A. Skolarikos is a member of EAU Guidelines panel on Urolithiasis and European Section of Urolithiasis (EULIS). B. Somani is a member of EAU Guidelines panel on Urolithiasis and European Section of Urolithiasis (EULIS).
Supporting information
Appendix S1. Supporting Information
Appendix S2. Supporting Information
Table S1. Risk of bias for randomized controlled trials (Risk of Bias 2 tool)
Table S2. Risk of bias for non‐randomized comparative trials (ROBINS‐I tool)
Table S3. Certainty of the evidence for each outcomes based on the GRADE approach
Figure S1. Forest plot for overall comparative analysis of continuous outcomes
Figure S2. Forest plot for analysis of binary outcomes in RCTs
Figure S3. Forest plot for analysis of continuous outcomes in RCTs
Figure S4. Forest plot for analysis of binary outcomes in semi‐rigid URS
Figure S5. Forest plot for analysis of continuous outcomes in semi‐rigid URS
Figure S6. Forest plot for analysis of binary outcomes in flexible URS/RIRS
Figure S7. Forest plot for analysis of continuous outcomes in flexible URS/RIRS
Figure S8. Forest plot for analysis of binary outcomes in flexible URS/RIRS vs mini‐PCNL
Figure S9. Forest plot for analysis of continuous outcomes in flexible URS/RIRS vs mini‐PCNL
ACKNOWLEDGEMENTS
None.
Tzelves L, Geraghty R, Juliebø‐Jones P, Yuan Y, Kapriniotis K, Castellani D, et al. Suction use in ureterorenoscopy: A systematic review and meta‐analysis of comparative studies. BJUI Compass. 2024;5(10):895–912. 10.1002/bco2.408
Funding information No funding was received.
REFERENCES
- 1. Juliebø‐Jones P, Keller EX, de Coninck V, Uguzova S, Tzelves L, Æsøy MS, et al. Controversies in ureteroscopy: lasers, scopes, ureteral access sheaths, practice patterns and beyond. Front Surg. 2023;10:1274583. 10.3389/fsurg.2023.1274583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tzelves L, Somani B, Berdempes M, Markopoulos T, Skolarikos A. Basic and advanced technological evolution of laser lithotripsy over the past decade: an educational review by the European Society of Urotechnology Section of the European Association of Urology. Turk J Urol. 2021;47(3):183–192. 10.5152/tud.2021.21030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tzelves L, Türk C, Skolarikos A. European Association of Urology Urolithiasis Guidelines: where are we going? Eur Urol Focus. 2021;7(1):34–38. 10.1016/j.euf.2020.09.011 [DOI] [PubMed] [Google Scholar]
- 4. Gauhar V, Chew BH, Traxer O, Tailly T, Emiliani E, Inoue T, et al. Indications, preferences, global practice patterns and outcomes in retrograde intrarenal surgery (RIRS) for renal stones in adults: results from a multicenter database of 6669 patients of the global FLEXible ureteroscopy Outcomes Registry (FLEXOR). World J Urol. 2023;41(2):567–574. 10.1007/s00345-022-04257-z [DOI] [PubMed] [Google Scholar]
- 5. Geraghty RM, Davis NF, Tzelves L, Lombardo R, Yuan C, Thomas K, et al. Best practice in interventional management of urolithiasis: an update from the European Association of Urology Guidelines Panel for Urolithiasis 2022. Eur Urol Focus. 2023;9(1):199–208. 10.1016/j.euf.2022.06.014 [DOI] [PubMed] [Google Scholar]
- 6. Tzelves L, Geraghty R, Lombardo R, Davis NF, Petřík A, Neisius A, et al. Duration of follow‐up and timing of discharge from imaging follow‐up, in adult patients with urolithiasis after surgical or medical intervention: a systematic review and meta‐analysis from the European Association of Urology Guideline Panel on Urolithiasis. Eur Urol Focus. 2023;9(1):188–198. 10.1016/j.euf.2022.06.016 [DOI] [PubMed] [Google Scholar]
- 7. Zhong W, Leto G, Wang L, Zeng G. Systemic inflammatory response syndrome after flexible ureteroscopic lithotripsy: a study of risk factors. J Endourol. 2015;29(1):25–28. 10.1089/end.2014.0409 [DOI] [PubMed] [Google Scholar]
- 8. Giulioni C, Castellani D, Traxer O, Gadzhiev N, Pirola GM, Tanidir Y, et al. Experimental and clinical applications and outcomes of using different forms of suction in retrograde intrarenal surgery. Results from a systematic review. Actas Urol Esp (Engl Ed). 2024;48(1):57–70. 10.1016/j.acuroe.2023.06.001 [DOI] [PubMed] [Google Scholar]
- 9. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89. 10.1186/s13643-021-01626-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS‐I: a tool for assessing risk of bias in non‐randomised studies of interventions. Bmj. 2016;355:i4919. 10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. Bmj. 2019;366:l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 12. Atkins D, Eccles M, Flottorp S, Guyatt GH, Henry D, Hill S, et al. Systems for grading the quality of evidence and the strength of recommendations I: critical appraisal of existing approaches The GRADE Working Group. BMC Health Serv Res. 2004;4(1):38. 10.1186/1472-6963-4-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sur RL, Agrawal S, Eisner BH, Haleblian GE, Ganpule AP, Sabnis RB, et al. Initial safety and feasibility of steerable ureteroscopic renal evacuation: a novel approach for the treatment of urolithiasis. J Endourol. 2022;36(9):1161–1167. 10.1089/end.2021.0759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tang QL, Liang P, Ding YF, Zhou XZ, Tao RZ. Comparative efficacy between retrograde intrarenal surgery with vacuum‐assisted ureteral access sheath and minimally invasive percutaneous nephrolithotomy for 1–2 cm infectious upper ureteral stones: a prospective, randomized controlled study. Front Surg. 2023;10:1200717. 10.3389/fsurg.2023.1200717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Du C, Song L, Wu X, Deng X, Yang Z, Zhu X, et al. A study on the clinical application of a patented perfusion and suctioning platform and ureteral access sheath in the treatment of large ureteral stones below L4 level. Int Urol Nephrol. 2019;51(2):207–213. 10.1007/s11255-018-2049-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lechevallier E, Luciani M, Nahon O, Lay F, Coulange C. Transurethral ureterorenolithotripsy using new automated irrigation/suction system controlling pressure and flow compared with standard irrigation: a randomized pilot study. J Endourol. 2003;17(2):97–101. 10.1089/08927790360587423 [DOI] [PubMed] [Google Scholar]
- 17. Zhang X, Liu Z, Chen X, Li D, Yang Z, Gu J, et al. The effect of application of a Soton ureteroscope on infection after flexible ureteroscopy lithotripsy. Wideochir Inne Tech Maloinwazyjne. 2022;17(1):232–239. 10.5114/wiitm.2021.107763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chen H, Qiu X, Du C, Xie D, Liu T, Wang G, et al. The comparison study of flexible ureteroscopic suctioning lithotripsy with intelligent pressure control versus minimally invasive percutaneous suctioning nephrolithotomy in treating renal calculi of 2 to 3 cm in size. Surg Innov. 2019;26(5):528–535. 10.1177/1553350619849782 [DOI] [PubMed] [Google Scholar]
- 19. Lai D, He Y, Li X, Chen M, Zeng X. RIRS with vacuum‐assisted ureteral access sheath versus MPCNL for the treatment of 2‐4 cm renal stone. Biomed Res Int. 2020;2020:8052013. 10.1155/2020/8052013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zhu Z, Cui Y, Zeng F, Li Y, Chen Z, Hequn C. Comparison of suctioning and traditional ureteral access sheath during flexible ureteroscopy in the treatment of renal stones. World J Urol. 2019;37(5):921–929. 10.1007/s00345-018-2455-8 [DOI] [PubMed] [Google Scholar]
- 21. Zhang LW, Fei X, Song Y. The clinical efficacy of novel vacuum suction ureteroscopic lithotripsy in the treatment of upper ureteral calculi. World J Urol. 2021;39(11):4261–4265. 10.1007/s00345-021-03722-5 [DOI] [PubMed] [Google Scholar]
- 22. Huang J, Yang Y, Xie H, Fu Z, Zhu F, Xie L, et al. Vacuum‐assisted dedusting lithotripsy in the treatment of kidney and proximal ureteral stones less than 3 cm in size. World J Urol. 2023;41(11):3097–3103. 10.1007/s00345-023-04595-6 [DOI] [PubMed] [Google Scholar]
- 23. Wu ZH, Wang YZ, Liu TZ, Wang XH, Zhang C, Zhang WB, et al. Comparison of vacuum suction ureteroscopic laser lithotripsy and traditional ureteroscopic laser lithotripsy for impacted upper ureteral stones. World J Urol. 2022;40(9):2347–2352. 10.1007/s00345-022-04075-3 [DOI] [PubMed] [Google Scholar]
- 24. Ding J, Su T, Zhang X, Qian S, Duan L, Huang Y, et al. Omnidirectional (flexible) ureteral access sheath: safety, efficacy, and initial experience report. J Endourol. 2023;37(11):1184–1190. 10.1089/end.2023.0358 [DOI] [PubMed] [Google Scholar]
- 25. Zhai Q, Zhang J, Wei Q, Zeng M, Song L, Zhang Y, et al. Clinical application of novel integrated suctioning semi‐rigid ureteroscopic lithotripsy. Minim Invasive Ther Allied Technol. 2023;32(6):314–322. 10.1080/13645706.2023.2225599 [DOI] [PubMed] [Google Scholar]
- 26. Qian X, Liu C, Hong S, Xu J, Qian C, Zhu J, et al. Application of suctioning ureteral access sheath during flexible ureteroscopy for renal stones decreases the risk of postoperative systemic inflammatory response syndrome. Int J Clin Pract. 2022;2022:9354714. 10.1155/2022/9354714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Deng X, Xie D, Huang X, Huang J, Song L, Du C. Suctioning flexible ureteroscopy with automatic control of renal pelvic pressure versus mini PCNL for the treatment of 2‐3‐cm kidney stones in patients with a solitary kidney. Urol Int. 2022;106(12):1293–1297. 10.1159/000521373 [DOI] [PubMed] [Google Scholar]
- 28. AlSmadi JK, Li X, Zeng G. Use of a modified ureteral access sheath in semi‐rigid ureteroscopy to treat large upper ureteral stones is associated with high stone free rates. Asian J Urol. 2019;6(3):217–221. 10.1016/j.ajur.2018.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tzelves L, Skolarikos A. Suction use during endourological procedures. Curr Urol Rep. 2020;21(11):46. 10.1007/s11934-020-00998-9 [DOI] [PubMed] [Google Scholar]
- 30. Gadzhiev N, Sergei B, Grigoryev V, Okhunov Z, Ganpule A, Pisarev A, et al. Evaluation of the effect of Bernoulli maneuver on operative time during mini‐percutaneous nephrolithotomy: a prospective randomized study. Investig Clin Urol. 2017;58(3):179–185. 10.4111/icu.2017.58.3.179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gauhar V, Somani BK, Heng CT, Gauhar V, Chew BH, Sarica K, et al. Technique, feasibility, utility, limitations, and future perspectives of a new technique of applying direct in‐scope suction to improve outcomes of retrograde intrarenal surgery for stones. J Clin Med. 2022;11(19). 10.3390/jcm11195710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Vassileva J, Zagorska A, Basic D, Karagiannis A, Petkova K, Sabuncu K, et al. Radiation exposure of patients during endourological procedures: IAEA‐SEGUR study. J Radiol Prot. 2020;40(4). 10.1088/1361-6498/abc351 [DOI] [PubMed] [Google Scholar]
- 33. Vassileva J, Zagorska A, Karagiannis A, Petkova K, Sabuncu K, Saltirov I, et al. Radiation exposure of surgical team during endourological procedures: International Atomic Energy Agency‐South‐Eastern European Group for Urolithiasis Research Study. J Endourol. 2021;35(5):574–582. 10.1089/end.2020.0630 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Supporting Information
Appendix S2. Supporting Information
Table S1. Risk of bias for randomized controlled trials (Risk of Bias 2 tool)
Table S2. Risk of bias for non‐randomized comparative trials (ROBINS‐I tool)
Table S3. Certainty of the evidence for each outcomes based on the GRADE approach
Figure S1. Forest plot for overall comparative analysis of continuous outcomes
Figure S2. Forest plot for analysis of binary outcomes in RCTs
Figure S3. Forest plot for analysis of continuous outcomes in RCTs
Figure S4. Forest plot for analysis of binary outcomes in semi‐rigid URS
Figure S5. Forest plot for analysis of continuous outcomes in semi‐rigid URS
Figure S6. Forest plot for analysis of binary outcomes in flexible URS/RIRS
Figure S7. Forest plot for analysis of continuous outcomes in flexible URS/RIRS
Figure S8. Forest plot for analysis of binary outcomes in flexible URS/RIRS vs mini‐PCNL
Figure S9. Forest plot for analysis of continuous outcomes in flexible URS/RIRS vs mini‐PCNL


