Abstract
Background
Emergency departments increasingly serve patients who prefer a language other than English. Honoring patients’ language preferences is crucial for quality and cultural appropriateness of care. We sought to assess whether time spent in caring for patients who preferred a language other than English differed from patients whose language preference was English. Secondarily, we sought to assess professional reimbursement across the two groups.
Methods
We retrospectively analyzed an existing dataset from a time‐in‐motion study that included direct observation measurements of emergency physicians’ time spent during patient encounters. Our primary outcome was physician time spent conducting patient care, comparing patients who preferred a language other than English to patients who preferred English. Secondarily, we sought to assess if relative value unit (RVU)‐based compensation differed across the two groups. We calculated descriptive statistics and performed multivariable regression.
Results
Across 218 patient encounters, physicians spent 18.6% longer on encounters with patients whose preferred a language other than English (median = 18.5 min, interquartile range [IQR] 14.8–27.9 min) than for those who preferred English (median = 15.6 min, IQR 11.5–22.9 min; p = 0.04). After controlling for other factors, patients’ preferred language was not associated with increased RVUs (β = −0.12, t = −1.94, p = 0.055).
Conclusions
Emergency physicians appear to spend more time caring for patients who prefer a language other than English. This additional effort during the care of this potentially vulnerable population may not be reflected in past and current reimbursement structures. Additional research is prudent as we seek to better address social determinants of health in care delivery and reimbursement systems.
1. BACKGROUND
In the United States, nearly 68 million people speak a language other than English at home, and this number has tripled in the last 40 years. 1 As this trend continues, emergency departments (EDs) will increasingly serve patients who prefer a language other than English. Patients’ language preferences in healthcare settings are associated with language proficiency, but other factors including their self‐perceived linguistic and literacy skills as well as their cultural preferences and values also contribute to their preferred language choice for healthcare settings. 2 , 3 There is no generally accepted standard to define and measure language proficiency; however, multiple studies have reported that patients with limited English language proficiency experience inequities in healthcare access and outcomes, as well as increased diagnostic testing and variable admission rates. 4 , 5 , 6 , 7
1.1. Importance
Honoring a patient's language preference is crucial for quality and cultural appropriateness of care but may add complexity to care delivery. While increased resource utilization has been demonstrated, 7 little is known how physicians’ time in direct care of these patients is impacted. Prior research is limited and focuses on primary care with one study showing that physicians spent similar time across non‐English‐speaking and English‐speaking patients. 8 However, another study showed that physicians spent more time with patients with limited English proficiency, prompting those authors to call for “additional reimbursement” to provide “high‐quality care” for those patients. 9
1.2. Goals of this investigation
We sought to assess if emergency physicians’ time spent in caring for patients who preferred a language other than English differed from patients whose language preference was English. As a secondary goal, we sought to assess professional fee‐for‐service compensation across the two groups.
The Bottom Line
Among 218 patient encounters directly observed during a time‐in‐motion study, emergency physicians spent 18.6% longer on encounters with patients who preferred a language other than English (median = 18.5 min, IQR 14.8–27.9 min) than for those who preferred English (median = 15.6 min, IQR 11.5–22.9 min; p = 0.04). In the same population, language preference was not associated with increased relative value unit generation, raising the possibility that patients who preferred a language other than English experienced a lower and inequitable relative value unit increase relative to physician time spent, potentially uncovering an important national health policy improvement opportunity related to advancing language access.
2. METHODS
2.1. Study design and setting
We retrospectively analyzed an existing dataset from a time‐in‐motion study that included direct observation measurements of physicians’ time spent during ED encounters. 10 The dataset included 218 encounters between January and November of 2021, during which trained research assistants (RAs) observed 11 attending emergency physicians at two sites: an urban, academic ED with approximately 65,000 annual adult encounters and an urban, community ED with approximately 43,000 annual encounters. The investigation was approved by the institutional review board.
2.2. Dataset description
The time‐in‐motion study dataset included only complete encounters involving a single ED attending physician and encounters not involving trainees. RAs timed physician activities in 15‐s increments, categorizing activities as: patient/family/surrogate interactions, ED staff interactions, consultant interactions, computer/documentation‐related activities, procedure‐related activities, and other. Ten encounters were observed by all RAs as part of inter‐rater reliability assessment, which was excellent. 10 Abstracted patient data within the original dataset included age, sex, triage score (emergency severity index [ESI]), disposition, and preferred language reported at registration.
2.3. Outcomes and measures
Our primary outcome was emergency physician time spent conducting patient care, comparing patients who preferred a language other than English to patients who preferred English. As a secondary outcome, we sought to assess if Current Procedural Terminology (CPT)/relative value unit (RVU)‐based compensation differed across the two groups. To accomplish the latter, we abstracted from our integrated billing system the evaluation and management (E&M) CPT codes for each encounter within the time‐in‐motion dataset and calculated their corresponding professional services total RVUs using the published 2021 CMS fee schedule. 11 We opted for RVUs, standard across all payors and self‐pay patients, as opposed to charges/payments that were subject to local, negotiated contractual adjustments.
2.4. Analysis
We calculated descriptive statistics and used chi‐square tests and Mann–Whitney U tests as appropriate for between‐group comparisons of physician time spent overall as well as sub‐categories of physician activities. Physician time spent during encounters was not normally distributed, so we built a log‐transformed least‐squares regression model with preferred language, categorical age (≤25, 26–45, 46–65, and ≥66 years), payer type, ESI, disposition, patient sex, and RVUs as independent variables with physician identifier as a fixed effect. For our secondary outcome analysis, we built as similar model but with identity‐linked RVUs as the outcome of interest and total physician time spent included as an explanatory variable in addition to the variables in the primary model. We used SPSS version 28 (IBM) for analysis.
3. RESULTS
Patients in 56 of 218 encounters (25.7%) reported a language preference other than English. A sample description and comparative statistics between patients who preferred English versus another language are reported in Table 1. Those reporting a preferred language other than English were younger and more likely to be insured by Medicaid.
TABLE 1.
Sample description and primary comparison of patients whose preferred language was English versus a language other than English.
| Preferred language | |||||||
|---|---|---|---|---|---|---|---|
| English | Other | ||||||
| n | % | n | % | χ 2 | p | ||
| Sex | Female | 85 | 52.5 | 32 | 57.1 | 0.37 | 0.55 |
| Male | 77 | 47.5 | 24 | 42.9 | |||
| Age group | ≤25 years | 28 | 17.3 | 17 | 30.4 | 7.4 a | 0.006 |
| 26–45 years | 62 | 38.3 | 20 | 35.7 | |||
| 46–65 years | 41 | 25.3 | 18 | 32.1 | |||
| ≥66 years | 31 | 19.1 | 1 | 1.8 | |||
| Disposition | Discharged | 134 | 82.7 | 51 | 91.1 | 2.26 | 0.13 |
| Admitted | 28 | 17.3 | 5 | 8.9 | |||
| Emergency severity | 2 | 27 | 16.7 | 8 | 14.3 | 0.68 a | 0.41 |
| Index (ESI) score | 3 | 86 | 53.1 | 27 | 48.2 | ||
| 4 | 43 | 26.5 | 19 | 33.9 | |||
| 5 | 6 | 3.7 | 2 | 3.6 | |||
| Current procedural | 99,282 (1.24) | 19 | 11.8 | 8 | 14.3 | 5.76 a | 0.02 |
| Terminology code | 99,283 (2.09) | 14 | 8.7 | 8 | 14.3 | ||
| (relative value unit) | 99,284 (3.55) | 71 | 44.1 | 30 | 53.6 | ||
| 99,285 (5.18) | 49 | 30.4 | 10 | 17.9 | |||
| 99,291 (8.11) | 8 | 5.0 | 0 | 0.0 | |||
| Payor type | Medicare | 39 | 24.1 | 4 | 7.14 | 15.51 | <0.001 |
| Medicaid | 68 | 42.0 | 40 | 71.4 | |||
| Commercial | 44 | 27.2 | 10 | 17.9 | |||
| None/self‐pay | 11 | 6.8 | 2 | 3.6 | |||
Ordinal value, used chi‐square for trend.
Overall, physicians spent 16.5 min during each encounter on median (interquartile range [IQR] 12.0–23.6 min). Physicians spent 18.6% longer on encounters with patients whose preferred a language other than English (median = 18.5 min, IQR 14.8–27.9 min) than for those who preferred English (median = 15.6 min, IQR 11.5–22.9 min; p = 0.04). This difference appeared to be accounted for predominantly in the patient/family/surrogate interaction sub‐category (median = 8.5 min, IQR 5.5–12.08 min vs. median = 6.0 min, IQR 3.75–9 min, U = 5797, p = 0.002). No other activity sub‐categories reached statistical significance.
For the primary outcome, regression model performance was R 2 = 0.33, F(22,184) = 4.15, p ≤ 0.001. Table 2 shows the model results. In the fully adjusted model, preferred language other than English was associated with 1.25x more time spent by the physician (β = 0.22, t = 3.30, p = 0.001).
TABLE 2.
Model results for physician time spent, controlling for individual physicians. a
| Variable | B | β | T | p |
|---|---|---|---|---|
| Language preference other than English | 0.105 | 0.219 | 3.265 | 0.001 |
| Sex | −0.010 | −0.024 | −0.0367 | 0.714 |
| Age 26–45 years | −0.024 | −0.055 | −0.647 | 0.519 |
| Age 46–65 years | 0.037 | 0.078 | 0.911 | 0.363 |
| Age ≥ 66 years | 0.017 | 0.029 | 0.284 | 0.777 |
| Disposition = admitted | 0.030 | 0.050 | 0.663 | 0.508 |
| Emergency severity index (ESI) = 3 | −0.022 | −0.051 | −0.548 | 0.584 |
| ESI = 4 | −0.134 | −0.288 | −2.896 | 0.004 |
| ESI = 5 | −0.134 | −0.106 | −1.483 | 0.140 |
| Payor type = Medicaid | −0.015 | −0.035 | −0.309 | 0.758 |
| Commercial | 0.008 | 0.017 | 0.161 | 0.872 |
| None/self‐pay | 0.006 | 0.007 | 0.086 | 0.931 |
Overall model performance: R 2 = 0.33, F(22,184) = 4.15, p = <0.001.
For the secondary outcome, regression model performance was R 2 = 0.46, F(22,184) = 7.00, p ≤ 0.001. Table 3 shows the model results. After controlling for other factors, patients’ preferred language was not associated with increased RVUs (β = ‐0.12, t = −1.94, p = 0.055). Distribution of RVU levels between non‐English versus English language preference is shown in Figure 1. Predictors of RVUs were ESI of 4.0 (β = −0.24, p = 0.007), disposition of admission (β = 0.34, p < 0.001), and physician time spent (β = 0.19, p = 0.004).
TABLE 3.
Model results for relative value units, controlling for individual physicians. a
| Variable | B | β | T | p |
|---|---|---|---|---|
| Language preference other than English | −0.408 | −0.119 | −1.935 | 0.055 |
| Sex | 0.106 | 0.035 | 0.588 | 0.557 |
| Age 26–45 years | 0.387 | 0.123 | 1.618 | 0.107 |
| Age 46–65 years | 0.259 | 0.076 | 0.992 | 0.323 |
| Age ≥ 66 years | 0.053 | 0.012 | 0.136 | 0.892 |
| Disposition = admitted | 1.418 | 0.337 | 5.290 | <0.001 |
| Emergency severity index (ESI) = 3 | −0.244 | −0.080 | −0.963 | 0.337 |
| ESI = 4 | −0.809 | −0.244 | −2.712 | 0.007 |
| ESI = 5 | −1.052 | −0.116 | −1.811 | 0.072 |
| Payor type = Medicaid | 0.084 | 0.028 | 0.272 | 0.786 |
| Commercial | 0.452 | 0.128 | 1.387 | 0.167 |
| None/Self‐pay | −0.815 | −0.120 | −1.742 | 0.83 |
| Total time spent by physician | 1.360 | 0.191 | 2.932 | 0.004 |
Overall model performance: R 2 = 0.46, F(22,184) = 7.00, p = < 0.001.
FIGURE 1.
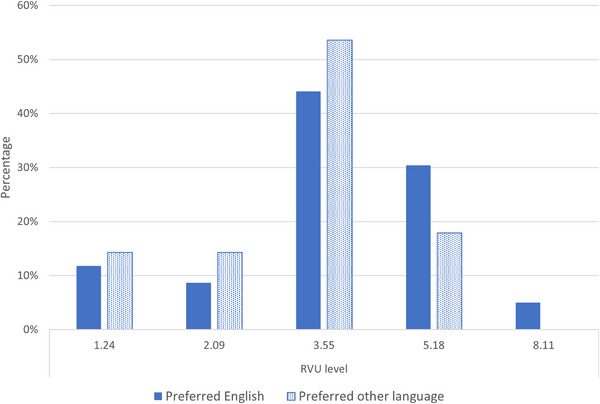
Proportion of encounters at each relative value unit (RVU) level by patient language preference.
4. LIMITATIONS
The database utilized for this investigation had characteristics that may limit generalizability. A relatively small number of physicians from a single academic department were observed, and their selection involved convenience sampling. Therefore, their patient care and documentation practices may not have reflected national norms, and their individual characteristics may have been drivers of observed differences in time spent with patients and RVUs generated. The database was not specifically powered for this investigation. While we attempted to control for observable confounders, the assumptions of ordinary least squares regression could have been inadvertently violated in our design. The RVU null result may reflect insufficient observations. Similarly, we were unable to draw conclusions about how sub‐categories other than patient/family/surrogate impacted overall time spent, opening the possibility that other subcategories also could have had disproportionate impact. We opted to report measures of statistical significance understanding that aspects of our design did not lend themselves to hypothesis testing research, but omission of statistical details would have made our findings less interpretable. Only E&M RVUs were included in our analysis, so it remains unknown if procedural RVUs may have affected reimbursement across the groups. The sample's ESI and patient sex distributions appeared similar to national trends, however it appeared to have a lower proportion of patients 66 years and older (14.7% vs. 17.8%) and higher proportion of patients age 45–65 (27.1% vs. 23.4%). 12 , 13 How this may have affected the results remains unclear and may represent a selection effect among patient encounters more likely to have a single emergency physician for the entire encounter and without trainees. Federal law requires offering interpreter services to patients, but patients were permitted to decline. Due to concerns of reliability of documentation of medical interpreter use, we did not consider whether an interpreter was used or the modality of interpretation. It is prudent to note that time spent by physicians is only one component of physician effort in patient care. In fact, in the determination of RVU valuation, physician “work” considerations include physicians’ mental and physical effort, technical skill, and stress, in addition to time spent. Time spent was the only component measured in our study due to feasibility of measurement and inherent subjectivity associated with the other components. 14
5. DISCUSSION
Our investigation revealed that emergency physicians spent more time caring for patients who preferred a language other than English compared to patients who preferred English. This is the first ED‐based investigation to explore this topic, and to date, research related to this topic has been lacking across healthcare in general. 8 , 9 Our results are significant in that they shed light onto how patient language preference may interact with the ED clinical environment as a social driver of health and potentially support prior literature suggesting that reimbursement systems may not adequately address additional resource needs related to patient language preference. 9
The observation that physicians spent more time with this potentially vulnerable population was promising in that they appeared to be addressing a real or perceived need for these patients. The majority of the difference was accounted for in time spent with patients/family/surrogates. Intuitively, that additional time was likely due to inefficiencies associated with communication: interpretation requires a message to be communicated twice, once by the source and once by the interpreter. Other factors such as verifying accuracy of communication exchange, asking repetitive or confirmatory questions, or having additional conversation also are possible. It also is conceivable that physicians spent more time in activities such a review of records or contacting providers familiar with the patients to address real or perceived communication gaps. To optimize language‐discordant interactions going forward, research is needed to better delineate why more time is utilized and how potentially to improve these interactions.
While physicians spent more time caring for patients who preferred a language other than English, it appeared that E&M reimbursement may not have been commensurate with the additional time spent for that population. Time spent was independently associated with RVUs, but patient language preference was not, raising the possibility that patients who preferred a language other than English experienced a lower and inequitable RVU increase relative to physician time spent than patients who preferred English. We could not draw firm conclusions in this regard due to unavoidable methodological limitations (especially that we were unable to measure many other potential drivers of RVU valuation), but a finding of lower RVUs for encounters with patients who preferred a language other than English relative to the amount of time spent would be interesting and important. More research in this area is prudent because if this observed trend proves true, it exposes a national health equity policy opportunity. In April 2022, CMS published its “Framework for Health Equity 2022–2032,” outlining a number of priorities including advancing language access. 15 Specifically, CMS cited that “each person [it] serves should receive effective, understandable, and respectful care that is responsive to their preferred languages or dialects.” Given that language preference is considered a priority driver of health, the potential that it is not adequately accounted for in reimbursement structures is meaningful. Coding of most ED encounters is not time‐based, but in 2023 (after our investigation period), coding guidelines were changed to better address social determinants of health in RVU valuation. Language preference and time spent may be interdependent in a conceptual sense, but our observational approach does not allow us to determine which factors may be causative, versus serve as proxies for other unmeasured variables. Nonetheless, we remain concerned that language preference may not be adequately addressed even in the new system as it does not appear to be included in the list of social drivers for which standardized coding methods exist,16,17 which would be prerequisite to valuation and reimbursement.
In conclusion, emergency physicians appear to spend more time caring for patients who prefer a language other than English compared to patients who prefer English. Notably, this additional time spent during the care of this potentially vulnerable population may not be reflected in past and current reimbursement structures. Additional research in this regard is prudent as we seek to better address social determinants of health in care delivery and our reimbursement systems.
AUTHOR CONTRIBUTIONS
Martin A. Reznek, Jennifer Edwards, and Celine Larkin conceived the study. Martin A. Reznek, Jennifer Edwards, Alexandra Sanseverino, and Celine Larkin supervised the conduct of the trial and data collection. Sean S. Michael and Celine Larkin provided statistical advice on study design and analyzed the data. Martin A. Reznek, Jennifer Edwards, Sean S. Michael, Jacqueline Furbacher, and Celine Larkin drafted the manuscript, and all authors contributed substantially to its revision. Martin A. Reznek takes responsibility for the paper as a whole. (Sean S. Michael contributed to this article in his personal capacity. The views expressed are those of the authors and do not necessarily represent the views of the United States Government or any government agency.)
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Biography
Martin Reznek, MD, MBA, is an attending physician and Professor and Executive Vice Chair for Clinical Operations and Education in the Department of Emergency Medicine at the UMass Chan Medical School and UMass Memorial Health in Worcester, Massachusetts.

Reznek MA, Edwards J, Michael SS, et al. Emergency physicians spend more time caring for patients who prefer a language other than English which may not be accounted for in reimbursement structures. JACEP Open. 2024;5:e13332. 10.1002/emp2.13332
Supervising Editor: Remle Crowe, PhD, NREMT
DATA AVAILABILITY STATEMENT
Deidentified partial datasets may be available upon publication of the manuscript and approval of the study site IRB following request to Dr. Reznek from investigators who provide an IRB letter of approval.
REFERENCES
- 1. Dietrich S, Hernandez E. Language use in the United States: 2019. United State Census Bureau; 2022. Accessed April 27, 204. https://www.census.gov/content/dam/Census/library/publications/2022/acs/acs‐50.pdf
- 2. Gee GC, Wals∖emann KM, Takeuchi DT. English proficiency and language preference: testing the equivalence of two measures. Am J Public Health. 2010;100(3):563‐569. doi: 10.2105/AJPH.2008.156976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ortega P, Shin TM, Martinez GA. Rethinking the term “limited english proficiency” to improve language‐appropriate healthcare for all. J Immigr Minor Health. 2022;24(3):799‐805. doi: 10.1007/s10903-021-01257-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ponce NA, Hays RD, Cunningham WE. Linguistic disparities in health care access and health status among older adults. J Gen Intern Med. 2006;21(7):786‐791. doi: 10.1111/j.1525-1497.2006.00491.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mui AC, Kang SY, Kang D, Domanski MD. English language proficiency and health‐related quality of life among Chinese and Korean immigrant elders. Health Soc Work. 2007;32(2):119‐127. doi: 10.1093/hsw/32.2.119 [DOI] [PubMed] [Google Scholar]
- 6. Ng E, Pottie K, Spitzer D. Official language proficiency and self‐reported health among immigrants to Canada. Health Rep. 2011;22(4):15‐23. [PubMed] [Google Scholar]
- 7. Schulson L, Novack V, Smulowitz PB, Dechen T, Landon BE. Emergency Department care for patients with limited English proficiency: a retrospective cohort study. J Gen Intern Med. 2018;33(12):2113‐2119. doi: 10.1007/s11606-018-4493-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tocher TM, Larson EB. Do physicians spend more time with non‐English‐speaking patients. J Gen Intern Med. 1999;14(5):303‐309. doi: 10.1046/j.1525-1497.1999.00338.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kravitz RL, Helms LJ, Azari R, Antonius D, Melnikow J. Comparing the use of physician time and health care resources among patients speaking English, Spanish, and Russian. Med Care. 2000;38(7):728‐738. doi: 10.1097/00005650-200007000-00005 [DOI] [PubMed] [Google Scholar]
- 10. Reznek MA, Mangolds V, Kotkowski KA, Samadian KD, Joseph J, Larkin C. Accuracy of physician self‐estimation of time spent during patient care in the emergency department. J Am Coll Emerg Physicians Open. 2023;4(2):e12923. doi: 10.1002/emp2.12923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Centers for Medicare & Medicaid Services. RVU21A . 2024. https://www.cms.gov/medicaremedicare‐fee‐service‐paymentphysicianfeeschedpfs‐relative‐value‐files/rvu21a
- 12. Chmielewski N, Moretz J. ESI triage distribution in U.S. emergency departments. Adv Emerg Nurs J. 2022;44(1):46‐53. doi: 10.1097/TME.0000000000000390 [DOI] [PubMed] [Google Scholar]
- 13. Centers for Disease Control and Prevention. Visits to physician offices and hospital emergency departments, by age sex, and race: United States selected years 2000–2018. 2024. https://www.cdc.gov/nchs/data/hus/2020‐2021/HCareVis.pdf
- 14. American Medical Association. The physician work component . 2024. https://www.ama‐assn.org/system/files/physician‐work‐component.pdf [Google Scholar]
- 15. Centers for Medicare and Medicaid Services. CMS framework for health equity 2022–2032 . 2024. https://www.cms.gov/files/document/cms‐framework‐health‐equity.pdf
- 16. Centers for Disease Control and Prevention. National Center for Health Statistics—ICD‐10‐CM. 2023. https://icd10cmtool.cdc.gov/?fy=FY2023 [PubMed]
- 17.Centers for Medicare and Medicaid Services. Using Z codes: The social determinants of health (SDOH) data journey to better outcomes. 2022. Accessed April 27, 2024. https://www.cms.gov/files/document/zcodes‐infographic.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Deidentified partial datasets may be available upon publication of the manuscript and approval of the study site IRB following request to Dr. Reznek from investigators who provide an IRB letter of approval.


