Abstract
Purpose
To characterize the epidemiology, mechanism (contact vs noncontact), management, and return-to-play (RTP) times for quarterbacks in the National Football League (NFL) who experienced ulnar collateral ligament (UCL) injuries.
Methods
Using the Pro Sports Transactions Archive, NFL quarterbacks who sustained UCL injuries between 1991 and 2023 were identified. Age at time of injury, mechanism of injury (contact vs noncontact), management strategy, and RTP time were recorded. In addition, player performance metrics including games played, quarterback rating, completion percentage, touchdowns, and interceptions were examined for the season before injury through the second season after injury. Player performance analysis was assessed using principal component analysis, which is a dimensionality reduction statistical method that compresses the several performance metrics into a single value, the first principal component.
Results
A total of 21 injuries in 20 players were identified. The mean age of quarterbacks at time of injury was 28.7 years (± 4.6 years standard deviation). Ten injuries occurred during contact with another player, and 11 injuries were noncontact. Most (n = 13) of UCL injuries were managed nonoperatively. Sixteen players achieved RTP, 4 of whom underwent repair or reconstruction (UCLR). Overall, the mean RTP time was 165.6 days (± 178.8 days standard deviation), but players who underwent UCLR had a longer average RTP time (359.0 days vs 98.25 days, P = .014). Injuries sustained after 2006 were associated with improved postinjury performance (P = .041), but older age at time of injury was associated with diminished postinjury performance (P = .048).
Conclusions
NFL quarterbacks sustain more noncontact UCL injuries and are undergoing UCLR at greater rates than previously reported. Although RTP rates are high and players demonstrate improved postinjury performance for injuries sustained after 2006, older age at the time of injury is associated with worse postinjury performance.
Level of Evidence
Level IV, therapeutic case series.
Injury to the ulnar collateral ligament (UCL) of the elbow is a well-documented cause of medial elbow pain and disability in overhead-throwing athletes with a predilection toward baseball pitchers.1, 2, 3, 4 The typical mechanism of UCL injury in overhead-throwing athletes is repetitive strain causing microtrauma to ligamentous fibers. Patients present with diminished throwing performance (accuracy, velocity, stamina, strength) secondary to posteromedial elbow pain and instability.5,6 Alternatively, traumatic rupture often is associated with acute pain and inability to throw, with or without an audible “pop.”6 However, American football poses a unique risk profile for UCL injury, given the combination of repetitive overhead throwing in addition to traumatic contact secondary to tackling, thus increasing the risk of acute injury, albeit via a different mechanism. Dodson et al.7 reported that 70% of UCL injuries in a subset of professional football quarterbacks were traumatic in nature. In addition, analysis of the National Collegiate Athletic Association across 25 varsity sports identified 3 times more elbow UCL injuries in contact athletes compared with strictly throwing athletes.8 Taken together, the intersection of repetitive overhead throwing and traumatic contact in American football quarterbacks presents an important and underexplored topic that warrants further investigation to enhance our understanding of UCL injuries and their management.
Although UCL injuries can be treated conservatively in most low-demand patients and recreational athletes, ulnar collateral ligament repair or reconstruction (UCLR)—colloquially known as “Tommy John surgery”—has been shown to successfully restore functionality, allowing high-level athletes to return to play (RTP).9,10 Interestingly, the rate of UCL injury as well as subsequent operative treatment is increasing, with epidemiologic literature estimating the rate of reconstruction in New York state alone grew by 343% between 2003 and 2014, projecting continued rapid growth through 2025.1,11,12 Currently, there is a paucity of literature discussing UCL injury in quarterbacks in the National Football League (NFL). Although existing studies capture a historical subset of this population, the modernization of biologic augmentation techniques such as platelet-rich plasma (PRP) injections and UCLR technique warrant a more contemporary review of injury pattern and management strategies.7,13, 14, 15, 16, 17, 18 The purpose of this study was to characterize the epidemiology, mechanism (contact vs noncontact), management, and RTP times for NFL quarterbacks who experienced UCL injuries. The hypotheses for this study are that quarterbacks with UCL injuries would have similar performance metrics after injury, injuries would be mostly traumatic in nature, and they would be managed nonoperatively with shorter RTP times compared with those managed operatively.
Methods
Data Collection
UCL injuries in NFL quarterbacks were identified from the Pro Sports Transactions Archive, which has been used in previous epidemiologic studies in professional sports.19, 20, 21, 22, 23 Extracted injuries were those that occurred between January 1, 1991, and February 1, 2023, a span of 29 full seasons and approximately 1 month of a 30th season. Using RStudio 2023.03.2 (RStudio, Boston, MA), player injury data were extracted, including player name, player team, date of injury, notes on injury reserve status, and injured body part. Player injury data were then further filtered for those specifically marked as elbow injuries and in quarterbacks only. Of these results, the authors manually checked each case to ensure it involved an injury to the UCL of the throwing arm. Players sustaining nonthrowing UCL injuries were excluded from the analysis. Players identified were then cross referenced and verified using team press releases in conjunction with media reports from sources affiliated with the Associated Press and game logs from https://www.pro-football-reference.com/, which provides data from the official statistics partner of the NBA, Sportradar US (Sportradar AG). Confirmed injuries were then cross referenced with reported injuries from a previous publication on this topic by Dodson et al.7 in 2010. Information including contact versus no-contact injury, postinjury time to RTP (in days), and whether the player underwent surgery were collected. Time to RTP was defined as return to active roster or full participation in team activities during preseason practices and was again verified by using team press releases, NFL.com, Associated Press affiliated media reports, and NFL-reference.com, when appropriate. In addition, pre- and postinjury performance data from Pro Football Reference were collected for each quarterback along with player physical traits, including height, weight, body mass index, and age at injury. Each player was assigned a numerical value (e.g., Player 1) for deidentification.
Statistical Analysis
Power analysis was conducted on the basis of time to RTP. Effect size was determined on the basis of historical data from Dodson et al.7 as well as relied on the assumption of equal standard deviation (SD) between players treated operatively and nonoperatively. Because of the limited data available regarding player performance and UCL injury, power analysis could not be calculated for other metrics, and power analysis for time to RTP was applied to these other metrics. Power analysis revealed that at least 18 injuries were needed to achieve a power greater than 0.9 at an effect size of 0.82 for changes in RTP, where we should be able to detect a mean difference of 0.82 of 1 SD between players of operative versus nonoperative treatments. Descriptive statistics including average time from injury to RTP as well as percent of contact versus noncontact injuries were calculated. Player performance analysis was assessed using principal component analysis (PCA), which is a dimensionality reduction statistical method that compresses the several performance metrics into a single value, the first principal component (PC1).24 Multiple orthopaedic studies have used PCA as a method to compare groups across multiple metrics, including studies investigating sports performance.24, 25, 26, 27, 28, 29, 30, 31 Analysis included the following statistics obtained from Pro Football Reference, for the season before injury and through 2 seasons after injury: games played, quarterback rating (QBR), completion percentage, number of touchdowns, and number of interceptions.32 QBR is a widely used calculation that incorporates 5 variables: pass attempts, completions, passing yards, touchdown passes, and interceptions.32 The change in each of the aforementioned performance metric was measured as the statistic 1 season after injury normalized to performance 1 season before injury. Overall performance via PC1 was first compared for players who underwent UCLR versus those who underwent nonoperative management. The PC1 was then compared between players injured before 2005 versus 2006 onwards (independent t test, alpha = 0.05). In addition, the PC1 was compared between players injured before 2005 versus 2006 onwards on the basis of operative versus nonoperative management (independent t test, alpha = 0.05).
Next, the relationship between age at the time of injury and change in player overall performance was analyzed. Overall performance was again measured using the PC1 from the PCA. The correlation between age at time of injury and PC1 was calculated (Pearson correlation coefficient, alpha = 0.05). Finally, the distribution of contact versus noncontact injury among older versus younger players was analyzed using the Fisher exact test. The mean age of injury from the sample population was used as a threshold to categorize players as older or younger.
Statistical significance for all comparative analyses was set a priori at alpha = 0.05. All statistics and data visualizations were conducted using Python 3.7 (Python Software Foundation, Wilmington, DE).
Results
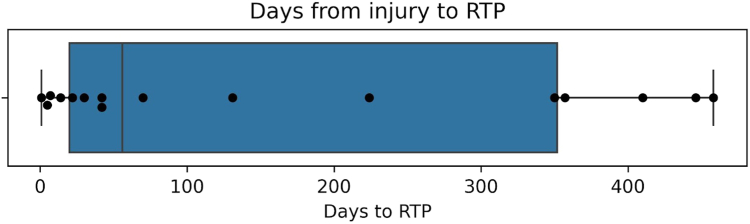
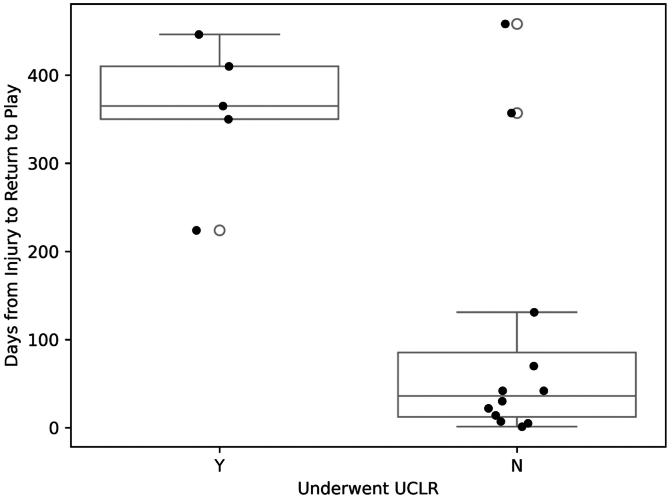
We identified 21 UCL injuries in 20 NFL quarterbacks from 1991 to 2023, and the characteristics of each player and injury are described in Table 1. One player suffered a UCL injury twice, and thus the separate injuries were categorized as Player 17a and Player 17b. The average age of quarterbacks at the time of injury was 28.5 years (± 1.73 years SD). Ten injuries occurred during contact with another player and 11 injuries were noncontact. Eight players underwent UCLR. Sixteen players returned to play at least 1 more season in the NFL after their injury. Of the 16 players, 9 continued to play at least 2 more seasons in the NFL after injury and 2 players are currently playing in their first season after their injury. Overall, the mean time from injury to RTP was 163.1 days (± 178.6 days SD) (Fig 1). There was a significant difference in RTP for players on the basis of management strategy, with UCLR averaging 359 days and nonoperative management averaging 98.25 days (P = .014) (Fig 2).
Table 1.
Player Demographics, Injury Characteristics, Treatment Plan, and Time for RTP, in Days
| Player | Age at Time of Injury | Year | Mechanism | Treatment | Days to RTP |
|---|---|---|---|---|---|
| 1 | 35 | 1991 | Noncontact | UCLR | 446 |
| 2 | 25 | 1994 | Contact | Non-op | 5 |
| 3 | 29 | 1998 | Noncontact | UCLR | N/A |
| 4 | 28 | 2001 | Noncontact | Non-op | 30 |
| 5 | 36 | 2001 | Noncontact | UCLR | 410 |
| 6 | 30 | 2003 | Noncontact | UCLR | N/A |
| 7 | 33 | 2004 | Contact | Non-op | 42 |
| 8 | 29 | 2004 | Contact | Non-op | 14 |
| 9 | 24 | 2005 | Noncontact | Non-op | 22 |
| 10 | 32 | 2007 | Noncontact | UCLR | 350 |
| 11 | 28 | 2008 | Contact | Non-op | 357 |
| 12 | 33 | 2008 | Contact | Non-op | 70 |
| 13 | 38 | 2008 | Contact | Non-op | 1 |
| 14 | 29 | 2008 | Contact | Non-op | 131 |
| 15 | 26 | 2013 | Noncontact | UCLR | N/A |
| 16 | 25 | 2016 | Noncontact | UCLR | N/A |
| 17a | 22 | 2018 | Noncontact | Non-op | 42 |
| 18 | 25 | 2019 | Noncontact | Non-op | 458 |
| 19 | 25 | 2020 | Contact | Non-op | 365 |
| 17b | 26 | 2022 | Contact | Non-op | 7 |
| 20 | 23 | 2023 | Contact | UCLR | 224 |
N/A, player did not play in an NFL game after injury; Non-op, nonoperative management; RTP, return to play; UCLR, ulnar collateral ligament reconstruction or repair.
Fig 1.
Boxplot visualizing the number of days between a player’s injury and RTP. Players who did not return to play were excluded from the plot. The 25th percentile is 20.0 days, the median is 56.0 days, and the 75th percentile is 357.0 days. The mean RTP is 163.1 days. (RTP, return to play.)
Fig 2.
Comparing mean time from injury to RTP among players who underwent UCLR versus those who did not (nonparametric t test, P = .014). Mean RTP for players who underwent UCLR was 359.0 days. Mean RTP for players who underwent nonoperative management was 98.25 days. (RTP, return to play; UCLR, ulnar collateral ligament reconstruction or repair.)
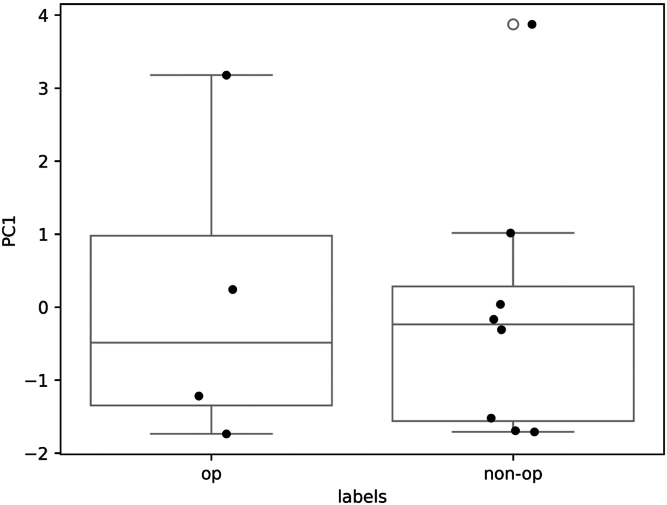
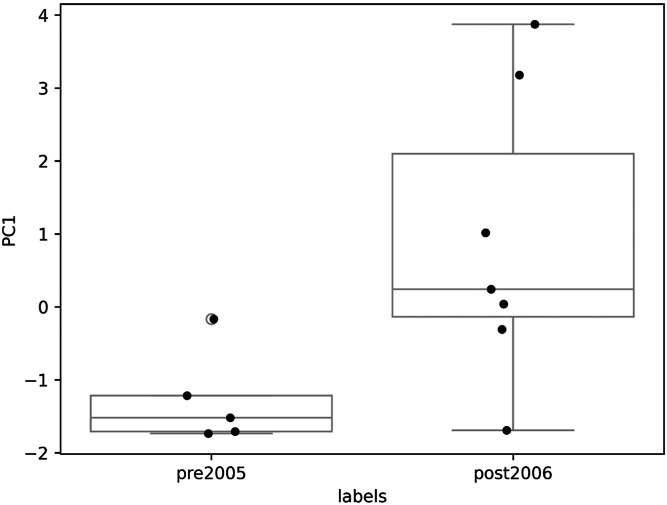
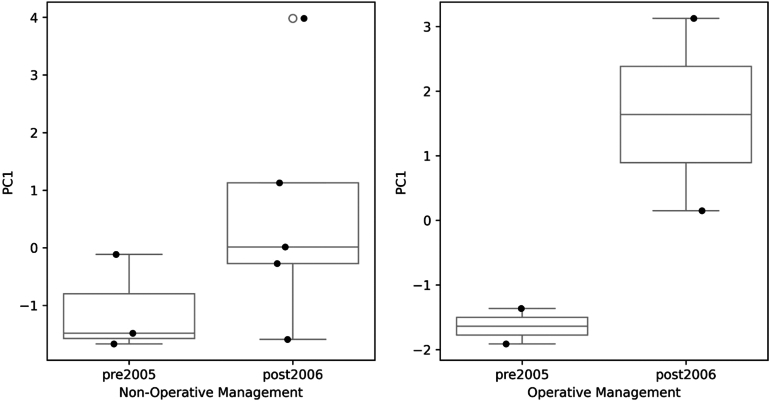
Of the players who returned to play at least 1 more season, 4 underwent UCLR and 12 underwent nonoperative management. There was no significant difference in change in performance between players who underwent UCLR and those who did not (independent t test, P = .888 (Fig 3). The performance of players injured before 2005 versus 2006 and onwards was compared using PCA in Figure 4. Players who were injured 2006 onwards showed a statistically significant improvement in performance compared with players injured before 2005 (independent t test, P = .041). The subset analysis was conducted on the basis of management type in Figure 5. For the players who underwent UCLR, 2 players were injured 2005 and before, and 2 players were injured 2006 and onward. Of the players who underwent UCLR, those injured 2006 and onward demonstrated a nonsignificant improvement in performance compared with those injured 2005 and before (independent t test, P = .16). For the players who underwent nonoperative management, 3 players were injured 2005 and before, and 2 players were injured 2006 and onward. This analysis was similar in that players injured 2006 and onward showed a nonsignificant improvement in performance (independent t test, P = .2).
Fig 3.
Comparison of mean PC1 of players who underwent UCLR and those who did not. Principal component analysis was used to analyze the change in performance 1 season before injury with 1 season after injury of the following: number of games played, number of touchdowns, number of interceptions, QBR, completion percentage, and number of passing yards. A greater PC1 indicates an improved performance compared with the season before injury; a lesser PC1 indicates a worse performance. An independent t test was used to compare the PC1 (P = .888). (PC1, first principal component; QBR, quarterback rating; UCLR, ulnar collateral ligament reconstruction or repair.)
Fig 4.
Comparison of mean PC1 of players injured before 2005 versus 2006 onwards. Principal component analysis was used to analyze the change in performance 1 season before injury with 1 season after injury of the following: number of games played, number of touchdowns, number of interceptions, QBR, completion percentage, and number of passing yards. The PC1 is a statistical representation of all 6 performance metrics. A greater PC1 indicates an improved performance compared with the season before injury; a lesser PC1 indicates a worse performance. An independent t test was used to compare the PC1 (P = .04). (PC1, first principal component; QBR, quarterback rating; UCLR, ulnar collateral ligament reconstruction or repair.)
Fig 5.
Analyzing the performance of players, subdivided by management, comparing mean PC1 of those who were injured before 2005 versus 2006 and onward. Principal component analysis was used to analyze the change in performance 1 season before injury with 1 season after injury of the following: number of games played, number of touchdowns, number of interceptions, QBR, completion percentage, and number of passing yards. A greater PC1 indicates an improved performance compared to the season before injury; a lesser PC1 indicates a worse performance. An independent t test was used to compare the PC1 (nonoperative: P = .2, UCLR: P = .16). (PC1, first principal component; QBR, quarterback rating; UCLR, ulnar collateral ligament reconstruction or repair.)
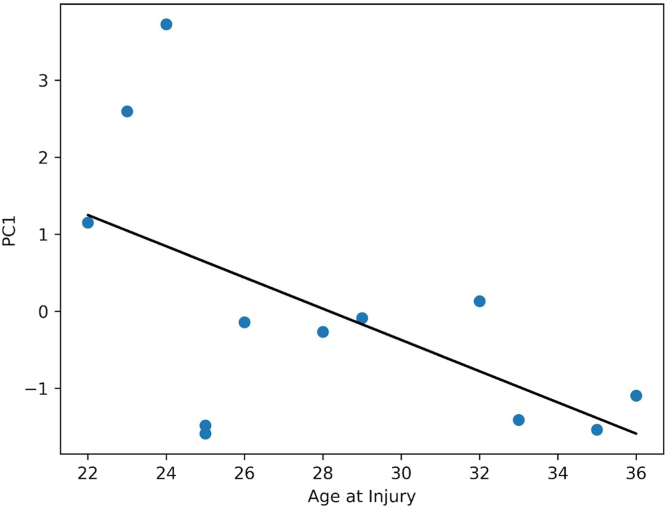
The distribution of quarterbacks who sustained contact versus noncontact injuries and age was analyzed. Players were categorized according to the mean age (28.7 years old) of the study. Ten players were 29 years or older and 11 players were younger than 29. Of the players who were above the mean age, 5 sustained contact injuries and 5 sustained noncontact injuries. Of the players who were below the mean age, 5 sustained contact injuries and 6 sustained noncontact injuries. The Fisher exact test revealed no significant difference in the number of contact versus noncontact injuries in the older and younger groups (P = 1.0). The relationship between age at the time of injury and change in overall performance 1 season after injury versus 1 season before injury is calculated in Figure 6. Overall performance was represented by the PC1, which demonstrated a significant negative correlation with age (P = .048).
Fig 6.
Assessing the relationship between age at time of injury and the change in player performance before and after injury. Principal component analysis was used to analyze the change in performance 1 season before injury with 1 season after injury of the following: number of games played, number of touchdowns, number of interceptions, QBR, completion percentage, and number of passing yards. Change in performance metric was determined by normalizing the metric from the first season after injury to that from the season before injury (P = .048) (QBR, quarterback rating.)
Discussion
The results of the current study identified 21 UCL injuries in 20 NFL quarterbacks from 1991 to 2023 and demonstrated overall high RTP rates, improved postinjury performance with injuries sustained after 2006, and inferior postinjury performance with older age at the time of injury. Although 16 players RTP with a mean time of 163.1 days, only 9 were able to play for at least 2 seasons after their injury. Injuries were roughly divided equally between both contact (n = 10) and noncontact mechanisms (n = 11), and 62% of injuries were managed nonoperatively. There was no difference in performance on the basis of management strategy (P = .888), but players injured from 2006 and beyond demonstrated superior postinjury performance (P = .041). Although not statistically significant, subgroup analysis demonstrated a trend toward improved postinjury performance for both nonoperative (P = .2) and UCLR (P = .16) for injuries sustained after 2006. Finally, increasing age at the time of injury was associated with worse postinjury performance (P = .048)
Although injuries to the UCL are more commonly described in baseball pitchers, the 4-phase American football throw is significantly different from the baseball pitch, with characteristics such as a heavier ball and slower rotational velocity, potentially reducing chronic injury rates.33,34 Although NFL quarterbacks face fewer repetitive stresses than baseball pitchers, they are more prone to contact-related injuries. A study by Dodson et al.7 covering UCL injuries in NFL quarterbacks from 1994 to 2008 found that 70% of these injuries were contact-related and nearly all (9/10) were managed nonoperatively. On the contrary, the current study’s findings show an equal distribution of contact and noncontact UCL injuries in NFL quarterbacks, suggesting that there may be a more notable effect of repetitive throwing motions than previously believed.35 In addition, the lack of correlation between player age and injury mechanism challenges the belief that overuse injuries primarily affect older quarterbacks. Although age did not correlate with the mechanism of injury, there was a negative correlation between age at time of injury and postinjury performance (P = .48). This association between age and postinjury performance may prompt a more conservative approach to RTP protocols for older NFL quarterbacks to safeguard their long-term performance. These results reshape our understanding of the causes of UCL injury among NFL quarterbacks and underscore the implications of age at injury on performance and management strategies.
When considering RTP after UCL injury, among the 16 players who returned to play, 12 players returned for at least 1 more season, whereas 9 played 2 or more postinjury seasons. A significant postinjury performance improvement was noted in post-2006 injuries compared with those sustained in years previously, regardless of management strategy (P = .04). This period represents a time of expanding interest in biologic therapies in sports medicine, in addition to crucial modifications to the UCLR techniques, as well as improved rehabilitation protocols.5,9,10,36, 37, 38, 39, 40, 41, 42, 43, 44, 45 As such, although it is possible that our results are confounded by heterogeneity of injury severity, they also may reflect the efficacy of post-2006 advances in the treatment of UCL injuries. For example, although elite throwing athletes with incomplete UCL injuries have demonstrated RTP rates of 54% to 85% at 6 to 21 weeks after targeted rehabilitation programs,2,16 multiple relatively recent investigations exploring the role of PRP therapy as an adjunct to this protocol have also demonstrated high RTP rates in throwing athletes.16, 17, 18,46,47 A 2024 systematic review and meta-analysis of 8 studies and 322 baseball players by Fucaloro et al.48 demonstrated high RTS rates when players had rehabilitation programs lasting at least 12 weeks (RTP = 87%-100%) and leukocyte-poor PRP preparations (73%-100%). Although all players in the current study who elected to pursue nonoperative management were able to RTP, the post-2006 improvements in postinjury performance may represent advances in our understanding of the surgical and nonsurgical management of UCL pathology over the past several decades.
The results of the current study show that greater than 36% of injuries underwent UCLR with a mean RTP of 359 days. Currently, the modified Jobe and Docking techniques are the most commonly used UCLR techniques and have similar RTP rates, ranging from 79.9% to 97% at approximately 12 to 18 months.2,3,14,15 Dodson et al.’s7 original cohort of NFL quarterbacks with complete tears (3/10) were all managed nonoperatively with a mean RTP of 67.3 days. Although these results suggest an expeditious RTP, interpretation of these findings is limited by the absence of any postinjury performance evaluation. Although not statistically significant, the results of the subgroup analysis demonstrate a trend toward improved postinjury performance for both the nonoperative (P = .2) and UCLR (P = 016) groups. Even though these results are limited by the small number of players in each group, this trend may again be reflective of the technical improvements in UCLR procedures that have occurred over the past 2 decades. Given the results of the current study in the context of the established literature, NFL quarterbacks appear to be undergoing UCLR at a rate greater than previously established.
Although RTP rates are important, no analysis on elite athletic injuries is complete without an assessment of athletic performance after RTP. The current study provides a nuanced understanding of the injury's implications on quarterback performance, highlighting that although historically many players successfully RTP, their postinjury performance levels are affected by age at the time of injury and year of injury. These findings suggest that RTP, although an important milestone, does not fully encapsulate the injury's long-term effect on an athlete's career. Our findings indicate that the quality of performance postinjury, particularly in a high-impact sport like professional football, may be more difficult to predict than previously thought. Such insights are crucial not only for clinicians and athletic trainers but also for players and team management in strategizing long-term player development and team composition in the wake of such injuries.
Limitations
Several limitations must be acknowledged. The retrospective nature of the study and reliance on publicly available data sources inherently limits the depth of injury specifics and treatment details we could access. This reliance on secondary data sources may lead to underreporting of injuries or incomplete data regarding the full spectrum of treatment modalities employed, particularly for grading of injury severity, duration of rehabilitation, use of biological augments such as PRP, and surgical techniques. Second, our analysis was confined to NFL quarterbacks, a highly specialized and elite athlete population. Therefore, the findings may not be generalizable to other athlete populations, including quarterbacks at different levels of play or athletes in other sports where throwing mechanics and injury risks differ. As a byproduct of this highly specialized group, the small sample size limits the statistical power for some of the analyses and may contribute to variability in the results as this increases the probability of encountering type II error. Furthermore, our analysis of player performance postinjury, although rigorous, did not account for all possible confounding factors, such as changes in team dynamics, coaching strategies, or personal factors affecting the athletes’ performance.
Conclusions
NFL quarterbacks sustain more noncontact UCL injuries and are undergoing UCLR at greater rates than previously reported. Although RTP rates are high and players demonstrate improved postinjury performance for injuries sustained after 2006, older age at the time of injury was associated with worse postinjury performance.
Disclosures
The authors report no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Petty D.H., Andrews J.R., Fleisig G.S., Cain E.L. Ulnar collateral ligament reconstruction in high school baseball players: Clinical results and injury risk factors. Am J Sports Med. 2004;32:1158–1164. doi: 10.1177/0363546503262166. [DOI] [PubMed] [Google Scholar]
- 2.Ford G.M., Genuario J., Kinkartz J., Githens T., Noonan T. Return-to-play outcomes in professional baseball players after medial ulnar collateral ligament injuries: Comparison of operative versus nonoperative treatment based on magnetic resonance imaging findings. Am J Sports Med. 2016;44:723–728. doi: 10.1177/0363546515621756. [DOI] [PubMed] [Google Scholar]
- 3.Thomas S.J., Paul R.W., Rosen A.B., et al. Return-to-play and competitive outcomes after ulnar collateral ligament reconstruction among baseball players: A systematic review. Orthop J Sports Med. 2020;8 doi: 10.1177/2325967120966310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walker C.M., Genuario J.W., Houck D.A., Murayama S., Mendez H., Noonan T.J. Return-to-play outcomes in professional baseball players after nonoperative treatment of incomplete medial ulnar collateral ligament injuries: A long-term follow-up study. Am J Sports Med. 2021;49:1137–1144. doi: 10.1177/0363546521996706. [DOI] [PubMed] [Google Scholar]
- 5.Chen F.S., Rokito A.S., Jobe F.W. Medial elbow problems in the overhead-throwing athlete. J Am Acad Orthop Surg. 2001;9:99. doi: 10.5435/00124635-200103000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Cain E.L., Dugas J.R., Wolf R.S., Andrews J.R. Elbow injuries in throwing athletes: A current concepts review. Am J Sports Med. 2003;31:621–635. doi: 10.1177/03635465030310042601. [DOI] [PubMed] [Google Scholar]
- 7.Dodson C.C., Slenker N., Cohen S.B., Ciccotti M.G., DeLuca P. Ulnar collateral ligament injuries of the elbow in professional football quarterbacks. J Shoulder Elbow Surg. 2010;19:1276–1280. doi: 10.1016/j.jse.2010.05.028. [DOI] [PubMed] [Google Scholar]
- 8.Li N.Y., Goodman A.D., Lemme N.J., Owens B.D. Epidemiology of elbow ulnar collateral ligament injuries in throwing versus contact athletes of the National Collegiate Athletic Association: Analysis of the 2009-2010 to 2013-2014 seasons. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967119836428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vitale M.A., Ahmad C.S. The outcome of elbow ulnar collateral ligament reconstruction in overhead athletes: A systematic review. Am J Sports Med. 2008;36:1193–1205. doi: 10.1177/0363546508319053. [DOI] [PubMed] [Google Scholar]
- 10.Langer P., Fadale P., Hulstyn M. Evolution of the treatment options of ulnar collateral ligament injuries of the elbow. Br J Sports Med. 2006;40:499–506. doi: 10.1136/bjsm.2005.025072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hodgins J.L., Vitale M., Arons R.R., Ahmad C.S. Epidemiology of medial ulnar collateral ligament reconstruction: A 10-year study in New York State. Am J Sports Med. 2016;44:729–734. doi: 10.1177/0363546515622407. [DOI] [PubMed] [Google Scholar]
- 12.Mahure S.A., Mollon B., Shamah S.D., Kwon Y.W., Rokito A.S. Disproportionate trends in ulnar collateral ligament reconstruction: Projections through 2025 and a literature review. J Shoulder Elbow Surg. 2016;25:1005–1012. doi: 10.1016/j.jse.2016.02.036. [DOI] [PubMed] [Google Scholar]
- 13.Kenter K., Behr C.T., Warren R.F., O’Brien S.J., Barnes R. Acute elbow injuries in the National Football League. J Shoulder Elbow Surg. 2000;9:1–5. doi: 10.1016/s1058-2746(00)80023-3. [DOI] [PubMed] [Google Scholar]
- 14.Arner J.W., Chang E.S., Bayer S., Bradley J.P. Direct comparison of modified Jobe and docking ulnar collateral ligament reconstruction at midterm follow-up. Am J Sports Med. 2019;47:144–150. doi: 10.1177/0363546518812421. [DOI] [PubMed] [Google Scholar]
- 15.Yoshida M., Takenaga T., Takeuchi S., et al. Ulnar collateral ligament reconstruction with the modified Jobe technique in baseball pitchers. Orthop J Sports Med. 2021;9 doi: 10.1177/2325967121998339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chauhan A., McQueen P., Chalmers P.N., et al. Nonoperative treatment of elbow ulnar collateral ligament injuries with and without platelet-rich plasma in professional baseball players: A comparative and matched cohort analysis. Am J Sports Med. 2019;47:3107–3119. doi: 10.1177/0363546519876305. [DOI] [PubMed] [Google Scholar]
- 17.Deal J.B., Smith E., Heard W., O’Brien M.J., Savoie F.H. Platelet-rich plasma for primary treatment of partial ulnar collateral ligament tears: MRI correlation with results. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117738238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dines J.S., Williams P.N., ElAttrache N., et al. Platelet-rich plasma can be used to successfully treat elbow ulnar collateral ligament insufficiency in high-level throwers. Am J Orthop (Belle Mead NJ) 2016;45:296–300. [PubMed] [Google Scholar]
- 19.Pro Sports Transactions Archive. https://www.prosportstransactions.com/
- 20.Morikawa L.H., Tummala S.V., Brinkman J.C., Buckner Petty S.A., Chhabra A. Effect of a condensed NBA season on injury risk: An analysis of the 2020 season and player safety. Orthop J Sports Med. 2022;10 doi: 10.1177/23259671221121116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin E., Tummala S.V., Morikawa L., et al. Strains/sprains and fractures are the most common hand and wrist injuries in National Basketball Association athletes who return to preinjury player efficiency and equal or greater true shooting percentage within two years of injury. Arthrosc Sports Med Rehabil. 2023;5 doi: 10.1016/j.asmr.2023.100829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bullock G.S., Ferguson T., Arundale A.H., Martin C.L., Collins G.S., Kluzek S. Return to performance following severe ankle, knee, and hip injuries in National Basketball Association players. PNAS Nexus. 2022;1 doi: 10.1093/pnasnexus/pgac176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tummala S.V., Morikawa L., Brinkman J.C., et al. Characterization of ankle injuries and associated risk factors in the National Basketball Association: Minutes per game and usage rate associated with time loss. Orthop J Sports Med. 2023;11 doi: 10.1177/23259671231184459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang Z., Castelló A. Principal components analysis in clinical studies. Ann Transl Med. 2017;5:351. doi: 10.21037/atm.2017.07.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McCormack S., Jones B., Scantlebury S., Collins N., Owen C., Till K. Using principal component analysis to compare the physical qualities between academy and international youth rugby league players. Int J Sports Physiol Perform. 2021;16:1880–1887. doi: 10.1123/ijspp.2021-0049. [DOI] [PubMed] [Google Scholar]
- 26.Goreham J.A., Landry S.C., Kozey J.W., Smith B., Ladouceur M. Using principal component analysis to investigate pacing strategies in elite international canoe kayak sprint races. Sports Biomech. 2023;22:1444–1459. doi: 10.1080/14763141.2020.1806348. [DOI] [PubMed] [Google Scholar]
- 27.Foster B.H., Shaw C.B., Boutin R.D., et al. A principal component analysis-based framework for statistical modeling of bone displacement during wrist maneuvers. J Biomech. 2019;85:173–181. doi: 10.1016/j.jbiomech.2019.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Daruwalla Z.J., Courtis P., Fitzpatrick C., Fitzpatrick D., Mullett H. An application of principal component analysis to the clavicle and clavicle fixation devices. J Orthop Surg Res. 2010;5:21. doi: 10.1186/1749-799X-5-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shalhoub S., Cyr A., Maletsky L.P. Correlation between knee anatomy and joint laxity using principal component analysis. J Orthop Res. 2022;40:2502–2509. doi: 10.1002/jor.25294. [DOI] [PubMed] [Google Scholar]
- 30.Welch N., Richter C., Moran K., Franklyn-Miller A. Principal component analysis of the associations between kinetic variables in cutting and jumping, and cutting performance outcome. J Strength Cond Res. 2021;35:1848–1855. doi: 10.1519/JSC.0000000000003028. [DOI] [PubMed] [Google Scholar]
- 31.Mantovani G., Lamontagne M., Varin D., Cerulli G.G., Beaulé P.E. Comparison of total hip arthroplasty surgical approaches by principal component analysis. J Biomech. 2012;45:2109–2115. doi: 10.1016/j.jbiomech.2012.05.041. [DOI] [PubMed] [Google Scholar]
- 32.Pro-Football-Reference.com.Pro Football Stats, History, Scores, Standings, Playoffs, Schedule & Records. https://www.pro-football-reference.com/
- 33.Fleisig G.S., Escamilla R.F., Andrews J.R., Matsuo T., Satterwhite Y., Barrentine S.W. Kinematic and kinetic comparison between baseball pitching and football passing. J Appl Biomech. 1996;12:207–224. [Google Scholar]
- 34.Kelly B.T., Backus S.I., Warren R.F., Williams R.J. Electromyographic analysis and phase definition of the overhead football throw. Am J Sports Med. 2002;30:837–844. doi: 10.1177/03635465020300061401. [DOI] [PubMed] [Google Scholar]
- 35.Erickson B.J., Hurley E.T., Mojica E.S., Jazrawi L.M., Ulnar Collateral Ligament – Delphi Consensus Group (UCL-DCG) Elbow ulnar collateral ligament tears: A modified consensus statement. Arthroscopy. 2023;39:1161–1171. doi: 10.1016/j.arthro.2022.12.033. [DOI] [PubMed] [Google Scholar]
- 36.Paletta G.A., Wright R.W. The modified docking procedure for elbow ulnar collateral ligament reconstruction: 2-year follow-up in elite throwers. Am J Sports Med. 2006;34:1594–1598. doi: 10.1177/0363546506289884. [DOI] [PubMed] [Google Scholar]
- 37.Murray M.M., Spindler K.P., Abreu E., et al. Collagen-platelet rich plasma hydrogel enhances primary repair of the porcine anterior cruciate ligament. J Orthop Res. 2007;25:81–91. doi: 10.1002/jor.20282. [DOI] [PubMed] [Google Scholar]
- 38.Han J., Meng H.X., Tang J.M., Li S.L., Tang Y., Chen Z.B. The effect of different platelet-rich plasma concentrations on proliferation and differentiation of human periodontal ligament cells in vitro. Cell Prolif. 2007;40:241–252. doi: 10.1111/j.1365-2184.2007.00430.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kawase T., Okuda K., Saito Y., Yoshie H. In vitro evidence that the biological effects of platelet-rich plasma on periodontal ligament cells is not mediated solely by constituent transforming-growth factor-β or platelet-derived growth factor. J Periodontol. 2005;76:760–767. doi: 10.1902/jop.2005.76.5.760. [DOI] [PubMed] [Google Scholar]
- 40.Smith J.J., Ross M.W., Smith R.K.W. Anabolic effects of acellular bone marrow, platelet rich plasma, and serum on equine suspensory ligament fibroblasts in vitro. Vet Comp Orthop Traumatol. 2006;19:43–47. [PubMed] [Google Scholar]
- 41.Dines J.S., ElAttrache N.S., Conway J.E., Smith W., Ahmad C.S. Clinical outcomes of the DANE TJ technique to treat ulnar collateral ligament insufficiency of the elbow. Am J Sports Med. 2007;35:2039–2044. doi: 10.1177/0363546507305802. [DOI] [PubMed] [Google Scholar]
- 42.Dodson C.C., Thomas A., Dines J.S., Nho S.J., Williams R.J., Altchek D.W. Medial ulnar collateral ligament reconstruction of the elbow in throwing athletes. Am J Sports Med. 2006;34:1926–1932. doi: 10.1177/0363546506290988. [DOI] [PubMed] [Google Scholar]
- 43.Hall M.P., Band P.A., Meislin R.J., Jazrawi L.M., Cardone D.A. Platelet-rich plasma: Current concepts and application in sports medicine. J Am Acad Orthop Surg. 2009;17:602–608. doi: 10.5435/00124635-200910000-00002. [DOI] [PubMed] [Google Scholar]
- 44.Virchenko O., Aspenberg P. How can one platelet injection after tendon injury lead to a stronger tendon after 4 weeks? Interplay between early regeneration and mechanical stimulation. Acta Orthop. 2006;77:806–812. doi: 10.1080/17453670610013033. [DOI] [PubMed] [Google Scholar]
- 45.Rohrbough J.T., Altchek D.W., Hyman J., Williams R.J., Botts J.D. Medial collateral ligament reconstruction of the elbow using the docking technique. Am J Sports Med. 2002;30:541–548. doi: 10.1177/03635465020300041401. [DOI] [PubMed] [Google Scholar]
- 46.Podesta L., Crow S.A., Volkmer D., Bert T., Yocum L.A. Treatment of partial ulnar collateral ligament tears in the elbow with platelet-rich plasma. Am J Sports Med. 2013;41:1689–1694. doi: 10.1177/0363546513487979. [DOI] [PubMed] [Google Scholar]
- 47.Conant B.J., German N.A., David S.L. The use of platelet-rich plasma for conservative treatment of partial ulnar collateral ligament tears in overhead athletes: A critically appraised topic. J Sport Rehabil. 2020;29:509–514. doi: 10.1123/jsr.2018-0174. [DOI] [PubMed] [Google Scholar]
- 48.Fucaloro SP, Kang AS, Bragg JT, Krivicich L, Salzler MJ. Return to sport after ulnar collateral ligament tears treated with platelet-rich plasma injections is influenced by length of rehabilitation and leukocyte content of injections: A systematic review [Published online March 18, 2024]. Arthroscopy. https://doi.org/10.1016/j.arthro.2024.03.017. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.