Abstract
Background
The introduction of enteral feeds for very preterm (< 32 weeks) or very low birth weight (< 1500 grams) infants is often delayed due to concern that early introduction may not be tolerated and may increase the risk of necrotising enterocolitis. However, prolonged enteral fasting may diminish the functional adaptation of the immature gastrointestinal tract and extend the need for parenteral nutrition with its attendant infectious and metabolic risks. Trophic feeding, giving infants very small volumes of milk to promote intestinal maturation, may enhance feeding tolerance and decrease the time taken to reach full enteral feeding independently of parenteral nutrition.
Objectives
To determine the effect of early trophic feeding versus enteral fasting on feed tolerance, growth and development, and the incidence of neonatal morbidity (including necrotising enterocolitis and invasive infection) and mortality in very preterm or VLBW infants.
Search methods
We used the standard search strategy of the Cochrane Neonatal Review Group. This included electronic searches of the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2012, Issue 12), MEDLINE, EMBASE and CINAHL (1980 until December 2012), conference proceedings and previous reviews.
Selection criteria
Randomised or quasi‐randomised controlled trials that assessed the effects of early trophic feeding (milk volumes up to 24 ml/kg/day introduced before 96 hours postnatal age and continued until at least one week after birth) versus a comparable period of enteral fasting in very preterm or very low birth weight infants.
Data collection and analysis
We extracted data using the standard methods of the Cochrane Neonatal Review Group with separate evaluation of trial quality and data extraction by two authors and synthesis of data using risk ratio, risk difference and mean difference.
Main results
Nine trials in which a total of 754 very preterm or very low birth weight infants participated were eligible for inclusion. Few participants were extremely preterm (< 28 weeks) or extremely low birth weight (< 1000 grams) or growth restricted. These trials did not provide any evidence that early trophic feeding affected feed tolerance or growth rates. Meta‐analysis did not detect a statistically significant effect on the incidence of necrotising enterocolitis: typical risk ratio 1.07 (95% confidence interval 0.67 to 1.70); risk difference 0.01 (‐0.03 to 0.05).
Authors' conclusions
The available trial data do not provide evidence of important beneficial or harmful effects of early trophic feeding for very preterm or very low birth weight infants. The applicability of these findings to extremely preterm, extremely low birth weight or growth restricted infants is limited. Further randomised controlled trials would be needed to determine how trophic feeding compared with enteral fasting affects important outcomes in this population.
Keywords: Animals; Humans; Infant, Newborn; Adaptation, Physiological; Child Development; Child Development/physiology; Enteral Nutrition; Enteral Nutrition/adverse effects; Enteral Nutrition/methods; Enterocolitis, Necrotizing; Enterocolitis, Necrotizing/prevention & control; Infant Formula; Infant, Premature; Infant, Very Low Birth Weight; Infant, Very Low Birth Weight/growth & development; Infant, Very Low Birth Weight/physiology; Milk; Milk, Human; Parenteral Nutrition; Parenteral Nutrition/adverse effects; Parenteral Nutrition/methods; Randomized Controlled Trials as Topic
Plain language summary
Early trophic feeding versus enteral fasting for very preterm or very low birth weight infants
There is insufficient evidence to determine whether feeding very preterm or very low birth weight infants small quantities of milk during the first week after birth (early trophic feeding) compared with fasting helps bowel development and improves subsequent feeding, growth and development. Analysis of nine trials does not suggest that this practice increases the risk of a severe bowel disorder called 'necrotising enterocolitis'. Further trials could provide more robust evidence to inform this key area of care.
Background
Description of the condition
Necrotising enterocolitis is an important cause of morbidity and mortality in very preterm (< 32 weeks) or very low birth weight (VLBW: < 1500 grams) infants. Extremely low birth weight (ELBW: < 1000 grams) and extremely preterm (< 28 weeks) infants are at highest risk (Rees 2007). Intrauterine growth restriction may be an additional specific risk factor, especially if associated with circulatory redistribution demonstrated by absent or reversed end‐diastolic flow velocities (AREDFV) in antenatal Doppler studies of the fetal aorta or umbilical artery (Bernstein 2000; Dorling 2005).
Most very preterm or VLBW infants who develop necrotising enterocolitis have received enteral milk feeds. Evidence exists that feeding with formula milk rather than breast milk increases the risk (Lucas 1990; Quigley 2007; Meinzen‐Derr 2009). The timing of the introduction of enteral feeding may also be an important modifiable risk factor for the development of necrotising enterocolitis (Henderson 2009). Observational data suggest that feeding strategies that include delaying the introduction of progressive enteral feeds until after five to seven days postnatally reduces the risk of necrotising enterocolitis in very preterm or VLBW infants (Patole 2005). However, enteral fasting during the early neonatal period also has potential disadvantages. Because gastrointestinal hormone secretion and motility are stimulated by enteral milk, delayed enteral feeding could diminish the functional adaptation of the immature gastrointestinal tract (Johnson 1976; Aynsley‐Green 1983; Berseth 1990). Consequent intestinal dysmotility may exacerbate feed intolerance leading to a delay in establishing enteral feeding independently of parenteral nutrition. Enteral fasting might also cause hyperbilirubinaemia by increasing enterohepatic recirculation of bilirubin and delaying hepatic enzyme maturation. Prolonging the duration of use of parenteral nutrition may be associated with infectious and metabolic complications that have adverse consequences for survival, duration of hospital stay, growth and development (Flidel‐Rimon 2004; Flidel‐Rimon 2006).
Description of the intervention
Trophic feeding (also referred to as minimal enteral nutrition, gut priming and hypocaloric feeding) was developed and adopted into clinical practice as an alternative to complete enteral fasting for very preterm or VLBW infants during the early neonatal period (Klingenberg 2012). Early trophic feeding is conventionally defined as giving small volumes of milk (typically 12 to 24 ml/kg/day) intragastrically starting within the first few days after birth, without advancing the feed volumes during the first week postnatally (McClure 2001). The primary aim of trophic feeding is to accelerate gastrointestinal physiological, endocrine and metabolic maturity and so allow infants to transition to full enteral feeding independent of parenteral nutrition more quickly. However, any beneficial effects may be negated if early trophic feeding increases the risk of necrotising enterocolitis in very preterm or VLBW infants.
Why it is important to do this review
This review focuses on the question of whether early trophic feeding compared with a similar period of enteral fasting improves feed tolerance without increasing the risk of necrotising enterocolitis in very preterm or VLBW infants. Other Cochrane reviews address the questions of whether introducing progressive enteral milk feeds (beyond trophic volumes) later or slowing the rate of advancement of feed volumes affects the risk of necrotising enterocolitis, mortality and other morbidities (Morgan 2011a; Morgan 2011b).
Objectives
To determine the effect of early trophic feeding versus enteral fasting on feed tolerance, growth and development, and the incidence of neonatal morbidity (including necrotising enterocolitis and invasive infection) and mortality in very preterm or VLBW infants.
Methods
Criteria for considering studies for this review
Types of studies
Randomised or quasi‐randomised controlled trials including cluster‐randomised trials.
Types of participants
VLBW (< 1500 grams) or very preterm (< 32 weeks) newborn infants.
Types of interventions
Early trophic feeding: enteral feeding with milk volumes up to 24 ml/kg/day (1 ml/kg/hour) beginning within four days after birth and continued for at least five days or until at least one week after birth versus enteral fasting for the same period.
Once progressive enteral feeding has started, infants should have received the same type of milk (breast milk or formula), the same route and mode of feeding (intragastric or transpyloric, bolus gavage or continuous) and the same rate of feed volume advancement in both groups.
Types of outcome measures
Primary outcomes
Feed intolerance: days to establish full enteral feeding independently of parenteral nutrition.
Necrotising enterocolitis confirmed by at least two of the following features:
abdominal radiograph showing pneumatosis intestinalis or gas in the portal venous system or free air in the abdomen;
abdominal distension with abdominal radiograph with gaseous distension or frothy appearance of bowel lumen (or both);
blood in stool;
lethargy, hypotonia or apnoea (or combination of these);
or a diagnosis confirmed at surgery or autopsy (Walsh 1986).
Secondary outcomes
All‐cause mortality prior to hospital discharge.
Growth: (i) Time to regain birth weight and rates of weight gain, linear growth, head growth or skinfold thickness growth up to six months of age corrected for preterm birth; (ii) Long‐term growth: weight, height or head circumference and/or proportion of infants who remain below the 10th percentile for the index population's distribution assessed at intervals from six months of age.
Neurodevelopment: death or severe neurodevelopmental disability defined as any one or combination of the following: non‐ambulant cerebral palsy, developmental delay (developmental quotient less than 70), auditory and visual impairment. Each component will be analysed individually as well as part of the composite outcome.
Incidence of invasive infection as determined by culture of bacteria or fungus from blood, cerebrospinal fluid, urine or from a normally sterile body space.
Duration of phototherapy for hyperbilirubinaemia (days).
Duration of hospital stay (days).
Search methods for identification of studies
We used the standard search strategy of the Cochrane Neonatal Group (http://neonatal.cochrane.org/).
Electronic searches
We searched the Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library 2012, Issue 12), MEDLINE (1980 to December 2012), EMBASE (1980 to December 2012) and CINAHL (1982 to December 2012) using the following text words and MeSH terms: [Infan*, OR Infant/, OR Preterm, OR Prem*, OR Infant premature/, OR Neonat*, OR New ADJ born, OR New?born, Infant newborn/, OR Very Low Birth Weight, OR VLBW, OR Extremely Low Birth Weight, OR ELBW, OR Infant Very Low Birth Weight/ OR Infant Extremely Low Birth Weight/] AND [Breast feeding, OR Breast feeding/, OR human milk, OR human milk/, OR formula, Infant formula/, OR Trophic feeding, OR minimal enteral nutrition, OR MEN, OR minimal enteral feeding, OR MEF, OR gut priming, OR enteral feed*, OR enteral nutrition/].
The search outputs were limited with the relevant search filters for clinical trials. We did not apply any language restriction.
We searched ClinicalTrials.gov and Current Controlled Trials for completed or ongoing trials.
Searching other resources
We examined reference lists in previous reviews and studies.
We examined the references in studies identified as potentially relevant. We also searched the abstracts from the annual meetings of the Pediatric Academic Societies (1993 to 2012), the European Society for Pediatric Research (1995 to 2012), the UK Royal College of Paediatrics and Child Health (2000 to 2012) and the Perinatal Society of Australia and New Zealand (2000 to 2012). We considered trials reported only as abstracts to be eligible if sufficient information was available from the report, or from contact with the authors, to fulfil the inclusion criteria.
Data collection and analysis
We used the standard methods of the Cochrane Neonatal Review Group (http://neonatal.cochrane.org/).
Selection of studies
Two review authors screened the title and abstract of all studies identified by the above search strategy. We reassessed the full text of any potentially eligible reports and excluded those studies that did not meet all of the inclusion criteria. Review authors discussed any disagreements until consensus was achieved.
Data extraction and management
We used a data collection form to extract relevant information from each included study. Two review authors extracted the data separately. We discussed any disagreements with the third author until we reached consensus.
Assessment of risk of bias in included studies
We used the criteria and standard methods of the Cochrane Neonatal Review Group to assess the methodological quality of any included trials. We requested additional information from the trial authors to clarify methodology and results as necessary. We evaluated and reported the following issues in the 'Risk of bias' tables:
-
Sequence generation: We categorised the method used to generate the allocation sequence as:
low risk: any random process e.g. random number table; computer random number generator;
high risk: any non random process e.g. odd or even date of birth; patient case‐record number;
unclear.
-
Allocation concealment: We categorised the method used to conceal the allocation sequence as:
low risk: e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes;
high risk: open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth;
unclear.
-
Blinding: We assessed blinding of participants, clinicians and care givers, and outcome assessors separately for different outcomes and categorised the methods as:
low risk;
high risk;
unclear.
-
Incomplete outcome data: We described the completeness of data including attrition and exclusions from the analysis for each outcome and any reasons for attrition or exclusion where reported. We assessed whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported or supplied by the trial authors, we re‐included missing data in the analyses. We categorised completeness as:
low risk: < 20% missing data;
high risk: > 20% missing data;
unclear.
Measures of treatment effect
We calculated risk ratio (RR) and risk difference (RD) for dichotomous data and mean difference (MD) for continuous data, with respective 95% confidence intervals (CI). We used a fixed‐effect model for meta‐analysis.
Assessment of heterogeneity
We examined the treatment effects of individual trials and heterogeneity between trial results by inspecting the forest plots if more than one trial was included in a meta‐analysis. We calculated the I² statistic for statistical heterogeneity. If substantial (I² > 50%) heterogeneity was detected, we explored the possible causes (for example, differences in study design, participants, interventions or completeness of outcome assessments) in sensitivity analyses.
Subgroup analysis and investigation of heterogeneity
We planned the following subgroup analyses:
trials in which most infants were exclusively formula‐fed;
trials in which most infants were at least partially fed with human milk (maternal or donor);
trials in which most participants were of ELBW (< 1000 grams) or extremely preterm (< 28 weeks);
trials in which participants were infants with intrauterine growth restriction, or infants with absent or reversed end‐diastolic flow velocities detected on antenatal Doppler studies of the fetal aorta or umbilical artery.
Results
Description of studies
We identified 17 articles using the above search strategy.
Included studies
Nine trials fulfilled the inclusion criteria (Dunn 1988; Meetze 1992; Troche 1995; Becerra 1996; Schanler 1999; McClure 2000; Sáenz de Pipaón 2003; van Elburg 2004; Mosqueda 2008; see table 'Characteristics of included studies').
Participants
The included studies were all undertaken since the late 1980s by investigators attached to neonatal units in Europe and North America. Most were small single‐centre studies. 754 infants participated in total (range 29 to 190). Most participants were appropriate‐for‐gestational age VLBW or very preterm infants receiving standard intensive care interventions such as mechanical ventilation and parenteral nutrition. In van Elburg 2004, participants were infants of birth weight less than 2000 grams who were small for gestational age (< 10th percentile for birth weight). We included this study because > 80% of participating infants were VLBW. Most of the other trials specifically excluded infants who were small for gestational age at birth and infants with congenital anomalies, gastrointestinal problems or neurological problems.
Interventions
Trophic feeding was generally started within the first three days after birth and continued for varying durations; either until infants were judged to be clinically stable (for example following endotracheal extubation or removal of umbilical catheters) or for pre‐defined intervals, generally 7 to 10 days after birth. Feeding volumes ranged from about 12 to 24 ml/kg/day. One trial administered milk at a rate of 25 ml/kg/day with no intention to increase this volume for six to eight days (Becerra 1996). Although this rate exceeded our definition of minimal enteral nutrition by 1 ml/kg/day, we made a consensus decision to include the trial.
In most trials, infants received either expressed breast milk or formula milk (diluted or full‐strength) or a mixture of breast milk and formula. In two trials, infants received only formula milk (Dunn 1988; Meetze 1992). Control infants received no enteral nutrition for at least one week after birth. Infants in both comparison groups received standard parenteral nutrition during the trial period.
In most trials, milk was administered by intermittent bolus gavage feeds via oro or nasogastric tube. In Schanler 1999, participating infants were also allocated to either bolus or continuous feeding using a factorial design. In Troche 1995, infants weighing < 800 grams at birth received feeds via a continuous infusion whereas those weighing > 800 grams at birth received intermittent bolus feeds.
Outcomes
Most trials assessed feed intolerance (variously defined) and incidence of necrotising enterocolitis. Short‐term growth parameters were reported in a variety of ways, most commonly time to regain birth weight and weight gain during the neonatal period (either as median and range or as mean and standard deviation). Most reports also gave information on adverse outcomes including mortality. None of the trials reported long‐term growth and neurodevelopmental outcomes for surviving infants.
Excluded studies
We excluded eight studies (LaGamma 1985; Ostertag 1986; Slagle 1988; Berseth 1992; Berseth 1993; Berseth 2003; Weiler 2006; Said 2008; see table 'Characteristics of excluded studies').
Risk of bias in included studies
Most of the trials had some methodological weaknesses. In four trials it was unclear whether allocation was concealed. Care givers were not blinded to treatment group in any trial. Few trials undertook blinded assessments for any of the outcomes, and several of the trials did not include results for all infants randomised (see table 'Characteristics of included studies').
Effects of interventions
Primary outcomes
Feed intolerance: time to establish full enteral feeding (outcome 1.1; eight trials)
Meta‐analysis of data from six trials that reported mean and standard deviation (SD) did not detect a statistically significant effect: mean difference (MD) ‐1.05 (95% confidence interval (CI) ‐2.61 to 0.51) days. The meta‐analysis contained significant statistical heterogeneity in (I² = 73%) (Analysis 1.1).
1.1. Analysis.
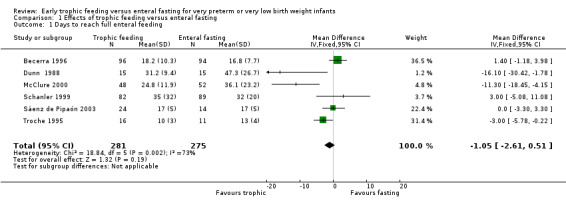
Comparison 1 Effects of trophic feeding versus enteral fasting, Outcome 1 Days to reach full enteral feeding.
Two trials reported median and range data. Neither detected a statistically significant difference: 32 days versus 32 days (Mosqueda 2008); 13 days versus 13 days (van Elburg 2004).
Necrotising enterocolitis (outcome 1.2; nine trials)
Meta‐analysis did not detect a statistically significant effect: typical risk ratio (RR) 1.07 (95% CI 0.67 to 1.70); typical risk difference (RD) 0.01 (95% CI ‐0.03 to 0.05). There was no evidence of heterogeneity (I² = 0%) (Analysis 1.2).
1.2. Analysis.
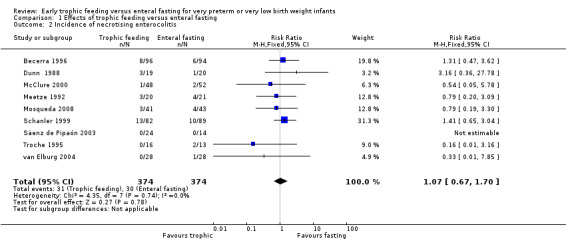
Comparison 1 Effects of trophic feeding versus enteral fasting, Outcome 2 Incidence of necrotising enterocolitis.
Secondary outcomes
Mortality (outcome 1.3; eight trials)
Meta‐analysis did not detect a statistically significant effect: typical RR 0.66 (95% CI 0.41 to 1.07); typical RD ‐0.04 (95% CI ‐0.10 to 0.01). There was no evidence of heterogeneity (I² = 0%) (Analysis 1.3).
1.3. Analysis.
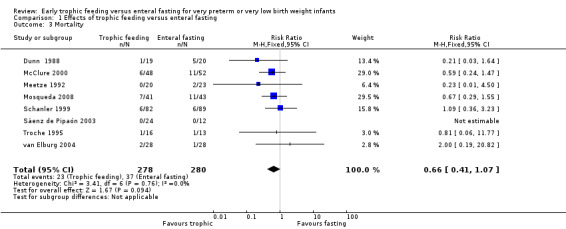
Comparison 1 Effects of trophic feeding versus enteral fasting, Outcome 3 Mortality.
Growth (outcome 1.4; eight trials)
None of the trials reported a statistically significant difference in the time to regain birth weight. Meta‐analysis of five trials with data as mean and SD: MD ‐0.01 (95% CI ‐0.96 to 0.95) days. There was no evidence of statistical heterogeneity (I² = 23%) (Analysis 1.4).
1.4. Analysis.
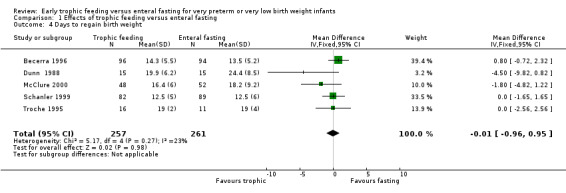
Comparison 1 Effects of trophic feeding versus enteral fasting, Outcome 4 Days to regain birth weight.
Two trials reported median and range data. Neither detected a statistically significant difference: 13 days versus 12 days (Mosqueda 2008); 11 days versus 10 days (van Elburg 2004).
McClure 2000 reported that the average rate of weight gain and head circumference gain during the six weeks after birth was borderline significantly higher in infants who had received trophic feeds:
Weight: reported MD 130 (95% CI 1 to 250) grams/week.
Head circumference: reported MD 0.7 (95% CI 0.1 to 1.3) cm/week
Mosqueda 2008 reported no statistically significant difference in rates of weight gain during the trial period: MD ‐7.3 (95% CI ‐19.2 to 4.6) grams/week.
Sáenz de Pipaón 2003 reported that the weight above birth weight attained by day 21 was not statistically significantly different (188 grams versus 190 grams).
Troche 1995 reported that infants in the trophic feeding group had a higher increase in weight over birth weight to day 30 (223 (SD 125) versus 95 (SD 161) grams).
Meetze 1992 reported no statistically significant difference in weight gain between the groups at day 30: 264 (SD 126) grams versus 213 (SD 142) grams. Increases in head circumference, length and mid‐arm circumference were reported to be similar for both groups.
Dunn 1988 measured growth throughout the study period up until 60 days of life and did not detect any significant differences between the two groups.
Long‐term growth parameters were not reported by any of the trials.
Neurodevelopment
None of the trials assessed neurodevelopmental outcomes.
Incidence of invasive infection (outcome 1.5; four trials)
Meta‐analysis of three trials did not detect a statistically significant difference: typical RR 1.06 (95% CI 0.72 to 1.56); typical RD 0.02 (95% CI ‐0.10 to 0.13). There was no evidence of heterogeneity (I² = 25%) (Analysis 1.5).
1.5. Analysis.
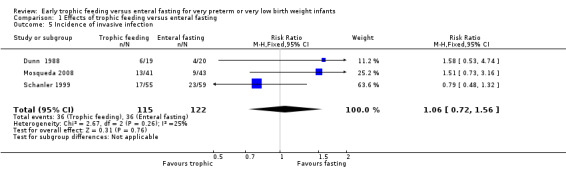
Comparison 1 Effects of trophic feeding versus enteral fasting, Outcome 5 Incidence of invasive infection.
McClure 2000 reported that infants in the minimal enteral nutrition group had a statistically significantly lower mean number of episodes of "culture‐confirmed sepsis" (0.5 versus 1.2 in control group). These data could not be included in the meta‐analysis.
Duration of phototherapy (days) (outcome 1.6; three trials)
Meta‐analysis did not detect a statistically significant effect: MD 0.35 (95% CI ‐0.29 to 0.99) days (Analysis 1.6).
1.6. Analysis.
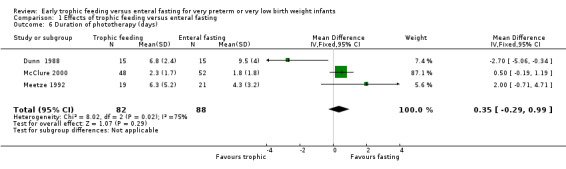
Comparison 1 Effects of trophic feeding versus enteral fasting, Outcome 6 Duration of phototherapy (days).
Duration of hospital stay (outcome 1.7; five trials)
Meta‐analysis of four trials that reported data as mean and SD did not detect a statistically significant effect: MD ‐3.9 (95% CI ‐11.5 to 3.8) days (Analysis 1.7). There was evidence of borderline statistical heterogeneity (I² = 48%).
1.7. Analysis.
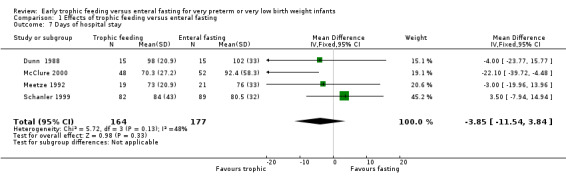
Comparison 1 Effects of trophic feeding versus enteral fasting, Outcome 7 Days of hospital stay.
One trial that reported median and range data did not find a statistically significant difference: 81 days versus 79.5 days (Mosqueda 2008).
Subgroup analyses
Exclusively formula milk‐fed infants: In two trials, infants received only formula milk as trophic feeds (Dunn 1988; Meetze 1992). In the other trials, infants received either breast milk or formula milk or a mixture. Subgroup data were not available.
Infants at least partially fed with breast milk: Subgroup data were not available.
Extremely low birth weight (ELBW) or extremely preterm infants: One trial restricted participation to ELBW infants (Mosqueda 2008). In the other trials, it is likely that less than one‐third of all participants were ELBW or extremely preterm but subgroup data were not available.
Infants with intrauterine growth restriction or infants with absent or reversed end‐diastolic flow velocities (AREDFV): In those trials where birth weight < 10th percentile was not an exclusion criterion, subgroup data were not available. One trial restricted participation to infants who were small for gestational age (birth weight < 10th percentile for reference population) (van Elburg 2004).
Discussion
Summary of main results
The available data from randomised controlled trials do not provide evidence that early trophic feeding compared to enteral fasting confers any substantial benefits for very preterm or very low birth weight (VLBW) infants. Although some trials reported that minimal enteral nutrition reduced the time taken to establish full enteral feeds, meta‐analysis of all of the available data did not detect a statistically significant effect.
The trial data do not suggest that minimal enteral nutrition is associated with important harms. Meta‐analyses did not detect statistically significant effects on the incidence of necrotising enterocolitis, invasive infection or all‐cause mortality. Only limited data on growth outcomes were found. Trials found inconsistent effects on short‐term growth and meta‐analysis did not reveal a significant difference in the time taken to regain birth weight. The clinical importance of any short‐term effects is unclear as no long‐term growth or developmental outcomes were assessed.
Overall completeness and applicability of evidence
These findings should be applied with caution. Although we did not find evidence of an effect on feed intolerance, the existence of substantial statistical heterogeneity in the meta‐analysis limits the validity of this finding. The heterogeneity was not explained by differences between trials in methodological quality or the type of intervention or participants. It may be that variations in enteral feeding protocols and practices contributed to heterogeneity.
These findings may not be applicable to some infants at highest risk of developing feed intolerance or necrotising enterocolitis. Only a minority of participants in the included trials were extremely low birth weight (ELBW) or extremely preterm infants or had evidence of intrauterine growth restriction. None of the trials specifically recruited infants with absent or reversed end‐diastolic flow velocities on Doppler ultrasound of the umbilical arteries. Furthermore, the risk‐benefit balance of enteral feeding strategies may differ between breast milk‐fed and formula‐fed very preterm or VLBW infants. One study reported that mothers who expressed breast milk for early trophic feeding were more likely to continue to provide breast milk as the ongoing principal form of nutrition for their infants (Schanler 1999). Further study to confirm and define the mechanism of this association is merited given that feeding with breast milk compared to formula reduces the risk of necrotising enterocolitis in very preterm or VLBW infants (Quigley 2007).
It is also unclear whether the findings can be applied to infants who receive continuous infusion of milk feeds as all of the infants in the included trials received enteral feeds as interval boluses. A recently described issue is that bolus administration of volumes up to 0.5 ml results in substantial retention of milk within standard gastric feeding tubes (which will then be aspirated prior to the next feed). Consequently, infants will not actually receive any milk intragastrically unless trophic feeding is delivered continuously (McHale 2010). Randomised controlled trials have reported conflicting findings about the effect on continuous enteral infusion on feed tolerance in very preterm and VLBW infants (Premji 2011).
Quality of the evidence
The included trials were generally of good methodological quality but in common with other trials of feeding interventions in this population it was not possible to mask care givers and clinical assessors to the nature of the intervention (Figure 1). This may be an important source of bias particularly in trials that did not use prespecified definitions of feed intolerance that mandated interrupting or ceasing feed volume advancement. Care givers or clinicians who were aware of the treatment group may have defined feed intolerance subjectively and differentially. Any surveillance and ascertainment biases secondary to the lack of blinding are more likely to have caused an over‐estimation of the incidence of feed intolerance or necrotising enterocolitis in infants who received minimal enteral nutrition.
1.
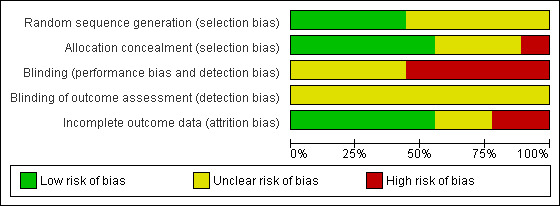
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Authors' conclusions
Implications for practice.
The available trial data do not provide strong evidence that early trophic feeding has important effects on feed intolerance, growth or development. There is no evidence that trophic feeding has adverse effects. For necrotising enterocolitis, the lower and bounds of the 95% CI of the number needed to treat for an additional harmful outcome (NNTH) estimate are consistent with either five more cases or three fewer cases in every 100 infants who receive early trophic feeding. For mortality, the NNTH 95% CI is consistent with one more case or 10 fewer cases in every 100 infants who receive early trophic feeding.
Implications for research.
Any new randomised controlled trials of early trophic feeding versus enteral fasting should aim to ensure the participation of extremely low birth weight (ELBW) and extremely preterm infants as well as infants with evidence of compromised intrauterine growth so that findings are applicable to these infants at highest risk of necrotising enterocolitis. Undertaking trials of feeding interventions in this population is problematic (Tyson 2007). It is difficult to perform a pragmatic trial that will ensure that care givers and investigators are unaware of the allocated feeding regimen. A priori agreements on objective definitions of feed intolerance and indications for interruption of enteral feeding and for investigation of necrotising enterocolitis may help minimise the impact of this source of bias. Trials should also aim to assess more objective outcomes, principally mortality and long‐term growth and development.
What's new
| Date | Event | Description |
|---|---|---|
| 6 February 2013 | New citation required and conclusions have changed | The title has been amended to 'Early trophic feeding versus enteral fasting for very preterm or very low birth weight infants' to emphasise the comparison with fasting rather than progressive feeding. The search strategy was updated in December 2012. One new study was assessed for eligibility but was excluded based on the definition of the interventions. Further (unpublished) data were obtained from current included trials and added to the meta‐analyses. |
| 27 December 2012 | New search has been performed | This updates the review 'Early trophic feeding for very low birth weight infants' (Bombell 2009). |
History
Protocol first published: Issue 4, 1997 Review first published: Issue 4, 1997
| Date | Event | Description |
|---|---|---|
| 7 March 2009 | New citation required and conclusions have changed | New authorship: Sarah Bombell, William McGuire. |
| 7 March 2009 | New search has been performed | This updates the review 'Trophic feedings for parenterally fed infants' by Tyson JE, Kennedy KA, Cochrane Database of Systematic Reviews 2005, Issue 3 (Tyson 2005). The title has been modified to 'Early trophic feeding for very low birth weight infants' and has a new authorship of Sarah Bombell and William McGuire. Changes made to the original protocol are outlined below: 1. The population has been restricted to very low birth weight and very preterm infants. 2. Early trophic feeding is defined as enteral feeding up to 24 ml/kg/day (1 ml/kg/hour) beginning within four days after birth and continued until at least one week after birth versus enteral fasting for at least one week after birth. On the subsequent introduction of progressive enteral feeding, infants should have received the same type of milk (breast milk or formula), the same route and mode of feeding (intragastric or transpyloric, bolus gavage or continuous), and the same rate of feed volume advancement in both groups. 3. Subgroup analyses of extremely low birth weight and extremely preterm infants and infants with evidence of intrauterine growth restriction or absent or reversed end‐diastolic flow velocities in Doppler studies of the fetal aorta or umbilical artery were prespecified. Search updated February 2009. Three new trials were included (Sáenz de Pipaón 2003; van Elburg 2004; Mosqueda 2008). Five trials included in the previous version of this review have been excluded because they did not fulfil the stricter definition of the intervention and comparison (Ostertag 1986; Slagle 1988; Berseth 1992; Berseth 1993; Berseth 2003). The main change to the findings and implications for practice is that the typical estimate for feed tolerance (time to full enteral feeding) is no longer statistically significant. |
| 28 October 2008 | Amended | Converted to new review format. |
| 31 March 2005 | New search has been performed | This review updates the existing review of 'Minimal enteral nutrition in parenterally fed neonates' that was published in The Cochrane Library, Disk Issue 4, 1997. Three new eligible trials (Berseth 2003; McClure 2000; Schanler 1999) have been found. |
| 31 March 2005 | New citation required and conclusions have changed | Substantive amendment. |
Acknowledgements
We thank Dr Schanler for providing further data from Schanler 1999 and Dr Sáenz de Pipaón for clarification on data from Sáenz de Pipaón 2003.
We are grateful to Ms Bethan Carter for developing and running the electronic search.
Data and analyses
Comparison 1. Effects of trophic feeding versus enteral fasting.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Days to reach full enteral feeding | 6 | 556 | Mean Difference (IV, Fixed, 95% CI) | ‐1.05 [‐2.61, 0.51] |
| 2 Incidence of necrotising enterocolitis | 9 | 748 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.67, 1.70] |
| 3 Mortality | 8 | 558 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.41, 1.07] |
| 4 Days to regain birth weight | 5 | 518 | Mean Difference (IV, Fixed, 95% CI) | ‐0.01 [‐0.96, 0.95] |
| 5 Incidence of invasive infection | 3 | 237 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.72, 1.56] |
| 6 Duration of phototherapy (days) | 3 | 170 | Mean Difference (IV, Fixed, 95% CI) | 0.35 [‐0.29, 0.99] |
| 7 Days of hospital stay | 4 | 341 | Mean Difference (IV, Fixed, 95% CI) | ‐3.85 [‐11.54, 3.84] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Becerra 1996.
| Methods | Randomised controlled trial | |
| Participants | VLBW infants with asphyxia, respiratory distress syndrome, suspected or documented sepsis, hypotension, hypo‐ or hyperglycaemia, or anaemia or polycythaemia. The proportion who received mechanical ventilation was not stated. Exclusions included imminently expected death, major congenital anomalies or metabolic conditions | |
| Interventions | Minimal enteral nutrition (N = 96) vs. enteral fasting (N = 94) until 7 days after birth. Intervention group received minimal enteral feeds of breast milk or preterm formula milk at 25 ml/kg/day for 1 week. Control infants were not fed until 6 to 8 days after birth | |
| Outcomes | Time to establish full enteral feeds Incidence of necrotising enterocolitis Time to regain birth weight |
|
| Notes | Data as reported in abstract or in correspondence with the principal investigator The method of administration of feeds was not described |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described ‐ reported in abstract form only |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not reported by likely that care givers and investigators were aware of allocation groups |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All data were accounted for |
Dunn 1988.
| Methods | Randomised controlled trial | |
| Participants | VLBW infants with respiratory distress syndrome treated with mechanical ventilation and with an umbilical artery catheter in situ. Setting: Rainbow Babies and Children's Hospital, Cleveland, USA |
|
| Interventions | Minimal enteral nutrition (N = 19) vs. enteral fasting (N = 20) until 9 days after birth. Intervention group infants received minimal enteral feeds from 48 hours at 15 to 20 ml/kg/day of diluted preterm formula milk | |
| Outcomes | Time to establish full enteral feeds Incidence of necrotising enterocolitis Growth: time to regain birth weight and growth throughout study period Duration of phototherapy Mortality Incidence of sepsis Duration of hospital stay |
|
| Notes | All infants received formula milk. Feeds were given by intermittent gavage nasogastric technique. Data enabling calculation of SD relating to duration of hospital stay were not provided. We have imputed this information from standard deviations provided by Meetze 1992, a trial with similar sample size, as recommended by the Cochrane Handbook |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Stratified into groups according to birth weight then randomised using cards in paired envelopes |
| Allocation concealment (selection bias) | High risk | Unclear if envelopes were sealed ‐ possibility that allocation groups could have been predicted |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No blinding of care givers or investigators after allocation |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No reference to whether interpretation of radiographs was blind |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 9 infants were excluded from some of the outcome data: 5 deaths in the control group, 1 death in the intervention group and 3 infants removed from the minimal enteral nutrition group due to severe unrecognised aortic coarctation, systemic candidiasis and ileus precluding the introduction of feeds. These infants have been included in intention‐to‐treat analysis. Uncertainty exists about whether these infants went on to develop necrotising enterocolitis as this is not formally reported. We have assumed they did not |
McClure 2000.
| Methods | Randomised controlled trial | |
| Participants | Infants weighing < 1750 grams at birth with respiratory distress syndrome who required mechanical ventilation beyond 48 hours. Setting: Leeds General Infirmary, UK |
|
| Interventions | Minimal enteral nutrition (N = 48) vs. enteral fasting (N = 52). Minimal enteral nutrition (0.5 to 1 ml/hour of expressed maternal breast milk or preterm formula) was given from day 3 until mechanical ventilation was discontinued. The control group received no enteral feeding while mechanical ventilation was provided | |
| Outcomes | Feeding tolerance; days to full enteral feeding Incidence of necrotising enterocolitis Time to regain birth weight and growth parameters during hospital admission Days to full oral intake, duration of parenteral nutrition Incidence of invasive infection |
|
| Notes | Both groups received parenteral nutrition. Following discontinuation of mechanical ventilation, "nutritive" enteral feedings were initiated at 1 ml/kg/hour and increased by 1 ml/kg/hour every 8 to 12 hours as tolerated All feeds were given by intermittent gavage |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence |
| Allocation concealment (selection bias) | Low risk | Blinding of investigators at the time of randomisation |
| Blinding (performance bias and detection bias) All outcomes | High risk | Care givers and investigators were not blinded to allocation groups after randomisation had occurred |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description of whether radiological assessment was blind. Laboratory staff were blinded to allocation groups |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All data were accounted for |
Meetze 1992.
| Methods | Randomised controlled trial | |
| Participants | Infants of birth weight 501 to 1250 grams and gestational age at birth 25 to 32 weeks Proportion of infants receiving mechanical ventilation not stated Setting: neonatal unit, Gainesville, USA |
|
| Interventions | Minimal enteral nutrition (N = 22) vs. enteral fasting (N = 25). The minimal enteral nutrition group received preterm formula beginning at 2.5 ml/kg/day on day 3 advancing to 22 ml/kg/day on day 14. During this time controls were not fed. Both groups received progressive enteral feeds from day 15 | |
| Outcomes | Incidence of necrotising enterocolitis Growth at day 30 Mortality Duration of phototherapy Duration of hospital stay |
|
| Notes | Infants receiving breast milk were excluded All feeds were given by intermittent bolus orogastric administration |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Stratified randomisation based on birth weight (method of randomisation not described) |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Care givers and investigators not blinded to intervention group |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Not all data were accounted for. 7 infants were not included in all components of the final analyses: 1 infant in the minimal enteral nutrition group developed necrotising enterocolitis on day 7 and was subsequently excluded from further analyses, 2 infants died and 4 parents withdrew consent. This accounts for 15% of all infants participating at time of randomisation. 6 other infants developed necrotising enterocolitis after day 20 and were included in all components of the analysis |
Mosqueda 2008.
| Methods | Randomised controlled trial | |
| Participants | ELBW infants < 24 hours old Infants with congenital anomalies, infants receiving inotrope support or exchange transfusion and infants with severe acidaemia were ineligible Setting: Neonatal Intensive Care Unit of Loyola University Medical Center, Maywood, USA |
|
| Interventions | Minimal enteral nutrition (N = 41) vs. enteral fasting (N = 43). Minimal enteral nutrition (12 ml/kg/day) with expressed breast milk or standard formula milk was given from day 2 until day 7. The control group received no enteral feeding. Both groups received standard parenteral nutrition. Both groups received progressive enteral feeds (increasing by 10 ml/kg/day) from day 8 | |
| Outcomes | Feeding tolerance; days to full enteral feeding Incidence of necrotising enterocolitis Time to regain birth weight and growth parameters during hospital admission Duration of hospital admission |
|
| Notes | Feeds were given intermittently as boluses of nasogastric or orogastric feeds | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not stated but unlikely that care givers and investigators were blinded to allocation groups |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear if interpretation of abdominal X‐rays was blind |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Overall 23 out of 84 infants were not included in all components of the analysis due to protocol violation, withdrawal of consent or death (8 in the minimal enteral feeding group, 15 in the control group). This equates to 27% of the initial infants at randomisation |
Schanler 1999.
| Methods | Randomised controlled trial | |
| Participants | Infants 26 to 30 weeks' gestation whose birth weight was appropriate for gestational age, who had no major congenital anomalies Setting: Texas Children's Hospital, Texas, USA |
|
| Interventions | Minimal enteral nutrition (N = 82) vs. enteral fasting (N = 89). The minimal enteral feeding group received 20 ml/kg/day of expressed breast milk or half‐strength preterm formula from day 4 to 14 after birth | |
| Outcomes | Feeding tolerance; days to full enteral feeding Incidence of necrotising enterocolitis Time to regain birth weight and growth parameters during hospital admission Incidence of invasive infection Mortality |
|
| Notes | This study used a factorial design in which infants were randomised to 4 groups (continuous minimal enteral feeds, intermittent bolus minimal enteral feeds, enteral fasting followed by continuous feeding, enteral fasting followed by bolus feeding) to allow simultaneous assessment of the use of both minimal enteral nutrition and continuous feedings vs. bolus. In this review, Schanler 1999 refers to outcomes reported for all infants in trophic feedings group vs. all control infants [February 2009: mortality data received from Dr Schanler.] [June 2012: incidence of infection data received from Dr Schanler] |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Stratification by gestational age and type of milk followed by randomisation using sealed opaque envelopes |
| Allocation concealment (selection bias) | Low risk | Adequate given the use of sealed envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Care givers and investigators not blinded following randomisation |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Intention‐to‐treat analysis |
Sáenz de Pipaón 2003.
| Methods | Randomised controlled trial | |
| Participants | Infants weighing < 1600 grams at birth. Exclusions included infants of diabetic mothers, major congenital anomalies and proven sepsis. Setting: La Paz University Hospital, Madrid, Spain |
|
| Interventions | Minimal enteral nutrition (N = 24) vs. enteral fasting (N = 12). On day 1, infants were randomly allocated to either minimal enteral nutrition (10 ml/kg/day on day 1, then 20 ml/kg/day through until day 7) or enteral fasting for 7 days | |
| Outcomes | This was primarily a metabolic study examining whether enteral leucine uptake was affected by trophic feeding Authors also reported time to establish full feeds Communication with authors revealed data were collected on the incidence of necrotising enterocolitis and mortality |
|
| Notes | March 2009: clarification of methods and outcome data received from Dr Saenz de Pipaon (principal investigator): "If the mother wished to give breast milk and the baby was allocated to the minimal enteral nutrition group, he or she started on day one to receive breast milk. If the mother was not able or did not wish to give breast milk the infant received formula. If the baby was allocated to the enteral fasting group, breast milk or formula was given from day seven." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Correspondence with principal investigator revealed randomisation involved sealed opaque envelopes with 2:1 allocation ratio |
| Allocation concealment (selection bias) | Low risk | Satisfactory |
| Blinding (performance bias and detection bias) All outcomes | High risk | No blinding of care givers or investigators |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement about blinding of radiological assessment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All data were accounted for |
Troche 1995.
| Methods | Randomised controlled trial | |
| Participants | Infants born at 25 to 30 weeks' gestation with respiratory distress, an umbilical artery catheter in situ, and an anticipated need for mechanical ventilation for at least 3 days. Infants with asphyxia or respiratory failure despite ventilatory support were excluded Setting: University of Boston, USA |
|
| Interventions | Minimal enteral nutrition (N = 16) vs. enteral fasting (N = 13) Infants in the minimal enteral nutrition group received maternal breast milk or standard formula beginning within 24 hours after birth at a rate of 0.5 to 1.0 ml/hour until the umbilical artery catheter was removed. Controls were fasted until the umbilical arterial catheter was removed. Both groups received parenteral nutrition beginning on day 3 |
|
| Outcomes | Feeding tolerance; days to full enteral feeding Incidence of necrotising enterocolitis Time to regain birth weight Mortality |
|
| Notes | In infants < 800g at birth, feeds were given by continuous infusion, for those > 800 g feeds were given as boluses | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not stated but likely that care givers and investigators were aware of intervention group after allocation |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2 infants developed necrotising enterocolitis but were then subsequently excluded from growth data |
van Elburg 2004.
| Methods | Randomised controlled trial | |
| Participants | Infants of birth weight < 2000 grams who were small for gestational age (< 10th percentile for birth weight) | |
| Interventions | Minimal enteral nutrition (N = 28) vs. enteral fasting (N = 28) Minimal enteral nutrition (0.5 ml every 2 hours for infants < 1000 grams, 1 ml every 2 hours for infants > 1000 grams) with expressed breast milk or preterm formula milk was given from day 2 for 5 days. The control group received no enteral feeding. Both groups received standard parenteral nutrition. Both groups received progressive enteral feeds (increasing by 10 ml/kg/day) from day 8 |
|
| Outcomes | Feeding tolerance; days to full enteral feeding Incidence of necrotising enterocolitis Time to regain birth weight and growth parameters during hospital admission Duration of intensive care admission |
|
| Notes | The primary aim of this study was to assess the effect of minimal enteral nutrition on intestinal permeability in preterm infants with intra‐uterine growth restriction The method of administration of feeds was not described |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Selection of cards designating the allocation group in sealed envelopes |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Care givers and investigators were not blinded to allocation groups |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear if interpretation of radiological images was blind |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Not all data were accounted for ‐ 25% lost to follow‐up due to incomplete data collection, death and one case of congenital CMV infection |
ELBW: extremely low birth weight SD: standard deviation VLBW: very low birth weight
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Berseth 1992 | This trial compared 2 minimal enteral nutrition regimens. Infants were randomly assigned to receive minimal enteral nutrition on postnatal days 3 to 5 (early feeding) or on days 10 to 14 (late feeding). The trial was excluded because infants did not have the same feeding regimen after completion of the early trophic feeding versus enteral fasting phase |
| Berseth 1993 | This trial did not assess the effect of minimal enteral nutrition. Both groups were fasted enterally during the first week after birth. In the intervention group, minimal enteral feeding was introduced 8 days after birth and controls were given the same volume of water enterally |
| Berseth 2003 | This randomised controlled trial compared minimal enteral nutrition with progressive enteral feed volume advancement (at daily increments of 20 ml/kg) |
| LaGamma 1985 | Although not clearly stated in the title or abstract, this was not a randomised controlled trial |
| Ostertag 1986 | This trial compared delayed versus early introduction of progressive enteral feeds (advanced by 10 ml/kg/day). This trial has been included in the Cochrane review of 'Delayed enteral feeding to prevent necrotising enterocolitis in very low birth weight infants' (Morgan 2011a) |
| Said 2008 | This trial compared delayed versus early introduction of enteral nutrition and may be eligible for inclusion in an update of the Cochrane review of 'Delayed enteral feeding to prevent necrotising enterocolitis in very low birth weight infants' (Morgan 2011a) |
| Slagle 1988 | This trial did not assess the effect of early minimal enteral nutrition. Both groups were fasted enterally during the first week after birth. Minimal enteral nutrition was introduced after 8 days in the intervention group |
| Weiler 2006 | Infants were randomly allocated to minimal enteral nutrition starting on either day 2 or day 4 after birth, that is both groups received 'minimal enteral nutrition' |
Contributions of authors
The review authors developed the protocol, undertook the literature search, appraised the articles, extracted and entered the data, and completed the review jointly.
Sources of support
Internal sources
Centre for Reviews and Dissemination, University of York, UK.
External sources
NIHR, UK.
-
Eunice Kennedy Shriver National Institute of Child Health and Human Development National Institutes of Health, Department of Health and Human Services, USA.
The Cochrane Neonatal Review Group has been funded in part with Federal funds from the Eunice Kennedy Shriver National Institute of Child Health and Human Development National Institutes of Health, Department of Health and Human Services, USA, under Contract No. HHSN267200603418C
Declarations of interest
None.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Becerra 1996 {published and unpublished data}
- Becerra M, Ambiado S, Kuntsman G, Figueroa A, Balboa P, Fernandez P, et al. Feeding VLBW infants; Effect of early enteral stimulation (EES) [abstract]. Pediatric Research 1996;39:304A. [Google Scholar]
Dunn 1988 {published data only}
- Dunn L, Hulman S, Weiner J, Kleigman R. Beneficial effects of early hypocaloric enteral feeding on neonatal gastrointestinal function: preliminary report of a randomized trial. Journal of Pediatrics 1988;112(4):622‐9. [DOI] [PubMed] [Google Scholar]
McClure 2000 {published and unpublished data}
- McClure RJ, Newell SJ. Randomised controlled trial of clinical outcome following trophic feeding. Archives of Disease in Childhood. Fetal and Neonatal Edition 2000;82(1):F29‐F33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClure RJ, Newell SJ. Randomised controlled trial of trophic feeding and gut motility. Archives of Disease in Childhood. Fetal and Neonatal Edition 1999;80(1):F54‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClure RJ, Newell SJ. Randomized controlled study of digestive enzyme activity following trophic feeding. Acta Paediatrica 2002;91(3):292‐6. [DOI] [PubMed] [Google Scholar]
Meetze 1992 {published data only}
- Meetze WH, Valentine C, McGuigan JE, Conlon M, Sacks N, Neu J. Gastrointestinal priming prior to full enteral nutrition in very low birth weight infants. Journal of Pediatric Gastroenterology and Nutrition 1992;15(2):163‐70. [DOI] [PubMed] [Google Scholar]
Mosqueda 2008 {published data only}
- Mosqueda E, Sapiegiene L, Glynn L, Wilson‐Costello D, Weiss M. The early use of minimal enteral nutrition in extremely low birth weight newborns. Journal of Perinatology 2008;28(4):264‐9. [DOI] [PubMed] [Google Scholar]
Sáenz de Pipaón 2003 {published and unpublished data}
- Sáenz de Pipaón M, VanBeek RH, Quero J, Perez J, Wattimena DJ, Sauer PJ. Effect of minimal enteral feeding on splanchnic uptake of leucine in the postabsorptive state in preterm infants. Pediatric Research 2003;53(2):281‐7. [DOI] [PubMed] [Google Scholar]
Schanler 1999 {published and unpublished data}
- Schanler RJ, Shulman RJ, Lau C, Smith EO, Heitkemper MM. Feeding strategies for premature infants: randomized trial of gastrointestinal priming and tube‐feeding method. Pediatrics 1999;103(2):434‐9. [DOI] [PubMed] [Google Scholar]
- Shulman RJ, Schanler RJ, Lau C, Heitkemper M, Ou C, Smith EO. Early feeding, antenatal glucocorticoids, and human milk decrease intestinal permeability in preterm infants. Pediatric Research 1998;44(4):519‐23. [DOI] [PubMed] [Google Scholar]
- Shulman RJ, Schanler RJ, Lau C, Heitkemper M, Ou C, Smith EO. Early feeding, feeding tolerance, and lactase activity in preterm infants. Journal of Pediatrics 1998;133(5):645‐9. [DOI] [PubMed] [Google Scholar]
Troche 1995 {published data only}
- Troche B, Harvey‐Wilkes K, Engle WD, Nielsen HC, Frantz ID, Mitchell ML, et al. Early minimal feedings promote growth in critically ill premature infants. Biology of the Neonate 1995;67(3):172‐81. [DOI] [PubMed] [Google Scholar]
van Elburg 2004 {published data only}
- Elburg RM, Berg A, Bunkers CM, Lingen RA, Smink EW, Eyck J, et al. Minimal enteral feeding, fetal blood flow pulsatility, and postnatal intestinal permeability in preterm infants with intrauterine growth retardation. Archives of Disease in Childhood, Fetal and Neonatal Edition 2004;89(4):F293‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Berseth 1992 {published data only}
- Berseth CL. Effect of early feeding on maturation of the preterm infant's small intestine. Journal of Pediatrics 1992;120(6):947‐53. [DOI] [PubMed] [Google Scholar]
Berseth 1993 {published data only}
- Berseth CL, Nordyke C. Enteral nutrients promote postnatal maturation of intestinal motor activity in preterm infants. American Journal of Physiology 1993;264(6 Pt 1):G1046‐51. [DOI] [PubMed] [Google Scholar]
Berseth 2003 {published and unpublished data}
- Berseth CL, Bisquera JA, Paje VU. Prolonging small feeding volumes early in life decreases the incidence of necrotizing enterocolitis in very low birth weight infants. Pediatrics 2003;111(3):529‐34. [DOI] [PubMed] [Google Scholar]
LaGamma 1985 {published data only}
- LaGamma EF, Ostertag S, Birenbaum H. Failure of delayed oral feedings to prevent necrotizing enterocolitis. American Journal of Diseases of Children 1985;139(4):385‐9. [DOI] [PubMed] [Google Scholar]
Ostertag 1986 {published data only}
- Ostertag SG, LaGamma EF, Reisen CE, Ferrentino FL. Early enteral feeding does not affect the incidence of necrotizing enterocolitis. Pediatrics 1986;77(3):275‐80. [PubMed] [Google Scholar]
Said 2008 {published data only}
- Said H, Elmetwally D, Said D. Randomised controlled trial of early versus late enteral feeding of prematurely born infants with birth weight <1200 grams. Kasr El Aini Medical Journal 2008;14:1‐10. [Google Scholar]
Slagle 1988 {published data only}
- Slagle TA, Gross SJ. Effect of early low‐volume enteral substrate on subsequent feeding tolerance in very low birth weight infants. Journal of Pediatrics 1988;113(3):526‐31. [DOI] [PubMed] [Google Scholar]
Weiler 2006 {published data only}
- Weiler HA, Fitzpatrick‐Wong SC, Schellenberg JM, Fair DE, McCloy UR, Veitch RR, et al. Minimal enteral feeding within 3 d of birth in prematurely born infants with birth weight < or = 1200 g improves bone mass by term age. American Journal of Human Nutrition 2006;83(1):155‐62. [DOI] [PubMed] [Google Scholar]
Additional references
Aynsley‐Green 1983
- Aynsley‐Green A. Hormones and postnatal adaptation to enteral nutrition. Journal of Pediatric Gastroenterology and Nutrition 1983;2(3):418‐27. [DOI] [PubMed] [Google Scholar]
Bernstein 2000
- Bernstein IM, Horbar JD, Badger GJ, Ohlsson A, Golan A. Morbidity and mortality among very‐low‐birth‐weight neonates with intrauterine growth restriction. The Vermont Oxford Network. American Journal of Obstetrics and Gynecology 2000;182(1 Pt 1):198‐206. [DOI] [PubMed] [Google Scholar]
Berseth 1990
- Berseth CL. Neonatal small intestinal motility: the motor responses to feeding in term and preterm infants. Journal of Pediatrics 1990;117(5):777‐82. [DOI] [PubMed] [Google Scholar]
Dorling 2005
- Dorling J, Kempley S, Leaf A. Feeding growth restricted preterm infants with abnormal antenatal Doppler results. Archives of Disease in Childhood. Fetal and Neonatal Edition 2005;90(5):F359‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Flidel‐Rimon 2004
- Flidel‐Rimon O, Friedman S, Lev E, Juster‐Reicher A, Amitay M, Shinwell ES. Early enteral feeding and nosocomial sepsis in very low birthweight infants. Archives of Disease in Childhood. Fetal and Neonatal Edition 2004;89(4):289‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Flidel‐Rimon 2006
- Flidel‐Rimon O, Branski D, Shinwell ES. The fear of necrotizing enterocolitis versus achieving optimal growth in preterm infants‐‐an opinion. Acta Paediatrica 2006;95(11):1341‐4. [DOI] [PubMed] [Google Scholar]
Henderson 2009
- Henderson G, Craig S, Brocklehurst P, McGuire W. Enteral feeding regimens and necrotising enterocolitis in preterm infants: a multicentre case‐control study. Archives of Disease in Childhood. Fetal and Neonatal Edition 2009;94(2):F120‐3. [DOI] [PubMed] [Google Scholar]
Johnson 1976
- Johnson CR. The trophic action of gastrointestinal hormones. Gastroenterology 1976;70(2):278‐88. [PubMed] [Google Scholar]
Klingenberg 2012
- Klingenberg C, Embleton ND, Jacobs SE, O’Connell LAF, Kuschel CA. Enteral feeding practices in very preterm infants: an international survey. Archives of Disease in Childhood. Fetal and Neonatal Edition 2012;97(1):F56‐61. [DOI] [PubMed] [Google Scholar]
Lucas 1990
- Lucas A, Cole TJ. Breast milk and neonatal necrotising enterocolitis. Lancet 1990;336(8730):1519‐23. [DOI] [PubMed] [Google Scholar]
McClure 2001
- McClure RJ. Trophic feeding of the preterm infant. Acta Paediatrica. Supplement 2001;90(436):19‐21. [DOI] [PubMed] [Google Scholar]
McHale 2010
- McHale SM, McCarthy R, O'Donnel CPF. How minimal is "minimal" enteral feeding?. Archives of Disease in Childhood. Fetal and Neonatal Edition 2010;95(2):F149‐50. [DOI] [PubMed] [Google Scholar]
Meinzen‐Derr 2009
- Meinzen‐Derr J, Poindexter B, Wrage L, Morrow AL, Stoll B, Donovan EF. Role of human milk in extremely low birth weight infants' risk of necrotizing enterocolitis or death. Journal of Perinatology 2009;29(1):57‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morgan 2011a
- Morgan J, Young L, McGuire W. Delayed introduction of progressive enteral feeds to prevent necrotising enterocolitis in very low birth weight infants. Cochrane Database of Systematic Reviews 2011, Issue 3. [DOI: 10.1002/14651858.CD001970.pub3] [DOI] [PubMed] [Google Scholar]
Morgan 2011b
- Morgan J, Young L, McGuire W. Slow advancement of enteral feed volumes to prevent necrotising enterocolitis in very low birth weight infants. Cochrane Database of Systematic Reviews 2011, Issue 3. [DOI: 10.1002/14651858.CD001241.pub3] [DOI] [PubMed] [Google Scholar]
Patole 2005
- Patole SK, Klerk N. Impact of standardised feeding regimens on incidence of neonatal necrotising enterocolitis: a systematic review and meta‐analysis of observational studies. Archives of Disease in Childhood. Fetal and Neonatal Edition 2005;90(2):147‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Premji 2011
- Premji SS, Chessell L. Continuous nasogastric milk feeding versus intermittent bolus milk feeding for premature infants less than 1500 grams. Cochrane Database of Systematic Reviews 2011, Issue 11. [DOI: 10.1002/14651858.CD001819.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Quigley 2007
- Quigley MA, Henderson G, Anthony MY, McGuire W. Formula milk versus donor breast milk for feeding preterm or low birth weight infants. Cochrane Database of Systematic Reviews 2007, Issue 4. [DOI: 10.1002/14651858.CD002971.pub2] [DOI] [PubMed] [Google Scholar]
Rees 2007
- Rees CM, Pierro A, Eaton S. Neurodevelopmental outcomes of neonates with medically and surgically treated necrotizing enterocolitis. Archives of Disease in Childhood. Fetal and Neonatal Edition 2007;92(3):193‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tyson 2007
- Tyson JE, Kennedy KA, Lucke JF, Pedroza C. Dilemmas initiating enteral feedings in high risk infants: how can they be resolved?. Seminars in Perinatology 2007;31(2):61‐73. [DOI] [PubMed] [Google Scholar]
Walsh 1986
- Walsh MC, Kliegman RM. Necrotizing enterocolitis: treatment based on staging criteria. Pediatric Clinics of North America 1986;33(1):179‐201. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Bombell 2009
- Bombell S, McGuire W. Early trophic feeding for very low birth weight infants. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD000504.pub3] [DOI] [PubMed] [Google Scholar]
Tyson 1997
- Tyson JE, Kennedy KA. Minimal enteral nutrition for promoting feeding tolerance and preventing morbidity in parenterally fed infants. Cochrane Database of Systematic Reviews 1997, Issue 4. [DOI: 10.1002/14651858.CD000504] [DOI] [PubMed] [Google Scholar]
Tyson 2005
- Tyson JE, Kennedy KA. Trophic feedings for parenterally fed infants. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD000504.pub2] [DOI] [PubMed] [Google Scholar]


