Abstract
Objectives
To evaluate a postpartum telephone-based lifestyle intervention to prevent diabetes in high-risk women with recent gestational diabetes mellitus (GDM).
Design
Multicentre parallel randomised clinical trial.
Setting
Specialised antenatal clinics in the Brazilian National System.
Methods
Lifestyle Intervention for Diabetes Prevention After Pregnancy compared (1:1) postpartum telephone support for lifestyle changes with conventional care in women with recent GDM at substantial risk for diabetes. Randomisation started on 28 March 2015 and ended on 13 March 2020, with the onset of the COVID-19 pandemic. We used Cox regression to estimate HRs for diabetes and analysis of covariance adjusted for follow-up time to assess weight change.
Outcomes
The primary outcome was incident diabetes ascertained with blinded measurements of oral glucose tolerance tests. The secondary outcome was a change in measured weight.
Results
We enrolled 5323 women with GDM, 2735 (51%) being at high risk. After invitations, baseline assessment and exclusions, we assigned 466 women to intervention (231) or control (235) groups. Attendance was satisfactory (≥7/20 phone sessions) in 75%. Over an average follow-up of 29.7 (15.6) months, 142 (30.5%) women progressed to diabetes, 75 (32%) in the control and 67 (29%) in the intervention group. There was no reduction in the incidence of diabetes (HR=0.84; 0.60–1.19) and only a non-significant 0.97 kg less weight gain (p=0.09). Among the 305 women randomised more than 1 year before the COVID-19 pandemic, the intervention did not reduce the incidence of diabetes (HR=0.71; 0.48–1.04) despite a 2.09 kg (p=0.002) lesser weight gain.
Conclusion
The strategy to identify women with GDM at high risk proved valid, as women often gained weight and frequently developed diabetes. Over a 30-month follow-up, telephone support for lifestyle changes at postpartum did not reduce weight gain or diabetes incidence, although only 75% attended the minimum number of telephone sessions. The COVID-19 pandemic negatively impacted trial conduction.
Trial registration number
Keywords: General diabetes, Obesity, Clinical Trial
STRENGTHS AND LIMITATIONS OF THIS STUDY.
Lifestyle Intervention for Diabetes Prevention After Pregnancy is a randomised clinical trial testing telephone-based lifestyle interventions to prevent incident diabetes in women with recent gestational diabetes mellitus (GDM).
It documented the utility of medication use to treat GDM as a marker of high risk to indicate the necessity of early postpartum interventions to prevent diabetes.
The clinically relevant primary outcome of incident diabetes was evaluated in 466 women over an average of 30 months.
The COVID-19 pandemic negatively impacted the trial, limiting interventions and participant adherence, and leading to premature trial closure.
Introduction
The prevalence of diabetes is rising in epidemic proportions,1 and efforts to halt new cases are highly needed. Although interventions are effective in preventing diabetes when applied to high-risk subjects,2 even in real-world settings,3 a key obstacle is identifying the high-risk individuals who could benefit most. To this end, the routine detection of gestational diabetes mellitus (GDM)4 provides an excellent opportunity to identify high-risk women for diabetes prevention.
Subgroup analyses of women with previous GDM in the Diabetes Prevention Programme (DPP) documented a 50% reduction in the incidence of diabetes.5 6 However, since the DPP intervention started about 9 years after the last pregnancy, many women with previous GDM likely had already developed diabetes. We do not know to what extent earlier intervention could be beneficial. Systematic reviews of trials initiated shortly after pregnancy suggest modest benefit and likely publication bias.7,9
The Committee on the Impact of Pregnancy on Long-term Health and the International Federation of Gynecology and Obstetrics (FIGO) Division on Maternal and Newborn Health recommend using pregnancy to identify high-risk women and start preventive intervention. Their Best Practice Advice includes yearly screening to identify women at high risk of progression and to consider insulin use during pregnancy as an indicator of priority.10 However, this means of high-risk identification has not been evaluated in clinical trials, and the benefits of early lifestyle intervention for these women at a time at which adoption of lifestyle changes may not be a priority have not been established.
To contribute to closing this gap in the evidence for diabetes prevention, we conducted a randomised controlled clinical trial to assess whether a lifestyle intervention delivered by telephone, compared with conventional care, reduces the incidence of type 2 diabetes and weight gain when offered to high-risk women with a recent pregnancy complicated by GDM.
Research design and methods
Study design
Lifestyle Intervention for Diabetes Prevention After Pregnancy (LINDA-Brasil) is a multicentre, parallel randomised clinical trial to prevent diabetes in high-risk women with recent GDM tailored for the early years after pregnancy. The full protocol is available elsewhere.11 The study protocol was registered with ClinicalTrials.gov on 23 December 2014 (NCT02327286). The telephone intervention was pretested in two small pilot studies followed by two focal group discussions.
Recruitment during pregnancy
Trained research assistants recruited study subjects at specialised prenatal care services of the Brazilian national health system (Sistema Único de Saúde) in six cities and consecutively enrolled pregnant women with GDM aged 18 years or older from 3 January 2014. Since the GDM diagnostic criteria were not settled in Brazil at the start of the study, we allowed the inclusion of cases regardless of the criteria applied. However, most were diagnosed with the International Association of Diabetes and Pregnancy Study Groups criteria.12 We did not recruit women living too far from or with difficulty returning to our study sites.
At pregnancy recruitment, we gathered information through interviews and chart reviews and offered folders addressing the importance of diabetes prevention and the benefits of breastfeeding. We then followed women by telephone to obtain the date and place of delivery, intention to breastfeed and breastfeeding practices, use of insulin and oral antidiabetic medication during the ensuing months of pregnancy, and last measured pregnancy and postpartum weights. These women formed our recruitment cohort.
Trial procedures
Starting 2 months after delivery and up to 24 months after pregnancy, trained clinical staff contacted all eligible women from our recruitment cohort by telephone to invite them to the trial. The main eligibility criterion was being at an elevated risk of type 2 diabetes. Although we initially considered defining high-risk based only on postpartum glucose testing, our pilot studies showed a low yield of testing, which led us to define high-risk based primarily on requiring insulin to treat GDM.13 As the increased prescription of oral hypoglycaemics (mainly metformin) during the trial diminished insulin use, we amended our protocol to extend eligibility to include those using these agents. Also, eligible were women presenting postpartum intermediate hyperglycaemia (fasting plasma glucose>100 mg/dL (5.6 mmol/L) or 2-hour plasma glucose>140 mg/dL (7.8 mmol/L)).14
We excluded those with (1) confirmed diabetes on two occasions (fasting plasma glucose≥126 mg/dL (7.0 mmol/L) or 2-hour glucose≥200 mg/dL (11.1 mol/L)) or unequivocal values on one occasion (both fasting and 2-hour plasma glucose values reaching these standard diabetes thresholds, fasting plasma glucose≥140 mg/dL (7.8 mmol/L) or 2-hour glucose≥270 mg/dL (15 mol/L)); (2) current use of antidiabetic medication; (3) poor attendance during trial preparation; or (4) presence of a health condition, such as a body mass index>40 kg/m2, restricting the ability to practice physical activity, affecting glucose tolerance or limiting participation or survival.
At the trial baseline, trained clinical staff applied a structured questionnaire, measured weight and height and conducted a standardised 2-hour 75 g oral glucose tolerance test (OGTT).14 They extracted additional information on prenatal care and delivery from the official pregnancy healthcare record brought by the participant. They excluded women who had diabetes and randomised the remaining women to two treatment groups between 28 January 2015 and 13 March 2020. Sequence generation was programmed by a staff biostatistician (RL) in a 1:1 ratio, stratified by centre, and performed in random blocks of sizes four and six. The centrally generated sequence was concealed, and the randomised allocations were provided automatically through the data entry system. The study started in Porto Alegre, followed by Fortaleza and Pelotas, and later was expanded to centres in São Paulo, Rio de Janeiro, and Curitiba.
To reduce losses to follow-up, we offered, to the extent possible, ways to cover participants’ transportation expenses to the study centres.
Treatment groups
The control group received conventional care for women with prior GDM based on guidelines for healthy eating,15 physical activity16 and breastfeeding.17 They received a small booklet with instructions about lifestyle changes, breastfeeding and the importance of periodically checking diabetes status.
The intervention group additionally received telephone support from trained personnel to implement lifestyle changes and a structured 173-page notebook with text and worksheets, a portable scale, a pedometer and a kit for milk extraction. The intervention was delivered individually and entirely via telephone by trained and certified health professionals. Together with each participant, we built modest but progressive goals for healthy eating, reducing sedentary behaviour, increasing physical activity, breastfeeding and gradually losing weight. When exclusive breastfeeding ended, we encouraged further enhancement of physical activity (online supplemental table 1).
Interventions were participant centred,17,20 allowing for individual adaptations within the limits of a standardised prevention programme with defined goals and structure. We based communications on social cognitive theory,21 using motivational interviewing22 and patient-centred approaches for primary care settings.23 Our instructions used the tactics of Prato RASO (flat plate),24 an acronym for Reduce unhealthy foods and behaviours, Augment healthy ones, Substitute harmful with healthy habits and maintain a continuing Observation of eating habits and physical activity.
The core curriculum comprised 20 sessions. The first seven, which formed the basic part of the programme, focused on the changes in eating and activity habits (part 1) and were generally offered in a standard sequence. The following seven sessions (part 2), which included problem resolution, managing stress, dealing with relapses and engaging in moderate and vigorous physical activities, were administered with greater flexibility in timing and order. The final sessions (part 3) were a booster of up to six more sessions to review and maintain progress and manage relapses (online supplemental table 2).
We initially offered weekly sessions during the first year, then biweekly and monthly. Although we designed the first 14 sessions to be completed within 1 year, they frequently extended over a longer period to allow women more time to review and absorb the materials covered. During the second year, we provided bi-monthly sessions until the entire curriculum was completed. Following its completion, we maintained at least yearly contact until we closed the trial.
Outcomes
We scheduled visits for outcome assessment at 6 months, 1 year and annually after that for both groups, always on different days, to avoid contamination across groups.
The primary outcome was incident type 2 diabetes, ascertained by OGTT in both groups and defined by a single value reaching standard criteria (fasting plasma glucose≥126 mg/dL (7.0 mmol/L) or 2-hour glucose≥200 mg/dL (11.1 mol/L)). Glucose determinations were done by certified lab staff blinded to patient allocation. Principal investigators, clinical staff, outcome assessors and participants remained blinded to glucose results during the trial. However, when a participant crossed a diabetes threshold, the laboratory notified the clinical staff, who referred the woman for treatment. Determinations were conducted on fresh samples by certified local labs. Repeated measurements at the Study’s central lab confirmed diabetes for all but 6 women with values extremely near the diabetes threshold; for an additional 16 subjects, we only had local lab measurements.
Our secondary outcome was measured weight change from baseline to last visit.
Statistical analyses
For design purposes, we estimated a cumulative 3-year incidence of diabetes of 25% for the control group. We further estimated a possible relative risk (RR) of 0.60, somewhat less than that observed in the DPP subgroup analysis of women with previous GDM (RR=0.47).5 Based on a Cox proportional hazards model testing a one-sided primary hypothesis at the 0.025 level and considering 90% power, we estimated that 740 women with recent GDM would be needed for the trial.
We monitored process indicators of the trial with monthly reports prepared by one biostatistician (RL) and reviewed by two principal investigators (MIS and BBD). Due to low recruitment (101 women) during the first 2 years, we selected three additional centres and rescheduled a meeting for data and safety monitoring and interim analysis for when the new centres would sum at least 100 women followed for at least 18 months.
With the onset of the COVID-19 pandemic, we ended randomisation on 13 March 2020, with 466 women randomised and eligible for the trial. During the restrictions impairing access to our clinical centres, we allowed glucose determinations to be performed by a certified commercial laboratory, permitting easy access for participants. To the degree possible, we maintained telephone counselling for the intervention group. We closed follow-up at the end of March 2021.
We described the baseline characteristics of the participants using absolute and relative frequencies for categorical variables and mean and SD for continuous variables. Our analyses were conducted as intention to treat. We estimated the incidence rate per 100 person-years using robust Poisson regression with log scale follow-up time as the offset. We described the probability of developing diabetes over time using Kaplan-Meier curves. For four women in the control and five in the intervention group, we censured follow-up at the estimated date at which they became pregnant during the trial. We performed multiple imputation for missing outcomes. We calculated the HR of developing diabetes via Cox proportional hazard models after testing the proportionality assumption. We compared post hoc subgroup differences in intervention effect by adding interaction terms to the Cox models. These comparisons were, for the most part, chosen based on findings of systematic reviews of trials of diabetes prevention following recent GDM. For our secondary outcome, we evaluated mean group differences in total weight change up to the diabetes diagnosis or censoring with analysis of covariance, adjusting for follow-up time.
We considered an alpha value of 5% when testing intervention effects and 10% when assessing effect modification by subgroup categories. All analyses and graphs were performed in SAS V.9.4.
Patient and public involvement
Patients or the public were not involved in the design, conduct, reporting or dissemination plans of our research. However, during pilot studies, we had two focal group discussions with women with recent GDM who gave meaningful suggestions for the telephone sessions.
Results
Description of the sample and follow-up
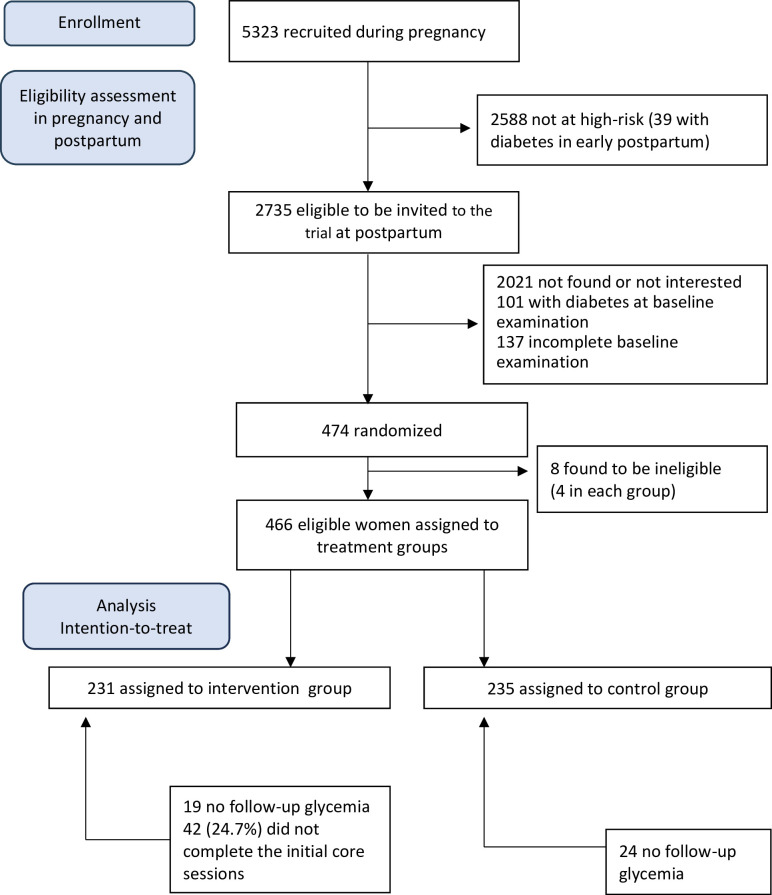
Among the 5323 women with GDM recruited during pregnancy, 2588 did not meet the criteria for high risk for incident type 2 diabetes, including 39 who were found to have diabetes at postpartum before they could be evaluated for trial entry. Among the remaining 2735 (51%) women at high risk, 2021 were not located after pregnancy or were not interested in participating. An additional 101 had diabetes detected at the trial’s baseline examination, 137 did not complete baseline exams and two had already participated in our pilot studies, thus leaving 474 women for randomisation. Eight women (four in each group) were found to be ineligible after randomisation and were excluded. Therefore, we assigned 466 women to the two treatment groups (intervention=231, control=235), constituting our sample for the intention-to-treat analysis (figure 1).
Figure 1. Flow chart for the analytic sample.
Most (69.5%) participants were from the Porto Alegre and Fortaleza centres. Most (66.5%) had entered the trial more than 1 year before the onset of the COVID-19 pandemic, which allowed them sufficient time to complete the initial sessions before the pandemic. About half were less than 6 months post delivery when entering the trial, aged<35 years and had a pregestational BMI≥30 kg/m2. Most had more than one child (70.8%) and had less than a university-level education (75.5%). About half (52.4%) required insulin to treat GDM, and 65.0% had pre-diabetes at baseline. Compared across all categories of these characteristics, intervention and control groups were similar (<20% differences), except for two categories with minimal numbers (enrolled at the Curitiba centre and of other ethnicities) (table 1).
Table 1. Baseline characteristics of the study sample.
| Characteristics | Total | Treatment groups | |||||
| Control | Intervention | ||||||
| N=466 | N=235 | N=231 | |||||
| N | % | 95% CI | % | 95% CI | % | 95% CI | |
| Centre | |||||||
| Porto Alegre | 207 | 44.4 | 39.9 to 48.9 | 44.3 | 37.9 to 50.6 | 44.6 | 38.2 to 51.0 |
| Fortaleza | 117 | 25.1 | 21.2 to 29.0 | 25.5 | 20.0 to 31.1 | 24.7 | 19.1 to 30.2 |
| São Paulo | 58 | 12.5 | 9.5 to 15.4 | 12.8 | 8.5 to 17.0 | 12.1 | 7.9 to 16.3 |
| Rio de Janeiro | 56 | 12,0 | 9.1 to 15.0 | 11.9 | 7.8 to 16.1 | 12.1 | 7.9 to 16.3 |
| Pelotas | 16 | 3.4 | 1.8 to 5.1 | 3.4 | 1.1 to 5.7 | 3.5 | 1.1 to 5.8 |
| Curitiba | 12 | 2.6 | 1.1 to 4.0 | 2.1 | 0.3 to 4.0 | 3,0 | 0.8 to 5.2 |
| Entry | |||||||
| Before March 2019 | 310 | 66.5 | 62.2 to 70.8 | 68.1 | 62.1 to 74.0 | 64.9 | 58.8 to 71.1 |
| After March 2019 | 156 | 33.5 | 29.2 to 37.8 | 31.9 | 26.0 to 37.9 | 35.1 | 28.9 to 41.6 |
| <6 months after birth | 188 | 40.6 | 36.1 to 45.0 | 37.5 | 31.3 to 43.6 | 43.7 | 37.3 to 50.1 |
| ≥6 months after birth | 277 | 59.4 | 55.0 to 63.9 | 62.5 | 56.4 to 68.7 | 56.3 | 49.9 to 62.7 |
| Age (years) | |||||||
| <35 | 233 | 50.8 | 46.2 to 55.3 | 51.5 | 45.1 to 58.0 | 50.0 | 43.5 to 56.5 |
| ≥35 | 226 | 49.2 | 44.7 to 53.8 | 48.5 | 41.0 to 54.9 | 50.0 | 43.5 to 56.5 |
| BMI before pregnancy | |||||||
| <30 kg/m2 | 226 | 48.9 | 42.5 to 55.3 | 48.9 | 42.5 to 55.3 | 48.1 | 41.6 to 54.5 |
| ≥30 kg/m2 | 240 | 51.1 | 47.0 to 56.0 | 51.1 | 44.7 to 57.5 | 51.9 | 45.5 to 58.4 |
| Number of children | |||||||
| 1 | 136 | 29.2 | 25.1 to 33.3 | 28.5 | 22.7 to 34.3 | 29.8 | 24.0 to 35.8 |
| 2 | 168 | 36.1 | 31.7 to 40.4 | 37,0 | 30.9 to 43.2 | 35.1 | 28.9 to 41.2 |
| 3+ | 162 | 34.7 | 30.4 to 39.1 | 34.5 | 28.4 to 40.5 | 35.1 | 28.9 to 41.2 |
| Schooling | |||||||
| Primary or less | 86 | 18.4 | 14.9 to 22.0 | 17.0 | 12.2 to 21.8 | 19.9 | 14.8 to 25.1 |
| Secondary* | 266 | 57.1 | 52.6 to 61.6 | 57.9 | 51.6 to 64.2 | 56.3 | 49.9 to 62.7 |
| University* | 114 | 24.5 | 20.6 to 28.4 | 25.1 | 19.6 to 30.7 | 23.8 | 18.3 to 29.3 |
| Insulin in pregnancy | |||||||
| Yes | 222 | 52.4 | 47.8 to 56.9 | 55.7 | 49.4 to 62.1 | 48.9 | 42.5 to 55.4 |
| No | 244 | 47.6 | 43.1 to 52.2 | 44.3 | 37.9 to 50.6 | 51.1 | 44.6 to 57.5 |
| Pre-diabetes at baseline | |||||||
| Yes | 163 | 65.0 | 60.7 to 69.4 | 66.8 | 60.8 to 72.8 | 63.2 | 57.0 to 69.4 |
| No | 303 | 35.0 | 30.7 to 39.3 | 33.2 | 27.2 to 39.2 | 36.8 | 30.6 to 43.0 |
Comparisons of treatment groups using Chi-squareχ2 or Fisher’´s exact tests did not reveal differences (all pp>0.16).
Complete or incomplete.
BMIbody mass index
Among the 231 women randomised to the intervention group, 57 (25%) did not complete the initial seven protocol sessions. Comparing the moment of randomisation relative to the onset of the pandemic, the fraction not completing this minimal participation was greater (27; 33%) among those randomised closer to the pandemic’s onset than those randomised earlier (30; 20%) (p=0.025).
A total of 43 (9.2%) women randomised did not return for glycaemia assessment (19 receiving the intervention and 24 controls). When randomisation occurred more than 1 year before the pandemic onset, we only lost 12 (3.9%), as opposed to 31 (19.9%) women when randomisation occurred after that. This differential participation resulted in the majority (72%) of women lost to follow-up, having been randomised close to the pandemic onset.
Incidence of diabetes
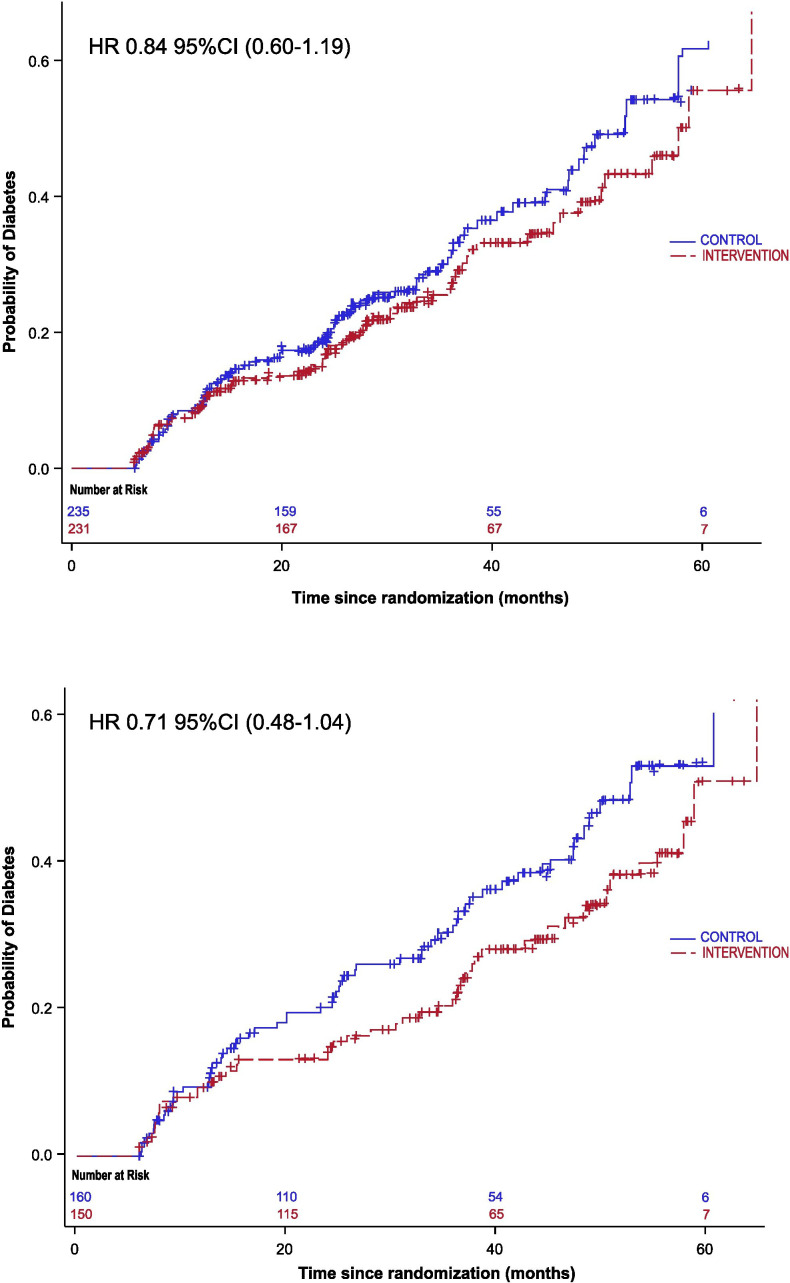
Over an average follow-up of 29.7 (15.6) months, 142 (30.5%) women progressed to diabetes, 75 (32%) in the control and 67 (29%) in the intervention group. The probability of developing diabetes increased steadily throughout the study in both groups, with 53% of the control group having developed diabetes at 5 years. Diabetes incidence was numerically lower in the intervention (11.5; 8.8–14.1 per 100 person-years) than in the control group (13.2; 10.3–16.2 per 100 person-years), with a resultant non-significant incidence reduction (HR=0.84; 0.60–1.19) overall and a somewhat larger one (HR=0.71; 0.48–1.04) for those entering the trial more distant from the COVID-19 pandemic (figure 2, table 2 top and online supplemental table 3).
Figure 2. Kaplan-Meier curves for the incidence of diabetes according to treatment group. Top graph: overall sample (n=466). Bottom graph: after excluding those randomised within 1 year before the COVID-19 pandemic (n=310). Intervention, red; control, blue.
Table 2. Main trial outcomes: incidence of diabetes (primary) and weight change (secondary).
| Incidence of diabetes (n=466) | |||||
| Cases/total | Incidence (per/100 PY) | 95% CI | HR | 95% CI | |
| Overall sample (n=466) | |||||
| Control | 75/235 | 13.2/100 PY | 10.3 to 16.2 | 0.84 | 0.60 to 1.19 |
| Intervention | 67/231 | 11.5/100 PY | 8.8 to 14.1 | ||
| Randomised≥1-year prior to the COVID-19 pandemic (n=310) | |||||
| Control | 64/160 | 14.9/100 PY | 11.4 to 18.5 | 0.71 | 0.48 to 1.04 |
| Intervention | 48/150 | 10.9/100 PY | 8.0 to 13.9 | ||
| Randomised<1-year prior to the COVID-19 pandemic (n=156) | |||||
| Control | 11/75 | 8.1/100 PY | 2.9 to 13.2 | 1.6 | 0.72 to 3.56 |
| Intervention | 19/81 | 13.0/100 PY | 7.2 to 14.7 | ||
| Weight measurements (n=466) | ||||
| Mean baseline weight (kg) 95% CI | Mean weight at last follow-up (kg) 95% CI | Mean weight gain* (kg) 95% CI | P value | |
| Overall sample (n=466) | ||||
| Control | 76.16 (74.49 to 77.84) | 79.83 (77.37 to 81.13) | 2.94 (2.11 to 3.76) | |
| Intervention | 75.94 (74.25 to 77.63) | 78.36 (75.83 to 79.64) | 1.97 (1.18 to 2.75) | |
| Difference | 0.97 (0.14 to 2.08) | 0.09 | ||
| Randomised≥1-year prior to the COVID-19 pandemic (n=310) | ||||
| Control | 75.14 (73.10 to 77.18) | 78.23 (76.01 to 80.45) | 3.09 (2.18 to 4.00) | |
| Intervention | 75.40 (73.21 to 77.58) | 76.28 (73.90 to 78.66) | 1.00 (0.10 to 1.91) | |
| Difference | 2.09 (0.79 to 3.39) | 0.002 | ||
| Randomised<1-year prior to the COVID-19 pandemic (n=156) | ||||
| Control | 78.34 (75.41 to 81.28) | 81.43 (77.94 to 84.92) | 2.62 (0.99 to 4.25) | |
| Intervention | 76.93 (74.27 to 79.59) | 80.44 (77.34 to 83.54) | 3.75 (2.29 to 5.20) | |
| Difference | −1.13 (−3.2 to 0.94) | 0.29 | ||
Adjusted for time of follow-up.
PY, person-years
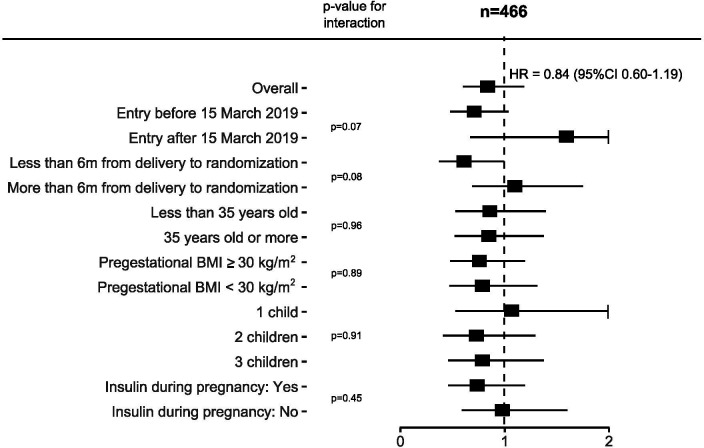
Post hoc subgroup analyses did not reveal substantial differences in effect, except for those randomised before 15 March 2019 (p for interaction=0.07) versus after 15 March and less than 6 months after delivery (p for interaction=0.08) versus more than 6 months (figure 3 and online supplemental table 3).
Figure 3. Effects of a telephone-based lifestyle intervention on the incidence of diabetes according to specific characteristics. N=466.
Effects on the secondary outcome: weight change
Total weight change from baseline to the last measured weight increased in both groups, 2.94 kg in the control versus 1.97 kg in the intervention group, with a mean difference of 0.97 kg (p=0.09). Among those randomised≥1-year before the COVID-19 pandemic (n=310), the mean increased weights were 3.09 kg vs 1.0 kg, with a mean difference of 2.09 kg (p=0.002) (table 2 bottom). Adjustment for baseline factors did not materially change the overall results, the adjusted difference being 0.99 kg (p=0.08).
Discussion
Main findings
The LINDA-Brasil telephone-based lifestyle intervention in women with recent GDM at high diabetes risk, over an average of 30 months of follow-up, produced no reduction in the incidence of diabetes. Though both treatment groups gained weight, those in the intervention group gained numerically less overall and 2 kg less when randomised more than 1 year before the onset of the COVID-19 pandemic. Overall, only 75% of the intervention group completed the seven core telephone sessions; for those randomised more than 1 year prior to the pandemic’s onset, completion was 80%.
Findings in the context of the literature
Our failure to find a reduction in diabetes incidence is consistent with the findings of the LIVING study, which was also negatively impacted by the COVID-19 pandemic and was not focused on high-risk GDM.25 Summary estimates from meta-analyses of lifestyle interventions after a recent GDM show conflicting results.7,9 The latest review, which included the LIVING study, estimated a 24% reduction in the incidence of diabetes (HR=0.76; 0.63–0.93), although analyses suggest that summary estimates of the benefit of lifestyle interventions were likely affected by publication bias.9
The slight weight difference achieved with our telephone intervention is also comparable to previous DPPs offered onsite shortly after a pregnancy complicated by GDM.25 26
Interpretation of the main study findings
These intention-to-treat analyses failed to show a reduction in the incidence of diabetes, mainly because a considerable proportion (25%) of the intervention group did not complete the core telephone sessions. Barriers to initiating and maintaining interventions during the postpartum period are well known.27 We recognised many of them in our pilot studies and shifted from the originally planned on-site lifestyle intervention to a remote one. However, despite multiple adaptations to facilitate intervention uptake, attendance remained incomplete. Although the main reason for this probably relates to the inherent difficulties of recent motherhood, we believe that frequent changes in residence and prepaid phone numbers and lack of motivation contributed, particularly when close to the COVID-19 pandemic.
Study limitations
First, our intervention to increase and sustain breastfeeding was hampered by trial entry occurring more distant from delivery (56.3%≥6 months after pregnancy). Second, an attrition bias is possible, as we had no follow-up for 43 (9.2%) women. However, these losses were similar in the intervention and control groups (19 and 24, respectively). Moreover, since most (72%) women not returning were randomised closer to the pandemic, this key reason for losses was likely non-differential with respect to outcomes. Third, recruitment shortfall, much due to the pandemic-induced premature closure of the trail, led to insufficient statistical power to affirm that the 16% lower incidence found was real.
Study strengths and contributions
Our study has important strengths and provides meaningful contributions. First, it showed that a strategy based principally on pharmacological treatment of GDM during pregnancy was effective in identifying women of very high risk postpartum (>50% incidence of diabetes at 3 years in controls). This strategy of identifying high-risk during rather than after pregnancy allows better preparation for postpartum interventions, including choosing to breastfeed. If applied routinely, it may also promote extending a healthier lifestyle adopted during pregnancy to the postpartum period and may motivate the return of women for early postpartum assessment. Moreover, medication use during pregnancy is a simple way to alert others—immediate family members, primary care providers, and health system administrators—of the need for prompt actions after birth.
Second, our study, particularly given its large sample size, longer duration of follow-up and simple means of finding those at greatest risk, adds information on the potential benefit of lifestyle interventions to the growing body of knowledge on diabetes prevention among women with a recent pregnancy complicated by GDM.7,9
Finally, since our intervention was entirely conducted by telephone, this study contributes to innovating remote intervention methodology for diabetes prevention.28
Applicability and future research
Our strategy of identifying high-risk GDM women is widely applicable in settings willing to establish trained teams to conduct lifestyle education at a distance. The widespread use of cell phones around the world facilitates its applicability. However, stimulating busy new mothers to change lifestyle, especially those with limited resources, is challenging, and the suboptimal adherence we obtained calls for further refinement of the intervention. Specifically, two issues are relevant in this regard.
First, identifying candidates for diabetes prevention during pregnancy permits initiation of interventions during pregnancy or soon after that, facilitating greater uptake of breastfeeding and maintenance of beneficial changes in diet and physical activity achieved during pregnancy.
Second, the delivery of remote interventions should incorporate new technology to qualify and expand virtual contact. New e-health approaches to substitute or complement telephone sessions allow a broader range of options, including, for example, text messaging and visual contact through communication apps.28 Further individualised actions may include remote support groups and home visits, particularly for those with low adherence. Additionally, remote support for lifestyle changes at early postpartum may be coupled with medications proven cost-effective when offered at postpartum.29
Final considerations
Of final note, multiple interactions with our study subjects amid their day-to-day activities during postpartum showed us the importance of public policies to support women and their families, including legislation to guarantee the right of temporary paid leave from work for women and their partners, provision of adequate time and space for breastfeeding, and stimulation of community support for parents caring alone for their babies.
Conclusions
The strategy used to identify women with GDM at high risk proved valid, as women often gained weight and frequently developed diabetes. Over a 30-month follow-up, telephone support for lifestyle changes at postpartum did not reduce weight gain or diabetes incidence, although only 75% attended the minimum number of telephone sessions. The COVID-19 pandemic negatively impacted the conduction of the trial.
supplementary material
Acknowledgements
The authors would like to thank the research teams of the LINDA-Brasil study for their valuable contributions.
Footnotes
Funding: The study received funding from Eli Lilly (Non-Communicable Diseases Partners Grant) and the Brazilian National Council for Scientific and Technological Development. The funders had no role in considering the study design or in the collection, analysis, interpretation of data, writing of the report or decision to submit the article for publication.
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2023-082572).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Ethics approval: This study involves human participants and was approved by Comitê de Ética em Pesquisa, Hospital de Clínicas de Porto Alegre, 563942/2010-0. Participants gave informed consent to participate in the study before taking part.
Data availability free text: Individual deidentified data sharing (including data dictionaries) will require approval from the ethics committee that initially approved the protocol and by the ethics committee at the institution where the new planned analysis will be performed. Federated analyses and metadata sharing can be arranged upon reasonable request. Data can be made available after the main planned reports have been published. All requests should be made to the corresponding author.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Contributor Information
Maria Inês Schmidt, Email: maria.schmidt@ufrgs.br.
Paula A Bracco, Email: paula.abracco@gmail.com.
Maria A Nunes, Email: maanunes@gmail.com.
Kadhija A Cherubini, Email: kadhija.cherubini@gmail.com.
Cristina D Castilhos, Email: cdcastilhos@hcpa.edu.br.
Jainara Z Spagiari, Email: jainaraspa@gmail.com.
Leony M Galliano, Email: lmgalliano@gmail.com.
Ruben Ladwig, Email: ruben.ladwig@proplan.ufrgs.br.
Fabricio B Del Vecchio, Email: fabricioboscolo@gmail.com.
Anelita H M Del Vecchio, Email: anelita1505@gmail.com.
Michele Drehmer, Email: midrehmer@hcpa.edu.br.
Adriana Costa Forti, Email: adrianaforti@uol.com.br.
Cristina Façanha, Email: crisffacanha@hotmail.com.
Lenita Zajdenverg, Email: lenitazaj@gmail.com.
Bianca de Almeida-Pititto, Email: bapititto@unifesp.br.
Rosângela Roginski Réa, Email: rosangelarea@uol.com.br.
Patrícia Medici Dualib, Email: patricia.dualib@uol.com.br.
Bruce B Duncan, Email: bbduncan@ufrgs.br.
Data availability statement
Data are available on reasonable request.
References
- 1.Zhou B, Lu Y, Hajifathalian K. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387:1513–30. doi: 10.1016/S0140-6736(16)00618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haw JS, Galaviz KI, Straus AN, et al. Long-term Sustainability of Diabetes Prevention Approaches: A Systematic Review and Meta-analysis of Randomized Clinical Trials. JAMA Intern Med. 2017;177:1808–17. doi: 10.1001/jamainternmed.2017.6040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Galaviz KI, Weber MB, Straus A, et al. Global Diabetes Prevention Interventions: A Systematic Review and Network Meta-analysis of the Real-World Impact on Incidence, Weight, and Glucose. Diabetes Care. 2018;41:1526–34. doi: 10.2337/dc17-2222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vounzoulaki E, Khunti K, Abner SC, et al. Progression to type 2 diabetes in women with a known history of gestational diabetes: systematic review and meta-analysis. BMJ. 2020;369:m1361. doi: 10.1136/bmj.m1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ratner RE, Christophi CA, Metzger BE, et al. Prevention of diabetes in women with a history of gestational diabetes: effects of metformin and lifestyle interventions. J Clin Endocrinol Metab. 2008;93:4774–9. doi: 10.1210/jc.2008-0772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aroda VR, Christophi CA, Edelstein SL, et al. The effect of lifestyle intervention and metformin on preventing or delaying diabetes among women with and without gestational diabetes: the Diabetes Prevention Program outcomes study 10-year follow-up. J Clin Endocrinol Metab. 2015;100:1646–53. doi: 10.1210/jc.2014-3761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goveia P, Cañon-Montañez W, Santos D de P, et al. Lifestyle Intervention for the Prevention of Diabetes in Women With Previous Gestational Diabetes Mellitus: A Systematic Review and Meta-Analysis. Front Endocrinol. 2018;9:583. doi: 10.3389/fendo.2018.00583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li N, Yang Y, Cui D, et al. Effects of lifestyle intervention on long‐term risk of diabetes in women with prior gestational diabetes: A systematic review and meta‐analysis of randomized controlled trials. Obes Rev. 2021;22:e13122. doi: 10.1111/obr.13122. [DOI] [PubMed] [Google Scholar]
- 9.Retnakaran M, Viana LV, Kramer CK. Lifestyle intervention for the prevention of type 2 diabetes in women with prior gestational diabetes: A systematic review and meta-analysis. Diabetes Obes Metab. 2023;25:1196–202. doi: 10.1111/dom.14966. [DOI] [PubMed] [Google Scholar]
- 10.Adam S, McIntyre HD, Tsoi KY, et al. Pregnancy as an opportunity to prevent type 2 diabetes mellitus: FIGO Best Practice Advice. Intl J Gynecology & Obste . 2023;160:56–67. doi: 10.1002/ijgo.14537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schmidt MI, Duncan BB, Castilhos C, et al. Lifestyle INtervention for Diabetes prevention After pregnancy (LINDA-Brasil): study protocol for a multicenter randomized controlled trial. BMC Pregnancy Childbirth. 2016;16:68. doi: 10.1186/s12884-016-0851-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Metzger BE, Gabbe SG, Persson B, et al. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33:676–82. doi: 10.2337/dc09-1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rayanagoudar G, Hashi AA, Zamora J, et al. Quantification of the type 2 diabetes risk in women with gestational diabetes: a systematic review and meta-analysis of 95,750 women. Diabetologia. 2016;59:1403–11. doi: 10.1007/s00125-016-3927-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American Diabetes Association Standards of Medical Care in Diabetes—2014. Diabetes Care. 2014;37:S14–80. doi: 10.2337/dc14-S014. [DOI] [PubMed] [Google Scholar]
- 15.Dos Santos MCS, Guedes Rodrigues WF, Simões Candeia RM, et al. Cadernos de atenção básica: saúde da criança, aleitamento materno e alimentação complementar. Rev enferm UFPE on line . 2018;12:280. doi: 10.5205/1981-8963-v12i1a230078p280-282-2018. [DOI] [Google Scholar]
- 16.Garber CE, Blissmer B, Deschenes MR, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334–59. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 17.Ministry of Health of Brazil Dietary guidelines for the Brazilian population. 2014
- 18.Rogers CR. Client-Centered Therapy: Its Current Practice, Implications, and Theory. Reprint edition. London: Constable; 1995. [Google Scholar]
- 19.Laine C, Davidoff F. Patient-centered medicine. A professional evolution. JAMA. 1996;275:152–6. [PubMed] [Google Scholar]
- 20.Beach MC, Inui T. Relationship-Centered Care Research Network. Relationship-centered care. A constructive reframing. J Gen Intern Med. 2006;21 Suppl 1:S3–8. doi: 10.1111/j.1525-1497.2006.00302.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. 1st. Englewood Cliffs, N.J: Prentice Hall; 1985. edn. [Google Scholar]
- 22.Miller WR, Rollnick S. Motivational Interviewing, Third Edition: Helping People Change. 3rd. New York, NY: The Guilford Press; 2012. edn. [Google Scholar]
- 23.Neuner-Jehle S, Schmid M, Grüninger U. The “Health Coaching” programme: a new patient-centred and visually supported approach for health behaviour change in primary care. BMC Fam Pract. 2013;14:100. doi: 10.1186/1471-2296-14-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schmidt MI, Duncan BB. In: Medicina Ambulatorial: Condutas de Atenção Primária Baseadas Em Evidências. 4th. Duncan BB, Schmidt MI, Giugliani ERJ, et al., editors. Porto Alegre: ArtMed; 2013. Obesidade: prevenção e tratamento. edn. [Google Scholar]
- 25.Tandon N, Gupta Y, Kapoor D, et al. Effects of a Lifestyle Intervention to Prevent Deterioration in Glycemic Status Among South Asian Women With Recent Gestational Diabetes: A Randomized Clinical Trial. JAMA Netw Open . 2022;5:e220773. doi: 10.1001/jamanetworkopen.2022.0773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.O’Reilly SL, Dunbar JA, Versace V, et al. Mothers after Gestational Diabetes in Australia (MAGDA): A Randomised Controlled Trial of a Postnatal Diabetes Prevention Program. PLoS Med. 2016;13:e1002092. doi: 10.1371/journal.pmed.1002092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Werner EF, Has P, Kanno L, et al. Barriers to Postpartum Glucose Testing in Women with Gestational Diabetes Mellitus. Am J Perinatol. 2019;36:212–8. doi: 10.1055/s-0038-1667290. [DOI] [PubMed] [Google Scholar]
- 28.Nanditha A, Thomson H, Susairaj P, et al. A pragmatic and scalable strategy using mobile technology to promote sustained lifestyle changes to prevent type 2 diabetes in India and the UK: a randomised controlled trial. Diabetologia. 2020;63:486–96. doi: 10.1007/s00125-019-05061-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bolou A, Drymoussi Z, Lanz D, et al. Metformin in the prevention of type 2 diabetes after gestational diabetes in postnatal women (OMAhA): a UK multicentre randomised, placebo-controlled, double-blind feasibility trial with nested qualitative study. BMJ Open. 2023;13:e073813. doi: 10.1136/bmjopen-2023-073813. [DOI] [PMC free article] [PubMed] [Google Scholar]