Abstract
Ebola virus causes severe hemorrhagic fever in primates, resulting in mortality rates of up to 100%, yet there are no satisfactory biologic explanations for this extreme virulence. Here we show that antisera produced by DNA immunization with a plasmid encoding the surface glycoprotein (GP) of the Zaire strain of Ebola virus enhances the infectivity of vesicular stomatitis virus pseudotyped with the GP. Substantially weaker enhancement was observed with antiserum to the GP of the Reston strain, which is much less pathogenic in humans than the Ebola Zaire and Sudan viruses. The enhancing activity was abolished by heat but was increased in the presence of complement system inhibitors, suggesting that heat-labile factors other than the complement system are required for this effect. We also generated an anti-Zaire GP monoclonal antibody that enhanced viral infectivity and another that neutralized it, indicating the presence of distinct epitopes for these properties. Our findings suggest that antibody-dependent enhancement of infectivity may account for the extreme virulence of the virus. They also raise issues about the development of Ebola virus vaccines and the use of passive prophylaxis or therapy with Ebola virus GP antibodies.
Ebola virus—a filamentous, enveloped, nonsegmented negative-strand RNA virus of the family Filoviridae—causes severe hemorrhagic fever in primates. The mortality rate in hosts infected with the Zaire strain is nearly 90%, while the Reston strain is less pathogenic in humans (2, 3, 16). The virus contains at least seven structural proteins (2, 16). One of the structural protein genes encodes both the virion surface glycoprotein (GP), which is responsible for virus penetration into cells (18, 26), and the nonstructural secretory glycoprotein (SGP) (17, 21). GP is expressed by transcriptional editing, resulting in the addition of an extra adenosine within a stretch of seven adenosines in the coding region (17, 21).
The SGP is found in high concentrations in the culture medium of infected cells and in the blood of acutely infected patients (17, 20), but its function is not fully understood. Recently, SGP, but not GP, was reported to bind to neutrophils and inhibit early neutrophil activation (29). While this function may explain the rapid dissemination of the virus throughout the body, it does not provide adequate insight into the pathophysiologic events leading to the extreme pathogenicity of Ebola virus Zaire and Sudan strains.
Previous studies of Ebola virus were limited by the biohazards associated with such investigations. Recent progress in the pseudotyping of vesicular stomatitis virus (VSV) and retrovirus has opened the way for functional studies of the Ebola virus GP without biosafety level 4 containment (18, 26, 29). To investigate the potential of the Ebola virus GP to induce neutralizing antibodies, we produced GP antisera by DNA immunization. As described here, the results suggest strain-specific, antibody-dependent enhancement of infection.
MATERIALS AND METHODS
Plasmids.
The Zaire and Reston GP and SGP genes containing a C-terminal histidine tag were cloned into a mammalian expression vector, pCAGGS/MCS, which contains the chicken β-actin promoter (12, 13), resulting in plasmids pCEboZGP, pCEboRGP, pCEboZSGP, pCEboRSGP, respectively. To obtain a soluble form of GP for antigen, we also constructed a plasmid (pCZGP643HIS) encoding the ectodomain of GP with a C-terminal histidine tag, using the same expression vector.
Immunization of mice.
Twice, at 4-week intervals, two 6-week-old female BALB/c mice were immunized with 20 μg of pCEboZGP or a control expression plasmid, pCAGGS/MCS, by in vivo electroporation (Square Electroporator CUY-21; BEX, Tokyo, Japan) as recommended by the manufacturer. Mice were injected intramuscularly with the plasmids, and then a pair of electronic needles were inserted into the DNA injection site to deliver electric pulses. Sera were collected 3 weeks after the second immunization. Pooled sera from two mice were used in each experiment. For gene gun immunization, eight or nine 6-week-old female BALB/c mice were immunized with 2 μg of pCEboZGP, pCEboRGP, or pCAGGS, using particle-mediated DNA immunization (Powderject XR-1 device; Powderject, Madison, Wis.) (7) twice, at 4-week intervals, followed by boosting 2 months later. Sera were obtained 3 weeks after the last immunization.
Infectivity enhancement and neutralization tests.
VSV pseudotyped with the Ebola virus Zaire GP or the Reston GP (VSVΔG∗-ZaireGP or VSVΔG∗-RestonGP, respectively), expressing green fluorescent protein, was generated as previously described (18). Sera were diluted and mixed with equal volumes of the pseudotyped viruses (104 infectious units on human kidney 293 cells), followed by 1.5 h of incubation. Infectivity was then determined with 293 cells by counting the fluorescent cells as described previously (18). The relative percentage of infected cells was determined by setting the number of infected cells in the presence of normal mouse serum (approximately 50 green fluorescent protein-positive cells per microscopic field) to zero.
Treatment of sera.
Antiserum and control serum were preincubated with 200 μg of protein A (Sigma) per ml for 30 min at room temperature, zymosan (20 mg/ml; Sigma) for 1 h at 37°C, or 0.05 M of EGTA for 30 min at room temperature, and then mixed with VSVΔG∗-ZaireGP. For heat-treatment, sera were incubated at 56°C for 30 min.
Production of SGPs.
SGPs were produced from 293T cells transfected with pCEboZSGP or pCEboRSGP. The amounts of SGPs in the supernatants were estimated by enzyme-linked immunosorbent assay (ELISA), using purified histidine-tagged SGPs and anti-polyhistidine monoclonal antibody (MAb).
Generation of monoclonal antibodies.
To obtain a soluble form of GP, 293T cells were transfected with pCZGP643HIS, and soluble GP was purified from the supernatants using a nickel-bead column (Qiagen). Mice were immunized twice with 293T cells expressing Zaire GP at 2-week intervals, followed by a booster injection 1 month later with the purified GP. The subsequent steps were done according to the standard procedure.
RESULTS
Strain-specific infectivity-enhancing activity of Ebola virus GP antiserum.
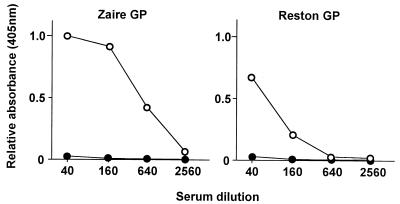
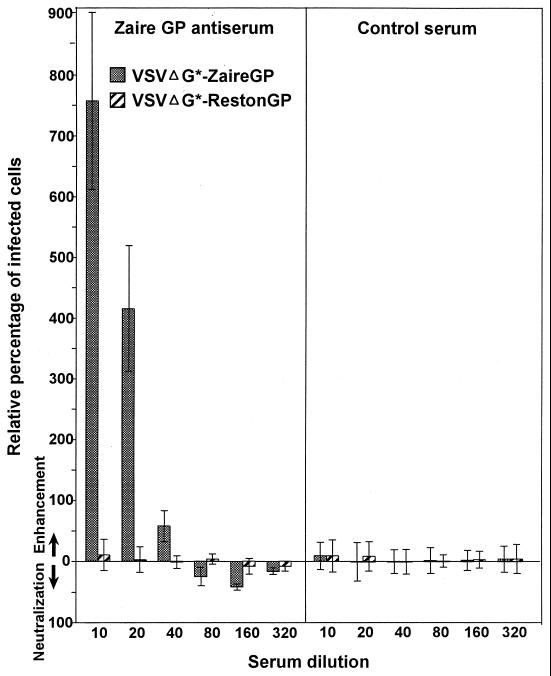
To generate antibody to the Zaire GP, we immunized mice with a plasmid expressing this protein, using in vivo electroporation. An ELISA detected Zaire GP-specific immunoglobulin G antibodies in serum samples collected from immunized animals (Fig. 1). The antibodies also bound to Reston GP, albeit to a lesser extent. We then tested the antiserum for neutralizing activity. Surprisingly, the infectivity of VSV pseudotyped with the Zaire GP (VSVΔG∗-ZaireGP) was strongly enhanced (Fig. 2); only minimal enhancement was seen with VSV pseudotyped with the Reston GP (VSVΔG∗-RestonGP). Limited neutralizing activity was observed when the serum was diluted to 1:80 or 1:160. These results suggest that specific epitopes on the GP mediate the enhancement of VSVΔG∗-ZaireGP infectivity.
FIG. 1.
Detection of Ebola virus GP-specific immunoglobulin G by ELISA. Human 293T cells transfected with pCEboZGP (Zaire GP) or pCEboRGP (Reston GP) were fixed with methanol and used as an antigen. To ensure that similar numbers of cells were GP positive in both samples, GP expression was examined by immunostaining plasmid-transfected cells using the VECTASTAIN ABC kit (Vector). Approximately 80% of plasmid-transfected cells expressed GP in both samples. The subsequent procedures were done as previously described (10). ○, Zaire GP antiserum; ●, control serum.
FIG. 2.
Infectivity-enhancing activities of Zaire GP antiserum against VSV pseudotyped with the Ebola virus GP. Each bar represents the relative percentage of infected cells (mean ± standard deviation (error bar). The number of infected cells given by normal mouse serum was set to zero. Experiments were done three times, and representative data are shown.
Antibody is responsible for infectivity-enhancing activity.
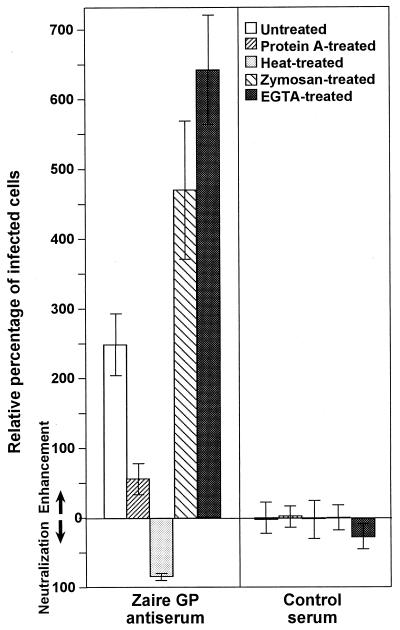
To confirm the involvement of antibody in this infectivity enhancement, we asked whether protein A, which binds the immunoglobulin Fc fragment, can interfere with the enhancing activity. As shown in Fig. 3, protein A reduced viral infectivity, supporting the hypothesis that enhancement depends on GP-specific antibodies. Several viruses elicit antibodies that enhance infectivity through binding of the virus-antibody complex to Fc receptors on cells (e.g., macrophages) via the Fc portion of immunoglobulins (4, 5, 9, 14). This mechanism likely enhances the interaction between the viral envelope protein and its receptor. However, since the human embryonic kidney 293 cells used as targets in this experiment probably lack Fc receptors (1), we suggest that interaction of anti-GP antibodies with an Fc receptor-like molecule on the cell surface is not a plausible mechanism for the enhanced infectivity of VSVΔG∗-ZaireGP.
FIG. 3.
Effects of protein A, heat treatment, and complement inhibitors on the infectivity-enhancing activity of Zaire GP antiserum. Antiserum and control serum (1:20 final dilution) were treated with heat or preincubated with protein A, zymosan, or EGTA. Other conditions and details were the same as described in the legend of Fig. 2.
The complement system is not involved in infectivity-enhancing activity by antibody.
When treated with heat (56°C, 30 min), the Zaire GP antiserum completely lost its enhancing activity, but neutralized the infectivity of VSVΔG∗-ZaireGP (Fig. 3), suggesting that heat-labile serum factors contribute to the virus's enhanced infectivity. One possibility is that the complement system, activated by antibody-GP complexes, facilitates virus entry into cells, as hypothesized for the antibody-dependent, complement-mediated enhancement of human immunodeficiency virus infection (4). However, pretreatment of the Zaire GP antiserum with zymosan and EGTA, both of which impair the complement system, did not reduce the enhancing activity; in fact, virus infectivity was further enhanced (Fig. 3). These findings strongly suggest that heat-labile factors, other than those involved in the complement system, are required for the enhancement of Ebola virus infectivity.
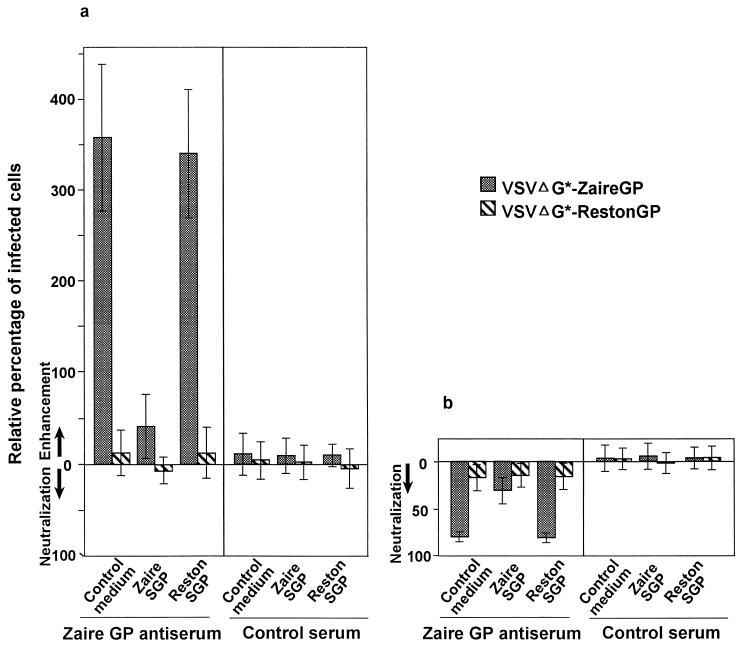
SGP shares enhancing and neutralization epitopes with GP.
We also investigated whether SGPs interfere with the enhancing and neutralizing activities of the antiserum (Fig. 4). The enhancing activity of untreated Zaire GP antiserum was reduced in the presence of Zaire SGP but not Reston SGP (Fig. 4a), confirming that epitope-specific antibodies are responsible for the enhancing activity. In the presence of Zaire SGP but not Reston SGP, the neutralizing activity of heat-treated Zaire GP antiserum was also reduced (Fig. 4b). These findings also substantiate the notion that GP molecules of different subtypes share only limited numbers of epitopes responsible for the neutralization or enhancement of viral infectivity.
FIG. 4.
Effects of SGPs on the infectivity-enhancing and neutralizing activities of Zaire GP antiserum. Untreated (a) and heat-treated (b) antisera (1:10) were incubated with Zaire or Reston SGP (5 μg/ml) or control supernatant (pCAGGS and transfected) for 30 min at room temperature and mixed with VSVΔG∗-ZaireGP or VSVΔG∗-RestonGP. Infectivity was then determined by titration on 293 cells. SGP alone did not affect virus infectivity. Error bars, standard deviations.
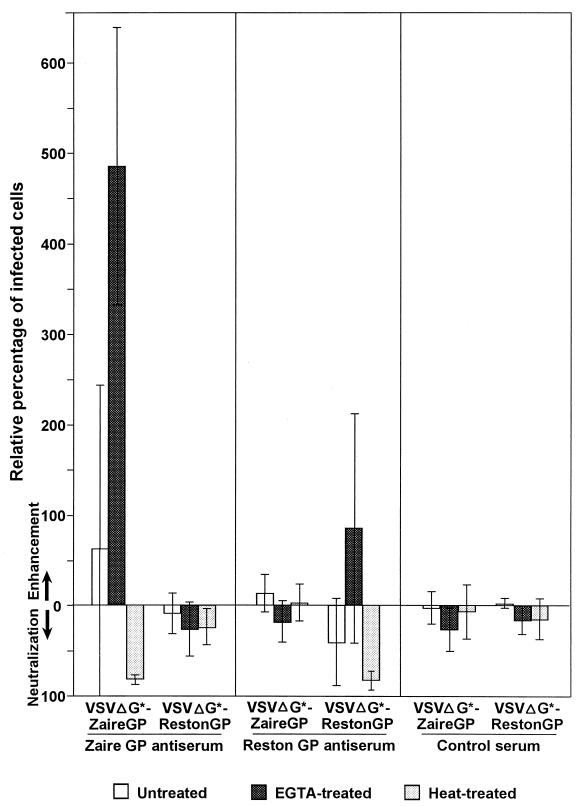
Reston GP induces less enhancing activity than does Zaire GP.
To confirm the above findings and further investigate the difference in immunogenicity between the Zaire and Reston GPs, we prepared antisera to both proteins in larger numbers of animals by gene gun immunization, a more widely used means of DNA immunization. The results (Fig. 5) were similar to those obtained by in vivo electroporation, although among the samples of Zaire and Reston GP antisera, only four of nine and two of nine, respectively, showed clear enhancing activity, resulting in a high standard deviation. This outcome could reflect lower antibody levels than were found in animals immunized by electroporation, since the enhancing activity of each mouse serum correlated with antibody levels measured by ELISA (not shown). Nevertheless, all of the Zaire GP antisera showed increased enhancing activity when treated with EGTA (Fig. 5). Only scant activity was produced by the Reston GP antisera, even after treatment with EGTA. As in the preceding experiments with electroporation, heat treatment resulted in marked neutralization of the respective viruses.
FIG. 5.
Infectivity-enhancing activities of Ebola virus GP antisera produced by gene gun immunization. Results are expressed as means ± standard deviations (error bars) for eight to nine mice. All other experimental conditions were as described in the legends of Fig. 2 and 3.
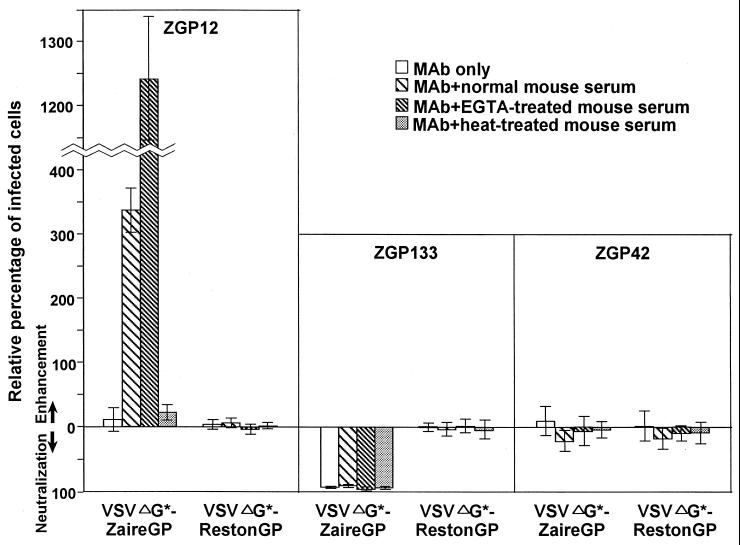
Presence of enhancing and neutralizing epitopes on GP.
To conclusively identify the presence of infectivity-enhancing epitopes on Zaire GP molecules, we generated MAbs to Zaire GP and examined their enhancing and neutralizing activities. Representative results are shown in Fig. 6. In the presence, but not the absence, of normal or EGTA-treated mouse serum, MAb ZGP12 strongly enhanced the infectivity of VSVΔG∗-ZaireGP, but neither neutralized nor enhanced that of VSVΔG∗-RestonGP. The addition of heat-treated mouse serum had no effect on the activity of ZGP12. By contrast, MAb ZGP133 neutralized VSVΔG∗-ZaireGP infectivity but not that of VSVΔG∗-RestonGP. This antibody did not enhance viral infectivity, even in the presence of EGTA-treated mouse serum. Although MAb ZGP42 failed to enhance or neutralize infectivity, it did react with the Zaire and Reston GPs in an ELISA (not shown). These findings provide compelling evidence that both neutralizing and enhancing epitopes exist on the Zaire GP molecule and that heat-labile serum factors are required for this antibody-mediated enhancing activity.
FIG. 6.
Infectivity-enhancing and neutralizing activities of monoclonal antibodies to Zaire GP. Hybridoma supernatants were pre-incubated with normal, EGTA-, or heat-treated mouse serum (10%, vol/vol) and then mixed with the viruses. All other experimental conditions were the same as described in the legend of Fig. 2.
DISCUSSION
Whether or not Ebola virus-infected animals generate neutralizing antibodies is controversial (8, 15), possibly because the coexistence of neutralizing and infectivity-enhancing antibodies in serum samples can affect the results of serologic assays, as shown in the present study. Here we show that both the neutralizing and enhancing activities of Zaire GP antiserum are reduced in the presence of Zaire SGP. Thus, in culture supernatants or patients' sera that contain large amounts of SGP (17, 20), serologic assays may not detect either neutralizing or enhancing activity. Even in the absence of SGP, the neutralizing activity could be masked by the enhancing activity or vice versa. Since DNA immunization is thought to induce an immune response similar to that of virus infection (6, 23, 24), the enhancing antibody activities observed with the Zaire GP antisera may reflect the normal responses of animals infected with Ebola virus.
The reduced pathogenicity of the Reston strain in humans, compared with those of Ebola virus Zaire or Sudan strains, lacks a satisfactory explanation. The increased cleavability of glycoproteins by furin and other ubiquitous proprotein convertases is an important determinant of pathogenicity for some viruses, including avian influenza and Newcastle disease viruses (11), and may account for the difference in virulence among Ebola viruses (22). However, since the role of Ebola virus GP cleavability in viral infectivity has not been unequivocally established (22, 27), we suggest that virulence might be affected by the capacity of the GP to induce infectivity-enhancing antibodies. While it appears that filovirus infections prohibit the induction of immune reaction, both human and nonhuman primates develop virus-specific antibodies which can be detected by immunofluorescent assay and Western blotting (3, 8). Although “data on the immune reaction during lethal outcome of Ebola and Marburg fevers are lacking in the available literature” (8), infectivity-enhancing antibodies might play a role in Ebola virus pathogenicity.
The proposed involvement of enhancing antibodies in the pathogenesis of filovirus infections may have precedent in immunization with inactivated Marburg virus antigens, which was associated with earlier deaths in immunized animals (8). Thus, our findings raise serious questions about the development of Ebola virus vaccines based on the GP. For example, induction of neutralizing antibodies that cross-react with different Ebola subtypes might prove difficult. More importantly, Ebola virus GP-based vaccines could exacerbate infections. In recent studies, DNA immunization of guinea pigs and mice with Ebola virus GP-or NP-expressing plasmids conferred protective immunity by inducing cytotoxic T-cell responses (neutralizing antibody was not detected in sera) (19, 28). Thus, attempts to develop Ebola virus vaccines should be aimed at activating specific cytotoxic T-cell responses rather than inducing antibody responses. Passive prophylaxis with Ebola virus GP antibodies should probably be restricted to neutralizing antibodies, as shown recently (25). Both the neutralizing and enhancing epitopes on GP molecules will need to be fully characterized to clarify the mechanism(s) of antibody-dependent enhancement of Ebola virus infection.
ACKNOWLEDGMENTS
We thank Michael Whitt for VSVΔG∗ virus, Anthony Sanchez for antiserum to GP/SGP, Krisna Wells and Martha McGregor for excellent technical assistance, and John Gilbert for editing the manuscript.
Support for this work came from NIAID Public Health Service research grants and from the Japan Health Sciences Foundation. S.W. is the recipient of the Japan Society for Promotion of Science Postdoctoral Fellowship for Research Abroad.
REFERENCES
- 1.Fanger M W, Guyre P M. Fc receptors. In: Roitt I M, Delves P J, editors. Encyclopedia of immunology. San Diego, Calif: Academic Press; 1992. pp. 544–549. [Google Scholar]
- 2.Feldmann H, Klenk H D, Sanchez A. Molecular biology and evolution of filoviruses. Arch Virol. 1993;7(Suppl.):81–100. doi: 10.1007/978-3-7091-9300-6_8. [DOI] [PubMed] [Google Scholar]
- 3.Fisher-Hoch S P, McCormick J B. Experimental filovirus infection. Curr Top Microbiol Immunol. 1999;235:117–143. doi: 10.1007/978-3-642-59949-1_8. [DOI] [PubMed] [Google Scholar]
- 4.Fust G. Enhancing antibodies in HIV infection. Parasitology. 1997;115(Suppl.):S127–S140. doi: 10.1017/s0031182097001819. [DOI] [PubMed] [Google Scholar]
- 5.Halstead S B, O'Rourke E J. Dengue viruses and mononuclear phagocytes. I. Infection enhancement by non-neutralizing antibody. J Exp Med. 1977;146:201–217. doi: 10.1084/jem.146.1.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hassett D E, Whitton J L. DNA immunization. Trends Microbiol. 1996;4:307–312. doi: 10.1016/0966-842x(96)10048-2. [DOI] [PubMed] [Google Scholar]
- 7.Haynes J R, McCabe D E, Swain W F, Widera G, Fuller J T. Particle-mediated nucleic acid immunization. J Biotechnol. 1996;44:37–42. doi: 10.1016/0168-1656(96)80298-7. [DOI] [PubMed] [Google Scholar]
- 8.Ignatyev G M. Immune response to filovirus infections. Curr Top Microbiol Immunol. 1999;235:205–217. doi: 10.1007/978-3-642-59949-1_11. [DOI] [PubMed] [Google Scholar]
- 9.Kanno H, Wolfinbarger J B, Bloom M E. Aleutian mink disease parvovirus infection of mink macrophages and human macrophage cell line U937: demonstration of antibody-dependent enhancement of infection. J Virol. 1993;67:7017–7024. doi: 10.1128/jvi.67.12.7017-7024.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kida H, Brown L E, Webster R G. Biological activity of monoclonal antibodies to operationally defined antigenic regions on the hemagglutinin molecule of A/Seal/Massachusetts/1/80 (H7N7) influenza virus. Virology. 1982;122:38–47. doi: 10.1016/0042-6822(82)90375-0. [DOI] [PubMed] [Google Scholar]
- 11.Klenk H-D, Garten W. Host cell proteases controlling virus pathogenicity. Trends Microbiol. 1994;2:39–43. doi: 10.1016/0966-842x(94)90123-6. [DOI] [PubMed] [Google Scholar]
- 12.Kobasa D, Rodgers M E, Wells K, Kawaoka Y. Neuraminidase hemadsorption activity, conserved in avian influenza A viruses, does not influence viral replication in ducks. J Virol. 1997;71:6706–6713. doi: 10.1128/jvi.71.9.6706-6713.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Niwa H, Yamamura K, Miyazaki J. Efficient selection for high-expression transfectants by a novel eukaryotic vector. Gene. 1991;108:193–200. doi: 10.1016/0378-1119(91)90434-d. [DOI] [PubMed] [Google Scholar]
- 14.Olsen C W, Corapi W V, Ngichabe C K, Baines J D, Scott F W. Monoclonal antibodies to the spike protein of feline infectious peritonitis virus mediate antibody-dependent enhancement of infection of feline macrophages. J Virol. 1992;66:956–965. doi: 10.1128/jvi.66.2.956-965.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peters C J, Khan A S. Filovirus diseases. Curr Top Microbiol Immunol. 1999;235:85–95. doi: 10.1007/978-3-642-59949-1_6. [DOI] [PubMed] [Google Scholar]
- 16.Peters C J, Sanchez A, Rollin P E, Ksiazek T G, Murphy F A. Filoviridae: Marburg and Ebola viruses. In: Fields B N, Knipe D M, Howley P M, editors. Fields virology. Philadelphia, Pa: Lippincott-Raven; 1995. pp. 1161–1176. [Google Scholar]
- 17.Sanchez A, Trappier S G, Mahy B W, Peters C J, Nichol S T. The virion glycoproteins of Ebola viruses are encoded in two reading frames and are expressed through transcriptional editing. Proc Natl Acad Sci USA. 1996;93:3602–3607. doi: 10.1073/pnas.93.8.3602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Takada A, Robison C, Goto H, Sanchez A, Murti K G, Whitt M A, Kawaoka Y. A system for functional analysis of Ebola virus glycoprotein. Proc Natl Acad Sci USA. 1997;94:14764–14769. doi: 10.1073/pnas.94.26.14764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vanderzanden L, Bray M, Fuller D, Roberts T, Custer D, Spik K, Jahrling P, Huggins J, Schmaljohn A, Schmaljohn C. DNA vaccines expressing either the GP or NP genes of Ebola virus protect mice from lethal challenge. Virology. 1998;246:134–144. doi: 10.1006/viro.1998.9176. [DOI] [PubMed] [Google Scholar]
- 20.Volchkov V E. Processing of the Ebola virus glycoprotein. Curr Top Microbiol Immunol. 1999;235:35–47. doi: 10.1007/978-3-642-59949-1_3. [DOI] [PubMed] [Google Scholar]
- 21.Volchkov V E, Becker S, Volchkova V A, Ternovoj V A, Kotov A N, Netesov S V, Klenk H D. GP mRNA of Ebola virus is edited by the Ebola virus polymerase and by T7 and vaccinia virus polymerases. Virology. 1995;214:421–430. doi: 10.1006/viro.1995.0052. [DOI] [PubMed] [Google Scholar]
- 22.Volchkov V E, Feldmann H, Volchkova V A, Klenk H D. Processing of the Ebola virus glycoprotein by the proprotein convertase furin. Proc Natl Acad Sci USA. 1998;95:5762–5767. doi: 10.1073/pnas.95.10.5762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Webster R G. Potential advantages of DNA immunization for influenza epidemic and pandemic planning. Clin Infect Dis. 1999;28:225–229. doi: 10.1086/515123. [DOI] [PubMed] [Google Scholar]
- 24.Whitton J L, Rodriguez F, Zhang J, Hassett D E. DNA immunization: mechanistic studies. Vaccine. 1999;17:1612–1619. doi: 10.1016/s0264-410x(98)00418-6. [DOI] [PubMed] [Google Scholar]
- 25.Wilson J A, Hevey M, Bakken R, Guest S, Bray M, Schmaljohn A L, Hart M K. Epitopes involved in antibody-mediated protection from Ebola virus. Science. 2000;287:1664–1666. doi: 10.1126/science.287.5458.1664. [DOI] [PubMed] [Google Scholar]
- 26.Wool-Lewis R J, Bates P. Characterization of Ebola virus entry by using pseudotyped viruses: identification of receptor-deficient cell lines. J Virol. 1998;72:3155–3160. doi: 10.1128/jvi.72.4.3155-3160.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wool-Lewis R J, Bates P. Endoproteolytic processing of the Ebola virus envelope glycoprotein: cleavage is not required for function. J Virol. 1999;73:1419–1426. doi: 10.1128/jvi.73.2.1419-1426.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Xu L, Sanchez A, Yang Z Y, Zaki S R, Nabel E G, Nichol S T, Nabel G J. Immunization for Ebola virus infection. Nat Med. 1998;4:37–42. doi: 10.1038/nm0198-037. [DOI] [PubMed] [Google Scholar]
- 29.Yang Z Y, Delgado R, Xu L, Todd R F, Nabel E G, Sanchez A, Nabel G J. Distinct cellular interactions of secreted and transmembrane Ebola virus glycoproteins. Science. 1998;279:1034–1037. doi: 10.1126/science.279.5353.1034. [DOI] [PubMed] [Google Scholar]