Abstract
Background
Antibiotic resistance (ABR) poses a major burden to global health and economic systems. ABR in community-acquired urinary tract infections (CA-UTIs) has become increasingly prevalent. Accurate estimates of ABR’s clinical and economic burden are needed to support medical resource prioritization and cost-effectiveness evaluations of urinary tract infection (UTI) interventions.
Objective
This study aims to systematically synthesize the evidence on the economic costs associated with ABR in CA-UTIs, using published studies comparing the costs of antibiotic-susceptible and antibiotic-resistant cases.
Methods
We searched the PubMed, Ovid MEDLINE and Embase, Cochrane Review Library, and Scopus databases. Studies published in English from January 1, 2008, to January 31, 2023, reporting the economic costs of ABR in CA-UTI of any microbe were included. Independent screening of titles/abstracts and full texts was performed based on prespecified criteria. A quality assessment was performed using the Integrated Quality Criteria for Review of Multiple Study Designs (ICROMS) tool. Data in UTI diagnosis criteria, patient characteristics, perspectives, resource costs, and patient and health economic outcomes, including mortality, hospital length of stay (LOS), and costs, were extracted and analyzed. Monetary costs were converted into 2023 US dollars.
Results
This review included 15 studies with a total of 57,251 CA-UTI cases. All studies were from high- or upper-middle-income countries. A total of 14 (93%) studies took a health system perspective, 13 (87%) focused on hospitalized patients, and 14 (93%) reported UTI pathogens. Escherichia coli, Klebsiella pneumoniae, and Pseudomonas aeruginosa are the most prevalent organisms. A total of 12 (80%) studies reported mortality, of which, 7 reported increased mortality in the ABR group. Random effects meta-analyses estimated an odds ratio of 1.50 (95% CI 1.29-1.74) in the ABR CA-UTI cases. All 13 hospital-based studies reported LOS, of which, 11 reported significantly higher LOS in the ABR group. The meta-analysis of the reported median LOS estimated a pooled excess LOS ranging from 1.50 days (95% CI 0.71-4.00) to 2.00 days (95% CI 0.85-3.15). The meta-analysis of the reported mean LOS estimated a pooled excess LOS of 2.45 days (95% CI 0.51‐4.39). A total of 8 (53%) studies reported costs in monetary terms—none discounted the costs. All 8 studies reported higher medical costs spent treating patients with ABR CA-UTI in hospitals. The highest excess cost was observed in UTIs caused by carbapenem-resistant Enterobacterales. No meta-analysis was performed for monetary costs due to heterogeneity.
Conclusions
ABR was attributed to increased mortality, hospital LOS, and economic costs among patients with CA-UTI. The findings of this review highlighted the scarcity of research in this area, particularly in patient morbidity and chronic sequelae and costs incurred in community health care. Future research calls for a cost-of-illness analysis of infections, standardizing therapy-pathogen combination comparators, medical resources, productivity loss, intangible costs to be captured, and data from community sectors and low-resource settings and countries.
Introduction
Urinary tract infections (UTIs) are infections of the kidneys, bladder, or urethra defined by a combination of clinical features and the presence of bacteria in urine. These are some of the most common conditions managed in primary care, with approximately 75% of women experiencing at least one episode in their lifetime [1]. Consequently, UTIs are the second most common reason for primary care antibiotic prescribing in England [2,3]. However, it is estimated that up to 50% of these prescriptions were inadequate [4,5]. If managed inappropriately, in cases such as undertreating, subsequent sequelae include recurrent infections, bacteremia, sepsis, and potential mortality [2]. In addition, inappropriate management of UTIs, including overusing antibiotics (ie, using antibiotics when not required or for prolonged durations), accelerates the emergence and transmission of antibiotic resistance (ABR) in the long-term [6]. An increasing level of ABR in the community poses challenges to infection due to the higher risk of first-line antibiotic regime failure [7]. In the United Kingdom, the susceptibility of Escherichia coli’s (E coli), the most common cause of UTIs, to first-line treatments of trimethoprim and nitrofurantoin is declining [8]. This may have resulted in a rise in bacteremia caused by drug-resistant Gram-negative bacteria (GNB), as over 40% of E coli bacteremia had a urinary source [9].
Drug-resistant UTIs impose an economic burden on individuals, health care systems, and society as a whole [10-13]. The reduced effectiveness of UTI antibiotics can lead to repeated and more extensive treatment, hospital admission and prolonged length of stay (LOS), increased medical costs, and mortality [14]. The UK government has set new commitments in the National Action Plan to improve the prevention and control of UTIs in the community, particularly for older adults, and to gain a better understanding of the economic impacts of ABR [15]. Despite the high prevalence of UTIs in the community, evidence of the financial and human costs associated with drug-resistant UTIs is scarce, particularly due to the difficulties in quantifying costs incurred outside secondary care [11]. An understanding of the clinical and economic burden of antibiotic-resistant UTIs is key to evaluating the cost-effectiveness of stewardship interventions, including those aimed at using point-of-care diagnosis, clinical decision support tools, and reducing prescribing in the community [16]. In this research, we sought to systematically synthesize the evidence on the economic burden associated with antibiotic-resistant community-acquired UTIs (CA-UTIs), using published studies comparing the costs of antibiotic-susceptible and antibiotic-resistant cases.
Methods
This systematic review followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidance [17] and was registered at PROSPERO (CRD42023374551).
Search Methods
We searched for studies estimating the economic costs attributable to antibiotic drug-resistant CA-UTIs published from January 1, 2008, to January 31, 2023, using a combination of broad-based (and wildcard) search criteria, including terms for UTI, community-acquired, ABR, and health economic cost. We searched the PubMed, Ovid MEDLINE and Embase, Cochrane Review Library, and Scopus databases using strings developed for each database (Table S2 in Multimedia Appendix 1). The bibliographies of the identified studies were also reviewed.
Study Selection
The study inclusion/exclusion criteria are presented in Table 1, including the Patient/Population, Intervention, Comparison, and Outcomes (PICO) eligibility. Two authors (NJZ and MW) independently screened the titles and abstracts of the records yielded from the database search and independently screened the full-text articles. The discrepancies during title/abstract screening and full-text screening were resolved by consulting the third author (EC). Any article comparing monetary or health economic costs of antibiotic-resistant versus susceptible CA-UTIs through clinical trials, observational designs (eg, cohort study, case-control study), or modeling approaches was included for full-text review.
Table 1. Study inclusion/exclusion criteria.
| Criteria | Inclusion | Exclusion | |
| Article type |
|
|
|
| Language |
|
|
|
| PICOa eligibility | |||
| Population |
|
|
|
| Intervention/exposure |
|
|
|
| Comparison/control |
|
|
|
| Outcomes |
|
|
|
PICO: Patient/Population, Intervention, Comparison, and Outcomes.
Data Extraction and Analysis
Data were extracted from the included studies, including study identifier, authors, journal, publication year, study design, data collection period, country/region, health care setting, perspective (patient, health system [representing payer or provider], or societal), patient population, number of patients, UTI diagnosis criteria, pathogen, sensitivity profile, treatment, and outcome. We synthesized the impact of ABR on health outcomes (eg, mortality), health care system (eg, hospital LOS, medication cost), and economic system (eg, productivity), and compared these for infections caused by resistant versus susceptible pathogens. The methods to estimate the cost of illness were categorized using a top-down approach for those studies that reported total costs on a population level irrespective of the specific method used to derive these costs or a bottom-up approach for those studies that reported average costs derived from accumulating measured costs from patient samples.
A meta-analysis was performed to synthesize the reported mortality and hospital LOS using a random effect model [18]. A random effects model assumes that the true effect size of the exposure varies from study to study due to study heterogeneity. Particularly, heterogeneities in this type of analysis occurred in definitions and categories of costs across health systems, settings, and disease types; cost measurement instruments; and unit prices. Thus, a random effects model was chosen to allow aggregating cost data from different studies by circumventing this heterogeneity. In the meta-analysis of mortality, we estimated pooled odds ratios based on the crude mortality rate [19]. In the meta-analysis of LOS, we applied both the transformation-based methods (ie, estimating the sample mean and SD from the median and sample size) [20,21] and median-based methods (ie, considering study-specific median differences and data distribution) [22], considering mean and variance and median and IQR were commonly used when reporting LOS, and the distribution of LOS was heavily right-tailed (eg, not normally distributed) [23,24]. We assessed the publication bias for the mortality outcome using a funnel plot and Egger test [25,26]. No meta-analysis was performed for economic costs due to the large variation in the resource costs and the methods used to determine the cost. To compare the reported monetary costs, the outcomes were converted into 2023 US dollars by inflating the cost to 2023 original currency estimates using annual inflation rates [27], then converting this into US dollars utilizing the 2023 average exchange rates [28].
Quality Assessment
The included studies were assessed using the Integrated Quality Criteria for Review of Multiple Study Designs (ICROMS) tool [29].
Results
Study Characteristics
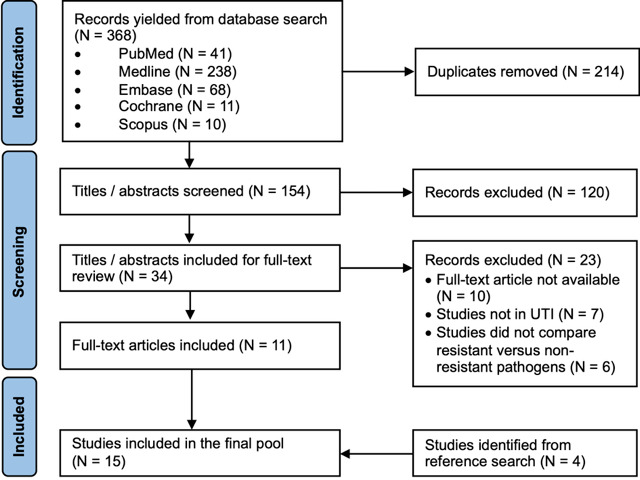
A total of 380 titles and abstracts were yielded from the database search; 214 duplicates were removed, and 132 abstracts were deemed irrelevant. A full-text review was performed on 34 studies, of which, 11 studies were included. Through reference search, another 4 studies were identified and included in the final study pool. Figure 1 summarizes the screening process in a PRISMA flowchart.
Figure 1. PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart. UTI: urinary tract infection.
The characteristics of the 15 identified studies are presented in Table 2 [12-14,30-41,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined]. The countries that individually produced the highest number of studies were the United States (n=5, 33%) [14,33,38,39,41], followed by Spain (n=3, 20%) [13,32,40] and South Korea (n=2, 13%) [30,36]. A total of 13 (87%) studies focused on patients who were hospitalized [12-14,30,32-36,38-41,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined], and 2 (13%) studies focused on primary care patients [31,37]. Additionally, 13 (87%) studies included adult patients of all genders [12-14,32-41,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined], of which, 1 study included patients 65 years and older [32]. Chang et al [30] and Little et al [31] (n=2, 13%) investigated adult female patients. All hospital-based studies had UTI diagnosed via the presence of symptoms, infection biomarkers, and microbiology culture confirmation, and differentiated community-acquired cases using the 48-hour cutoff time after admission. Two (13%) studies reported hospital-acquired UTI [14,39]. The community-based study recruited patients with urinary tract symptoms (suspected UTI) or a history of dysuria and frequency [31,37]. In total, 57,251 CA-UTI cases were reported, and 47,131 UTI cases were analyzed (Table S3 in Multimedia Appendix 1).
Table 2. Study characteristics: data collection period, patient population, and identified pathogens.
| Study | Country | Period | Population | Organisms identified | ||
| Gram-negative | Gram-positive | Fungi | ||||
| Chang et al [30], 2016 | South Korea | January 2001-December 2010 | Hospitalized female patients with COa-APNb defined by presence of fever (≥38.0 °C), pyuria (5‐10 leukocytes per HPFc upon urine microscopic examination), bacteriuria (≥105/ml clean voided urine or ≥104/ml catheterized urine) |
|
—d | — |
| Sozen et al [12], 2015 | Turkey | July 2012-June 2014 | Hospitalized patients with positive urine culture <48 hours after admission, without hospitalization or urological surgery during the last month |
|
— | — |
| Little et al [31], 2009 | UK | April 2002-May 2003 | Female patients aged 17‐70 years recruited from primary care practices with suspected UTIe or a history of dysuria and frequency |
|
Not reported | Not reported |
| Tabak et al [14], 2018 | US | January 2013-September 2015 | Hospitalized adult patients with urine culture <3 days after admission, with Gram-negative pathogens isolated and tested for carbapenem susceptibility |
|
— | — |
| Madrazo et al [32], 2021 | Spain | January 2016-December 2019 | Hospitalized patients aged ≥65 years with CAf-UTI and positive urine culture |
|
|
Candida spp |
| Wozniak et al [34], 2022 | Australia | January 2012-September 2016 | Hospitalized patients with positive urine culture <48 hours after admission with >2 species identified (>105 CFUsg/ml, 103/ml for cystitis, 104/ml for pyelonephritis) |
|
|
|
| Zilberberg et al [41], 2017 | US | 2009-2013 | Hospitalized adult patients aged ≥18 years with CO-UTI defined by ICD-9h code, positive urine culture, and antibiotic treatment beginning <48 hours after admission and continuing for at least 3 consecutive days or until discharge |
|
— | — |
| Mark et al [33], 2021 | US | January 2017-June 2019 | Hospitalized patients aged ≥18 years with febrile UTI defined by fever, ICD-10i code of UTI, pyelonephritis, or sepsis, urine culture (EKP species >100,000 CFUs/ml) |
|
— | — |
| Kim et al [36], 2013 | South Korea | March 2010-February 2011 | Hospitalized patients admitting emergency department or outpatient clinic from the community with CA-APN defined by pyuria (≥5‐9 WBCj/HPF), fever (≥37.8 °C), and positive urine culture collected at the time of admission |
|
|
— |
| François et al [37], 2016 | France | January 2012-February 2013 | Female patients aged >18 years recruited from GPsk with UTI symptoms and followed up for 8 weeks |
|
— | — |
| Cheong et al [35], 2022 | Korea | January 2018-December 2019 | Hospitalized patients aged ≥19 years with ICD-10 code of CA-APN <48 hours after admission, defined by fever (≥37.8 °C), pyuria (≥4‐9 WBC/HPF), positive urine or blood culture, and symptoms or signs relevant to APN |
|
— | — |
| MacVane et al [38], 2013 | US | September 2011-August 2012 | Hospitalized patients aged ≥18 years with UTI present ≤48 hours after admission defined by positive urine culture (≥10,000 CFUs) |
|
— | — |
| Esteve-Palau et al [13], 2015 | Spain | August 2010-July 2013 | Hospitalized patients aged ≥18 years with symptomatic CA- or CO-HAl-UTI ≤48 hours after admission including cystitis, pyelonephritis, acute prostatitis, and urosepsis, defined by increases in urinary frequency, urgency, dysuria, or suprapubic tenderness, a positive urine culture of Escherichia coli (>105 CFUs/ml) |
|
— | — |
| Rozenkiewicz et al [40], 2021 | Spain | January 2011-January 2016 | Hospitalized patients aged ≥18 years with symptomatic CA-UTI (identified ≤48 hours after admission and not AHAm) including cystitis, pyelonephritis, acute prostatitis, urinary sepsis, and confusion state associated with UTI, defined by fever (>38 °C), urinary urgency, polyuria, dysuria or suprapubic pain, a positive urine culture (>105 CFUs/ml) |
|
— | — |
| Cardwell et al [39], 2016 | US | July 2013-September 2013 | Hospitalized patients aged ≥18 years with fever, chills, rigors, nausea, or vomiting; hematuria; altered mental status; suprapubic or flank pain; costovertebral angle tenderness; urinary frequency, urgency, or dysuria; and treatment for UTI ≤24 hours after admission |
|
|
— |
CO: community-onset.
APN: acute pyelonephritis.
HPF: high-power field.
Not applicable.
UTI: urinary tract infection.
CA: community-acquired.
CFU: colony-forming unit.
ICD-9: International Classification of Diseases, Ninth Revision.
ICD-10: International Statistical Classification of Diseases, Tenth Revision.
WBC: white blood cell.
GP: general practice.
HA: hospital-acquired.
AHA: ambulatory health care associated.
Of the 15 studies, 14 (93%) reported the pathogens identified, of which, all reported GNB [12-14,30-41,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined], 4 (29%) reported Gram-positive bacteria [32,34,36,39], 1 (7%) reported fungi [32], 3 (21%) exclusively reported UTI caused by E coli [13,30,37], 1 (7%) reported UTI caused by K pneumoniae [40]. E coli, K pneumoniae, and P aeruginosa are the most frequently identified organisms. Among the studies in specific antibiotic-pathogen combinations, 2 studies assessed carbapenem-resistant organisms, specifically GNB and Enterobacterales [14,41]. Mark et al [33] examined E coli, K pneumoniae, and Proteus mirabilis (P mirabilis) resistance to third-generation cephalosporins. Sozen et al [12] and MacVane et al [38] examined extended-spectrum β-lactamases– or inducible β-lactamases–producing GNB.
All the included studies estimated the clinical and economic outcomes of patients recruited from single or multiple health facilities. François et al [37] provided a national-level estimate of the infection incidence and costs derived from the study cohort. No study performed sensitivity analysis. The results of the quality assessment are presented in Table S5 in Multimedia Appendix 1. All studies met the minimum required score. Of the 15 studies, 6 (40%) failed to meet the minimum required criteria [13,30,37,38,40,41].
The Burden of ABR UTIs
When quantifying the burden attributable to ABR, the included studies compared patient outcomes, health system outcomes, and economic costs of the CA-UTI cases caused by resistant pathogens against those caused by nonresistant pathogens. The most reported outcomes were mortality, hospital LOS, and economic costs due to antibiotic treatment (Table S4 in Multimedia Appendix 1). A health system perspective was taken by all except 1 study when estimating the costs [12-14,30-41,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined]. François et al [37] took a societal perspective and included productivity loss due to absenteeism. When comparing the patients with resistant and nonresistant CA-UTIs, 4 studies matched case and control [13,14,38,41], 2 studies adjusted patient characteristics and other risk factors when reporting outcomes [33,35], other studies performed no matching or adjusting.
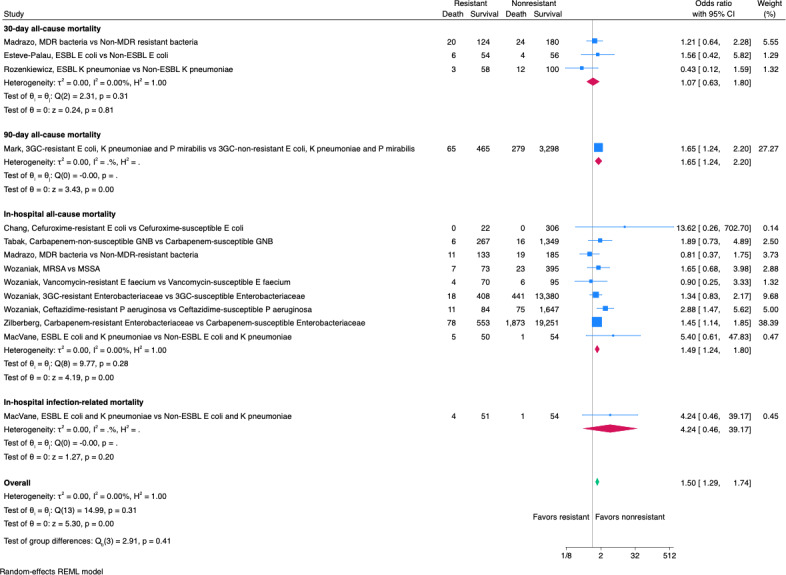
A total of 12 studies reported mortality, including in-hospital all-cause mortality [14,30,32,34,38,41], in-hospital infection-related mortality [38], 30-day all-cause mortality [13,32,40], and 90-day all-cause mortality [33] (Table S4 A in Multimedia Appendix 1). A total of 7 studies reported higher crude mortality among the patients with antibiotic-resistant UTIs [13,14,32-34,38,41,undefined,undefined], of which, 1 study demonstrated the statistical significance [41]. The pooled odds ratios of mortality outcomes for resistant UTIs are presented in Figure 2. Results presented odds ratios of resistant compared to nonresistant infections. The blue squares centered at the point estimate the effect size, with horizontal lines depicting the 95% CIs, and the sizes of the blue squares correspond to the patient group sizes. The overall effect sizes are represented by diamonds centered on their estimated values with the diamond width corresponding to the CI length. The random effects model estimated an overall odds ratio of 1.50 (95% CI 1.29-1.74), suggesting that ABR increased the overall mortality. The subgroup analysis conducted for different mortality outcomes suggested increased odds of in-hospital all-cause mortality (Figure 2). No publication bias was detected for mortality (Figure S1 in Multimedia Appendix 1).
Figure 2. Pooled mortality of urinary tract infections [13,14,30,32-34,undefined,undefined,38,40,41,undefined]. 3GC: third-generation cephalosporin-resistant; ESBL: extended-spectrum β-lactamase; GNB: Gram-negative bacteria; MDR: multidrug resistant; MRSA: methicillin-resistant Staphylococcus aureus; MSSA: methicillin-sensitive Staphylococcus aureus.
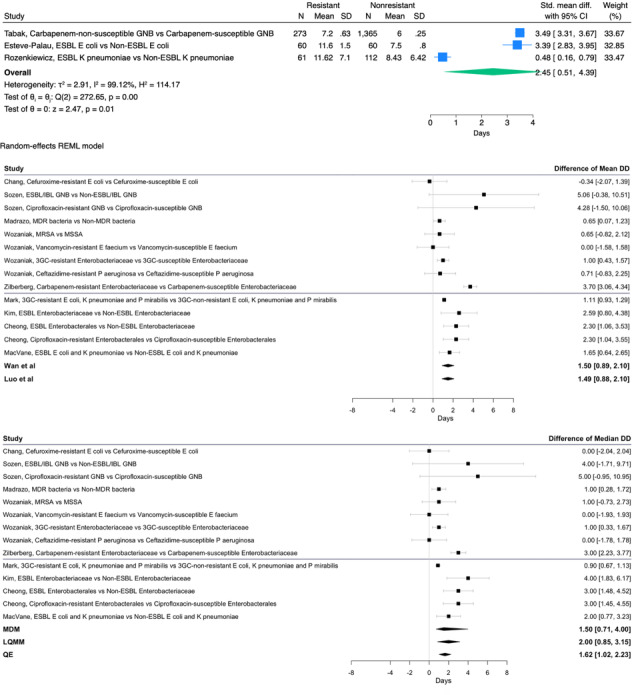
All 13 hospital-based studies reported LOS [12-14,30,32-36,38-41,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined,undefined], among which, 11 reported significantly higher LOSs associated with antibiotic-resistant UTIs (Table S4 B in Multimedia Appendix 1) [12-14,32-36,38,40,41,undefined,undefined,undefined,undefined,undefined,undefined]. Cardwell et al [39] reported higher LOS among patients with clinical failure due to inappropriate antibiotic therapies for resistant infections. The meta-analysis of studies reported LOS in mean and SD estimates of a pooled excess LOS of 2.45 days (95% CI 0.51‐4.39; Figure 3A). The meta-analysis of studies reported LOS in median and IQR estimates of a pooled excess LOS, ranging from the lowest value of 1.50 days (95% CI 0.71-4.00), estimated by the median of the differences of medians method, to the highest value of 2.00 days (95% CI 0.85-3.15), estimated by the linear quantile mixed models method (Figure 3A).
Figure 3. (A) Pooled mean difference in length of stay of urinary tract infections. (B) Pooled median difference in length of stay of urinary tract infections [12-14,20,21,30,32-36,undefined,undefined,undefined,undefined,38,40,41]. 3GC: third-generation cephalosporin-resistant; ESBL: extended-spectrum β-lactamase; GNB: Gram-negative bacteria; IBL: inducible β-lactamase; LQMM: linear quantile mixed model; MDM: median of the differences of medians; MDR: multidrug resistant; MRSA: methicillin-resistant Staphylococcus aureus; MSSA: methicillin-sensitive Staphylococcus aureus; QE: test for residual heterogeneity; REML: restricted or residual maximum likelihood.
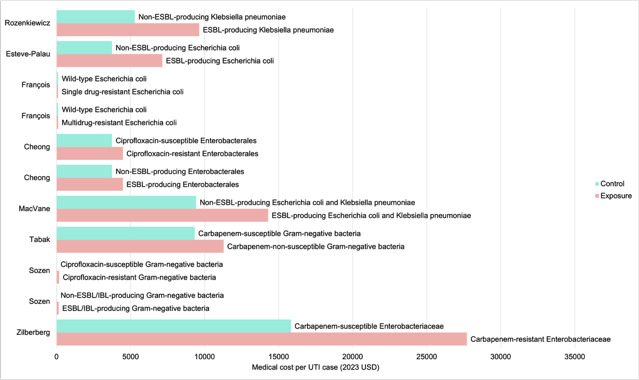
A total of 8 studies reported costs in monetary terms (Table S4 C in Multimedia Appendix 1) [12-14,35,37,38,40,41,undefined,undefined], including 5 that reported costs in US dollars [12,14,35,38,41] and 3 that reported costs in euros [13,37,40] (Figure 4). None of the included studies discounted the costs. Considering only 2 studies explicitly stated the year of which the costs were adjusted to [12,37], the end year of the data collection period was used to convert the reported costs into 2023 US dollars. A total of 8 studies reported direct medical costs incurred in secondary care, including emergency department costs [13,33] and outpatient parenteral antibiotic therapy costs in 1 study [13,33]. All 8 studies reported higher medical costs spent treating patients with resistant UTIs in hospitals. The highest excess cost was observed in UTIs caused by carbapenem-resistant Enterobacterales [41]. François et al [37] reported costs incurred in primary care, specifically, the costs of GP visits due to UTI symptoms. The primary care costs of single- or multidrug-resistant E coli UTIs were not significantly higher than those caused by susceptible E coli.
Figure 4. Medical cost of antibiotic-resistant urinary tract infections [12-14,35,37,38,40,41]. ESBL: extended-spectrum β-lactamase; IBL: inducible β-lactamase; UTI: uniary tract infection.
Discussion
This review concluded that there is an economic burden attributable to ABR in CA-UTIs, including the costs for patients and health systems as well as costs at the societal level. The review included 15 studies, which were overrepresented by research from high-income countries, hospital settings, and infections caused by E coli and K pneumoniae. All studies were cross-sectional with a limited patient sample size. No sensitivity analysis was performed to quantify the level of uncertainty in the results. The meta-analysis provided pooled estimates of the odds ratio of mortality and mean differences in hospital LOS. The reported variation in economic costs was also synthesized.
We found that no systematic review on the economic burden of ABR in CA-UTIs had been conducted. The increased mortality among the patients with ABR CA-UTIs in this review was less profound, as opposed to the existing research in other types of infections, such as bacteremia [40-42] or health care–associated UTIs [43]. Overall, ABR is attributed to an increased mortality odds ratio of 1.50. The increased odds of mortality can be explained by the higher risk of treatment failure and UTI complications such as bacteremia and sepsis. The varied types of mortality outcomes reported reduced the comparability across studies. Most of the hospital-based studies reported a longer LOS experienced by the patients in the ABR group. We used multiple modeling methods for the hospital LOS meta-analysis and estimated that the excess duration of hospitalization ranged from 1.50 to 2.45 days. All the studies that captured the costs in monetary terms reported excess medical costs in the ABR group, with the highest excess medical costs being US $11,884.32 per case of CA-UTI caused by carbapenem-resistant Enterobacterales [42,43]. The findings of this review highlighted the scarcity of research in quantifying the economic burden of ABR, particularly in four areas. First, besides mortality, evidence of other types of patient burden associated with ABR is lacking, such as morbidity (clinical failure, time to clinical stability, secondary infections) and chronic sequelae (recurrent infections). Second, existing research has been restricted to those cases present in the hospitals; the cases managed and the costs incurred in primary care settings were not captured. However, the pathogen distributions and treatment options varied substantially for hospital-acquired and CA-UTIs, and for CA-UTIs managed in the community and in hospitals; community-based investigation is urgently needed to generate a comprehensive understanding across the whole health economy [42,43]. Third, the types of medical resource costs remained largely inconsistent, which further reduced the validity of the excess costs estimated. Last, all the identified studies were limited in patient cohort size and follow-up duration and lacked analysis to address uncertainty, which led to concerns about the results’ generalizability.
This review has two limitations. First, we only searched for studies published in English. Second, we did not include those studies where the primary focus was to perform an economic evaluation of CA-UTI treatment or prevention measures and the included estimated costs of drug-resistant cases. These limitations provide scope for further research.
There is a pressing need to build an understanding of the economics of AMR. The evidence to provide a full economic case for interventions tackling AMR is lacking. In this review, we identified knowledge and methodological gaps in existing research particularly relevant to quantifying costs associated with ABR that occurred in the community. Future research calls for cost-of-illness analysis of infections standardizing therapy-pathogen combination comparators, medical resources, productivity loss, and intangible costs to be captured, as well as data from community sectors and low-resource settings and countries.
supplementary material
Acknowledgments
This research was funded by the National Institute for Health Research (NIHR) Health Protection Research Unit in Healthcare Associated Infections and Antimicrobial Resistance at Imperial College London in partnership with the UK Health Security Agency (previously Public Health England), in collaboration with Imperial College Health Partner, University of Cambridge, University of Warwick, and the Department of Health and Social Care, who funded Centre for Antimicrobial Optimisation at Imperial College London. AH is an NIHR senior investigator. PA is supported by the NIHR Applied Research Collaboration Northwest London. This report is independent research funded by the NIHR.
The authors want to thank Hossam W Almadhoon for his help with the assessment of publication bias.
The lead author affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as originally planned (and, if relevant, registered) have been explained.
Abbreviations
- ABR
antibiotic resistance
- CA-UTI
community-acquired urinary tract infection
- GNB
Gram-negative bacteria
- ICROMS
Integrated Quality Criteria for Review of Multiple Study Designs
- LOS
length of stay
- PICO
Patient/Population, Intervention, Comparison, and Outcomes
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- UTI
urinary tract infection
The views expressed in this publication are those of the authors and not necessarily those of the National Health Service, the NIHR, the Department of Health and Social Care, or the UK Health Security Agency.
Footnotes
Authors’ Contributions: NJZ and PA developed the concept and methodology for this research. NJZ and MW undertook the literature search, screening, and data extraction. NJZ conducted the meta-analysis. NJZ, MW, and EC performed the quality assessment. NJZ drafted the initial manuscript. NJZ, EC, MW, CB, AH, and PA contributed toward the data interpretation, revision of the manuscript, and finalization for submission. PA is the guarantor of the study. The corresponding author attests that all listed authors meet the International Committee of Medical Journal Editors criteria for authorship and that no others who meet the criteria have been omitted.
Data Availability: All data generated or analyzed during this study are included in this published article and Multimedia Appendix 1. Additional information about this review can be found on PROSPERO (CRD42023374551).
Contributor Information
Nina Jiayue Zhu, Email: jiayue.zhu09@imperial.ac.uk.
Misghina Weldegiorgis, Email: m.weldegiorgis@imperial.ac.uk.
Emma Carter, Email: e.carter21@imperial.ac.uk.
Colin Brown, Email: colin.brown@ukhsa.gov.uk.
Alison Holmes, Email: Alison.holmes@imperial.ac.uk.
Paul Aylin, Email: p.aylin@imperial.ac.uk.
References
- 1.Urinary tract infection (lower) - women. Clinical knowledge summaries (CKS) National Institute for Health and Care Excellence. [14-10-2023]. https://cks.nice.org.uk/topics/urinary-tract-infection-lower-women/ URL. Accessed.
- 2.Gharbi M, Drysdale JH, Lishman H, et al. Antibiotic management of urinary tract infection in elderly patients in primary care and its association with bloodstream infections and all cause mortality: population based cohort study. BMJ. 2019 Feb 27;364:l525. doi: 10.1136/bmj.l525. doi. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shallcross L, Rockenschaub P, Blackburn R, Nazareth I, Freemantle N, Hayward A. Antibiotic prescribing for lower UTI in elderly patients in primary care and risk of bloodstream infection: a cohort study using electronic health records in England. PLoS Med. 2020 Sep 21;17(9):e1003336. doi: 10.1371/journal.pmed.1003336. doi. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Woodford HJ, George J. Diagnosis and management of urinary tract infection in hospitalized older people. J Am Geriatr Soc. 2009 Jan;57(1):107–114. doi: 10.1111/j.1532-5415.2008.02073.x. doi. Medline. [DOI] [PubMed] [Google Scholar]
- 5.Menting SGP, Redican E, Murphy J, Bucholc M. Primary care antibiotic prescribing and infection-related hospitalisation. Antibiotics (Basel) 2023 Nov 30;12(12):1685. doi: 10.3390/antibiotics12121685. doi. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.UK Health Security Agency English surveillance programme for antimicrobial utilisation and resistance (ESPAUR): report 2021 to 2022. GOV.UK. 2022. [16-09-2024]. https://assets.publishing.service.gov.uk/media/65cf498ee1bdec001132225c/ESPAUR-report-2022-to-2023.pdf URL. Accessed.
- 7.Lishman H, Costelloe C, Hopkins S, et al. Exploring the relationship between primary care antibiotic prescribing for urinary tract infections, Escherichia coli bacteraemia incidence and antimicrobial resistance: an ecological study. Int J Antimicrob Agents. 2018 Dec;52(6):790–798. doi: 10.1016/j.ijantimicag.2018.08.013. doi. Medline. [DOI] [PubMed] [Google Scholar]
- 8.Kahlmeter G, Åhman J, Matuschek E. Antimicrobial resistance of Escherichia coli causing uncomplicated urinary tract infections: a European update for 2014 and comparison with 2000 and 2008. Infect Dis Ther. 2015 Dec;4(4):417–423. doi: 10.1007/s40121-015-0095-5. doi. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bou-Antoun S, Davies J, Guy R, Johnson AP, Sheridan EA, Hope RJ. Descriptive epidemiology of Escherichia coli bacteraemia in England, April 2012 to March 2014. Euro Surveill. 2016 Sep 1;21(35):30329. doi: 10.2807/1560-7917.ES.2016.21.35.30329. doi. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Öztürk R, Murt A. Epidemiology of urological infections: a global burden. World J Urol. 2020 Nov;38(11):2669–2679. doi: 10.1007/s00345-019-03071-4. doi. Medline. [DOI] [PubMed] [Google Scholar]
- 11.Yang X, Chen H, Zheng Y, Qu S, Wang H, Yi F. Disease burden and long-term trends of urinary tract infections: a worldwide report. Front Public Health. 2022 Jul 27;10:888205. doi: 10.3389/fpubh.2022.888205. doi. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sozen H, Caylak S, Cetinkaya M, et al. Clinical and economic outcomes associated with urinary tract infections caused by extended spectrum beta-lactamase producing bacteria in a tertiary care hospital. Stud Ethno Med. 2015 Aug;9(9):173–179. doi: 10.1080/09735070.2015.11905432. doi. [DOI] [Google Scholar]
- 13.Esteve-Palau E, Solande G, Sánchez F, et al. Clinical and economic impact of urinary tract infections caused by ESBL-producing Escherichia coli requiring hospitalization: a matched cohort study. J Infect. 2015 Dec;71(6):667–674. doi: 10.1016/j.jinf.2015.08.012. doi. Medline. [DOI] [PubMed] [Google Scholar]
- 14.Tabak YP, Sung AH, Ye G, Vankeepuram L, Gupta V, McCann E. Attributable clinical and economic burden of carbapenem-non-susceptible gram-negative infections in patients hospitalized with complicated urinary tract infections. J Hosp Infect. 2019 May;102(1):37–44. doi: 10.1016/j.jhin.2018.11.018. doi. Medline. [DOI] [PubMed] [Google Scholar]
- 15.Department of Health and Social Care UK 5-year action plan for antimicrobial resistance 2019 to 2024. GOV.UK. Jan 24, 2019. [12-08-2024]. https://www.gov.uk/government/publications/uk-5-year-action-plan-for-antimicrobial-resistance-2019-to-2024 URL. Accessed.
- 16.Turner D, Little P, Raftery J, et al. Cost effectiveness of management strategies for urinary tract infections: results from randomised controlled trial. BMJ. 2010 Feb 5;340:c346. doi: 10.1136/bmj.c346. doi. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PLoS Med. 2009 Jul 21;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. doi. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hedges LV, Vevea JL. Fixed- and random-effects models in meta-analysis. Psychological Methods. 1998;3(4):486–504. doi: 10.1037/1082-989X.3.4.486. doi. [DOI] [Google Scholar]
- 19.Chang BH, Hoaglin DC. Meta-analysis of odds ratios: current good practices. Med Care. 2017 Apr;55(4):328–335. doi: 10.1097/MLR.0000000000000696. doi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. 2018 Jun;27(6):1785–1805. doi: 10.1177/0962280216669183. doi. Medline. [DOI] [PubMed] [Google Scholar]
- 21.Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014 Dec 19;14:135. doi: 10.1186/1471-2288-14-135. doi. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McGrath S, Sohn H, Steele R, Benedetti A. Meta-analysis of the difference of medians. Biom J. 2020 Jan;62(1):69–98. doi: 10.1002/bimj.201900036. doi. Medline. [DOI] [PubMed] [Google Scholar]
- 23.Williford E, Haley V, McNutt LA, Lazariu V. Dealing with highly SKEWED hospital length of stay distributions: the use of gamma mixture models to study delivery hospitalizations. PLoS One. 2020 Apr 20;15(4):e0231825. doi: 10.1371/journal.pone.0231825. doi. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.S H, Subbiah M, Srinivasan MR. Fitting length of stay in hospitals using transformed distributions. Commun Statistics Case Stud Data Analysis Applications. 2018 Jan 2;4(1):1–8. doi: 10.1080/23737484.2018.1445979. doi. [DOI] [Google Scholar]
- 25.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997 Sep 13;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. doi. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lin L, Chu H. Quantifying publication bias in meta-analysis. Biometrics. 2018 Sep;74(3):785–794. doi: 10.1111/biom.12817. doi. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Inflation calculator. CPI Inflation Calculator. [14-10-2023]. https://www.in2013dollars.com/ URL. Accessed.
- 28.IMF exchange rates. International Monetary Fund. [14-10-2023]. https://www.imf.org/external/np/fin/ert/GUI/Pages/CountryDataBase.aspx URL. Accessed.
- 29.Zingg W, Castro-Sanchez E, Secci FV, et al. Innovative tools for quality assessment: Integrated Quality Criteria for Review of Multiple Study Designs (ICROMS) Public Health. 2016 Apr;133:19–37. doi: 10.1016/j.puhe.2015.10.012. doi. Medline. [DOI] [PubMed] [Google Scholar]
- 30.Chang UI, Kim HW, Wie SH. Use of cefuroxime for women with community-onset acute pyelonephritis caused by cefuroxime-susceptible or -resistant Escherichia coli. Korean J Intern Med. 2016 Jan;31(1):145–155. doi: 10.3904/kjim.2016.31.1.145. doi. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Little P, Turner S, Rumsby K, et al. Dipsticks and diagnostic algorithms in urinary tract infection: development and validation, randomised trial, economic analysis, observational cohort and qualitative study. Health Technol Assess. 2009 Mar;13(19):1–73. doi: 10.3310/hta13190. doi. Medline. [DOI] [PubMed] [Google Scholar]
- 32.Madrazo M, Esparcia A, López-Cruz I, et al. Clinical impact of multidrug-resistant bacteria in older hospitalized patients with community-acquired urinary tract infection. BMC Infect Dis. 2021 Dec 7;21(1):1232. doi: 10.1186/s12879-021-06939-2. doi. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mark DG, Hung YY, Salim Z, Tarlton NJ, Torres E, Frazee BW. Third-generation cephalosporin resistance and associated discordant antibiotic treatment in emergency department febrile urinary tract infections. Ann Emerg Med. 2021 Sep;78(3):357–369. doi: 10.1016/j.annemergmed.2021.01.003. doi. Medline. [DOI] [PubMed] [Google Scholar]
- 34.Wozniak TM, Dyda A, Lee X. The increased length of hospital stay and mortality associated with community-associated infections in Australia. Open Forum Infect Dis. 2022 May 17;9(5):fac133. doi: 10.1093/ofid/ofac133. doi. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cheong T, Ahn J, Kim YS, Pai H, Kim B. Quantitative evaluation of the economic impact of antimicrobial resistance on the treatment of community-acquired acute pyelonephritis in Korea. Infect Chemother. 2022 Sep;54(3):456–469. doi: 10.3947/ic.2022.0057. doi. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim B, Kim J, Seo MR, et al. Clinical characteristics of community-acquired acute pyelonephritis caused by ESBL-producing pathogens in South Korea. Infection. 2013 Jun;41(3):603–612. doi: 10.1007/s15010-013-0441-z. doi. Medline. [DOI] [PubMed] [Google Scholar]
- 37.François M, Hanslik T, Dervaux B, et al. The economic burden of urinary tract infections in women visiting general practices in France: a cross-sectional survey. BMC Health Serv Res. 2016 Aug 9;16(a):365. doi: 10.1186/s12913-016-1620-2. doi. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.MacVane SH, Tuttle LO, Nicolau DP. Impact of extended-spectrum β-lactamase-producing organisms on clinical and economic outcomes in patients with urinary tract infection. J Hosp Med. 2014 Apr;9(4):232–238. doi: 10.1002/jhm.2157. doi. Medline. [DOI] [PubMed] [Google Scholar]
- 39.Cardwell SM, Crandon JL, Nicolau DP, McClure MH, Nailor MD. Epidemiology and economics of adult patients hospitalized with urinary tract infections. Hosp Pract (1995) 2016;44(1):33–40. doi: 10.1080/21548331.2016.1133214. doi. Medline. [DOI] [PubMed] [Google Scholar]
- 40.Rozenkiewicz D, Esteve-Palau E, Arenas-Miras M, et al. Clinical and economic impact of community-onset urinary tract infections caused by ESBL-producing Klebsiella pneumoniae requiring hospitalization in Spain: an observational cohort study. Antibiotics (Basel) 2021 May 15;10(5):585. doi: 10.3390/antibiotics10050585. doi. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zilberberg MD, Nathanson BH, Sulham K, Fan W, Shorr AF. Carbapenem resistance, inappropriate empiric treatment and outcomes among patients hospitalized with enterobacteriaceae urinary tract infection, pneumonia and sepsis. BMC Infect Dis. 2017 Apr 17;17(1):279. doi: 10.1186/s12879-017-2383-z. doi. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McLeod M, Ahmad R, Shebl NA, Micallef C, Sim F, Holmes A. A whole-health-economy approach to antimicrobial stewardship: analysis of current models and future direction. PLoS Med. 2019 Mar 29;16(3):e1002774. doi: 10.1371/journal.pmed.1002774. doi. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Antimicrobial Resistance Collaborators Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022 Feb 12;399(10325):629–655. doi: 10.1016/S0140-6736(21)02724-0. doi. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


