Highlights
-
•
Pelvic radiotherapy in patients with transplanted kidneys poses unique clinical challenges.
-
•
Proton therapy has been used in gynecologic cancers post-hysterectomy with reduced dose to pelvic organs at risk.
-
•
Patient with renal transplant and early-stage, intermediate-risk cervical cancer treated with surgery and proton therapy.
-
•
Treatment was well tolerated with a disease-free interval of 14 months and preserved renal function.
-
•
Case highlights the advantage of shared decision-making and novel use of proton therapy in treating gynecological cancer.
Abstract
Cervical adenocarcinoma is the second most common histology of cervical cancer and treatment can involve surgery, radiotherapy, systemic therapy, and any combination of the three. Photon external beam radiation therapy and brachytherapy have been the mainstay of radiation treatment options for cervical cancer. Here, we report a case of a 41-year-old patient who had a prior renal transplant and was diagnosed with early-stage, intermediate-risk adenocarcinoma treated with modified radical hysterectomy plus adjuvant proton-beam therapy and vaginal brachytherapy. Treatment was well tolerated with a disease-free interval of 14-months and preserved renal function.
1. Introduction
The mainstay treatment for early-stage, presumed low-risk cervical cancer is radical hysterectomy. Adjuvant radiotherapy improves locoregional control in cases with intermediate risk factors for recurrence per the Sedlis criteria: depth of cervical stromal invasion, lymphovascular invasion, and tumor size (Sedlis et al., 1999; Rotman et al., 2006). In an ancillary analysis of three GOG surgical trials, where patients received no adjuvant therapy, the only factor independently associated with recurrence for adenocarcinoma was tumor size greater than 4 cm. (Levinson et al., 2021). For bulky stage IB or locally advanced cervical cancer, definitive treatment with external beam radiotherapy, brachytherapy, and platinum-containing chemotherapy is standard of care (Eifel et al., 2004, Keys et al., 1999, Peters et al., 2000, Rose PG et al., 2007, Whitney et al., 1999).
Like squamous cell carcinoma, most cases of endocervical adenocarcinoma are associated with high-risk human papilloma virus (HPV) strains (Hodgson et al., 2019). As a result, protective factors against cervical cancer include early vaccination against HPV, regular cervical cancer screening, and the use of condoms during intercourse (Bowden et al., 2023). Risk factors, however, include tobacco smoking, immunosuppression, long-term usage of oral contraceptives, and behaviors associated with increased risk for HPV infection. (Chelimo et al., 2013). According to the Organ Procurement and Transplantation Network, in 2022 37.8 % of organ recipients were women, and of those, 16.9 % were women under the age of 34 (“National Data - OPTN”, 2024, Transplants, 2022). Most organ transplants require some degree of immunosuppression, posing a risk of persistent HPV infection and HPV-associated cancers, including cervical, post-transplant.
Photon external beam radiotherapy, plus or minus vaginal brachytherapy, is the standard treatment modality for adjuvant treatment of cervical cancers with risk factors for recurrence. Proton therapy has been used to treat a variety of cancers and has been increasingly used in breast and prostate cancers, as it has less off-target effects than photon therapy while preserving tumor coverage (Lin et al., 2016).There have been several dosimetric studies of proton therapy in gynecologic cancers, typically in the post-hysterectomy setting, with demonstration of reduced dose to the small bowel, large bowel, kidneys, spinal cord, pelvic bone marrow, and kidneys (Marnitz et al., 2015, Milby et al., 2012, van de Sande et al., 2016, Vyfhuis et al., 2019, Xu et al., 2018). Clinically, proton therapy has been used to treat patients with uterine, cervical, or vaginal carcinoma post-hysterectomy with adjuvant pelvic or extended field radiotherapy showing promising low rates of acute grade 3 + toxicity and excellent in field disease control. (Arians et al., 2023, Lin et al., 2016, Xu et al., 2018). However, none of the studies of proton therapy reported the use of these treatment modalities in the context of patient with a pelvic kidney transplant. Here, we present a case of early-stage cervical adenocarcinoma in a 41-year-old woman status post renal transplant on chronic immunosuppression treated with adjuvant proton therapy and vaginal brachytherapy.
2. Case
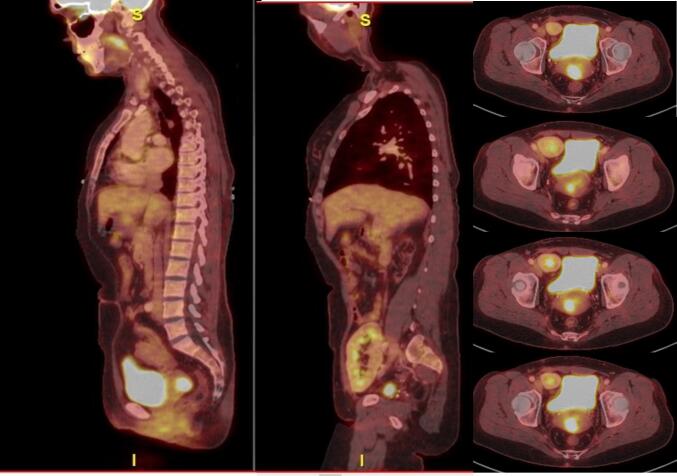
A 41-year-old White G2P0020 female presented with a chief concern of a 2.5-year history of intermittent postcoital vaginal bleeding. Pap smear approximately 7 years prior was positive for high-risk HPV and subsequent colposcopy was normal. Pap 2 years prior to presentation was negative for intraepithelial lesion or malignancy with no HPV testing performed. On pelvic exam, discharge was noted to be coming from cervix and Pap smear showed HPV16-positive adenocarcinoma in situ. Endocervical and endometrial curettage showed fragments of invasive endocervical adenocarcinoma with fragments of secretory endometrium. Subsequent cold-knife conization demonstrated invasive moderately differentiated endocervical adenocarcinoma with deep margins, focal invasion of the ectocervix and lymphovascular space invasion. Fluorodeoxyglucose positron emission tomography (FDG-PET) scan show ed a 5 cm endocervical hypermetabolic mass and bilateral level IIA cervical lymph nodes, favored to be reactive, but otherwise no lymphadenopathy or distant metastatic disease (Fig. 1).
Fig. 1.
FDG-PET Imaging at Diagnosis. Sagittal and axial sections depicting uptake by tumor, and the distance of tumor to pelvic kidney, respectively.
Her past medical history was significant for ulcerative colitis and a living donor kidney transplant in the right pelvis 7 years prior to presentation after developing dialysis-dependent chronic kidney disease secondary to atypical hemolytic uremic syndrome. She was on mycophenolate and tacrolimus for immunosuppression at the time of cervical cancer diagnosis. She was a former social smoker with a 5-pack-year history.
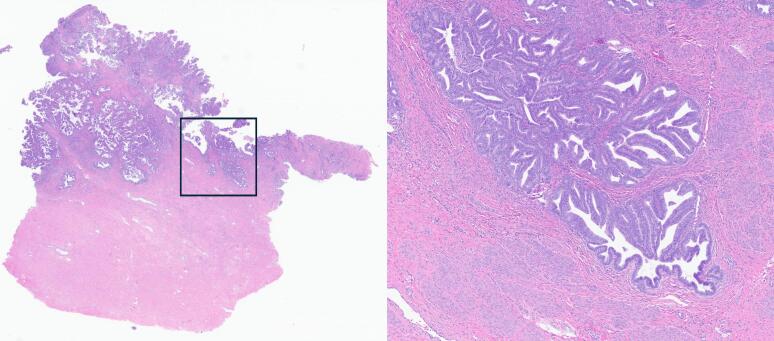
She presented to our institution for further management. Pelvic exam demonstrated a visible 2.5 cm lesion within the central portion of the cervix. Cervix was mobile with no evidence of parametrial extension on bimanual exam. Renal evaluation showed serum creatinine level of 1.45 mg/dL and estimated GFR (eGFR) of 46. Patient was advised on the risks of surgery and the use of frozen pathology to determine extent of disease invasion as well as the possibility of requiring adjuvant radiotherapy and systemic therapy depending on the extent of the disease. Through shared-decision making, patient consented to proceed with modified radical hysterectomy with possible bilateral oophorectomy, if frozen pathology showed intermediate-risk disease or higher given the need for adjuvant radiotherapy in the treatment regimen. She underwent modified radical hysterectomy, bilateral pelvic sentinel lymphadenectomy, and left completion pelvic lymphadenectomy. A transplant surgeon was present during the entire procedure to assist with intraoperative navigation around the transplanted kidney. On frozen section pathology, the tumor was an adenocarcinoma measuring 2 × 2 × 5 cm with a depth of invasion of at least 5 mm. Due to multiple intermediate risk features as indications for adjuvant radiotherapy, a bilateral oophorectomy was performed. Final pathology demonstrated 2018 FIGO Stage IB3 adenocarcinoma, HPV-16 positive, with 3–5 mm depth of stromal invasion confined to the superficial one third of the endocervix (Fig. 2). Surgical margins were negative. There was no parametrial invasion and ovaries and fallopian tubes were benign. Two left and one right pelvic sentinel lymph nodes and an additional 12 left pelvic lymph nodes were negative.
Fig. 2.
Endocervical Histology. Low-power magnification (left) view depicts intermediate stromal invasion of the tumor relative to the tissue underneath. High-power magnification (right) view from insert box depicts characteristic features of adenocarcinoma, such as prominent hyperchromasia alongside formation of glandular structures.
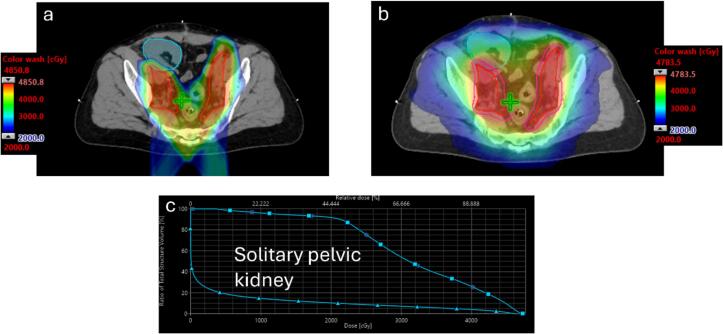
After surgery, the patient was recommended to undergo adjuvant radiotherapy with intensity modulated proton therapy (IMPT). The initial request for proton coverage was denied and peer-to-peer with a board certified radiation oncologist was performed. After a thorough discussion of the patient’s history and dosimetric comparison of her IMRT and proton plans, with particular emphasis on the mean and V20Gy to the right pelvic kidney, the denial was overturned. Clinical target volumes included the vaginal cuff and regional lymph nodes including the bilateral obturator, internal and external iliac, and common iliac lymph nodes. Prescription dose was 4500 cGy in 25 fractions. She also received 1000 cGy in two fractions of vaginal cuff brachytherapy with a multi-channel vaginal cylinder. Planning parameters included dose to 95 % (D95%) of the clinical target volume to receive > 100 % of the prescribed dose and dose to 20 % of the transplanted kidney to receive less than 20 Gy. Dose constraints for the bowel, rectum, and bladder were consistent with cooperative group studies (Klopp et al., 2018). Achieved metrics for the transplanted kidney were D20% of 4.31 Gy and V20Gy of 10.3 %. Fig. 3 shows representative slices of the dose color wash for IMPT (Fig. 3a) and volumetric modulated radiotherapy (VMAT; Fig. 3b) plans as well as the comparison dose-volume histogram (DVH; Fig. 3c) for the two plans.
Fig. 3.
External beam radiotherapy plan details. Representative isodose wash from intensity modulated proton therapy (IMPT) (Fig. 4a) versus volumetric modulated radiation therapy (VMAT) plan (Fig. 4b) showing dose to the clinical target volume (red) and solitary pelvic kidney (cyan). The low dose color wash is set at 2000 cGy for both plans. Fig. 4cis the dose volume histogram (DVH) showing dose to the solitary right pelvic kidney for IMPT (triangle) and VMAT (square) plans.
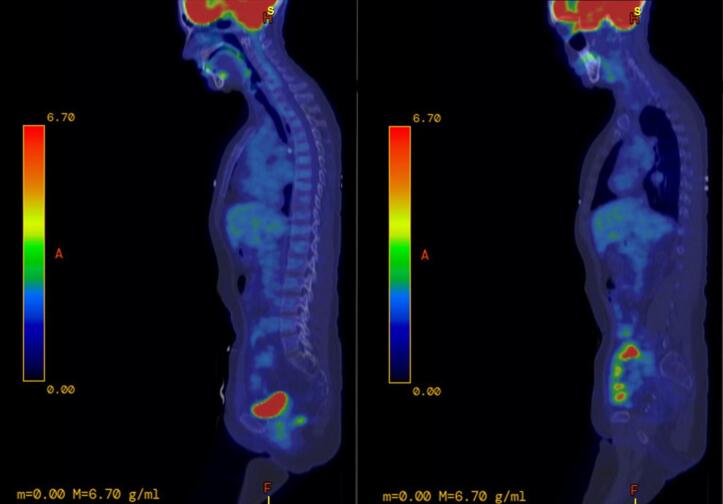
During treatment, the patient experienced grade 1 fatigue managed with rest and urinary urgency and dysuria, managed with phenazopyridine and acetaminophen. At her 3-month follow-up, the patient reported transient urinary urgency and dysuria after treatment, but symptoms had resolved by the time of the follow up visit. She had resumed normal sexual activity with no dyspareunia or vaginal bleeding. FDG-PET showed no evidence of residual or recurrent disease; however, there were inflammatory changes in the rectum (Fig. 4). Serum creatinine was 1.20 mg/dL and eGFR 58. Seven months after treatment, the patient reported hematochezia and diarrhea for several weeks consistent with her prior ulcerative colitis flares. Serum creatinine was 1.36 mg/dL and eGFR 50 mL/min. At subsequent follow-up at 10.5 months after completion of radiotherapy, patient reported near resolution of colitis flare with a 10–12 lb weight gain, but persistent postcoital bleeding. Pelvic exam showed atrophied and friable vaginal mucosa without evidence of recurrent disease. CT abdomen and pelvis was negative for recurrent or metastatic disease. Creatinine was 1.5 mg/dL and eGFR 44 mL/min. At 14 months follow-up, conservative management with systemic and topical estrogen had improved postcoital vaginal bleeding, although it had not completely resolved. Creatinine decreased to 1.26 mg/dLwith an increase in eGFR to 54 mL/min.
Fig. 4.
Sagittal slice of positron emission tomography-computed tomography (PET-CT) scan 3 months after treatment showing no residual fluorodeoxyglucose uptake, and anatomical changes consistent with a hysterectomy, bilateral salpingo-oophorectomy and lymphadenectomy.
3. Discussion
Although cervical cancer following kidney transplantation is uncommon, transplanted pelvic kidneys can impose a challenge in the treatment of pelvic cancers requiring surgery and radiotherapy. In the setting of intermediate-risk cervical cancer, definitive treatment would have included pelvic external beam radiotherapy, brachytherapy, and concurrent weekly cisplatin (Chino et al., 2020). However, given the patient’s renal transplant, there was a concern of radiation and chemotherapeutic-induced nephrotoxicity with these guideline-suggested treatment modalities. Through shared-decision making, the patient opted for surgery; as if she were to meet low-risk criteria, surgery alone would have been appropriate treatment. Even in the setting of intermediate-risk disease, upfront surgery would offer debulking of disease with possible reduction of risk to the transplanted kidney due to lower radiation dose required in the adjuvant versus definitive settings and avoidance of nephrotoxic chemotherapy used in the definitive approach.
Our patient was initially treated with an open hysterectomy as this surgical approach has been shown to have significantly higher rates of disease-free survival at 4.5 years compared to minimally invasive surgeries in patients with IA2-IIA cervical cancer. (Ramirez et al., 2018). A bilateral salpingo-oophorectomy was performed due to the need for adjuvant radiation as patient’s frozen pathology revealed intermediate-risk disease, (Sedlis et al., 1998). As radiation-induced premature ovarian failure can occur in doses as low as 200 cGy (Hilal et al., 2022) and was expected to occur in her case. The histology of the cancer alone also carried a higher risk as adenocarcinoma has been associated with a higher rate of ovarian metastasis than squamous cell carcinoma (Sutton et al., 1992). A series of case reports in patients with incidental, functioning unilateral pelvic kidneys showed that photon therapy at doses required for treatment lead to loss of the pelvic kidney, although these patients had no side effects as their contralateral retroperitoneal kidneys were still functioning (Bakri et al., 1993, Lataifeh et al., 2007, Rosenshein et al., 1980). One case report detailed photon therapy in a renal transplant patient with stage IIB cervical adenocarcinoma, where a modified field that spared the transplanted kidney and common iliac vessels was used (Ripley et al., 1995). The patient eventually suffered from buttock pain due to cancer recurrence and died from disease progression 21 months after completion of radiotherapy.
At least two case reports have detailed allograft autotransplantation to the contralateral area of the pelvis or to the upper abdomen with revascularization of the kidney with the splenic artery in the context of invasive vulvar carcinoma and stage IIB squamous cell cervical carcinoma, respectively (Abouna et al., 1994, DeRoover et al., 2000)- these patients were able to tolerate photon therapy with successful target coverage and preservation of adequate kidney function. Although autotransplantation followed by photon therapy has shown success in some cases, a second surgery would pose risks, be technically complex and impact patient quality of life such as the lifetime use of nephrostomy bags. Alternatively, a case series showed 4 cases of patients with renal transplants who underwent intensity modulated proton therapy for anal cancer, which led to eradication of the cancer with maintenance of functioning kidney (Buchberger et al., 2019).
Protons are positively charged particles that continuously lose energy as they interact with the tissue they traverse and lose a significant amount of energy very rapidly prior to stopping causing the Bragg peak phenomenon (Chhabra et al., 2016). In proton radiotherapy therapy, the Bragg peak is modifiable based on the initial energy of the proton, and any structure distal to the Bragg peak receives negligible radiation exposure. This is in sharp contrast to the traditional photon therapy, which attenuates exponentially and results in more dose distal to the tumor. Prior authorization for proton therapy in adults poses an administrative burden and significant barrier to timely patient care (Gupta et al., 2019). Fortunately, a peer-to-peer discussion overtuned the initial denial, as the benefit of proton therapy in this unique case was readily apparent. A previous small study analyzed the efficacy of proton beam therapy in patients with gynecological cancers post-hysterectomy and showed that patients receiving proton therapy had reduced gastrointestinal, hematologic, and genitourinary toxicities while maintaining at least the same efficacy as intensity modulated radiation therapy (Lin et al., 2016). Our treatment plan comparisons between proton and photon therapy showed similar findings including larger sparing of the surface area of the kidney parenchyma. (Fig. 3). Although not the primary indication for proton therapy, small bowel dose was lower with proton therapy, which is beneficial given her history of ulcerative colitis as patients with inflammatory bowel disease may be at higher risk for severe acute and late radiation toxicity (Willett et al., 2000). There was no advantage in rectum coverage between our proton and photon treatment plans due to the posterior beam arrangement. A vaginal cuff brachytherapy boost was delivered to optimize local control, as a vaginal cuff recurrence would be difficult to salvage in the setting of a transplanted kidney, while allowing for a lower dose prescription for external beam radiotherapy to minimize dose to the transplanted pelvic kidney.
This case of a 41-year-old patient with history of renal transplant diagnosed with early-stage, intermediate-risk adenocarcinoma highlights the advantage of both shared decision making and use of proton therapy in the treatment of gynecological cancer. Proton therapy was associated with satisfactory therapeutic effects while sparing kidney function, preventing the need for lifelong dialysis or another transplant. The efficacy and advantages of proton therapy in the treatment of gynecological malignancies should be further assessed through prospective trials.
4. Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author Contributions
Pedro Versuti Del Cioppo Vasques was a major contributor in writing the manuscript and compiling the patient’s history. Drs. Garda and Bakkum-Gamez were both involved in the patient’s care with Dr. Garda being the radiologist oncologist and Dr. Bakkum-Gamez being the primary surgeon in the case. Dr. Dean was the transplant surgeon present during the patient’s tumor debulking surgery. Dr. Molligan was the pathologist involved in the case. All authors read and approved the final manuscript.
CRediT authorship contribution statement
Pedro Versuti Del Cioppo Vasques: Writing – review & editing, Writing – original draft, Project administration, Investigation, Data curation, Conceptualization. Jamie N. Bakkum-Gamez: Writing – review & editing, Writing – original draft, Supervision, Project administration, Investigation, Funding acquisition, Data curation, Conceptualization. Patrick G. Dean: Writing – original draft, Investigation. Jeremy F. Molligan: Writing – original draft, Investigation. Allison E. Garda: Writing – review & editing, Writing – original draft, Supervision, Resources, Project administration, Methodology, Investigation, Formal analysis, Conceptualization.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: [Dr. Bakkum-Gamez is an editor for Gynecology Oncology Reports and is an inventor of Mayo Clinic intellectual property licensed to Exact Sciences (Madison, WI), and may receive royalties paid to Mayo Clinic].
Acknowledgement and funding
This work was supported by the MSTP grant T32GM145408 and Mayo Clinic Comprehensive Cancer Center Support Grant (P30 CA015083).
References
- “National Data - OPTN.” Organ Procurement and Transplantation Network, optn.transplant.hrsa.gov/data/view-data-reports/national-data/#. Accessed 8 June 2024.
- Abouna G.M., Micaily B., Lee D.J., Kumar M.S., Jahshan A.E., Lyons P. Salvage of a kidney graft in a patient with advanced carcinoma of the cervix by reimplantation of the graft from the pelvis to the upper abdomen in preparation for radiation therapy. Transplantation. 1994;58(4):520–522. doi: 10.1097/00007890-199408270-00021. [DOI] [PubMed] [Google Scholar]
- Arians N., Lindel K., Krisam J., Oelmann-Avendano J.T., Meixner E., König L., Hoerner-Rieber J., Wark A., Forster T., Weykamp F., Lang K., Schneeweiss A., Ellerbrock M., Mielke T., Herfarth K., Debus J. Treatment tolerability and toxicity of postoperative proton beam therapy for gynecologic malignancies: results of the prospective phase 2 APROVE trial. Int. J. Radiat. Oncol. Biol. Phys. 2023;116(4):825–836. doi: 10.1016/j.ijrobp.2023.01.004. Epub 2023 Jan 13 PMID: 36642110. [DOI] [PubMed] [Google Scholar]
- Bakri Y.N., Mansi M., Sundin T. Stage IIB carcinoma of the cervix complicated by an ectopic pelvic kidney. Int. J. Gynecol. & Obstetrics. 1993;42(2):174–176. doi: 10.1016/0020-7292(93)90634-9. [DOI] [PubMed] [Google Scholar]
- Bowden S.J., Doulgeraki T., Bouras E., Markozannes G., Athanasiou A., Grout-Smith H., Kechagias K.S., Ellis L.B., Zuber V., Chadeau-Hyam M., Flanagan J.M., Tsilidis K.K., Kalliala I., Kyrgiou M. Risk factors for human papillomavirus infection, cervical intraepithelial neoplasia and cervical cancer: an umbrella review and follow-up Mendelian randomisation studies. BMC Med. 2023;21(1):274. doi: 10.1186/s12916-023-02965-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchberger D., Kreinbrink P., Kharofa J. Proton therapy in the treatment of anal cancer in pelvic kidney transplant recipients: A case series. Int. J. Particle Therapy. 2019;6(1):28–34. doi: 10.14338/ijpt-19-00067.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chelimo C., Wouldes T.A., Cameron L.D., Elwood J.M. Risk factors for and prevention of human papillomaviruses (HPV), genital warts and cervical cancer. J Infect. 2013 Mar;66(3):207–217. doi: 10.1016/j.jinf.2012.10.024. Epub 2012 Oct 26 PMID: 23103285. [DOI] [PubMed] [Google Scholar]
- Chhabra A., Langen K., Mehta M.P. An overview of modern proton therapy. Chin. Clini. Oncol. 2016;5(4):48. doi: 10.21037/cco.2016.05.06. [DOI] [PubMed] [Google Scholar]
- Chino J., Annunziata C.M., Beriwal S., Bradfield L., Erickson B.A., Fields E.C., Fitch K., Harkenrider M.M., Holschneider C.H., Kamrava M., Leung E., Lin L.L., Mayadev J.S., Morcos M., Nwachukwu C., Petereit D., Viswanathan A.N. Radiation therapy for cervical cancer: Executive summary of an ASTRO clinical practice guideline. Practical Radiation Oncology. 2020;10(4):220–234. doi: 10.1016/j.prro.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeRoover A., Verni M.P., Taylor R.J. Renal allograft autotransplantation before pelvic irradiation. Transplantation. 2000;70(5):844–846. doi: 10.1097/00007890-200009150-00023. [DOI] [PubMed] [Google Scholar]
- Eifel P.J., Winter K., Morris M., Levenback C., Grigsby P.W., Cooper J., Rotman M., Gershenson D., Mutch D.G. Pelvic irradiation with concurrent chemotherapy versus pelvic and para-aortic irradiation for high-risk cervical cancer: an update of radiation therapy oncology group trial (RTOG) 90–01. J. Clin. Oncol. 2004;22(5):872–880. doi: 10.1200/JCO.2004.07.197. PMID: 14990643. [DOI] [PubMed] [Google Scholar]
- Gupta A., Khan A.J., Goyal S., Millevoi R., Elsebai N., Jabbour S.K., Yue N.J., Haffty B.G., Parikh R.R. Insurance approval for proton beam therapy and its impact on delays in treatment. Int. J. Radiat. Oncol. Biol .Phys. 2019;104(4):714–723. doi: 10.1016/j.ijrobp.2018.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilal L., Cercek A., Navilio J., Hsu M., Zhang Z., Brady P., Wu A.J., Reyngold M., Cuaron J.J., Romesser P.B., Zinovoy M., Nusrat M., Pappou E., LaGratta M., Garcia-Aguilar J., Paty P., Abu-Rustum N., Leitao M.M., Crane C.H., Hajj C. Factors associated with premature ovarian insufficiency in young women with locally advanced rectal cancer treated with pelvic radiation therapy. Adv. Radiat. Oncol. 2022;7(1) doi: 10.1016/j.adro.2021.100801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodgson A., Park K.J. Cervical adenocarcinomas: A heterogeneous group of tumors with variable etiologies and clinical outcomes. Arch. Pathol. & Lab. Med. 2019;143(1):34–46. doi: 10.5858/arpa.2018-0259-ra. [DOI] [PubMed] [Google Scholar]
- Keys H.M., Bundy B.N., Stehman F.B., Muderspach L.I., Chafe W.E., Suggs C.L., 3rd, Walker J.L., Gersell D. Cisplatin, radiation, and adjuvant hysterectomy compared with radiation and adjuvant hysterectomy for bulky stage IB cervical carcinoma. N. Engl. J. Med. 1999;340(15):1154–1161. doi: 10.1056/NEJM199904153401503. PMID: 10202166. [DOI] [PubMed] [Google Scholar]
- Klopp AH, Yeung AR, Deshmukh S, Gil KM, Wenzel L, Westin SN, Gifford K, Gaffney DK, Small W Jr, Thompson S, Doncals DE, Cantuaria GHC, Yaremko BP, Chang A, Kundapur V, Mohan DS, Haas ML, Kim YB, Ferguson CL, Pugh SL, Kachnic LA, Bruner DW. Patient-Reported Toxicity During Pelvic Intensity-Modulated Radiation Therapy: NRG Oncology-RTOG 1203. J Clin Oncol. 2018 Aug 20;36(24):2538-2544. doi: 10.1200/JCO.2017.77.4273. Epub 2018 Jul 10. Erratum in: J Clin Oncol. 2019 Mar 20;37(9):761. doi: 10.1200/JCO.19.00369. Erratum in: J Clin Oncol. 2020 Apr 1;38(10):1118. doi: 10.1200/JCO.20.00346. PMID: 29989857; PMCID: PMC6097832. [DOI] [PMC free article] [PubMed]
- Lataifeh I., Amarin Z., Jaradat I. Stage IIB carcinoma of the cervix that is associated with pelvic kidney: A therapeutic dilemma. Am. J. Obstetrics and Gynecol. 2007;197(6) doi: 10.1016/j.ajog.2007.08.056. [DOI] [PubMed] [Google Scholar]
- Levinson K., Beavis A.L., Purdy C., Rositch A.F., Viswanathan A., Wolfson A.H., Kelly M.G., Tewari K.S., McNally L., Guntupalli S.R., Ragab O., Lee Y.-C., Miller D.S., Huh W.K., Wilkinson K.J., Spirtos N.M., Van Le L., Casablanca Y., Holman L.L., Fader A.N. Beyond Sedlis—a novel histology-specific nomogram for predicting cervical cancer recurrence risk: An NRG/gog ancillary analysis. Gynecol. Oncol. 2021;162(3):532–538. doi: 10.1016/j.ygyno.2021.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin L.L., Kirk M., Scholey J., Taku N., Kiely J.B., White B., Both S. Initial report of pencil beam scanning proton therapy for posthysterectomy patients with gynecologic cancer. Int. J. Radiat. Oncol. biology*physics. 2016;95(1):181–189. doi: 10.1016/j.ijrobp.2015.07.2205. [DOI] [PubMed] [Google Scholar]
- Marnitz S., Wlodarczyk W., Neumann O., Koehler C., Weihrauch M., Budach V., Cozzi L. Which technique for radiation is most beneficial for patients with locally advanced cervical cancer? Intensity modulated proton therapy versus intensity modulated photon treatment, helical tomotherapy and volumetric arc therapy for primary radiation - an intraindividual comparison. Radiat. Oncol. 2015;17(10):91. doi: 10.1186/s13014-015-0402-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milby A.B., Both S., Ingram M., Lin L.L. Dosimetric comparison of combined intensity-modulated radiotherapy (IMRT) and proton therapy versus IMRT alone for pelvic and para-aortic radiotherapy in gynecologic malignancies. Int. J. Radiat. Oncol. Biol. Phys. 2012;82(3):e477–e484. doi: 10.1016/j.ijrobp.2011.07.012. Epub 2011 Dec 15 PMID: 22177626. [DOI] [PubMed] [Google Scholar]
- Peters WA 3rd, Liu PY, Barrett RJ 2nd, Stock RJ, Monk BJ, Berek JS, Souhami L, Grigsby P, Gordon W Jr, Alberts DS. Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervix. J Clin Oncol. 2000 Apr;18(8):1606-13. doi: 10.1200/JCO.2000.18.8.1606. Corrected and republished in: J Clin Oncol. 2023 Oct 10;41(29):4605-4612. PMID: 10764420. [DOI] [PubMed]
- Ramirez P.T., Frumovitz M., Pareja R., Lopez A., Vieira M., Ribeiro R., Buda A., Yan X., Shuzhong Y., Chetty N., Isla D., Tamura M., Zhu T., Robledo K.P., Gebski V., Asher R., Behan V., Nicklin J.L., Coleman R.L., Obermair A. Minimally invasive versus abdominal radical hysterectomy for cervical cancer. New Eng. J. Med. 2018;379(20):1895–1904. doi: 10.1056/nejmoa1806395. [DOI] [PubMed] [Google Scholar]
- Ripley D., Levenback C., Eifel P., Lewis R.M. Adenocarcinoma of the cervix in a renal transplant patient. Gynecologic Oncology. 1995;59(1):151–155. doi: 10.1006/gyno.1995.1283. [DOI] [PubMed] [Google Scholar]
- Rose PG, Ali S, Watkins E, Thigpen JT, Deppe G, Clarke-Pearson DL, Insalaco S; Gynecologic Oncology Group. Long-term follow-up of a randomized trial comparing concurrent single agent cisplatin, cisplatin-based combination chemotherapy, or hydroxyurea during pelvic irradiation for locally advanced cervical cancer: a Gynecologic Oncology Group Study. J Clin Oncol. 2007 Jul 1;25(19):2804-10. doi: 10.1200/JCO.2006.09.4532. Epub 2007 May 14. PMID: 17502627. [DOI] [PubMed]
- Rosenshein N.B., Lichter A.S., Walsh P.C. Cervical cancer complicated by a pelvic kidney. J. Urol. 1980;123(5):766–767. doi: 10.1016/s0022-5347(17)56123-6. [DOI] [PubMed] [Google Scholar]
- Rotman M., Sedlis A., Piedmonte M.R., Bundy B., Lentz S.S., Muderspach L.I., Zaino R.J. A phase III randomized trial of postoperative pelvic irradiation in stage IB cervical carcinoma with poor prognostic features: Follow-up of a Gynecologic Oncology Group Study. Int. J. Radiat. Oncology*biology*physics. 2006;65(1):169–176. doi: 10.1016/j.ijrobp.2005.10.019. [DOI] [PubMed] [Google Scholar]
- Sedlis A., Bundy B.N., Rotman M.Z., Lentz S.S., Muderspach L.I., Zaino R.J. A randomized trial of pelvic radiation therapy versus no further therapy in selected patients with stage IB carcinoma of the cervix after radical hysterectomy and pelvic lymphadenectomy: A Gynecologic Oncology Group Study. Gynecologic Oncology. 1999;73(2):177–183. doi: 10.1006/gyno.1999.5387. [DOI] [PubMed] [Google Scholar]
- Sutton G.P., Bundy B.N., Delgado G., Sevin B.U., Creasman W.T., Major F.J., Zaino R. Ovarian metastases in stage IB carcinoma of the cervix: a Gynecologic Oncology Group study. Am. J. Obstet. Gynecol. 1992;166(1 Pt 1):50–53. doi: 10.1016/0002-9378(92)91828-x. PMID: 1733218. [DOI] [PubMed] [Google Scholar]
- Transplants in the U.S. by Recipient Gender: U.S. Transplants Performed : January 1, 1988 - May 31, 2023. (2023, June 22). Retrieved June 23, 2022.
- van de Sande M.A., Creutzberg C.L., van de Water S., Sharfo A.W., Hoogeman M.S. Which cervical and endometrial cancer patients will benefit most from intensity-modulated proton therapy? Radiother Oncol. 2016;120(3):397–403. doi: 10.1016/j.radonc.2016.06.016. Epub 2016 Jul 21 PMID: 27452411. [DOI] [PubMed] [Google Scholar]
- Vyfhuis MAL, Fellows Z, McGovern N, Zhu M, Mohindra P, Wong J, Nichols EM. Preserving Endocrine Function in Premenopausal Women Undergoing Whole Pelvis Radiation for Cervical Cancer. Int J Part Ther. 2019 Summer;6(1):10-17. doi: 10.14338/IJPT-D-19-00061.1. Epub 2019 Aug 23. PMID: 31773044; PMCID: PMC6871630. [DOI] [PMC free article] [PubMed]
- Whitney C.W., Sause W., Bundy B.N., Malfetano J.H., Hannigan E.V., Fowler W.C., Jr, Clarke-Pearson D.L., Liao S.Y. Randomized comparison of fluorouracil plus cisplatin versus hydroxyurea as an adjunct to radiation therapy in stage IIB-IVA carcinoma of the cervix with negative para-aortic lymph nodes: a Gynecologic Oncology Group and Southwest Oncology Group study. J. Clin. Oncol. 1999;17(5):1339–1348. doi: 10.1200/JCO.1999.17.5.1339. PMID: 10334517. [DOI] [PubMed] [Google Scholar]
- Willett C.G., Ooi C.J., Zietman A.L., Menon V., Goldberg S., Sands B.E., Podolsky D.K. Acute and late toxicity of patients with inflammatory bowel disease undergoing irradiation for abdominal and pelvic neoplasms. Int. J. Radiat. Oncol. Biol. Phys. 2000;46(4):995–998. doi: 10.1016/s0360-3016(99)00374-0. PMID: 10705022. [DOI] [PubMed] [Google Scholar]
- Xu MJ, Maity A, Vogel J, Kirk M, Zhai H, Both S, Lin LL. Proton Therapy Reduces Normal Tissue Dose in Extended-Field Pelvic Radiation for Endometrial Cancer. Int J Part Ther. 2018 Winter;4(3):1-11. doi: 10.14338/IJPT-17-00027.1. Epub 2018 Mar 21. PMID: 31773009; PMCID: PMC6871568. [DOI] [PMC free article] [PubMed]