Abstract
Background
Lateral lumbar interbody fusion (LLIF) is commonly used to address various lumbar pathologies. LLIF using the prone transpsoas (PTP) approach has several potential advantages, allowing simultaneous access to the anterior and posterior columns of the spine. The aim of this study was to report the 1-year outcomes of LLIF via PTP.
Methods
This is a retrospective review of 97 consecutive patients who underwent LLIF via PTP. Radiographic parameters, including lumbar-lordosis, segmental-lordosis, anterior disc height, and posterior disc height, were measured on preoperative, initial-postoperative, and 1-year postoperative imaging. Patient-reported outcomes measures, including Oswestry Disability Index, visual analog scale (VAS), pain EQ5D, and postoperative complications, were reviewed.
Results
Ninety-seven consecutive patients underwent 161 levels of LLIF. Fifty-seven percent underwent 1-level LLIF, 30% 2-level LLIF, 6% 3-level LLIF, and 7% 4-level LLIF. The most common level was L4 to L5 (35%), followed by L3 to L4 (33%), L2 to L3 (21%), and L1 to L2 (11%). Significant improvements were noted at initial and 1-year postoperative periods in lumbar-lordosis (2° ± 10°, P = 0.049; 3° ± 9°, P = 0.005), segmental-lordosis (6° ± 5°, P < 0.001; 5° ± 5°, P < 0.001), anterior disc height (8 mm ± 4 mm, P < 0.001; 7 mm ± 4 mm, P < 0.001), and posterior disc height (3 mm ± 2 mm, P < 0.001; 3 mm ± 2 mm, P < 0.001). Significant improvements were seen in Oswestry Disability Index at 6 weeks (P = 0.002), 6 months (P < 0.001), and 1 year (P < 0.001) postoperatively; pain EQ5D at 6 weeks (P < 0.001), 6 months (P < 0.001), and 1 year (P < 0.001) postoperatively; and leg and back visual analog scale at 2 weeks (P < 0.001), 6 months (P < 0.001), and 1 year (P < 0.001) postoperatively. The average length of stay was 2.5 days, and the most common complications were ipsilateral hip flexor pain (46%), weakness (59%), and contralateral hip flexor pain (29%).
Conclusion
PTP is a novel way of performing LLIF. These 1-year data support that PTP is an effective, safe, and viable approach with similar patient-reported outcome measures and complications profiles as LLIF performed in the lateral decubitus position.
Level of Evidence
4.
Keywords: lumbar stenosis, interbody fusion, prone-transpsoas, lateral, transpsoas, single-position surgery, lumbar plexus
Introduction
Lateral lumbar interbody fusion (LLIF) is a minimally invasive technique utilized to address various lumbar spine pathologies and perform lumbar fusions.1–3 It provides an alternative to other interbody techniques with benefits including a tissue-sparing minimally invasive approach, reduced blood loss, large surface area for fusion, restoration of segmental lordosis (SL), and indirect decompression.2,4 LLIF has traditionally been performed in the lateral decubitus position, often requiring an intraoperative change in patient position to access the posterior column for anything other than simple instrumentation. Single-position surgery techniques have been explored to minimize changes in patient positioning and to reduce the anesthetic and operating room time.5–10
Prone transpsoas (PTP) approach is a novel way of performing an LLIF described by Pimenta et al, allowing simultaneous access to both the anterior and posterior columns.10,11 The patient is placed in the prone position and secured with a bolster system, which stabilizes the patient and allows lateral bend of the lumbar spine. This positioning provides access to the anterior and posterior columns, negating the need for an intraoperative change in patient positioning, which can prolong both the anesthetic and operating room time.10,12
As these techniques were only recently described, there is a paucity of studies that have evaluated the safety and efficacy of performing an LLIF via the PTP approach.11–16 Walker et al reported on 30 consecutive patients with spondylolisthesis treated with a prone lateral (n = 15) and dual position approach (n = 15) and demonstrated a greater improvement in postoperative SL in the prone lateral group with similar improvements in pelvic tilt, disc height, and spondylolisthesis reduction.14 Farber et al conducted a retrospective review of 28 patients who underwent the prone lateral approach for lumbar fusion and reported an 11% complication rate, a 23% subsidence rate, and demonstrated improvements in 3-month Oswestry Disability Index (ODI) and visual analog scale (VAS) back and leg.15 Pimenta et al performed a retrospective multicenter review of 32 patients who underwent a PTP approach and reported improvement in SL and spinopelvic parameters.11 NaPier et al reported on 72 patients undergoing a PTP approach with anterior docking technique and demonstrated no vascular, bowel, or visceral complications, improvements in ODI and VAS as well as SL, total lumbar lordosis (LL), and spinopelvic parameters.12 Our early clinical outcomes study highlighted improvement in radiographic parameters (LL, anterior disc height [ADH], and posterior disc height [PDH]) and clinical outcomes (ODI, VAS, and EQ5D) in 82 consecutive patients who underwent LLIF via a PTP approach.13
Most studies published to date have evaluated the early outcomes and perioperative complication rates. It is important to understand the longer-term complication profile, as well as radiographic and clinical outcomes of LLIF performed via PTP approach, to determine whether the technique should continue to be adopted. The aim of this study was to review the 1-year outcomes of LLIF performed via PTP approach with respect to radiographic parameters, patient-reported outcome measures (PROMs), and complication rates.
Materials and Methods
After institutional review board approval, the medical records of all patients who underwent a single- or multilevel PTP LLIF from November 2021 to November 2023, with at least 1-year follow-up, were retrospectively reviewed. All patients underwent an LLIF using the PTP patient positioner (AlphaTec, Carlsbad, CA) positioning system and SafeOps neuromonitoring system (AlphaTec, Carlsbad, CA). A minimum of 1-year follow-up was required for inclusion. Data collected from the record review included the number of LLIF levels; demographic factors including age, gender, and body mass index; and medical comorbidities including American Society of Anesthesiology class.
Radiographic parameters were from the preoperative, initial postoperative, postoperative day 1 or 2, and 1-year postoperative lumbar radiographs. At each time point, LL, SL, ADH, and PDH were measured. LL is defined by the angle from the superior endplate of L1 to the superior endplate of S1. SL was defined by the angle between the inferior endplate of the superiorly instrumented vertebrae and the superior endplate of the inferiorly instrumented vertebrae. ADH and PDH were defined as the distances between the superior and inferior endplates of the instrumented vertebrae.
All of the measurements were performed by a single investigator to improve internal reliability.
Patient-Reported Outcomes
PROMs, including ODI, pain portion of EQ5D (pain), and VAS leg and back, were collected from all patients pre- and postoperatively. To determine patients’ perceived postoperative improvement, a Global Rating of Change (GROC) score was collected. This is a 15-point scale that ranges from −7 (“a very great deal worse”) to +7 (“a very great deal better”), with 0 indicating no change from the preoperative symptom state. Finally, patients were asked at each postoperative visit if they were at a symptom level that they deemed acceptable. This was used to determine the proportion of patients with a patient-acceptable symptom state (PASS). Patients without available outcome measures either due to lack of follow-up or completion were excluded from analysis.
Complications
The medical record of each included patient was reviewed for all intraoperative and postoperative complications, including hip flexor pain and weakness.
Statistical Analysis
The number of 1-, 2-, 3-, and 4-level instrumentations, disc spaces instrumented, levels at which interbodies were placed, number of transforaminal lumbar interbody fusion levels, and number of anterior lumbar interbody fusion levels were expressed as proportions of the whole. For radiographic outcomes, paired-sample t tests were used to compare the initial postoperative and the 1-year postoperative radiographic measurements to the preoperative measurements. Similarly, paired-sample t tests were used to compare PROMs at 2 weeks, 6 weeks, 6 months, and 1 year to the preoperative measurements. GROC pain and functional scores were reported as the proportion of patients who reported at least a +2 (“a little bit better”) and those that reported at least a +5 (“quite a bit better”). A cutoff of 2 (“a little bit better”) was chosen because it indicates the percentage of patients that experienced at least mild improvement from the procedure. A cutoff of 5 (“quite a bit better”) was subsequently chosen as it indicates the proportion of patients who perceived a significant benefit from the procedure. The percentage of patients reporting a positive PASS was reported as a proportion of the whole. The GROC and PASS scores were added to the analysis as they allow correlation of established outcome measures with the patient-specific experience. This information is useful because there is no established minimal clinically important difference for this particular procedure in this patient population.17 All statistical analyses were performed using SPSS (v28, IBM, Armonk, NY). A P value of 0.05 or less was considered statistically significant.
Results
A total of 97 patients underwent the PTP approach with a total of 161 levels of LLIF. There were 54 female patients (56%) and 43 male patients (44%) in the study. Fifty-five patients (57%) underwent a 1-level PTP, 29 patients (30%) underwent a 2-level PTP, 6 patients (7%) underwent a 3-level PTP, and 7 patients (7%) underwent a 4-level PTP. Forty patients (41%) underwent a 1-level fusion, 25 patients (26%) underwent a 2-level fusion, 15 patients (16%) underwent a 3-level fusion, 15 patients (16%) underwent a 4-level fusion, and 2 patients (2%) underwent a 5-level fusion. Single-level transforaminal lumbar interbody fusion was performed at another level in 15 patients (16%). Single-level anterior lumbar interbody fusion was performed at another level in 2 patients (2%). The most common level of PTP was L4-5 with 56 patients (35%), followed by 53 patients (33%) with L3-L4 PTP, 34 patients (21%) with L2-L3 PTP, and 18 patients (11%) with L1-L2 PTP (Table 1).
Table 1.
Demographics of study participants.
| Characteristics | n (%) |
| No. of patients | 97 |
| No. of levels | 161 |
| No. of PTP levels | |
| 1 | 55 (57) |
| 2 | 29 (30) |
| 3 | 6 (6) |
| 4 | 7 (7) |
| No. of PTP levels | |
| 2 | 29 (30) |
| 3 | 6 (6) |
| 4 | 7 (7) |
| Total No. of levels fused | |
| 1 | 40 (41) |
| 2 | 25 (26) |
| 3 | 15 (16) |
| 4 | 15 (16) |
| 5+ | 2 (2) |
| Level of PTP | |
| L1−L2 | 18 (11) |
| L2−L3 | 34 (21) |
| L3−L4 | 53 (33) |
| L4−L5 | 56 (35) |
| No. of transforaminal lumbar interbody fusion levels | |
| 0 | 76 (79) |
| 1 | 15 (16) |
| 2 | 5 (5) |
| 3 | 1 (1) |
| No. of anterior lumbar interbody fusion levels | |
| 0 | 94 (97) |
| 1 | 2 (2) |
| 2 | 1 (1) |
| Gender, female | 54 (56) |
| Age, y, mean (SD) | 62 (11) |
| Body mass index, mean (SD) | 30 (7) |
| Comorbidities | |
| Hypertension | 69 (71) |
| Hyperlipidemia | 42 (43) |
| Diabetes | 18 (19) |
| Coronary artery disease | 9 (9) |
| Congestive heart failure | 1 (1) |
| Chronic obstructive pulmonary disease | 11 (11) |
| Chronic kidney disease | 6 (6) |
| ASA classification | |
| 1 | 2 (2) |
| 2 | 58 (60) |
| 3 | 37 (37) |
Abbreviations: ASA, American Society of Anesthesiology; PTP, prone transpsoas.
Note: Data presented as n (%) unless otherwise indicated.
Significant improvements were noted at initial (2° ± 10°, P = 0.049) and 1-year (3° ± 9°, P = 0.005) postoperative periods in LL, SL (6° ± 5°, P < 0.001; 5° ± 5°, P < 0.001), ADH (8 mm ± 4 mm, P < 0.001; 7 mm ± 4 mm, P < 0.001), and PDH (3 mm ± 2 mm, P < 0.001; 3 mm ± 2 mm, P < 0.001; Table 2). Subsidence of the interbody device was noted in 6 patients (6%). Significant improvements were seen in ODI at 6 weeks (P = 0.002), 6 months (P < 0.001), and 1-year (P < 0.001) postoperatively; pain EQ5D at 6 weeks (P < 0.001), 6 months (P < 0.001), and 1-year (P < 0.001) postoperatively; leg and back VAS at 2 weeks (P < 0.001), 6 months (P < 0.001), and 1-year (P < 0.001) postoperatively (Table 3). The mean length of stay was 2.5 ± 4.5 days.
Table 2.
Mean (SD) change in radiographic parameters.
| Radiographic Measurement | N | Mean (SD) Change Compared With Preoperation | P |
| LL (°) | 95 | ||
| Initial postoperative | 2 (10) | 0.049 | |
| 1 y postoperative | 3 (9) | 0.005 | |
| SL (°) | 155 | ||
| Initial postoperative | 6 (5) | <0.001 | |
| 1 y postoperative | 5 (5) | <0.001 | |
| ADH (mm) | 155 | ||
| Initial postoperative | 8 (4) | <0.001 | |
| 1 y postoperative | 7 (4) | <0.001 | |
| PDH (mm) | 155 | ||
| Initial postoperative | 3 (2) | < 0.001 | |
| 1 y postoperative | 3 (2) | < 0.001 |
Abbreviations: ADH, anterior disc height; LL, lumbar lordosis; PDH, posterior disc height; SL, segmental lordosis.
Table 3.
Mean (SD) change in patient-reported outcomes.
| Patient-Reported Outcomes | n | Mean (SD) Change Compared With Preoperation | P |
| ODI | |||
| 2 wk | 41 | 3.7 (22.8) | 0.307 |
| 6 wk | 48 | −8.7 (18.3) | 0.002 |
| 6 mo | 45 | −24.2 (15.1) | <0.001 |
| 1 y | 42 | −21.7 (19.6) | <0.001 |
| Pain EQ5D | |||
| 2 wk | 43 | 0.00 (0.21) | 0.9 |
| 6 wk | 51 | 0.12 (0.2) | <0.001 |
| 6 mo | 47 | 0.17 (0.2) | <0.001 |
| 1 y | 45 | 0.19 (0.3) | <0.001 |
| Leg VAS | |||
| 2 wk | 48 | −2.6 (3.9) | <0.001 |
| 6 wk | 52 | −3.5 (3.5) | <0.001 |
| 6 mo | 48 | −4.6 (2.7) | <0.001 |
| 1 y | 46 | −4.4 (3.6) | <0.001 |
| Back VAS | |||
| 2 wk | 48 | −1.7 (2.8) | <0.001 |
| 6 wk | 52 | −3.5 (2.7) | <0.001 |
| 6 mo | 48 | −4.3 (2.3) | <0.001 |
| 1 y | 46 | −4.2 (2.6) | <0.001 |
Abbreviations: ODI, Oswestry Disability Index; VAS, visual analog scale.
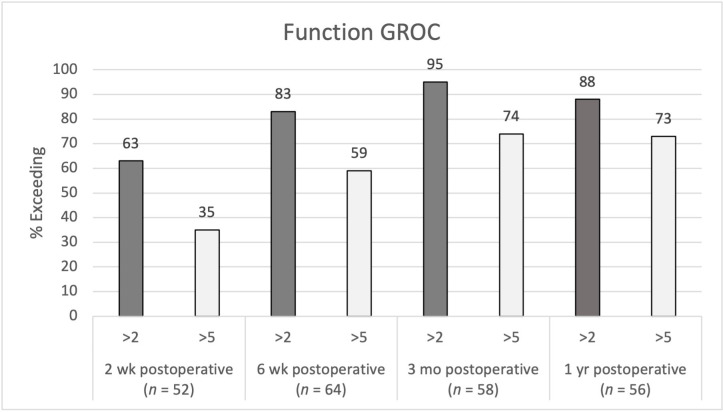
With respect to function, at 2 weeks from the surgery, 63% of patients reported at least a “little bit better” function as compared with their preoperative state, improving to 83% at 6 weeks, 95% at 3 months, and 88% at 1 year from surgery. Thirty-five percent of patients reported that their function was “quite a bit better” at the 2 weeks time point, 59% at 6 weeks, 74% at 3 months, and 73% at 1 year (Figure 1).
Figure 1.
Function Global Rating of Change (GROC) postoperative scores at 2 wk, 6 wk, 3 mo, and 1 y.
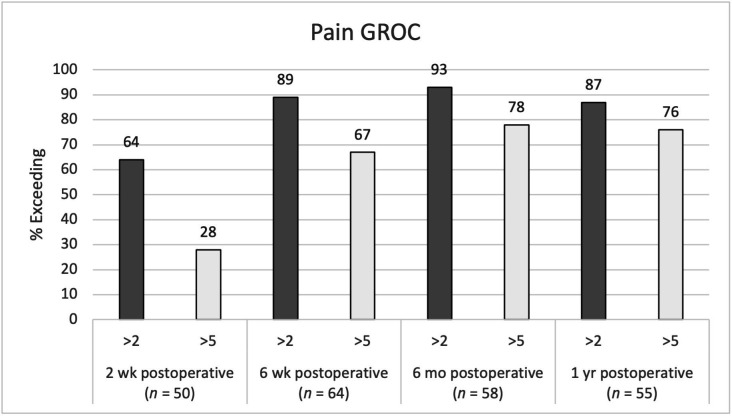
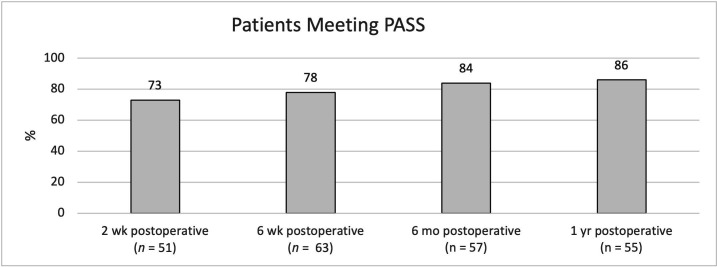
Patients had a similar trend with respect to pain postoperatively. At 2 weeks from the surgery, 64% of patients reported at least a “little bit better” pain as compared with their preoperative state. This improved to 89% at 6 weeks, 93% at 6 months, and 87% at 1 year. 28% of patients reported “quite a bit better” at the 2 weeks time point, 67% at 6 weeks, 78% at 6 months, and 76% at 1 year (Figure 2). At 2 weeks from surgery, 73% of patients reported an acceptable symptomatic state, improving to 78% at 6 weeks, 84% at 6 months, and 86% at 1 year (Figure 3).
Figure 2.
Pain Global Rating of Change (GROC) postoperative scores at 2 wk, 6 wk, 6 mo, and 1 y.
Figure 3.
Patient-acceptable symptom state (PASS) postoperative scores at 2 wk, 6 wk, 6 mo, and 1 y.
The most common complications were ipsilateral hip flexor pain in 45 patients (46%), weakness in 57 patients (59%), and contralateral hip flexor pain in 28 patients (29%). There was ipsilateral thigh numbness in 23 patients (24%) and contralateral hip flexor weakness in 21 patients (22%). There were 2 femoral nerve palsies (2%), both of which resolved within 3 months following surgery. PTP was aborted in 2 patients (2%) due to lack of a safe neurological working corridor. There were 8 patients (8%) who had an anterior longitudinal ligament rupture; all were recognized intraoperatively and addressed with lateral plate fixation. There was no occurrence of bowel injury or vascular injury in the study. There were 2 deaths; however, these were unrelated to the surgical procedure: one was secondary to complications from an aspiration pneumonia postoperatively and the other cause was unknown—having occurred 2 weeks postoperatively when the patient was found deceased at home (Table 4).
Table 4.
Postoperative complications of study participants.
| Complication | n (%) |
| Intraoperative complications | |
| ALL rupture | 8 (8) |
| Aborted prone transpsoas level | 2 (2) |
| Postoperative neuromotor complications | |
| Ipsilateral hip flexor pain | 45 (46) |
| Ipsilateral hip flexor weakness | 57 (59) |
| Ipsilateral thigh numbness | 23 (24) |
| Contralateral hip flexor pain | 28 (29) |
| Contralateral hip flexor weakness | 21 (22) |
| Femoral nerve palsy | 2 (2) |
| Postoperative medical complications | |
| Urinary retention | 8 (8) |
| Deep vein thrombosis | 1 (1) |
| Pneumonia | 1 (1) |
| Altered mental status | 5 (5) |
| Urosepsis | 3 (3) |
| Death | 2 (2) |
| Other complications | |
| Abdominal wall pseudohernia | 1 (1) |
| Subsidence on 1-y radiographs | 6 (6) |
Abbreviation: ALL, anterior longitudinal ligament.
Discussion
PTP is a novel approach to perform an LLIF. Given its novelty, it is essential for surgeons to understand the long-term outcomes and complication profile. As such, if the complications, radiographic outcomes, and PROMs of patients undergoing a PTP are comparable or improved as compared with a traditional lateral approach, it should be considered given its inherent benefits. There have been several studies that have evaluated the outcomes of PTP; however, all have focused on short-term outcomes.11–16
The present study, to the authors’ knowledge, is currently the largest patient series with the longest follow-up period reported. The data demonstrate that patients undergoing LLIF via PTP have statistically significant improvements in all radiographic parameters, including LL, SL, ADH, and PDH. This finding is clinically significant as surgeons rely on the power of interbody placement to restore disc and foraminal height, thus allowing for indirect decompression, restoration of SL, and maintenance of improvement of sagittal alignment. In addition, there was a significant improvement in PROMs including ODI, pain EQ5D, and VAS leg and back at 6 weeks, 6 months, and 1 year. Seventy-three percent of patients reported significant improvement in function and 76% of patients reported significant improvement in pain at 1-year following surgery.
The overall effect of spinal deformity on health status can vary; however, restoring a normal sagittal balance has been shown to be the most reliable predictor of clinical symptoms.18 Even though our cohort did not necessarily have a sagittal plane deformity, it is vital to pay attention to the restoration of SL as its lack can ultimately contribute to the development of adjacent segment degeneration and potentially revision. Issa et al conducted a retrospective review of 78 patients who underwent 106 levels of LLIF and reported that LLIF reliably improves LL and disc space height.19 Anteriorly placed interbody devices provided the greater segmental angular correction than posteriorly placed cages, and cage height, lordosis angle, and material did not impact radiographic parameters.19 Bakare et al performed a retrospective analysis of LLIF over a 5.5-year period and reported that lateral interbody devices greatly improved SL at the index level.20
Alimi et al investigated the functional and radiological impact of LLIF in degenerative disc disease population.21 They evaluated 145 levels of LLIF in 90 patients, with an average follow-up of 12.6 months. The study demonstrated an increase in lumbar sagittal lordosis of 5.3 postoperatively (P < 0.0001) and 2.9 at the latest follow-up (P = 0.014). Philips et al reported on a prospective multicenter study in which 107 patients underwent LLIF. They demonstrated a significant increase in immediate postoperative LL (P < 0.001) with some loss of lordosis over time; however, it remained significantly greater than the preoperative value at the 24-month follow-up (P < 0.001).22 The mean disc height was also improved immediately postoperatively and at 24 months (P < 0.001).22
Our data demonstrate that LLIF performed via PTP improves both LL (3°, P = 0.005) and SL (5°, P < 0.001) immediately and at 1 year postoperatively. The improvement in LL and SL was maintained at the final follow-up, demonstrating that this is comparable to other studies.18–22
Agarwal et al investigated 126 patients who underwent stand-alone LLIF and demonstrated a durable improvement in ODI and EQ5D scores at 5-year follow-up and in VAS score at 2-year follow-up.23 In their study, Alimi et al demonstrated improvements in ODI (21.1%) and VAS for back (3.7), buttock (3.6), and leg (3.7) following LLIF.21 Campbell et al conducted a retrospective review of 18 patients who underwent LLIF and showed an average improvement in ODI score of 26 points by the 6-month follow-up as well as Short Form-12 physical and mental component summary scores.1 Similarly, Philips et al demonstrated significant improvements in ODI, VAS back, VAS leg, Short Form-36 mental component summary, and short form-36 physical component summary at the 24-month follow-up in their prospective multicenter trial.22
Our data demonstrated improvements in ODI at 6 weeks (P = 0.002), 6 months (P < 0.001), and 1 year (P < 0.001) following surgery. The change in ODI at 2 weeks was not statistically significant, likely due to the expected recovery from surgical trauma, as the change became significant by 6 weeks and persisted at later time points. Results from the EQ5D were similar, with improvements becoming statistically significant at 6 weeks (P < 0.001) and persisting at 6 months (P < 0.001) and 1 year (P < 0.001) following surgery. Leg and back VAS demonstrated significant improvement at 2 weeks (P < 0.001), 6 months (P < 0.001), and 1 year (P < 0.001) postoperatively. The PROMs in our study are comparable to those previously reported in the literature in patients undergoing LLIF in the lateral decubitus position.21–23
Rodgers et al reported on a prospective analysis of 600 patients undergoing LLIF in the lateral decubitus position and identified a 6.2% incidence of perioperative complications, average length of stay of 1.2 days, no wound infections, visceral injuries or vascular injuries, and a 0.7% transient neurological deficit. At 1-year follow-up, 86.7% of patients were satisfied with their procedure and 90.7% stated that they would undergo the procedure again.24 Kotwal et al evaluated 118 patients undergoing LLIF with a 2-year follow-up and reported significant improvement in VAS for pain (53%), ODI (43%), Short Form-12 physical components summary (41%) scores, along with improvements in disc height, coronal angulation, lordotic angulation, and Cobb angle. Their most common complication was described to be transient thigh pain, which was present in 36% of patients.25
Tohmeh et al reported on the results of a prospective multicenter study in which 102 patients underwent LLIF via a direct lateral approach at L3 to L4 and/or L4 to L5.26 They noted a 27.5% incidence of hip flexion weakness, 17.6% of new postoperative upper medial thigh sensory loss, and 2.9% incidence of transient motor deficits.26 Lee et al evaluated the extent of injury to the psoas muscle by measuring hip flexion strength immediately in 33 patients and noted a statistically significant reduction in strength (P = 0.0001) 2 days following surgery.27 This was noted to be temporary as it resolved by 2 weeks following surgery.27 Hijji et al performed a systematic review evaluating the medical and surgical complications of LLIF, including 6819 patients who underwent LLIF with 11,325 levels fused. The most commonly reported complication was a transient neurological complication with a rate of 36.07% and a persistent neurological complication with a rate of 3.98%.28 These findings are comparable to the ones identified in our study with the most common complications being ipsilateral hip flexor pain and weakness.
Nakashima et al prospectively evaluated 30 patients undergoing a 2-staged fusion with 108 levels of LLIF followed by posterior fixation for adult spinal deformity.29 There was an improvement in LL by 47.5% and PT by 64.5% following LLIF but before posterior fixation. Endplate injury was identified in 21 levels (19.4%) on computed tomography with an SL angle of 5.3° ± 8.4° at levels without endplate injury and 1.9° ± 5.9° at levels with endplate injury.29 There was an ALL rupture identified on 7 levels (6.5%), with a significantly larger SL angle correction (P < 0.0001).29 Faber et al evaluated the complications associated with a single-position prone LLIF in which 10 studies were analyzed with 286 patients, undergoing a mean of 1.3 levels per patients. Eighteen intraoperative complications were identified with 3 cases of cage subsidence (3.8%), 5 cases of anterior longitudinal ligament rupture (2.3%), and no major vascular or peritoneal injuries.16 There was a 17.8% incidence of hip flexor weakness and 13.3% incidence of thigh and groin sensory symptoms.16 Our data demonstrate that LLIF performed via PTP had an anterior longitudinal ligament rupture in 8 patients (8%), which is comparable to the rates reported in the lateral decubitus position, demonstrating that PTP does not significantly increase the risk of an inadvertent ALL injury.
The strengths of the present study include the large number of patients included, a robust data set including prospectively collected clinical outcomes and radiographic outcomes, and a relatively long follow-up period of 1 year for a novel technique.
Limitations of the study include its retrospective design, data collection from a single center, and lack of complete PROM data on some patients due to patient compliance with data collection. The procedures were performed by 3 surgeons, which can increase variability; however, it also improves the generalizability of results. Another limitation of the study is the lack of a matched cohort who underwent LLIF via the lateral decubitus approach. However, we were able to compare our large cohort to others reported in the literature. In this study, we found no overt difference in either clinical or radiological outcomes and no difference in the complications profiles when comparing PTP to the lateral decubitus position.1,19–27,29
Conclusion
LLIF performed via the PTP approach is a safe and effective method of treating patients with lumbar spine pathology. Performing the procedure in the prone position allows the surgeon to access both the anterior and posterior columns of the spine, and it has a comparable clinical outcomes and complications profile as compared with LLIF performed in the lateral decubitus position. Our study demonstrated improvements in radiographic parameters (LL, SL, ADH, and PDH) and PROMs, which were sustained at 1-year follow-up. Future prospective studies are needed to further evaluate long-term outcomes.
References
- 1. Campbell PG, Nunley PD, Cavanaugh D, et al. Short-term outcomes of lateral lumbar interbody fusion without decompression for the treatment of symptomatic degenerative spondylolisthesis at L4-5. Neurosurg Focus. 2018;44(1):2017.10.FOCUS17566. 10.3171/2017.10.FOCUS17566 [DOI] [PubMed] [Google Scholar]
- 2. McGowan JE, Kanter AS. Lateral approaches for the surgical treatment of lumbar spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):313–322:S1042-3680(19)30018-X. 10.1016/j.nec.2019.02.005 [DOI] [PubMed] [Google Scholar]
- 3. Lehmen JA, Gerber EJ. MIS lateral spine surgery: a systematic literature review of complications, outcomes, and economics. Eur Spine J. 2015;24(S3):287–313. 10.1007/s00586-015-3886-1 [DOI] [PubMed] [Google Scholar]
- 4. Goyal A, Kerezoudis P, Alvi MA, Goncalves S, Bydon M. Outcomes following minimally invasive lateral transpsoas interbody fusion for degenerative low grade lumbar spondylolisthesis: a systematic review. Clin Neurol Neurosurg. 2018;167:122–128. 10.1016/j.clineuro.2018.02.020 [DOI] [PubMed] [Google Scholar]
- 5. Buckland AJ, Ashayeri K, Leon C, et al. Single position circumferential fusion improves operative efficiency, reduces complications and length of stay compared with traditional circumferential fusion. Spine J. 2021;21(5):810–820. 10.1016/j.spinee.2020.11.002 [DOI] [PubMed] [Google Scholar]
- 6. Quiceno E, Hartman C, Godzik J, Pacult MA, Hemphill C, Uribe JS. Single position spinal surgery for the treatment of grade II spondylolisthesis: a technical note. J Clin Neurosci. 2019;65:145–147. 10.1016/j.jocn.2019.03.016 [DOI] [PubMed] [Google Scholar]
- 7. Walker CT, Godzik J, Xu DS, Theodore N, Uribe JS, Chang SW. Minimally invasive single-position lateral interbody fusion with robotic bilateral percutaneous pedicle screw fixation: 2-dimensional operative video. Oper Neurosurg. 2019;16(4):E121–E121. 10.1093/ons/opy240 [DOI] [PubMed] [Google Scholar]
- 8. Ouchida J, Kanemura T, Satake K, Nakashima H, Ishikawa Y, Imagama S. Simultaneous single-position lateral interbody fusion and percutaneous pedicle screw fixation using O-arm-based navigation reduces the occupancy time of the operating room. Eur Spine J. 2020;29(6):1277–1286. 10.1007/s00586-020-06388-6 [DOI] [PubMed] [Google Scholar]
- 9. Ziino C, Konopka JA, Ajiboye RM, Ledesma JB, Koltsov JCB, Cheng I. Single position versus lateral-then-prone positioning for lateral interbody fusion and pedicle screw fixation. J Spine Surg. 2018;4(4):717–724. 10.21037/jss.2018.12.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pimenta L, Taylor WR, Stone LE, Wali AR, Santiago-Dieppa DR. Prone transpsoas technique for simultaneous single-position access to the anterior and posterior lumbar spine. Oper Neurosurg. 2020;20(1):E5–E12. 10.1093/ons/opaa328 [DOI] [PubMed] [Google Scholar]
- 11. Pimenta L, Amaral R, Taylor W, et al. The prone transpsoas technique: preliminary radiographic results of a multicenter experience. Eur Spine J. 2021;30(1):108–113. 10.1007/s00586-020-06471-y [DOI] [PubMed] [Google Scholar]
- 12. NaPier Z. Prone transpsoas lateral interbody fusion (PTP LIF) with anterior docking: preliminary functional and radiographic outcomes. N Am Spine Soc J. 2023;16:100283. 10.1016/j.xnsj.2023.100283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wellington IJ, Antonacci CL, Chaudhary C, et al. Early clinical outcomes of the prone transpsoas lumbar interbody fusion technique. Int J Spine Surg. 2023;17(1):112–121. 10.14444/8390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Walker CT, Farber SH, Gandhi S, Godzik J, Turner JD, Uribe JS. Single-position prone lateral interbody fusion improves segmental lordosis in lumbar spondylolisthesis. World Neurosurg. 2021;151:e786–e792. 10.1016/j.wneu.2021.04.128 [DOI] [PubMed] [Google Scholar]
- 15. Farber SH, Naeem K, Bhargava M, Porter RW. Single-position prone lateral transpsoas approach: early experience and outcomes. J Neurosurg Spine. 2022;36(3):358–365. 10.3171/2021.6.SPINE21420 [DOI] [PubMed] [Google Scholar]
- 16. Farber SH, Valenzuela Cecchi B, O’Neill LK, et al. Complications associated with single-position prone lateral lumbar interbody fusion: a systematic review and pooled analysis. J Neurosurg Spine. 2023;39(3):380–386. 10.3171/2023.4.SPINE221180 [DOI] [PubMed] [Google Scholar]
- 17. Copay AG, Subach BR, Glassman SD, Polly DW, Schuler TC. Understanding the minimum clinically important difference: a review of concepts and methods. Spine J. 2007;7(5):541–546. 10.1016/j.spinee.2007.01.008 [DOI] [PubMed] [Google Scholar]
- 18. Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine. 2005;30(6):682–688. 10.1097/01.brs.0000155425.04536.f7 [DOI] [PubMed] [Google Scholar]
- 19. Issa TZ, Lee Y, Lambrechts MJ, et al. The impact of cage positioning on lumbar lordosis and disc space restoration following minimally invasive lateral lumbar interbody fusion. Neurosurg Focus. 2023;54(1):E7. 10.3171/2022.10.FOCUS22607 [DOI] [PubMed] [Google Scholar]
- 20. Bakare AA, Fessler DR, Wewel JT, Fontes RBV, Fessler RG, O’Toole JE. Changes in segmental and lumbar lordosis after lateral lumbar interbody fusion with different lordotic cage angulations. Int J Spine Surg. 2021;15(3):440–448. 10.14444/8066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Alimi M, Hofstetter CP, Cong G-T, et al. Radiological and clinical outcomes following extreme lateral interbody fusion. SPI. 2014;20(6):623–635. 10.3171/2014.1.SPINE13569 [DOI] [PubMed] [Google Scholar]
- 22. Phillips FM, Isaacs RE, Rodgers WB, et al. Adult degenerative scoliosis treated with XLIF: clinical and radiographical results of a prospective multicenter study with 24-month follow-up. Spine. 2013;38(21):1853–1861. 10.1097/BRS.0b013e3182a43f0b [DOI] [PubMed] [Google Scholar]
- 23. Agarwal N, White MD, Roy S, et al. Long-term durability of stand-alone lateral lumbar interbody fusion. Neurosurgery. 2023;93(1):60–65. 10.1227/neu.0000000000002371 [DOI] [PubMed] [Google Scholar]
- 24. Rodgers WB, Gerber EJ, Patterson J. Intraoperative and early postoperative complications in extreme lateral interbody fusion: an analysis of 600 cases. Spine. 2011;36(1):26–32. 10.1097/BRS.0b013e3181e1040a [DOI] [PubMed] [Google Scholar]
- 25. Kotwal S, Kawaguchi S, Lebl D, et al. Minimally invasive lateral lumbar interbody fusion. J Spinal Disord Tech. 2015;28(4):119–125. 10.1097/BSD.0b013e3182706ce7 [DOI] [PubMed] [Google Scholar]
- 26. Tohmeh AG, Rodgers WB, Peterson MD. Dynamically evoked, discrete-threshold electromyography in the extreme lateral interbody fusion approach. J Neurosurg Spine. 2011;14(1):31–37. 10.3171/2010.9.SPINE09871 [DOI] [PubMed] [Google Scholar]
- 27. Lee Y-P, Regev GJ, Chan J, et al. Evaluation of hip flexion strength following lateral lumbar interbody fusion. Spine J. 2013;13(10):1259–1262. 10.1016/j.spinee.2013.05.031 [DOI] [PubMed] [Google Scholar]
- 28. Hijji FY, Narain AS, Bohl DD, et al. Lateral lumbar interbody fusion: a systematic review of complication rates. Spine J. 2017;17(10):1412–1419. 10.1016/j.spinee.2017.04.022 [DOI] [PubMed] [Google Scholar]
- 29. Nakashima H, Kanemura T, Satake K, et al. Factors affecting postoperative sagittal alignment after lateral lumbar interbody fusion in adult spinal deformity: posterior osteotomy, anterior longitudinal ligament rupture, and endplate injury. Asian Spine J. 2019;13(5):738–745. 10.31616/asj.2018.0275 [DOI] [PMC free article] [PubMed] [Google Scholar]