Abstract
This study explores how mental illness shapes transitions to marriage among unwed mothers using augmented data from the Fragile Families and Child Wellbeing study (N = 2,351). We estimate proportional hazard models to assess the effects of mental illness on the likelihood of marriage over a 5-year period following a nonmarital birth. Diagnosed mental illness was obtained from the survey respondents’ prenatal medical records. We find that mothers with mental illness are about two thirds as likely as mothers without mental illness to marry, even after controlling for demographic characteristics, and that human capital, relationship quality, partner selection, and substance abuse appear to explain only a small proportion of the effect of mental illness on marriage.
Keywords: depression, marriage, mental health
Nonmarital childbearing has increased dramatically in the United States over the past 50 years, with over one third of births today occurring outside of marriage. The rates among poor and minority parents are particularly high. Although many unmarried mothers eventually marry, they do so at a slow rate (Graefe & Lichter, 2002). Concerns about the consequences of this demographic change for children, families, and society have fueled extensive research on determinants of marriage among low-income couples. The predominant focus has been on economic factors such as employment and education. A potential determinant that has been relatively unexplored in this context is mental health, despite evidence that unmarried parents have high rates of mental illness (DeKlyen, Brooks-Gunn, McLanahan, & Knab, 2006; Teitler, Reichman, & Nepomnyaschy, 2004) and there are documented links between mental health and marriage. Most research on mental health and marriage has focused on the effects of marriage on mental health (see Gove, Hughes, & Style, 1983) or the effects of mental illness on relationship quality (see Larson & Holman, 1994) or divorce (see Wade & Pevalin, 2004), but some studies have examined the effects- of mental illness on marriage—the focus of this paper.
Stevens (1969) used panel data on women admitted to a London mental hospital and compared that group to the general population, both pre- and postadmission. She found that schizophrenia decreased the likelihood of being married at the time of hospitalization and of subsequently marrying, but that affective disorders had no association with current or subsequent marriage. Rushing (1979), using cross-sectional data from a Tennessee hospital, found that schizophrenia was negatively associated with being married at the time of hospitalization, particularly for males. Recently, Agerbo, Byrne, Eaton, and Mortensen (2004), using Danish registry data, found that schizophrenia decreased the likelihood that individuals (women or men) entered marital unions over a 25-year period. Studying schizophrenia, although it is a severe disorder and relatively rare, is useful for assessing the direction of causality because it is less likely to be caused by social circumstances than many other mental illnesses, including depression (Dohrenwend et al., 1992). But the effects cannot necessarily be generalized to other mental illnesses.
Bartel and Taubman (1986), using panel data on veterans, examined the effects of psychoses (e.g., schizophrenia), neuroses (e.g., mood disorders), and other mental illnesses on the likelihood of marriage. They found that neuroses that were diagnosed when the individual was young reduced the likelihood of marriage, but that recent diagnoses did not. They found no associations for psychoses or other mental illnesses. Simon (2002) found no evidence that risk for depression, as measured by the Center for Epidemiological Studies Depression Scale, affects transitions to marriage, and Lamb, Lee, and DeMaris (2003) found no evidence that it affects transitions to marriage among individuals who have never cohabited. Forthofer, Kessler, Story, and Gotlib (1996), using national panel data that includes the Composite Interview Diagnostic Instrument (CIDI)—which assesses mental disorders according to the definitions and criteria of International Classification of Diseases-10 and Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV) (Robins et al. 1988)—found that affective disorders (particularly depression) and conduct disorder reduce the likelihood of marriage for both men and women. The authors did not assess the effects of psychoses, which have low rates of sensitivity in the CIDI (Cooper, Peters, & Andrews, 1998).
The evidence from this body of literature suggests that there are large negative effects of schizophrenia, and more modest effects of depression and other mental disorders, on marriage. Several knowledge gaps remain, however. First, the magnitudes of the effects are difficult to ascertain because few studies report effect sizes in terms of risk ratios for mentally ill to not mentally ill. Second, the findings may not apply to unmarried parents. Mental illness may affect nonmarital fertility but not subsequent marriage behavior, or it could compound economic or other hardships associated with unwed parenthood, leading to stronger negative effects on marriage than for the general population. Finally, the mechanisms by which mental illness affects marriage have been neither articulated nor explored.
Prior research suggests several mediators that may be important. The first is human capital: There are demonstrated links between mental illness and educational attainment (Berndt et al., 2000; Currie & Stabile, 2006), mental illness and employment (Ettner, Frank, & Kessler, 1997; Marcotte & Wilcox-Gok, 2001), and human capital and marriage (see Waite & Spitze, 1981). The second is relationship quality: Research on the effects of mental illness on marital disruption (cited earlier), social functioning (Tweed, 1993), and relationships with family (Nicholson, Sweeney, & Geller, 1998) suggests that cognitive deficits or behaviors of individuals with mental illness may adversely affect their ability to communicate effectively, resolve conflicts, or engage in mutually rewarding relationships. A third potential mediator is partner selection: Cognitive deficits associated with some mental illnesses may lead to poor choices of partners and relationships that have poor long-term prospects, or potential mates may be deterred as a result of cognitive deficits, behaviors, or stigma associated with mental illness (Link, Cullen, Frank, & Wozniak, 1987; Phelan, Link, Stueve, & Pescosolido, 2000). Finally, substance abuse, which is highly comorbid with mental illness (Epstein, Barker, Vorburgur, & Murtha, 2004), is a potential mediator: Substance abuse is considered a mental disorder (and is classified as such according to DSM-IV), but it can also be caused by other types of mental illness (Harris & Edlund, 2005) and may have damaging effects on individuals’ lives that affect their prospects for healthy relationships and marriage.
In this study, we advance knowledge about the role of mental illness on marriage by focusing on unmarried mothers (a policy-relevant population at high risk for mental illness), assessing the extent to which mental illness contributes to low rates of marriage in this population and investigating human capital, relationship quality, partner selection, and substance abuse as potential mediators.
Method
We used data from the Fragile Families and Child Wellbeing Study (hereafter, FF), which follows a cohort of parents and their newborn children. Mothers were interviewed in the hospital shortly after giving birth (baseline) and over the telephone 1, 3, and 5 years later. Baseline interviews were conducted with 3,712 unmarried mothers and a comparison group of 1,196 married mothers between 1998 and 2000 (see Reichman, Teitler, Garfinkel, & McLanahan, 2001, for details). Response rates of unmarried mothers were 87% at baseline, 90% at 1 year, 87% at 3 years, and 87% at 5 years. The 3,712 births are representative of nonmarital births in U.S. cities with at least 200,000 people.
Additional data are being collected from the mothers’ and infants’ hospital medical records (from the birth) and, at this time, are available for 3,517 (72%) of the baseline sample (2,714 unmarried, 803 married). The medical records provide rich data on the mothers’ health history, including preexisting mental illness. We are therefore able to establish that the mental illness preceded the birth. However, the timing of onset of mental illness was not available. The analyses are based on the four waves of the FF survey augmented with the medical record data.
Information on mothers’ mental health history, psychiatric medications, and substance abuse or addiction was collected from laboratory test results, notes, and International Classification of Diseases-9 (ICD-9) codes in the medical records. Our primary measure of mental illness excludes drug- and alcohol-related diagnoses because we are interested in the potential mediating effect of substance abuse. Because substance abuse is considered mental illness according to DSM-IV, however, we conducted supplementary analyses with a measure of mental illness that includes substance abuse diagnoses. The main measure of mental illness includes schizophrenia, bipolar disorder, anxiety disorder, eating disorders, depression, and all other nonsubstance abuse DSM-IV mental illness diagnoses.
We focused on mothers who were unmarried at the time of the birth. Our outcome is marriage, either to the baby’s father or to someone else. We used information from the 1-, 3-, and 5-year follow-up interviews to determine marital status of the mother at each month after her baseline interview until her final interview date or until she married. For the 14% of cases for which exact marriage dates were unavailable, we imputed dates on the basis of the mother’s report of her marital status at each wave.
The following demographic characteristics (reported by the mother at baseline), all of which may be associated with mental illness and have been shown in much prior research to be associated with marriage, are included as controls in multivariate analyses: the mother’s race/ethnicity (non-Hispanic Black, Hispanic, and other non-White vs. non-Hispanic White), nativity (U.S.-born vs. foreign-born), number of other children (none vs. one or more), and age (21 – 29 and 30+ years vs. < 21).
As indicated earlier, we explored the mediating role of several sets of factors. To characterize human capital, we included the mother’s education (high school education or equivalent, some college education, and college graduate vs. less than a high school education), physical health status (excellent, very good, or good vs. fair or poor), and employment (whether she was employed at all in the 12 months preceding her 1-year follow-up interview), as well as the following proxies for income, which is a manifestation of human capital: whether the birth was covered by Medicaid (vs. private, other, or no insurance), whether the mother received welfare or food stamps in the 12 months prior to the birth, and whether at least 30% of households in the mother’s census tract had income below the poverty line. Other than employment, all of these measures were based on mothers’ baseline data.
To characterize relationship quality, we included whether the mother was cohabiting with the child’s father at the time of the birth, whether the mother had any children with another father at the time of the birth, the number of months the mother knew the father before the child was conceived (12+ months vs. <12 months), and the number of romantic partners the mother had prior to the child’s father (61 vs. 0 – 5). The cut-offs were based on the distributions in the data.
For quality of partners, we included measures of whether the child’s father was employed or in school, whether the father had ever hit or slapped the mother or often insulted or criticized her, whether the father had ever been in prison or jail (from the mother’s 1-year follow-up interview), whether the father had problems such as keeping a job or getting along with family and friends because of alcohol or drug use, and whether the father had any physical or mental health condition that limited the amount or kind of work he could do. Unless noted otherwise, all measures of relationship quality and partner selection are based on mothers’ reports at baseline.
To measure maternal substance abuse, we combined information from the baseline surveys and the medical records. That information includes having had drug or alcohol problems that interfered with work or personal relationships (from the survey), having been treated for substance use (from the survey), and positive prenatal drug test results, ICD-9 codes for substance abuse, and progress notes indicating substance abuse (from the medical records).
We employed an event history approach to model the effect of mental illness on the likelihood of marriage. Specifically, we estimated Cox proportional hazard models in which duration is measured in months from the child’s birth. All mothers who reported that they were unmarried at baseline and completed 1-year follow-up interviews are included, whether or not they completed subsequent follow-up interviews. Individuals who did not marry during the observation period are right-censored at the time of their last interview. The proportional hazard models were estimated with Stata version 9.0 (StataCorp., 2005). We employed the commonly used Breslow approximation method to handle ties (marriages that occur in the same month), a technique that is appropriate when events are rare relative to the size of the at-risk sample. In our case, this assumption is valid because less than 1% of the sample married in any given month. We tested the sensitivity of our results to various sample restrictions and an alternative measure of mental illness.
By using panel data, we are confident that mental illness preceded marriage if one took place. Advantages of using event history analysis are that we do not have to choose an arbitrary time point at which to assess marital status and can include data from respondents regardless of how long they stayed in the study. Our analysis strategy does not entirely address the possibility that, even with the rich FF data, there are unmeasured variables associated with both mental illness and marriage (unobserved heterogeneity). We addressed this possibility indirectly in supplementary analyses that distinguish between mental illnesses that may be socially triggered and those that are unlikely to have social causes.
We estimated six models: Model 1 includes no covariates and therefore measures the unconditional (total) association between mental illness and marriage. Model 2 measures the association between mental illness and marriage net of demographic characteristics. The next four models, all of which control for demographic characteristics, explore the role of the potential mediators described above: Model 3 includes measures of the mother’s human capital, Model 4 includes measures of the parents’ relationship quality, Model 5 includes attributes of the father (to test for the potential mediating role of partner selection), and Model 6 includes maternal substance abuse.
Of the 3,710 mothers that were unmarried at baseline, we excluded 417 (11%) for whom 1-year follow-up interviews were not completed, 930 (25%) for whom medical record data were not available, and 12 (<1%) because of missing data on variables for which fewer than 3% of cases had missing values. These exclusions resulted in a sample of 2,351 cases. For variables that had missing values for more than 3% of observations (maternal employment, length of parents’ relationship, number of mother’s previous romantic relationships, all of the father variables, and census-tract poverty), we used dummy variables for missing data in order to minimize sample loss.
Results
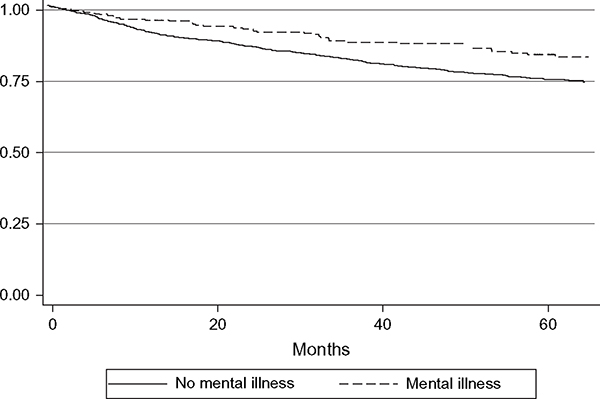
Figure 1 shows transitions to marriage among mothers with and without preexisting diagnosed mental illness over a period of 5.5 years. It plots the Kaplan-Meier nonparametric estimates of the survivor function (the probability of remaining unmarried) at each month and indicates that mothers with mental illness were less likely than those without mental illness to marry at any time over the observation period. By 1 year after giving birth, 10% of the mothers without mental illness had married, compared to 5% of the mothers with mental illness. By 5 years, the respective figures were 26% and 16%, that is, mothers with mental illness were about 40% less likely to have married.
Figure 1.
Proportion Remaining Unmarried 0 – 65 Months After Giving Birth (Kaplan-Meier Survival Estimates, N = 2,351).
Table 1 shows characteristics of the sample by mothers’ mental illness status. Mothers with preexisting mental illness were more likely to be non-Hispanic White, less likely to be Hispanic, less likely to be foreign born, more likely to have had previous births, and older at the time of the birth than mothers without preexisting mental illness, although many of the differences are not substantial. With the exception of race/ethnicity, the demographic characteristics that previous research indicates are positively associated with marriage are negatively associated with mental illness.
Table 1.
Sample Characteristics by Mental Illness, Percentages (N = 2,351)
| Mental Illness (n = 292) | No Mental Illness (n = 2,059) | |
|---|---|---|
|
| ||
| Demographics | ||
| Non-Hispanic White*** | 22 | 12 |
| Non-Hispanic Black | 57 | 56 |
| Hispanic*** | 17 | 29 |
| Other non-White | 4 | 3 |
| Born in United States*** | 94 | 87 |
| First birth** | 32 | 39 |
| Age <21 years** | 30 | 37 |
| Age 21 – 29 years | 46 | 51 |
| Age 30+ years*** | 24 | 12 |
| Human capital | ||
| Less than high school*** | 53 | 40 |
| High school graduate | 30 | 34 |
| Some college*** | 16 | 23 |
| College graduate | 1 | 3 |
| Good, very good, or excellent health*** | 83 | 92 |
| Employed*** | 69 | 77 |
| Medicaid birth*** | 85 | 75 |
| Received welfare or food stamps*** | 57 | 44 |
| 30+% poor in census tract** | 28 | 23 |
| Relationship stability | ||
| Cohabiting with father at baseline** | 41 | 49 |
| Any children with another father*** | 51 | 40 |
| Knew father 12+ months | 83 | 80 |
| 6+ romantic relationships before father | 6 | 4 |
| Partner selection | ||
| Father unemployed and not in school** | 18 | 12 |
| Father has activity-limiting physical or mental health condition*** | 10 | 6 |
| Father ever in jail*** | 49 | 36 |
| Father hit/slapped or insults/criticizes mother*** | 8 | 4 |
| Father abuses alcohol or drugs*** | 13 | 5 |
| Behavior | ||
| Mother has substance abuse problem*** | 44 | 11 |
p < .05.
p < .01 (based on chi-square tests for equal proportions).
Although the differences in demographic profiles of mothers with and without mental illness are unremarkable, the two groups differ substantially in terms of human capital, relationships, father characteristics, and maternal substance abuse. Mothers with mental illness were more likely than mothers without mental illness to have suboptimal physical health (17% vs. 8%) and low levels of education (e.g., 53% of mothers with mental illness had less than a high school education, compared to 40% of those without mental illness). They were less likely to have been employed (69% vs. 77%), more likely to have been covered by Medicaid for the birth (85% vs. 75%), more likely to have received welfare or food stamps at baseline (57% vs. 44%), and more likely to have lived in a poor neighborhood (28% vs. 23%). They were less likely to have cohabited with the father at baseline (41% vs. 49%) and more likely to have had children with another father (51% vs. 40%). There are no significant differences in the length of time the mother knew the father before conception of the focal child or the number of previous romantic partners. Mothers with mental illness were more likely than those without mental illness to report at baseline that the father was not employed or in school (18% vs. 12%), that they have been abused by the child’s father (8% vs. 4%), that the father had ever been in prison or jail (49% vs. 36%), that the father had substance abuse problems (13% vs. 5%), and that the father had an activity-limiting physical or mental health condition (10% vs. 6%). Finally, mothers with mental illness were 4 times more likely than mothers without mental illness to have substance use problems (44% vs. 11%).
Table 2 presents the proportional hazard results. The hazard ratio for diagnosed mental illness (other than substance abuse diagnoses) in the first model is .599, indicating that mothers with mental illness are 60% as likely as mothers without mental illness to marry in any given month, conditional on still being unmarried the previous month. Because Model 1 includes no covariates, this estimate is similar to the ratio of marriage rates at the 5-year mark as shown in Figure 1. Adding the demographic measures in Model 2, the estimated effect of mental illness remains virtually unchanged from that in Model 1. Among the demographic characteristics, the strongest predictor of marriage is race/ethnicity.
Table 2.
Effects of Mental Illness on Marriage (N = 2,351)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |
|---|---|---|---|---|---|---|
|
| ||||||
| Mental illness | 0.599** (.001) | 0.571** (.001) | 0.628** (.005) | 0.598** (.002) | 0.630** (.005) | 0.608** (.003) |
| Non-Hispanic Black | 0.412** (.000) | 0.451** (.000) | 0.487** (.000) | 0.424** (.000) | 0.412** (.000) | |
| Hispanic | 0.752* (.033) | 0.850 (.235) | 0.800 (.098) | 0.749* (.033) | 0.750 (.033) | |
| Other non-White | 0.773 (.332) | 0.760 (.304) | 0.881 (.635) | 0.727 (.232) | 0.770 (.326) | |
| Bom in United States | 0.858 (.273) | 0.818 (.166) | 0.966 (.806) | 0.947 (.702) | 0.877 (.353) | |
| First birth | 1.044 (.659) | 0.905 (.330) | 1.138 (.312) | 1.028 (.776) | 1.044 (.658) | |
| Age 21 – 29 years | 1.133 (.227) | 0.977 (.831) | 1.111 (.311) | 1.085 (.434) | 1.131 (.236) | |
| Age 30+ years | 1.202 (.222) | 0.946 (.724) | 1.213 (.207) | 1.095 (.550) | 1.213 (.199) | |
| High school graduate | 1.198 (.109) | |||||
| Some college | 1.486** (.002) | |||||
| College graduate | 2.593** (.000) | |||||
| Good, very good, or excellent health | 0.945 (.725) | |||||
| Employed | 0.966 (.760) | |||||
| Medicaid birth | 0.919 (.431) | |||||
| Received welfare or food stamps | 0.902 (.295) | |||||
| 30+% poor in census tract | 0.762* (.029) | |||||
| Cohabiting with father at baseline | 2.004** (.000) | |||||
| Any children with another father | 1.048 (.706) | |||||
| Knew father 12+ months | 0.809 (.059) | |||||
| 6+ romantic relationships before father | 0.864 (.527) | |||||
| Father unemployed and not in school | 1.602* (.013) | |||||
| Father has activity-limiting physical or mental condition | 0.783 (.271) | |||||
| Father ever in jail | 0.748** (.004) | |||||
| Father hit/slapped or insults/criticizes mother | 1.120 (.625) | |||||
| Father abuses alcohol or dmgs | 0.725 (.185) | |||||
| Mother has substance abuse problem | 0.804 (.133) | |||||
| Log likelihood | −3844 | −3807 | −3788 | −3774 | −3778 | −3806 |
Results presented are proportional hazard ratios (p values in parentheses).
p < .10.
p < .05.
Model 3, which includes measures of the mother’s human capital as potential mediators, indicates that low education and poor neighborhoods are negatively associated with marriage. None of the other measures of human capital is a statistically significant independent predictor of marriage. Together, the measures of human capital account for some of the effect of mental illness on marriage (they increase the hazard ratio for mental illness by 5.7 percentage points, from .571 to .628).
From Model 4 we find that the measures of relationship quality explain little of the association between mental illness and marriage (the hazard ratio for mental illness is .598 compared to .571 in Model 2). Of this set of measures, only baseline cohabitation is independently predictive of marriage. Although baseline cohabitation rates varied significantly by mental illness (Table 1), the mental illness-cohabitation link is not sufficiently strong to explain the association between mental illness and marriage. The results from Model 5 indicate that, although many father attributes are associated with marriage, they, too, account for only some of the association between mental illness and marriage—about the same proportion that was explained by the measures of human capital. That is, most of the effect of mental illness on marriage does not appear to be due to mentally ill mothers choosing or attracting partners who possess traits that mark them as unsuitable as husbands. Finally, Model 6 indicates that substance abuse explains very little of the association between mental illness and marriage (the hazard ratio for mental illness is .608 compared to .571 in Model 2).
Overall, the proportional hazard results indicate that, although the hypothesized mediators (human capital, relationship quality, partner selection, and substance abuse) explain some of the mental illness effect on marriage, most of the effect remains unexplained. When all sets of potential mediators were included together (not shown), they accounted for somewhat more of the mental illness effect than any one set did; however, most still remained unexplained (the estimated hazard ratio of mental illness in a model with all covariates included was .69, which was statistically significant at p < .05).
We conducted two model specification tests (results not shown in table). The first, the link test, regresses the outcome on the linear predictor from the original regression estimates and the squared linear predictor. A statistically significant estimate of the squared term is an indication of model misspecification. In our case, the p value of the squared term was insignificant (p > .30). The other test, the Schoenfeld residual test, indicated that the effects of all but one variable (older maternal age) were constant over time. Eliminating age from the model did not affect the estimate or significance of mental illness. For mental illness, our main analysis variable, the p value from the Schoenfeld test that the residuals were associated with time was greater than .50.
To further explore our results and assess robustness, we estimated supplemental sets of models with specific sample restrictions or using an alternative measure of mental illness (results not shown). First, we considered that mothers with diagnosed mental health problems that require ongoing treatment may be reluctant to marry for fear of losing Medicaid benefits. To test this, we stratified the sample by whether the birth was covered by Medicaid and reestimated the models in Table 2. The findings for both subgroups were very similar to those for the full sample, suggesting that Medicaid eligibility does not explain the effect of mental illness on marriage. Second, we excluded cases with missing data indicators and found that the results were insensitive to this sample restriction. Third, we ran a set of models using a measure of mental illness that included substance abuse diagnoses (from the medical records) and, again, found that the results were very similar to those in Table 2.
To investigate whether the estimated associations between mental illness and marriage appear to be causal, we ran a set of models with a measure of mental illness that incorporated information from the survey in addition to the medical records (results not shown). Although the medical records data are very valuable for picking up cases with a large range of diagnosed mental illnesses (including rare diagnoses such as schizophrenia) and for differentiating between diagnosed substance abuse and non-substance-abuse disorders, they are limited in terms of isolating specific non-substance-abuse diagnoses. However, by augmenting these data with CIDI-based diagnoses from the 1-year follow-up interview, we were able to differentiate between mothers with depression (with or without other mental illnesses), those with mental illness other than depression, and those without mental illness. Comparing effects across these groups allows us to explore the causal mechanism as, among women, depression is more likely than other types of mental illness to be caused by social circumstances (Dohrenwend et al., 1992). We coded respondents as depressed if they had a diagnosis of mental illness (not related to substance abuse) from the medical records and a diagnosis of depression during the past 12 months according to the CIDI. We coded them as having another mental illness if they had a diagnosed mental illness (not related to substance abuse) according to the medical records but did not have depression during the past 12 months according to the CIDI. Both of these groups are compared to those who did not have any non-substance-abuse mental illness diagnoses indicated in their medical records. We found that the effects of mental illnesses other than depression were as large are those of depression, suggesting that the association is not solely attributable to omitted “social” factors.
We also explored the potential mediating roles of mother’s cognitive ability, the mother’s impulsivity, and the father’s impulsivity (results not shown). For the mother’s cognitive ability and impulsivity, we added relevant measures that were available from the 3-year mother interview, separately, to the model with demographic characteristics (Model 2). For the father’s impulsivity, we added a relevant measure from the 1-year father interview to the partner selection model (Model 5). We found that the measures of mothers’ cognitive ability and impulsivity explained some of the mental illness effect (father’s impulsivity did not), but that adding the additional mother measures to a “full” model that included these measures in addition to demographics, human capital, relationship quality, partner selection, and substance abuse did not change the estimated effect of mental illness in that model (the hazard ratio remained at .69).
Finally, we considered another potential explanation—that rather than limiting opportunities or imposing constraints, mental illness alters individuals’ intentions to marry or tastes for marriage. To test this, we estimated models that included the demographic measures from Model 2 plus a measure from the mother’s baseline report of how likely it was that she would marry anyone in the future (a “pretty good” or “almost certain” chance vs. “no chance,” “a little chance,” or “a 50 – 50 chance”). We found that marriage expectations do explain some of the mental illness effect. Including this measure increased the mental illness hazard ratio to .67 (from .57), and it remained statistically significant (not shown in tables).
Conclusions
Using data from a recent birth cohort study, we produced population-based estimates of the effects of mental illness on marriage among unmarried mothers—a group of much research and policy interest—over a 5-year period following the birth of a child. We found that mothers with preexisting diagnosed mental illness are 43% less likely than mothers without mental illness to marry, even after controlling for demographic characteristics. To the extent that it is possible to compare this figure with findings from previous studies, it appears to be in line with estimates for the overall population. Two facts suggest that the association is causal: The mental illness diagnoses preceded the observation period, and the effects are not confined to depression diagnoses (i.e., they exist also for mental illnesses that are less likely to be socially determined).
Our findings are subject to certain limitations. We used a strict definition of mental illness—diagnosed conditions that were recorded in the mother’s hospital medical record prior to the birth. To the extent that there are undiagnosed cases of mental illness, our effects would be underestimated. We could not disaggregate specific diagnoses, so it is possible that some types of mental illness have much larger effects than our estimates suggest and that others have no effect. More research is needed to explore the effects of specific types of mental illness. Measures of the hypothesized mechanisms are limited in the data, so our investigation of potential mediators should be considered preliminary. Also because of data limitations, we were unable to test other possible mechanisms such as poor executive functioning, which is a symptom of many types of mental illness (Nelson, Sax, & Strakowski, 1998; Schillerstrom, 2001) and associated with life course trajectories (e.g., Bandura, 2001; Hitlin & Elder, 2007). Another possibility that we were unable to explore is that the stigma of mental illness negatively affects individuals’ perceptions of themselves as being marriage worthy (Link, 1987; Link, Cullen, Struening, Shrout, & Dohrenwend, 1989).
Whether our estimated effects should be considered large or small large depends on whether one is interested in the effect of mental illness on the likelihood that an individual unmarried mother will marry or the importance of mental illness as a barrier to marriage among the population of unmarried mothers. From the first vantage point, the effects are substantial. As a barrier to marriage, however, mental illness appears to play a very small role, because marriage rates are very low in this population (even among mothers without mental illness) and because the prevalence of mental illness is not high (even in this high-risk population). In other words, improving the treatment of mental illness (or even eradicating it) would have little impact on marriage rates of unmarried parents.
Our more novel finding concerns how mental illness affects marriage. We tested highly plausible mechanisms that we categorized broadly as human capital, relationships, partner selection, and behavior. Our findings suggest that none of these explanations accounts for much of the mental illness effect. Even combined, all of the potential mediators we considered fell short, leading us to conclude that either there are other important and as-of-yet unexplored factors at play (e.g., decision-making ability or self-image) or that the factors we investigated are important through complex interactions (e.g., relationships may moderate effects of mental illness). Our finding that mental illness appears to affect tastes for marriage should also be further explored. More generally, our findings underscore the need to broaden research on the determinants of marriage and possibly other relationship types to include individuals’ thought processes—a direction that has been taken in qualitative studies of marriage and cohabitation and could be extended to national surveys.
Acknowledgments
This research was supported by Grant R01-HD-35301 from the National Institute of Child Health and Human Development and Grant 005324 from the National Poverty Center at the University of Michigan. The authors are grateful to Ofira Schwartz-Soicher for valuable research assistance.
Contributor Information
Julien O. Teitler, Columbia University
Nancy E. Reichman, Robert Wood Johnson Medical School.
References
- Agerbo E, Byrne M, Eaton WW, & Mortensen PB (2004). Marital and labor market status in the long run in schizophrenia. Archives of General Psychiatry, 61, 28 – 33. [DOI] [PubMed] [Google Scholar]
- Bartel A, & Taubman P (1986). Some economic and demographic consequences of mental illness. Journal of Labor Economics, 4, 243 – 256. [Google Scholar]
- Bandura A (2001). Social cognitive theory: An agentic perspective. Annual Review of Psychology, 52, 1 – 26. [DOI] [PubMed] [Google Scholar]
- Berndt ER, Koran LM, Finkelstein SN, Gelenberg AJ, Kornstein SG, Miller IM, et al. (2000). Lost human capital from early-onset chronic depression. American Journal of Psychiatry, 157, 940 – 947. [DOI] [PubMed] [Google Scholar]
- Cooper L, Peters L, & Andrews G (1998). Validity of the composite International Diagnostic Interview (CIDI) Psychosis Module in a psychiatric setting. Journal of Psychiatric Research, 32, 361 – 368. [DOI] [PubMed] [Google Scholar]
- Currie J, & Stabile M (2006). Child mental health and human capital accumulation: The case of ADHD. Journal of Health Economics, 25, 1094 – 1118. [DOI] [PubMed] [Google Scholar]
- DeKlyen M, Brooks-Gunn J, McLanahan S, & Knab J (2006). The mental health of married, cohabiting, and non-coresident parents with infants. American Journal of Public Health, 96, 1836 – 1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dohrenwend BP, Levav I, Shrout PE, Schwartz S, Naveh G, Link BG, et al. (1992). Socioeconomic status and psychiatric disorders: The causation-selection issue. Science, 255, 946– 952. [DOI] [PubMed] [Google Scholar]
- Epstein J, Barker P, Vorburgur M, & Murtha C (2004). Serious mental illness and its co-occurrence with substance use disorders, 2002. DHHS publication No. SMA 04–3905, Analytic Series A-24. Rockville, MD: Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Ettner S, Frank RG, & Kessler RC (1997). The impact of psychiatric disorders on labor market outcomes. Industrial and Labor Relations Review, 51, 64 – 81. [Google Scholar]
- Forthofer MS, Kessler RC, Story AL, & Gotlib IH (1996). The effects of psychiatric disorders on the probability and timing of first marriage. Journal of Health and Social Behavior, 37, 121 – 132. [PubMed] [Google Scholar]
- Gove WR, Hughes M, & Style CB (1983). Does marriage have positive effects on the psychological well-being of the individual? Journal of Health and Social Behavior, 24, 122 – 131. [PubMed] [Google Scholar]
- Graefe DR, & Lichter DT (2002). Marriage among unwed mothers: Whites, blacks and Hispanics compared. Perspectives on Sexual and Reproductive Health, 34, 286 – 293. [PubMed] [Google Scholar]
- Harris KM, & Edlund MJ (2005). Self-medication of mental health problems: New evidence from a national survey. Health Services Research, 40, 117 – 137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hitlin S, & Elder GH (2007). Agency: An empirical model of an abstract concept. In Macmillan R (Ed.), Advances in life course research (vol. 11, pp. 33 – 67). Amsterdam: Elsevier/JAI Press. [Google Scholar]
- Lamb KA, Lee GR, & DeMaris A (2003). Union formation and depression: Selection and relationship effects. Journal of Marriage and Family, 65, 953 – 962. [Google Scholar]
- Larson JH, & Holman TB (1994). Premarital predictors of marital quality and stability. Family Relations, 43, 228 – 237. [Google Scholar]
- Link BG 1987. Understanding labeling effects in the area of mental disorders: An empirical assessment of the effects of expectations of rejection. American Sociological Review, 52, 96 – 112. [Google Scholar]
- Link BG, Cullen FT, Frank J, & Wozniak JF (1987). The social rejection of former mental patients: Understanding why labels matter. American Journal of Sociology, 92, 1461 – 1500. [Google Scholar]
- Link BG, Cullen FT, Struening E, Shrout PE, & Dohrenwend BP (1989). A modified labeling theory approach to mental disorders: An empirical assessment. American Sociological Review, 54, 400 – 423. [Google Scholar]
- Marcotte DE, & Wilcox-Gok V (2001). Estimating the employment and earnings costs of mental illness: Recent developments in the United States. Social Science and Medicine, 53, 21 – 27. [DOI] [PubMed] [Google Scholar]
- Nelson EB, Sax KW, & Strakowski SM (1998). Attention performance in patients with psychotic and nonpsychotic major depression and schizophrenia. American Journal of Psychiatry, 155, 137 – 139. [DOI] [PubMed] [Google Scholar]
- Nicholson J, Sweeney EM, & Geller JL (1998). Focus on women: Mothers with mental illness: II. Family relationships and the context of parenting. Psychiatric Services, 49, 643 – 649. [DOI] [PubMed] [Google Scholar]
- Phelan JC, Link BG, Stueve A, & Pescosolido BA (2000). Public conceptions of mental illness in 1950 and 1996: What is mental illness and is it to be feared? Journal of Health and Social Behavior, 41, 188 – 207. [Google Scholar]
- Reichman NE, Teitler JO, Garfinkel I, & McLanahan S (2001). Fragile Families: Sample and design. Children and Youth Services Review, 23, 303 – 326. [Google Scholar]
- Robins LN, Wing JK, Wittchen HU, Helzer JE, Burke J, Farmer A, et al. (1988). The Composite International Diagnostic Interview: An epidemiologic instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Archives of General Psychiatry, 45, 1069 – 1077. [DOI] [PubMed] [Google Scholar]
- Rushing WA (1979). Marital status and mental disorder: Evidence in favor of a behavioral model. Social Forces, 58, 540 – 556. [Google Scholar]
- Schillerstrom J (2001). Executive control function in psychiatric and medical illness. Journal of Psychiatric Practice, 8, 160 – 169. [DOI] [PubMed] [Google Scholar]
- Simon RW (2002). Revisiting the relationships among gender, marital status, and mental health. American Journal of Sociology, 107, 1065 – 1096. [DOI] [PubMed] [Google Scholar]
- StataCorp (2005). Stata Statistical Software: Release 9. College Station, TX: StataCorp LP. [Google Scholar]
- Stevens BC (1969). Probability of marriage and fertility of women suffering from schizophrenia or affective disorders. Population Studies, 23, 435 – 454. [DOI] [PubMed] [Google Scholar]
- Teitler JO, Reichman NE, & Nepomnyaschy L (2004). Sources of support, child care, and hardship among unwed mothers, 1999 – 2001. Social Service Review, 78, 125 – 148. [Google Scholar]
- Tweed DL (1993). Depression-related impairment: Estimating concurrent and lingering effects. Psychological Medicine, 23, 373 – 386. [DOI] [PubMed] [Google Scholar]
- Wade TJ, & Pevalin DJ (2004). Marital transitions and mental health. Journal of Health and Social Behavior, 45, 155 – 170. [DOI] [PubMed] [Google Scholar]
- Waite LJ, & Spitze GD (1981). Young women’s transition to marriage. Demography, 18, 681 – 694. [PubMed] [Google Scholar]